AFRS review Pathogenesis Underling or acquired hypersensitivity to






- Slides: 12
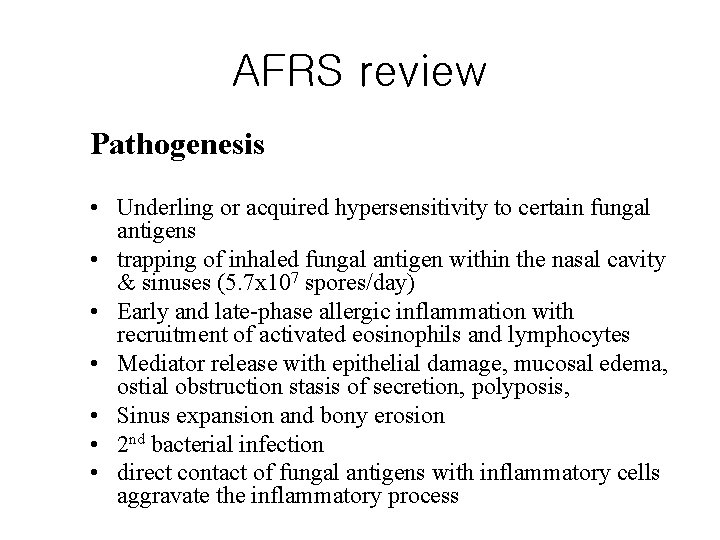
AFRS review Pathogenesis • Underling or acquired hypersensitivity to certain fungal antigens • trapping of inhaled fungal antigen within the nasal cavity & sinuses (5. 7 x 107 spores/day) • Early and late-phase allergic inflammation with recruitment of activated eosinophils and lymphocytes • Mediator release with epithelial damage, mucosal edema, ostial obstruction stasis of secretion, polyposis, • Sinus expansion and bony erosion • 2 nd bacterial infection • direct contact of fungal antigens with inflammatory cells aggravate the inflammatory process
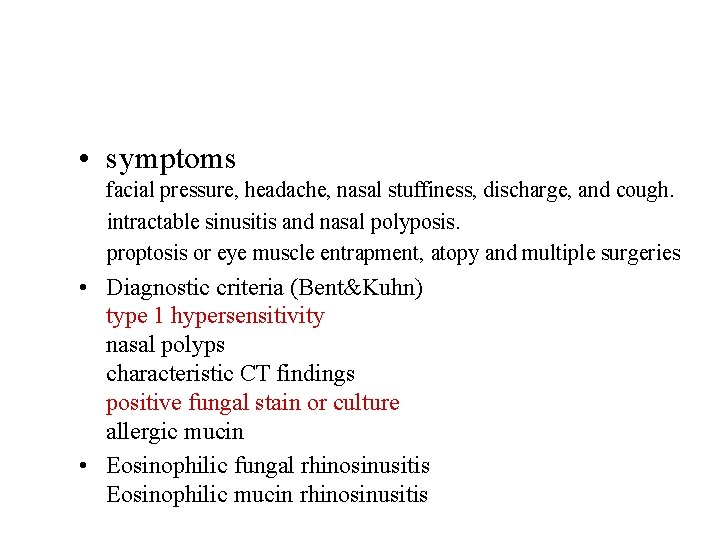
• symptoms facial pressure, headache, nasal stuffiness, discharge, and cough. intractable sinusitis and nasal polyposis. proptosis or eye muscle entrapment, atopy and multiple surgeries • Diagnostic criteria (Bent&Kuhn) type 1 hypersensitivity nasal polyps characteristic CT findings positive fungal stain or culture allergic mucin • Eosinophilic fungal rhinosinusitis Eosinophilic mucin rhinosinusitis


