Advanced Airway Management AIRWAY MANAGEMENT Airway can be
Advanced Airway Management
AIRWAY MANAGEMENT
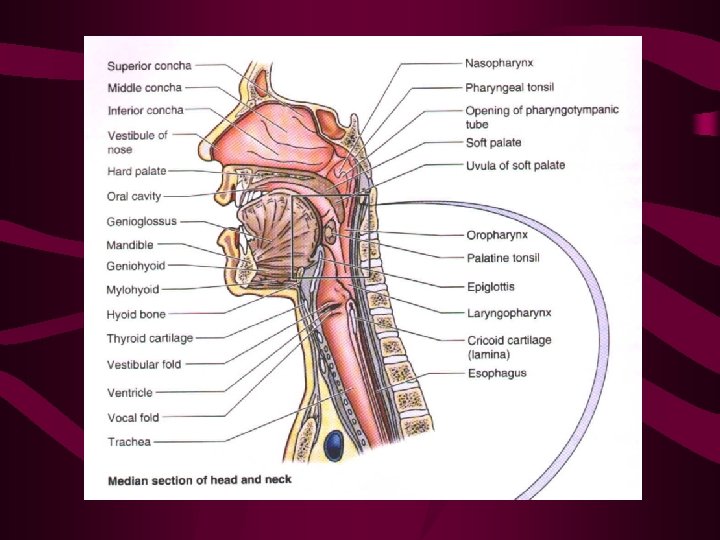
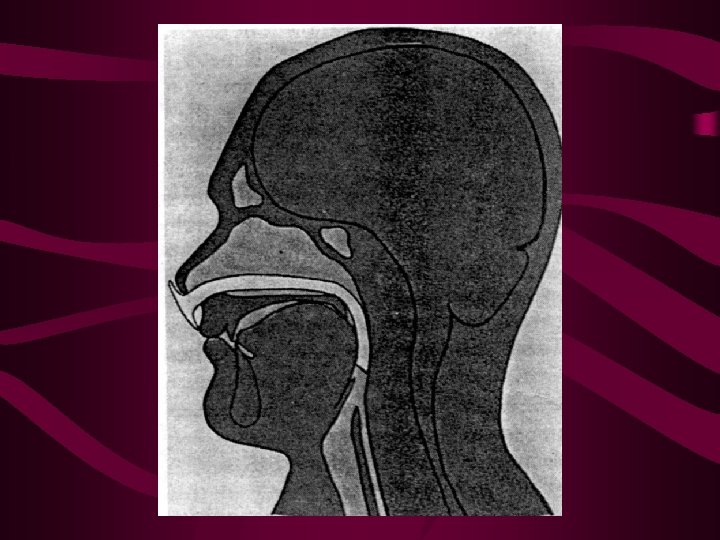
Airway can be managed: • By airway opening manoeuvres or artificial airway adjuncts with or without mask ventilation • By a tube from environment to below vocal cords • By a tube connected to a mask that seals glottic opening, air is delivered to laryngeal inlet • By a tube that isolates oesophagus from airway
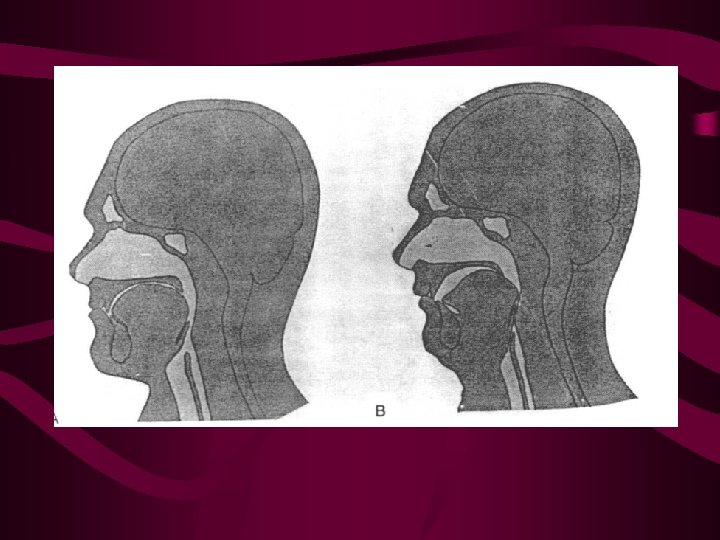
Airway opening techniques - Head tilt + chin lift - Head tilt + neck lift + jaw thrust (Triple airway manoeuvre) - Thumb jaw lift - Modified jaw thrust
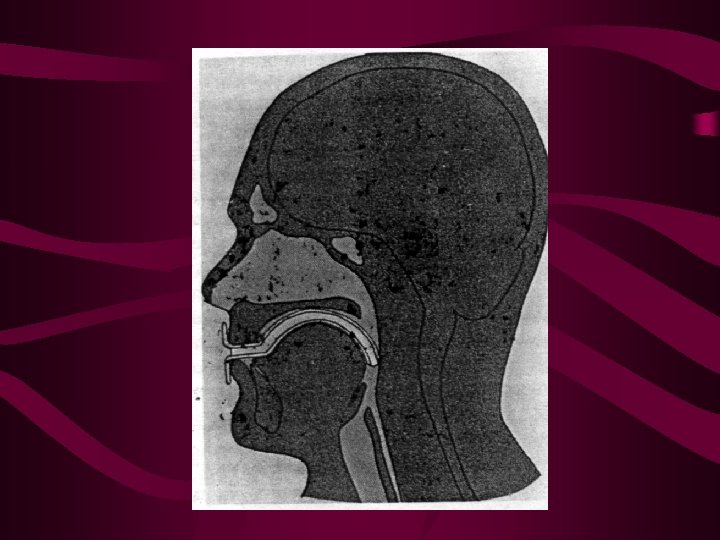
Artificial adjuncts / pharyngeal intubation Oropharyngeal airway: - Unconscious patients - As bite block in semi conscious patients Nasopharyngeal airway: - Trismus, IMF, coma - Contraindicated in bleeding disorders, nasal infections, injury to cribriform plate
Artificial adjuncts / pharyngeal intubation • Suctioning • Mask ventilation: - Beard, snoring, edentulous patients, facial deformities, external facial burns, tumours, infections - In adult with a possible full stomach - X - Paediatric airway - Problems: Pulmonary aspiration


