Adverse Drug Reactions and Drug Interactions Drug Poisoning


- Slides: 27

Adverse Drug Reactions and Drug Interactions, Drug Poisoning and Management Dr. Saed M. Aldalaen 2019 -2020
Adverse Reaction During the last few years , adverse drug reactions are increased , due to increase the number of drugs in use. They are responsible: - about 5% of admission to hospitals - 10 -20% of hospital inpatients

Adverse Reaction • Are more severe than side effect , and always undesirable effect. They are a range of untoward effects of drugs that cause mild to severe side effects. Side effect • Are physiological effects not related to desired drug effects. All drugs have side effects , desirable or undesirable. E. g. Diphenhydramine , H 1 antagonist, ( used in motion sickness, ) (drowsiness , sedating effect)
Drugs most commonly causing adverse reactions : • Warfarin (Bleeding disorder) , It is important to frequently monitoring and adjust the anticoagulant effect. Normal INR : 2. 0 -3. 0 • Digoxin ( Decrease serum level of potassium, predispose a patient to digoxin toxicity) Cardiac effect cause dysrhythmia
• Steroids Cushing like syndrome : redistribution of body fat, puffy face, increase body hair growth, insomnia and increase risk of infection) • Oral contraceptive Most adverse effects are believed to be due to estrogen component ( Breast fullness, depression and headache ) but cardiovascular effects reflect the action of both estrogen and progestin ( thromboembolism, hypertension) Contraindications In the presence of cerebrovascular and thromboembolic disease , estrogen-dependent neoplasms , liver disease and migraine headache.
• Potassium (Spironolactone) ⁻ Hyper. Kalemia ⁻ Gynecomastia & impotence ⁻ Gastric upset & peptic ulcer ⁻ Is contra-indicated in renal failure because of the risk of hyperkalemia • Diuretics • Adverse effects: - Hypovolemia - Hypokalemia - Hyponatraemia - Hyperuricaemia & even precipitation of gout
Classification of ADRs Type A (Augmented): - Common (account for 80%) - Due to excessive of pharmacological activity of drug -Predictable - Dose-related Can be relived if a lower dose regimen or the drug is stopped for a time - e. g. warfarin causing bleeding
They can be due to : - Incorrect dose - Increments sensitivity of organs , sensitivity of the heart to digoxin leading to toxicity in pts with Kdeficiency - Decreased elimination e. g. Gentamycin eliminations in renal failure causing accumulation and damage of ears
Classification of ADRs Type B (idiosyncratic): - Will occur only in some people - Are due to unusual interaction of patient with the drug - Not dose-related - Unpredictable - Account for most drug fatalities - e. g. carbamazepine induced skin rash
Among the known causes are: • Genetic factors Is related to the genetic make-up of the individuals. e. g. - subjects of tissues type HL- AD 3 are more likely to suffer from gold toxicity. - Primaquine (anti malarial agent ), causes break down of red cells in a number of people of African and Indian descent. • Host factors Host disease may predispose to a certain adverse reaction. E. g. pts with infectious mononucleosis (fever glandular) are liable to get a rash if given ampicillin
• Allergic reactions When the patient has been exposed to a certain drug on some occasion , and has resulted in the production of an antibody against this drug. Sometimes these antibodies combine with a drug in such a way as to cause damage to tissues and produce the symptoms of allergic reactions.
