ADULT BOWEL INTUSSUSCEPTIONS RADIOLOGY APPEARANCE AND IDENTIFICATION OF
ADULT BOWEL INTUSSUSCEPTIONS: RADIOLOGY APPEARANCE AND IDENTIFICATION OF A CAUSATIVE LEAD POINT N. MEKKI, R. KHARRAT, S. BOURKHIS, R. BEN NACEUR, F. BEN AMARA, N. MNIF. CHARLE NICOLLE’S HOSPITAL, TUNISIA
Introduction: � Intussusception in adults is an unusual cause of bowel obstruction: � 1% of all bowel obstructions. � 5 % of all intussusceptions. � 80 -90 %: due to an underlying pathology. � The growing use of computed tomography (CT) and magnetic resonance imaging (MRI) has led to increased detection of intussusceptions as mostly unsuspected clinically, presented with non-specific abdominal pain.
Objectives : q To describe the characteristic radiologic features of intussusception according to location. q To illustrate pathologies which cause intussusceptions. q To correlate the different features with the pathologic findings.
Materials and methods : � We made a retrospective study, over 1 -year period (2011). � 6 cases of adult bowel intussusceptions: Sex ratio: 4 men/ 2 women. Age : vary from 21 to 60 years, mean age: 38 years. � Explorations: 5 patients was explored by abdominal enhanced CT examination General Electric (GE) 16 slices. One patient was explored by MRI GE 1. 5 Tesla.
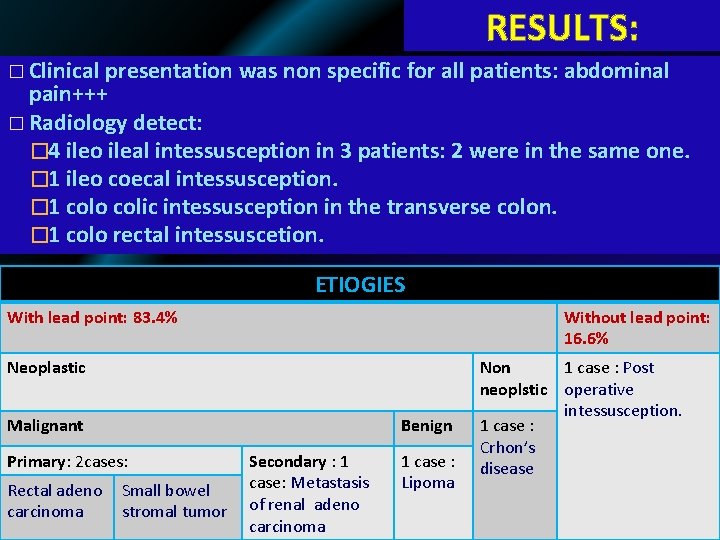
RESULTS: � Clinical presentation was non specific for all patients: abdominal pain+++ � Radiology detect: � 4 ileo ileal intessusception in 3 patients: 2 were in the same one. � 1 ileo coecal intessusception. � 1 colo colic intessusception in the transverse colon. � 1 colo rectal intessuscetion. ETIOGIES With lead point: 83. 4% Without lead point: 16. 6% Neoplastic Malignant Benign Primary: 2 cases: Rectal adeno carcinoma Small bowel stromal tumor Secondary : 1 case: Metastasis of renal adeno carcinoma 1 case : Lipoma Non 1 case : Post neoplstic operative intessusception. 1 case : Crhon’s disease
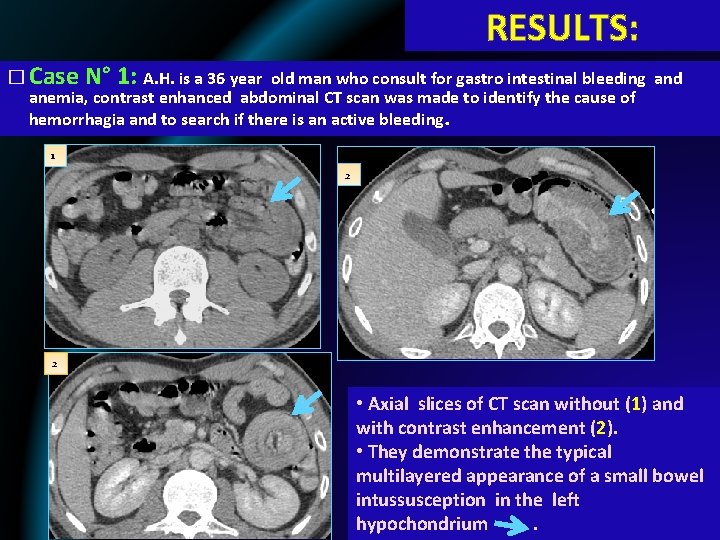
RESULTS: � Case N° 1: A. H. is a 36 year old man who consult for gastro intestinal bleeding and anemia, contrast enhanced abdominal CT scan was made to identify the cause of hemorrhagia and to search if there is an active bleeding. 1 2 2 • Axial slices of CT scan without (1) and with contrast enhancement (2). • They demonstrate the typical multilayered appearance of a small bowel intussusception in the left hypochondrium .
