Advanced Fetal Monitoring A Multidisciplinary Approach to Promote
- Slides: 19
Advanced Fetal Monitoring: A Multidisciplinary Approach to Promote Patient Safety and Reduce Risk for Litigation 2016 Conference Outcomes and Survey Results Joan E. Edwards, Ph. D, RNC, CNS, FAAN jedwards 3@twu. edu
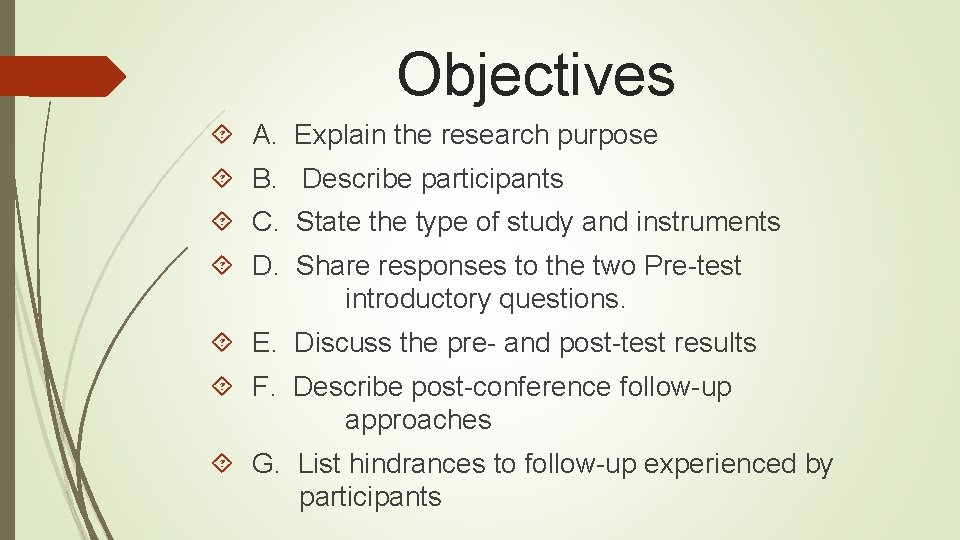
Objectives A. Explain the research purpose B. Describe participants C. State the type of study and instruments D. Share responses to the two Pre-test introductory questions. E. Discuss the pre- and post-test results F. Describe post-conference follow-up approaches G. List hindrances to follow-up experienced by participants
Communication and Collaboration Morbidity/Mortality (Kasselbaum et al. , 2014) Patient safety and quality issues (The Joint Commission, 2008) Standardization of evidence-based interdisciplinary team