AF ablation with 3 D mapping our technique
AF ablation with 3 D mapping: our technique and results Dr Dhiraj Gupta MRCP MD DM Liverpool Heart and Chest Hospital Northern UK AF experts Best Practice meeting Langdale Hotel, Cumbria 5 Feb 2010
Schema Our approach to AF ablation at LHCH Our reasons for each step Our in-lab and follow-up results
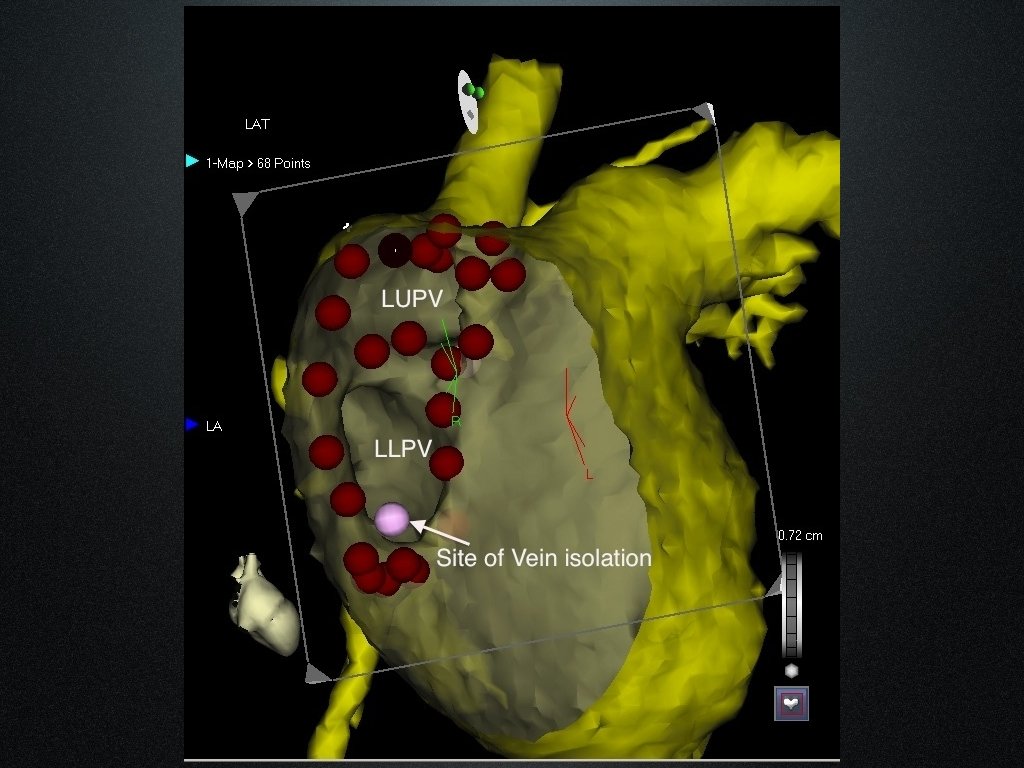
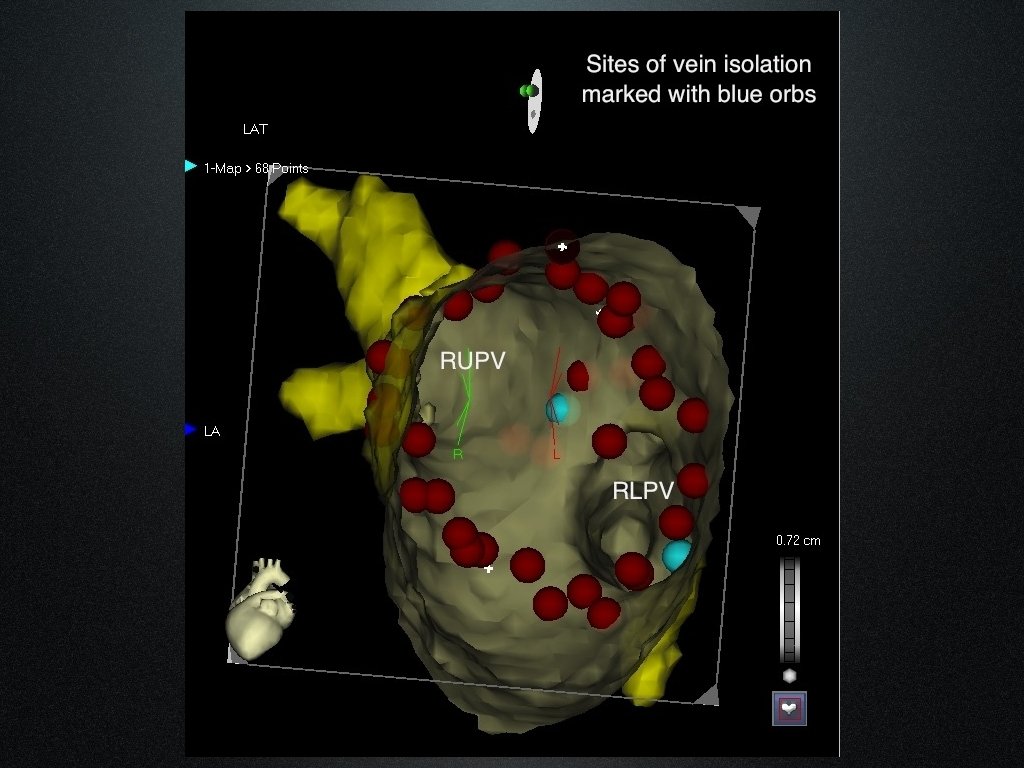
Our approach in a nutshell • PVAI with Wide area circumferential ablation • CT image integration using CARTO • Individualised lesion set prescription • Aim to ablate out of AF, ideally to SR • Procedure duration limit of 5 hours
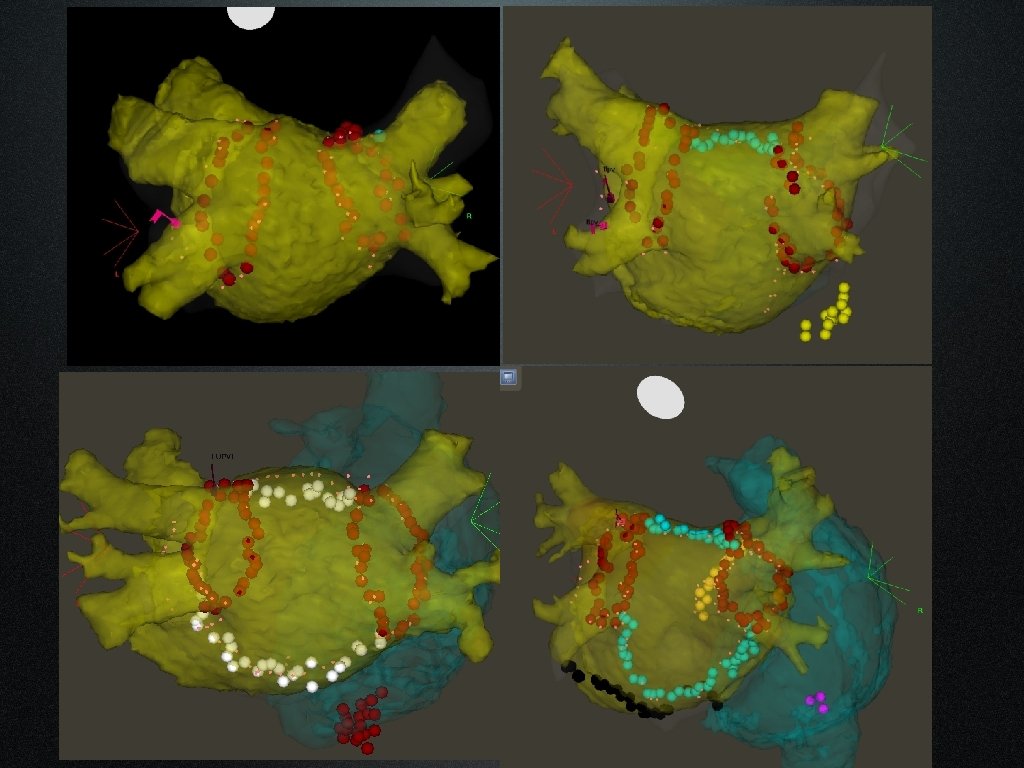
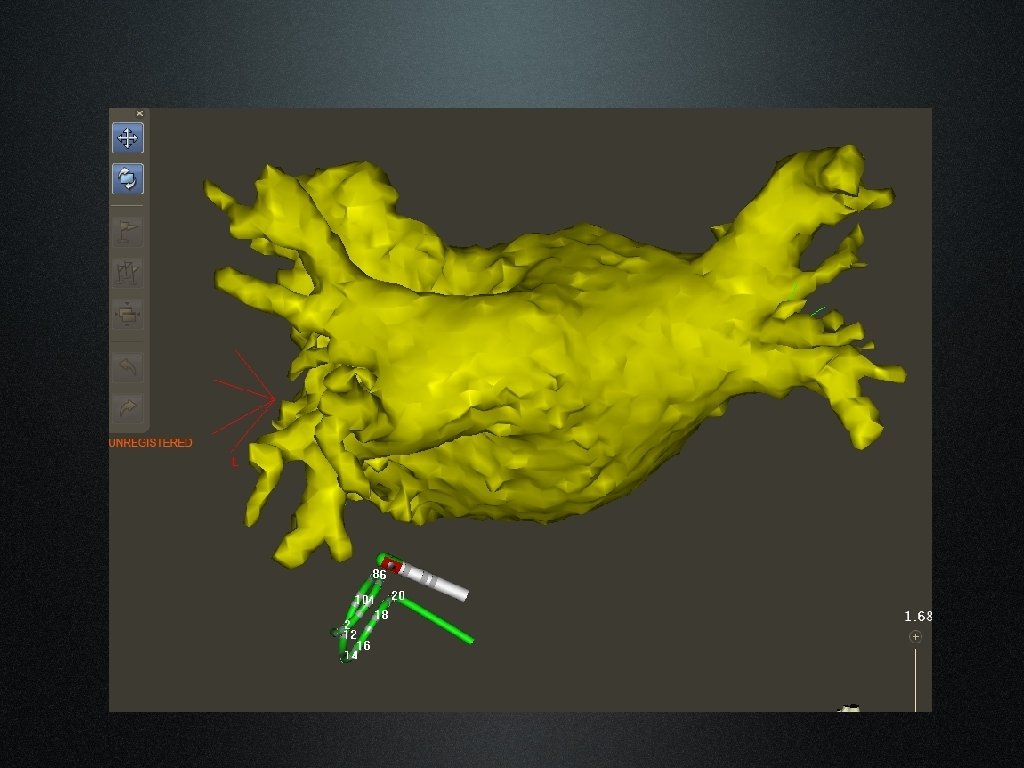
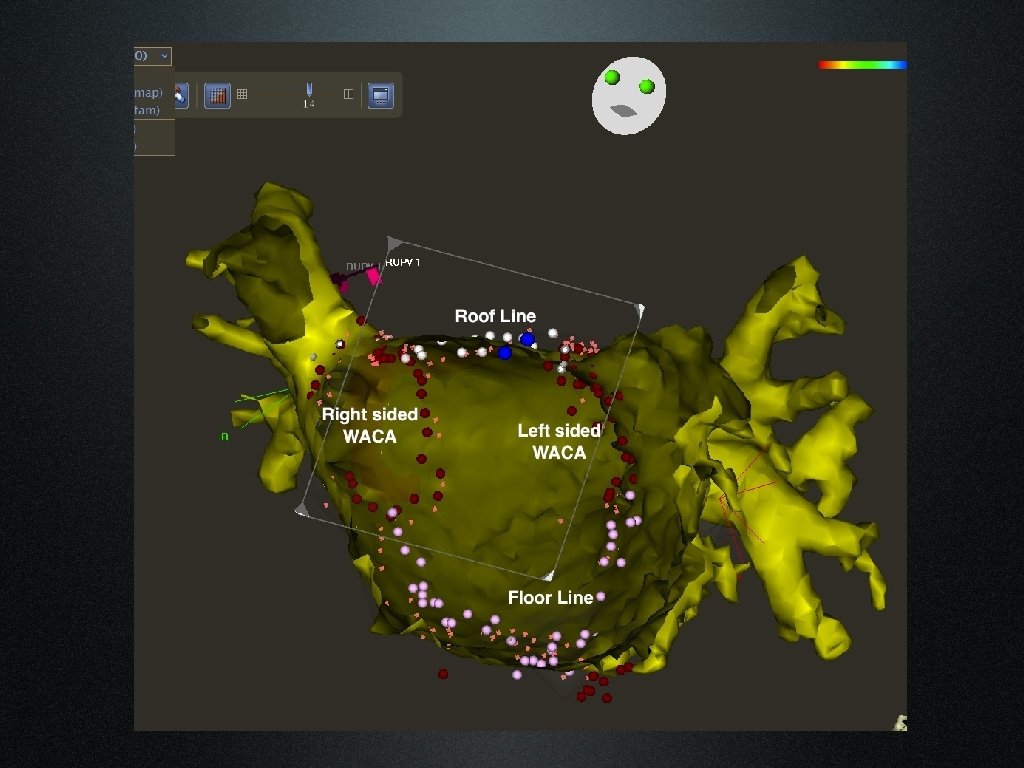
CT image registration • Critical part of the process • 2 steps • Single point Landmark registration • Surface Registration with Fast Anatomical Mapping • Takes 5 -10 minutes
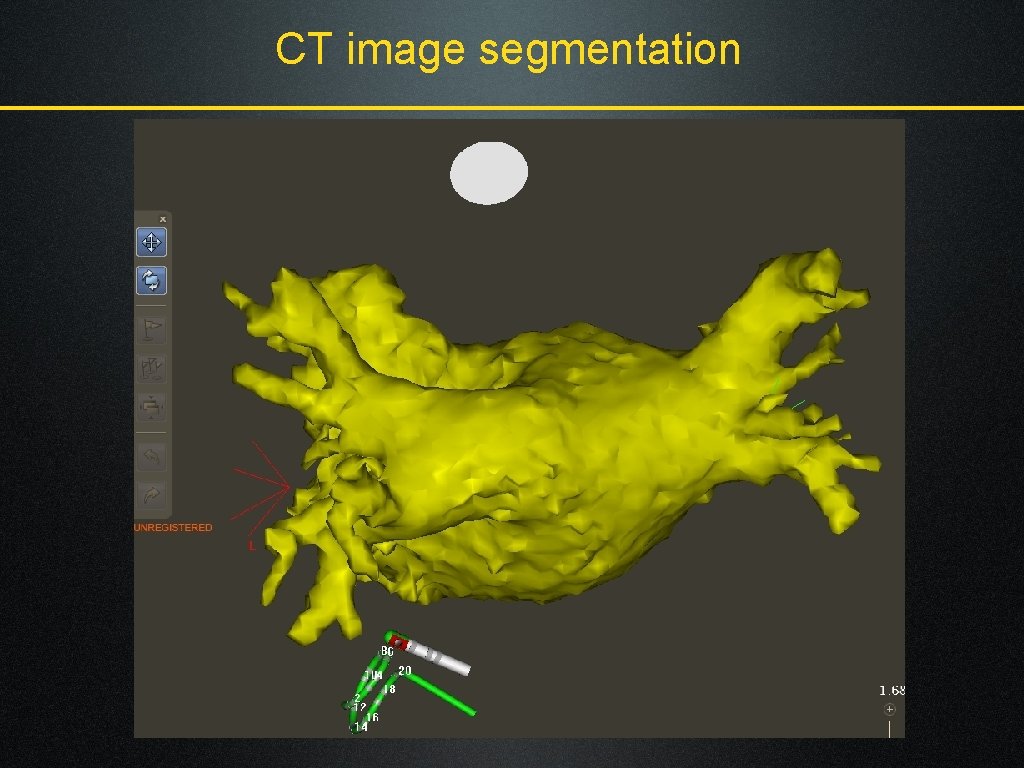
CT image segmentation
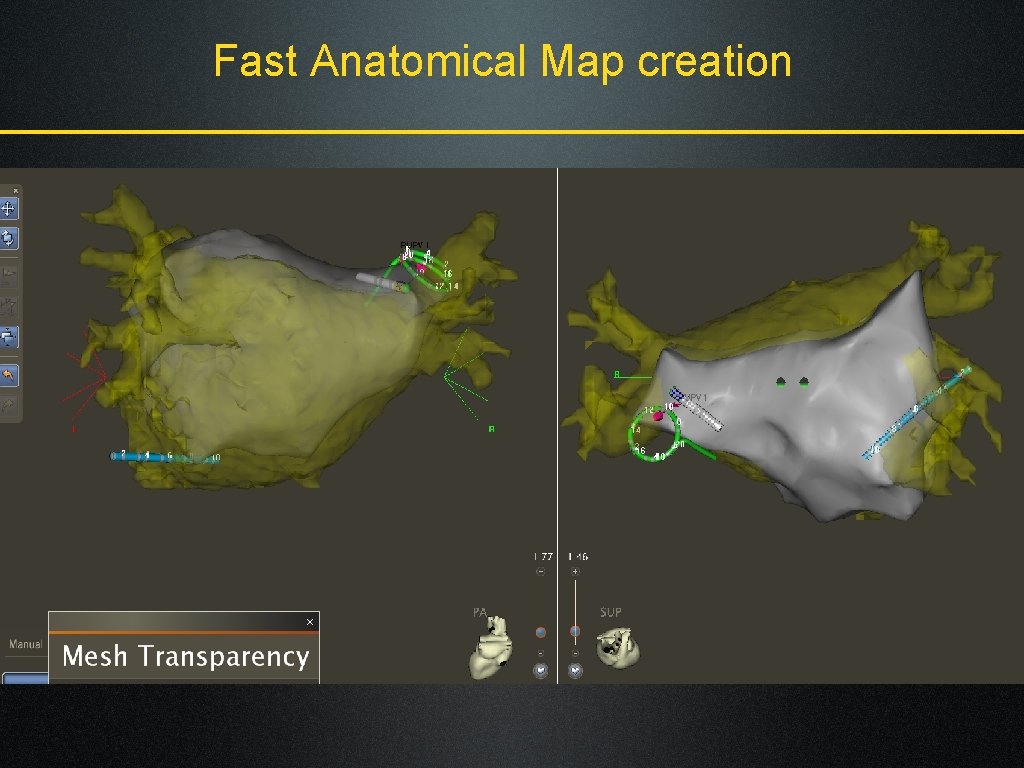
Fast Anatomical Map creation