Translaryngeal tracheal intubation • Oral or nasal route • Under direct or indirect vision (flexible fibreoptic laryngoscope or rigid laryngoscope) • In awake or anaesthetised / unconscious state • Awake intubations if maintenance of airway not possible after induction, hemodynamic instability, intestinal obstruction
Orotracheal intubation under direct vision • Indications: - Maintenance of patent airway - Pulmonary toilet - Positive pressure ventilation, oxygenation • Contraindications: - Cervical spine injury - Fracture anterior cranial fossa - Retropharyngeal swelling - Fractured larynx
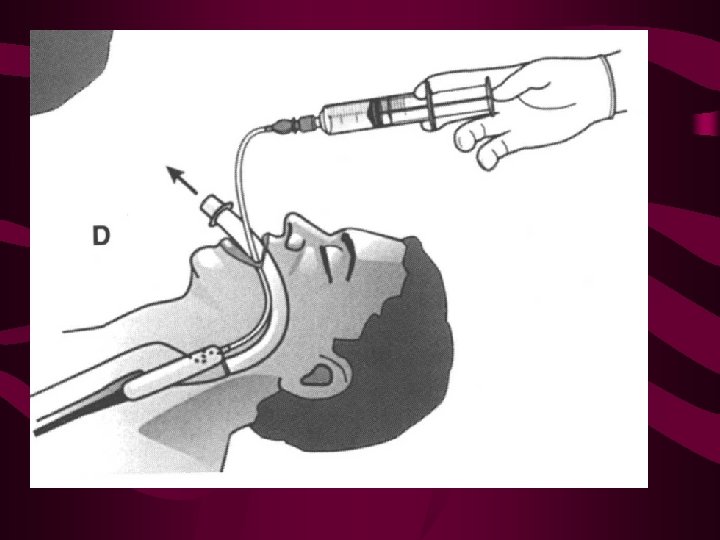
Nasotracheal intubation Advantages over oral intubation: – less chances of dislodgement – better tolerated in awake patient – no risk of biting over tube – easy insertion in neck movement impairment – may produce bacteremia Retrograde catheter guided translaryngeal blind intubation
Confirmation of placement of ETT - Intubation under direct vision - Inspection of chest expansion, Auscultation - Capnometry - Fibreoptic bronchoscopy through ETT - Negative pressure devices - Pulse oximetry, Condensation in tube, movements in reservoir bag, CXR, Cuff palpation, Vital signs, Tube markings
Transtracheal intubation • Needle/Catheter cricothyroidotomy for transtracheal jet ventilation • Emergency cricothyroidotomy • Minitracheostomy, percutaneous dilational cricothyroidotomy, rapid percutaneous tracheostomy