work training and education (Contratti et al. , 2012; Miller & Miller, 2013; Maxfield, et al. , 2013; Riley et al. , 2016) Communication, common terminology and interprofessional teamwork (Contratti et al. , 2012; Harper and Maloney, 2016; Klipfel et al. , 2014; Lyndon, 2006; Lyndon et al. , 2011; Lyndon et al. , 2015; Matzke et al. , 2014; Maxfield et al. , 2013; Riley et al, 2016; Simpson, 2005) Timeliness of Interventions (Lyndon et al. , 2015; Riley et al. , 2016)
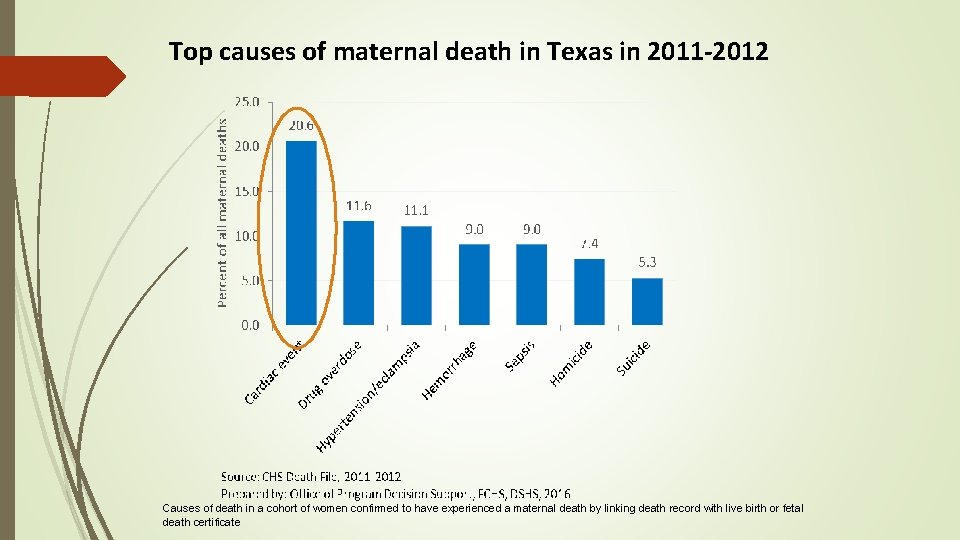
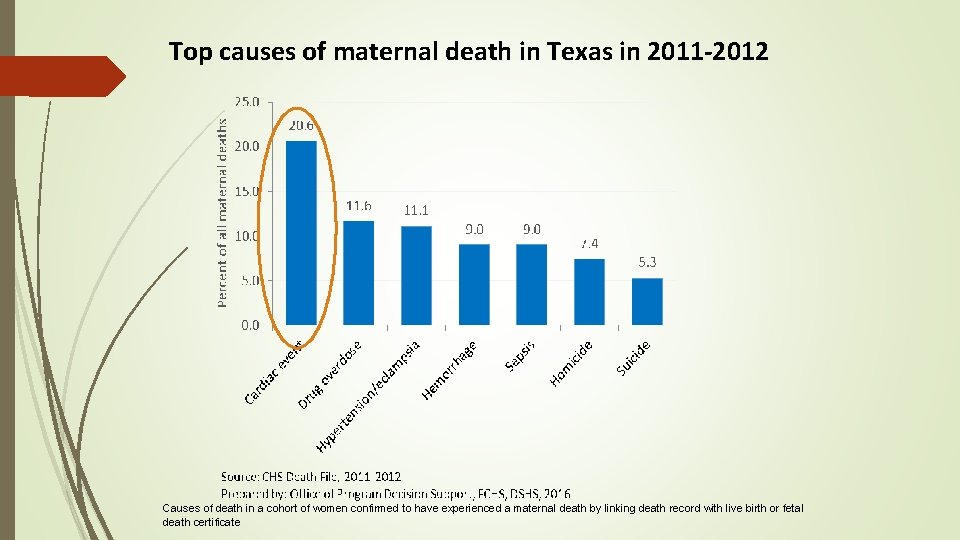
Top causes of maternal death in Texas in 2011 -2012 Causes of death in a cohort of women confirmed to have experienced a maternal death by linking death record with live birth or fetal death certificate
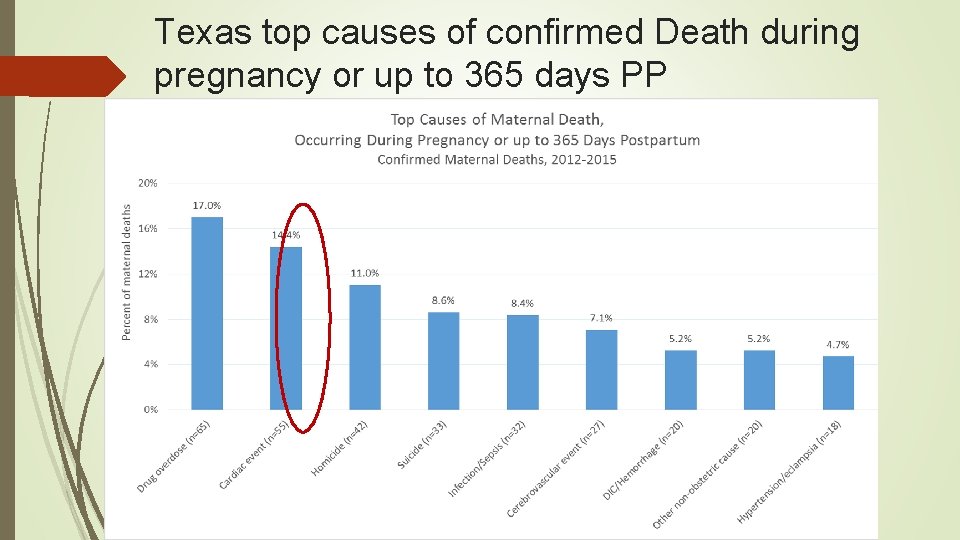
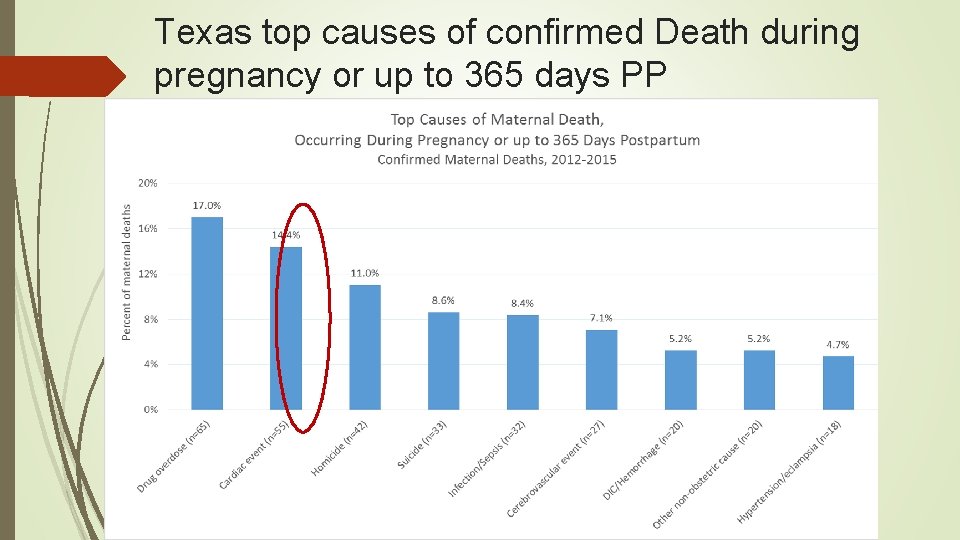
