Advancing Social Work Practice with Clients Understanding the


- Slides: 32
Advancing Social Work Practice with Clients: Understanding the DSM 5 Social Work and the DSM-5: Mood and Anxiety Disorders Robin Gearing, Ph. D December 6, 2013
Overview Mood and Anxiety Disorders: 1. What has changed? 2. What has stayed the same? 3. What is the significance of this revision to clinical social work practice?
DSM • Strength of the DSM is to provide a common language for describing psychopathology • More of a dictionary that creates a set of labels and defines each, than a “Bible” for the field (Insel, 2013)
Social Work: Be Informed, (then) Be Critical Clinical and practicing social workers: – Should familiarize themselves with the DSM-5 and related controversies Then – Be able to apply critical thinking to the question of their client’s diagnoses and treatment relevant to their context (Littrell & Lacasse, 2012)

DSM-5 and Culture • The cultural formulation interview guide will help clinicians to assess cultural factors influencing patients’ perspectives of their symptoms and treatment options – Includes questions about patients’ background in terms of their culture, race, ethnicity, religion or geographical origin (APA, 2013) • Practice application of criteria across individual demographic characteristics (e. g. , cultures, race, sex, age)?
Mood Disorders • Depression (melancholia) was recognized as a medical illness by Hippocrates (460 -377 BC) • Depression can be considered across a spectrum, with symptoms and severity assessed on a continuum – Unitary Theory of Depression (Akiskal & Mc. Kinney, 1973) – Severe, moderate, and mild depressions may not be points on a single spectrum • Depression can be a symptom or a disorder • Mood is disproportionate to external stressors
Depressive Disorders
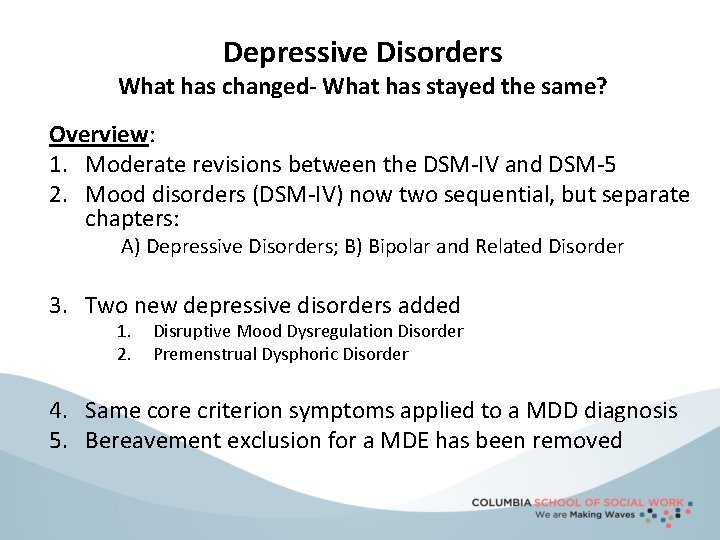
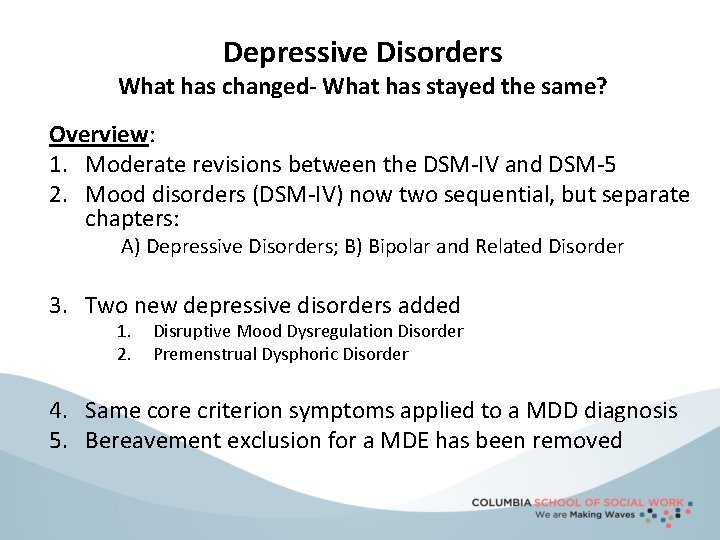
Depressive Disorders What has changed- What has stayed the same? Overview: 1. Moderate revisions between the DSM-IV and DSM-5 2. Mood disorders (DSM-IV) now two sequential, but separate chapters: A) Depressive Disorders; B) Bipolar and Related Disorder 3. Two new depressive disorders added 1. 2. Disruptive Mood Dysregulation Disorder Premenstrual Dysphoric Disorder 4. Same core criterion symptoms applied to a MDD diagnosis 5. Bereavement exclusion for a MDE has been removed
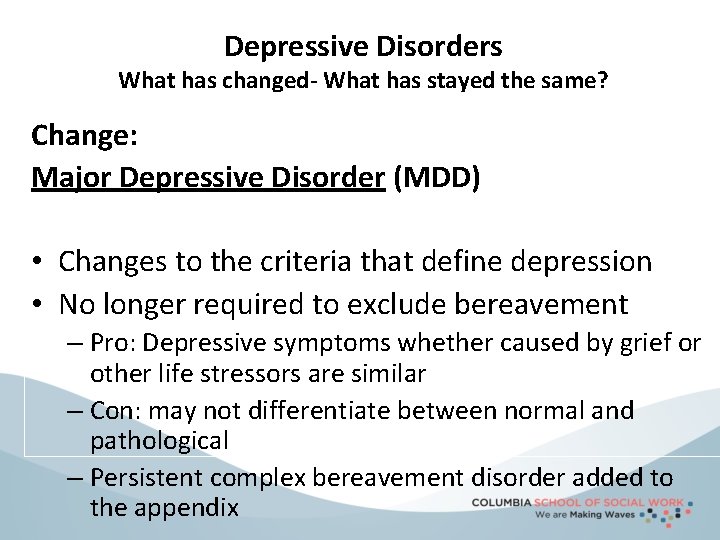
Depressive Disorders What has changed- What has stayed the same? Change: Major Depressive Disorder (MDD) • Changes to the criteria that define depression • No longer required to exclude bereavement – Pro: Depressive symptoms whether caused by grief or other life stressors are similar – Con: may not differentiate between normal and pathological – Persistent complex bereavement disorder added to the appendix
Depressive Disorders What has changed- What has stayed the same? Change: Persistent Depressive Disorder (Dsythymia) • Name changed: – From Dsythymia – To Persistent Depressive Disorder – Criteria are the same
