Advanced Nursing Skills Day Keith Rischer RN MA
- Slides: 38
Advanced Nursing Skills Day Keith Rischer RN, MA, CEN 1
Today’s Objectives… IV Meds Ø In a simulated clinical situation, demonstrate hanging an IV piggyback and calculate correct rate and set up on Horizon pump. Ø In a simulated clinical situation, demonstrate calculation to safely administer IV medication bolus per PDA and administer. Ø In a simulated clinical situation, calculate correct dose of Heparin bolus and drip rate per SCH policy and protocol. Carb Counting-Insulin Ø In a simulated clinical situation, calculate the correct dose of insulin to administer based on CHO intake at meal. Ø In a simulated clinical situation, based on sliding scale calculate the correct dose to administer and demonstrate correct technique to mix Regular and NPH or Lente. Ø Demonstrate correct technique to administer insulin via insulin pen. 2
Today’s Objectives… IV Insertion Ø State the veins of the hands and arms that could be used for intravenous insertion for all ages. Ø Implement measures to promote venous distention. Ø State potential complications when initiating IV therapy and measures to prevent complications. Ø Demonstrate IV insertion, dressing of the IV site and application of a saline lock safely with the simulation arm. Central-Arterial Lines Ø Identify indications for placement of central/arterial lines. Ø Identify significance of CVP and normal ranges Ø Describe nursing responsibilities and priorities for the client with central/arterial lines. Ø State potential complications and measures to prevent complications with central/arterial lines. 3