Texas top causes of confirmed Death during pregnancy or up to 365 days PP
Miller & Miller Conference Objectives Identify common areas of team failure related to EFM Discuss a standardized, inter-disciplinary evidence based approaches to intrapartum collaboration Apply standardized terminology and principles of interpretation to FHR tracings
Dr. Joanie Hare
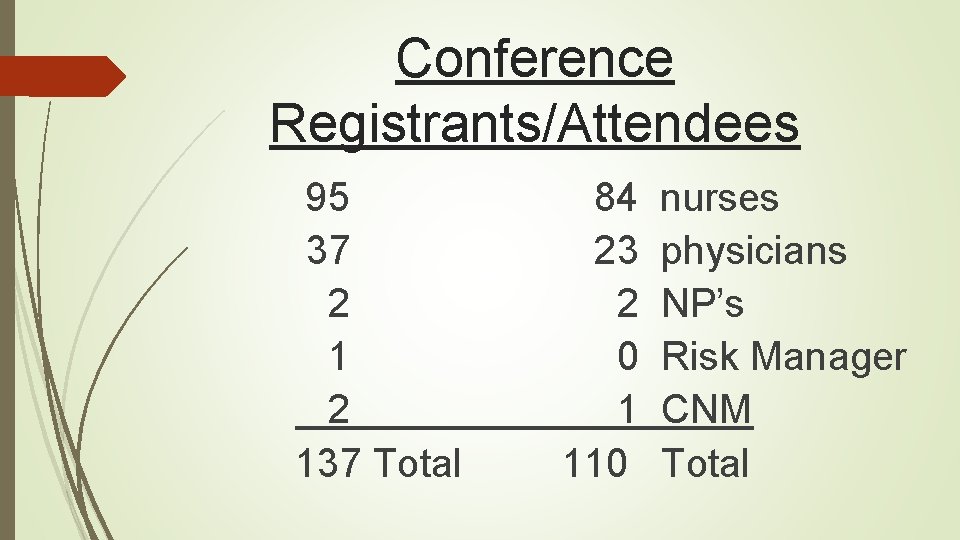
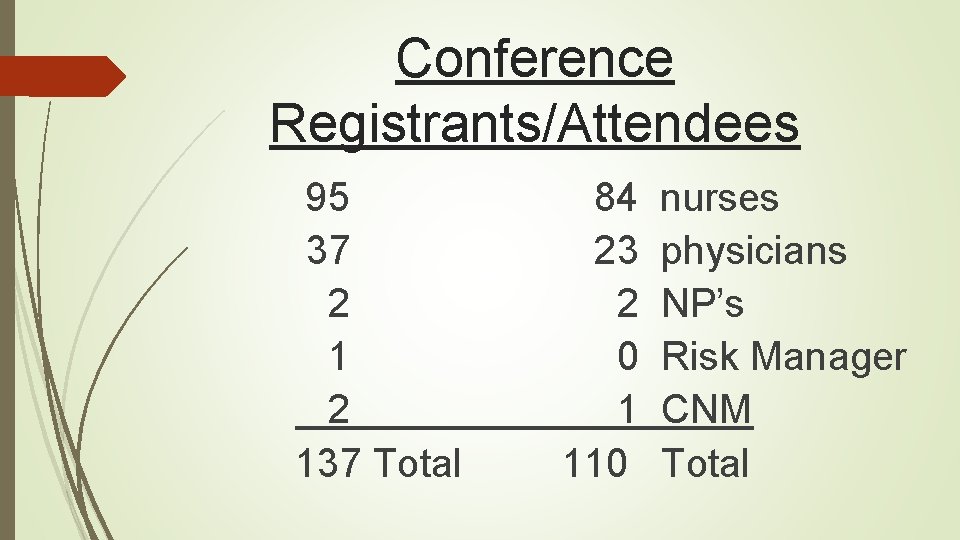
Conference Registrants/Attendees 95 37 2 137 Total 84 23 2 0 1 110 nurses physicians NP’s Risk Manager CNM Total
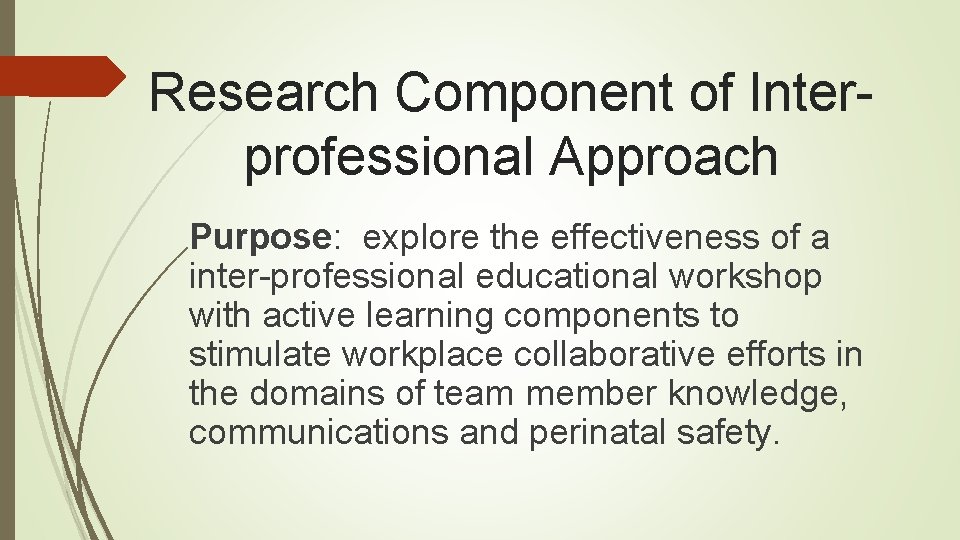
Research Component of Interprofessional Approach Purpose: explore the effectiveness of a inter-professional educational workshop with active learning components to stimulate workplace collaborative efforts in the domains of team member knowledge, communications and perinatal safety.
