Adult Spinal Deformity Whats new in treatment Emre








- Slides: 33

Adult Spinal Deformity What’s new in treatment? Emre Acaroglu MD Ankara Spine center Ankara, Turkey 1
Scheme • What is the best treatment? • Do complications affect results? • A new score to decrease the rate of mechanical complications 2

Identifying The Best Treatment in Adult Spinal Deformity: A Decision Analysis Approach Emre Acaroglu 1, Aysun Cetinyurek Yavuz 2, Umit Ozgur Guler 1, Selcen Yuksel 3, Yasemin Yavuz 4, Selim Ayhan 1, Montse Domingo. Sabat 5, Ferran Pellise 6, Francisco Javier Sanchez Perez-Grueso 7, Ahmet Alanay 8, Ibrahim Obeid 9, Frank Kleinstück 10, European Spine Study Group-ESSG 1 Ankara Spine Center, Ankara, Turkey 2 Biostatistics, Clin. IST-eu, Nijmegen, Netherlands 3 Biostatistics, Yildirim Beyazit University School of Medicine, Ankara, Turkey 4 Biostatistics, Ankara University School of Medicine, Ankara, Turkey 5 Fundacio Institut de Recerca Vall d’Hebron, Barcelona, Spain 6 Spine Unit, Hospital Universitari Vall d’Hebron, Barcelona, Spain 7 Spine Unit, Hospital Universitari La Paz, Madrid, Spain 8 Comprehensive Spine Center, Acibadem Maslak Hospital, Istanbul, Turkey 9 Spine Unit, Bordeaux University Hospital, Bordeaux, France 10 Spine Center, Schulthess Klinik, Zürich, Switzerland 11/22/2020 European Spine Study Group 3

Purpose • To identify the best (optimum) treatment in ASD • Using a statistical “decision analysis” model • Hypotheses: – Surgery may yield better overall clinical results – Surgery is associated with more complications and overall burden 11/22/2020 European Spine Study Group 4