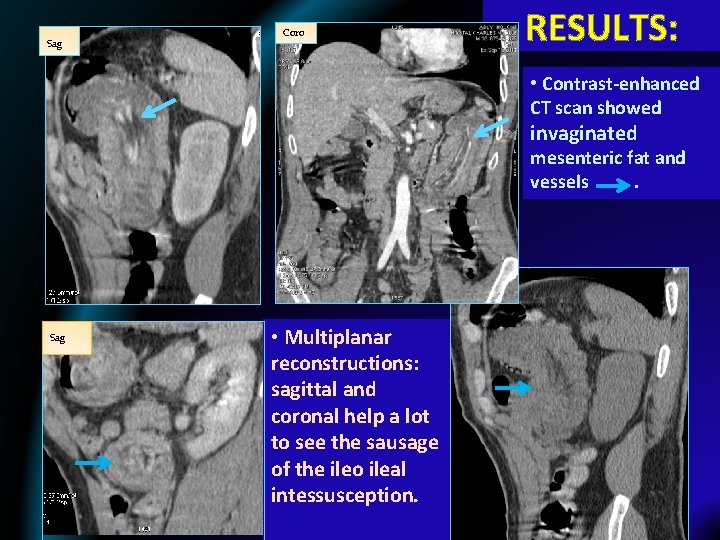
Sag RESULTS: Coro • Contrast-enhanced CT scan showed invaginated mesenteric fat and vessels . Sag Sag • Multiplanar reconstructions: sagittal and coronal help a lot to see the sausage of the ileo ileal intessusception.
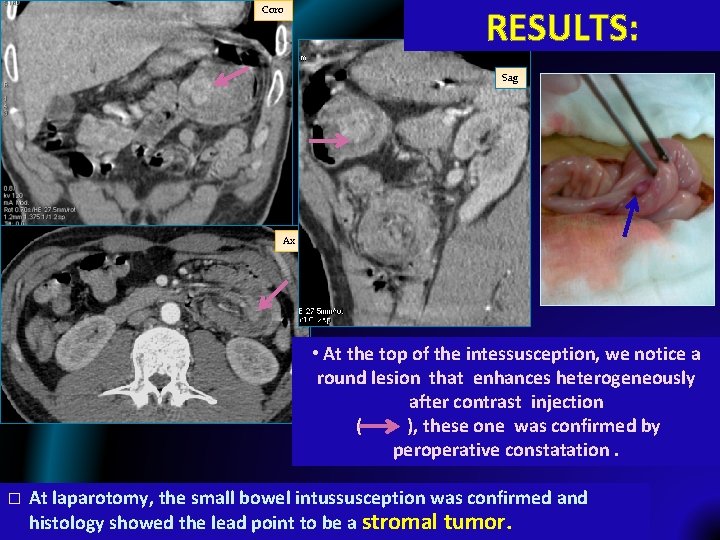
Coro RESULTS: Sag Ax • At the top of the intessusception, we notice a round lesion that enhances heterogeneously after contrast injection ( ), these one was confirmed by peroperative constatation. � At laparotomy, the small bowel intussusception was confirmed and histology showed the lead point to be a stromal tumor.
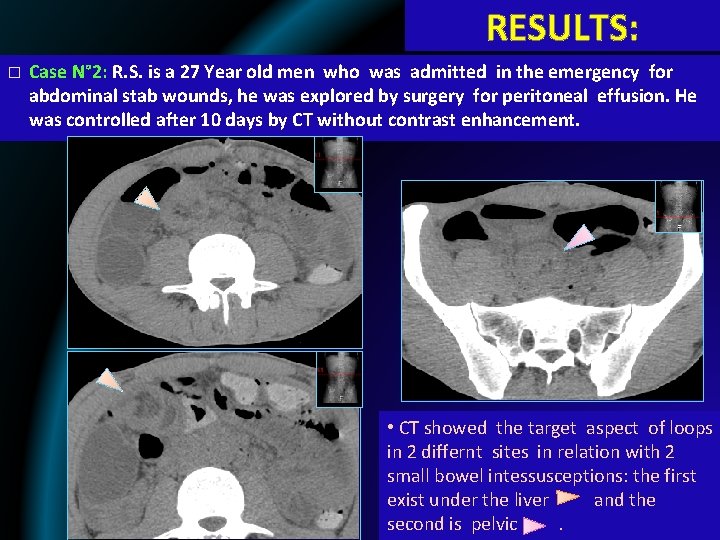
RESULTS: � Case N° 2: R. S. is a 27 Year old men who was admitted in the emergency for abdominal stab wounds, he was explored by surgery for peritoneal effusion. He was controlled after 10 days by CT without contrast enhancement. • CT showed the target aspect of loops in 2 differnt sites in relation with 2 small bowel intessusceptions: the first exist under the liver and the second is pelvic.