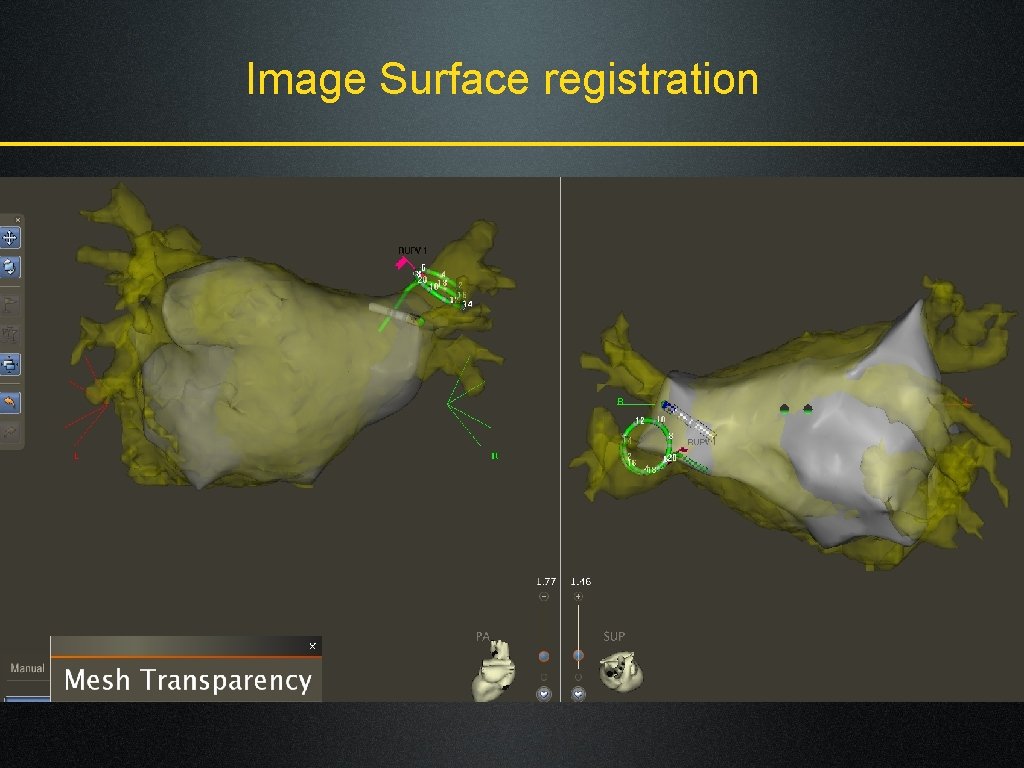
Image Surface registration
Why the individualised approach? • Heterogeneity amongst AF population • Trigger removal vs Substrate Modification • Aim to achieve high single procedure success rates • Incremental risk with multiple procedures • That’s what the patient wants • That’s what the health economists want!
Patient selection criteria • Patients not offered Catheter ablation if • Very long standing Persistent AF (>3 years) • Very large LA (>5. 