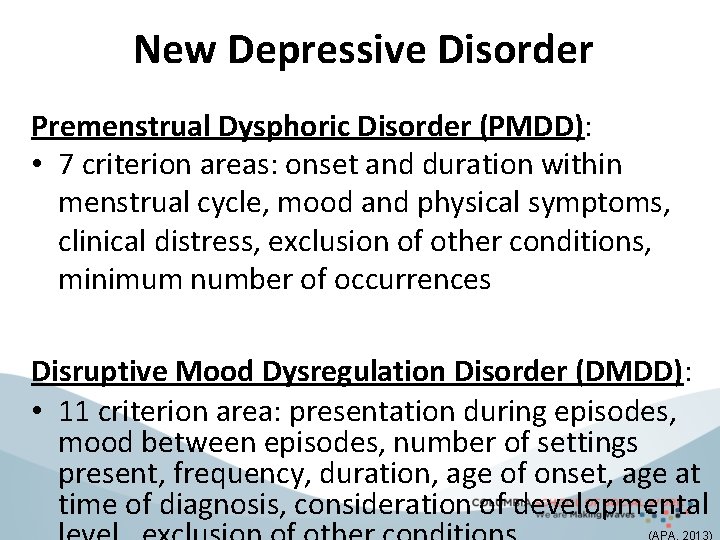
New Depressive Disorder Premenstrual Dysphoric Disorder (PMDD): • 7 criterion areas: onset and duration within menstrual cycle, mood and physical symptoms, clinical distress, exclusion of other conditions, minimum number of occurrences Disruptive Mood Dysregulation Disorder (DMDD): • 11 criterion area: presentation during episodes, mood between episodes, number of settings present, frequency, duration, age of onset, age at time of diagnosis, consideration of developmental
Depressive Disorders Implications of Changes? Overview of Implications: 1. Bereavement exclusion: – Difficulty distinguishing normal from pathological depression 2. Having a cognitive construct, hopeless, in depression: – As a feeling criteria to define one’s depressed mood most of the day, nearly every day 3. Premenstrual Dysphoric Disorder – Potential stigmatization of women
Depressive Disorders Implications of Changes? 4. Disruptive Mood Dysregulation Disorder – Address concerns of potential overdiagnosis/overtreatment of bipolar Dx in children – One condition or perhaps a modifier? Explosive outbursts can occur with other conditions (e. g. , ADHD, ODD, mania, depression, autism, anxiety, schizophrenia)
Bipolar and Related Disorders
Bipolar and Related Disorders: What has changed- What has stayed the same? Overview: 1. Bipolar and Related Disorders is a separate chapter 2. Minimal Bipolar changes between DSM-IV and DSM-5 3. Criterion A for manic/hypomanic episodes § Now includes a focus on changes in activity and energy, as well as mood § More narrowly defined: Present most of the day,