Today’s Objectives… Chest Tubes Ø Identify indications for placement of chest tubes. Ø Describe the principles and patho that support the use of chest tubes. Ø Describe nursing responsibilities and priorities for the client with chest tubes. Ø Identify significance of bubbling in the waterseal chamber and what assessments are required by nurse. ET-Ventilator Ø Identify indications for placement of endotracheal tube/ventilator. Ø Describe nursing responsibilities and priorities for the client during intubation with ventilator. Ø Identify principles of ABG interpretation and relevance to ventilator management. Ø Describe different modes of ventilation and significance of ventilator settings. Ø State potential complications and measures to prevent complications with ventilator. 4
Insulin & Carb Counting Ø Time action profiles of… • • Novolog Regular Lente NPH Mixing Ø Insulin pen Ø 5
IV Med Administration Principles COMPATIBILITY Ø Correctly calculate rate of IV push to q 1530 seconds Ø Label all syringes brought into room once aspirated Ø Assess site Ø Aseptic technique w/port Ø Knowledge of most common side effects Ø 6
IV Meds Ø IV Push • • Ø IV Piggyback • • Ø Morphine 4 mg/1 cc PDA 1 mg per minute…how much volume q minute Rocephin 1 Gram in 50 cc bag Give over 30”-what do you set IV pump to infuse IV Heparin • • 215 lbs. 70 u/kg bolus…. 15 u/kg hourly rate 7
SAVE that Line! ØS: Scrupulous hand hygiene • Before and after contact w/vascular access device and prior to insertion ØA: Aseptic technique • During catheter insertion & care ØV: Vigorous friction to hubs • With alcohol whenever you make or break a connection to give meds, flush ØE: Ensure patency • Flush all lumens w/adequate amount of saline or heparin to maintain patency per hospital policy 8
