Affection of third eyelid ANATOMY AND PHYSIOLOGY The

- Slides: 29
Affection of third eyelid
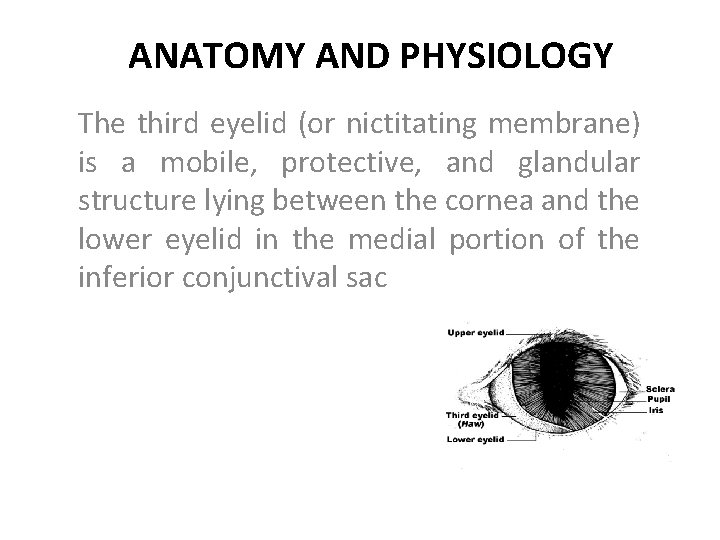
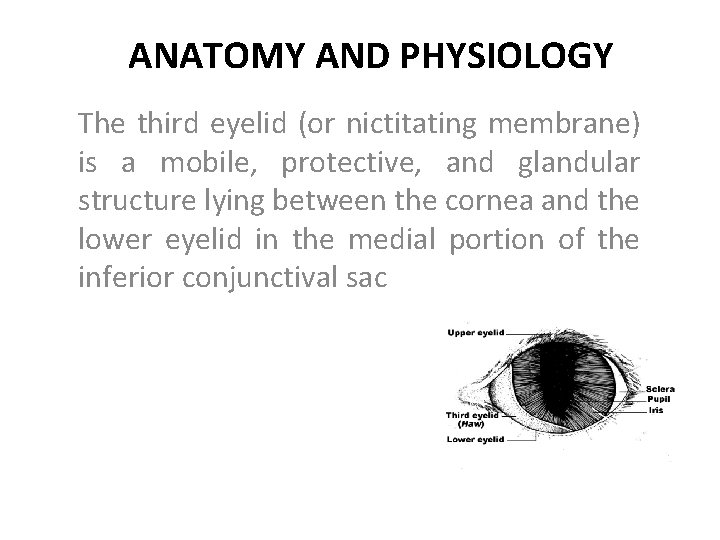
ANATOMY AND PHYSIOLOGY The third eyelid (or nictitating membrane) is a mobile, protective, and glandular structure lying between the cornea and the lower eyelid in the medial portion of the inferior conjunctival sac
The third eyelid consists of the following: • A T-shaped cartilaginous “skeleton” • The gland of the third eyelid • Conjunctiva covering the bulbar and palpebral surfaces • Numerous superficial lymphoid follicles under the bulbar surface
Important functions: • Distribution of the precorneal tear film • Protection of the cornea • Production of aqueous and immunoglobulin for the tear film (in domestic mammals)
• Removal of the third eyelid or its gland predisposes to the following problems: • Increased corneal exposure, drying of the cornea, • Corneal trauma and chronic keratitis • A chronic conjunctivitis that is often purulent and frequently resistant to treatment • Decreased tear production
EXAMINATION • The clinician can easily examine the palpebral surface of the third eyelid by digitally retropulsing the globe through the upper lid. • The bulbar surface is examined after application of topical anesthesia and the use of forceps or mosquito hemostats to grasp the leading edge of the third eyelid just outside the horizontal arm of the cartilage. • The membrane can then be reflected to examine the bulbar surface and the space between the third eyelid and the globe
• This is a common site foreign bodies to become lodged. The bulbar surface is normally follicular and may become more so with so called follicular conjunctivitis. • Perhaps the most common abnormality of the third eyelid noted during an ocular examination is unusual prominence. • Prominence of the third eyelid can also indicate other orbital, neurologic, or ocular diseases, (include the following) • Horner’s syndrome (sympathetic denervation) • Third eyelid protrusion (or “haws”) syndrome • Space-occupying orbital lesions that push the membrane across the eye from its base
• With a small globe due to microphthalmos or phthisis bulbi • With enophthalmos due to active retraction of the globe in painful ocular conditions or due to loss of orbital contents as in dehydration, atrophy, or fibrosis • With tetanus, especially in large animals • Tranquilization (e. g. , with acetylpromazine)
DISEASES OF THE THIRD EYELID • Because third eyelid has two surfaces of conjunctiva and is intimately associated and confluent with the rest of the conjunctiva, it is predictably involved in many conjunctival disorders.