Patients and Methods • International multicentre prospective database • ASD Patients – Overall n=968 • Included n=535 (1 year f-up) • non-surgical (NS): 371 • surgical (S): 164 11/22/2020 European Spine Study Group 5

Patients and Methods – Decision Analysis • Baseline – Outcome probabilities » improvement (↓ in ODI > 8 pts) » no change » deterioration (↑ in ODI > 8 pts) » Death / complete paralysis No improvement – The values of preference – utilities – Combine information and assign quality adjusted life expectancy (QALE) 11/22/2020 European Spine Study Group 6
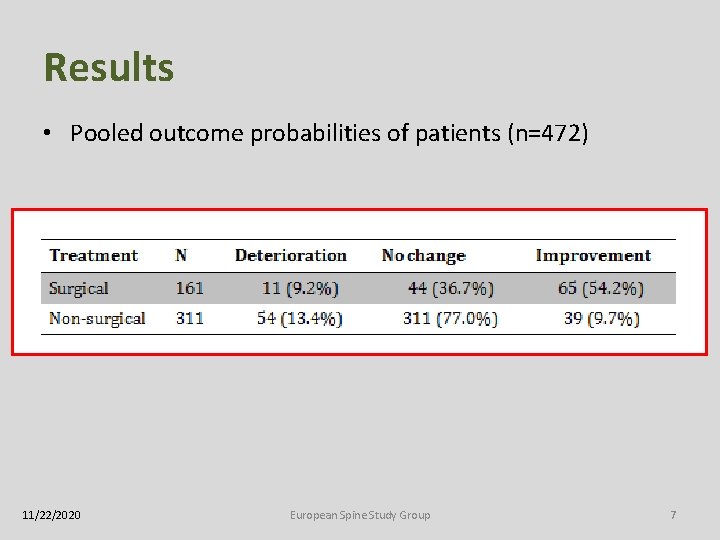
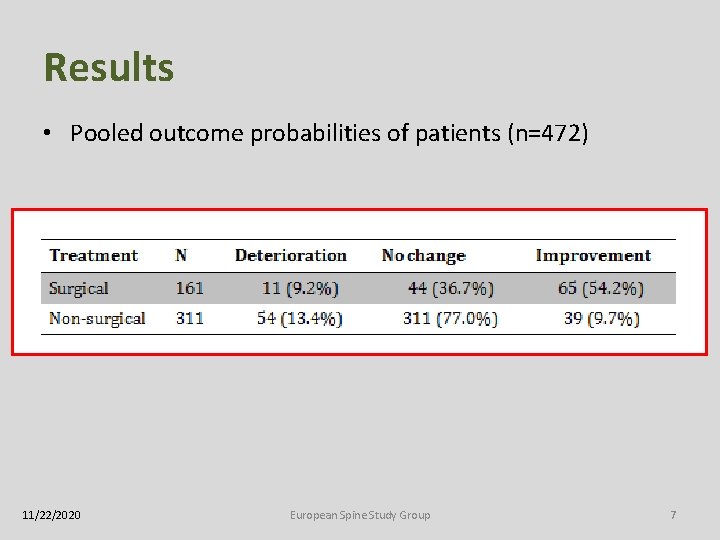
Results • Pooled outcome probabilities of patients (n=472) 11/22/2020 European Spine Study Group 7
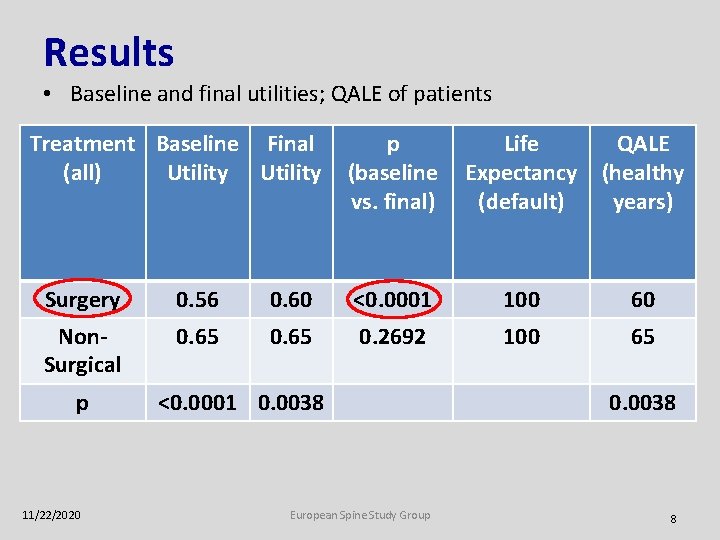
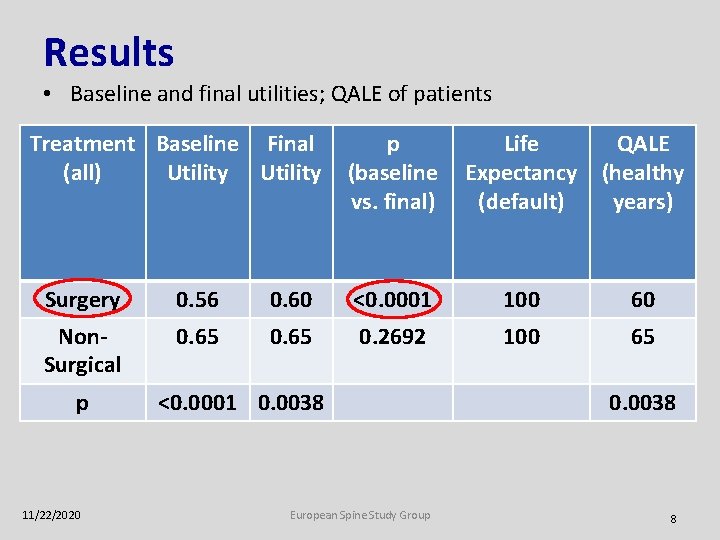
Results • Baseline and final utilities; QALE of patients Treatment Baseline Final (all) Utility p Life QALE (baseline Expectancy (healthy vs. final) (default) years) Surgery 0. 56 0. 60 <0. 0001 100 60 Non. Surgical 0. 65 0. 2692 100 65 p 11/22/2020 <0. 0001 0. 0038 European Spine Study Group 0. 0038 8

Conclusions • No single best treatment • Conservative treatment – Higher QALE (up to 6%) • Secondary to higher baseline QALE • Surgical treatment – Significantly higher increase in QALE – Chances of improvement at first year significantly better than non-surgical 11/22/2020 European Spine Study Group 9
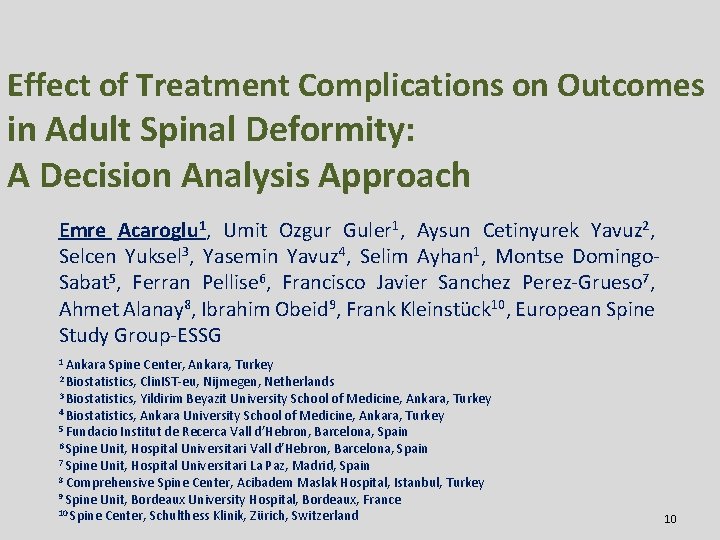
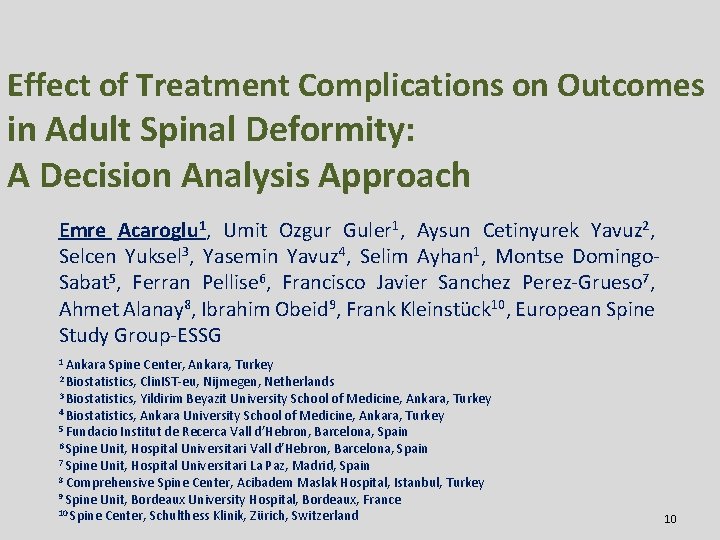
Effect of Treatment Complications on Outcomes in Adult Spinal Deformity: A Decision Analysis Approach Emre Acaroglu 1, Umit Ozgur Guler 1, Aysun Cetinyurek Yavuz 2, Selcen Yuksel 3, Yasemin Yavuz 4, Selim Ayhan 1, Montse Domingo. Sabat 5, Ferran Pellise 6, Francisco Javier Sanchez