Advanced cardiac life support Dariush Abtahi MD Anesthesia
Advanced cardiac life support Dariush Abtahi MD Anesthesia Department, SBUMC
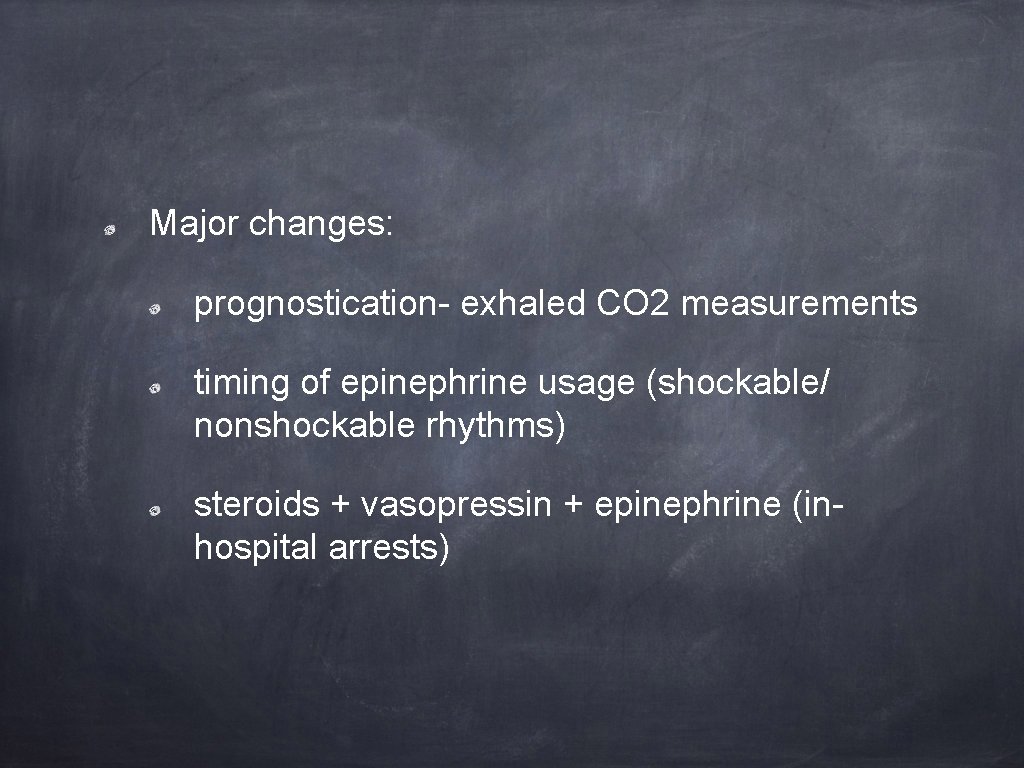
Major changes: prognostication- exhaled CO 2 measurements timing of epinephrine usage (shockable/ nonshockable rhythms) steroids + vasopressin + epinephrine (inhospital arrests)

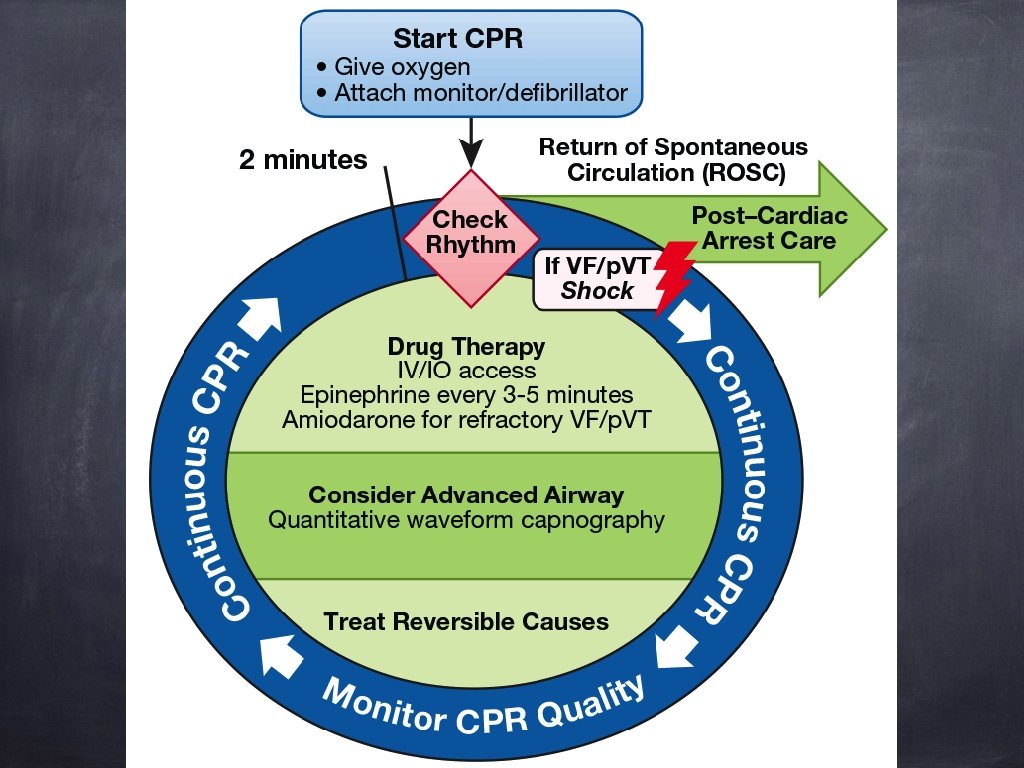
high-quality CPR defibrillation within minutes ACLS + post–cardiac arrest care BLS VF/pulseles s VT �� Survival - vascular access - drug delivery - advanced airways �� ROSC Survival?