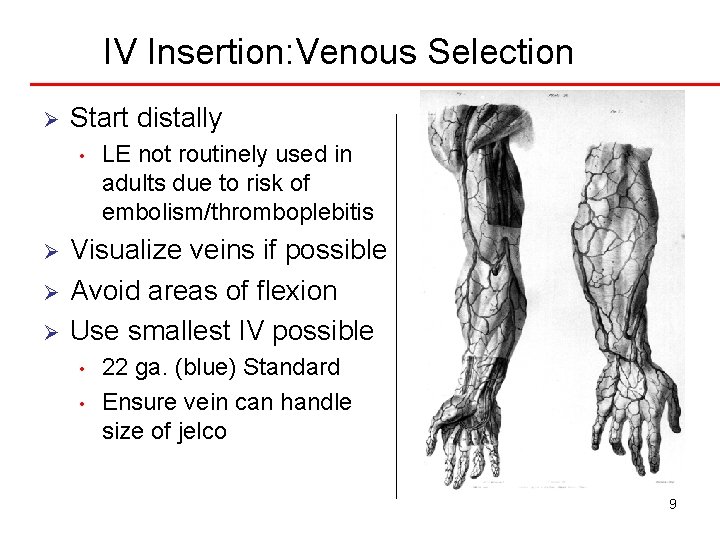
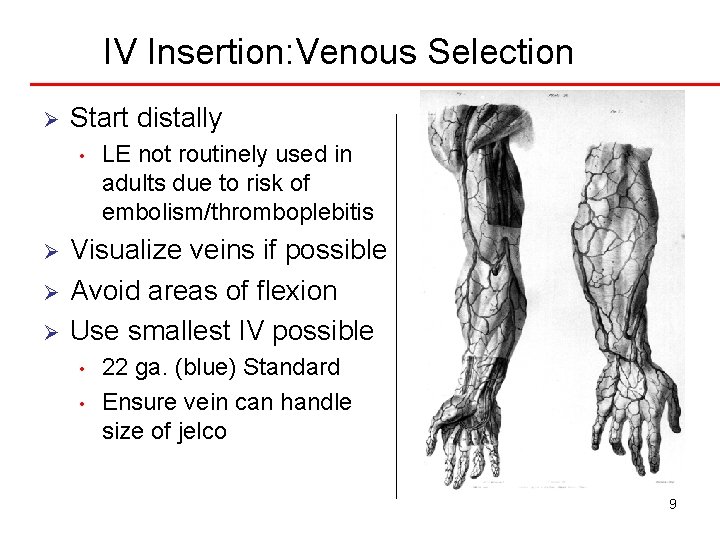
IV Insertion: Venous Selection Ø Start distally • Ø Ø Ø LE not routinely used in adults due to risk of embolism/thromboplebitis Visualize veins if possible Avoid areas of flexion Use smallest IV possible • • 22 ga. (blue) Standard Ensure vein can handle size of jelco 9
Principles of IV Therapy BP cuff-keep on opposite arm if continuous IV infusion Ø Do not use PIV same side as pt. who has had axillary node dissection, dialysis shunt Ø Hair removal if needed-use clippers or scissors Ø 10
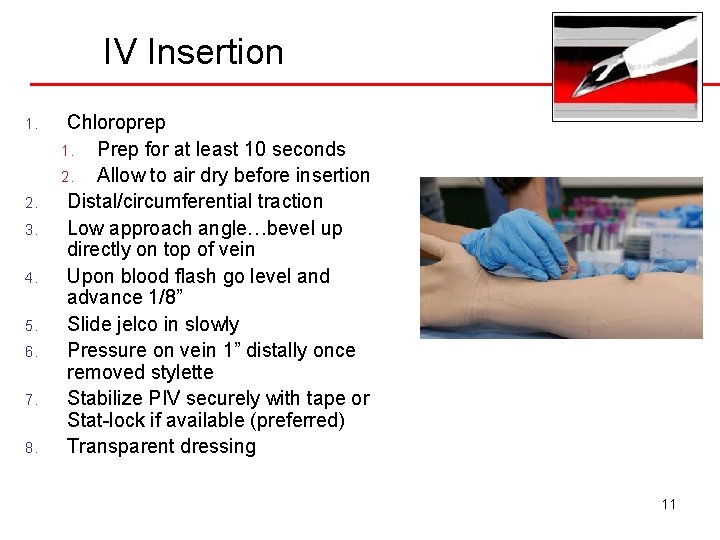
IV Insertion 1. 2. 3. 4. 5. 6. 7. 8. Chloroprep 1. Prep for at least 10 seconds 2. Allow to air dry before insertion Distal/circumferential traction Low approach angle…bevel up directly on top of vein Upon blood flash go level and advance 1/8” Slide jelco in slowly Pressure on vein 1” distally once removed stylette Stabilize PIV securely with tape or Stat-lock if available (preferred) Transparent dressing 11
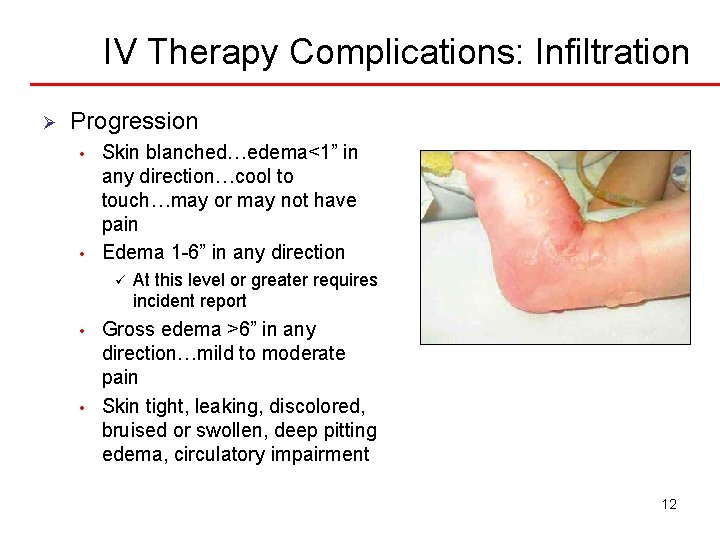
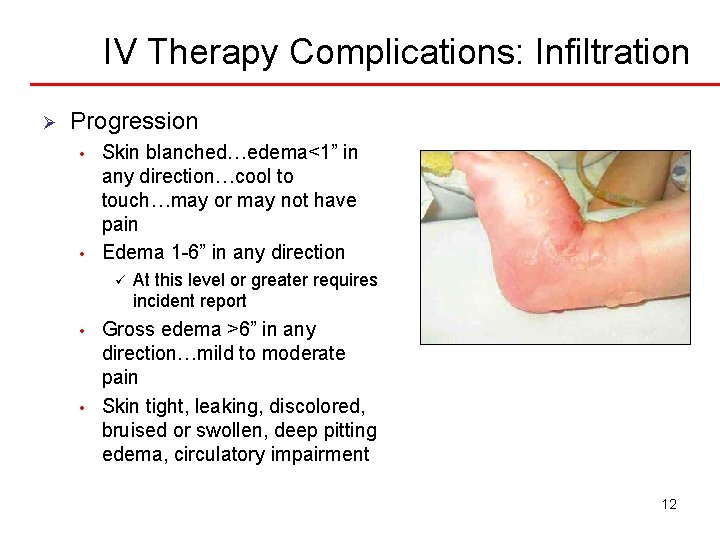
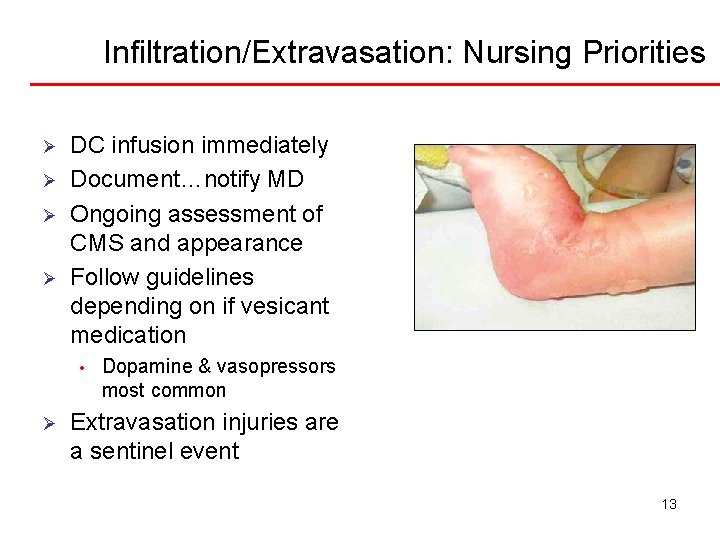
IV Therapy Complications: Infiltration Ø Progression • • Skin blanched…edema<1” in any direction…cool to touch…may or may not have pain Edema 1 -6” in any direction ü • • At this level or greater requires incident report Gross edema >6” in any direction…mild to moderate pain Skin tight, leaking, discolored, bruised or swollen, deep pitting edema, circulatory impairment 12
