Advance Directives How to Reconcile Proxies Surrogates Living





- Slides: 36
Advance Directives: How to Reconcile Proxies, Surrogates, Living Wills and MOLSTs CHALLENGES IN HEALTH CARE MARGARET E. SOMERSET, ESQ. E. RUSSELL KENYON, ESQ SEPTEMBER 26, 2019
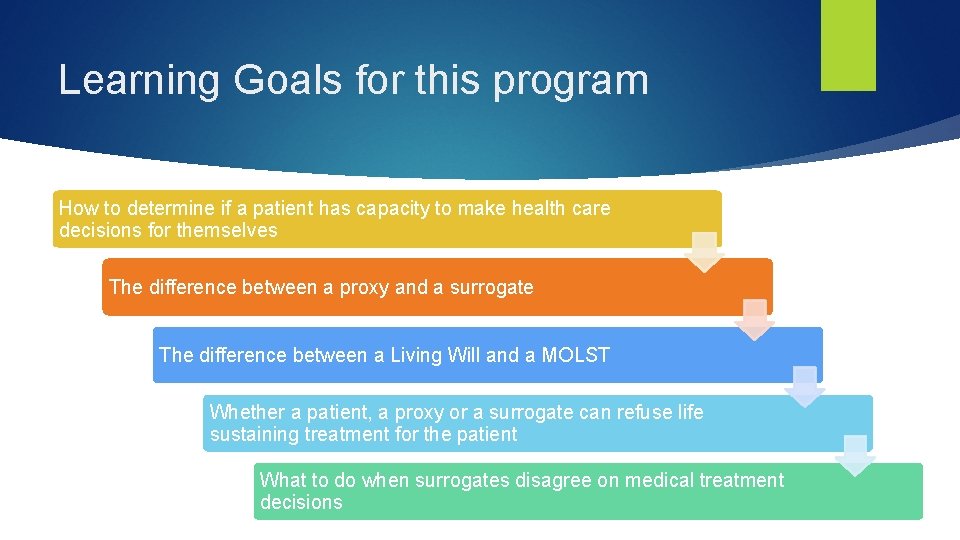
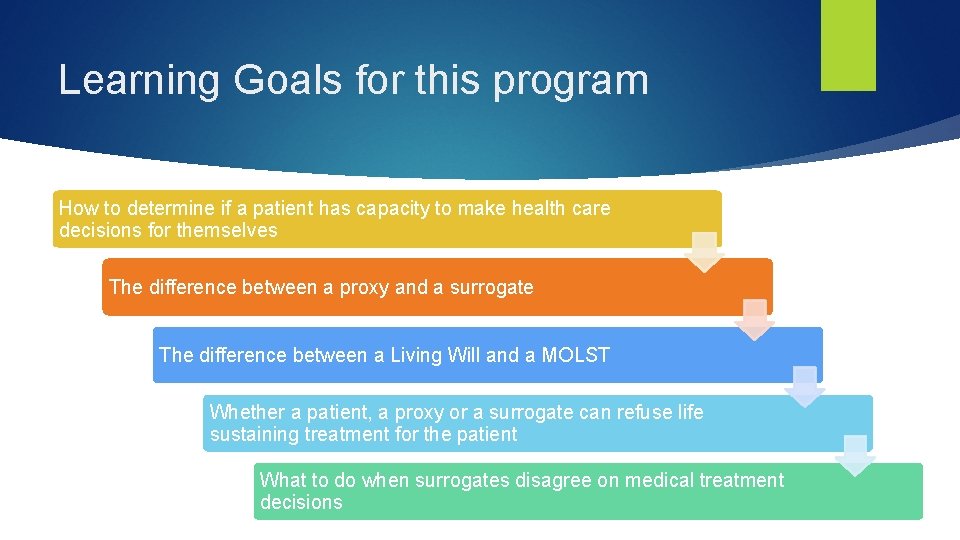
Learning Goals for this program How to determine if a patient has capacity to make health care decisions for themselves The difference between a proxy and a surrogate The difference between a Living Will and a MOLST Whether a patient, a proxy or a surrogate can refuse life sustaining treatment for the patient What to do when surrogates disagree on medical treatment decisions
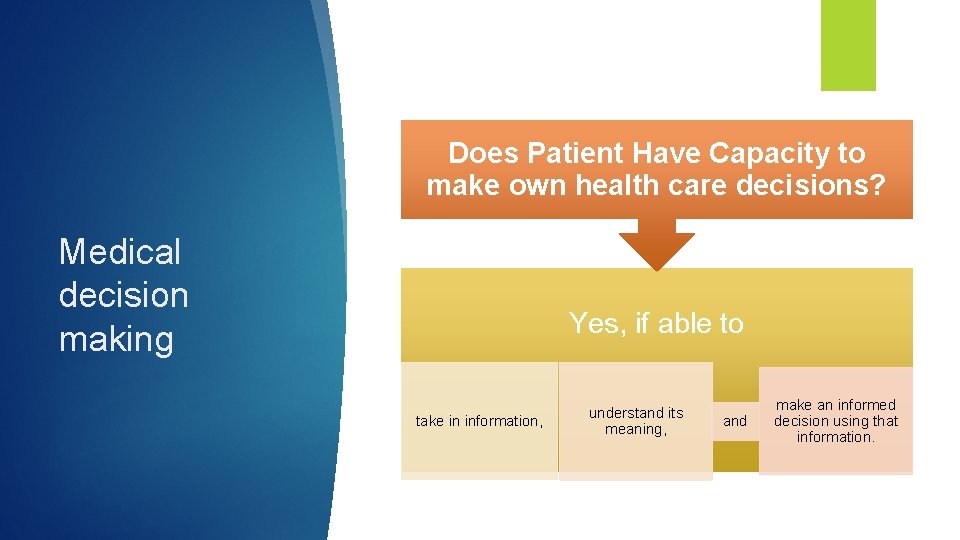
Does Patient Have Capacity to make own health care decisions? Medical decision making Yes, if able to take in information, understand its meaning, and make an informed decision using that information.