High-quality CPR mechanical parameters: chest compression: rate/depth rate: 100 -120/min depth: 5 -6 cm adequacy of relaxation minimization of pauses

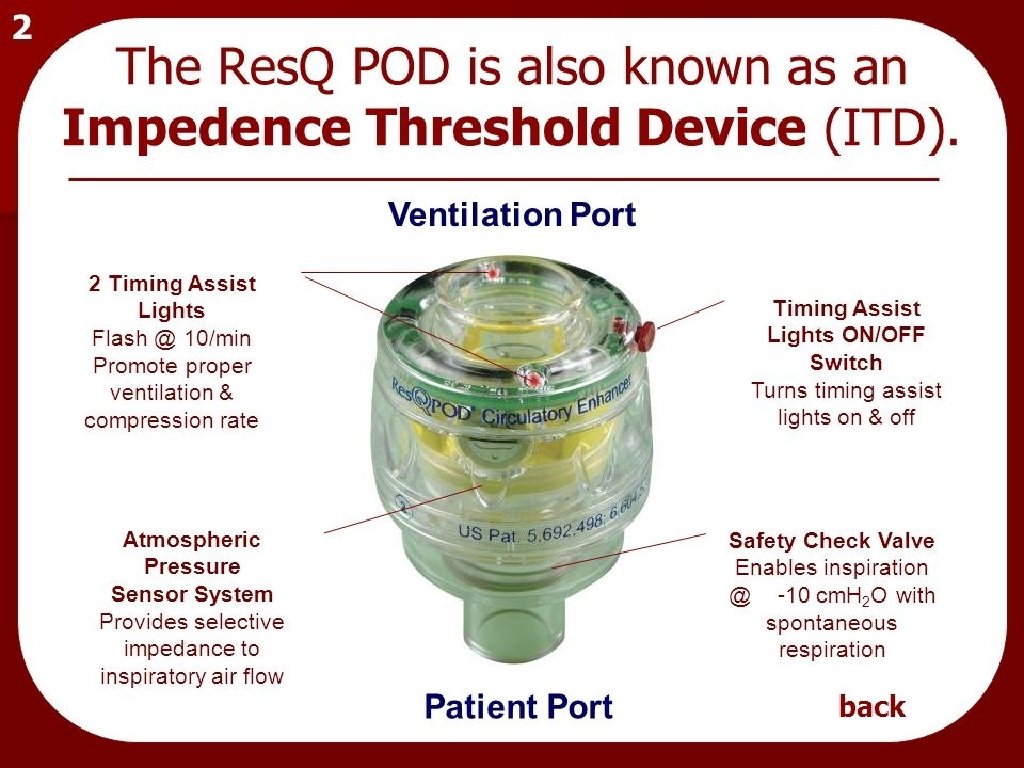
True. CPR Coaching Device


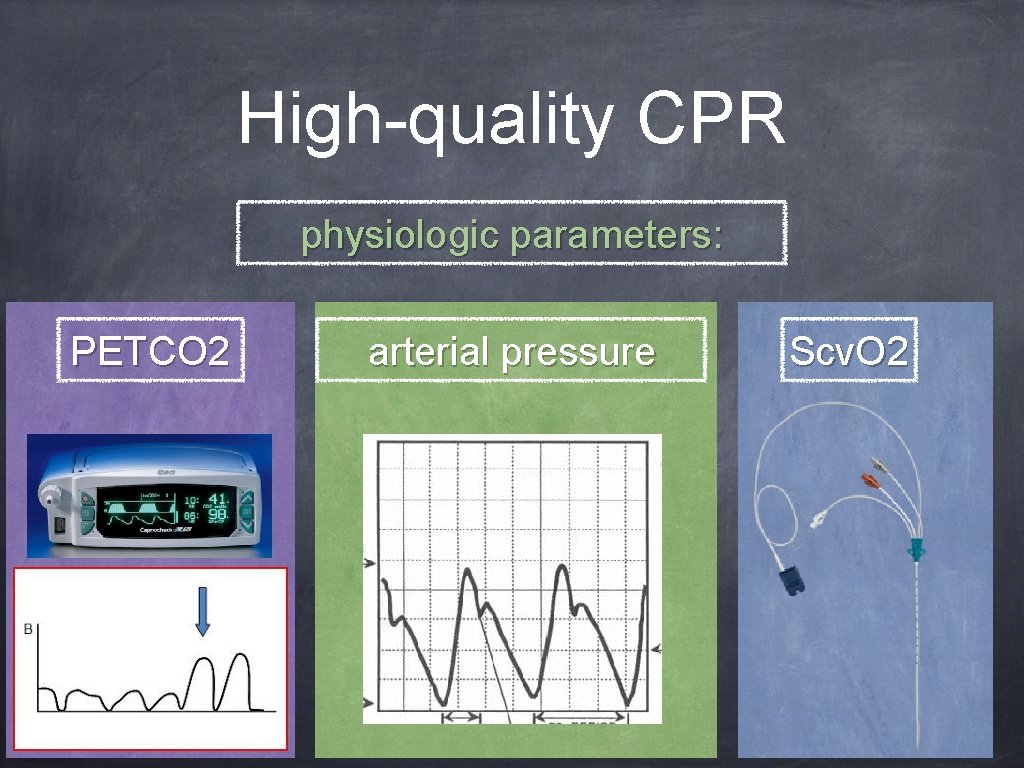
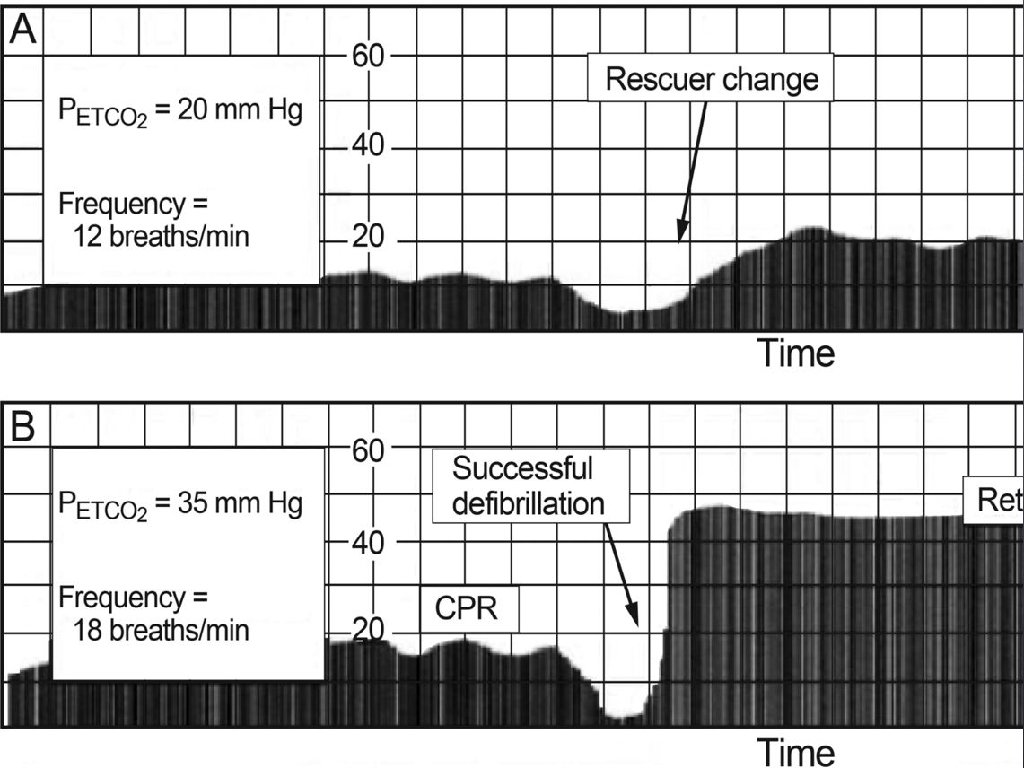
High-quality CPR physiologic parameters: PETCO 2 arterial pressure Scv. O 2

compression rate: 100 -120/minute ventilations: 1 breath/6 sec (10/ minute) advanced airway synchronized compression– ventilation ratio of 30: 2 continuous compression without pauses for ventilation