Bipolar and Related Disorders: What has changed- What has stayed the same? Overall these are essentially the same Bipolar I Disorder Bipolar II Disorder Hypomanic Episode Except there is a change to the criteria that define Manic Episode and Hypomanic Episode • Criterion changes to mood presentation, length of the episode, and distinct from typical behavior • New specifiers: with anxious distress, with mixed features • New diagnostic codes for a single episode and recurrent episodes of differing severity levels and other specifiers
Bipolar and Related Disorders What has changed- What has stayed the same? Overall Cyclothymic Disorder is essentially the same Except there is a new specifier: with anxious distress
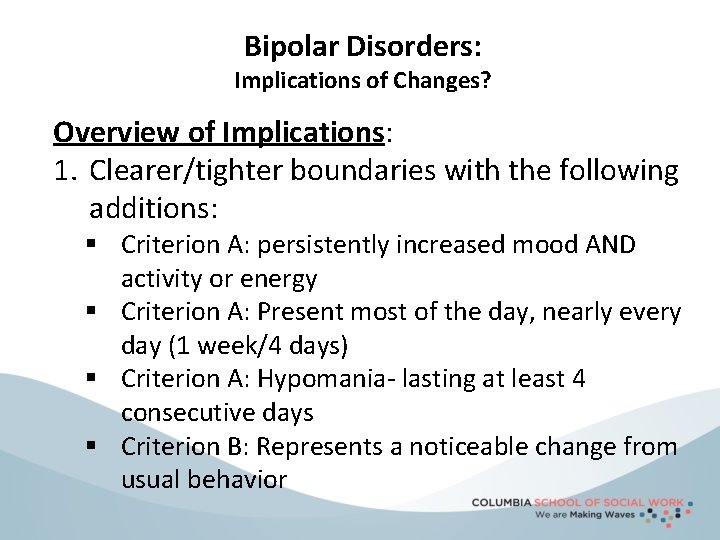
Bipolar Disorders: Implications of Changes? Overview of Implications: 1. Clearer/tighter boundaries with the following additions: § Criterion A: persistently increased mood AND activity or energy § Criterion A: Present most of the day, nearly every day (1 week/4 days) § Criterion A: Hypomania- lasting at least 4 consecutive days § Criterion B: Represents a noticeable change from usual behavior
Anxiety Disorders
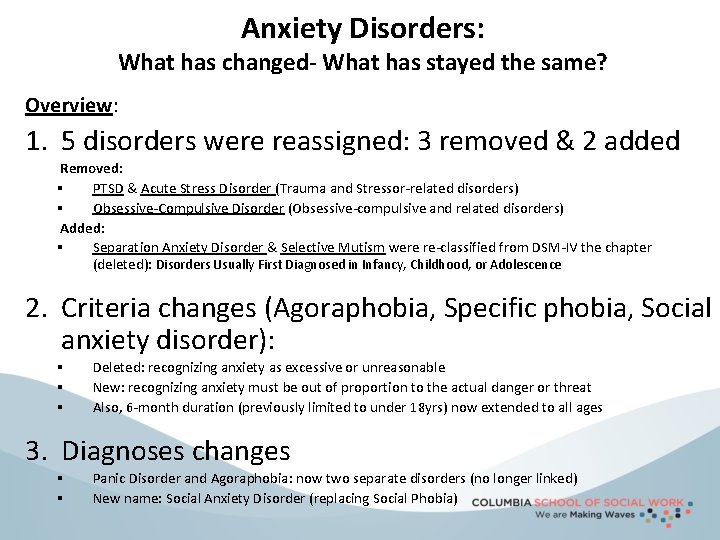
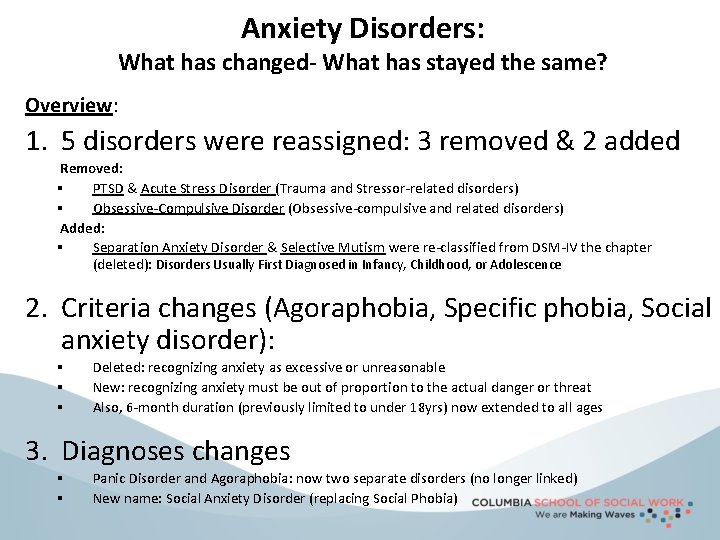