Medical decision making Patient who has capacity* has the right to accept or refuse all health care treatment
Medical decision making Patient who has capacity* can refuse life sustaining treatment
Medical decision making Patient cannot direct medical provider to cause suicide
Capacity is presumed unless 2 Physician assessment Medical decision making concludes that patient is incapacitated Or Patient has been previously determined to lack capacity Or A guardian has been appointed
Medical decision making If Patient has been determined to lack capacity to make own health care decisions – who makes decisions? Health Care Proxy Health Care Surrogate
Proxy vs Surrogate Proxy is created by written document Surrogate is selected if there is no written proxy The FHCDA identifies appropriate surrogates
POA vs Proxy and Surrogate A Power of Attorney (POA) has NO authority to Make health care decisions- for the patient. Can only request medical information Or request medical billing information
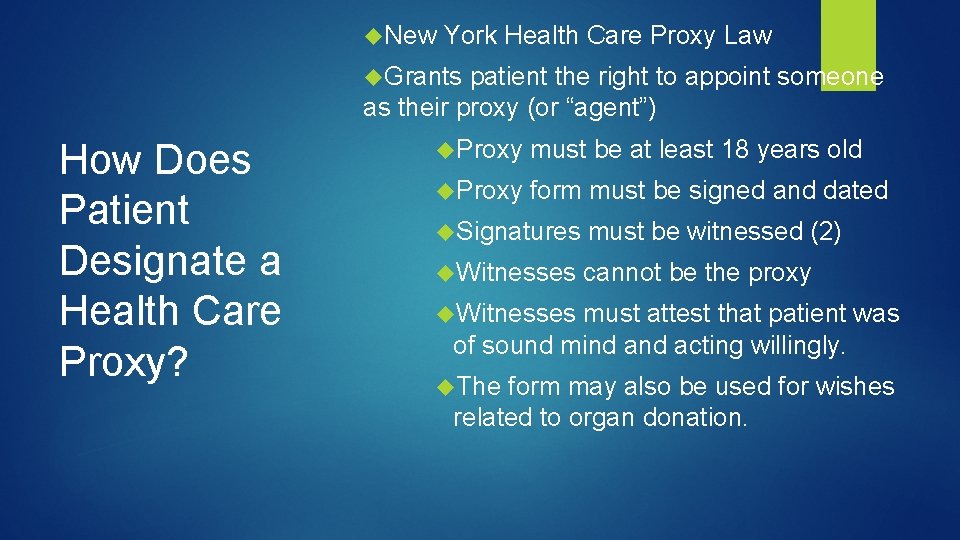
New York Health Care Proxy Law Grants patient the right to appoint someone as their proxy (or “agent”) How Does Patient Designate a Health Care Proxy? Proxy must be at least 18 years old Proxy form must be signed and dated Signatures must be witnessed (2) Witnesses cannot be the proxy Witnesses must attest that patient was of sound mind acting willingly. The form may also be used for wishes related to organ donation.
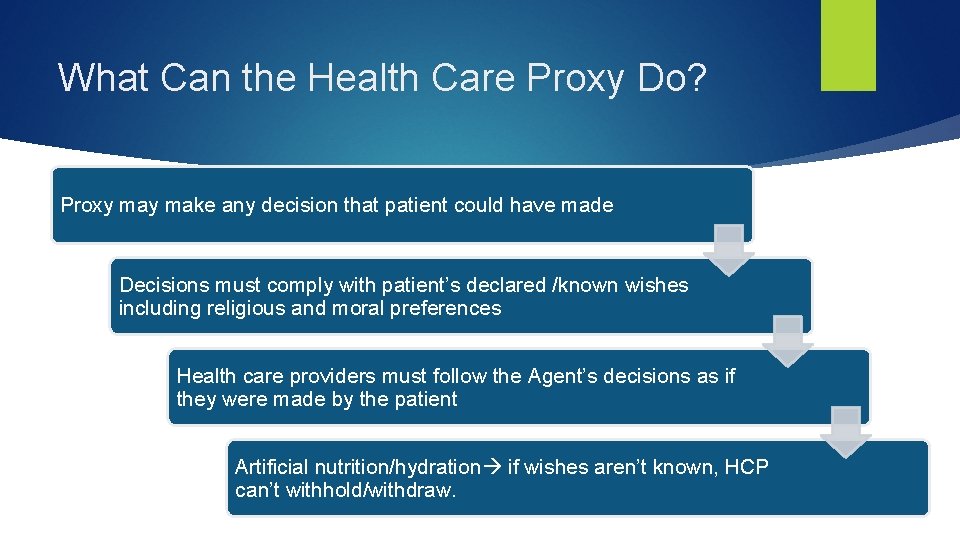
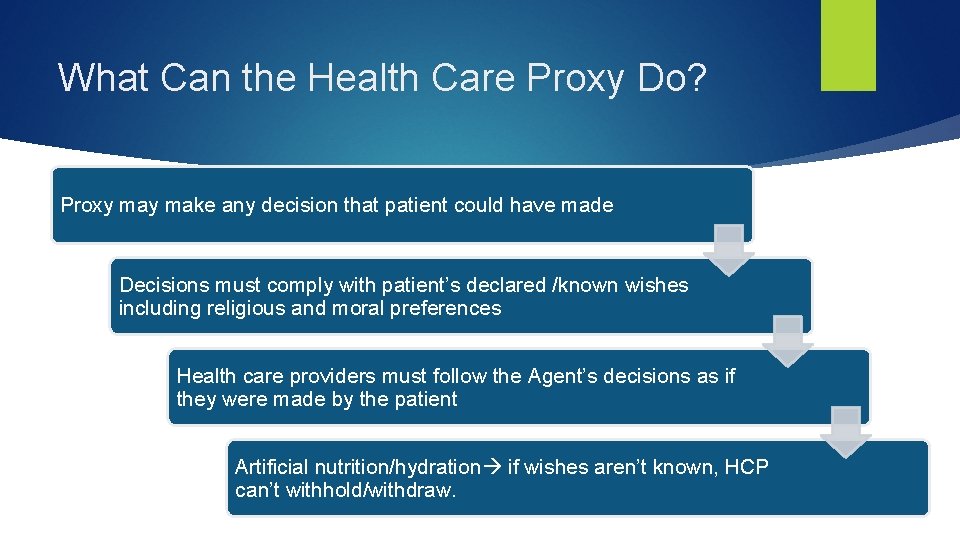
What Can the Health Care Proxy Do? Proxy make any decision that patient could have made Decisions must comply with patient’s declared /known wishes including religious and moral preferences Health care providers must follow the Agent’s decisions as if they were made by the patient Artificial nutrition/hydration if wishes aren’t known, HCP can’t withhold/withdraw.