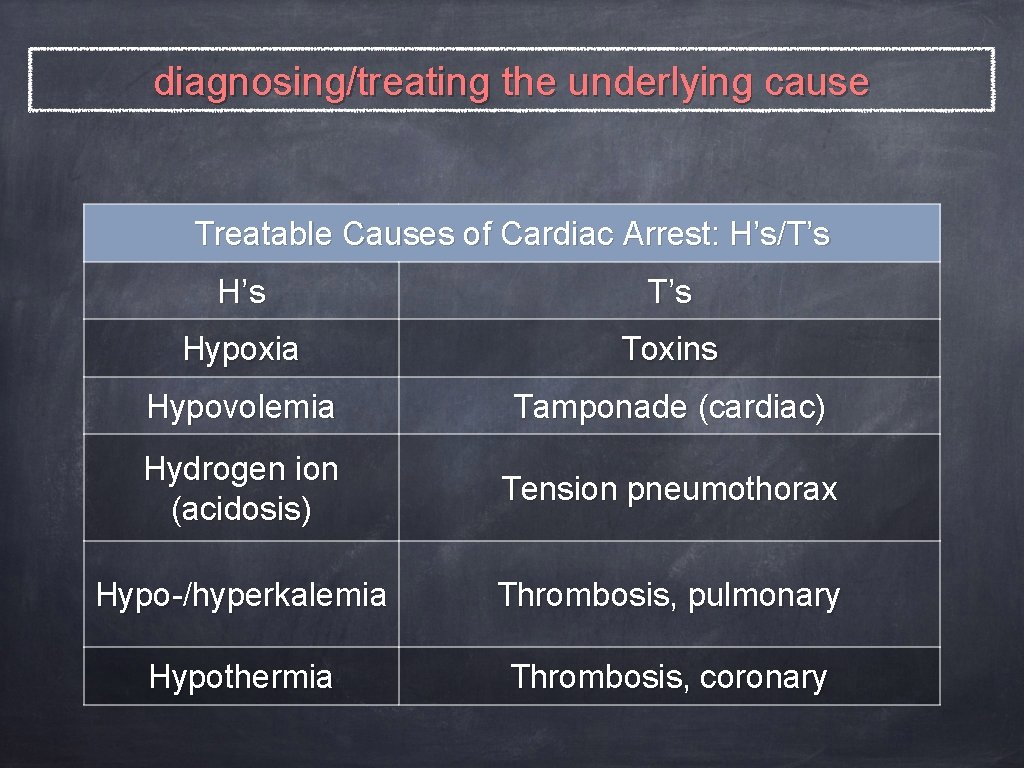
diagnosing/treating the underlying cause Treatable Causes of Cardiac Arrest: H’s/T’s H’s T’s Hypoxia Toxins Hypovolemia Tamponade (cardiac) Hydrogen ion (acidosis) Tension pneumothorax Hypo-/hyperkalemia Thrombosis, pulmonary Hypothermia Thrombosis, coronary

If ROSC→ post–cardiac arrest care hypoxemia hypotension STEMI therapeutic hypothermia avoid rearrest survival
the majority of resuscitative efforts do not result in ROSC