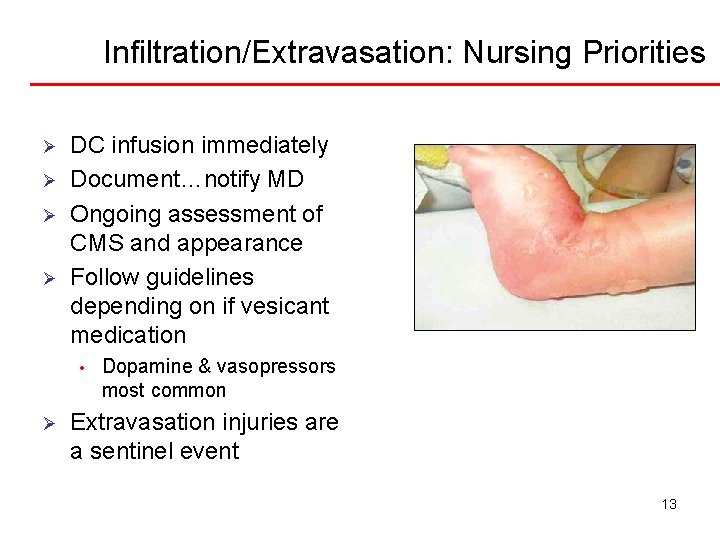
Infiltration/Extravasation: Nursing Priorities Ø Ø DC infusion immediately Document…notify MD Ongoing assessment of CMS and appearance Follow guidelines depending on if vesicant medication • Ø Dopamine & vasopressors most common Extravasation injuries are a sentinel event 13
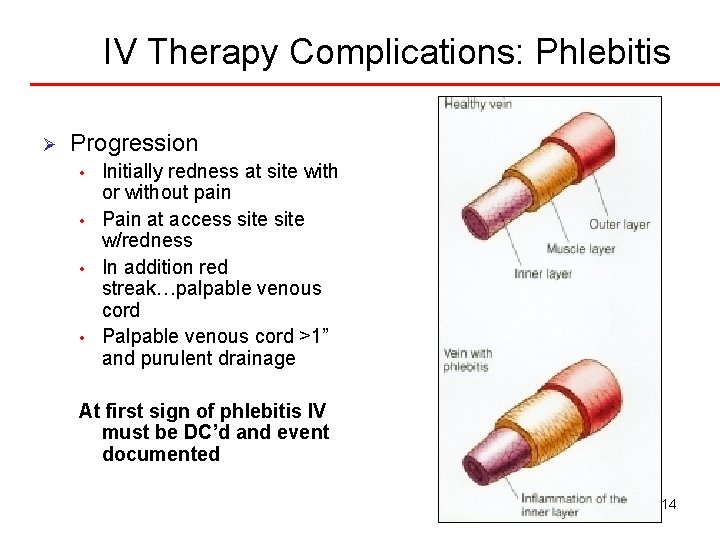
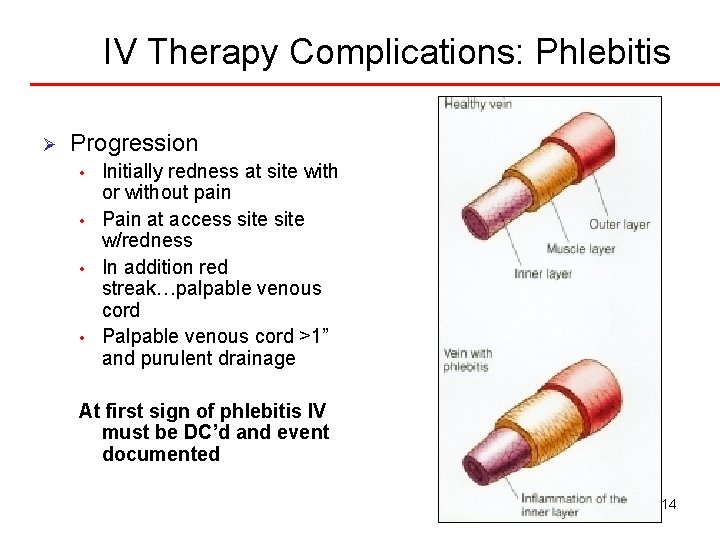
IV Therapy Complications: Phlebitis Ø Progression • • Initially redness at site with or without pain Pain at access site w/redness In addition red streak…palpable venous cord Palpable venous cord >1” and purulent drainage At first sign of phlebitis IV must be DC’d and event documented 14
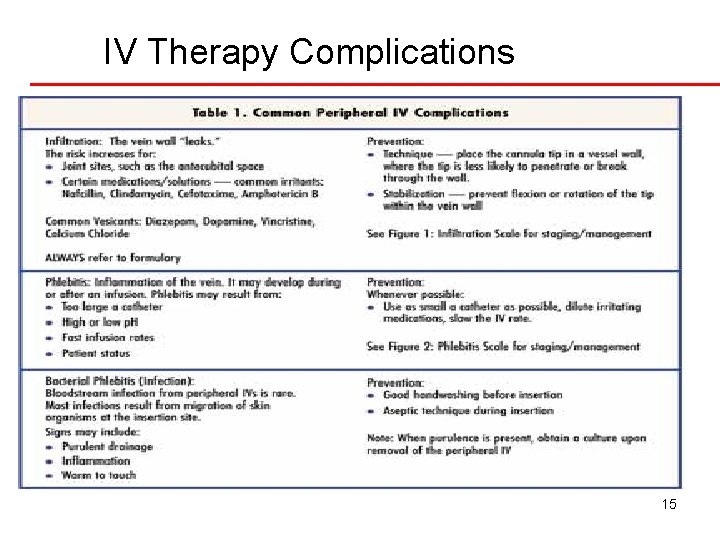
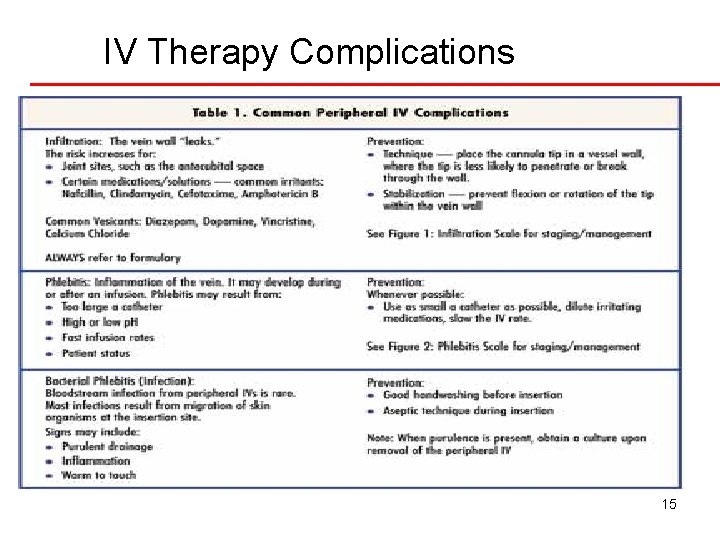
IV Therapy Complications 15
IV Therapy Complications: Infection Ø Prevention • • Ø Use aseptic technique when accessing ports and upon insertion Monitor site and integrity of dressing Infection Present • • Blood cultures from catheter and separate venous site Monitor for sepsis 16
Site Assessment • • • Assess tenderness by palpation Redness Moisture/leaking Swelling distally if continous infusion Dressing labeled ü Date inserted ü Size of IV jelco ü Initials of nurse • If >4 days since inserted DC and restart 17
Nursing Responsibilities Ø Ø Frequent IV site assessment Be aware of medications that irritate vein Vigilant with meds that can cause cellular damage if infiltrate Infiltrated? • • Stop IV immediately Elevate extremity Warm packs Check w/pharmacy if additional measures needed 18