Perez-Grueso 7, Ahmet Alanay 8, Ibrahim Obeid 9, Frank Kleinstück 10, European Spine Study Group-ESSG 1 Ankara Spine Center, Ankara, Turkey 2 Biostatistics, Clin. IST-eu, Nijmegen, Netherlands 3 Biostatistics, Yildirim Beyazit University School of Medicine, Ankara, Turkey 4 Biostatistics, Ankara University School of Medicine, Ankara, Turkey 5 Fundacio Institut de Recerca Vall d’Hebron, Barcelona, Spain 6 Spine Unit, Hospital Universitari Vall d’Hebron, Barcelona, Spain 7 Spine Unit, Hospital Universitari La Paz, Madrid, Spain 8 Comprehensive Spine Center, Acibadem Maslak Hospital, Istanbul, Turkey 9 Spine Unit, Bordeaux University Hospital, Bordeaux, France 10 Spine Center, Schulthess Klinik, Zürich, Switzerland 10
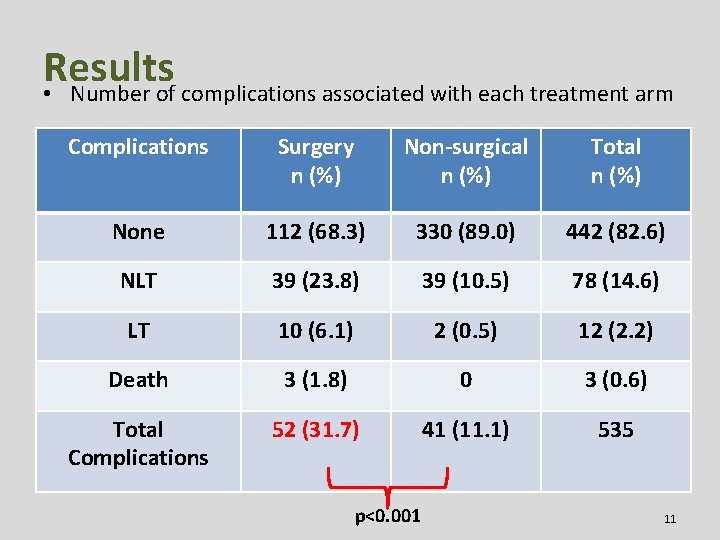
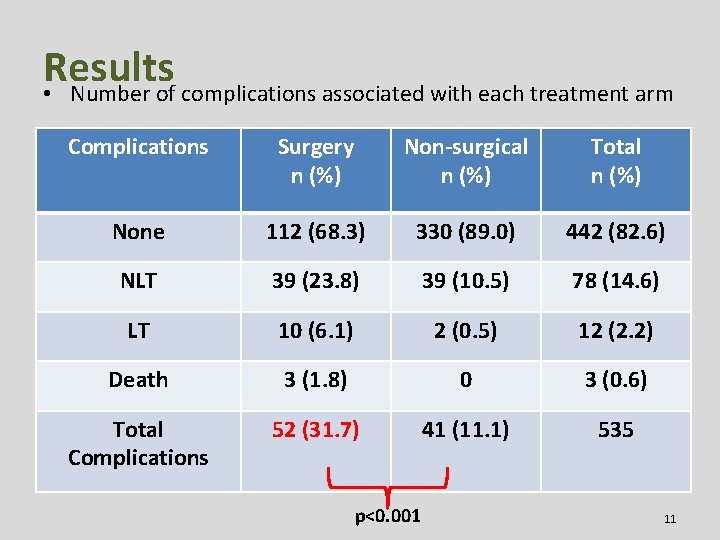
Results • Number of complications associated with each treatment arm Complications Surgery n (%) Non-surgical n (%) Total n (%) None 112 (68. 3) 330 (89. 0) 442 (82. 6) NLT 39 (23. 8) 39 (10. 5) 78 (14. 6) LT 10 (6. 1) 2 (0. 5) 12 (2. 2) Death 3 (1. 8) 0 3 (0. 6) Total Complications 52 (31. 7) 41 (11. 1) 535 p<0. 001 11
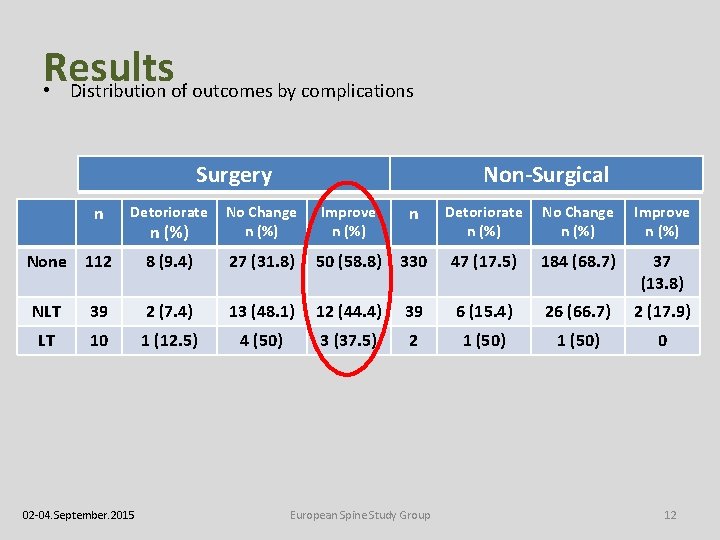
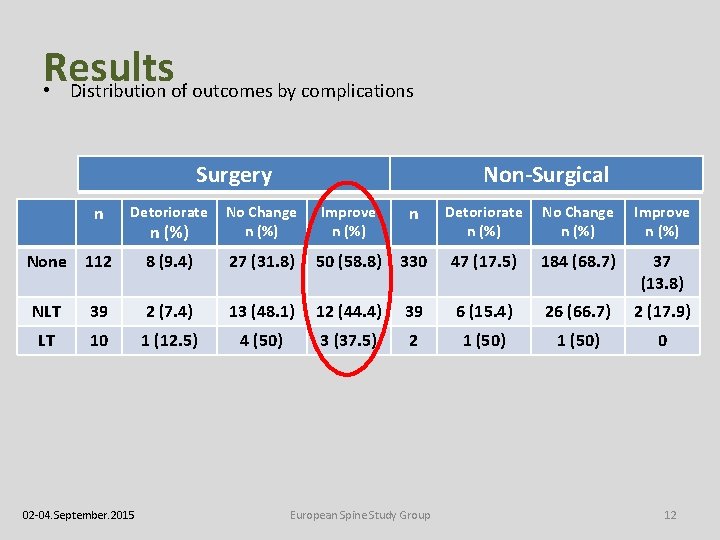
Results • Distribution of outcomes by complications Surgery Non-Surgical n Detoriorate n (%) No Change n (%) Improve n (%) None 112 8 (9. 4) 27 (31. 8) 50 (58. 8) 330 47 (17. 5) 184 (68. 7) 37 (13. 8) NLT 39 2 (7. 4) 13 (48. 1) 12 (44. 4) 39 6 (15. 4) 26 (66. 7) 2 (17. 9) LT 10 1 (12. 5) 4 (50) 3 (37. 5) 2 1 (50) 0 02 -04. September. 2015 European Spine Study Group 12
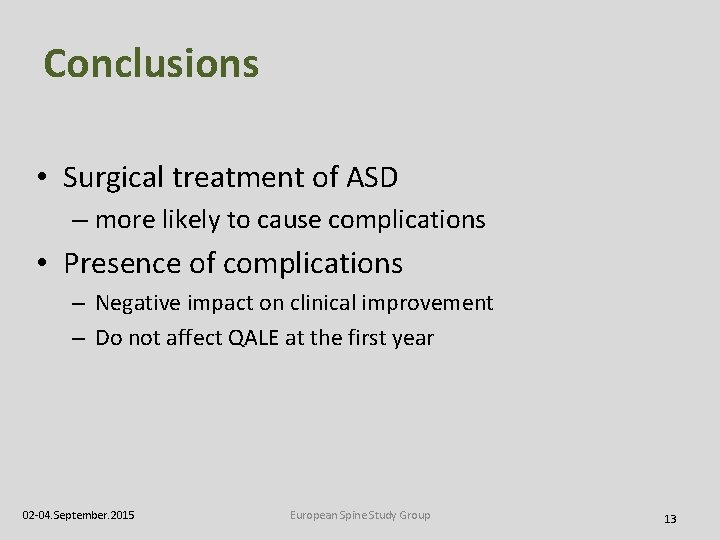