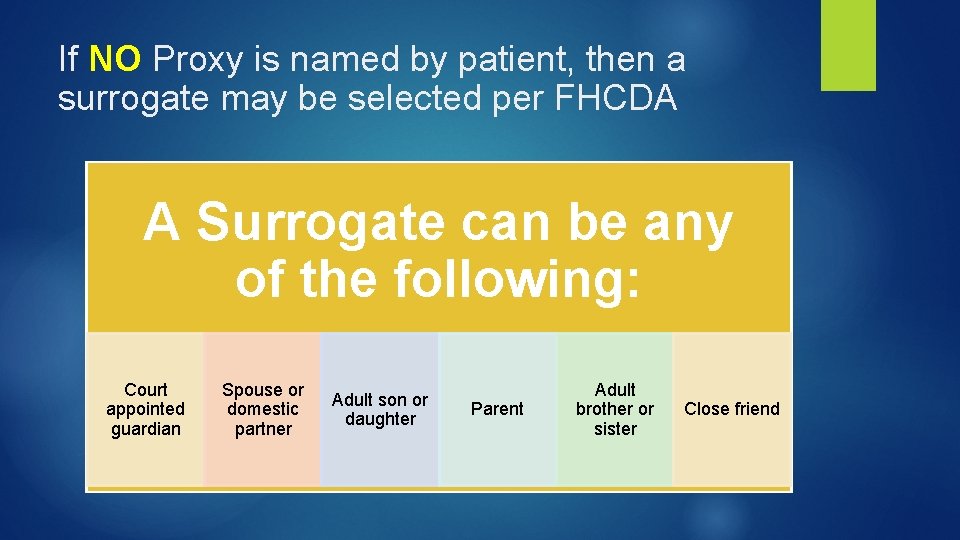
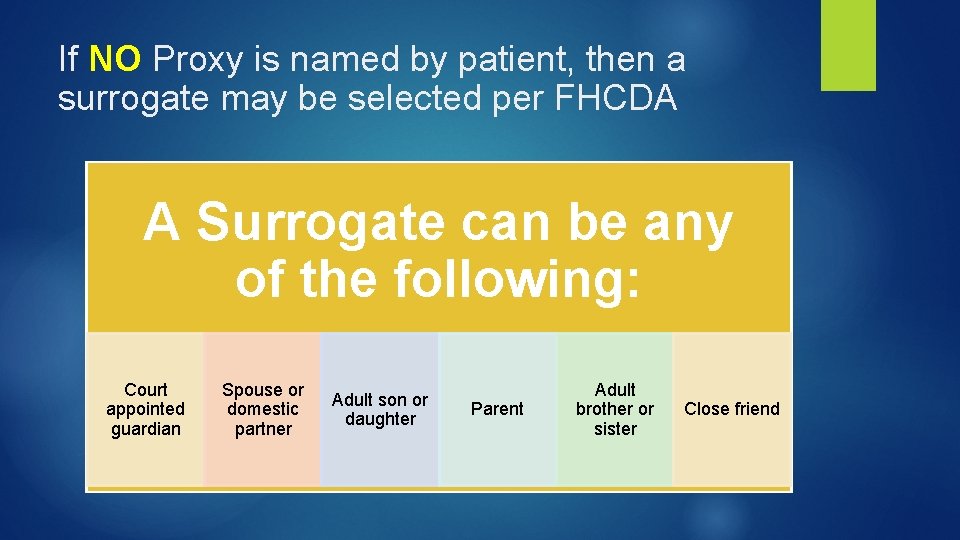
If NO Proxy is named by patient, then a surrogate may be selected per FHCDA A Surrogate can be any of the following: Court appointed guardian Spouse or domestic partner Adult son or daughter Parent Adult brother or sister Close friend

What Can the Surrogate Do? Only acts when patient loses capacity and patient has no proxy. Decisions must comply with patient’s known wishes including patient’s religious or moral beliefs

Determining a patient’s wishes where we have writings: Living Wills, MOLSTs and Advanced Directives
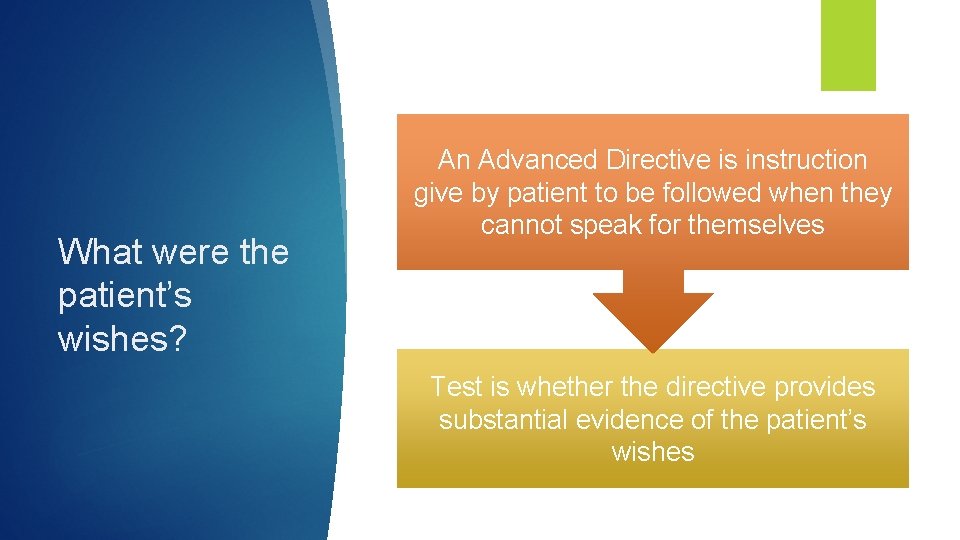
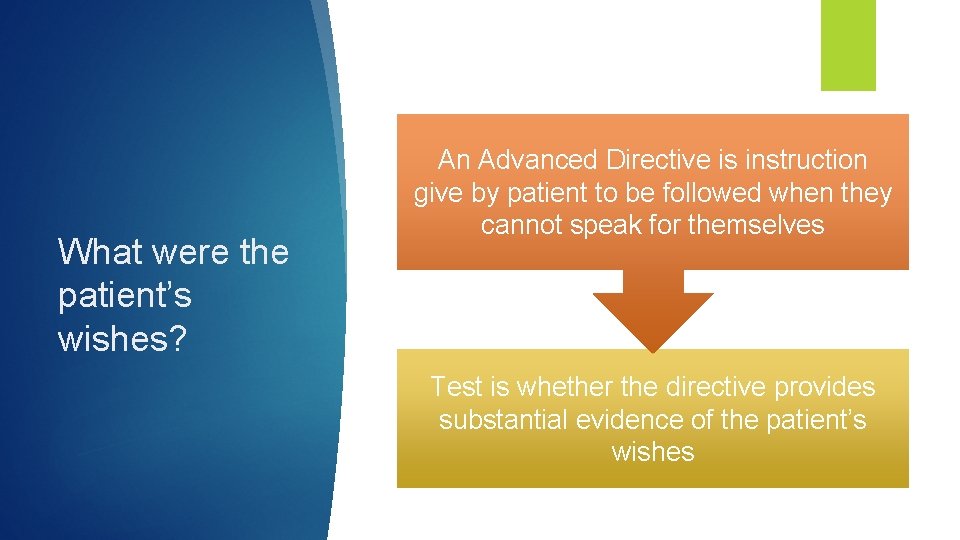
What were the patient’s wishes? An Advanced Directive is instruction give by patient to be followed when they cannot speak for themselves Test is whether the directive provides substantial evidence of the patient’s wishes
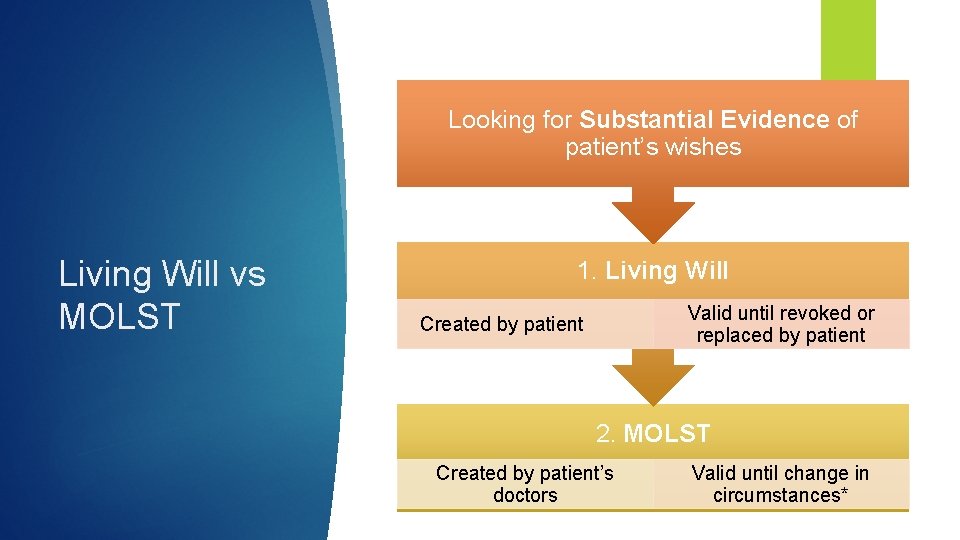
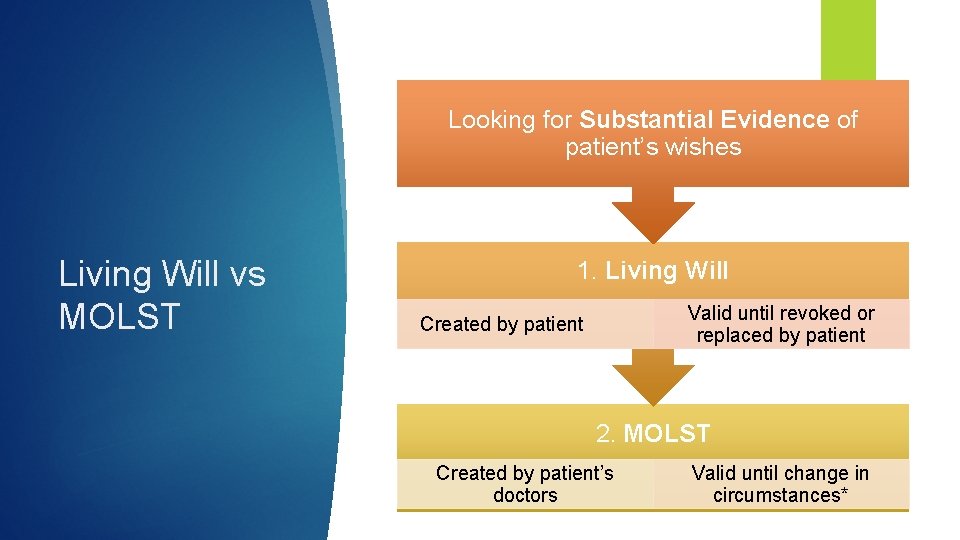