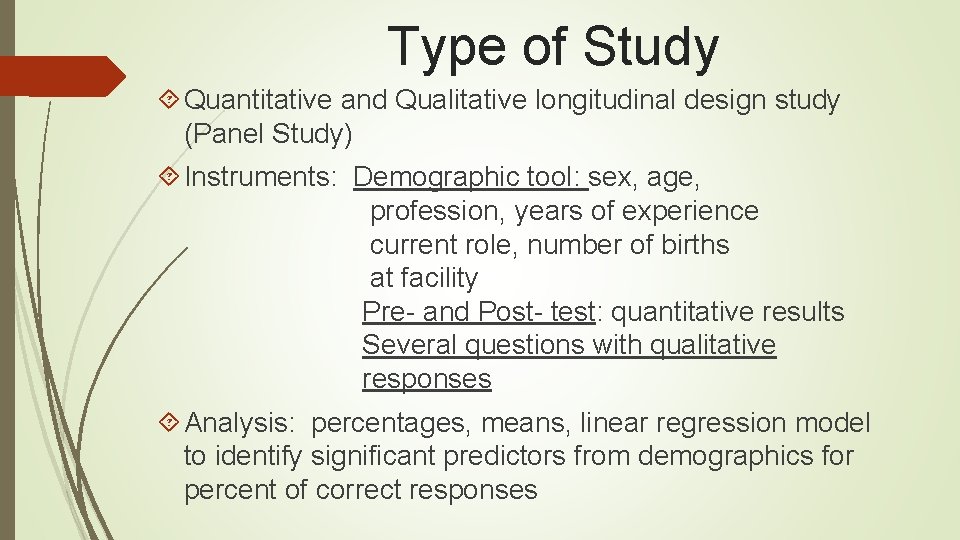
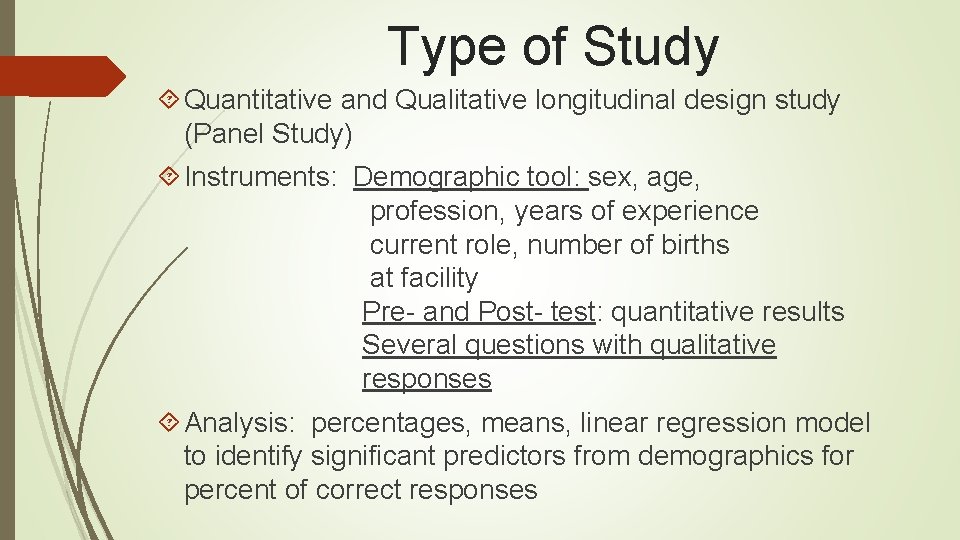
Type of Study Quantitative and Qualitative longitudinal design study (Panel Study) Instruments: Demographic tool: sex, age, profession, years of experience current role, number of births at facility Pre- and Post- test: quantitative results Several questions with qualitative responses Analysis: percentages, means, linear regression model to identify significant predictors from demographics for percent of correct responses
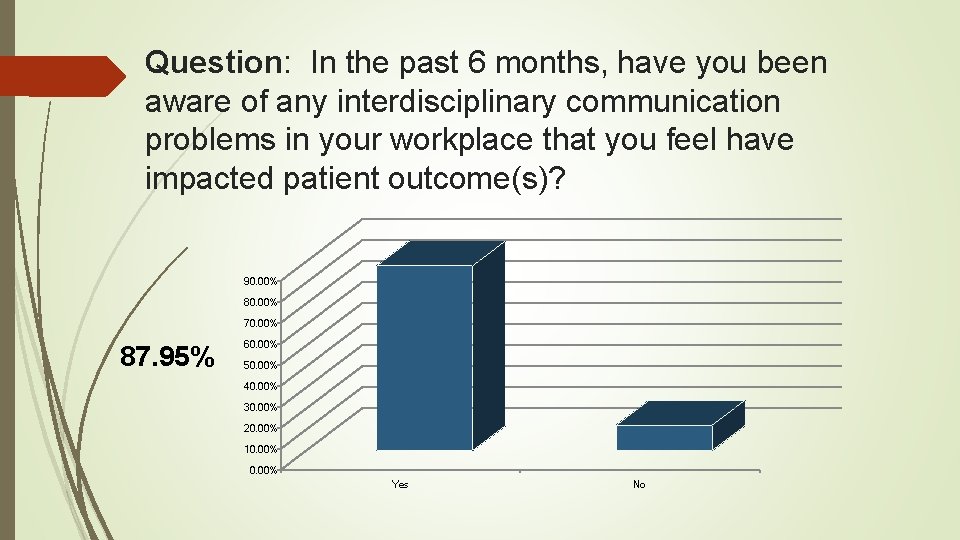
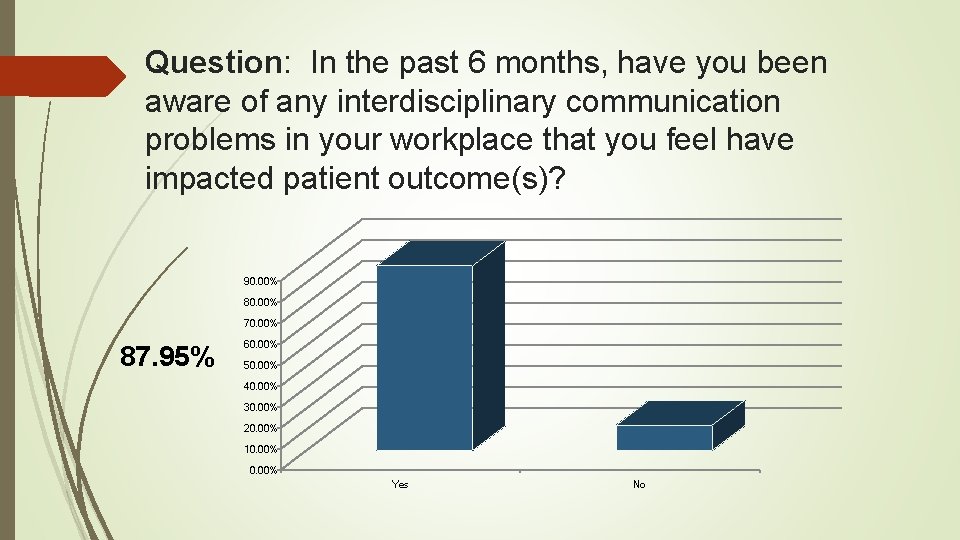
Question: In the past 6 months, have you been aware of any interdisciplinary communication problems in your workplace that you feel have impacted patient outcome(s)? 90. 00% 80. 00% 70. 00% 87. 95% 60. 00% 50. 00% 40. 00% 30. 00% 20. 00% 10. 00% Yes No
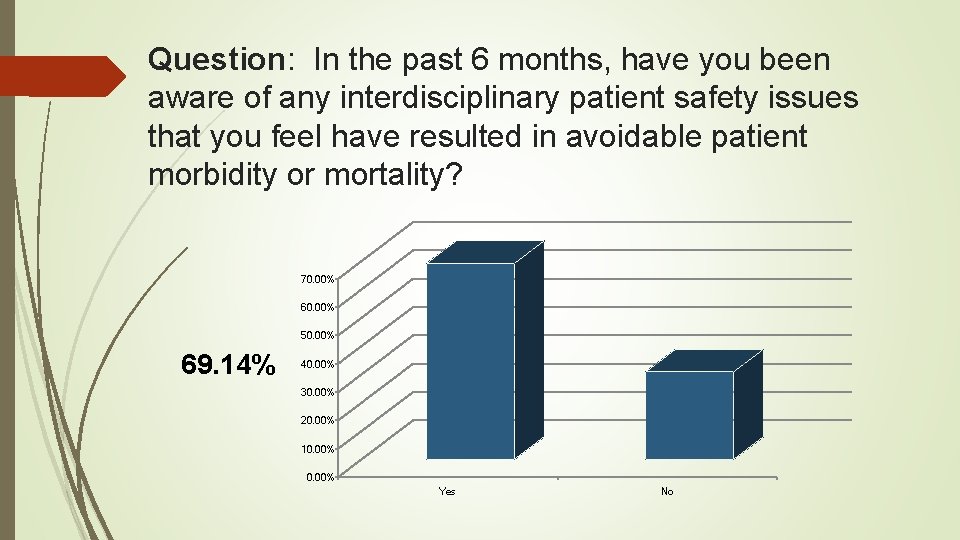
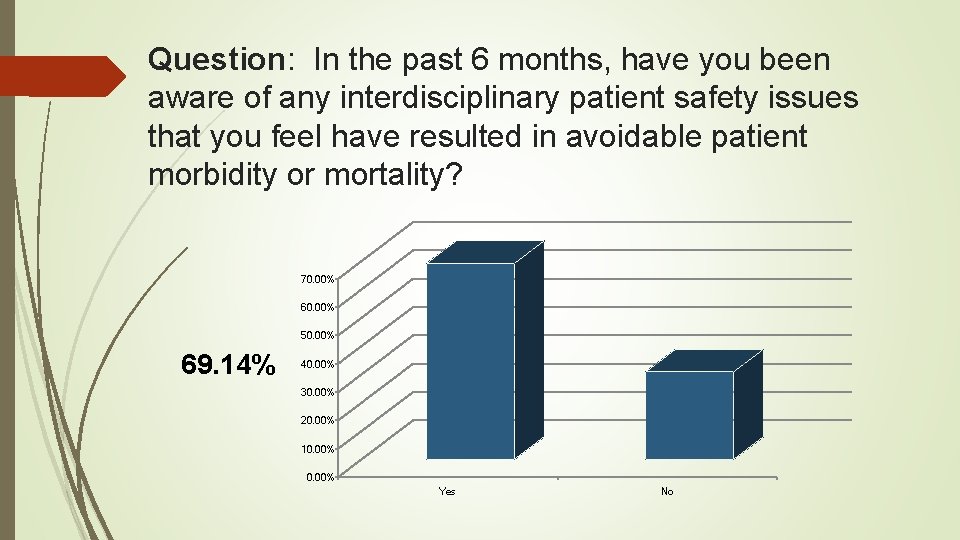
Question: In the past 6 months, have you been aware of any interdisciplinary patient safety issues that you feel have resulted in avoidable patient morbidity or mortality? 70. 00% 60. 00% 50. 00% 69. 14% 40. 00% 30. 00% 20. 00% 10. 00% Yes No
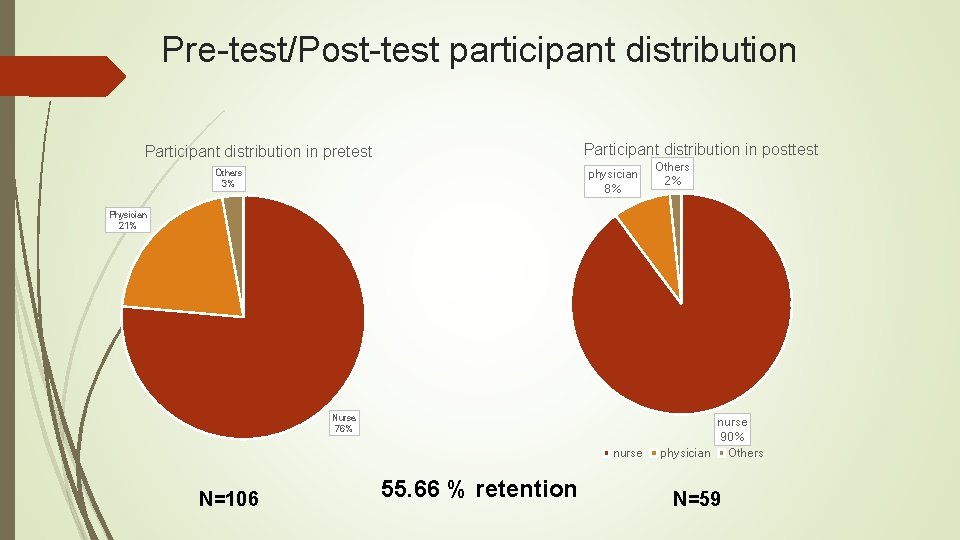
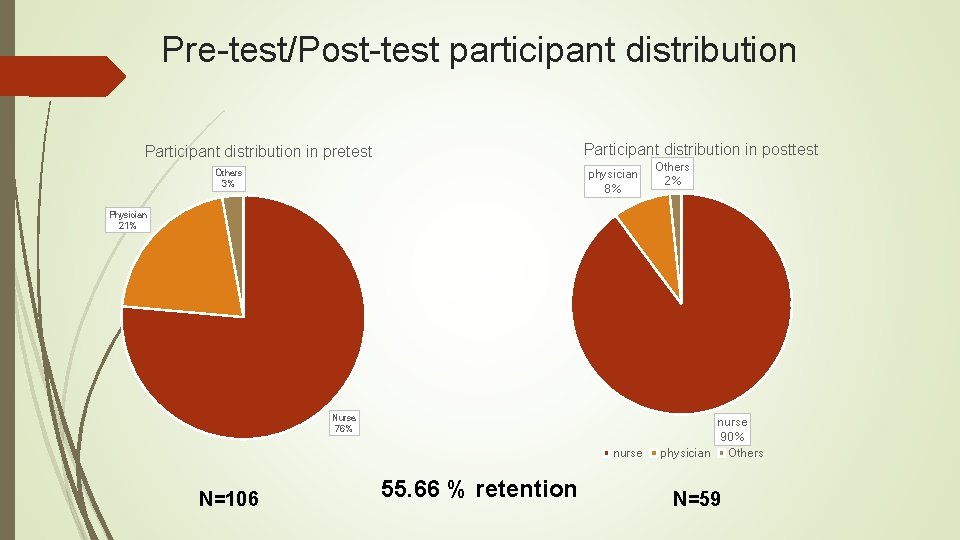
Pre-test/Post-test participant distribution Participant distribution in posttest Participant distribution in pretest physician 8% Others 3% Others 2% Physician 21% Nurse 76% nurse N=106 55. 66 % retention nurse 90% physician Others N=59
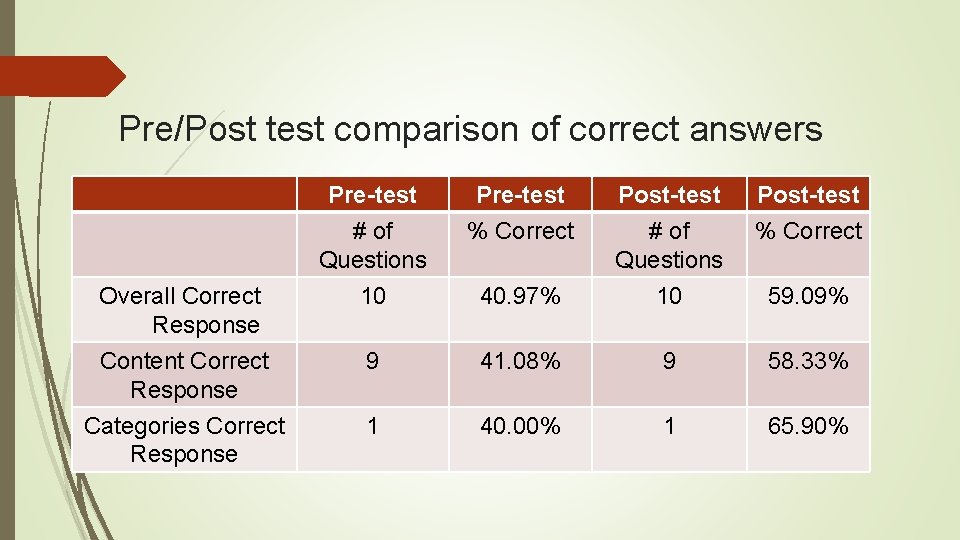