5 cm) • Morbid Obesity (BMI >40), Sleep Apnea • Significant RA dilatation (>LA) • Patients not offered first redo at least for 6 months • Not offered Second redo if still in Ps. AF
Not all AF patients are the same • True PAF • Short lived episodes, short history, normal sized LA • Sustained PAF: 2 or more of the following • AF episodes>24 hours, History of AF > 5 years, LA size >4. 5 cm, Age >65 years, Documented flutter, High AF burden (most days) • Persistent AF • Long standing Persistent AF (>12 months)
Minimum RF Lesion set • True PAF • PVAI using WACA • Sustained PAF • + LA roof line + RA flutter line • Persistent AF • + LA floor line + Mitral isthmus line • Long standing Persistent AF • + Epicardial CS ablation+ CAFÉ ablation
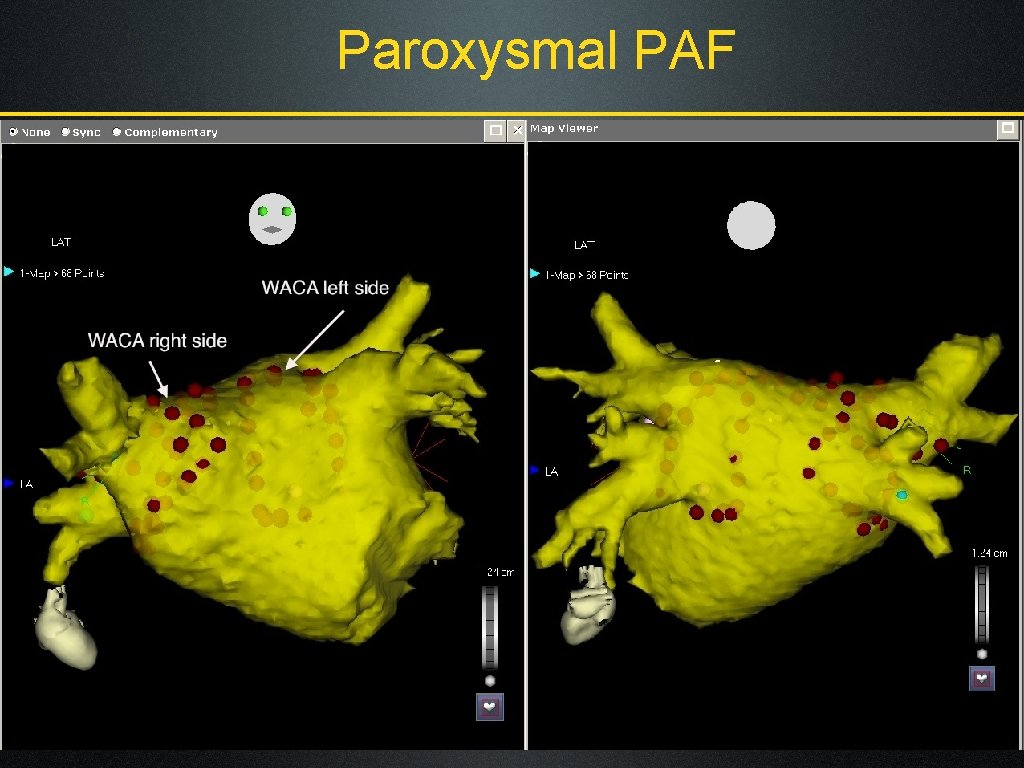
Paroxysmal PAF
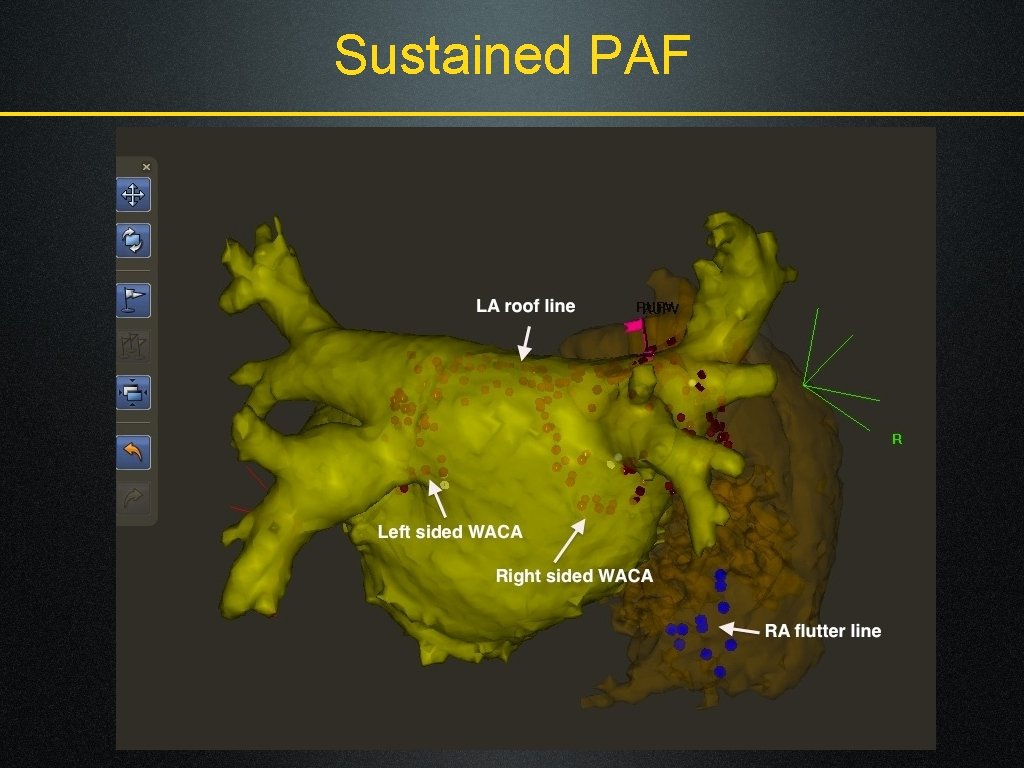
Sustained PAF
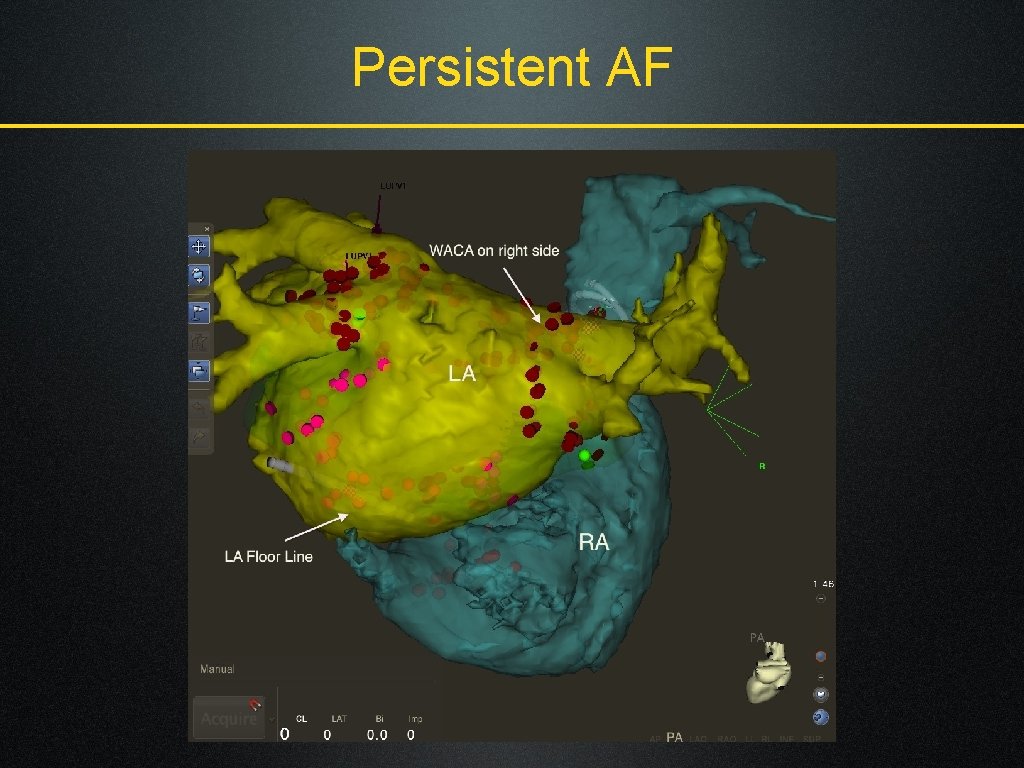
Persistent AF
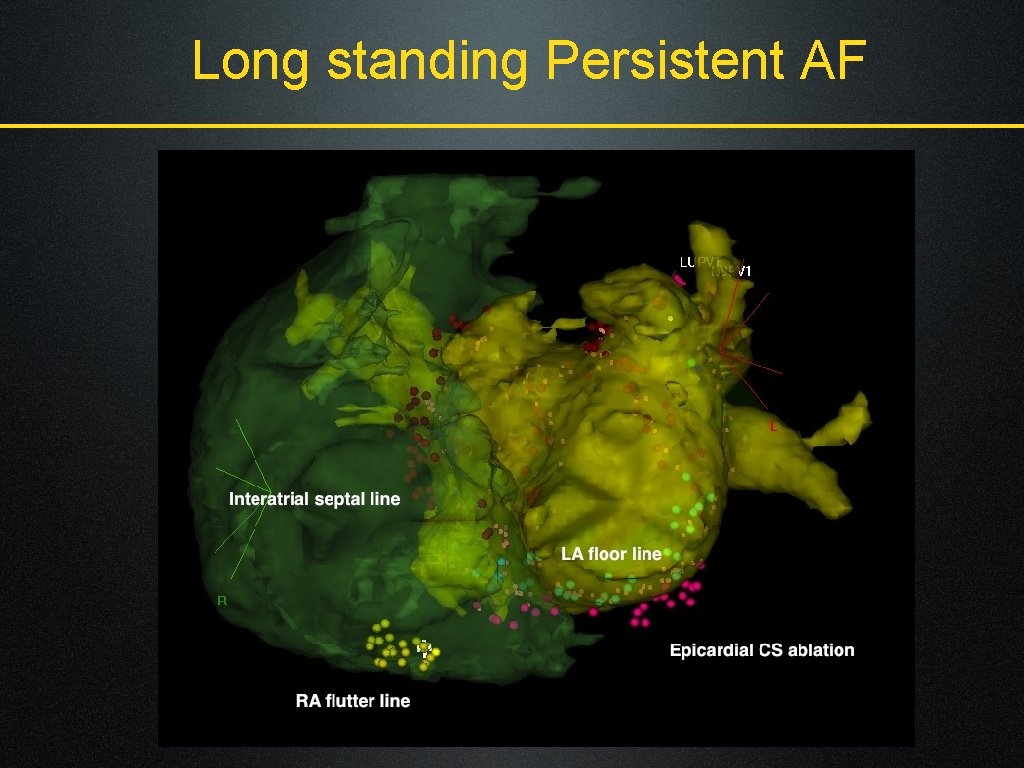
Long standing Persistent AF
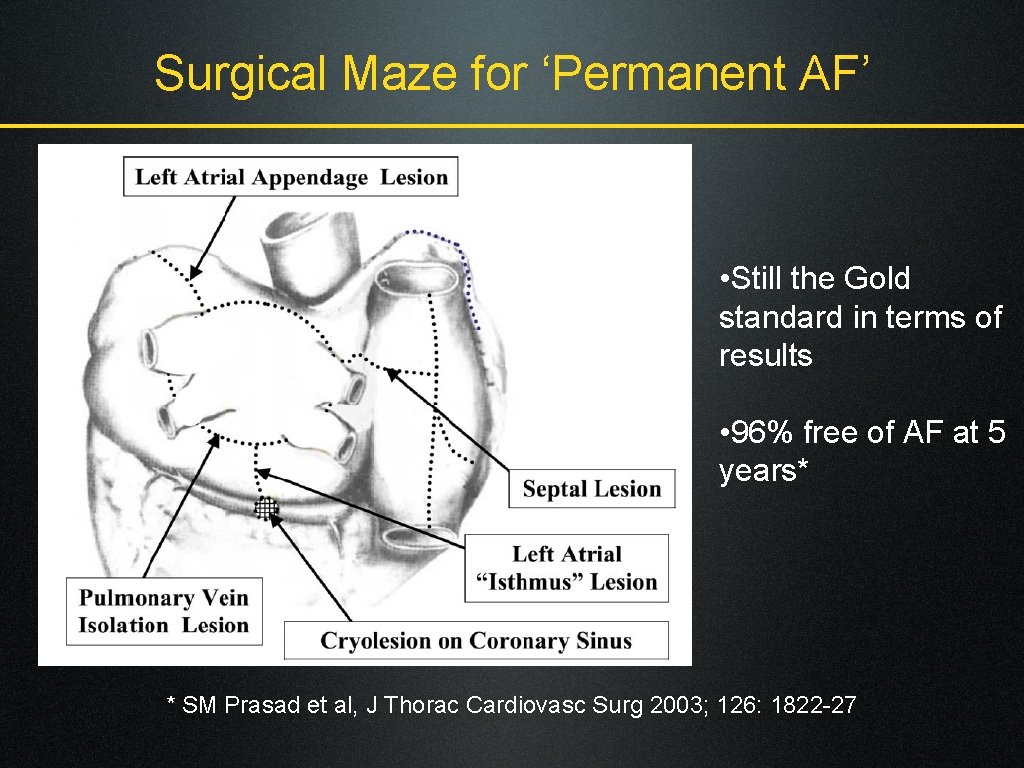
Surgical Maze for ‘Permanent AF’ • Still the Gold standard in terms of results • 96% free of AF at 5 years* * SM Prasad et al, J Thorac Cardiovasc Surg 2003; 126: 1822 -27