Conclusions • Surgical treatment of ASD – more likely to cause complications • Presence of complications – Negative impact on clinical improvement – Do not affect QALE at the first year 02 -04. September. 2015 European Spine Study Group 13
Impact of Resolved Early Major Complications on Two-Year Outcome Following Adult Spine Deformity Surgery Núñez S, Pellisé F, Vila A, Domingo M, Haddad S, Sánchez Pérez. Grueso F, Acaroglu E, Alanay A, Obeid I, Kleinstück F European Spine Study Group
Aim • To investigate the impact of early major complications, considered to be resolved at 6 months, on PROMs and on the likeness of reaching MCID two-years after adult deformity surgery.
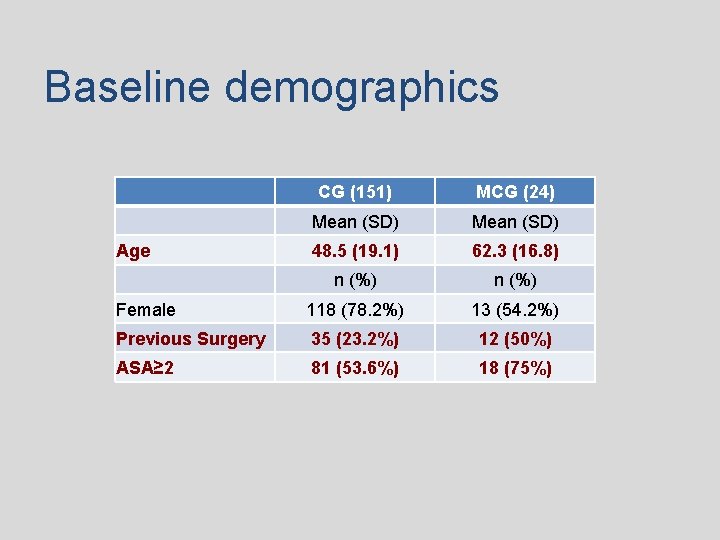
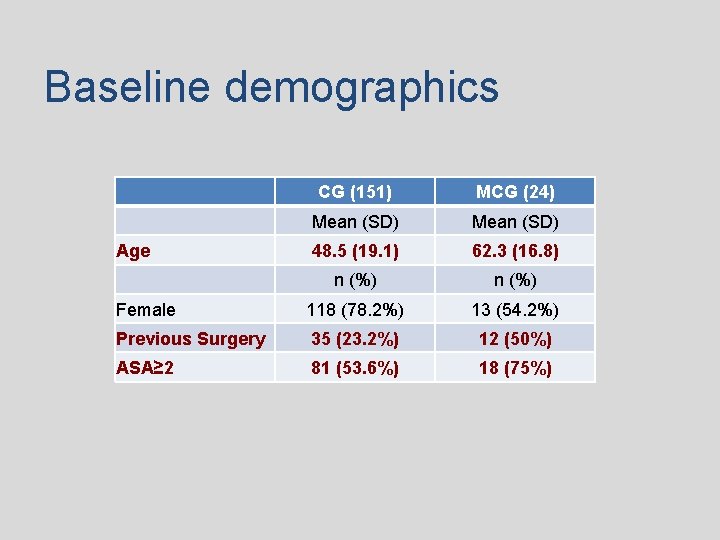
Baseline demographics CG (151) MCG (24) Mean (SD) Age 48. 5 (19. 1) 62. 3 (16. 8) n (%) Female 118 (78. 2%) 13 (54. 2%) Previous Surgery 35 (23. 2%) 12 (50%) ASA≥ 2 81 (53. 6%) 18 (75%)
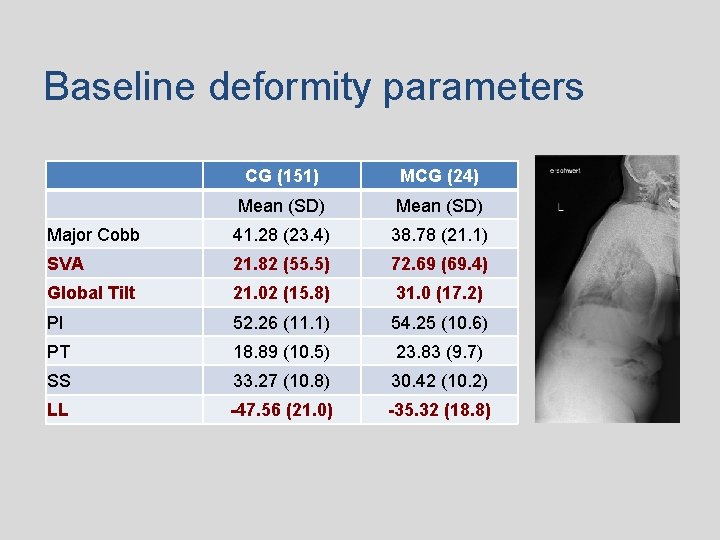
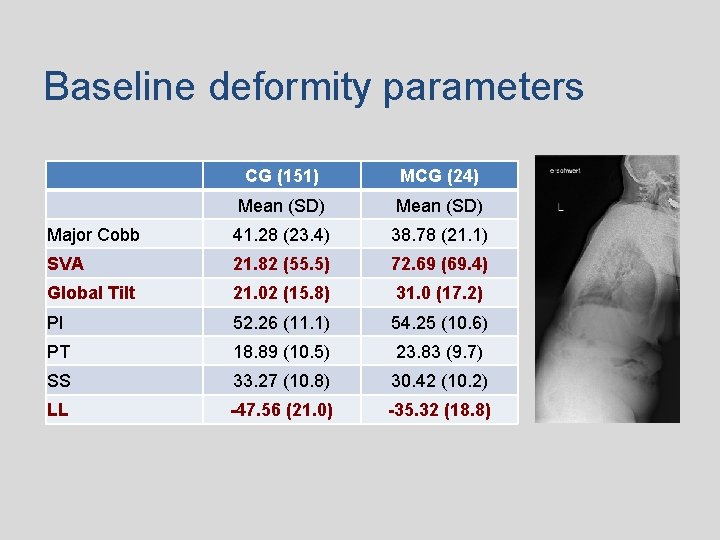
Baseline deformity parameters CG (151) MCG (24) Mean (SD) Major Cobb 41. 28 (23. 4) 38. 78 (21. 1) SVA 21. 82 (55. 5) 72. 69 (69. 4) Global Tilt 21. 02 (15. 8) 31. 0 (17. 2) PI 52. 26 (11. 1) 54. 25 (10. 6) PT 18. 89 (10. 5) 23. 83 (9. 7) SS 33. 27 (10. 8) 30. 42 (10. 2) LL -47. 56 (21. 0) -35. 32 (18. 8)
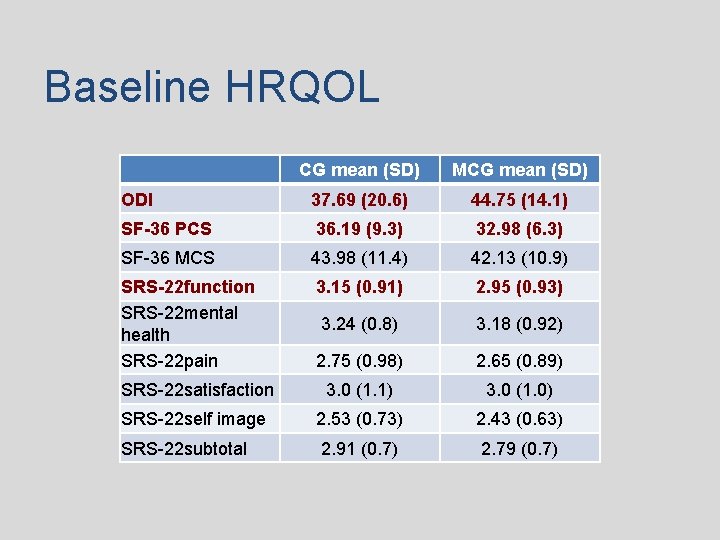
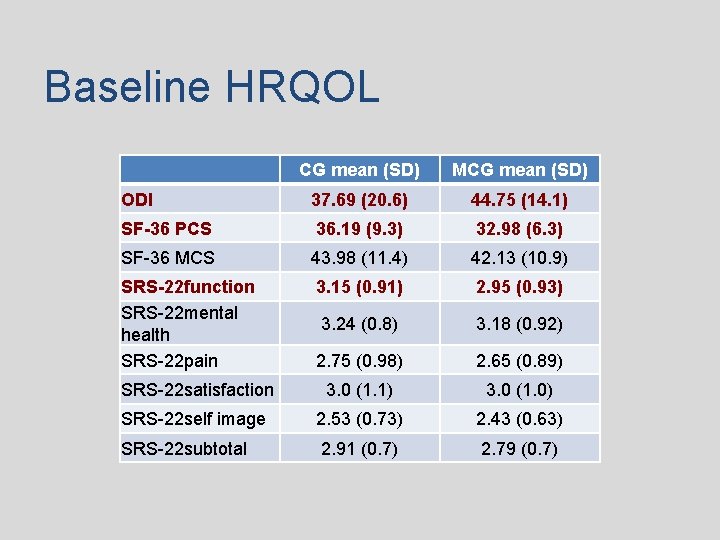
Baseline HRQOL CG mean (SD) MCG mean (SD) ODI 37. 69 (20. 6) 44. 75 (14. 1) SF-36 PCS 36. 19 (9. 3) 32. 98 (6. 3) SF-36 MCS 43. 98 (11. 4) 42. 13 (10. 9) SRS-22 function SRS-22 mental health SRS-22 pain 3. 15 (0. 91) 2. 95 (0. 93) 3. 24 (0. 8) 3. 18 (0. 92) 2. 75 (0. 98) 2. 65 (0. 89) SRS-22 satisfaction 3. 0 (1. 1) 3. 0 (1. 0) SRS-22 self image 2. 53 (0. 73) 2. 43 (0. 63) SRS-22 subtotal 2. 91 (0. 7) 2. 79 (0. 7)