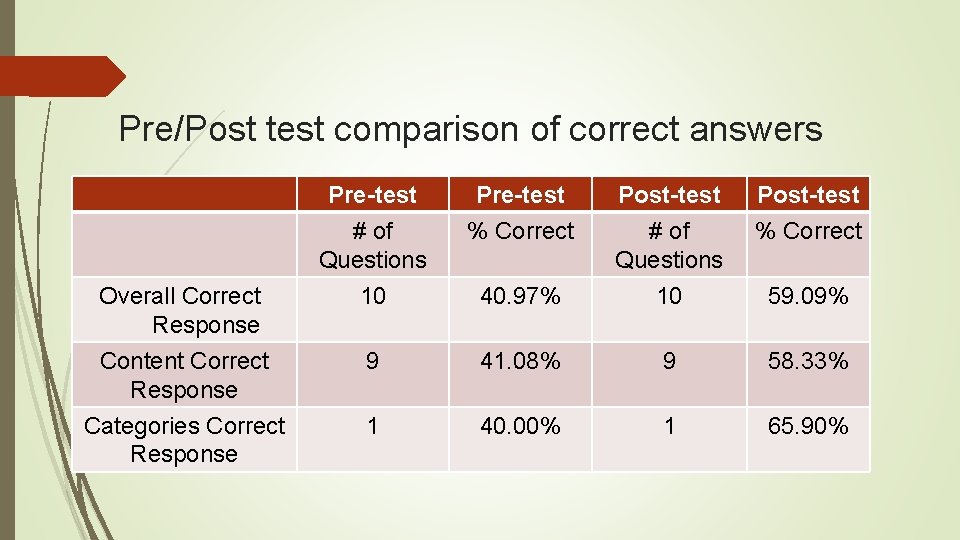
Pre/Post test comparison of correct answers Overall Correct Response Content Correct Response Categories Correct Response Pre test # of Questions 10 Pre test % Correct Post test % Correct 40. 97% Post test # of Questions 10 9 41. 08% 9 58. 33% 1 40. 00% 1 65. 90% 59. 09%
Implementation approaches (post-conference) Education: Presentation Meeting Post test Online module Education comparison Perinatal educator MFM Drs regular mtg FHR Interpretation Transfer of knowledge through peers Formulate a plan Academic environment Little support from administration for more education
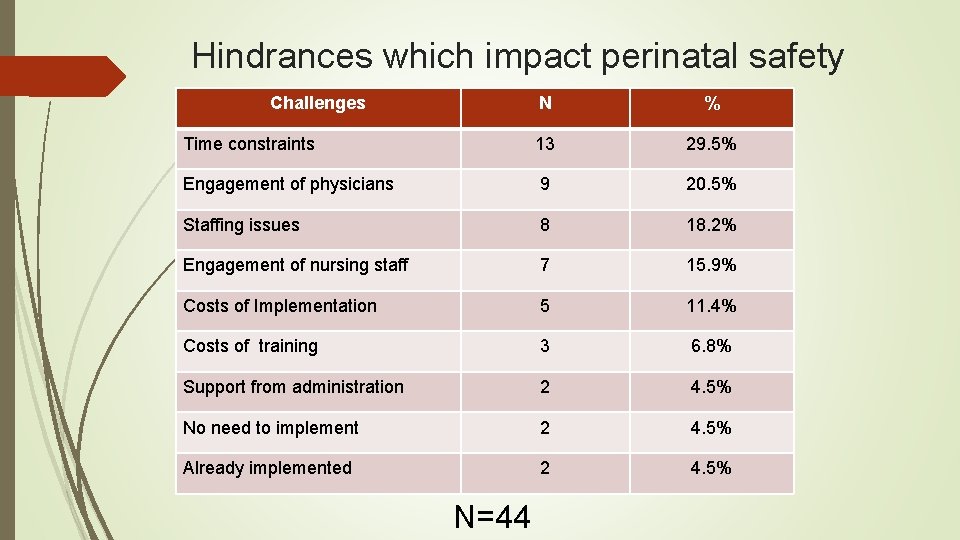
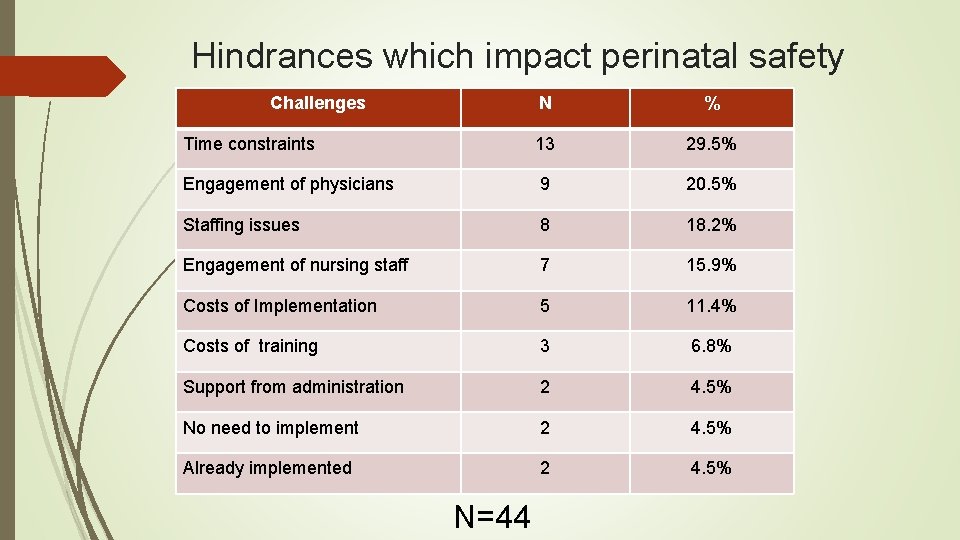
Hindrances which impact perinatal safety Challenges N % Time constraints 13 29. 5% Engagement of physicians 9 20. 5% Staffing issues 8 18. 2% Engagement of nursing staff 7 15. 9% Costs of Implementation 5 11. 4% Costs of training 3 6. 8% Support from administration 2 4. 5% No need to implement 2 4. 5% Already implemented 2 4. 5% N=44
Lessons Learned One conference does not bring about change Participants identified a need for the provision of educational offerings A follow-up luncheon session with key physician and nurse participants proved extremely helpful for determining next steps Those who attended were passionate about this approach for inter-professional learning and interaction