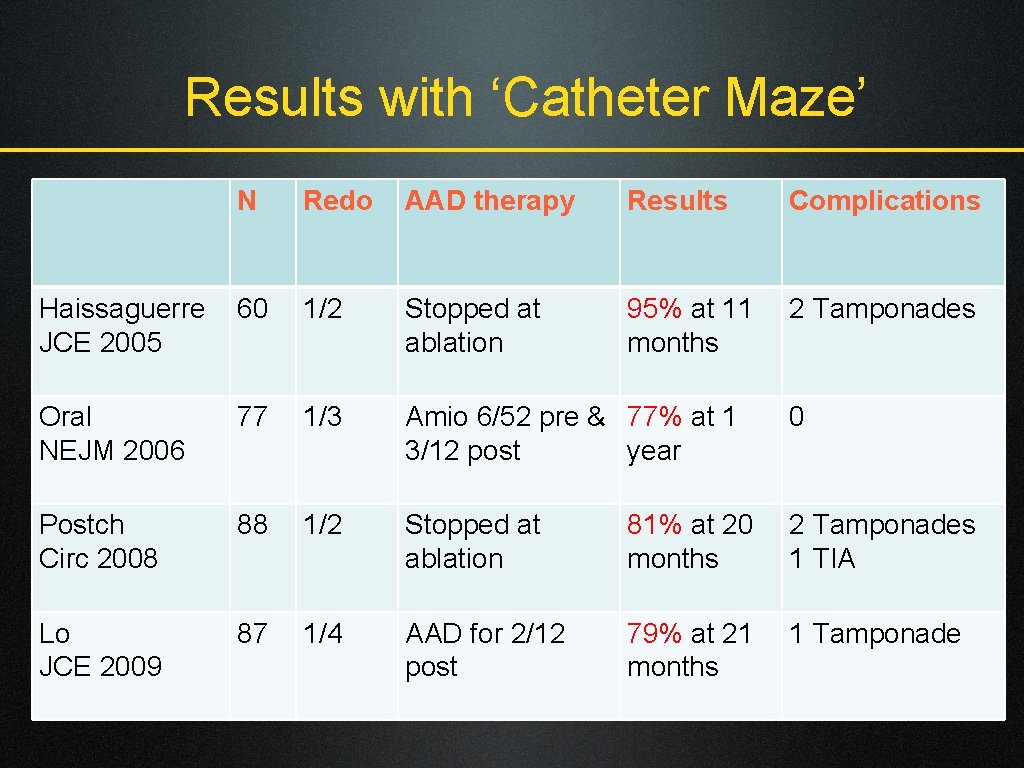
Results with ‘Catheter Maze’ N Redo AAD therapy Results Complications Haissaguerre JCE 2005 60 1/2 Stopped at ablation 95% at 11 months 2 Tamponades Oral NEJM 2006 77 1/3 Amio 6/52 pre & 77% at 1 3/12 post year 0 Postch Circ 2008 88 1/2 Stopped at ablation 81% at 20 months 2 Tamponades 1 TIA Lo JCE 2009 87 1/4 AAD for 2/12 post 79% at 21 months 1 Tamponade
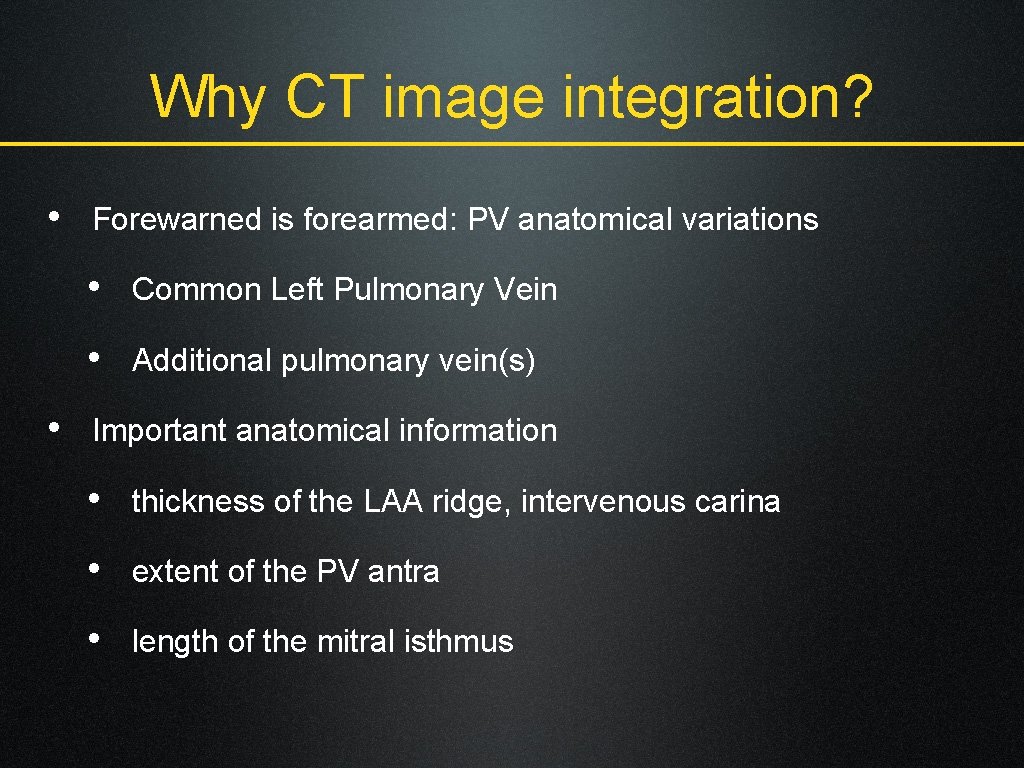
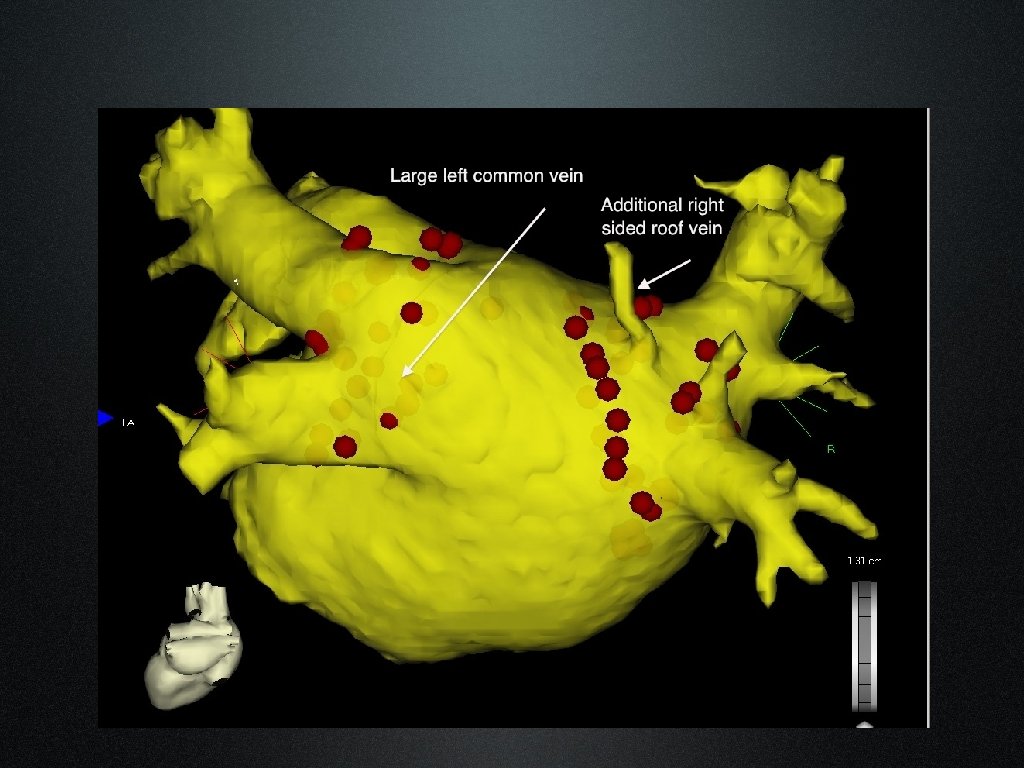
Why CT image integration? • Forewarned is forearmed: PV anatomical variations • Common Left Pulmonary Vein • Additional pulmonary vein(s) • Important anatomical information • thickness of the LAA ridge, intervenous carina • extent of the PV antra • length of the mitral isthmus
Why CT image integration? • Dramatically reduces procedural fluoro times: • <10 minutes for PAF cases • 10 -20 minutes for Ps. AF cases • Decreases fatigue • Removes ‘the fear of the unknown’…. . • Demystifies AF ablation for the nurses/ radiographers!