Looking for Substantial Evidence of patient’s wishes Living Will vs MOLST 1. Living Will Valid until revoked or replaced by patient Created by patient 2. MOLST Created by patient’s doctors Valid until change in circumstances*
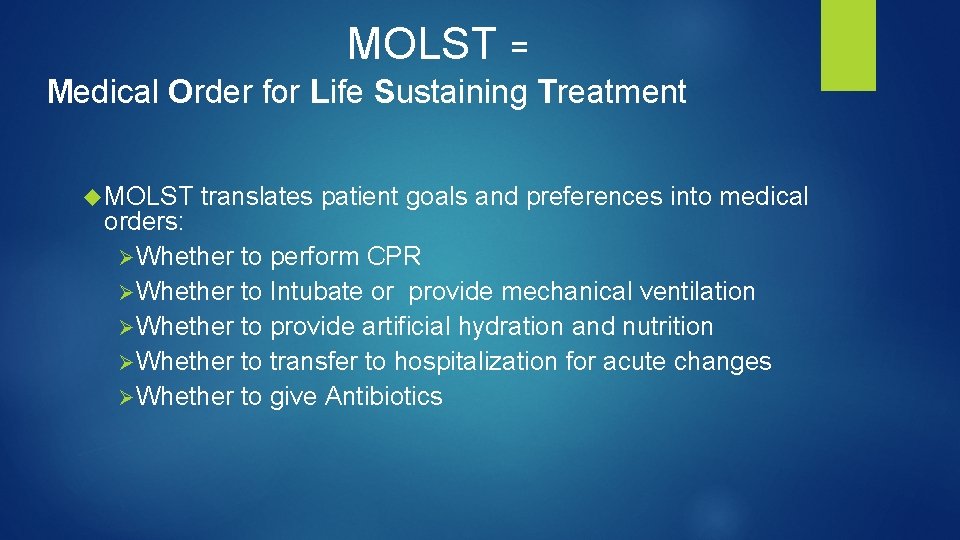
MOLST = Medical Order for Life Sustaining Treatment MOLST translates patient goals and preferences into medical orders: Ø Whether to perform CPR Ø Whether to Intubate or provide mechanical ventilation Ø Whether to provide artificial hydration and nutrition Ø Whether to transfer to hospitalization for acute changes Ø Whether to give Antibiotics
MOLST What is continued enforceability? Q - When a patient in a hospital with DNR order is transferred to a nursing home, does the nursing home need to get the resident's or surrogate's consent again to re-enter the DNR order? Will the nursing home ever have to get that consent? A - The FHCDA provides that the attending physician at the nursing home can enter the DNR order without having to get another consent. The nursing home will never have to get that consent, unless the DNR order is revoked or suspended, and the issue is whether to enter it again.