Laryngeal mask airway • Intermediate in design and function between face mask and ETT • Applications: – Primarily meant for awake intubation – For emergency airway management after failed intubation – Children with congenital anomalies – Beard, facial deformities, burns, submandibular soft tissue non compliance

Patients more at risk for aspiration • • • Full stomach (<8 hours fasting) Trauma Intra abdominal pathology Oesophageal disease Pregnancy Obesity
Oesophageal airways • Indications: – Medical personnel not trained in ETT insertion – ETT intubation equipment not available – Attempts at ETT insertion unsuccessful – Contraindicated in gag reflex, oesophageal injury, caustic ingestion. • Types: Oesophageal obturator airway, tracheo oesophageal airway, Oesophageal tracheal combitube
Difficult airway algorithm 1. Assess basic management problems: • Difficult intubation • Difficult ventilation • Difficulty with patient co operation 2. Consider basic management choices: • Non surgical technique vs surgical technique • Awake vs Anaesthetized Intubation • Preservation vs ablation of sp. ventilation
3. Develop primary and alternative strategies: – Awake intubation: - Non surgical intervention - Airway secured by surgical access – Intubation under anaesthesia: - If unsuccessful, return to spontaneous or mask ventilation or awaken patient or emergency surgical access
Complications of laryngoscopy and intubation - Tooth dislodgement, Soft tissue injury - Coughing, laryngospasm, vomitting, aspiration - Injury: trachea, spinal cord, Oesophageal intubation - Hypoxemia, hypercarbia - Hypertension, tachycardia, arrhythmia, bradycardia - Myocardial ischaemia, Brain stem herniation - Complications of nasal intubation
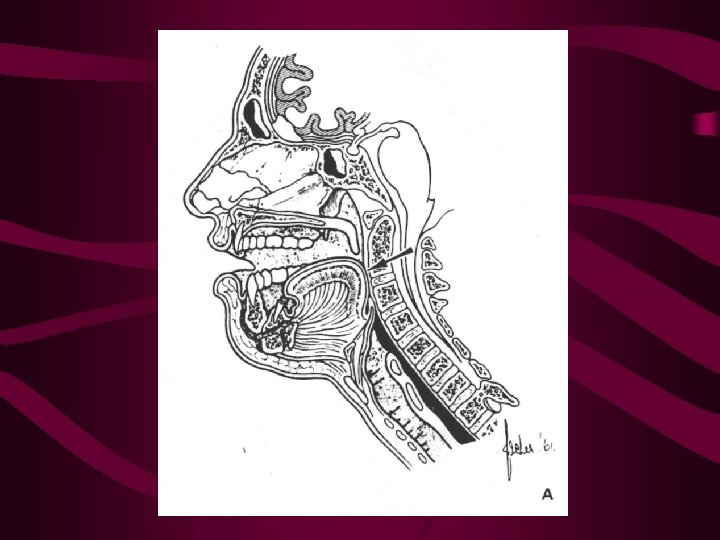
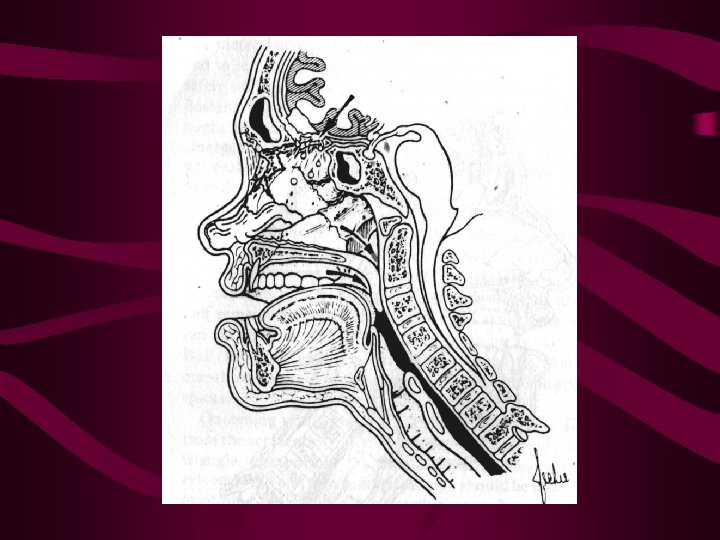
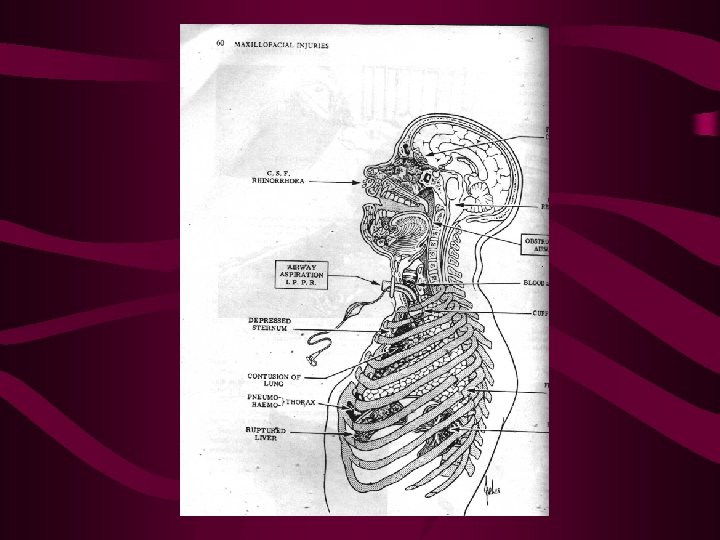
Airway maintenance in maxillofacial injuries • Obstruction by blood clot, vomit, saliva, bone, teeth dentures • Inhalation of any of the above • Relationship of head injury to hypoxia, with blood loss resulting in hypovolemia • Fractures of mandible & maxilla (fig)
Mnemonic in ATLS • • • Airway maintenance with cervical spine control Breathing Circulation with haemorrhage control Discerning the neurological status Complete physical evaluation
Recognition of acute respiratory failure Examinations should include: – Mandibular mobility – Size and mobility of tongue – State and fragility of dentition – Amount and viscosity of secretions – Presence of haemorrhage or masses – Auscultation and percussion of lung fields
Systematic approach to airway management – Recognize airway obstruction – Clear airway (manual & suction) – Reposition patient – Artificial airway – Perform ET intubation – Cricothyroidotomy – Tracheostomy
