Advanced Arrhythmia Management Tachyarrhythmias In conjunction with the


- Slides: 38
Advanced Arrhythmia Management - Tachyarrhythmias In conjunction with the remote simulation program simulation session Module C 6 This project was possible due to funding made available by Health Workforce Australia
Sponsor This project was possible due to funding made available by Projects within NSW are overseen by the NSW Ministry of Health on behalf of HWA

Introductions October 20 © Health Workforce Australia
General Aims • Learn in a team setting • Blend clinical skills with team skills • Reflect critically on practice October 20 © Health Workforce Australia
Session Objectives 1. Use a structured approach to rapid assessment of tachyarrhythmias 2. Apply the 'unstable’ versus ‘stable’ decision tree to early management 3. Review common tachyarrhythmias 4. Identify pre-malignant tachyarrhythmias (indications for cardiac pacing) 5. Perform electrical and chemical cardioversion 6. Rehearse synchronous electrical cardioversion October 20 © Health Workforce Australia
Ground Rules • • • October 20 Participation Privacy Confidentiality Disclaimer Debriefing Mobile phones © Health Workforce Australia
A Structured Approach to Arrhythmias 1. Apply the “unstable v stable” rule 2. Use a methodical approach to diagnose the rhythm 3. Seek the underlying cause and contributors October 20 © Health Workforce Australia
“Stable or Unstable? ” This reflects Cardiac Output(CO) in one of three functional categories: STABLE –CO adequate to perfuse end organs UNSTABLE - CO inadequate to perfuse end organs (Shock) CARDIAC ARREST – No CO October 20 © Health Workforce Australia
The unstable patient – clinical criteria – Altered level of consciousness – Chest pain- ongoing – Dyspnoea from acute LVF – BP< 80 mm. Hg – HR > 150/min October 20 © Health Workforce Australia
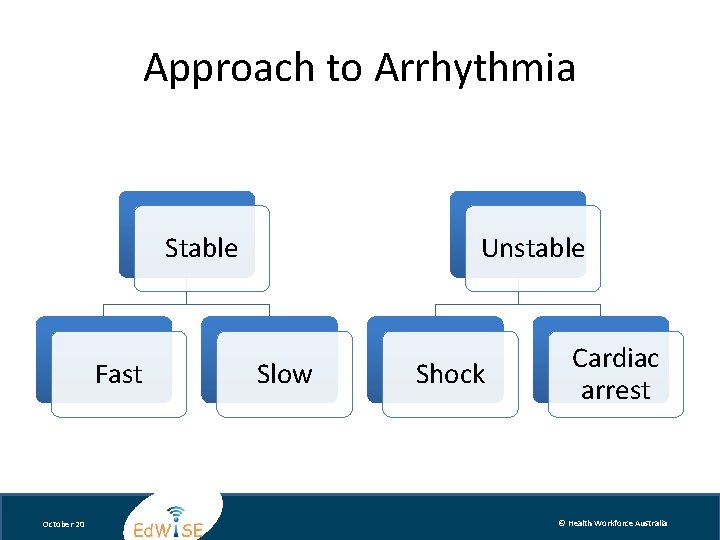
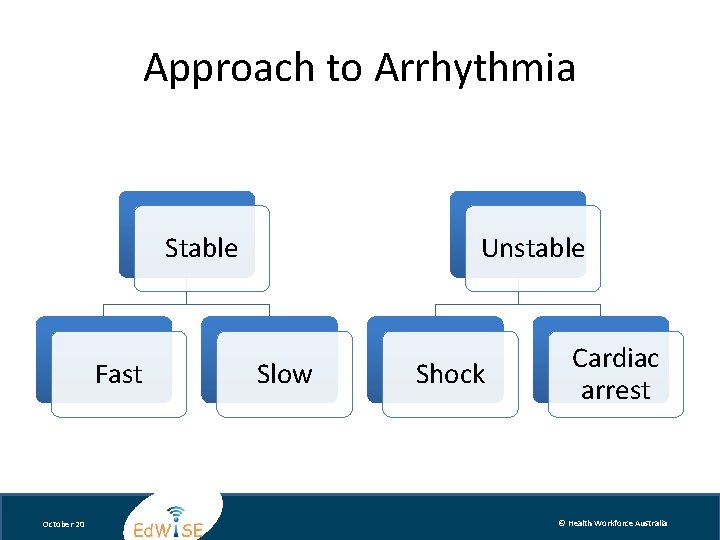
Approach to Arrhythmia Stable Fast October 20 Unstable Slow Shock Cardiac arrest © Health Workforce Australia