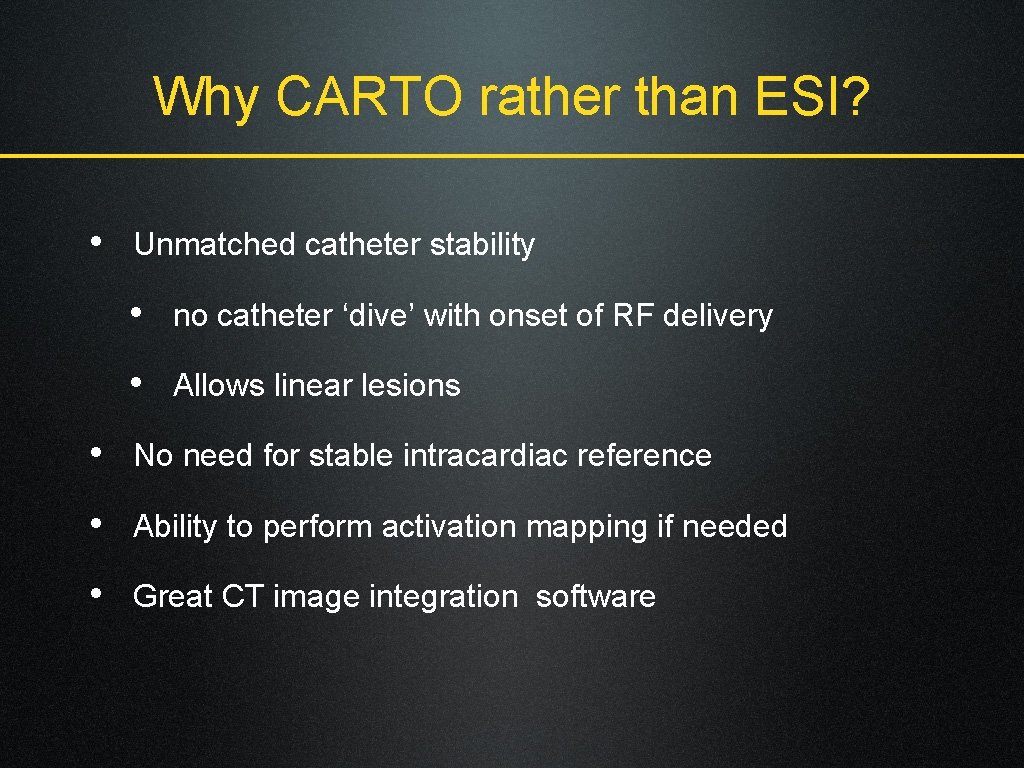
Why CARTO rather than ESI? • Unmatched catheter stability • no catheter ‘dive’ with onset of RF delivery • Allows linear lesions • No need for stable intracardiac reference • Ability to perform activation mapping if needed • Great CT image integration software
Advances with CARTO-3 • Hybrid of impedance and magnetic catheter location • Ability to see all catheters • Ability to create fast anatomical maps • Makes CT image integration easier • More streamlined patient set-up
Why WACA? • PV ostial/ antral triggers • Substrate modification by Atrial debulking • Less risk of PV stenosis • Quicker than segmental PVI • Easy to anchor linear lesions on either side • ‘Et tu, Bordeaux? !’
Why our RF settings? • Continuous RF: 35 W, 50°C, 10 ml/ min flow • Quicker signal obliteration than 30/25 W • Short procedure time (20 -30’ per WACA) • Prevents peri-lesion edema (? reconnection risk) • RF controlled by Foot pedal • Frees up a cardiac physiologist • Imposes discipline on use of X-ray pedal!
Our results 131 consecutive pts. between Jan 08 -July 09
Individualised ablation strategy • True PAF (n=45) • PVAI using WACA • Sustained PAF (n=31) • + LA roof line+ RA flutter line • Ps AF (n=22) • + LA floor line+ Mitral isthmus line • Long standing Ps AF (n=33) • + Epicardial CS ablation+ CAFÉ ablation
In-lab results • All patients received prescribed minimum lesion set • Mean Procedure time 173 min (98 -300) • Fluoroscopy times • Mean 26. 5 min (13 -58) (as pre-CARTO 3 era) • Now with CARTO-3 (n=36): Mean 14 min (6 -21) • Complications • 1 tamponade (PVI group), 1 AV fistula
Our follow-up strategy • Antiarrhythmic drug therapy for 2 -3 months • Early post-op arrhythmias • DC CV if sustained and poorly tolerated (n=1) • No redo ablation procedure for at least 6 months • Mean follow up 11. 3 months (6 -24)
Our Clinical Results • Definition of Procedural Success: • No symptoms beyond 3 months, AND • Absence of AF/AT on 24 hour Holter at 6 mo • Single procedure success rates at 6 months • PAF 84% • Ps. AF 86% • Sustained PAF 77% (p=0. 05) • Long standing Ps. AF 64% (p<0. 001)
Conclusions • Single procedure success should be the goal • Most patients need substrate modification in addition to trigger removal • This needs application of linear lesions • 3 D mapping guided ablation the gold standard

Acknowledgements to Dr Richard Schilling, my mentor and guide Thank You www. heartrhythmspecialist. co. uk
- Slides: 36