Advanced Alternative Payment Model for Radiation Therapy October
Advanced Alternative Payment Model for Radiation Therapy October 22, 2020

Agenda • Delay in the Model until July 1, 2021 • Radiation Oncology Administrative Portal (ROAP) Walk-Through • https: //app. innovation. cms. gov/ROAP/IDMLogin? start. URL=%2 FROAP • Help Desk Discussion • Phone: 1 -844 -711 -2664, option 5 • Email: Radiation. Therapy@cms. hhs. gov • New Questions from ACRO Members • Future ACRO Webinars on Secure Data Portal, etc. – Date TBD 2
New Questions from ACRO Members • With the delay in the APM until July 1, 2021, will model participants still qualify for a 5% bonus? • Please explain CMS rationale for requiring providers to submit quality reporting data on ALL patients, not just Medicare and how the Agency expects providers to spend more money to provide this information at lower reimbursement. • Please provide guidance for providers who have staff turnover and cannot access username or password information from CMS Help Desk. • How will CMS handle reconciliation of duplicate services without impacting beneficiary access or quality of care such as when a patient is referred for external beam and another modality provided by another provider location, (e. g. brachytherapy or stereotactic radiosurgery) under the following scenarios: • 1. Lung cancer patient coughing up blood w/brain mets requiring treatment w/fractionated chest radiation and stereotactic radiosurgery at another facility. • 2. Cervix cancer patient requiring external beam radiation at one facility and brachytherapy by another physician at another facility. • 3. Rectal cancer patient with solitary liver metastasis (not one of the 16 diagnoses) treated with neoadjuvant chemoradiotherapy and SBRT to liver lesion. • Please provide guidance on the logistics of billing and coding, particularly when there is more than one applicable diagnosis code. • What is my practice's MIPS status in 2021? When I log into my QPP account, there is no indication that I am in the RO-APM. In fact, I was able to request a hardship exemption from Promoting Interoperability. Will I be penalized for not submitting MIPS quality measures if MIPS doesn't know that I should now be exempt? • There are several diagnoses we treat that fall outside the model--skin cancer, multiple myeloma, DCIS breast, lung mets, liver mets, . . . etc. When billing for these diagnoses via FFS, I assume I should be exempt from MIPS quality reporting--right? • What is the difference between "expected payment" and "predicted payment"? • CMS expects practices to absorb the cost of treating metastases after triggering an episode for a primary diagnosis. What's to keep a practice that triggers an episode for a lung cancer patient, who within 3 weeks of starting thoracic radiation, gets diagnosed with a bone met, after 3 which the practice submits code D 48. 0 (neoplasm of uncertain behavior of bone) and billing FFS for palliative bone XRT?
Items for Information • CMMI FAQS (October 2, 2020) https: //innovation. cms. gov/media/document/ro-model-faqs • September 23 Slide Deck 4