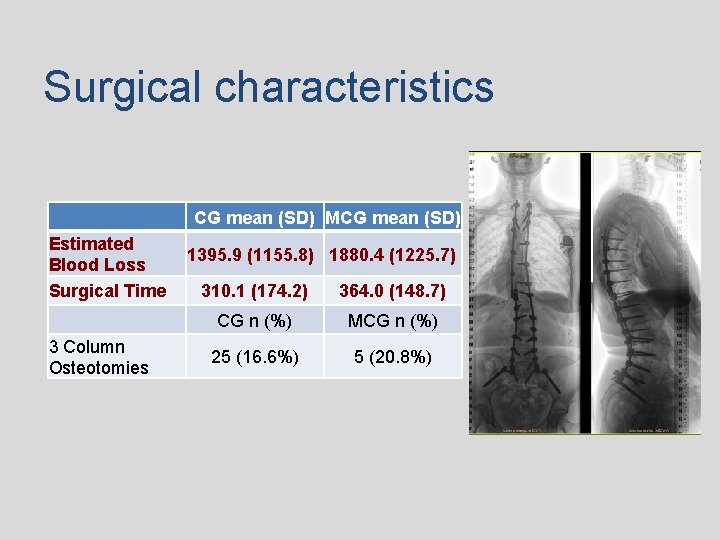
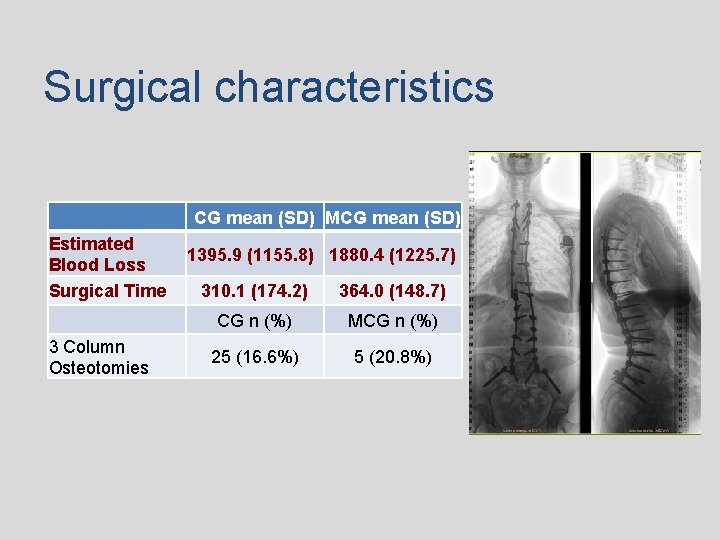
Surgical characteristics Estimated Blood Loss Surgical Time 3 Column Osteotomies CG mean (SD) MCG mean (SD) 1395. 9 (1155. 8) 1880. 4 (1225. 7) 310. 1 (174. 2) 364. 0 (148. 7) CG n (%) MCG n (%) 25 (16. 6%) 5 (20. 8%)
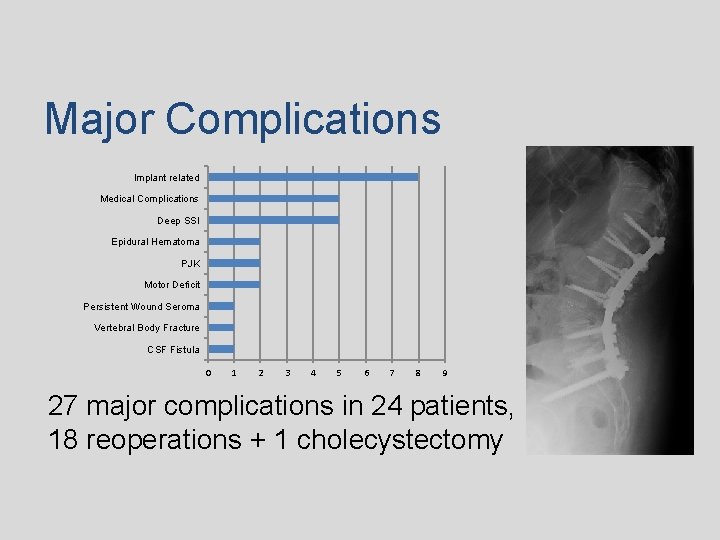
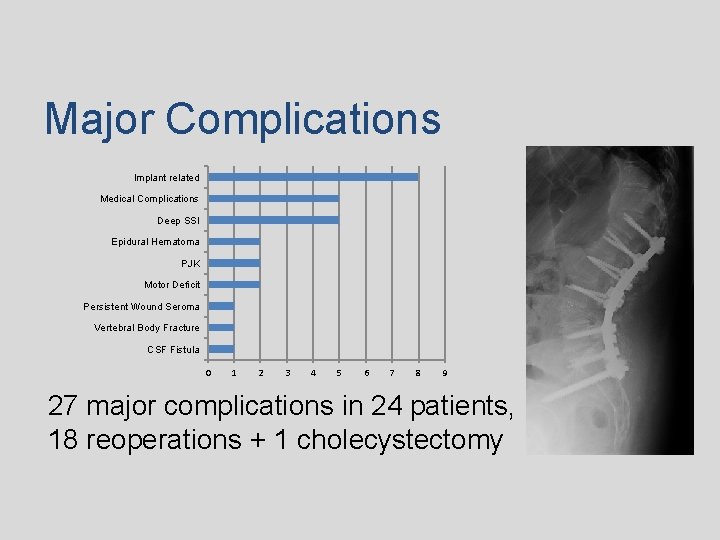
Major Complications Implant related Medical Complications Deep SSI Epidural Hematoma PJK Motor Deficit Persistent Wound Seroma Vertebral Body Fracture CSF Fistula 0 1 2 3 4 5 6 7 8 9 27 major complications in 24 patients, 18 reoperations + 1 cholecystectomy
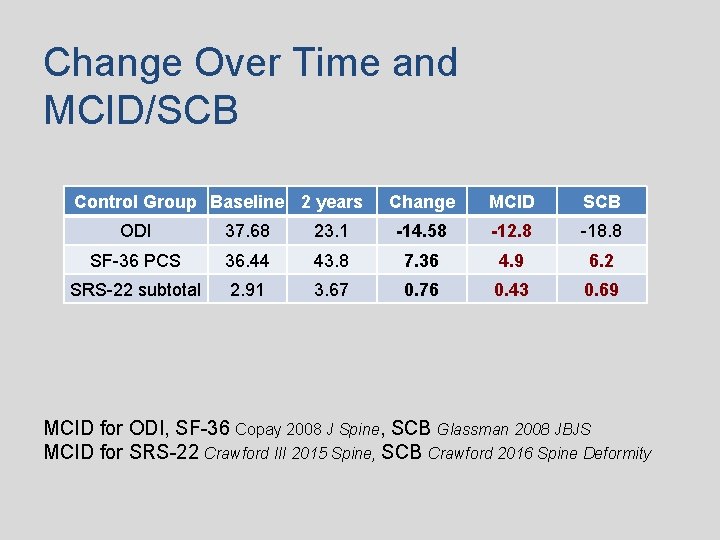
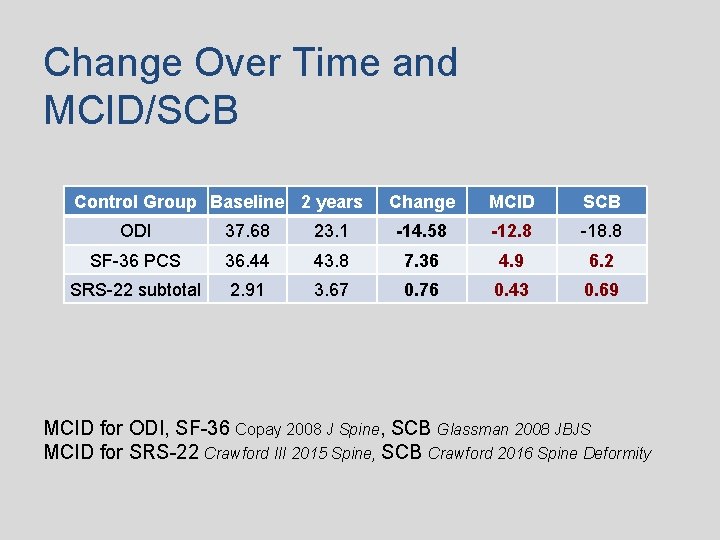
Change Over Time and MCID/SCB Control Group Baseline 2 years Change MCID SCB ODI 37. 68 23. 1 -14. 58 -12. 8 -18. 8 SF-36 PCS 36. 44 43. 8 7. 36 4. 9 6. 2 SRS-22 subtotal 2. 91 3. 67 0. 76 0. 43 0. 69 MCID for ODI, SF-36 Copay 2008 J Spine, SCB Glassman 2008 JBJS MCID for SRS-22 Crawford III 2015 Spine, SCB Crawford 2016 Spine Deformity
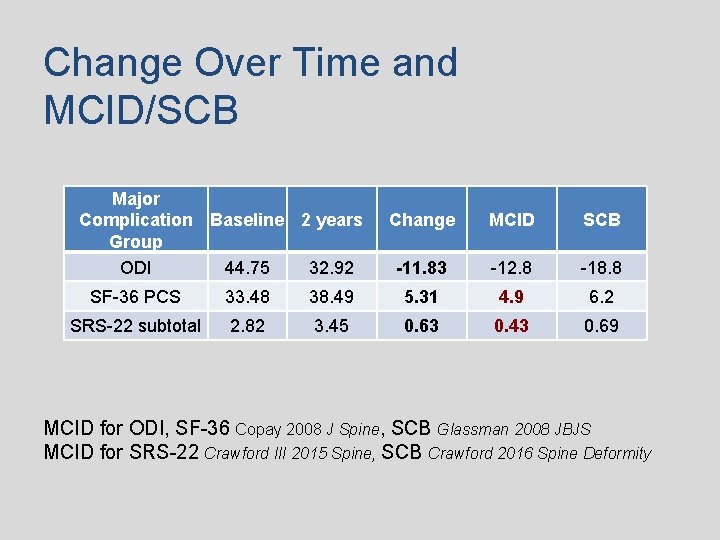
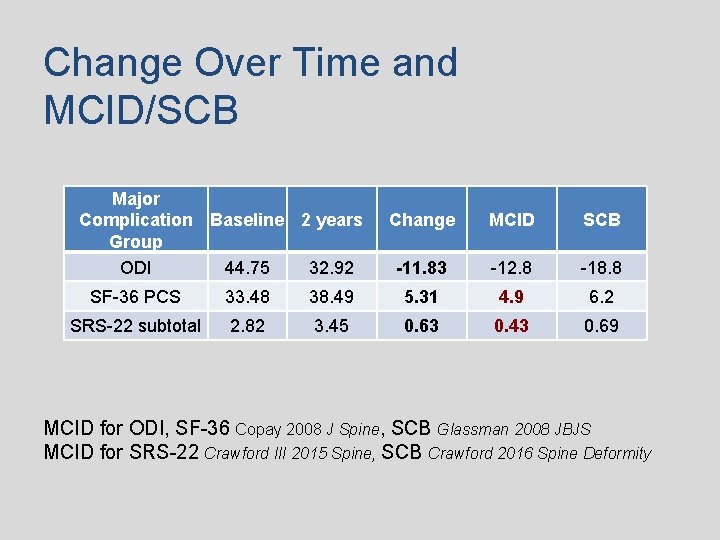
Change Over Time and MCID/SCB Major Complication Baseline 2 years Group ODI 44. 75 32. 92 Change MCID SCB -11. 83 -12. 8 -18. 8 SF-36 PCS 33. 48 38. 49 5. 31 4. 9 6. 2 SRS-22 subtotal 2. 82 3. 45 0. 63 0. 43 0. 69 MCID for ODI, SF-36 Copay 2008 J Spine, SCB Glassman 2008 JBJS MCID for SRS-22 Crawford III 2015 Spine, SCB Crawford 2016 Spine Deformity

Conclusions • Patients with major complications; – If resolved six months after surgery, • achieved a significant improvement reaching MCID values for SF-36 and SRS 22 at two years.