Rhythm-Based Management
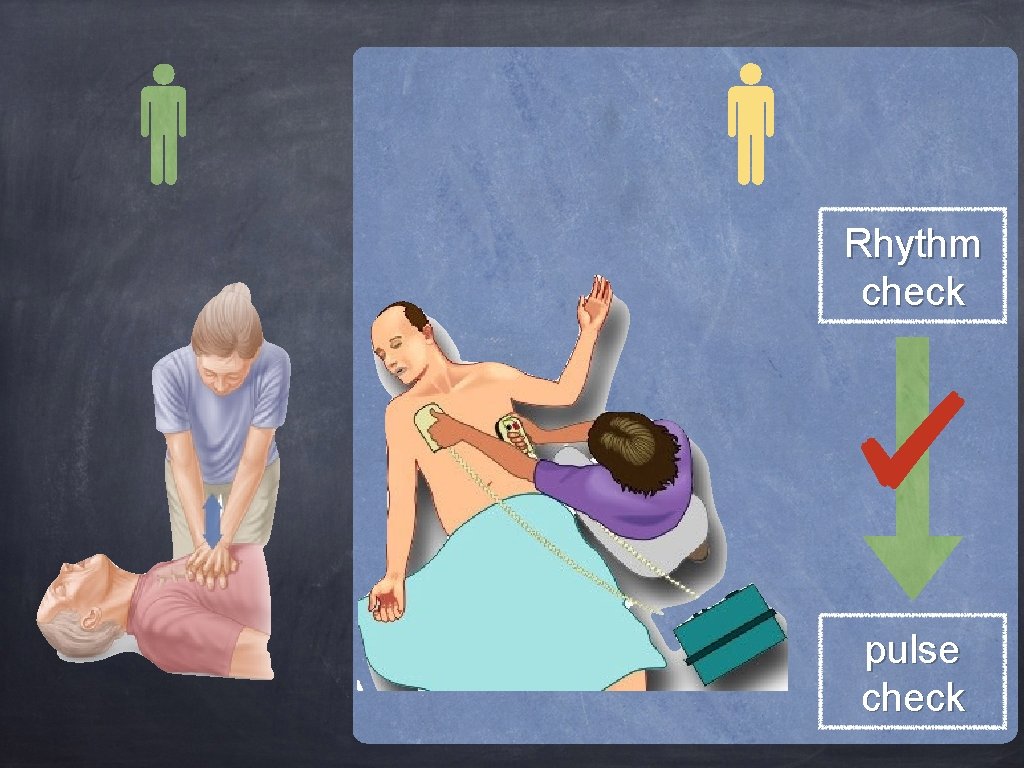
Rhythm check pulse check

VF/Pulseless VT 2 minutes CPRimmediately AED manual defibrillator CPR Check Rhythm
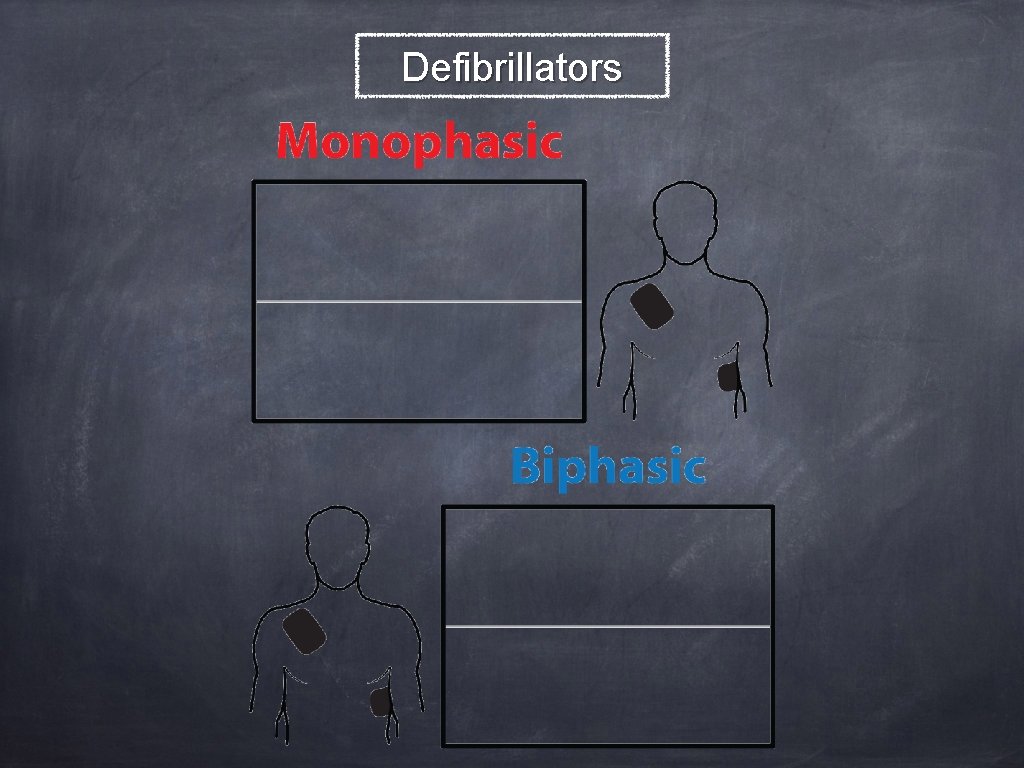
Defibrillators
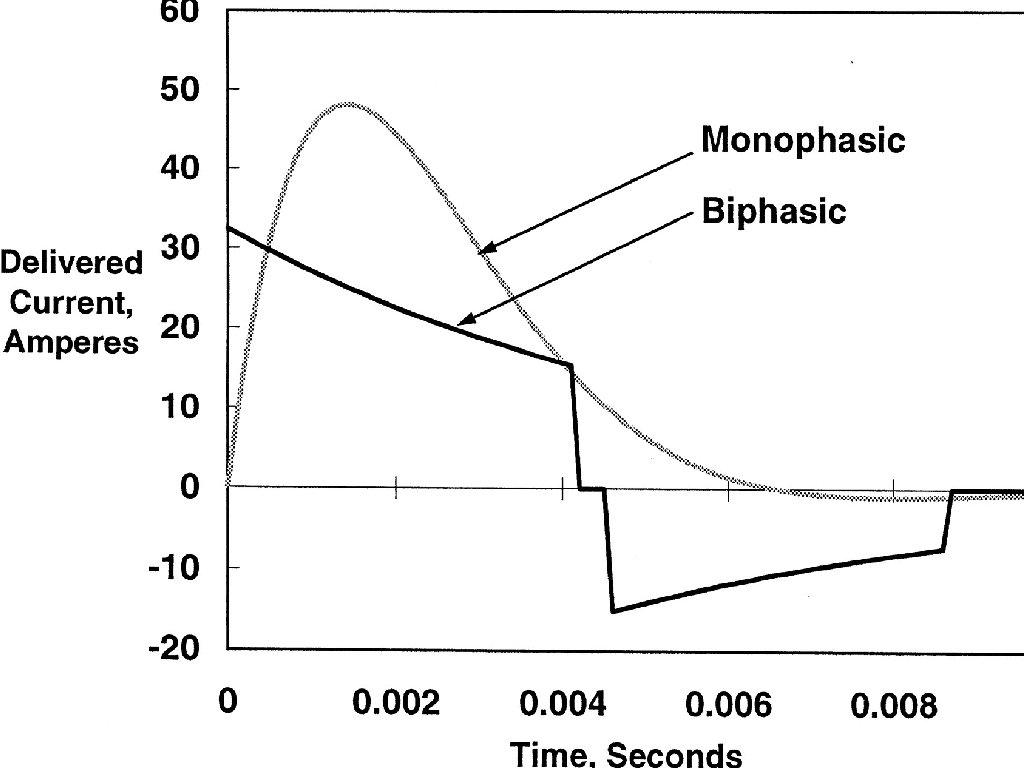
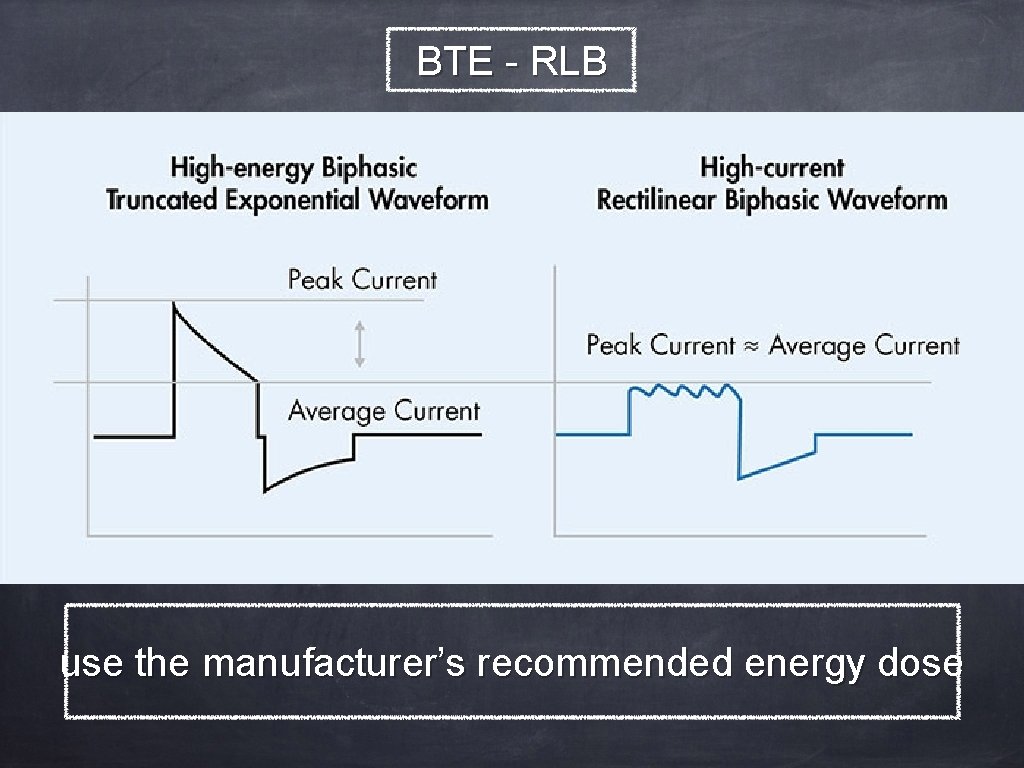
BTE - RLB use the manufacturer’s recommended energy dose
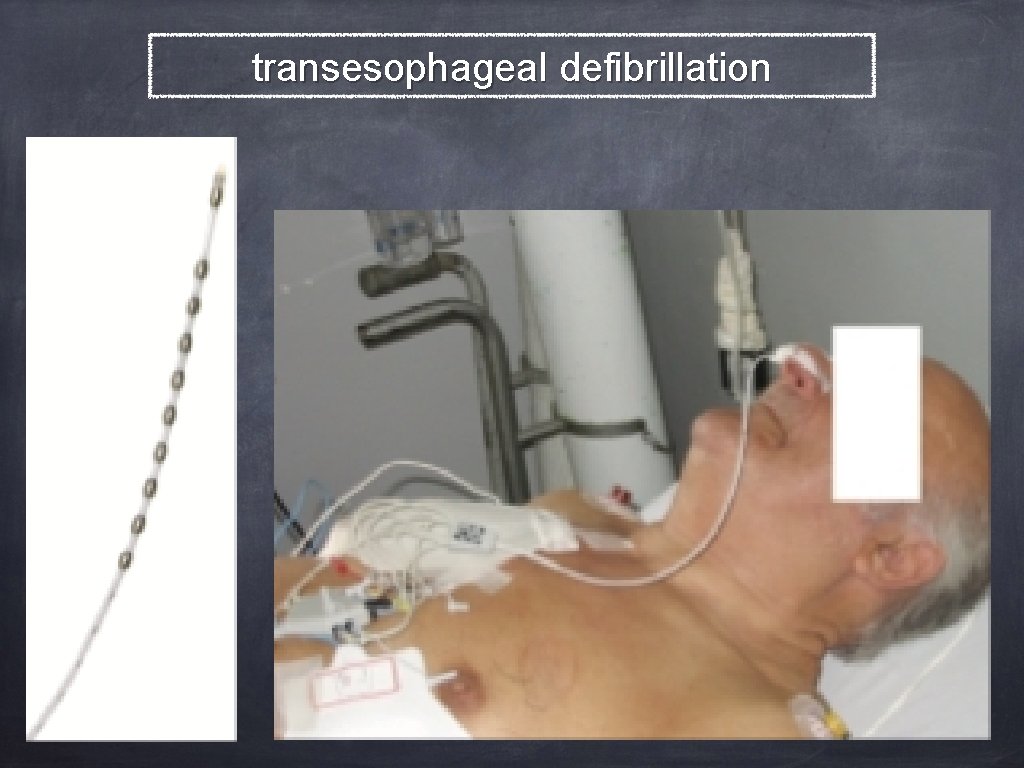
transesophageal defibrillation
Medications
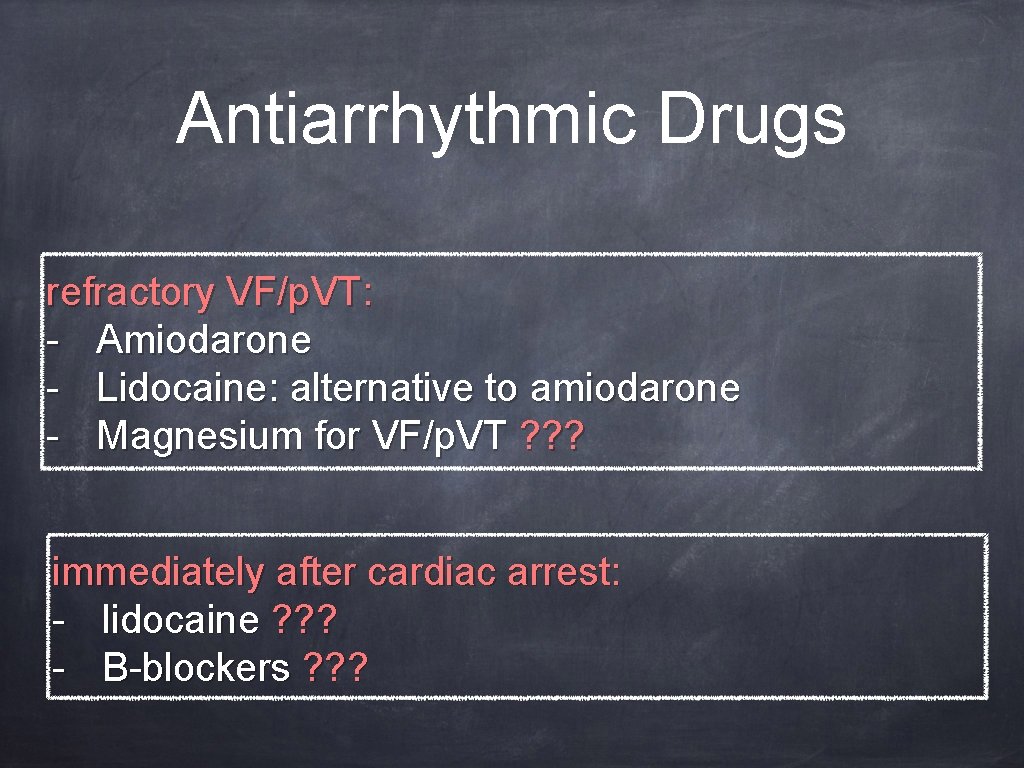
Antiarrhythmic Drugs refractory VF/p. VT: - Amiodarone - Lidocaine: alternative to amiodarone - Magnesium for VF/p. VT ? ? ? immediately after cardiac arrest: - lidocaine ? ? ? - Β-blockers ? ? ?
Vasopressors Drugs Standard-dose epinephrine (1 mg/3 -5 minutes) non- shockable rhythm: as soon as feasible
Vasopressors Drugs High-dose epinephrine (0. 1 -0. 2 mg/kg): β-blocker overdose calcium channel blocker overdose when titrated to real-time physiologically monitored parameters
Vasopressors Drugs Vasopressin: as a substitute for epinephrine ? ? ? Vasopressin + epinephrine as a substitute for standard-dose epinephrine ? ? ?
Steroids OHCA ? ? ? IHCA: vasopressin + epinephrine + methylprednisolone + post-arrest hydrocortisone

Access for Parenteral Medications
Timing of Access No chest compressions interruption insufficient evidence: exact time parameters which drugs should be administered
Peripheral IV Drug Delivery + 20 m. L bolus of IV fluid Briefly elevating the extremity during/after drug administration ? ? ?