Nursing Responsibilities Ø Primary/secondary tubing changed per hospital policy • • Q 4 days (ANW) TPN/Lipids changed q day Intermittent IVPB tubing changed q 24 hours Ø When IV dc’d assess site and make sure jelco tip intact Ø If Heparin used to flush central access device…assess for HIT Ø 19
PIV Troubleshooting Ø Pain • Ø Distal occlusion alarm on IV pump • • Ø AC site-extend arm Flush site and assess for occlusion Leakage • Ø Assess site…always a red flag and IV should be DC’d unless has irritating solution infusing Make sure is not from loose attachment to jelco ? Infiltration • • Flush IV slowly w/5 -10 cc NS Assess for leakage/swelling/pain 20
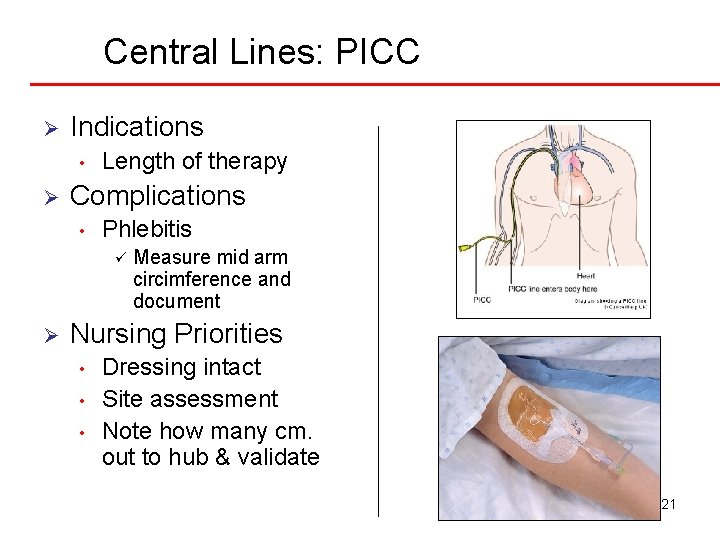
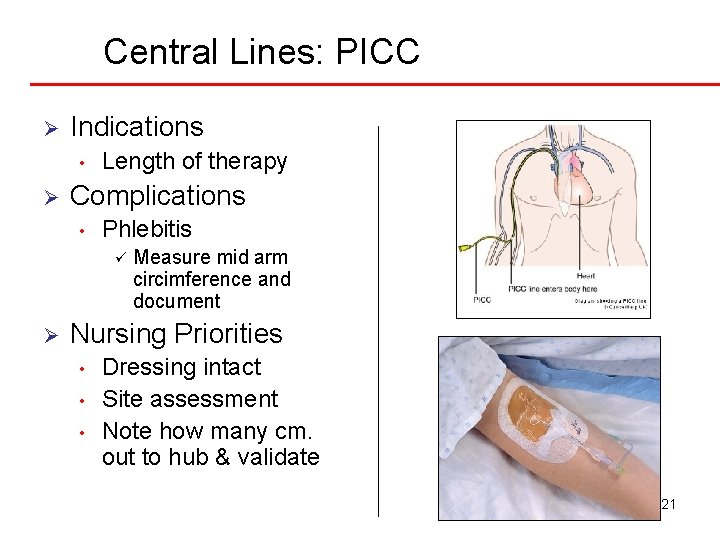
Central Lines: PICC Ø Indications • Ø Length of therapy Complications • Phlebitis ü Ø Measure mid arm circimference and document Nursing Priorities • • • Dressing intact Site assessment Note how many cm. out to hub & validate 21
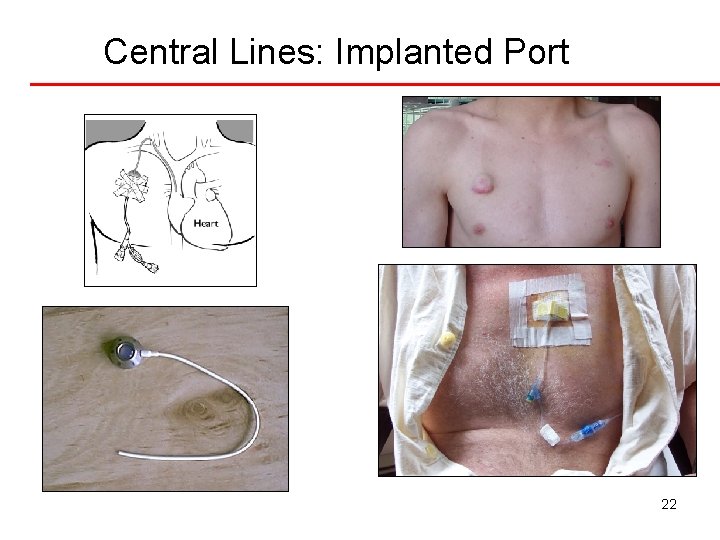
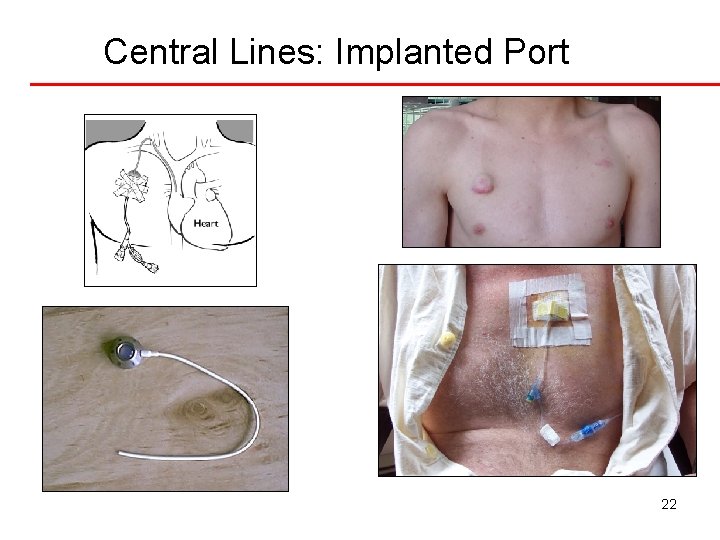
Central Lines: Implanted Port 22
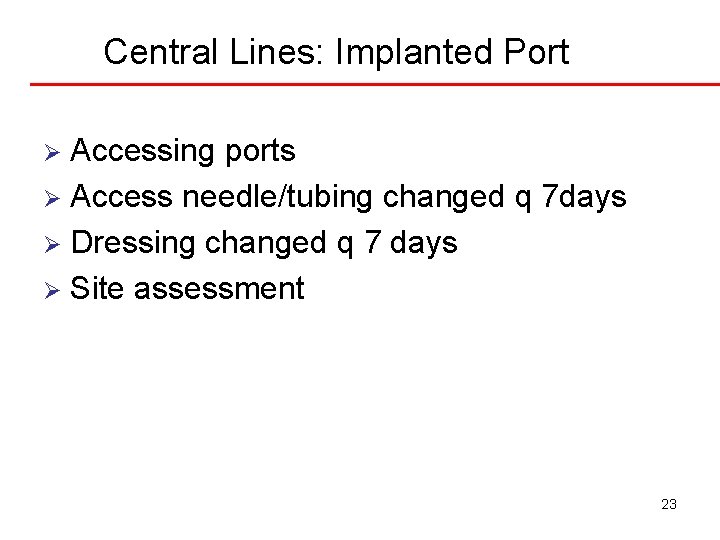
Central Lines: Implanted Port Accessing ports Ø Access needle/tubing changed q 7 days Ø Dressing changed q 7 days Ø Site assessment Ø 23
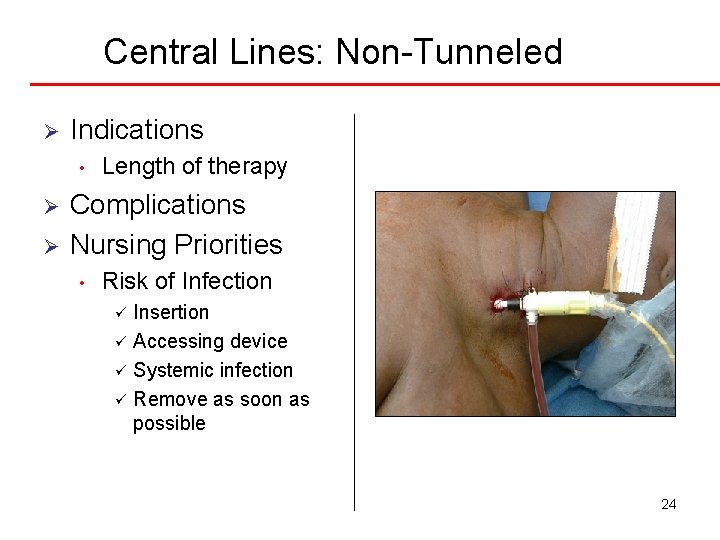
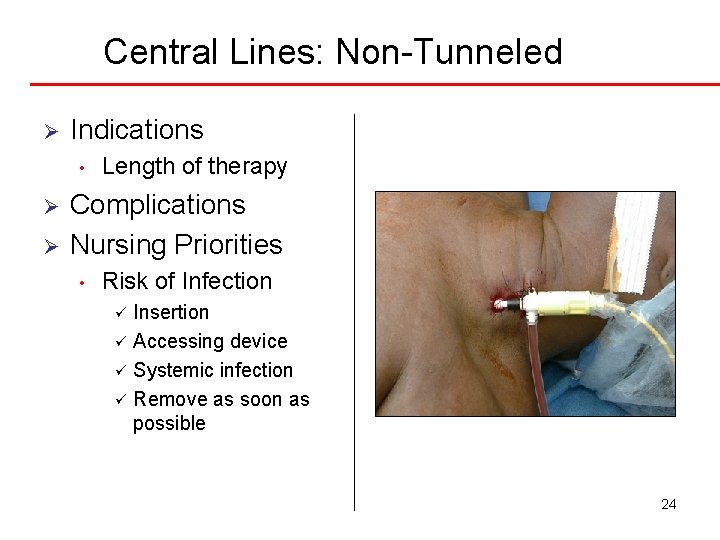
Central Lines: Non-Tunneled Ø Indications • Ø Ø Length of therapy Complications Nursing Priorities • Risk of Infection Insertion ü Accessing device ü Systemic infection ü Remove as soon as possible ü 24
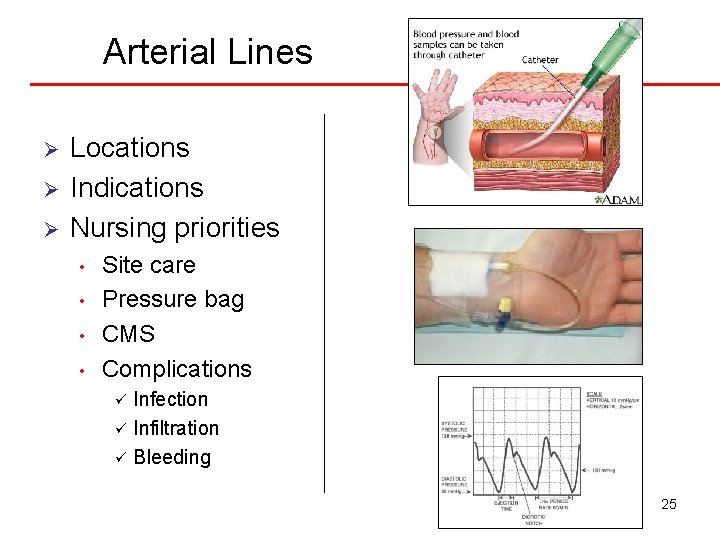