Amelanotic Leading Edge of the Third Eyelid • Congenital absence of melanin on the free or leading edge of the third eyelid in some individuals reveals normal, well-vascularized conjunctiva, which is frequently mistaken by owners or breeders for third eyelid protrusion or inflammation. • This appearance is not abnormal, however, and does not require surgical correction
• When such eyes become inflamed for other reasons, the amelanotic third eyelid may appear more visible because the conjunctival vasculature is not obscured by pigment. • eyelids are presumed to be at higher risk for solar-induced neoplasms, such as hemangioma, hemangiosarcoma, and squamous cell carcinoma
Eversion or Scrolling of the Third Eyelid • Eversion of the third eyelid or “scrolled third eyelid” refers to rolling out of the margin of the membrane due to abnormal curvature of the vertical portion of the T-shaped cartilage • This condition may be unilateral or bilateral, • Most commonly seen in young dogs • it occasionally develops in middle-aged dogs. • It is common in Weimaraners, Saint Bernards, Newfoundlands, Great Danes, German shorthaired pointers, and Irish settersbeen • Injuries and improper suturing of the third eyelid may also result in eversion
• The condition develops because of the bending of the cartilage during growing period. Symptoms: There is increased visibility of the membrane. Watery to Mucoid discharge. Close examination reveals the deformity of the cartilage (inversion or eversion) • Associated with the conjunctivitis in long standing cases. • •
• Treatment: • Surgical excision of the bend area of the cartilage is done under general anaesthesia. • Incision closure is normally not required. • ·If required (normally when the gland is exposed), closure of the wound is done by using 4 -0 to 6 -0 chromic catgut/nylon/Vicryl applying simple continuous pattern. • Postoperatively install topical antibiotics with corticosteroids for 5 -7 days.
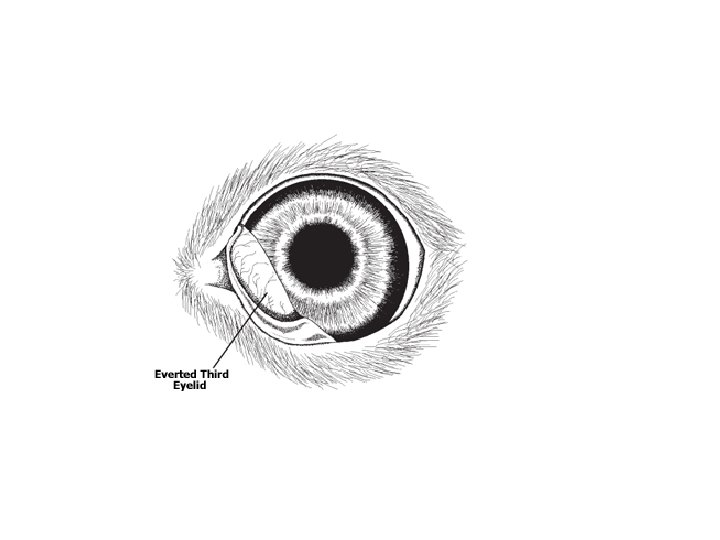
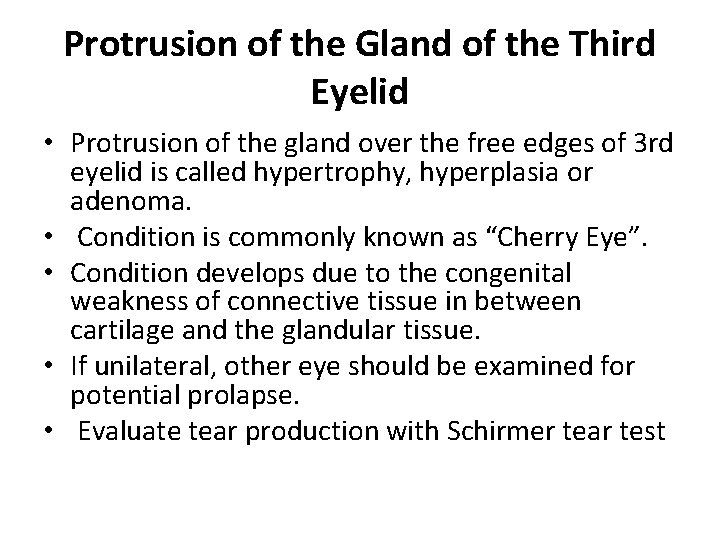