Advanced Alternative Payment Model for Radiation Therapy September 23, 2020

Issue Proposed Rule ACRO Request Final Rule Payment Stability PFS Rule Issue (note: treatment, imaging inputs maintained in 2021) ACRO supported Expect similar treatment in 2021 PFS Prospective vs Retrospective Prospective case rate; development of new case rate codes; payment made to radiation oncologist ACRO supported Included. Other benefits include: (1) qualifies as Advanced APM, (2) not subject to prior authorization, (3) bypasses SNF consolidated billing Episode 90 -day episode after trigger code (77261, 77262, 77263); payments cover all 77 xxx services during 90 -day period for 17 disease sites ACRO supported Included, except for 16 disease sites (kidney cancer is excluded) Discount / Efficiency Factor Combined effect of 6. 6% reduction in payment by PY 5 Align discount with OCM to 2. 75% Proposed Exclusions No accounting for small and rural practices Exclude patients treated at multiple centers, or with brachytherapy RT modalities in the Model: 3 DCRT, IMRT, SRS, SBRT, IGRT, PBT and brachy; IORT excluded Discount factor reduced by 0. 25% for PC and TC If less than 60 episodes in last 3 years, CMS will not blend and will have a 20% stop loss. If less than 20 episodes, CMS will include an opt-out option. CMS also will consider hardship exemption in subsequent rulemaking for a future PY. Case Mix / Experience Adjustment Provider-specific experience adjustment Cancer-specific experience adjustment CMS argues that case mix model incorporates cancer type. Withholds Quality, clinical data, end-of-episode Adjust thresholds to ease provider burden CMS is finalizing a reduced incorrect payment withhold of 1% rather than 2%. Quality withhold maintained at 2%. RO may bill EOE claim after 28 days rather than 90. Demo Start Date Requests comment on Jan 1, 2020 or April 1, 2020 start 2019 pre-pandemic request: April 1, 2020 start date. Intra-pandemic request: Delay start date until January 1, 2022. Delayed until January 1, 2021. Demo applies to 30% of eligible Medicare beneficiary episodes from a random selection of Core Based Statistical Areas (CBSA), down from 40% in the proposed version. 2
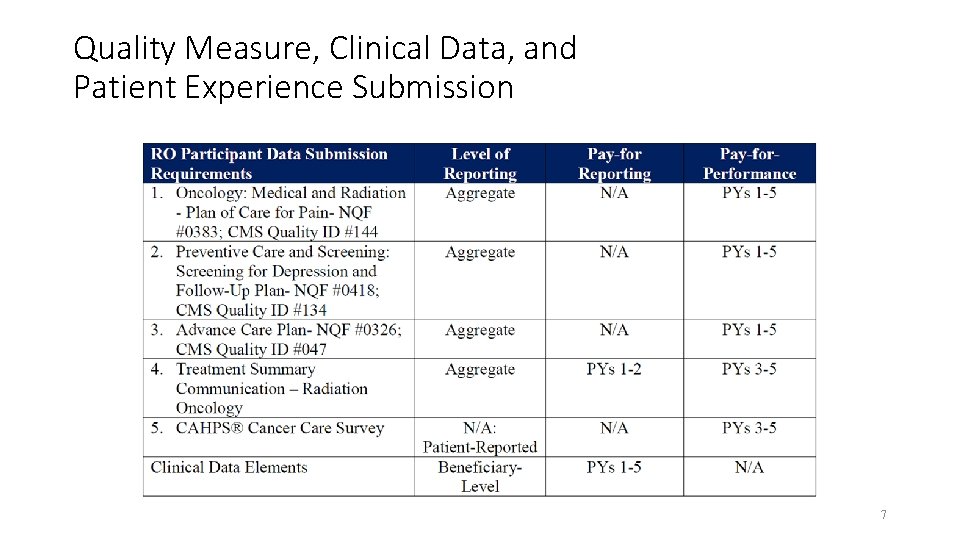
Quality Measure, Clinical Data, and Patient Experience Submission 7
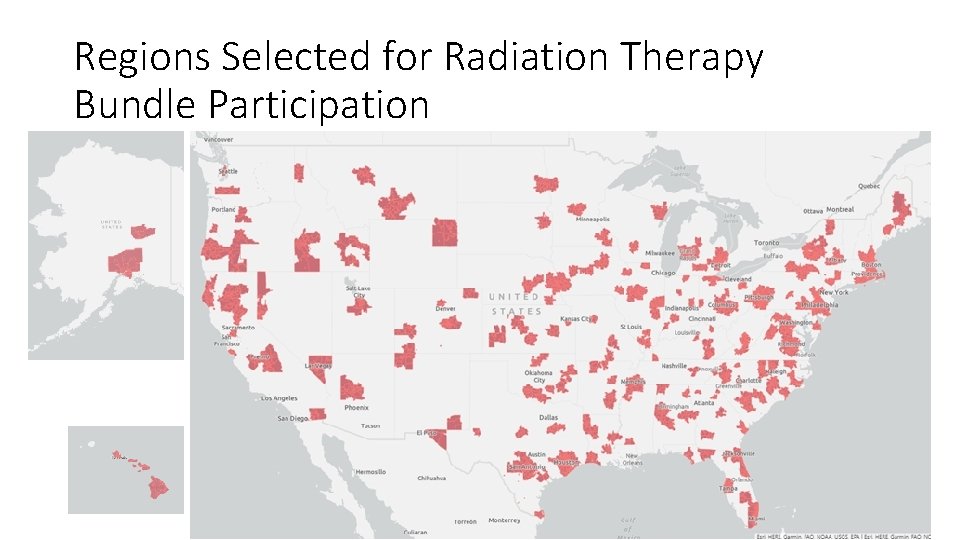
Regions Selected for Radiation Therapy Bundle Participation Source: Radiation Oncology Model Participating Zip Code List