A methodical approach to diagnosing rhythm Lets rehearse October 20 © Health Workforce Australia
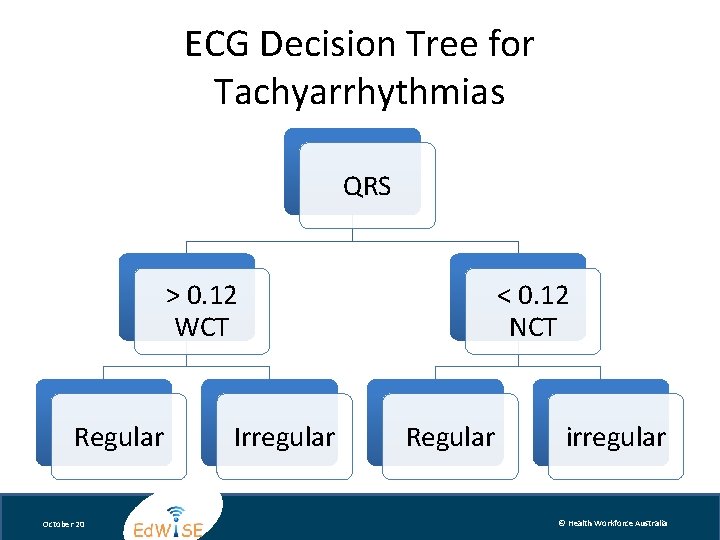
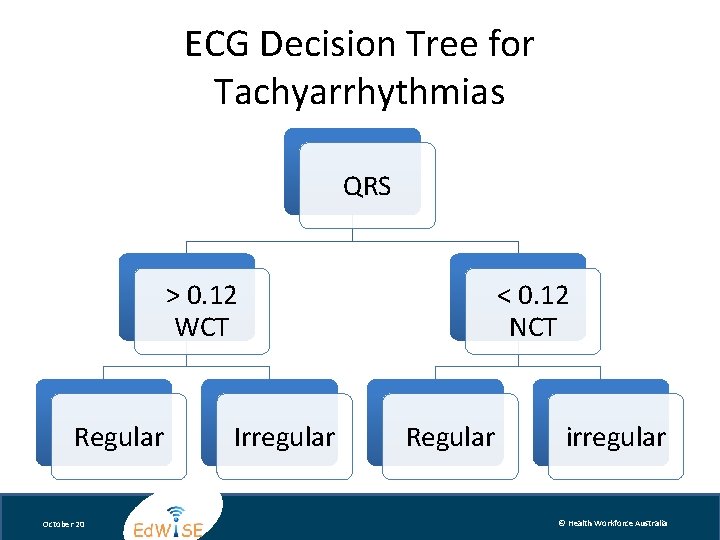
ECG Decision Tree for Tachyarrhythmias QRS > 0. 12 WCT Regular October 20 Irregular < 0. 12 NCT Regular irregular © Health Workforce Australia
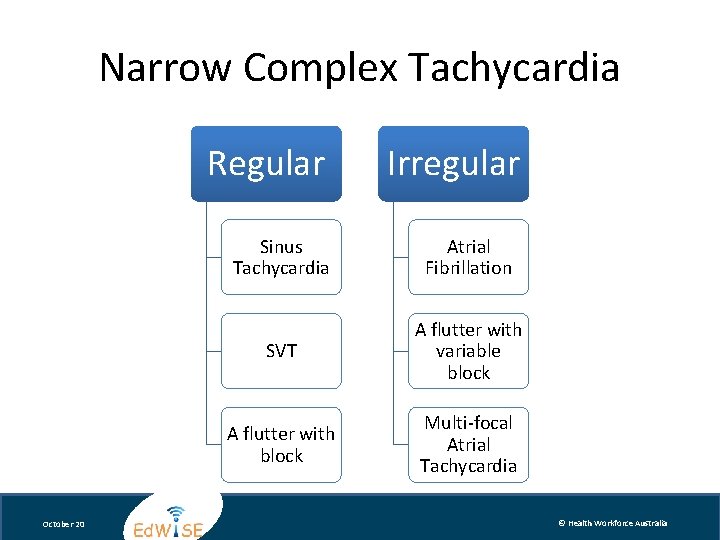
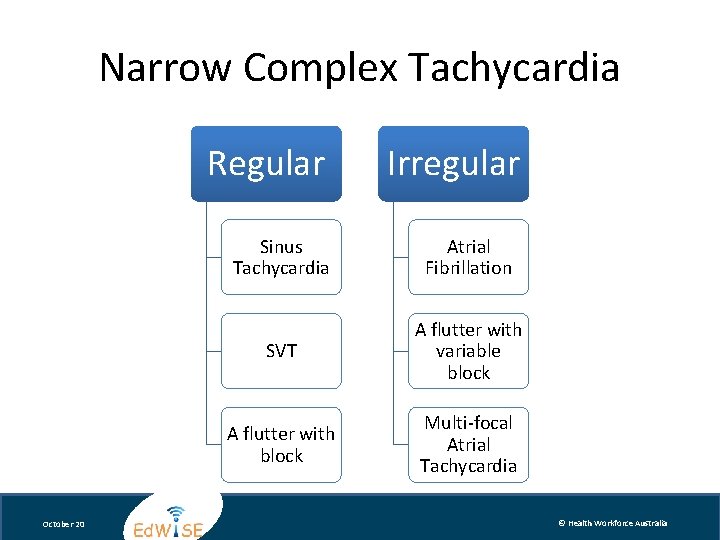
Narrow Complex Tachycardia Regular October 20 Irregular Sinus Tachycardia Atrial Fibrillation SVT A flutter with variable block A flutter with block Multi-focal Atrial Tachycardia © Health Workforce Australia
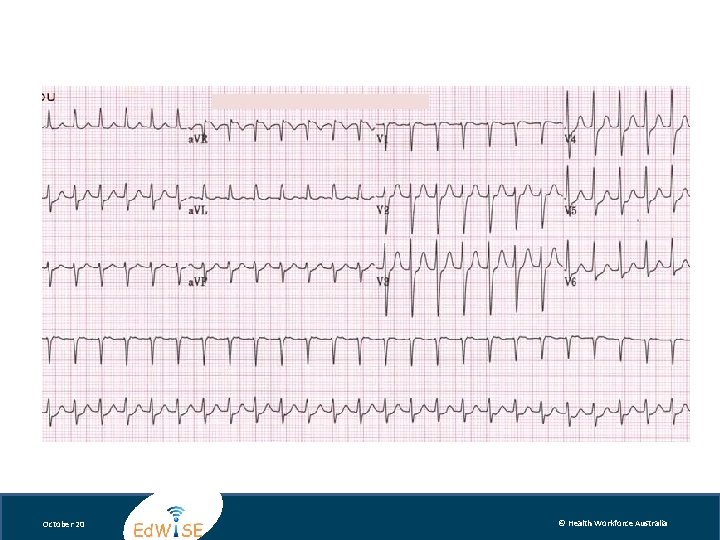
Jackson Brown, 25 presents with anxiety and palpitations What does his ECG suggest? October 20 © Health Workforce Australia
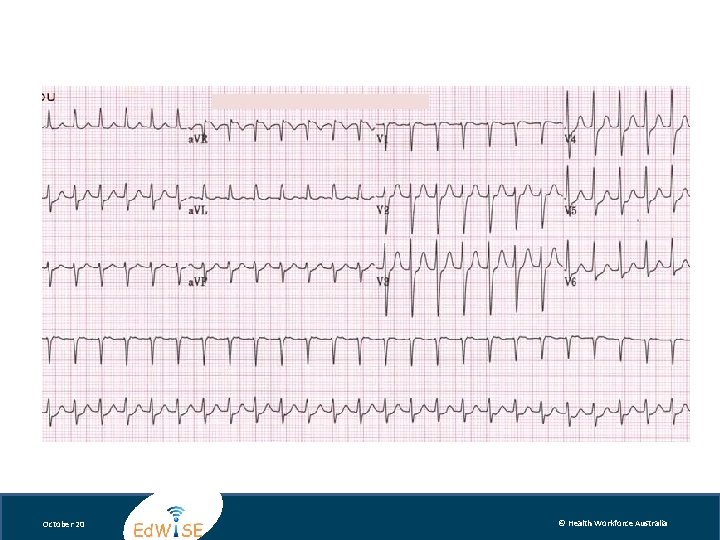
October 20 © Health Workforce Australia
Management of SVT • Unstable patient Urgent Synchronised cardioversion • Stable patient: 1. Vagal manoeuvers 2. Adenosine 3. Calcium channel blockers 4. Beta blockers October 20 © Health Workforce Australia