MOLST = What is continued enforceability? Q - If a patient is admitted to a hospital with a DNR order that was issued in another hospital or nursing home or a nonhospital DNR order, can the attending physician issue an order to continue the DNR order? A - The order that arrived with the patient remains effective until an attending physician examines the patient. That physician must then continue the order, unless the physician determines that the order is no longer appropriate or authorized. In deciding whether the order is still appropriate, the physician should consider whether the difference in response time to a cardiac arrest in the hospital might mean that the prognosis following CPR for the patient would be different, and whether a discussion with the decision-maker for the non-hospital order is warranted. Before canceling the order, the attending physician must make reasonable efforts to notify the person who made the decision. If such notice cannot reasonably be made prior to canceling the order, the attending physician must make such notice as soon as reasonably possible after cancellation. (Revised September 8, 2010).
MOLST = What is continued enforceability? Q - If a patient is admitted to a hospital with a non-hospital DNR order (including a MOLST form), or with a DNR order that was entered at another facility, can that be honored even if the patient had consented to it prior to the current hospitalization? A - Yes. The provisions governing non-hospital DNR orders and inter-institutional transfers obligate the hospital to honor such orders. Hospital emergency services personnel may disregard a nonhospital order not to resuscitate if they believe in good faith that consent to the order has been revoked, or that the order has been cancelled; or if family members or others on the scene (other than such personnel) object to the order and physical confrontation appears likely; and hospital emergency services physicians may direct that the nonhospital order not to resuscitate be disregarded if other significant and exceptional medical circumstances warrant disregarding the order. If the patient is admitted, the medical orders to withhold life-sustaining treatment remain effective until an attending physician examines the patient, whereupon the attending physician must continue the orders, unless the physician determines that the order is no longer appropriate or authorized. There is no requirement to secure another consent from the surrogate. (Added September 8, 2010).
Determining a patient’s wishes where there is nothing in writing
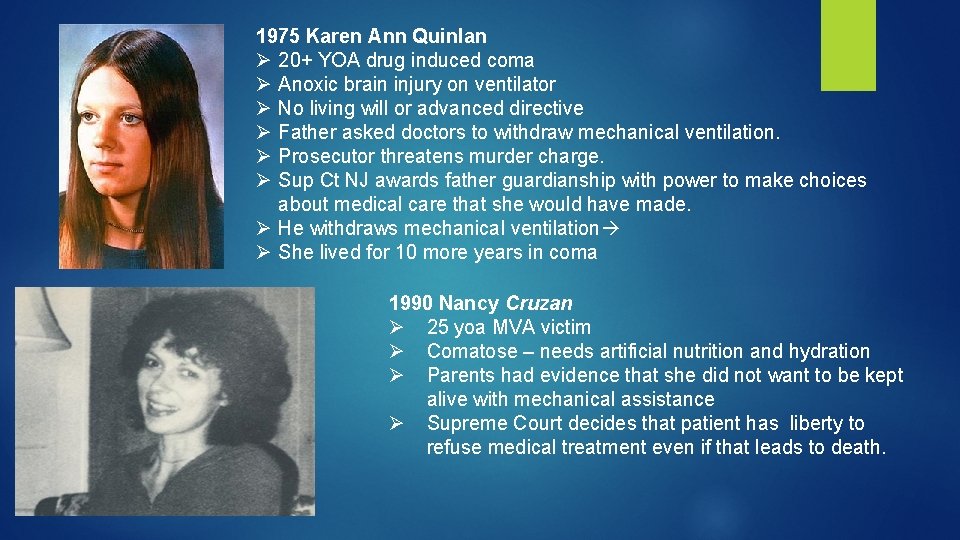
1975 Karen Ann Quinlan Ø 20+ YOA drug induced coma Ø Anoxic brain injury on ventilator Ø No living will or advanced directive Ø Father asked doctors to withdraw mechanical ventilation. Ø Prosecutor threatens murder charge. Ø Sup Ct NJ awards father guardianship with power to make choices about medical care that she would have made. Ø He withdraws mechanical ventilation Ø She lived for 10 more years in coma 1990 Nancy Cruzan Ø 25 yoa MVA victim Ø Comatose – needs artificial nutrition and hydration Ø Parents had evidence that she did not want to be kept alive with mechanical assistance Ø Supreme Court decides that patient has liberty to refuse medical treatment even if that leads to death.