Long Term Goals Community standardization of processes & tools to decrease maternal morbidity and mortality Promotion of a Houston area culture of safety thru effective physician/nurse relationships Community standardization of education and teamwork for physicians and nurses from local university level through areas of practice Hospital champions to ensure sustainability of proposed standardization
References Contratti, F. , Ng, G. , & Deeb, J. (2012). Interdisciplinary team training: Five lessons learned. American Journal of Nursing, 112(6), 47 -52. DOI: 10. 1097/01. NAJ. 0000415127. 84605 Harper, M. & Maloney, P. (2016). Nursing professional development: Revision of the scope and standards of nursing. Journal for Nurses in Professional Development, 32(3), 171 -173. doi: 10. 10097/NND. 0000000255 Kassebaum, N. , Bertozzi-Villa, A. , Coggeshall, M. S. , Shackelford, K. A. , Steiner, C. , & Lozano, R. (2014). Global, regional, and national levels and causes of maternal mortality during 1990– 2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet, 384(9947), 980– 1004. http: //dx. doi. org/10. 1016/S 0140 -6736(14)60696 -6 Klipfel, J, Carolan, B. , Brytowski, N. , Mitchell, C. , Gettman, M. & Jacobson, T. (2014). Patient safety improvement through in situ simulation interdisciplinary team training, Urologic Nursing. 34(1), 39 -46. doi: 10. 7257/1053 -816 X. 2014. 34. 1. 39 Lyndon, A. (2006). Communication and teamwork in patient care: How much can we learn from aviation? JOGNN, 35(4), 538 – 546. Lyndon, A. , Johnson, M. C. , Bingham, D. , Napolitano, P. G. , Joseph, G. , Maxfield, D. G. , & O’Keeffe, D. F. (2015). Transforming communication and safety culture in intrapartum care: A multi-organization blueprint. Journal of Obstetric, Gynecologic and Neonatal Nursing, 44(3), 341 -349. Doi: 10. 