Tracheostomy • Semiconscious after head injury • To facilitate adequate tarcheo bronchial toilet • Management of concomitant problems • Need for prolonged positive pressure ventilation: • when injuries are severe enough to cause hypercarbia or hypoxia • for control of cerebral oedema
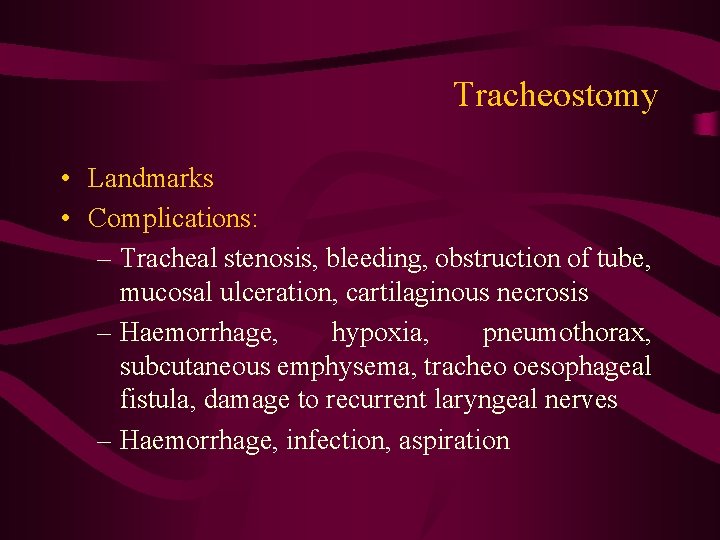
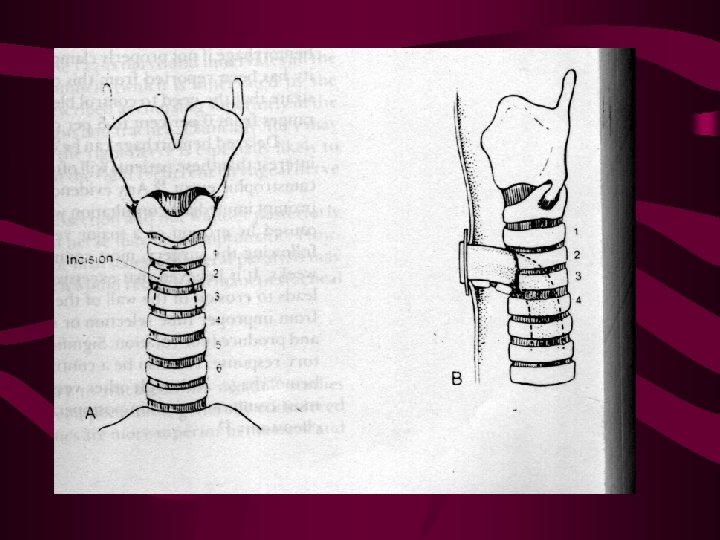
Tracheostomy • Landmarks • Complications: – Tracheal stenosis, bleeding, obstruction of tube, mucosal ulceration, cartilaginous necrosis – Haemorrhage, hypoxia, pneumothorax, subcutaneous emphysema, tracheo oesophageal fistula, damage to recurrent laryngeal nerves – Haemorrhage, infection, aspiration
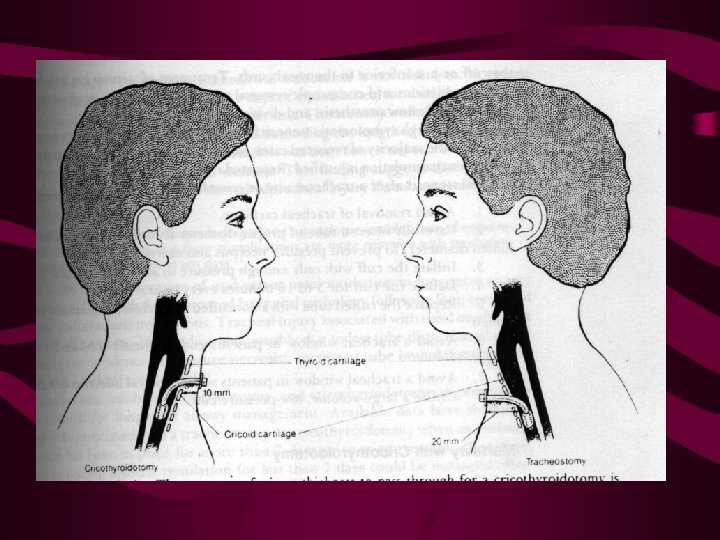
Cricothyroidotomy • Advantages: – More rapid – Less complications – Improved cosmetic result – Less soft tissue thickness to pass through • Contraindicated in children, laryngeal infection
Modified Forms of Respiration • Reflexes which act to protect the respiratory system: – Cough- forceful, spasmodic exhalation of a large volume of air – Sneeze- sudden forceful exhalation from the nose – Hiccough- sudden inspiration caused by spasmodic contraction of the diaphragm & glottic closure – Gag reflex- spastic pharyngeal & esophageal reflex caused by stimulation of posterior pharynx – Sighing- hyperinflation of lungs, opens atelectic alveoli
The ability to breathe and the ability to protect the airway are not always the same.