What is current standards for proxy or surrogate If the patient’s wishes are not known? Agent must act in the patient’s best interest Decisions on major medical treatments require 2 Physician concurrence Special tests if withdrawing or withholding LST

Where patient’s wishes are not known Decisions to withdraw or withhold life sustaining treatment Neither Proxy nor Surrogate can withhold or withdraw life sustaining treatment 2 physician concurrence under “futility standard” or court order
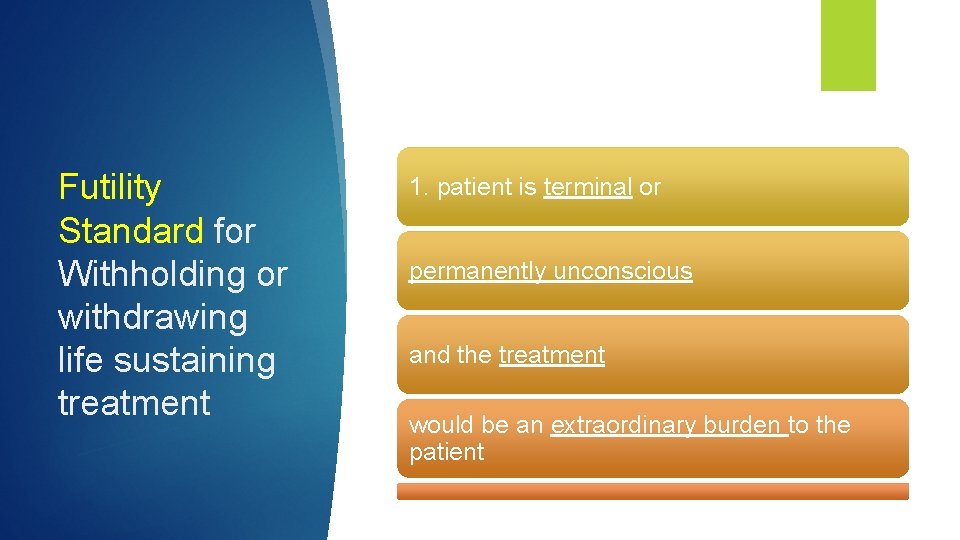
Futility Standard for Withholding or withdrawing life sustaining treatment 1. patient is terminal or permanently unconscious and the treatment would be an extraordinary burden to the patient
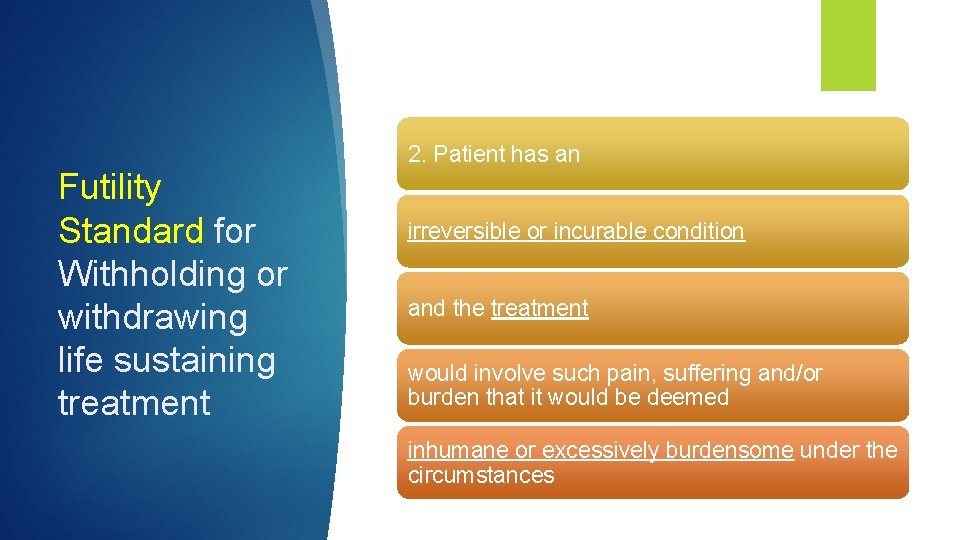
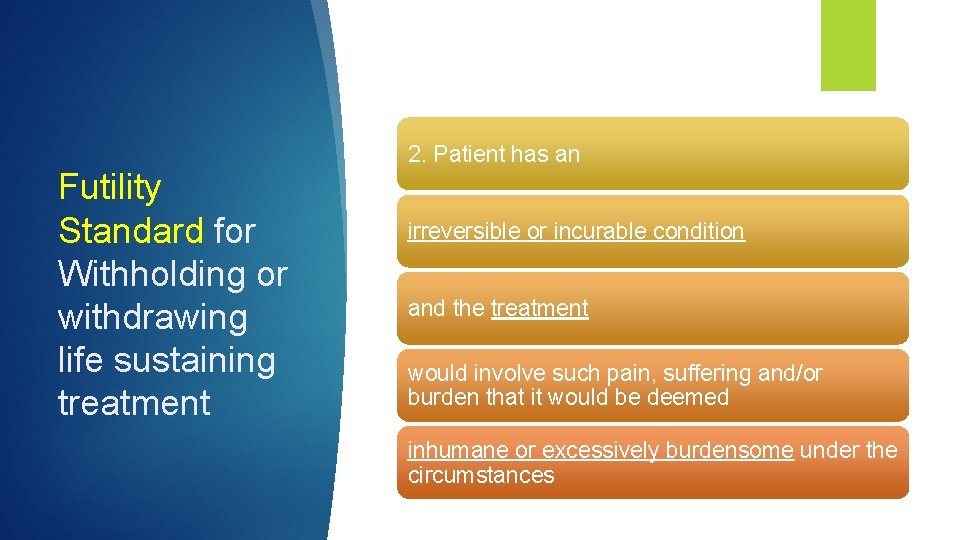
2. Patient has an Futility Standard for Withholding or withdrawing life sustaining treatment irreversible or incurable condition and the treatment would involve such pain, suffering and/or burden that it would be deemed inhumane or excessively burdensome under the circumstances