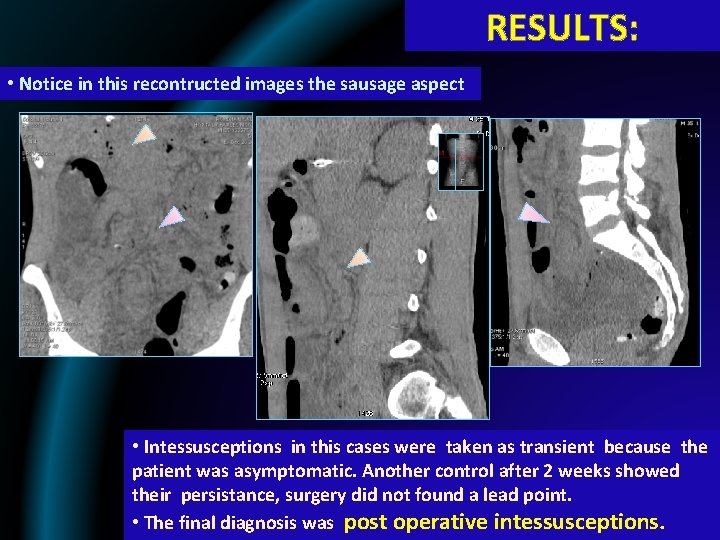
RESULTS: • Notice in this recontructed images the sausage aspect • Intessusceptions in this cases were taken as transient because the patient was asymptomatic. Another control after 2 weeks showed their persistance, surgery did not found a lead point. • The final diagnosis was post operative intessusceptions.
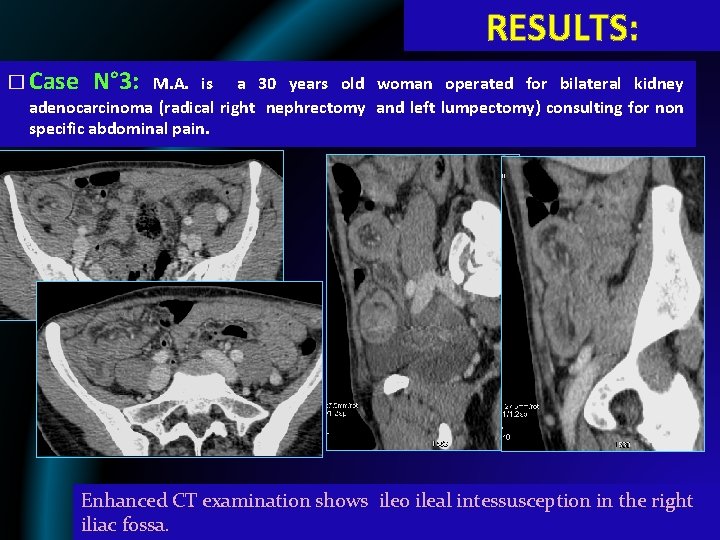
RESULTS: � Case N° 3: M. A. is a 30 years old woman operated for bilateral kidney adenocarcinoma (radical right nephrectomy and left lumpectomy) consulting for non specific abdominal pain. Enhanced CT examination shows ileo ileal intessusception in the right iliac fossa.
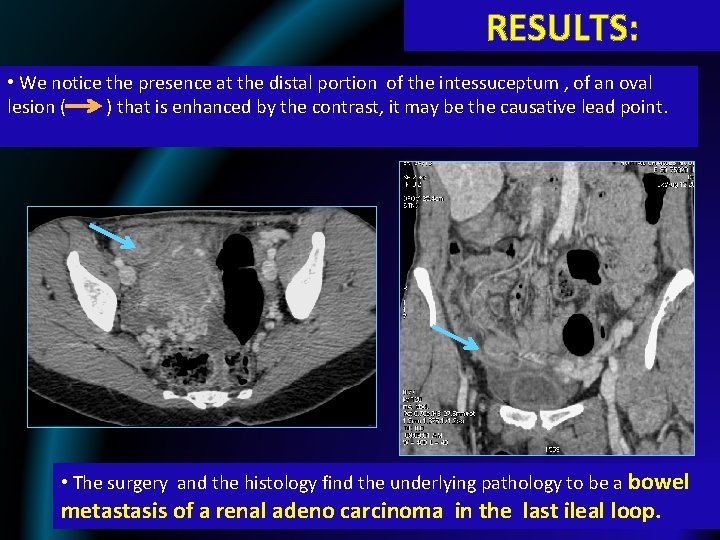
RESULTS: • We notice the presence at the distal portion of the intessuceptum , of an oval lesion ( ) that is enhanced by the contrast, it may be the causative lead point. • The surgery and the histology find the underlying pathology to be a bowel metastasis of a renal adeno carcinoma in the last ileal loop.