ASSESSMENT • BSI/ scene safety • General impression • Identify and correct any life threatening conditions: • Responsiveness/ c-spine • Airway • Breathing • Circulation
GENERAL IMPRESSION • POSITION – Tripod – Bolt upright • COPD • CHF • Able to speak in sentences
AIRWAY • Is it patent? – Snoring, gurgling or stridor may indicate potential problems – Secretions, objects, blood, vomitus present • Neck – JVD (jugular vein distention) – TD (tracheal deviation, tugging)
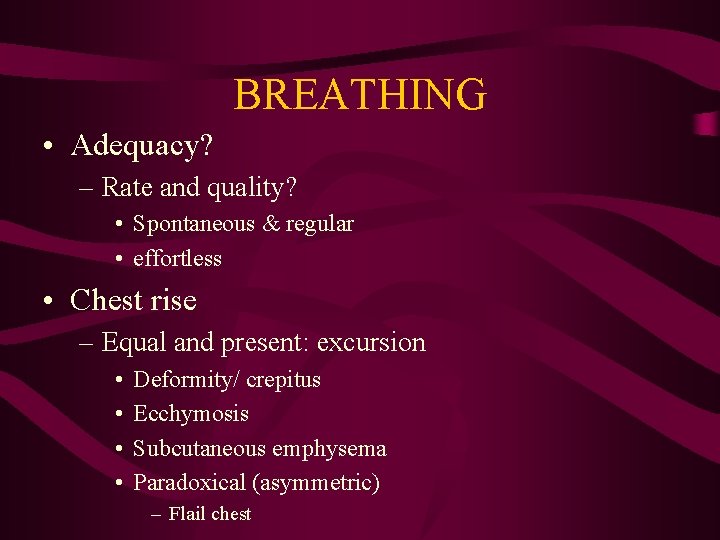
BREATHING • Adequacy? – Rate and quality? • Spontaneous & regular • effortless • Chest rise – Equal and present: excursion • • Deformity/ crepitus Ecchymosis Subcutaneous emphysema Paradoxical (asymmetric) – Flail chest
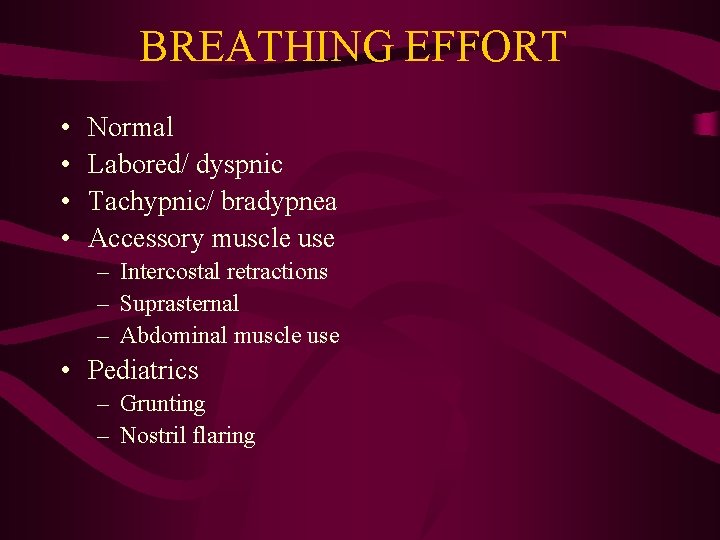
BREATHING EFFORT • • Normal Labored/ dyspnic Tachypnic/ bradypnea Accessory muscle use – Intercostal retractions – Suprasternal – Abdominal muscle use • Pediatrics – Grunting – Nostril flaring

BREATH SOUNDS • • • CTA bilat Diminished Rhonci Rales Wheezing
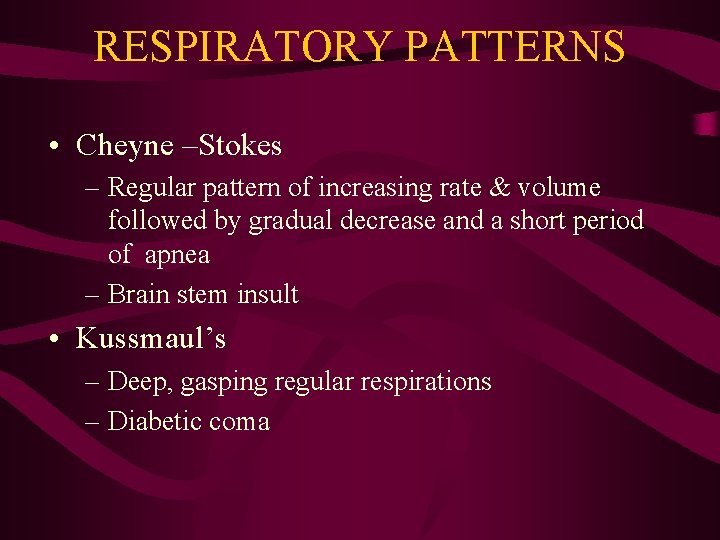
RESPIRATORY PATTERNS • Cheyne –Stokes – Regular pattern of increasing rate & volume followed by gradual decrease and a short period of apnea – Brain stem insult • Kussmaul’s – Deep, gasping regular respirations – Diabetic coma
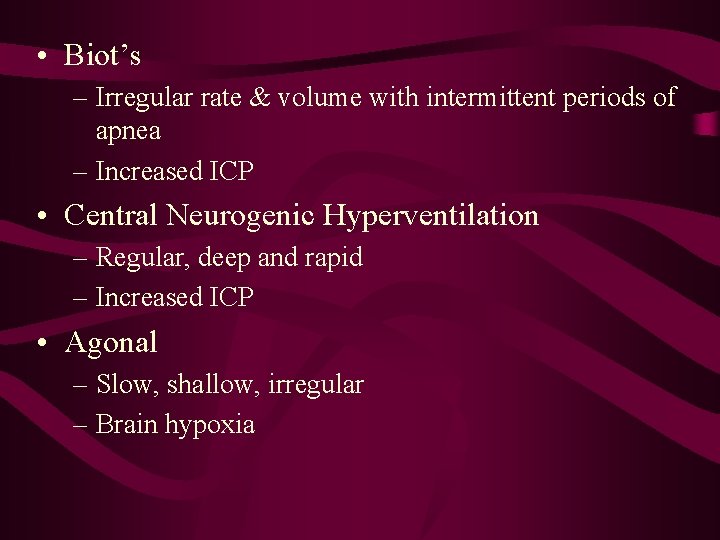
• Biot’s – Irregular rate & volume with intermittent periods of apnea – Increased ICP • Central Neurogenic Hyperventilation – Regular, deep and rapid – Increased ICP • Agonal – Slow, shallow, irregular – Brain hypoxia
PULSUS PARADOXUS • Decrease in systolic BP > 10 mm HG during inspiration • Caused by increase in intrathoracic pressure – COPD • Interference with ventricular filling • Results in decreased BP