Classification of ADRs Type C (Chronic): - Due to long-term exposure - e. g. analgesic nephropathy Type D (Delayed): - e. g. carcinogenesis, or short-term exposure at a critical time (teratogenesis)
Classification of ADRs Type E (Ending of use): - Discontinuation of chronic therapy suddenly - e. g. opioid causing the withdrawal syndrome • Physical and psychological effect of withdrawal syndrome: • • • Within 12 hours craving for the drug, rhinorrhoea, Lacrimation, shivering, hyperventilation Nausea, diarrhoea, colic Increase HR & BP, mydriasis, flushing Methadone & clonidine are useful
Causes of ADRs 1. The patient: - Age (over 60 or under one month) - Genetic factors - Previous history of ADR - Hepatic or renal diseases
Causes of ADRs 2. The drug - Narrow therapeutic index, e. g. warfarin, digoxin - Antimicrobials have a tendency to cause allergy and may lead to type B reactions - Ingredients of a formulation, e. g. colouring, flavouring agents
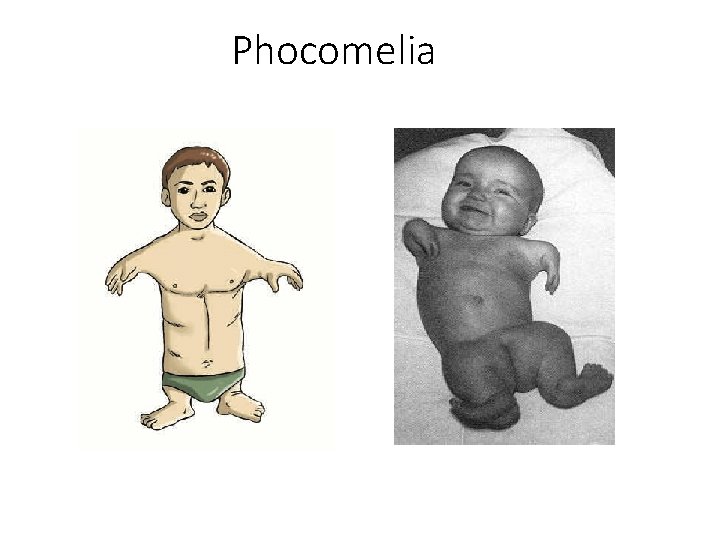
Causes of ADRs 3. The prescriber: - A drug is used for an inappropriately long time - At a critical phase in pregnancy • • • Thalidomide: phocomelia Cytotoxic drugs: multiple congenital malformations Vitamin A derivates (isotretinoin): craniofacial defects Steroids: cleft lip and or cleft palate Warfarin: skeletal abnormalities - Given with other drugs (drug-drug interactions)
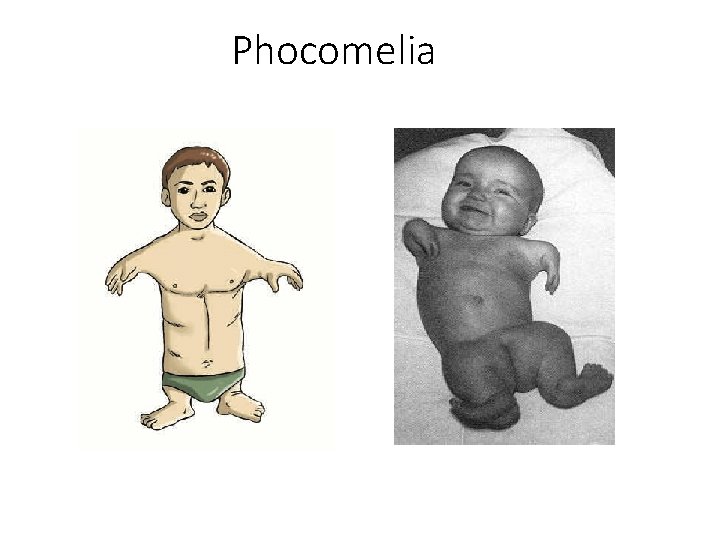
Phocomelia
Drug Interactions • defined as a change in the pharmacologic effect of a drug when it is given together with another drug • A drug interaction may be: - Beneficial: e. g. naloxone is given to treat morphine overdose - Harmful: e. g. oral contraceptive is metabolized rapidly when a metabolic enzyme inducer drug (phenytoin) is added
Clinical Importance of Drug Interactions • Drugs that have a small therapeutic index, e. g. warfarin, digoxin • Drugs that are enzyme inducer or inhibitors e. g. rifampicin • Drugs that are used long-term, e. g. oral contraceptives • Patients with impaired liver or kidney function • In the elderly