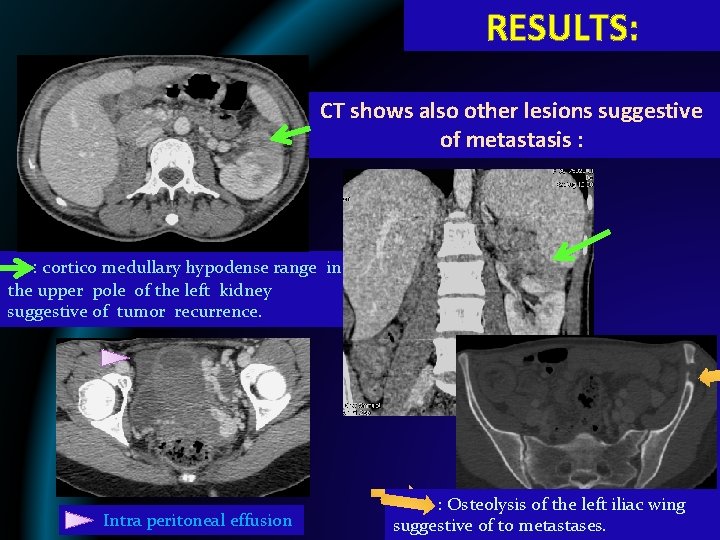
RESULTS: CT shows also other lesions suggestive of metastasis : : cortico medullary hypodense range in the upper pole of the left kidney suggestive of tumor recurrence. Intra peritoneal effusion : Osteolysis of the left iliac wing suggestive of to metastases.
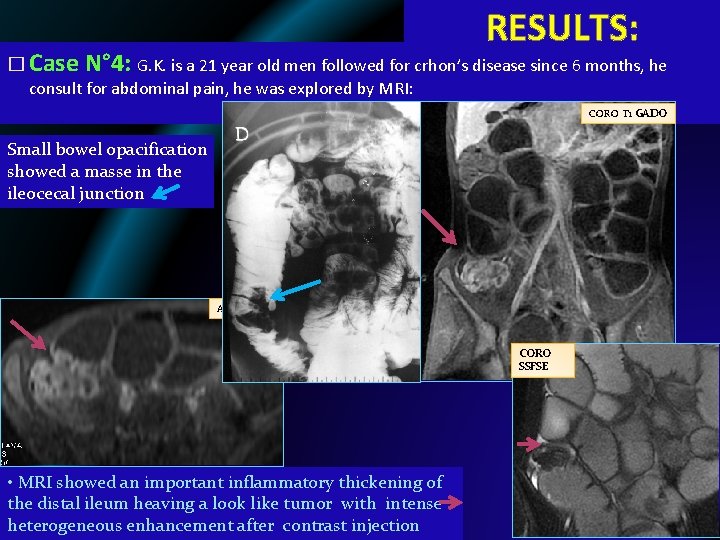
RESULTS: � Case N° 4: G. K. is a 21 year old men followed for crhon’s disease since 6 months, he consult for abdominal pain, he was explored by MRI: CORO T 1 GADO Small bowel opacification showed a masse in the ileocecal junction AX T 1 GADO CORO SSFSE • MRI showed an important inflammatory thickening of the distal ileum heaving a look like tumor with intense heterogeneous enhancement after contrast injection CORO SSFSE
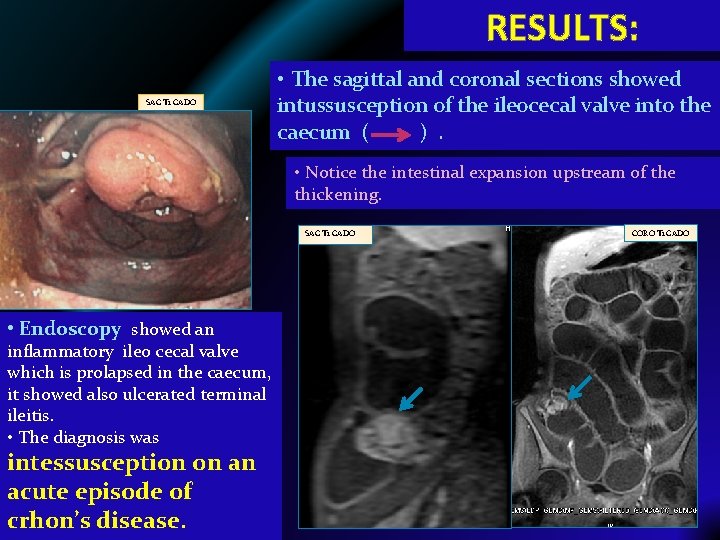
RESULTS: SAG T 1 GADO • The sagittal and coronal sections showed intussusception of the ileocecal valve into the caecum ( ). • Notice the intestinal expansion upstream of the thickening. SAG T 1 GADO • Endoscopy showed an inflammatory ileo cecal valve which is prolapsed in the caecum, it showed also ulcerated terminal ileitis. • The diagnosis was intessusception on an acute episode of crhon’s disease. CORO T 1 GADO