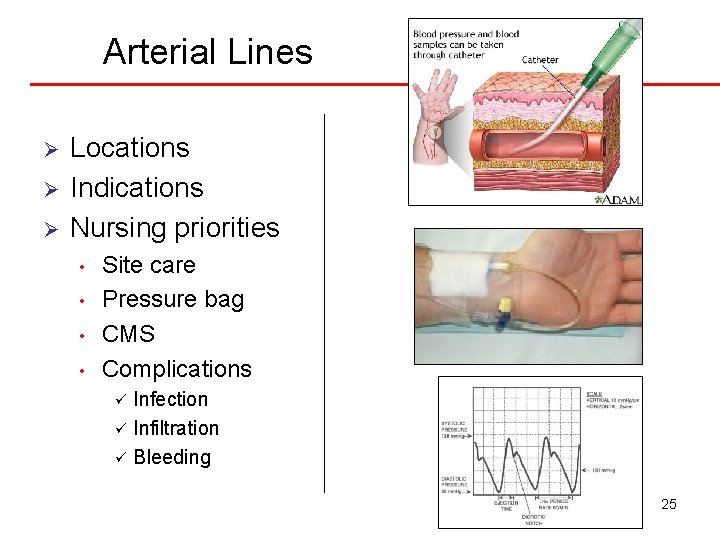
Arterial Lines Ø Ø Ø Locations Indications Nursing priorities • • Site care Pressure bag CMS Complications Infection ü Infiltration ü Bleeding ü 25
Blood Product Administration Minimum 22 g. (blue hub) IV-prefer 20 g. (pink) or 18 g. (green) Ø Informed consent obtained Ø Administer within 30” once received from Blood Bank Ø Blood tubing with filter-use NS to prime/flush Ø • • Validate pt. , type of blood product, expiration date, blood tag # VS before, 15” after initiation, end of each Infuse PRBC’s over 2 hours (appx 300 cc/unit) Consider Lasix chaser if hx CHF 26
Complications Blood Products Ø Circulatory Overload Acute Hemolytic Reaction • Chills, fever, flushing, tachycardia, SOB, hypotension, acute renal failure, shock, cardiac arrest, death Febrile-Nonhemolytic Reaction • Sudden onset of chills, fever, temp elevation >1 degree C. headache, anxiety Mild Allergic Reaction • Flushing, urticaria, hives 27
Nursing Responsibilities STOP transfusion Ø Maintain IV site-disconnect from IV and flush with NS Ø Notify blood bank/MD Ø Recheck ID Ø Monitor VS Ø Treat sx per MD orders Ø Save bag and tubing-send to blood bank Ø 28
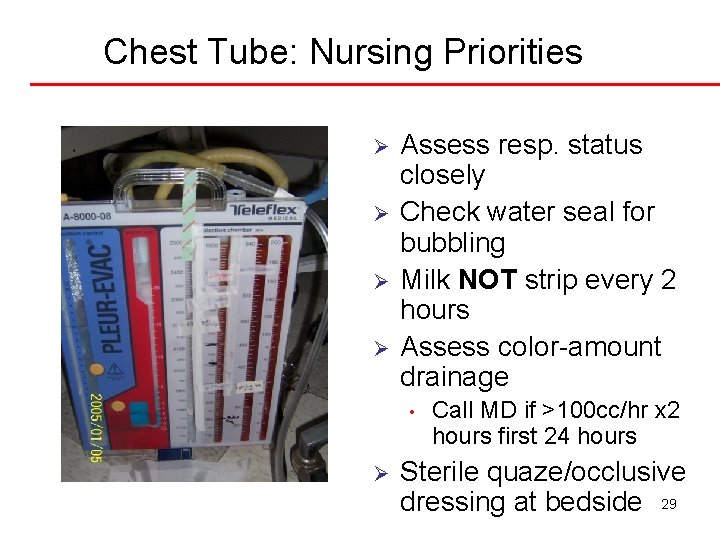
Chest Tube: Nursing Priorities Ø Ø Assess resp. status closely Check water seal for bubbling Milk NOT strip every 2 hours Assess color-amount drainage • Ø Call MD if >100 cc/hr x 2 hours first 24 hours Sterile quaze/occlusive dressing at bedside 29