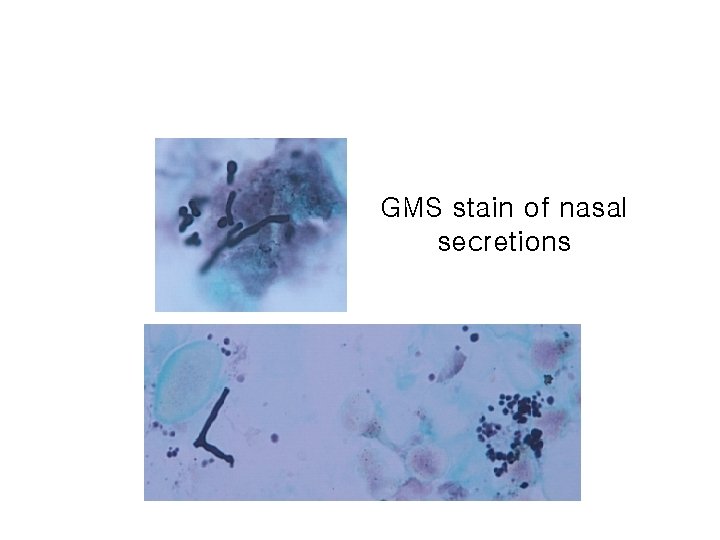
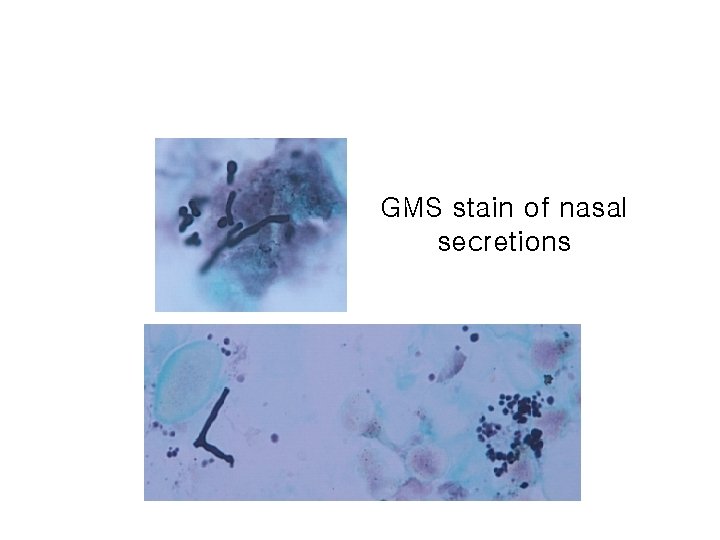
GMS stain of nasal secretions

• Treatment of choice generally is surgery Systemic steroids may be indicated: prednisone (0. 5 mg/kg) Topical nasal steroids are helpful postoperatively. Aggressive nasal salt-water washes are recommended. Immune therapy for specific allergens is controversial

AFRS cycle Saline irrigation surgery Inhaled fungus Proliferation Antigen exposure Stasis of secretion Decreased ventilation & drainage Genetic predisposition (atopy) Type I & III reaction Anatomic obstruction Bacterial sinusitis Mast cell & eosinophil degranulation Immune complex formation? Mucosal edema & inflammation Immunotherapy steroid

Hypothetic pathogenesis of EFRS • Underling or acquired hypersensitivity to certain fungal antigens • trapping of inhaled fungal antigen within the nasal cavity & sinuses • direct contact of fungal antigens with epithelial cells and release cytokine (TSLP, IL-6, IL-8, GMCSF, etc) • Activated dendritic cells & T- lymphocytes polarization • Increase tissue eosinophils and phagocytic activity • eosinophil migrate to nasal and sinus cavity to attack fungal elements and release granule protein • mucosal epithelial cells damage with mucosal edema, ostial obstruction, polyposis • direct contact of fungal antigens with inflammatory

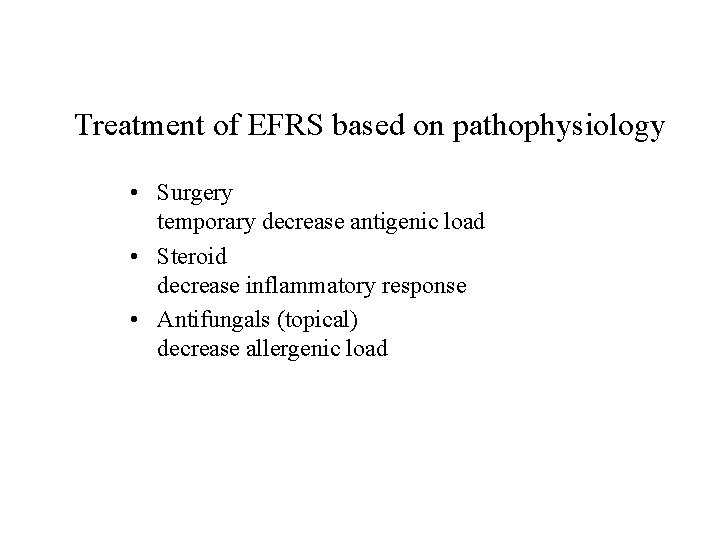
Treatment of EFRS based on pathophysiology • Surgery temporary decrease antigenic load • Steroid decrease inflammatory response • Antifungals (topical) decrease allergenic load