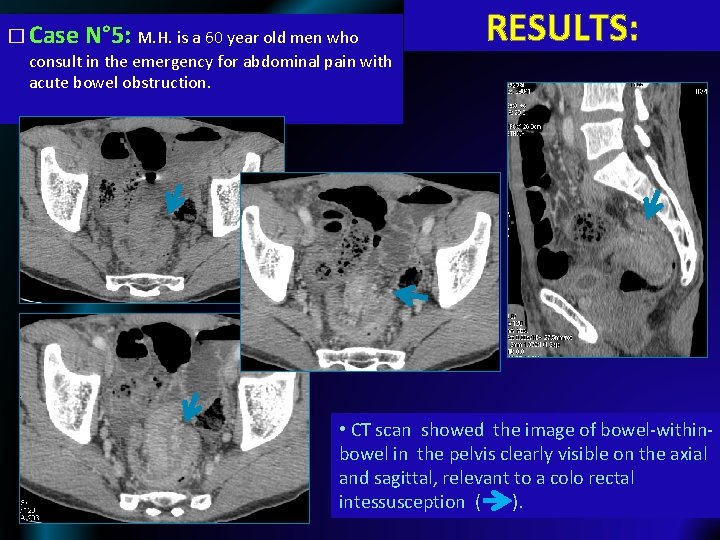
� Case N° 5: M. H. is a 60 year old men who consult in the emergency for abdominal pain with acute bowel obstruction. RESULTS: • CT scan showed the image of bowel-withinbowel in the pelvis clearly visible on the axial and sagittal, relevant to a colo rectal intessusception ( ).
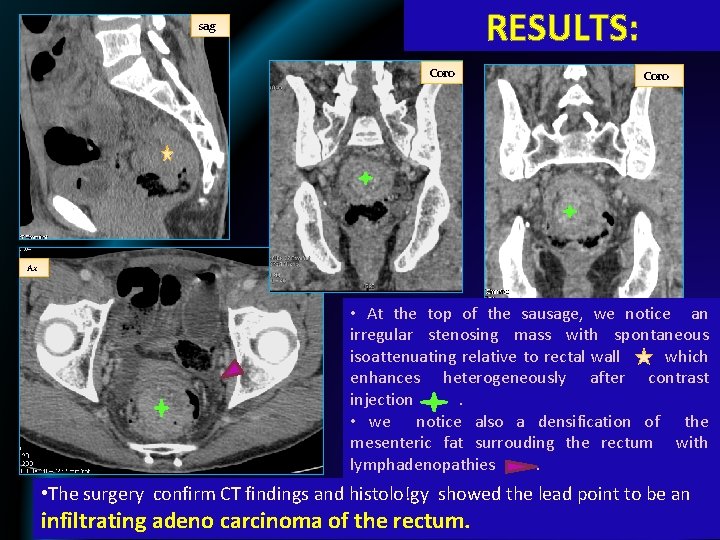
RESULTS: sag Coro Ax • At the top of the sausage, we notice an irregular stenosing mass with spontaneous isoattenuating relative to rectal wall which enhances heterogeneously after contrast injection. • we notice also a densification of the mesenteric fat surrouding the rectum with lymphadenopathies. • The surgery confirm CT findings and histolo!gy showed the lead point to be an infiltrating adeno carcinoma of the rectum.
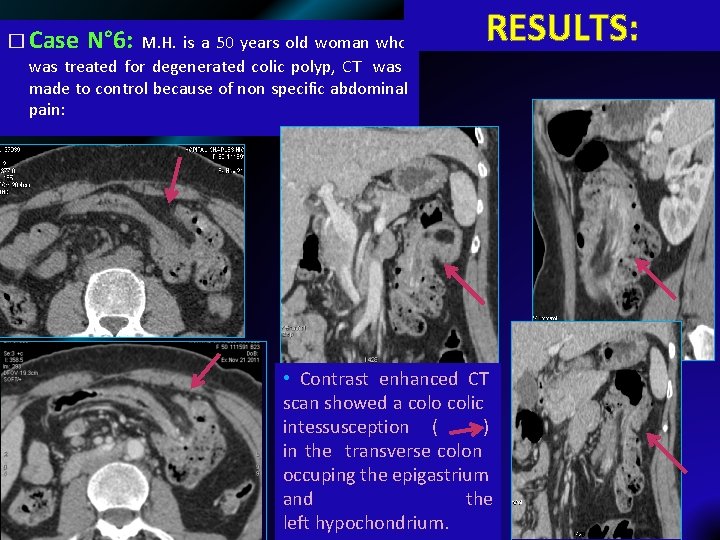
� Case N° 6: M. H. is a 50 years old woman who RESULTS: was treated for degenerated colic polyp, CT was made to control because of non specific abdominal pain: • Contrast enhanced CT scan showed a colo colic intessusception ( ) in the transverse colon occuping the epigastrium and the left hypochondrium.