Mechanical Ventilation Ø Ø The use of an ET and POSITIVE pressure to deliver O 2 at preset tidal volume Modes • Assist Control (AC) ü ü • Synchronized Intermittent Mandatory Ventilation (SIMV) ü ü • • TV & rate preset Additional resp. receive preset TV Additional resp. receive own TV Used for weaning Continuous Positive Airway Pressure (CPAP) Bi-pap ü ü Non-mechanical receive both insp. & exp. Pressures w/facemask 30
Mechanical Ventilation Ø Terminology • • Rate Tidal volume ü • Fraction of inspired O 2 concentration (Fi. O 2) ü • • Use lowest possible to maintain O 2 sats Positive End Expiratory Pressure (PEEP) Minute volume ü Ø 10 -15 cc/kg RR x TV AC 12 -TV 600 -50%-+5 31
Mechanical Ventilation: Adverse Effects Ø Complications • • • Aspiration Infection-VAP Stress ulcer of GI tract Tracheal damage Ventilator dependancy Decreased cardiac output ü • Positive pressure decr. venous return & CO Barotrauma ü pneumothorax 32
Mechanical Ventilation: Nursing Priorities Ø Ø Ø Monitor VS-breath sounds closely Assess ET securement/length at lip Clearance of secretions • • • Ø Sedation • Ø Ø Closed suction-maintains sterility Do not do routinely Pre-oxygenate Propofol Oral care Nutritional support 33
Mechanical Ventilation: Nursing Priorities Ø Ventilator Alarm Troubleshooting • High pressure ü Secretions-needs sx ü Tubing obstructed or kinked ü Biting ET • Low pressure ü Disconnection of tubing ü Follow tubing from ET to ventilator 34
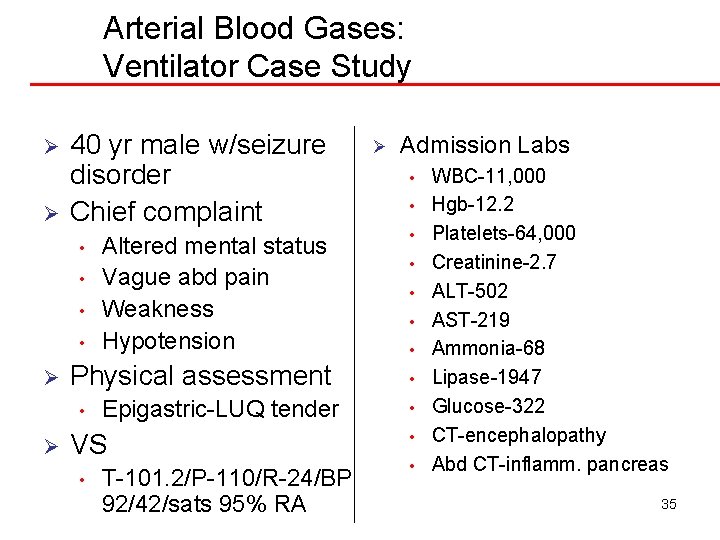
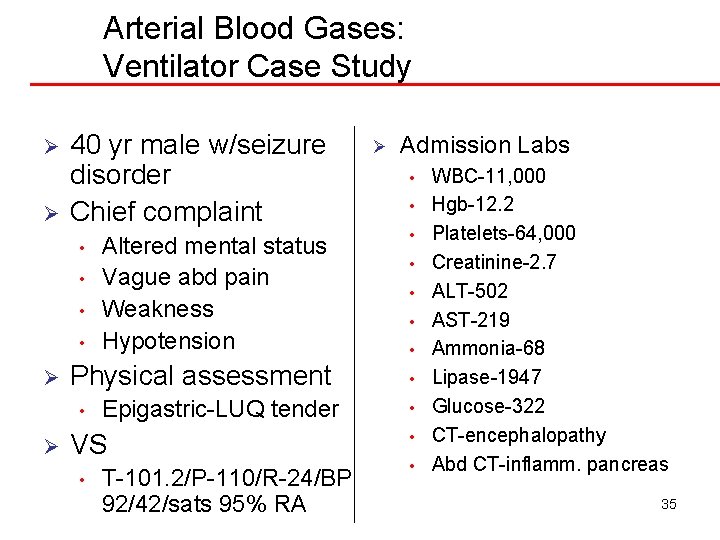
Arterial Blood Gases: Ventilator Case Study Ø Ø 40 yr male w/seizure disorder Chief complaint • • Ø Physical assessment • Ø Altered mental status Vague abd pain Weakness Hypotension Epigastric-LUQ tender VS • T-101. 2/P-110/R-24/BP 92/42/sats 95% RA Ø Admission Labs • • • WBC-11, 000 Hgb-12. 2 Platelets-64, 000 Creatinine-2. 7 ALT-502 AST-219 Ammonia-68 Lipase-1947 Glucose-322 CT-encephalopathy Abd CT-inflamm. pancreas 35