1111/1552 -6909. 12575 Lyndon, A. , Zlatnik, M. , & Wachter, R. (2011). Effective physician-nurse communication: a patient safety essential for labor & delivery. American Journal of Obstetrics and Gynecology, 205(2), 91 -96. doi: 10. 1016/j. ajog. 2011. 04. 021 Matzake, B, . Houston, S. , Fisher, U, . Bradshaw, M. (2014) Using a team-centered approach to evaluate effectiveness of nurse -physician communication Journal of Obstetric and Gynecologic and Neonatal Nurses, 43(6), 684 -694. DOI: 10: 1111/1552 -6902 -12496 Maxfield, D. G. , Lyndon, A. , Kennedy, H. P. , O’keeffe, D. , Zlatnik, M. (2013). Confronting safety gaps across labor & delivery teams. American Journal of Obstetrics and Gynecology, 209(5), 402 -408 e 3. http: //dx. doi. org/10. 1016/j. ajog. 2013. 07. 013 Miller, L. & Miller, D. (2013). A collaborative interdisciplinary approach to electronic fetal monitoring. Journal of Perinatal and Neonatal Nursing, 27(2), 126 -133. DOI: 10. 1097/JPN. Ob 013 e 31828 ee 7 fe Riley, W. , Meredith, L. , Price, R. , Miller, K. , Begun, J. , Mc. Cullough, M. , & Davis, S. (2016). Decreasing malpractice claims by reducing preventable perinatal harm. Health Services Research. 51(6 Part 2), 2453 -2471. DOI: 10. 1111/1475 -6773. 