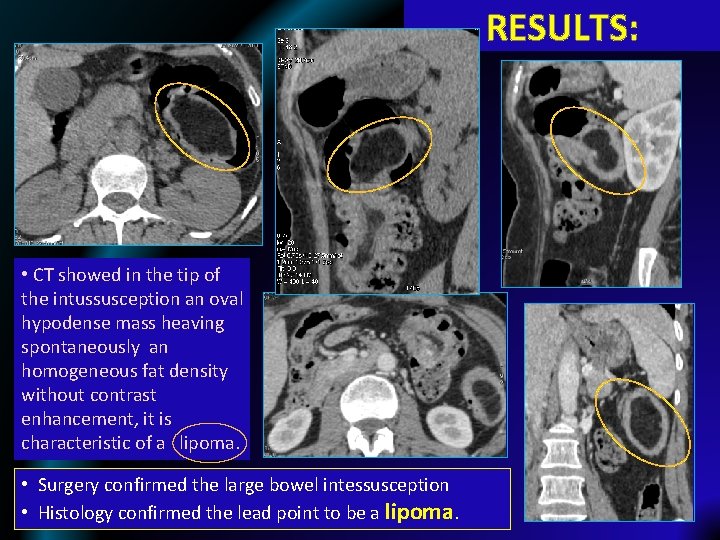
RESULTS: • CT showed in the tip of the intussusception an oval hypodense mass heaving spontaneously an homogeneous fat density without contrast enhancement, it is characteristic of a lipoma. • Surgery confirmed the large bowel intessusception • Histology confirmed the lead point to be a lipoma.
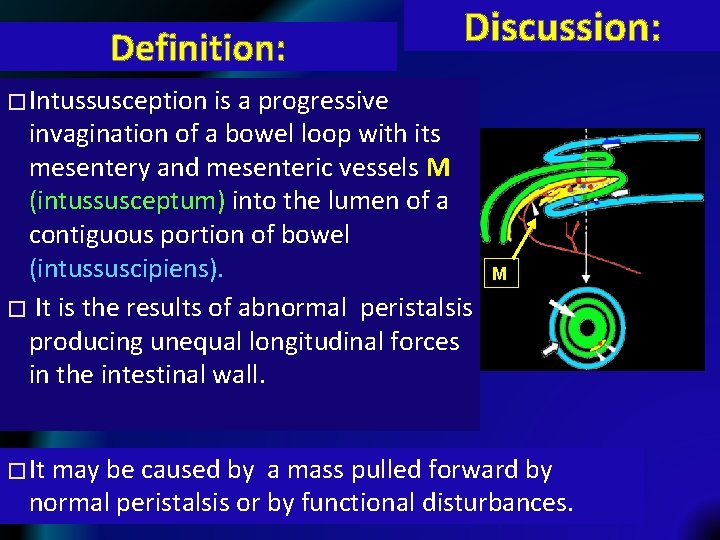
Definition: Discussion: � Intussusception is a progressive invagination of a bowel loop with its mesentery and mesenteric vessels M (intussusceptum) into the lumen of a contiguous portion of bowel (intussuscipiens). � It is the results of abnormal peristalsis producing unequal longitudinal forces in the intestinal wall. � It M may be caused by a mass pulled forward by normal peristalsis or by functional disturbances.
Discussion: � Symptoms are often chronic: several weeks to months, may be occasionally acute, it may be related to the lead point. � Unlike children, the most common symptoms of intussusception in adult are non specific: �Abdominal pain, nausea and vomiting +++ �Less frequently: constipation, fever, weight loss, diarrhea; �It is often asymptomatic, especially in chronic invaginations or without leadpoint. � Physical examination is often unremarkable, sometimes note palpable mass.