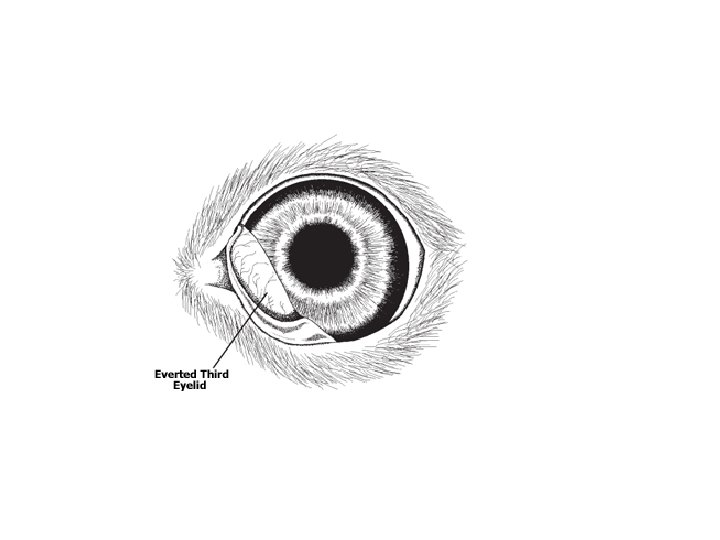
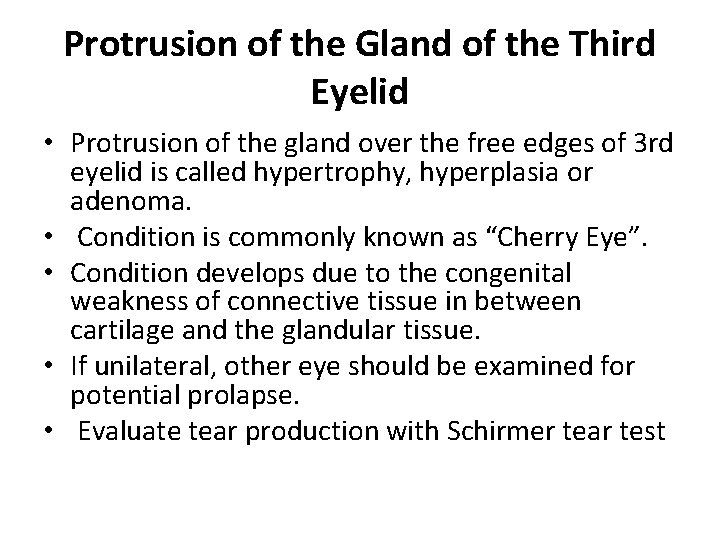
Protrusion of the Gland of the Third Eyelid • Protrusion of the gland over the free edges of 3 rd eyelid is called hypertrophy, hyperplasia or adenoma. • Condition is commonly known as “Cherry Eye”. • Condition develops due to the congenital weakness of connective tissue in between cartilage and the glandular tissue. • If unilateral, other eye should be examined for potential prolapse. • Evaluate tear production with Schirmer tear test
• most commonly in dogs and occasionally in cats. • The appearance is characteristic, with the gland of the third eyelid protruding as a reddish follicular mass from behind a usually “floppy” margin of the third eyelid • Genetically predisposed, especially brachycephalic
• Studies confirm clinical experience that keratoconjunctivitis sicca is commonly seen, often years later, in animals, especially those of susceptible breeds in which the third eyelid or its gland was removed. • Also, complications have been reported in prolapsed glands left in the prolapsed position
Treatment: • The gland should be surgically replaced to retain essential lacrimal function and to prevent the exposed gland overlying conjunctiva from becoming dry, inflamed, secondarily infected, and cosmetically unappealing. • Prolapsed glands of the third eyelid should never be removed because the gland of the third eyelid is a significant contributor to precorneal tear film production. • Alternately, if the above procedure fails, surgical removal of the gland is done. • • Check haemorrhage with topical adrenaline Postoperatively install topical antibiotics with corticosteroids for 57 days.

• Corrective surgical procedures may be broadly categorized as “anchoring” or “pocket” techniques. • The original anchoring method involved suturing the gland to the ventral aspect of the globe. • This had a relatively high rate of recurrence owing to difficulty accessing and suturing to the sclera, and too frequently resulted in globe penetration during suturing.