A score to predict/prevent mechanical complications 24
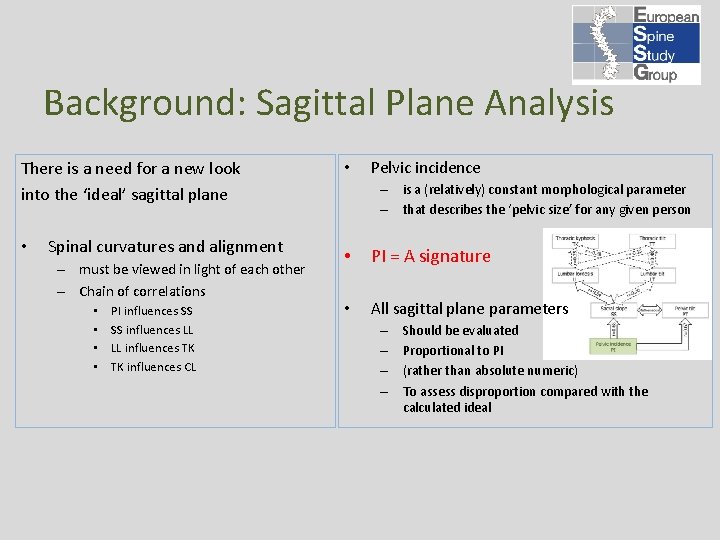
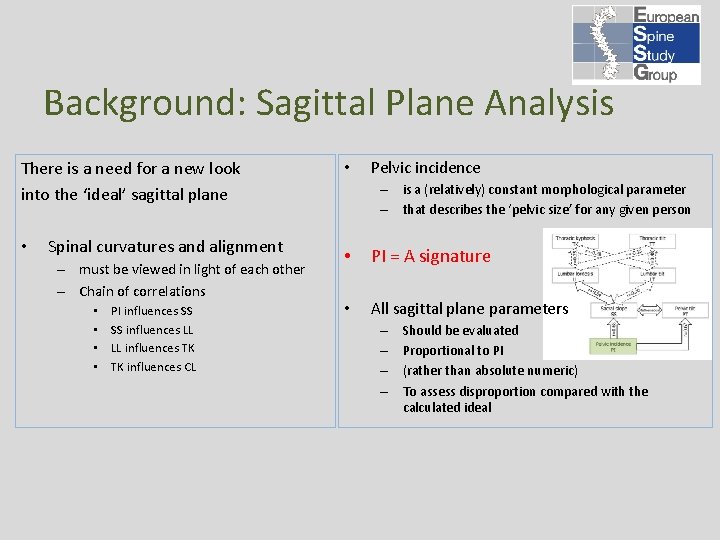
Background: Sagittal Plane Analysis There is a need for a new look into the ‘ideal’ sagittal plane • Spinal curvatures and alignment – must be viewed in light of each other – Chain of correlations • • PI influences SS SS influences LL LL influences TK TK influences CL • Pelvic incidence – is a (relatively) constant morphological parameter – that describes the ‘pelvic size’ for any given person • PI = A signature • All sagittal plane parameters – – Should be evaluated Proportional to PI (rather than absolute numeric) To assess disproportion compared with the calculated ideal
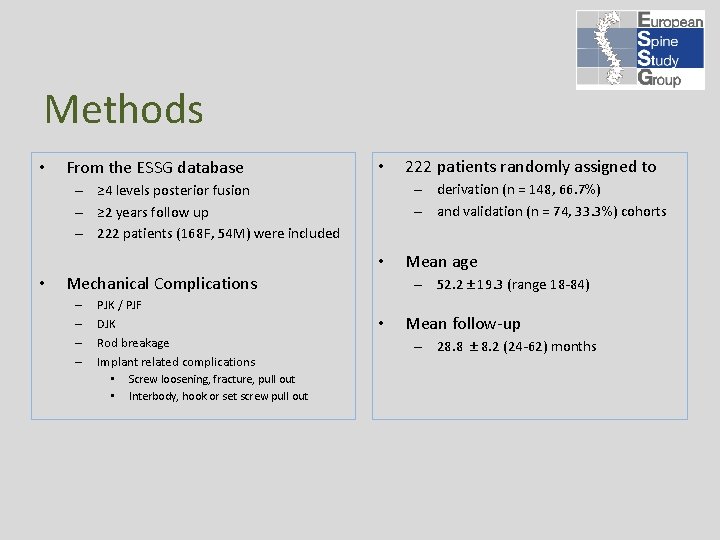
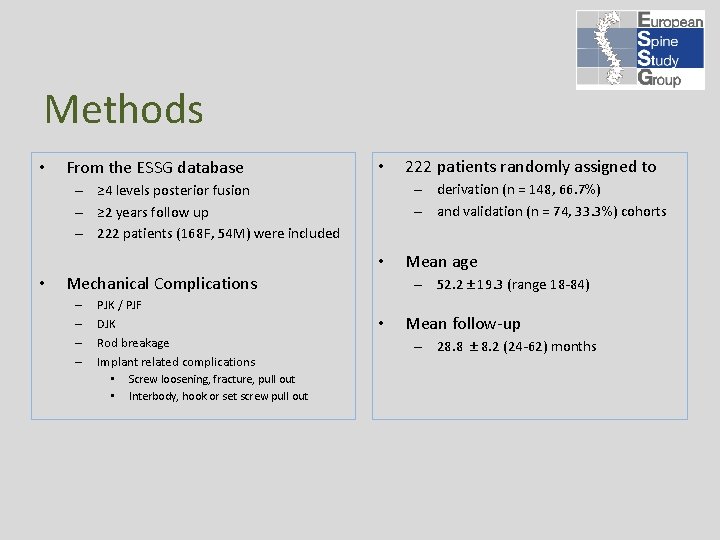
Methods • From the ESSG database • – derivation (n = 148, 66. 7%) – and validation (n = 74, 33. 3%) cohorts – ≥ 4 levels posterior fusion – ≥ 2 years follow up – 222 patients (168 F, 54 M) were included • • Mechanical Complications – – PJK / PJF DJK Rod breakage Implant related complications • Screw loosening, fracture, pull out • Interbody, hook or set screw pull out 222 patients randomly assigned to Mean age – 52. 2 ± 19. 3 (range 18 -84) • Mean follow-up – 28. 8 ± 8. 2 (24 -62) months
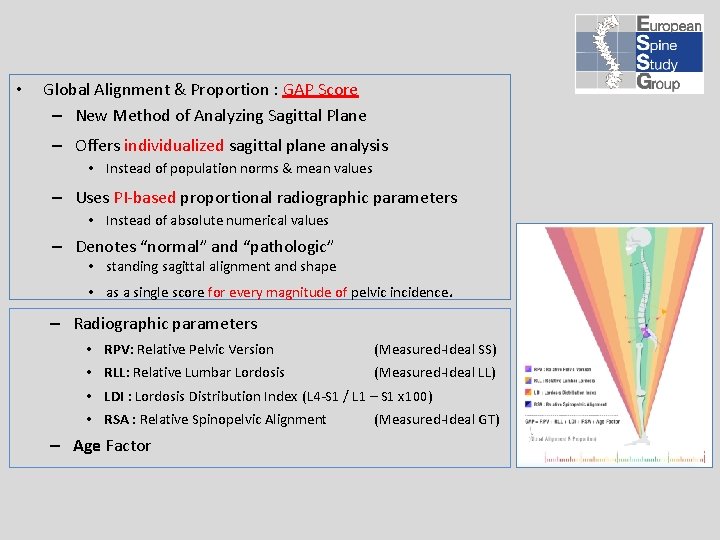
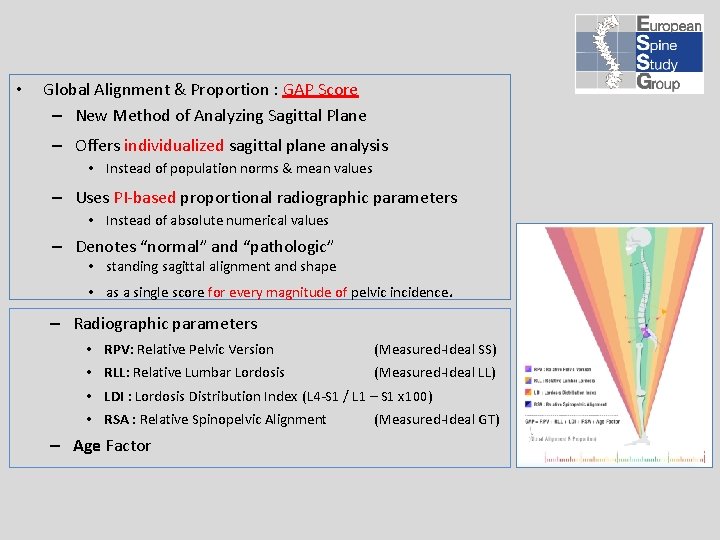
• Global Alignment & Proportion : GAP Score – New Method of Analyzing Sagittal Plane – Offers individualized sagittal plane analysis • Instead of population norms & mean values – Uses PI-based proportional radiographic parameters • Instead of absolute numerical values – Denotes “normal” and “pathologic” • standing sagittal alignment and shape • as a single score for every magnitude of pelvic incidence. – Radiographic parameters • RPV: Relative Pelvic Version (Measured-Ideal SS) • RLL: Relative Lumbar Lordosis (Measured-Ideal LL) • LDI : Lordosis Distribution Index (L 4 -S 1 / L 1 – S 1 x 100) • RSA : Relative Spinopelvic Alignment – Age Factor (Measured-Ideal GT)