Identifying Potential Drug Interactions 1. Outside the body: - Drugs can interact when they are mixed with other drugs, e. g. i. v. infusion or syringe 2. Interactions at the site of absorption: - Direct interaction in intestine is a cause of reduced absorption - Addition of vasoconstrictors, e. g. adrenaline to local anaesthetic to delay absorption and prolong local anaesthesia
Identifying Potential Drug Interactions 3. Interactions during distribution 4. Interactions during metabolism: - Enzyme induction by drugs, increases metabolism, leading to therapeutic failure (oral contraceptives-phenytoin) - Enzyme inhibition, e. g. cimetidine is an inhibitor of CYP 450 enzymes
Drug poisoning
Principles of Treatment of Drug poisoning • Successful treatment of acute poisoning depends on a combination of: - Speed - Common sense - Nature of the poison - The amount taken - The time
Principles of Treatment of Drug poisoning • The majority of those admitted to hospital require only observation and medical and nursing supportive measures while they metabolise and eliminate the poison • Some require a specific antidote or specific measure to increase elimination
Identification of the poison • The key pieces of information are: - The identity of the substance taken - The dose - The time passes since taken the poison
Identification of the poison • Biochemical screens of plasma or urine for seriously ill or unconscious patients • Response to a specific antidote may provide a diagnosis, e. g. dilatation of constricted pupils and increased respiratory rate after i. v. naloxone (opioid poisoning)
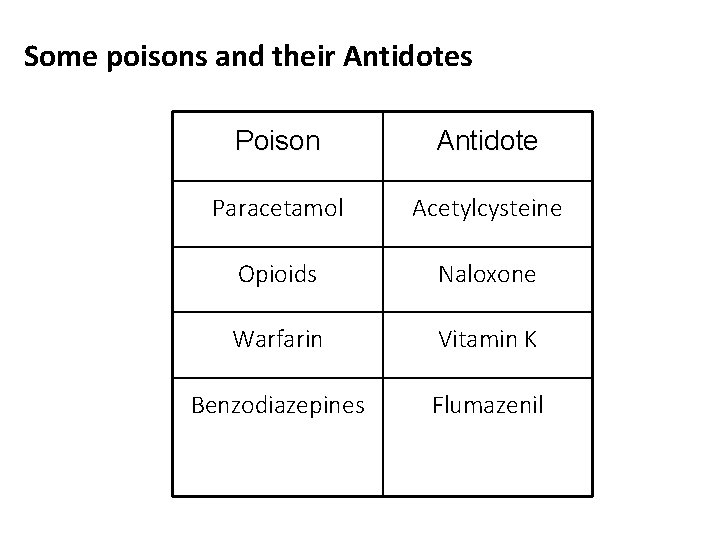
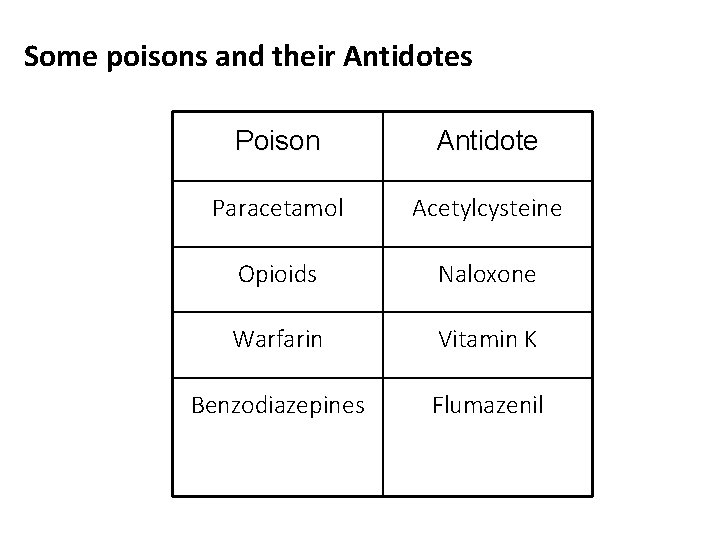
Some poisons and their Antidotes Poison Antidote Paracetamol Acetylcysteine Opioids Naloxone Warfarin Vitamin K Benzodiazepines Flumazenil