DEFINITIONS • Hypoxemia – Reduction of O 2 in arterial blood • Hypoxia – Insufficient O 2 available to meet O 2 requirements • Hypercarbia – Increased level of CO@ in blood
Monitoring • Pulse oximetry • End tidal CO 2 – Quantitative • capnography – Qualitative • Colormetric – Purple to yellow
CAPNOGRAPHY- Et. CO 2 • • Standard of care in hospital Immediate response to extubation Stand up in court to prove intubation Waveform indicative: – Normal – Obstructed airway- do you NEED a B-2 agonist?
WAVEFORM • Normal – Acute upstroke- exhalation – Acute down stroke- inhalation – Straight across – Shark fin- lower airway obstruction
Advanced Airway Management • • • Manual airway control Ventilation Oxygenation …Proceed to advanced management Allows for correction of: – Profound hypoxia – hypercarbia
• Followed by advanced adjunct placement ASAP – Prevent gastric inflation – Prevent aspiration
• • Endotracheal tube Combitube Pt. L LMA
Endotracheal Intubation • When ventilating an unresponsive patient through conventional methods cannot be achieved • Protect the airway • Prolonged artificial respiration required • Patients with or likely to experience upper airway compromise • Decreased tidal volume- bradypnea • Airway obstruction
Advantages • • • Controls the airway Facilitates ventilation/ O 2 Prevents gastric inflation Allows for direct suctioning Medication administration
Disadvantages • Requires extensive and ongoing training for proficiency • Requires specialized equipment • Bypasses physiological function of upper airway – Warm – Filter – Humidify
Complications with Intubated Patients • • Displacement Obstruction Pneumothorax Equipment failure • Contraindicated in epiglottitis