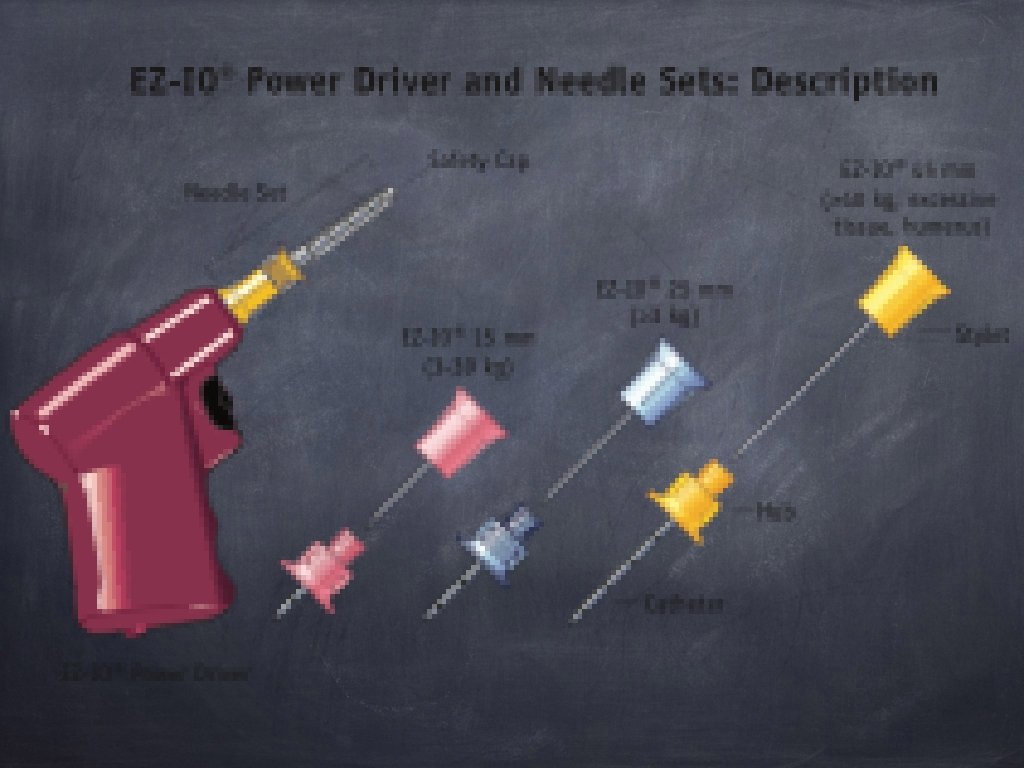
IO Drug Delivery All ACLS drugs efficacy and effectiveness ? ? ? if no IV access Commercially available kits
Central IV Drug Delivery trained provider Advantages: �� peak drug concentrations �� drug circulation times monitor Scv. O 2 and estimate CPP
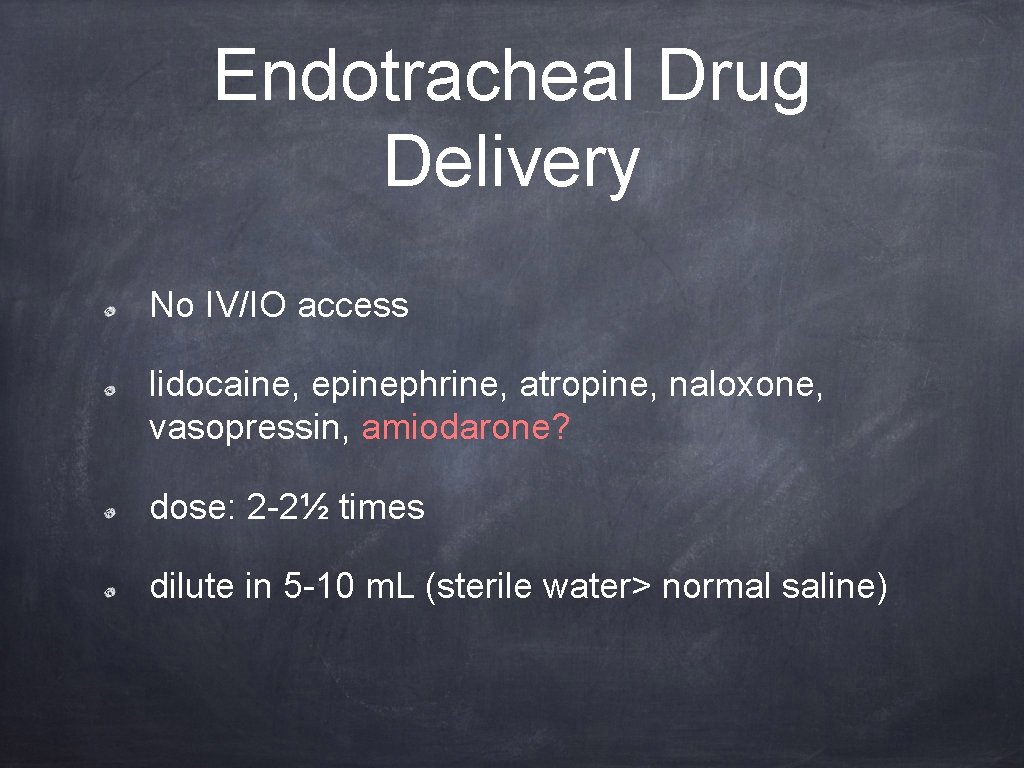
Endotracheal Drug Delivery No IV/IO access lidocaine, epinephrine, atropine, naloxone, vasopressin, amiodarone? dose: 2 -2½ times dilute in 5 -10 m. L (sterile water> normal saline)