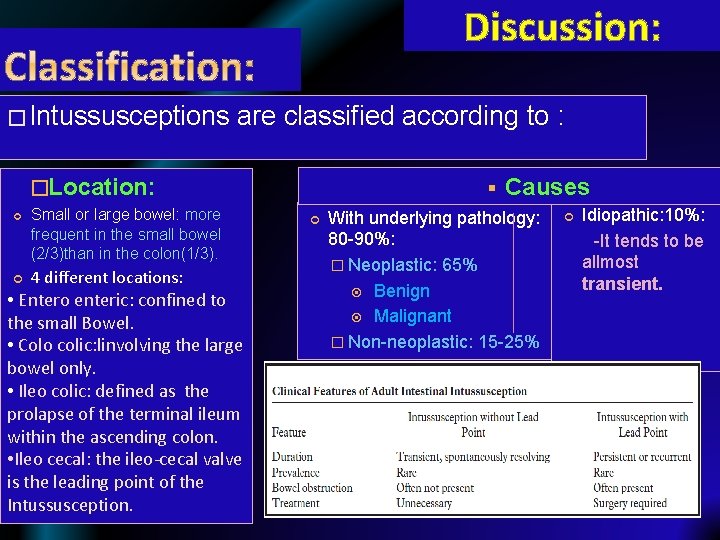
Discussion: � Intussusceptions are classified according to : �Location: Small or large bowel: more frequent in the small bowel (2/3)than in the colon(1/3). 4 different locations: • Entero enteric: confined to the small Bowel. • Colo colic: linvolving the large bowel only. • Ileo colic: defined as the prolapse of the terminal ileum within the ascending colon. • Ileo cecal: the ileo-cecal valve is the leading point of the Intussusception. § Causes With underlying pathology: 80 -90%: � Neoplastic: 65% Benign Malignant � Non-neoplastic: 15 -25% Idiopathic: 10%: -It tends to be allmost transient.
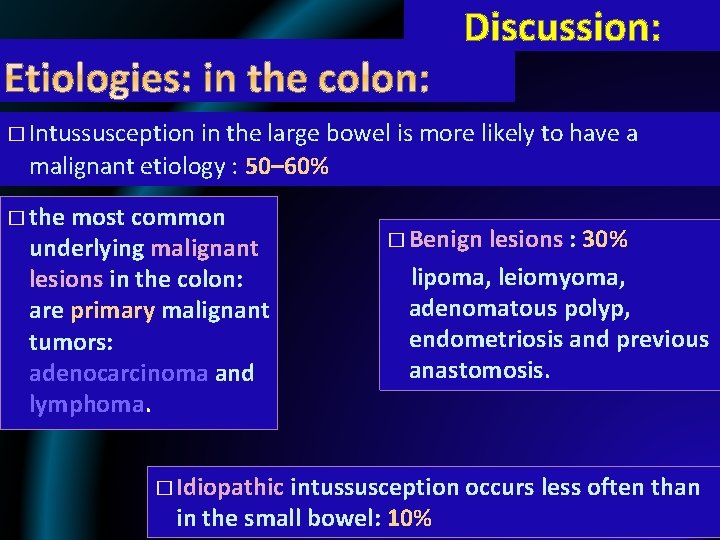
Discussion: � Intussusception in the large bowel is more likely to have a malignant etiology : 50– 60% � the most common underlying malignant lesions in the colon: are primary malignant tumors: adenocarcinoma and lymphoma. � Benign lesions : 30% lipoma, leiomyoma, adenomatous polyp, endometriosis and previous anastomosis. � Idiopathic intussusception occurs less often than in the small bowel: 10%
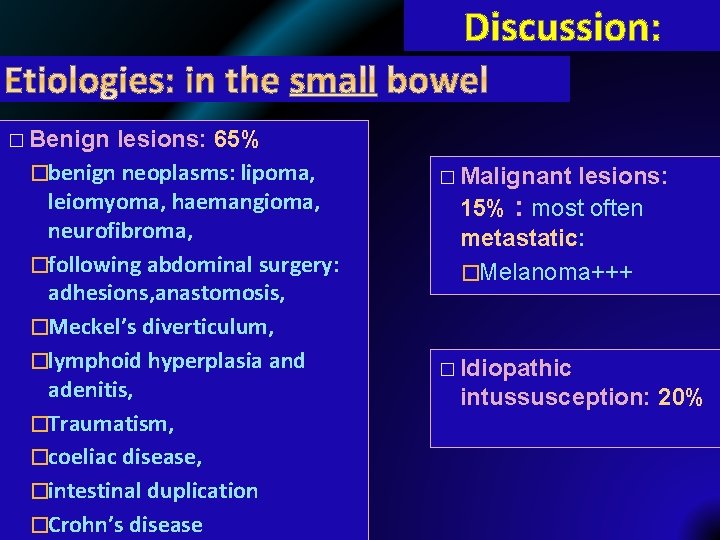
Discussion: � Benign lesions: 65% �benign neoplasms: lipoma, leiomyoma, haemangioma, neurofibroma, �following abdominal surgery: adhesions, anastomosis, �Meckel’s diverticulum, �lymphoid hyperplasia and adenitis, �Traumatism, �coeliac disease, �intestinal duplication �Crohn’s disease � Malignant lesions: 15% : most often metastatic: �Melanoma+++ � Idiopathic intussusception: 20%
Discussion: � CT constitute the main imaging modality because of its virtually pathognomonic appearance: bowel-within-bowel: �It appears as a complex soft tissue mass, consisting of the outer intussuscipiens and the central intussusceptum. � There is often an eccentric area of fat density within the mass representing the intussuscepted mesenteric fat. �the mesenteric vessels are often visible within it.