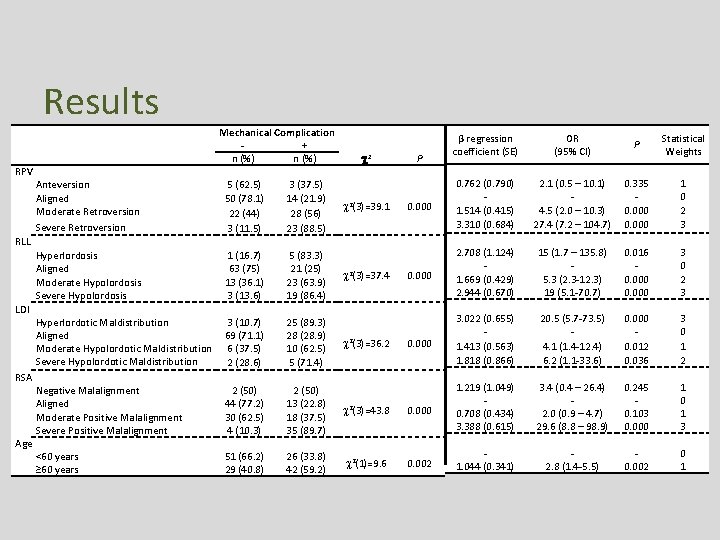
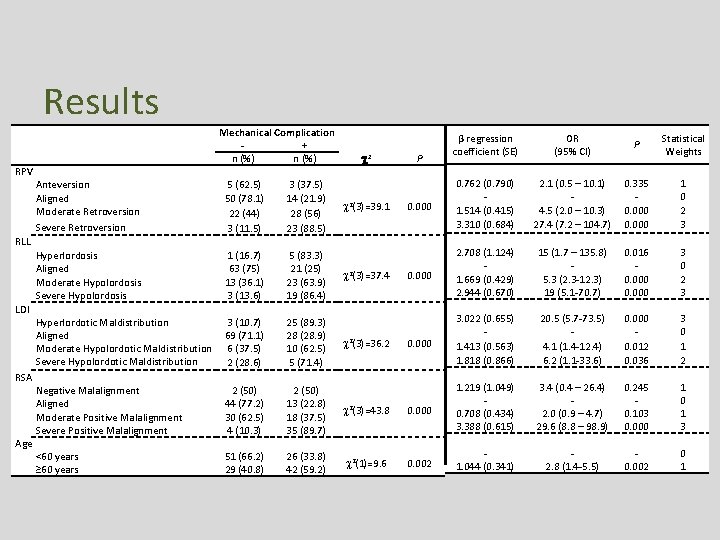
Results Risk Factors Mechanical Complication + n (%) 2 RPV Anteversion 5 (62. 5) 3 (37. 5) Aligned 50 (78. 1) 14 (21. 9) 2(3)=39. 1 Moderate Retroversion 22 (44) 28 (56) Severe Retroversion 3 (11. 5) 23 (88. 5) RLL Hyperlordosis 1 (16. 7) 5 (83. 3) Aligned 63 (75) 21 (25) 2(3)=37. 4 Moderate Hypolordosis 13 (36. 1) 23 (63. 9) Severe Hypolordosis 3 (13. 6) 19 (86. 4) LDI Hyperlordotic Maldistribution 3 (10. 7) 25 (89. 3) Aligned 69 (71. 1) 28 (28. 9) 2(3)=36. 2 Moderate Hypolordotic Maldistribution 6 (37. 5) 10 (62. 5) Severe Hypolordotic Maldistribution 2 (28. 6) 5 (71. 4) RSA Negative Malalignment 2 (50) Aligned 44 (77. 2) 13 (22. 8) 2(3)=43. 8 Moderate Positive Malalignment 30 (62. 5) 18 (37. 5) Severe Positive Malalignment 4 (10. 3) 35 (89. 7) Age <60 years 51 (66. 2) 26 (33. 8) 2(1)=9. 6 ≥ 60 years 29 (40. 8) 42 (59. 2) P 0. 000 0. 002 β regression coefficient (SE) OR (95% CI) P Statistical Weights 0. 762 (0. 790) 1. 514 (0. 415) 3. 310 (0. 684) 2. 708 (1. 124) 1. 669 (0. 429) 2. 944 (0. 670) 3. 022 (0. 655) 1. 413 (0. 563) 1. 818 (0. 866) 1. 219 (1. 049) 0. 708 (0. 434) 3. 388 (0. 615) 1. 044 (0. 341) 2. 1 (0. 5 – 10. 1) 4. 5 (2. 0 – 10. 3) 27. 4 (7. 2 – 104. 7) 15 (1. 7 – 135. 8) 5. 3 (2. 3 -12. 3) 19 (5. 1 -70. 7) 20. 5 (5. 7 -73. 5) 4. 1 (1. 4 -12. 4) 6. 2 (1. 1 -33. 6) 3. 4 (0. 4 – 26. 4) 2. 0 (0. 9 – 4. 7) 29. 6 (8. 8 – 98. 9) 2. 8 (1. 4 -5. 5) 0. 335 0. 000 0. 016 0. 000 0. 012 0. 036 0. 245 0. 103 0. 000 0. 002 1 0 2 3 3 0 1 2 1 0 1 3 0 1
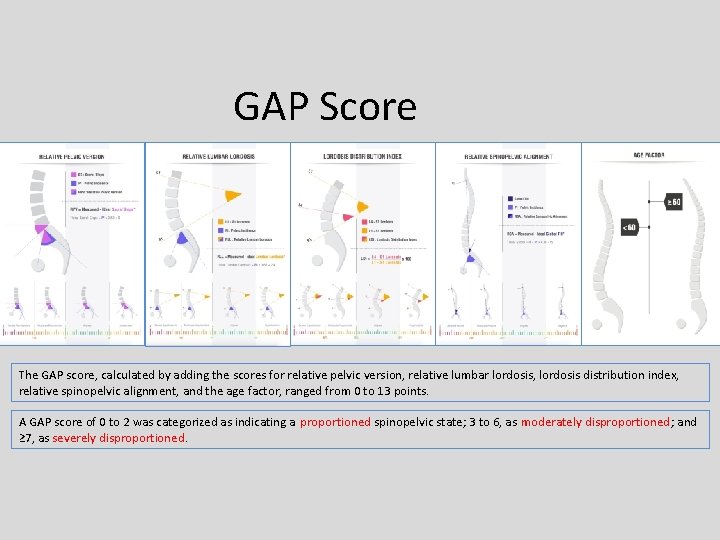
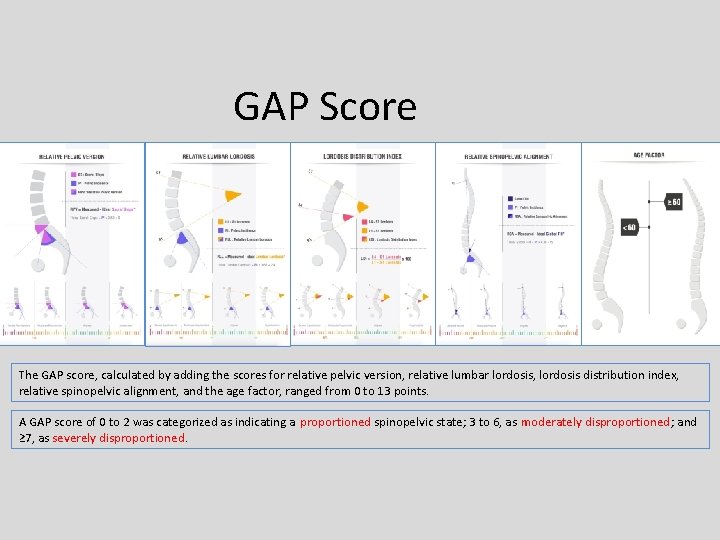
GAP Score The GAP score, calculated by adding the scores for relative pelvic version, relative lumbar lordosis, lordosis distribution index, relative spinopelvic alignment, and the age factor, ranged from 0 to 13 points. A GAP score of 0 to 2 was categorized as indicating a proportioned spinopelvic state; 3 to 6, as moderately disproportioned; and ≥ 7, as severely disproportioned.