Possible Occurring Complications • • • Bleeding Laryngeal swelling Laryngospasm Vocal cord damage Mucosal necrosis Barotrauma Dental trauma Laryngeal trauma Esophageal placement
Laryngoscope • Move tongue and epiglottis • Allows visualization of cords and glottis • Miller- straight – Lift epiglottis – pediatrics • Macintosh- curved – Fits in valeculla – More room for visualization – Reduced trauma/ gag reflex

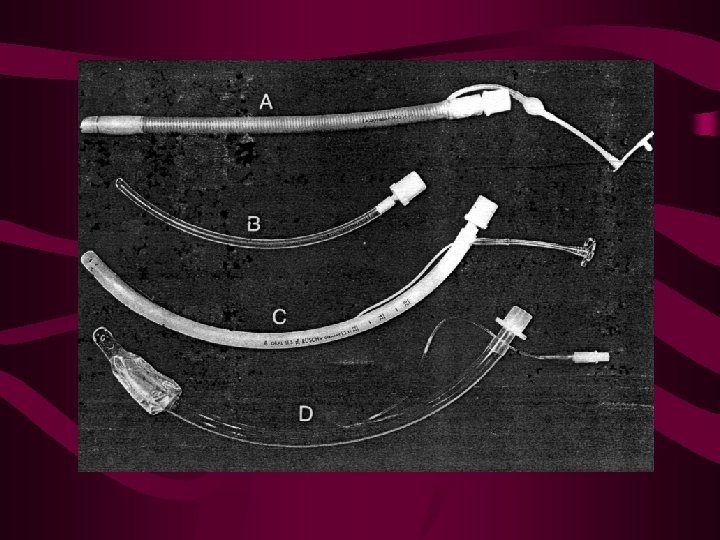
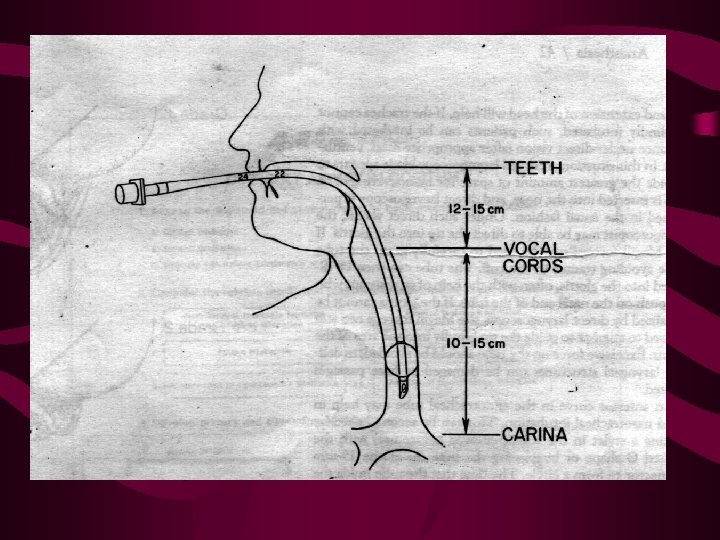
ETT • 15 mm universal adapter • 2. 5 -9. 0 mm diameter • 12 -32 cm length – Male- 23 cm 8. 0 -8. 5 mm – Female- 21 cm 7. 5 -8. 0 mm • Balloon cuff – Occludes tracheal lumen – Pilot balloon • magill forceps
• • • Direct observation Breathing & apneic BSI- goggles & gloves Position- sniffing Preoxygenate – Replace nitrogen stores with O 2 • Assemble & check equipment
Verify Placement • • Esophageal intubation detector CO 2 detector Auscultation Et. CO 2 Capnography – 35 -45 mm Hg – Hyperventilation in head injury with herniation 3035 mm HG
ASPIRATION • Partially dissolved food • Protein dissolving enzymes • Hydrochloric acid
Pathophysiology • • Increased interstitial fluid due to injury Pulmonary edema Destruction of alveoli ARDS – Impaired gas exchange – Hypoxemia – Hypercarbia – Increased mortality
Prevention • Cricoid pressure • Suctioning – Tonsil tip – Whistle tip • Positioning
Hazards of Suctioning • • Cardiac dysrhythmias Increased BP/ HR Decreased BP/ HR Gag reflex – Cough – Increased ICP – Decreased CBF
Multilumen Airways • Combitube • Pharyngotracheal Lumen Airway
Advantages • Blind insertion • Facial seal is not necessary • Can be placed in esophagus or trachea
Contraindications • • • < 16 years old < 5 feet tall or > 6 ft 7 in tall (4 ft combi) Ingestion of caustic substances Esophageal disease Presence of gag reflex
- Slides: 72