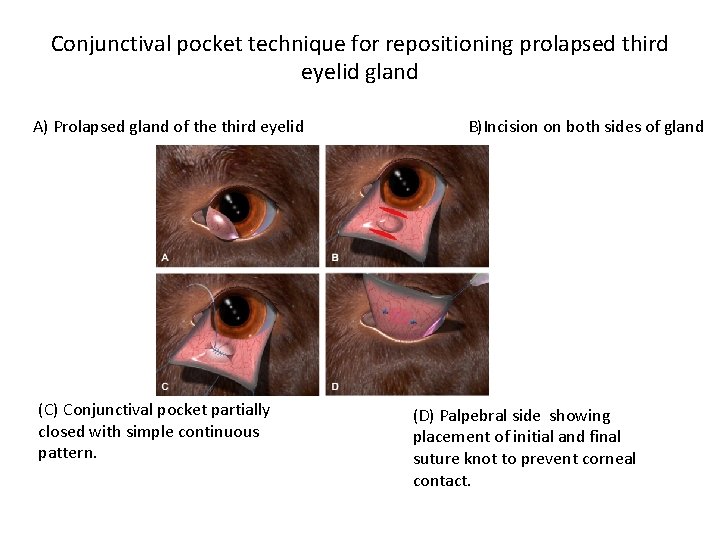
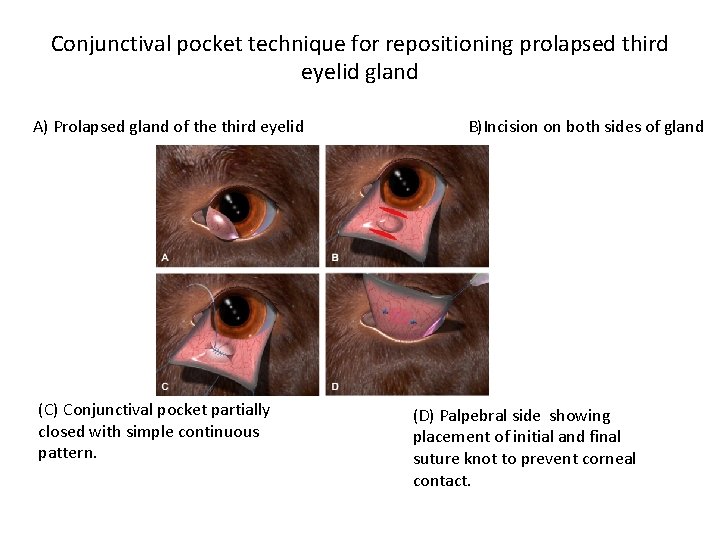
Conjunctival pocket technique for repositioning prolapsed third eyelid gland A) Prolapsed gland of the third eyelid (C) Conjunctival pocket partially closed with simple continuous pattern. B)Incision on both sides of gland (D) Palpebral side showing placement of initial and final suture knot to prevent corneal contact.
NEOPLASMS AFFECTING THE THIRD EYELID • Squamous cell carcinoma commonly involves the third eyelid in cattle and horses • Amelanotic or poorly pigmented third eyelids appear more susceptible. • Third eyelid squamous cell carcinoma is sometimes also seen in small animals • adenocarcinoma of the canine third eyelid in dogs between 10 and 16 years of age, observed frequent • Identification of a third eyelid neoplasm should stimulate a thorough assessment of the orbit, regional lymph nodes, and distant sites for metastases or extension.
• Surgical excision is recommended for all malignant tumors other than lymphoma, • which can be treated via systemic chemotherapy. • For focal masses near the third eyelid free margin resection of the mass and surrounding normal tissue may be possible for Larger tumors necessitate complete excision of the third eyelid and surrounding conjunctiva
TRAUMA TO THE THIRD EYELID • Injuries to the third eyelid occur as a result of fights, motor vehicle accidents, and foreign body penetration. • Usually, tears involving the conjunctiva only do not require suturing. Smallflaps off the leading edge can be safely removed. • Larger lacerations, especially those involving the free margin and creating larger loose flaps, may benefit from careful appositional suturing with knots placed on the anterior surface so as to avoid frictional irritation of the cornea
• Although some retraction takes place during healing, a functional third eyelid can often be retained. • In some circumstances grafting of oral mucous membrane may be useful for replacing large defects.
INFLAMMATORY DISORDERS OF THE THIRD EYELID • The third eyelid is predictably involved in most conjunctival disorders. ü The third eyelid can be involved pannus ü Eosinophilic keratoconjunctivitis of cats and horses ü Ligneous conjunctivitis of dogs ü Habronemiasis of horses ü Nodular granulomatous episclerokeratoconjunctivitis of dogs
• Plasma cell infiltration of 3 rd eyelid is a specific disease of German shepherd. • The cause is not established but considered as some immunological defect. • Symptoms: • Bilateral inflammation with depigmentation of the edges of the 3 rd eyelid. • Associated with the Mucoid discharge. • Thickening of the eyelid as disease progresses. • May be associated with keratitis.
• Treatment: • Immediate sub-conjunctival injection of corticosteroid. • Topical antibiotics and corticosteroids ointments for 10 -14 days, 6 -8 times