Bundled Payment Overview § Base payment • Varies by cancer • Represents national-average payment for HOPD episodes • Will be updated for inflation factors § Case mix adjustment • Single adjustment for provider • Represents differences in provider payments versus national average from ‘predicted’ factors, including age, sex, mortality, chemotherapy, major procedure, and type of cancer ― Case mix calculated using HOPD episodes • Same historical factor will be applied to every prospective episode regardless of actual patient characteristics § Experience adjustment • Single adjustment for provider • Represents differences in provider payments versus national average from ‘non-predicted’ factors (generally # of fractions & treatment modality) • Same historical factor will be applied to every prospective episode § Blend factor • Applied to experience adjustment to move providers towards the national average ― Providers with experience adjustments >1 will move down 10% towards the national average in first year, increasing to 30% in fifth year ― Providers with experience adjustments <1 will move up 10% towards the national average in each year 9
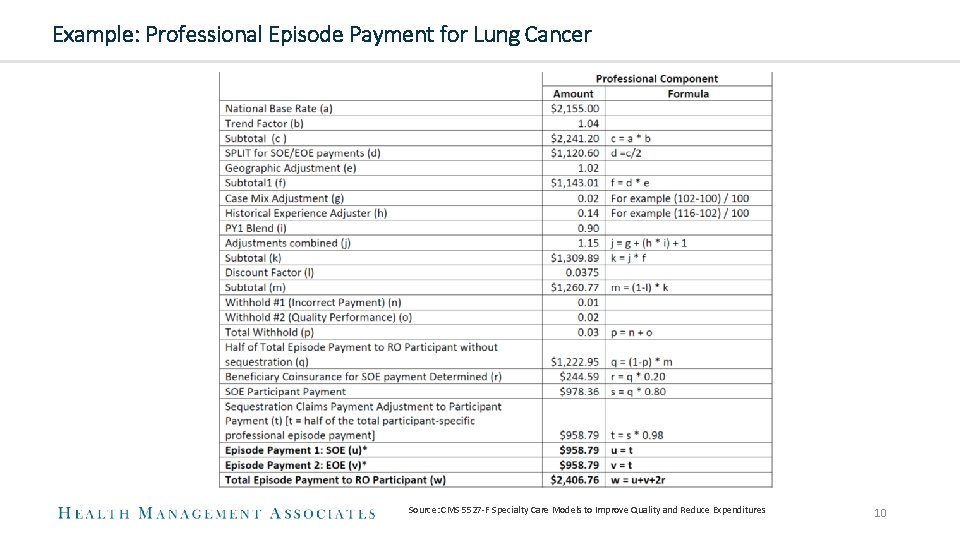
Example: Professional Episode Payment for Lung Cancer Source: CMS 5527 -F Specialty Care Models to Improve Quality and Reduce Expenditures 10

Example: Technical Episode Payment for Lung Cancer Source: CMS 5527 -F Specialty Care Models to Improve Quality and Reduce Expenditures 11

PY 1 Estimated Impact—Final Bundle Impact by Provider Type Impact by Treatment Modality -2. 5% Source: HMA analysis of RO_Episode_File Uterine Cancer -21. 9% Any_Proton Any_SRS Upper GI Cancer Pancreatic Cancer Colorectal Cancer CNS Tumor Cervical Cancer Breast Cancer Brain Metastases Bone Metastases Bladder Cancer 10. 0% 5. 0% 0. 0% -5. 0% -10. 0% -15. 0% -20. 0% -25. 0% Any_CEB -19. 7% Any_IMRT Prostate Cancer -19. 5% Any_brachy Impact by Cancer Type -10. 3% -10. 1% Lymphoma -9. 0% 3. 7% 1. 2% Lung Cancer -5. 9% -7. 0% 0. 5% Liver Cancer -5. 7% -5. 4% 15. 1% Head and Neck Cancer -5. 6% FREESTANDING % change in estimated payments OUTPATIENT Anal Cancer % change in estimated payments Total 12