Discussion: � When the CT beam is parallel to its longitudinal axis of the intussusc eption, it appears as a sausage-shaped mass. � Sometimes as reniform or “pseudokidney” mass: it is due to edema, mural thickening, and vascular compromise. � When the beam is perpendicular to the longitudinal axis, it appear as a ‘‘target’’ mass.
Discussion: � CT examination allow to: �Detect and confirm the diagnosis of intessusception. �Show the exact location: small or large bowel. �Appreciate the viability of invaginated loops. �Distinguish between Intussusception without a lead point: no signs of proximal bowel obstruction, target-like or sausage-shaped mass, layering effect. Intussusception with a lead point: signs of bowel obstruction, bowel wall edema with loss of the classic three-layer appearance due to impaired mesenteric circulation and demonstration of the lead mass. CT help reducing the number of unnecessary surgical
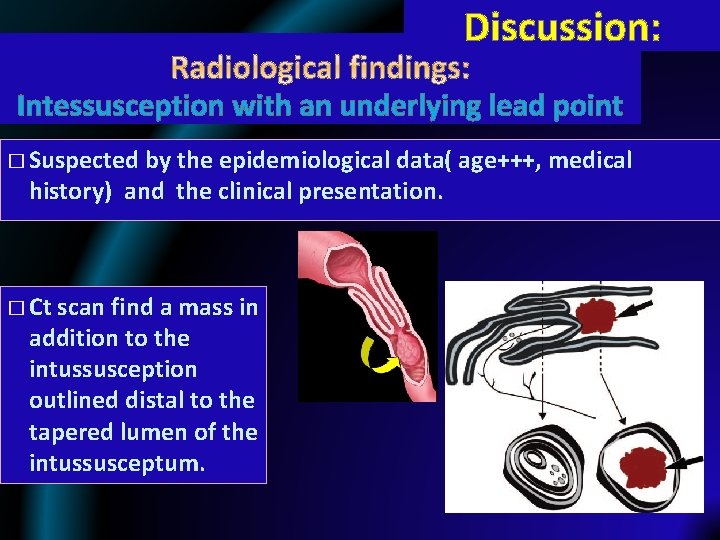
Discussion: Intessusception with an underlying lead point � Suspected by the epidemiological data( age+++, medical history) and the clinical presentation. � Ct scan find a mass in addition to the intussusception outlined distal to the tapered lumen of the intussusceptum.
Discussion: Intessusception with an underlying lead point � The mass’s type is established by the study of its spontanous density and enhancement: for example: Lipoma: fat density wihout containing blood vessels to be distinguished from mesenteric fat and without enhancement. Other malignant tumors (primary or metastatic): tissular density with heterogenous enhancement. � Neoplastic lead point VS Non-neoplastic one: �significantly longer �significantly larger diameter �significantly more proximal dilatation of small bowel downstream.
Discussion: Transcient intessusception: � More frequent in the small bowel than in the colon � It is most frequently detected incidentally and is presumed to be innocuous. � Reported in adults with: �Celiac disease �Crohn disease
Discussion: Magnetic Resonance Imaging (MRI) � Recent developments in MRI with ultrafast multiplanar techniques now allow for rapid evaluation of bowel obstruction. � The multiplanar HASTE (half-fourier single shot turbo spin echo): SSFSE is particularly useful in the diagnosis of intussusception. � The high contrast resolution between the increased signal of the trapped intraluminal fluid and the intermediate to low signal of the bowel wall can clearly demonstrate the pathology.
Discussion: � There is no universal agreement upon the correct treatment of adult intussusception, � The surgery decision is based on: �The epidemiological data: age, medical history. . �The clinical presentation: acute abdominal pain, bowel obstruction, digestive hemorrhagia. . . �The imaging findings: if a lead point is found or not, If there is ischemic bowel signs: � The type of intervention depends essentially on the intraoperative findings.
Conclusion: � Intussusception in adults is an infrequent cause of intestinal obstruction. � Preoperative diagnosis is difficult as symptoms can be intermittent and long standing. � More frequent use of computed tomography in undiagnosed abdominal pain increases the pick up rates.
- Slides: 33