GAP SCORE (Global Alignment and Proportion) PARAMETERS SCORING Relative Pelvic Version ( RPV = Measured - Ideal Sacral Slope * ) Severe Retroversion Moderate Retroversion -15 o RPV Subgroups Score Anteversion Aligned -7 o +5 o Moderate Hypolordosis -25 o Aligned Hyperlordosis Severe Hypolordotic 40% Aligned 50% Moderate Positive < -25 : -25 – -14. 1 : -14 – 11 : > 11 : Severe Hypolordosis. . . . Moderate Hypolordosis. . . . Aligned. . . . Hyperlordosis. . . Proportioned 3 2 0 3 Total Score : 3 - 6 Hyperlordotic < 40 % : 40 – 49 % : 50 – 80 % : > 80 % : Severe Hypolordotic Maldistribution. . . . Moderate Hypolordotic Maldistribution. . Aligned. . . . Hyperlordotic Maldistribution. . . . . 2 1 0 3 80% Aligned + 10 o +18 o Total Score : 0 – 2 LDI Subgroups Age Factor RSA Subgroups Negative -7 o > 18 : 18 – 10. 1 : 10 – -7 : < -7 : Severe Positive Malalignment……………. Moderate Positive Malalignment………. . Aligned……………. . . . . Negative Malalignment. . . . 3 1 0 1 † Ideal Global Tilt = PI x 0. 48 – 15 Age Subgroups Adult Elderly 60 Moderately Disproportioned Total Score 7 Relative Spinopelvic Alignment ( RSA = Measured - Ideal Global Tilt † ) Severe Positive 3 2 0 1 ✢ Ideal Lumbar Lordosis = PI x 0. 62 + 29 Lordosis Distribution Index ( LDI = L 4 -S 1 Lordosis / L 1 - S 1 Lordosis x 100 ) Moderate Hypolordotic Severe Retroversion. . . . Moderate Retroversion. . . . Aligned. . . . Anteversion. . . RLL Subgroups +11 o -14 o < -15 : -15 – -7. 1 : -7 – 5 : > 5 : * Ideal Sacral Slope = PI x 0. 59 + 9 Relative Lumbar Lordosis ( RLL = Measured - Ideal Lumbar Lordosis ✢ ) Severe Hypolordosis CATEGORIES < 60 years : ≥ 60 years : Adult…………………. . . Elderly Adult. . . ……. . . . 0 1 Severely Disproportioned The parameters column includes a scale-based view of the subgroups of each parameter using the cutoff points. The scoring column includes the statistical weights of the parameter subgroups. The categories column includes the categorization of the GAP score.
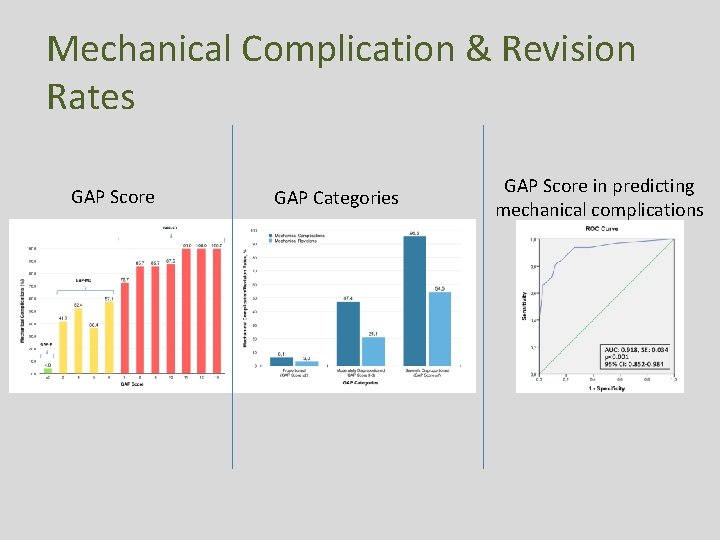
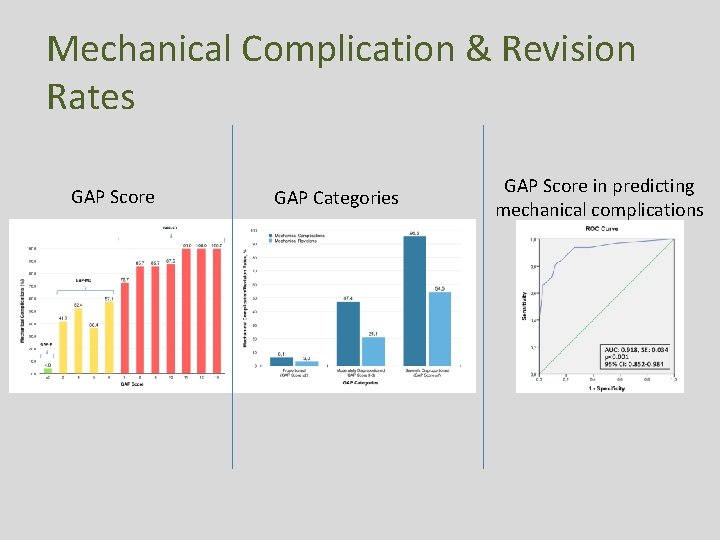
Mechanical Complication & Revision Rates GAP Score GAP Categories GAP Score in predicting mechanical complications

Conclusion • GAP score – is a new PI-based proportional method of analyzing – the individualized sagittal plane • GAP score – is an all-inclusive single score – that offers a ‘one-size fits all’ solution – for every size of pelvic incidence • Preoperative planning & setting surgical goals in the sagittal plane – on the basis of the individualized proportional indices reflected by the GAP score – may decrease the rate of mechanical complications.
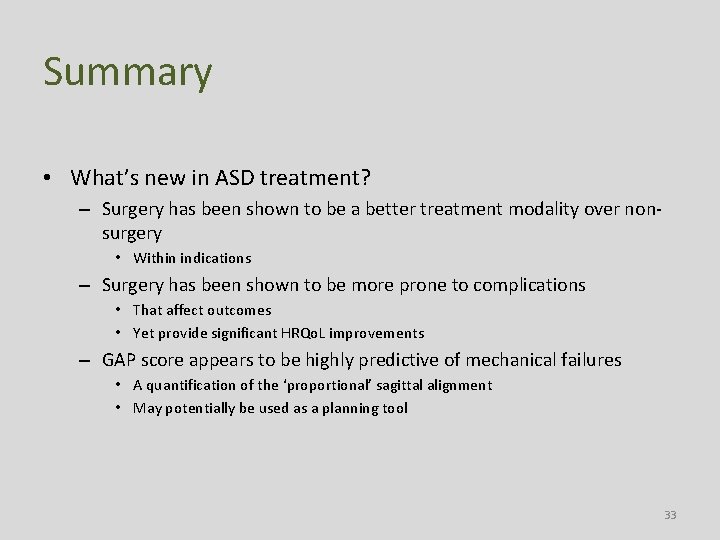
Summary • What’s new in ASD treatment? – Surgery has been shown to be a better treatment modality over nonsurgery • Within indications – Surgery has been shown to be more prone to complications • That affect outcomes • Yet provide significant HRQo. L improvements – GAP score appears to be highly predictive of mechanical failures • A quantification of the ‘proportional’ sagittal alignment • May potentially be used as a planning tool 33
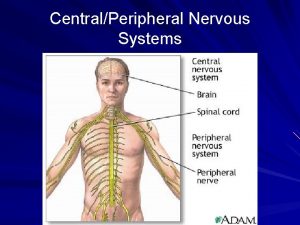
 Spinal nerves
Spinal nerves Spine meninges
Spine meninges Innervations of the brachial and lumbar enlargements
Innervations of the brachial and lumbar enlargements Spinal cord structure
Spinal cord structure Adult treatment panel iii
Adult treatment panel iii Serkan yurttutan
Serkan yurttutan Süleyman emre kocacan
Süleyman emre kocacan Türkiye güzeli gizem memiç
Türkiye güzeli gizem memiç Mehmet emre cihangir
Mehmet emre cihangir Emre erkovan
Emre erkovan Salih emre önal
Salih emre önal Ahmet emre yaprak
Ahmet emre yaprak Mehmet emre yurttutan
Mehmet emre yurttutan Dr alpagut
Dr alpagut Emre yengel
Emre yengel Emre yengel
Emre yengel Mehmet emre arı
Mehmet emre arı Prof dr emre alhan
Prof dr emre alhan Mustafa emre ilal
Mustafa emre ilal Emre uzun bilkent
Emre uzun bilkent Mehmet emre yurttutan
Mehmet emre yurttutan Emre hamurtekin
Emre hamurtekin Ali emre gezgin
Ali emre gezgin Bahaeddin eravci
Bahaeddin eravci Emre telatar
Emre telatar Netrografi
Netrografi çek örneği
çek örneği Yunus emre sarı
Yunus emre sarı Emre market landau
Emre market landau Mustafa emre ilal
Mustafa emre ilal Ie342
Ie342 Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Gun stock deformity
Gun stock deformity Kaiser wilhelm deformity
Kaiser wilhelm deformity