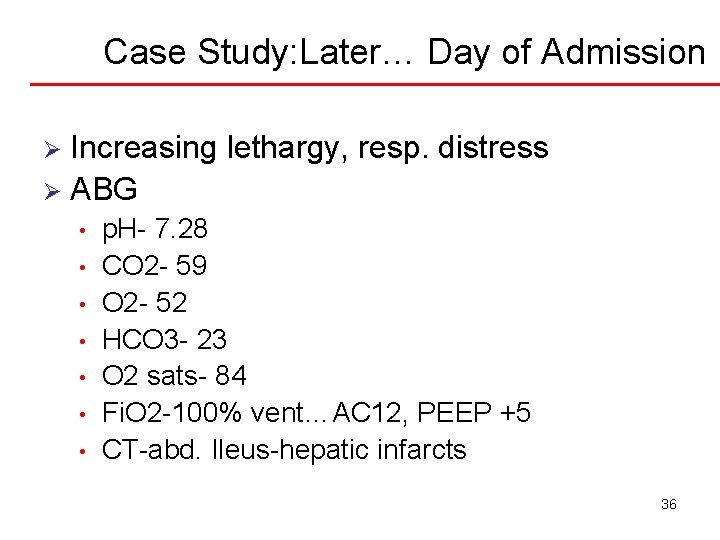
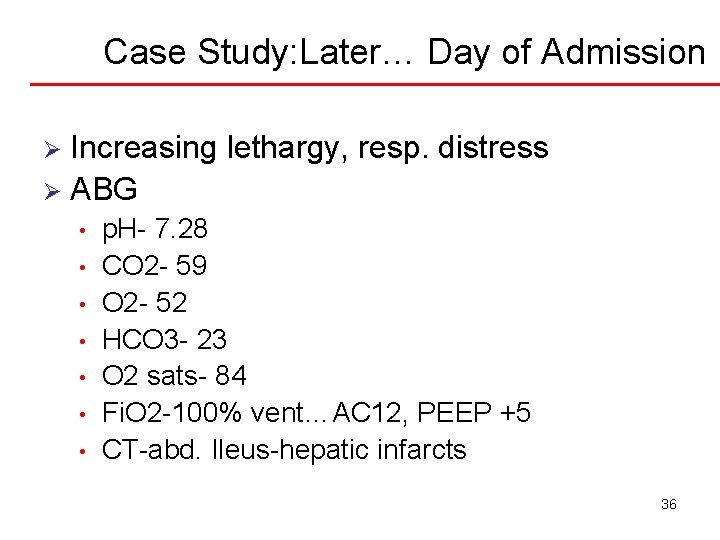
Case Study: Later… Day of Admission Increasing lethargy, resp. distress Ø ABG Ø • • p. H- 7. 28 CO 2 - 59 O 2 - 52 HCO 3 - 23 O 2 sats- 84 Fi. O 2 -100% vent…AC 12, PEEP +5 CT-abd. Ileus-hepatic infarcts 36
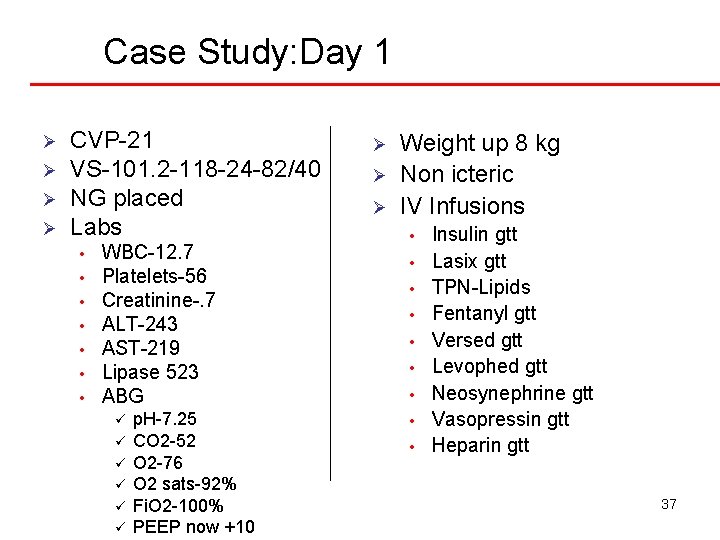
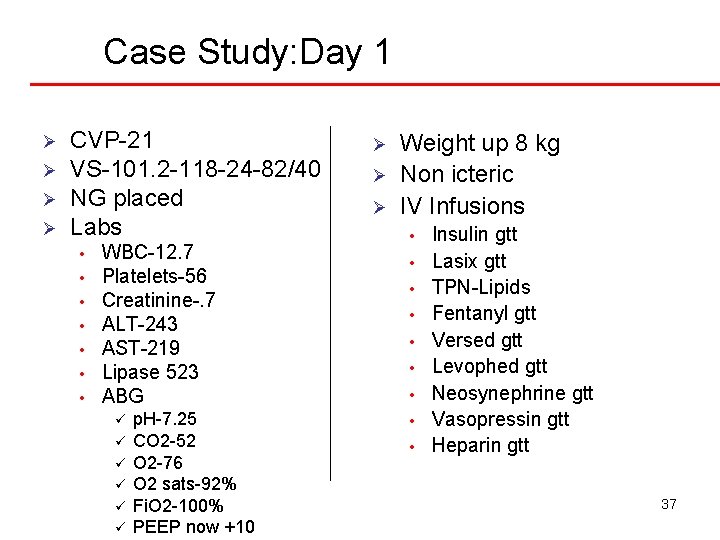
Case Study: Day 1 Ø Ø CVP-21 VS-101. 2 -118 -24 -82/40 NG placed Labs • • WBC-12. 7 Platelets-56 Creatinine-. 7 ALT-243 AST-219 Lipase 523 ABG ü ü ü p. H-7. 25 CO 2 -52 O 2 -76 O 2 sats-92% Fi. O 2 -100% PEEP now +10 Ø Ø Ø Weight up 8 kg Non icteric IV Infusions • • • Insulin gtt Lasix gtt TPN-Lipids Fentanyl gtt Versed gtt Levophed gtt Neosynephrine gtt Vasopressin gtt Heparin gtt 37
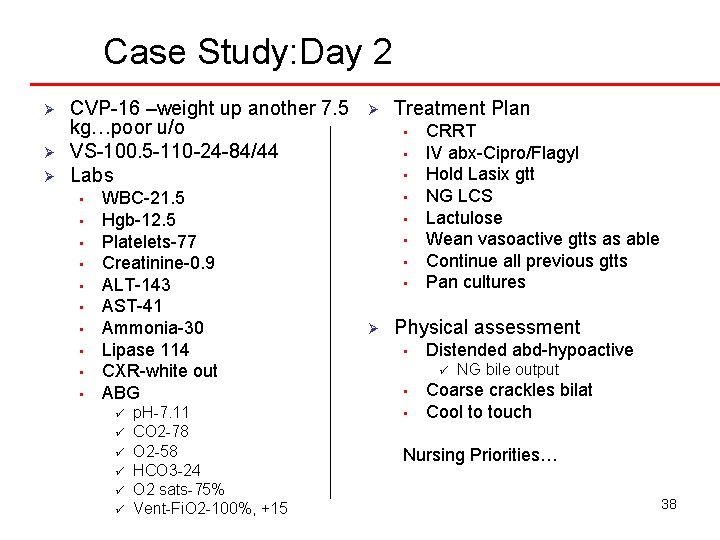
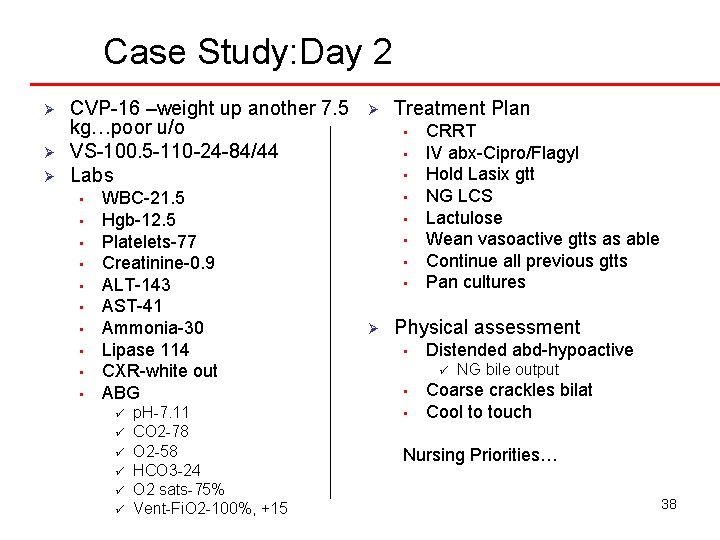
Case Study: Day 2 Ø Ø Ø CVP-16 –weight up another 7. 5 kg…poor u/o VS-100. 5 -110 -24 -84/44 Labs • • • WBC-21. 5 Hgb-12. 5 Platelets-77 Creatinine-0. 9 ALT-143 AST-41 Ammonia-30 Lipase 114 CXR-white out ABG ü ü ü p. H-7. 11 CO 2 -78 O 2 -58 HCO 3 -24 O 2 sats-75% Vent-Fi. O 2 -100%, +15 Ø Treatment Plan • • Ø CRRT IV abx-Cipro/Flagyl Hold Lasix gtt NG LCS Lactulose Wean vasoactive gtts as able Continue all previous gtts Pan cultures Physical assessment • Distended abd-hypoactive ü • • NG bile output Coarse crackles bilat Cool to touch Nursing Priorities… 38