Mel Brooks, 75 presents with fatigue and palpitations What does his ECG suggest? October 20 © Health Workforce Australia
October 20 © Health Workforce Australia
Management of AF • Unstable Syncronised cardioversion with sedation and analgesia • Stable patient Duration of AF (<48 hours) Rate or Rhythm control Prevent thromboembolism (CHADS 2 score) October 20 © Health Workforce Australia
Wide Complex Tachycardia Regular VT October 20 Irregular Polymorphic VT BBB/aberrancy • Sinus tachycardia • SVT • A flutter • AF (WPW) • A flutter (variable block) © Health Workforce Australia
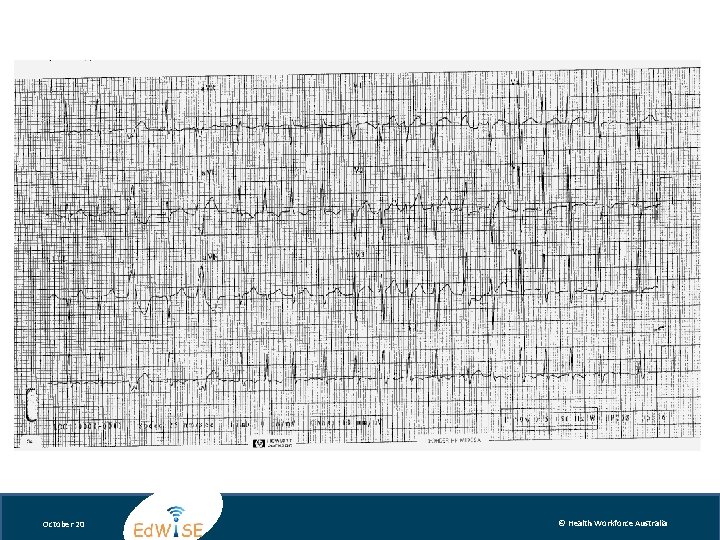
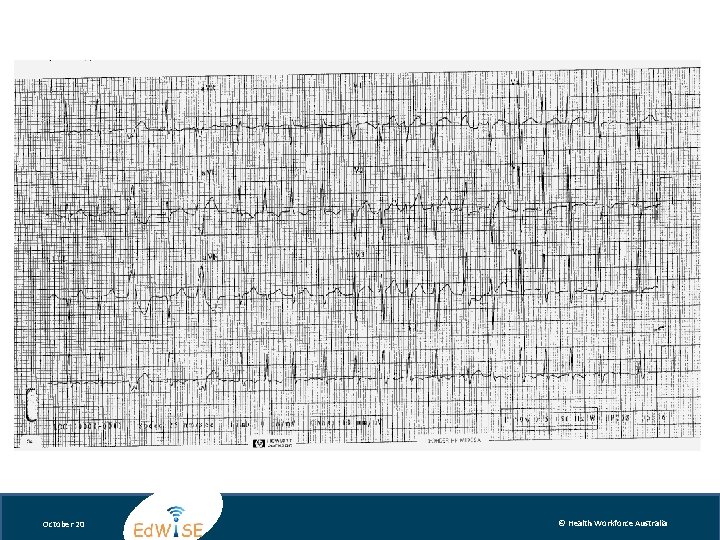
Lucille Ball, 75 presents with fatigue and palpitations What does her ECG suggest? October 20 © Health Workforce Australia
October 20 © Health Workforce Australia
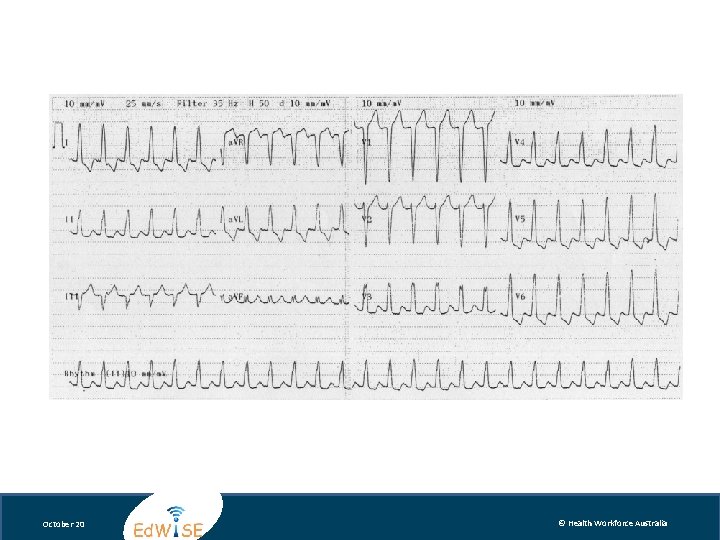
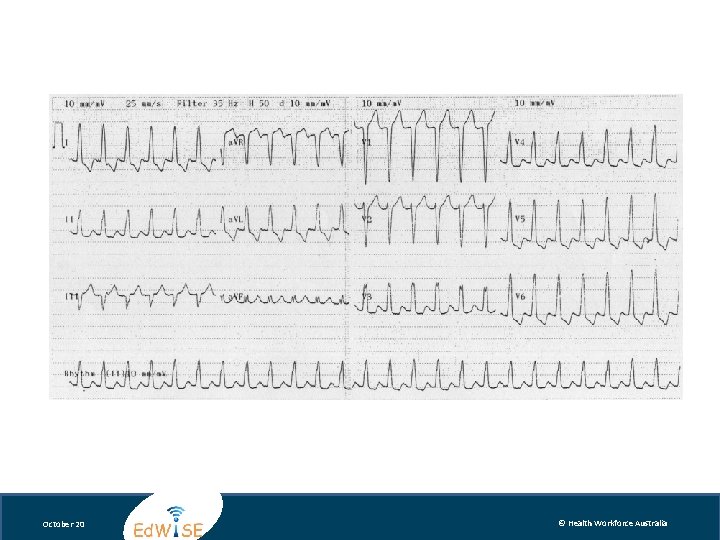
Benny Hill, 85 presents with a fractured hip What does his ECG suggest? October 20 © Health Workforce Australia