PY 1 Estimated Impact by Modality & Fractions—Final Bundle Conventional External Beam Episodes 41+ services 0% 31 -40 services 14% 21 -30 services 22% IMRT Episodes 41+ services 20% 31 -40 services 27% 11 -20 services 28% -3. 0% -13. 4% -18. 2% -22. 7% -37. 4%-34. 3% 11 -20 services 21 -30 services 31 -40 services 41+ services % chg in episode payments 24. 3% 8. 3% 1 -10 services 11 -20 services 11% 1 -10 services 36% 54. 3% 28. 4% 1 -10 services 9% 21 -30 services 32% 36. 4% 8. 8% -8. 6% 1 -10 services Source: HMA analysis of RO_Episode_File -3. 4% -22. 3% -25. 2% -22. 9% 11 -20 services 21 -30 services -21. 4% -20. 7% -24. 6% 31 -40 services 41+ services 13

PY 1 Estimated Impact Distribution—Final Bundle Professional Provider Impact Technical Provider Impact 374 289 143 # of technical providers # of professional providers 251 153 112 82 252 207 94 51 16 <-10% to - -9% to - -8% to - -7% to - -6% to - -5% to 9% 8% 7% 6% 5% 0% % chg in estimated payments 9 20 >0% <-8% 41 1 -8% to - -7% to - -6% to - -5% to - -4% to - -3% to 7% 6% 5% 4% 3% 0% % chg in estimated payments Source: HMA analysis of RO_Episode_File, limited to providers with >100 episodes >0% 14
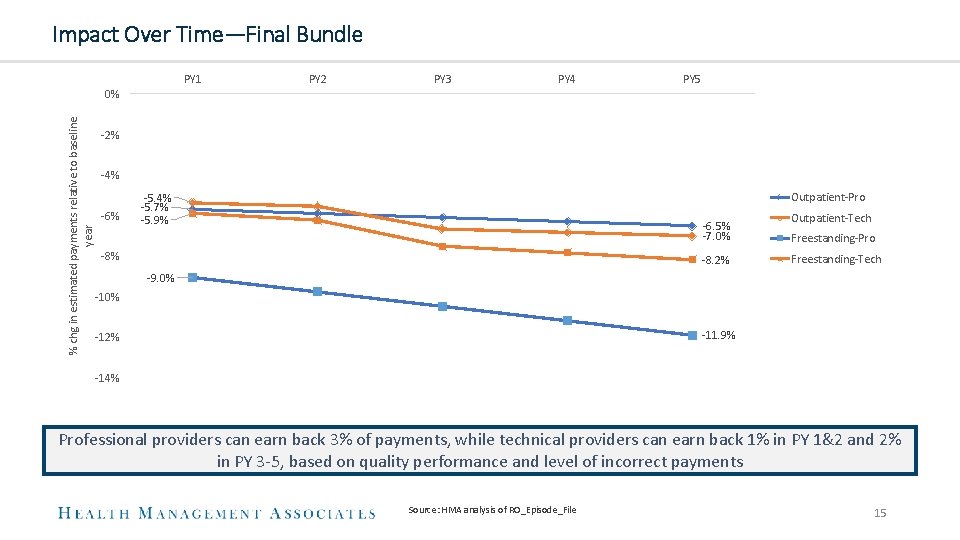
Impact Over Time—Final Bundle PY 1 PY 2 PY 3 PY 4 PY 5 % chg in estimated payments relative to baseline year 0% -2% -4% -6% Outpatient-Pro -5. 4% -5. 7% -5. 9% -6. 5% -7. 0% -8. 2% Outpatient-Tech Freestanding-Pro Freestanding-Tech -9. 0% -11. 9% -12% -14% Professional providers can earn back 3% of payments, while technical providers can earn back 1% in PY 1&2 and 2% in PY 3 -5, based on quality performance and level of incorrect payments Source: HMA analysis of RO_Episode_File 15
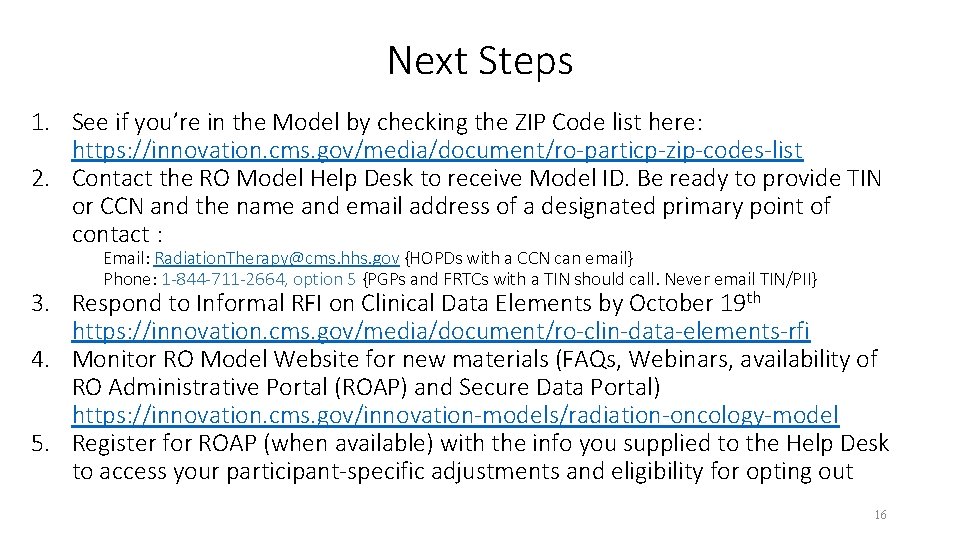
Next Steps 1. See if you’re in the Model by checking the ZIP Code list here: https: //innovation. cms. gov/media/document/ro-particp-zip-codes-list 2. Contact the RO Model Help Desk to receive Model ID. Be ready to provide TIN or CCN and the name and email address of a designated primary point of contact : Email: Radiation. Therapy@cms. hhs. gov {HOPDs with a CCN can email} Phone: 1 -844 -711 -2664, option 5 {PGPs and FRTCs with a TIN should call. Never email TIN/PII} 3. Respond to Informal RFI on Clinical Data Elements by October 19 th https: //innovation. cms. gov/media/document/ro-clin-data-elements-rfi 4. Monitor RO Model Website for new materials (FAQs, Webinars, availability of RO Administrative Portal (ROAP) and Secure Data Portal) https: //innovation. cms. gov/innovation-models/radiation-oncology-model 5. Register for ROAP (when available) with the info you supplied to the Help Desk to access your participant-specific adjustments and eligibility for opting out 16