12551 Simpson, K. (2005). Failure to rescue: Implications for evaluating quality of care during labor and birth. Journal of Perinatal and Neonatal Nursing, 19(1), 24 -34. The Joint Commission. (2008). Improving America’s hospitals: The Joint Commission’s report on quality and safety 2008. Retrieved from http: //www. jointcommission. org/Patient. Safety/National. Pateint. Safety. Goals/
 Advanced fetal monitoring test answers
Advanced fetal monitoring test answers Nichd fetal monitoring
Nichd fetal monitoring Ctg dr c bravado
Ctg dr c bravado Multidisciplinary software development team
Multidisciplinary software development team Multidisciplinary studies epcc
Multidisciplinary studies epcc Multidisciplinary vs interdisciplinary
Multidisciplinary vs interdisciplinary Conflict in multidisciplinary teams
Conflict in multidisciplinary teams Uksn almora
Uksn almora Examples of transdisciplinary approach
Examples of transdisciplinary approach Multisectoral and multidisciplinary
Multisectoral and multidisciplinary Reflection on multidisciplinary team
Reflection on multidisciplinary team Multidisciplinary nature of environmental studies ppt
Multidisciplinary nature of environmental studies ppt Interdisciplinary multidisciplinary transdisciplinary
Interdisciplinary multidisciplinary transdisciplinary Multidisciplinary
Multidisciplinary Stroke volume variation
Stroke volume variation Usoap cma
Usoap cma Continuous monitoring approach
Continuous monitoring approach Continuous monitoring approach
Continuous monitoring approach Continuous monitoring approach
Continuous monitoring approach Ongoing monitoring
Ongoing monitoring