October 20 © Health Workforce Australia
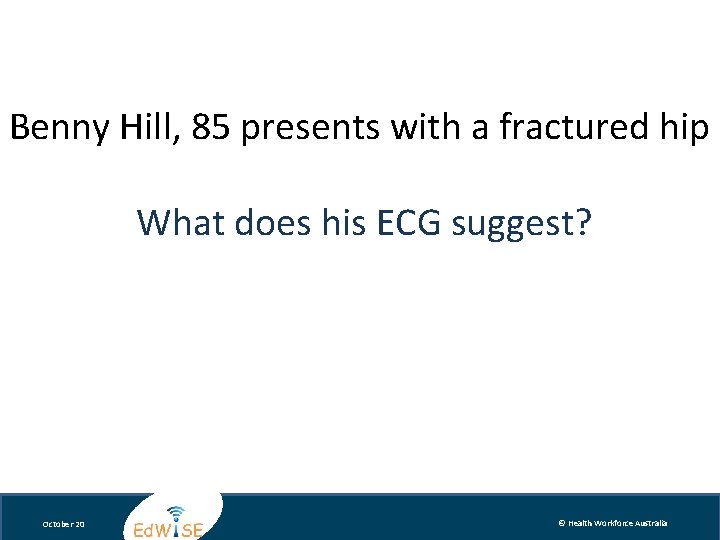
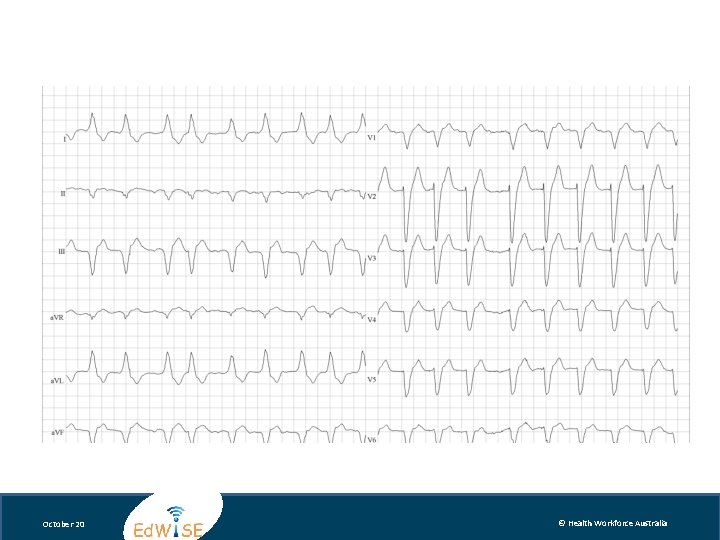
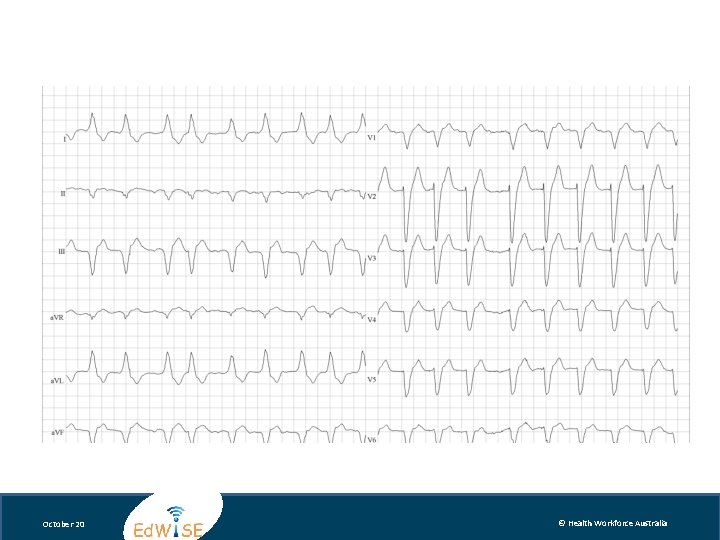
Charlton Heston, 75 presents with chest pain and dyspnoea What does his ECG suggest? October 20 © Health Workforce Australia

October 20 © Health Workforce Australia
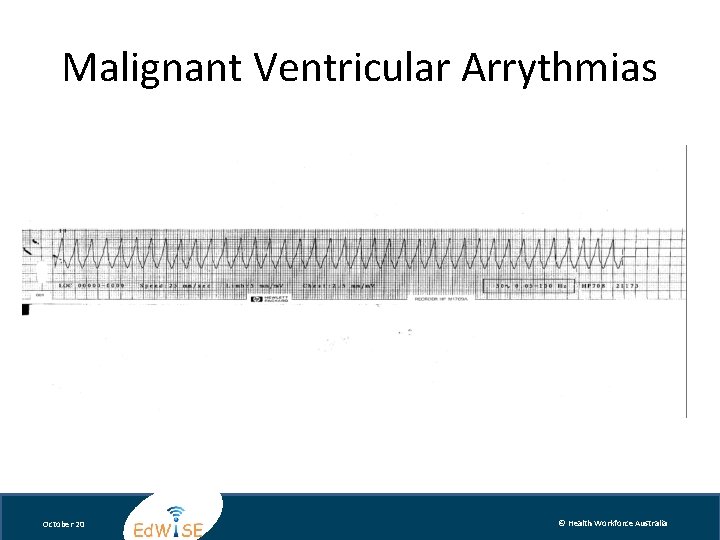
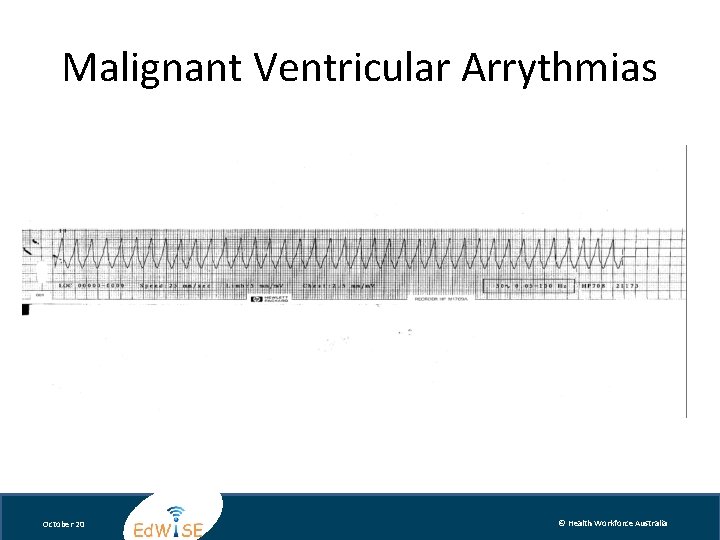
Malignant Ventricular Arrythmias October 20 © Health Workforce Australia
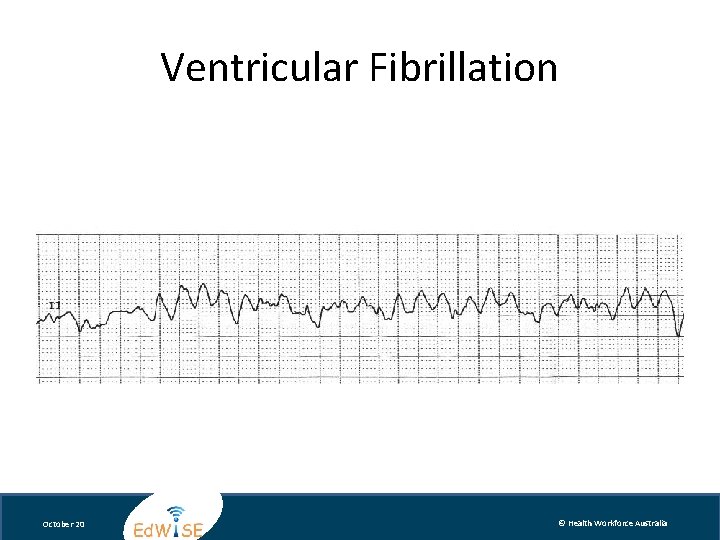
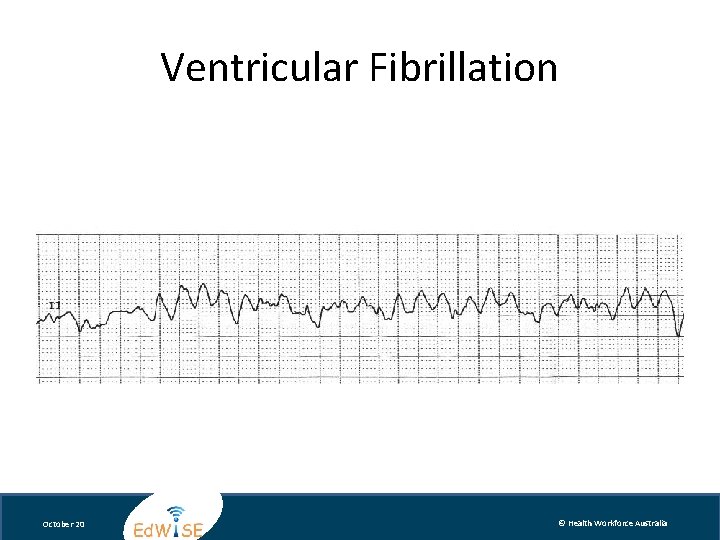
Ventricular Fibrillation October 20 © Health Workforce Australia
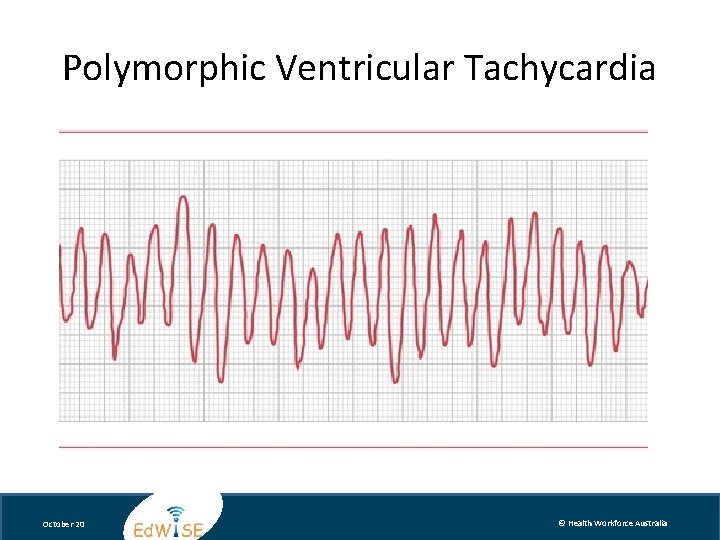
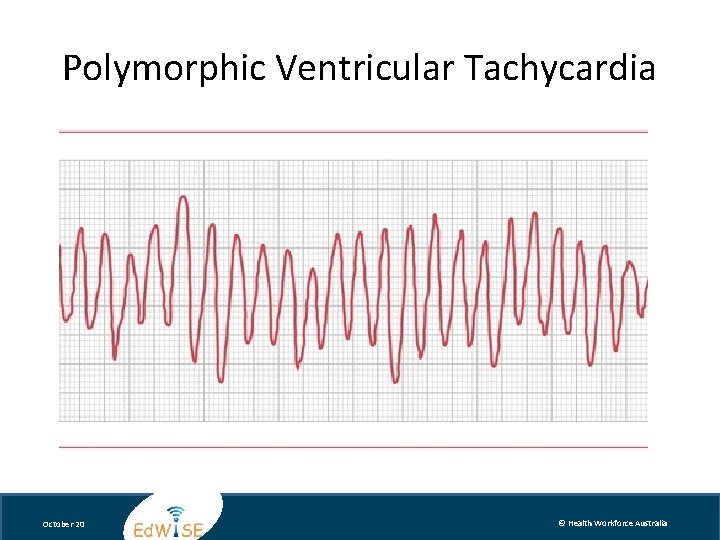
Polymorphic Ventricular Tachycardia October 20 © Health Workforce Australia
Cardioversion • Synchronized electrical therapy to reset the normal electrical activity • Equipment – Defibrillator • Procedural Sedation and Analgesia(IV) – Midazolam 0. 1 mg/kg; Fentanyl 1 microgram/kg • Personnel • Procedure October 20 © Health Workforce Australia