Anxiety Disorders: What has changed- What has stayed the same? Overview: 1. 5 disorders were reassigned: 3 removed & 2 added Removed: § PTSD & Acute Stress Disorder (Trauma and Stressor-related disorders) § Obsessive-Compulsive Disorder (Obsessive-compulsive and related disorders) Added: § Separation Anxiety Disorder & Selective Mutism were re-classified from DSM-IV the chapter (deleted): Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence 2. Criteria changes (Agoraphobia, Specific phobia, Social anxiety disorder): § § § Deleted: recognizing anxiety as excessive or unreasonable New: recognizing anxiety must be out of proportion to the actual danger or threat Also, 6 -month duration (previously limited to under 18 yrs) now extended to all ages 3. Diagnoses changes § § Panic Disorder and Agoraphobia: now two separate disorders (no longer linked) New name: Social Anxiety Disorder (replacing Social Phobia)
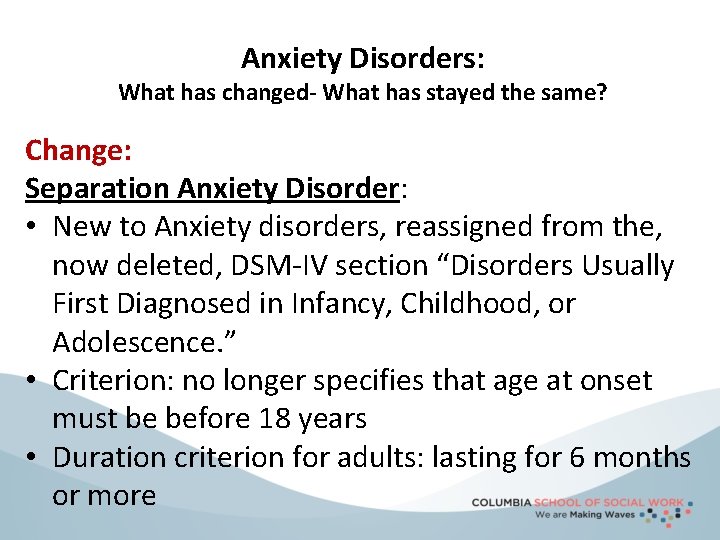
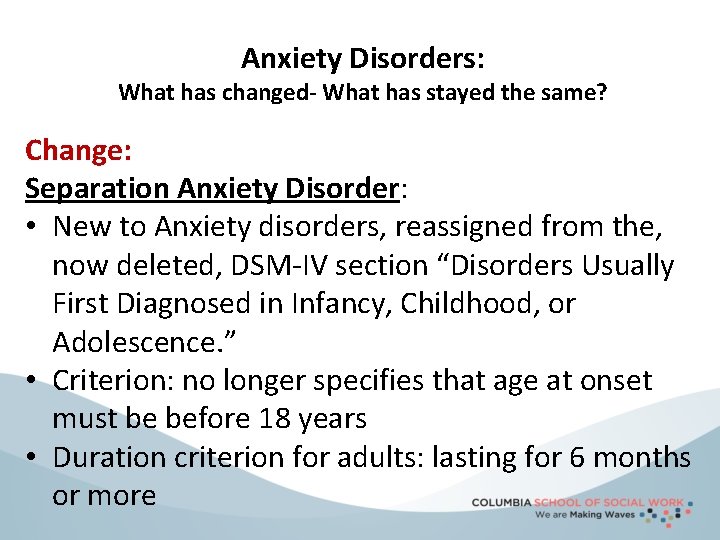
Anxiety Disorders: What has changed- What has stayed the same? Change: Separation Anxiety Disorder: • New to Anxiety disorders, reassigned from the, now deleted, DSM-IV section “Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence. ” • Criterion: no longer specifies that age at onset must be before 18 years • Duration criterion for adults: lasting for 6 months or more
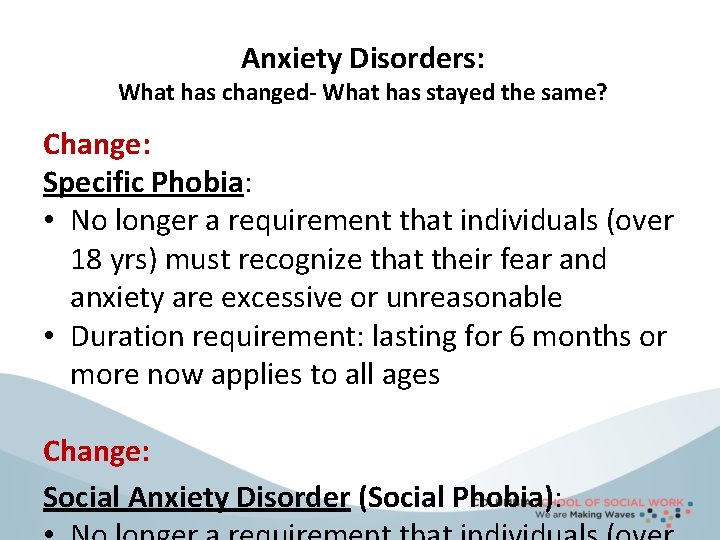
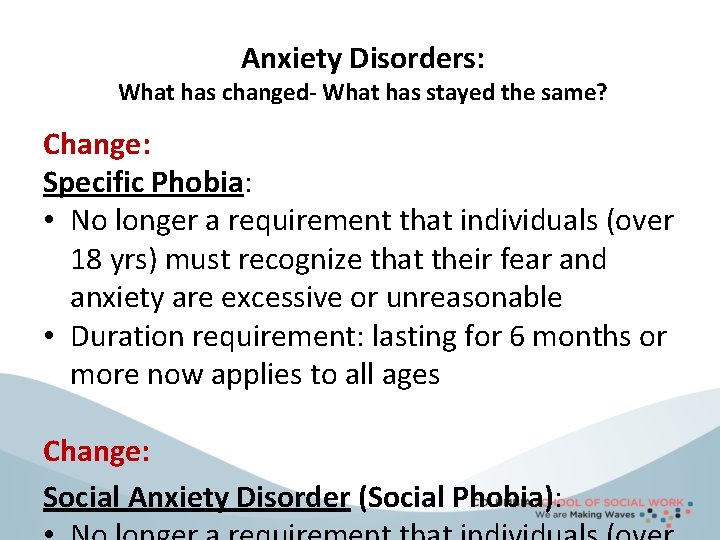