Questions?

FOR ADDITIONAL QUESTIONS CONTACT CMS RO Model Help Desk Radiation. Therapy@cms. hhs. gov Jason Mc. Kitrick, ACRO Government Relations & Economics Committee Staff jmckitrick@libertypartnersgroup. com 18
Appendix—Case Mix § Case mix is meant to adjust the prospective payment to account for treatment factors that are known to increase or decrease episode payments § CMMI Process • Use cases from hospital (no freestanding) • Calculate single model that predicts change in payment for limited set of variables ― Age, Gender, Died during episode, Chemotherapy, Major procedure ― Model produces values that are the same for every cancer type—essentially assumes spending associated with (for example) age <65 is the same regardless of type of cancer • Apply rates from model to actual episodes at each provider to calculate ‘predicted’ spending ― Sum all predicted values for single provider • Calculate national average (OPD-based) payment for each cancer type • Apply national average to actual episodes at each provider to calculate ‘expected’ spending ― Sum all expected values for a single provider • Case mix = (Sum of Predicted – Sum of Expected) / Sum of Expected • Provider’s case mix will remain constant for the first year of the performance period ― Case mix will be based on provider’s episode mix from 2016 -2018 20

Appendix—Experience & Blend § The Experience Factor adjusts a provider’s prospective episode payments up or down based on their historical payments § The Blend Factor adjusts a provider’s prospective episode payments based on whether they have historically been above or below average § CMMI Process • Calculate each provider’s Experience Factor ― Utilize the Predicted and Expected payments from the case mix calculation ― Experience Factor = (Sum of Actual – Sum of Predicted) / Sum of Expected • Provider’s Experience Factor will remain constant for the entire 5 -year performance period • Apply Blend Factor ― If Experience Factor is <0, Blend Factor = 0. 9 ― If Experience Factor is >0, Blend Factor is 0. 9 for first year, declining to 0. 7 by fifth year • Prospective payment = Cancer-specific base rate * Provider case mix * (1+ (Experience Factor * Blend Factor) ― The efficiency factor dampens the upward or downward adjustment of the experience factor o If a provider’s average episode has been +10% above average, the Blend Factor increases the prospective bundle by +9% in Year 1 and +7% in Year 5 o If a provider’s average episode has been -10% below average, the Blend Factor decreases the prospective bundle by -9% in Year 1 and -9% in Year 5 21
- Slides: 21