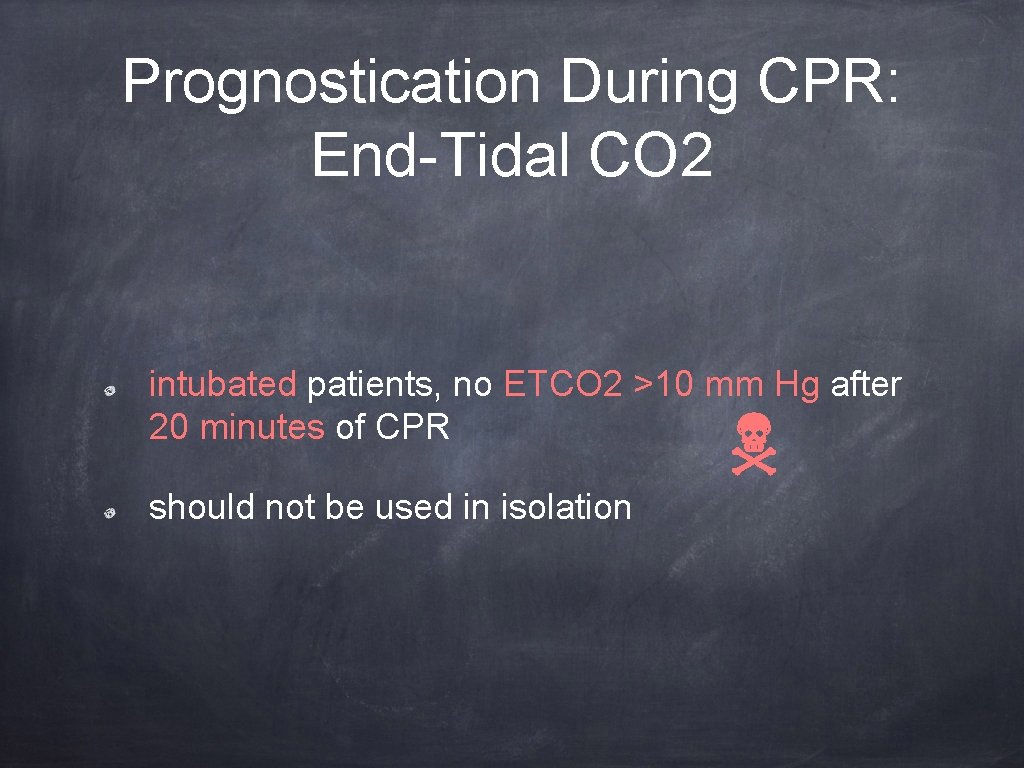
Prognostication During CPR: End-Tidal CO 2 intubated patients, no ETCO 2 >10 mm Hg after 20 minutes of CPR should not be used in isolation
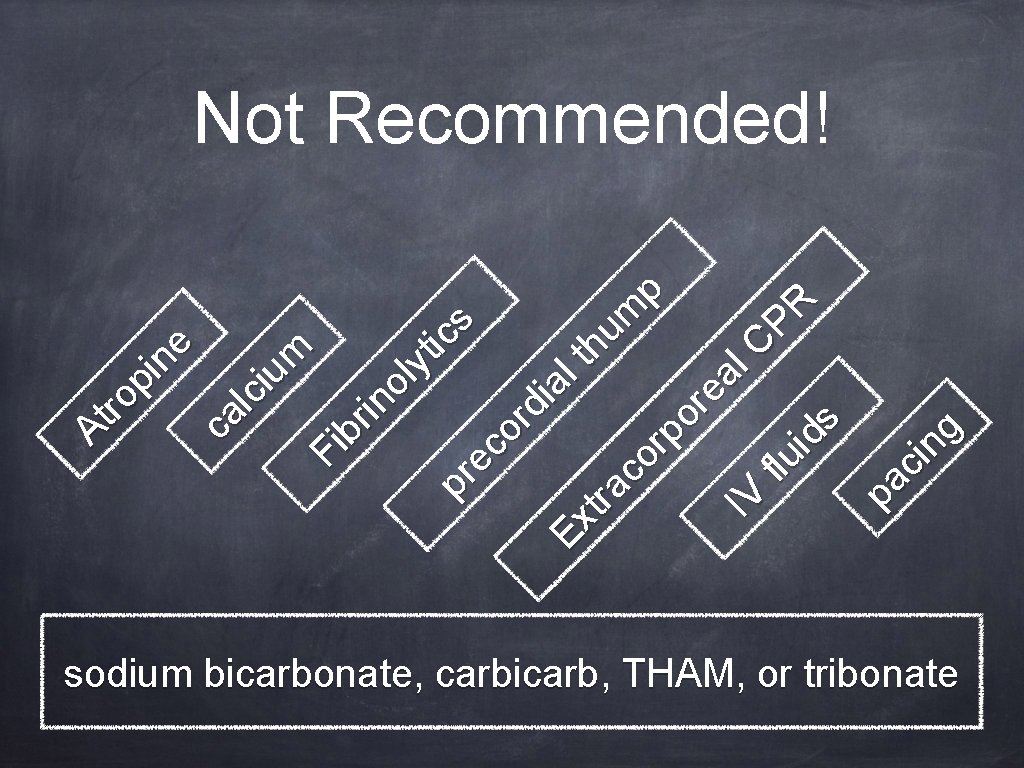
pa ci ng Fi br in ol yt ic pr s ec or di al E th xt ra um co p rp or ea IV l. C fl u P R id s At ro pi ne ca lc iu m Not Recommended! sodium bicarbonate, carbicarb, THAM, or tribonate
When Should Resuscitative Efforts Stop? clinical judgment respect for human dignity
- Slides: 39