Anxiety Disorders: What has changed- What has stayed the same? Change: Specific Phobia: • No longer a requirement that individuals (over 18 yrs) must recognize that their fear and anxiety are excessive or unreasonable • Duration requirement: lasting for 6 months or more now applies to all ages Change: Social Anxiety Disorder (Social Phobia):
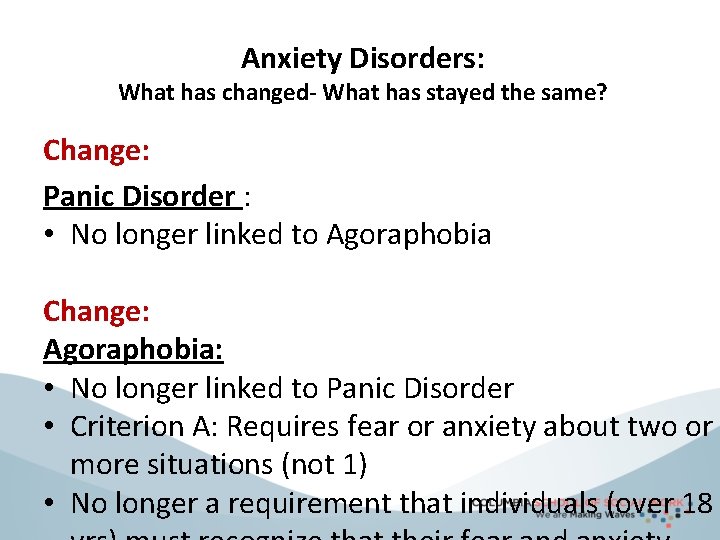
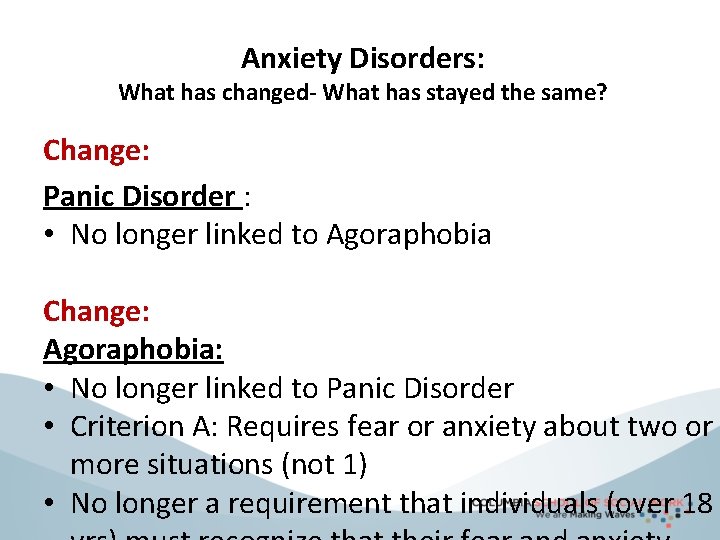
Anxiety Disorders: What has changed- What has stayed the same? Change: Panic Disorder : • No longer linked to Agoraphobia Change: Agoraphobia: • No longer linked to Panic Disorder • Criterion A: Requires fear or anxiety about two or more situations (not 1) • No longer a requirement that individuals (over 18
Anxiety Disorders: What has changed- What has stayed the same? Change: Generalized Anxiety Disorder (GAD): • Minor wording changes
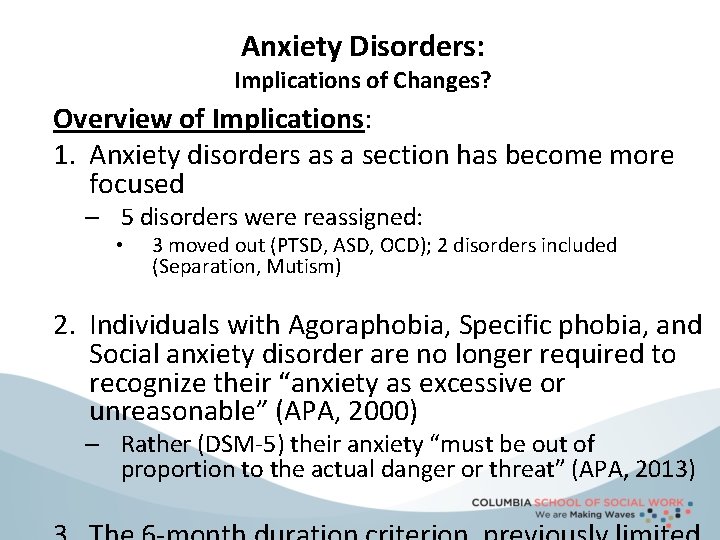
Anxiety Disorders: Implications of Changes? Overview of Implications: 1. Anxiety disorders as a section has become more focused – 5 disorders were reassigned: • 3 moved out (PTSD, ASD, OCD); 2 disorders included (Separation, Mutism) 2. Individuals with Agoraphobia, Specific phobia, and Social anxiety disorder are no longer required to recognize their “anxiety as excessive or unreasonable” (APA, 2000) – Rather (DSM-5) their anxiety “must be out of proportion to the actual danger or threat” (APA, 2013)
Reliability - Validity • The strength of each of the editions of DSM has been “reliability” – – each edition has ensured that clinicians use the same terms in the same ways • The weakness is its lack of validity – Unlike our definitions of ischemic heart disease, lymphoma, or AIDS, the DSM diagnoses are based on a consensus about clusters of clinical symptoms, not any objective laboratory measure
NIMH Research Domain Criteria (RDo. C) • Diagnosis in mental disorders is based on clinical observation and patients’ phenomenological symptom reports • The current diagnostic system is not informed by recent breakthroughs in genetics; and molecular, cellular and systems neuroscience

NIMH Research Domain Criteria (RDo. C) • RDo. C is intended as a framework to guide classification of patients for research studies, not as an immediately useful clinical tool • The initial steps must be to build a sufficient research foundation that can eventually inform the best approaches for clinical diagnosis and treatment • It is hoped that by creating a framework that interfaces directly with genomics, neuroscience, and behavioral science, progress in explicating
Mission Creep One of the most serious problems for the DSM-5 is that it extends the concept of mental disorder. It can be used to diagnose those who only have subclinical symptoms or problems (Paris, 2013, p. 40)
False-Positives Concerns with the potential for false-positives
Be Informed, (then) Be Critical • Practicing social workers should familiarize themselves with the many controversies related to DSM-5 • Apply critical thinking to the question of diagnoses relevant to their practice context (Littrell & Lacasse, 2012)
DSM-5 Won’t Solve the Overdiagnosis Problem— but Clinicians Can (Phelps, 2013)