Resolving conflicts with advanced directives, surrogates and proxies
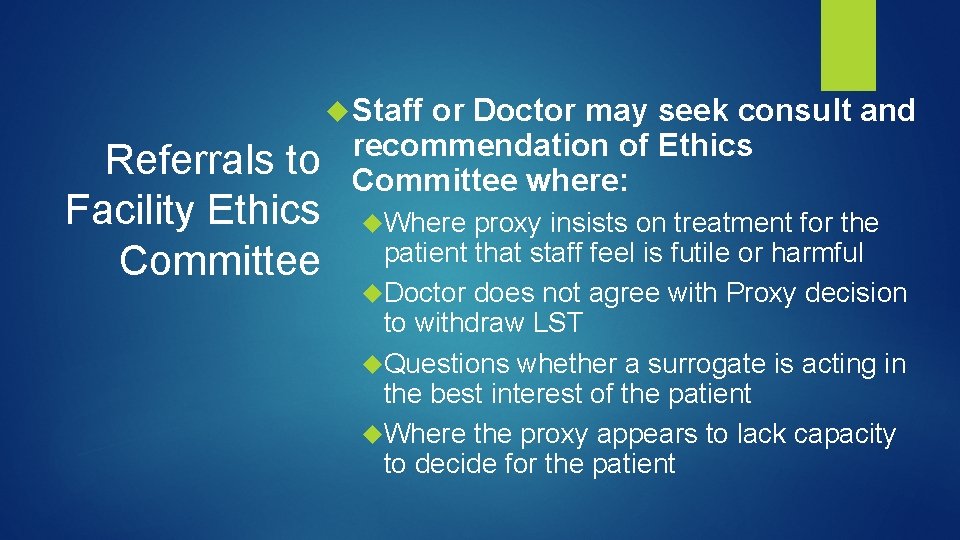
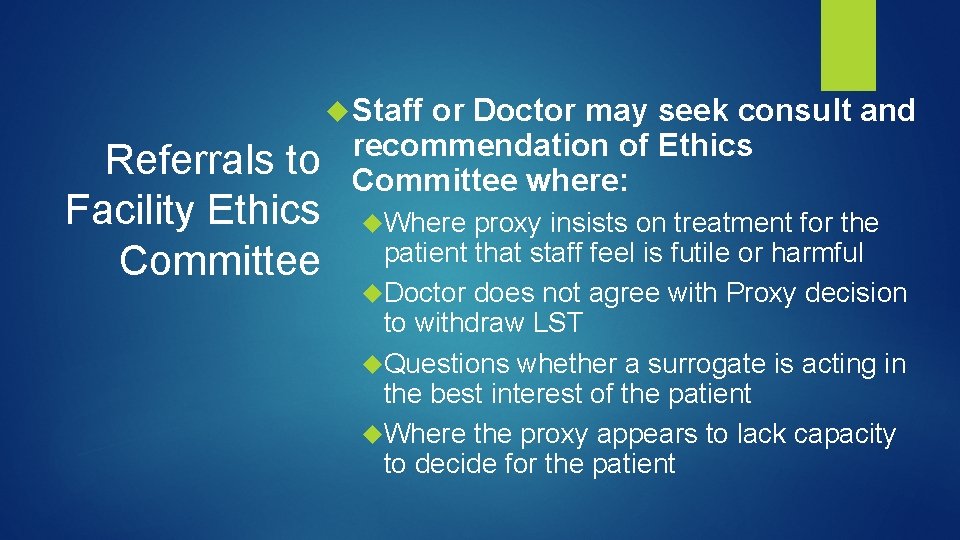
Staff Referrals to Facility Ethics Committee or Doctor may seek consult and recommendation of Ethics Committee where: Where proxy insists on treatment for the patient that staff feel is futile or harmful Doctor does not agree with Proxy decision to withdraw LST Questions whether a surrogate is acting in the best interest of the patient Where the proxy appears to lack capacity to decide for the patient
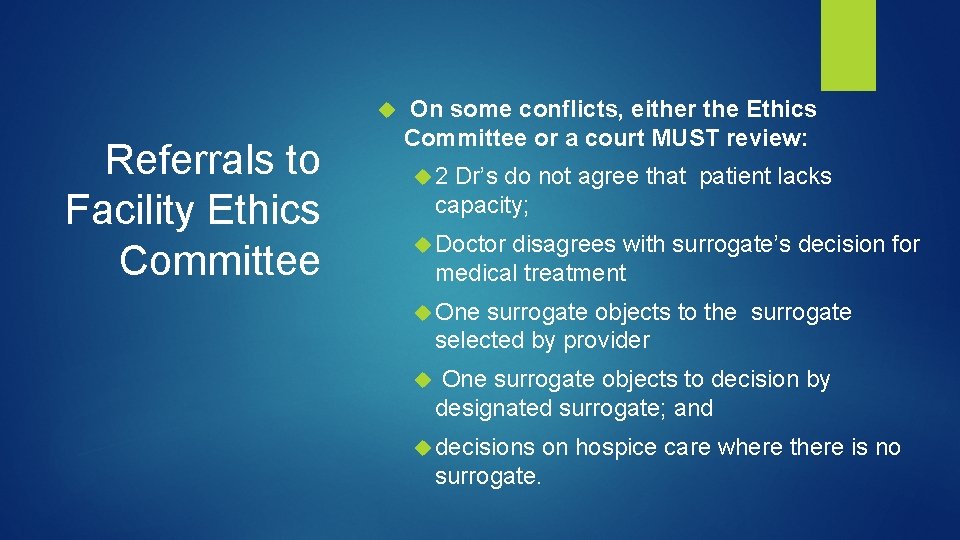
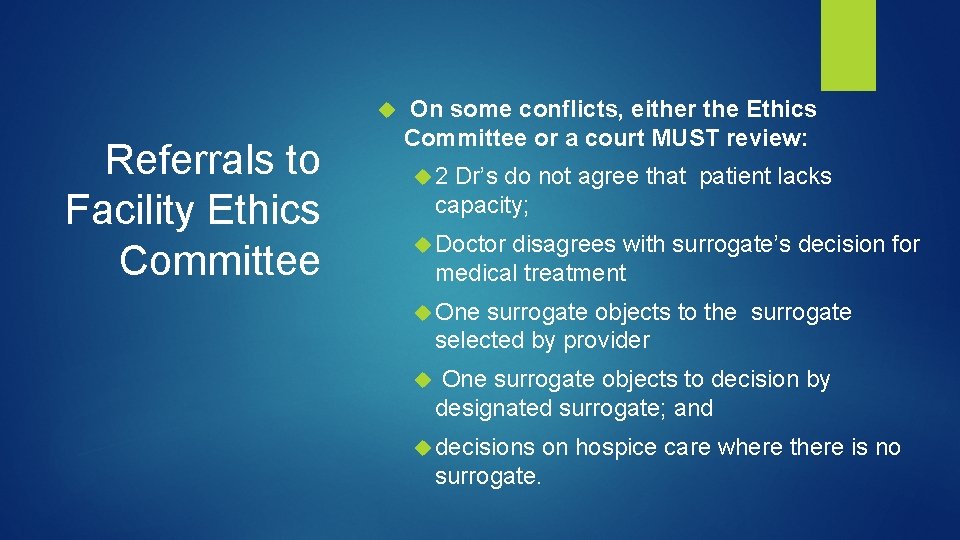
Referrals to Facility Ethics Committee On some conflicts, either the Ethics Committee or a court MUST review: 2 Dr’s do not agree that patient lacks capacity; Doctor disagrees with surrogate’s decision for medical treatment One surrogate objects to the surrogate selected by provider One surrogate objects to decision by designated surrogate; and decisions on hospice care where there is no surrogate.