Summary • Determine clinically if stable or unstable • Unstable requires urgent intervention • Assess ECG for QRS width and regularity to guide diagnosis and management • Cardioversion requires sedation and analgesia, Defibrillate during an arrest • Treat WCT as VT unless you know better! October 20 © Health Workforce Australia
Let’s Practice - the Case October 20 © Health Workforce Australia
History • Richie Rich 70 -year-old man presents with SOB and palpitations after a session of lawn bowls this evening. He has a significant cardiac history. He has been triaged and placed into the resuscitation bay. October 20 © Health Workforce Australia
In Summary… • Use a structured approach to assessment of patients with tachyarrhythmias. • Guide decisions on electrical and chemical cardioversion with clinical criteria • Use care when using sedative drugs in this patient population • Be an effective teammember October 20 © Health Workforce Australia
References • • e. TG complete March 2012. Accessed through www. use. hcn. com. au Australian Resuscitation Guidelines. Accessed through www. resus. org. au ECGpedia. Accessed through www. en. ecgpedia. org Tintinalli’s Emergency Medicine. Accessed through http: //proxy 14. use. hcn. com. au/ Atlas of Emergency Medicine. Accessed through: http: //proxy 14. use. hcn. com. au/content. aspx? aid=6008102 www. torsades. org Nation Health and Medical Research Council Rate or rhythm control for recurrent atrial fibrillation Emergency Care Evidence in Practise Series 2008 October 20 © Health Workforce Australia
Acknowledgments C 6 Topic expert author: Marian Lee C 6 Simulation session author: Timothy Tan, Morgan Sherwood, Clare Richmond Cardiac Module Expert Working Party and Peer Review Team Michael Bastick FACEM Gosford Hospital Sandra Cheng Simulation Fellow SCSSC John Kennedy FACEM Royal North Shore Hospital Marian Lee FACEM Prince of Wales Hospital John Mc. Kenzie FACEM Australian Institute for Clinical Education (AICE) Clare Richmond FACEM Royal Prince Alfred Hospital Morgan Sherwood Simulation Fellow SCSSC Timothy Tan Simulation Fellow SCSSC John Vassiliadis FACEM Royal North Shore Hospital Educational consultants: Stephanie O’Regan Nurse Educator SCSSC Leonie Watterson Director Simulation Division SCSSC John Vassiliadis Deputy Director SCSSC Clare Richmond FACEM Royal Prince Alfred Hospital Morgan Sherwood Simulation Fellow SCSSC October 20 © Health Workforce Australia
Disclaimer Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However the authors, editor and publisher are not responsible for errors or omissions or for any consequences from the application of the information in this presentation and make no warranty, express or implied, with respect to the contents of the presentation. Copyright and Permission to Reproduce This work is copyright. It may be reproduced for study or training purposes subject to the inclusion of an acknowledgement of the source: Health Workforce Australia Ed. WISE program. It may not be reproduced for commercial usage or sale. October 20 © Health Workforce Australia