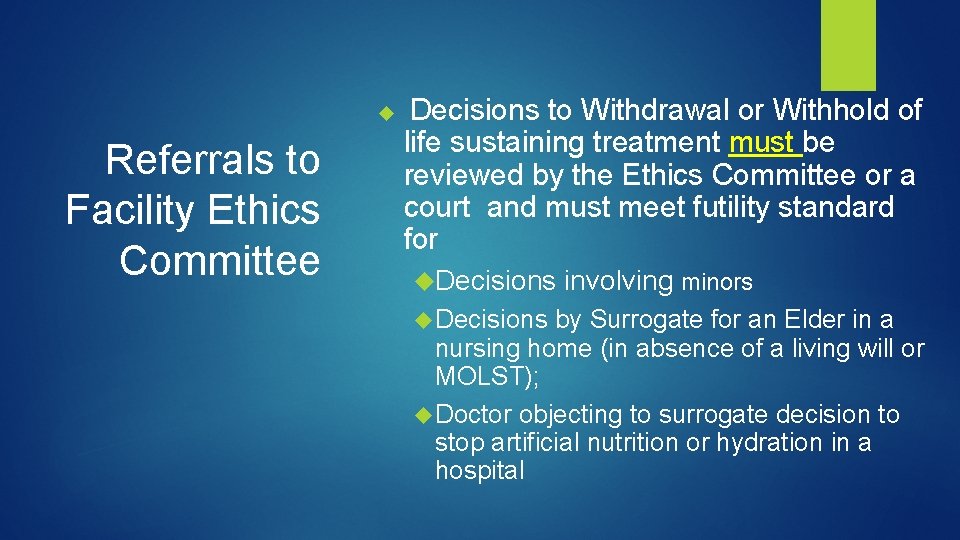
Referrals to Facility Ethics Committee Decisions to Withdrawal or Withhold of life sustaining treatment must be reviewed by the Ethics Committee or a court and must meet futility standard for Decisions involving minors Decisions by Surrogate for an Elder in a nursing home (in absence of a living will or MOLST); Doctor objecting to surrogate decision to stop artificial nutrition or hydration in a hospital
Conflicts between Proxy and Patient’s Directives Conflict #1: Proxy decision is inconsistent with patient’s written advanced directive. Solution: A: If Proxy can show more current evidence of the patient’s wishes to support alternate treatment chosen by proxy, then proxy’s decision can be honored Solution B: Medical team can seek assistance of Ethics Committee to provide recommendation on how to reconcile conflict
Conflicts between Surrogates Conflict #2: Multiple relatives, who all qualify as surrogates, disagree on choice of treatment for patient. Solution: A: Choice of treatment should comport with patient’s declared wishes – look for substantial evidence of the patient’s wishes in writings or discussions with family and friends Solution B: Medical team can seek assistance of Ethics Committee to provide recommendation on how to reconcile conflict

Conflicts on life sustaining treatment Conflict Terminal Illness? Incurable Disease? Seek Ethics review • Conflict #3: Proxy or Surrogate wishes to withdraw life sustaining treatment but the patient’s written directives are silent on whether they would want treatment to be withdrawn under these circumstances. • Solution: A: Determine if patient is suffering from a terminal illness. If so, ask if the proposed treatment is futile. . • Solution B: Determine if the patient is suffering from an incurable condition. If so, ask whether the treatment would cause the patient pain or suffering such that the treatment would be inhumane

Questions and Answers
 Advantages and disadvantages of advance directives
Advantages and disadvantages of advance directives Swmbh
Swmbh Idph advance directives
Idph advance directives What are the types of advance directives
What are the types of advance directives Document indexing methods
Document indexing methods C++ static reflection
C++ static reflection Paleoclimate proxies
Paleoclimate proxies Control account number
Control account number 4-1 computing your total checking account deposit answers
4-1 computing your total checking account deposit answers First reconcile with your brother
First reconcile with your brother 2-2 reconcile a bank statement
2-2 reconcile a bank statement Reconciled medical definition
Reconciled medical definition How to reconcile in quickbooks 2015
How to reconcile in quickbooks 2015 Living non living dead
Living non living dead This organelle often ships proteins to the golgi apparatus
This organelle often ships proteins to the golgi apparatus Pyramid hesd
Pyramid hesd Is a moss living or nonliving
Is a moss living or nonliving Fsis directives
Fsis directives What are jsp directives
What are jsp directives New approach directives
New approach directives Forest service office of tribal relations
Forest service office of tribal relations Assembler directives of 8086
Assembler directives of 8086 Phases of assembler
Phases of assembler Commander's intent example
Commander's intent example Personal directives act
Personal directives act Language processor
Language processor Compiler control directives in c
Compiler control directives in c Data related operators and directives in assembly language
Data related operators and directives in assembly language Examples of eu directives
Examples of eu directives 8051 assembly language programming examples
8051 assembly language programming examples Iec directives
Iec directives Audit board of ethiopia
Audit board of ethiopia Ce directives
Ce directives Nws directives
Nws directives Simple sic assembler
Simple sic assembler Advance image search
Advance image search Sculptor persona
Sculptor persona