Adrenergic agonists overview n The adrenergic drugs affect
- Slides: 42
Adrenergic agonists
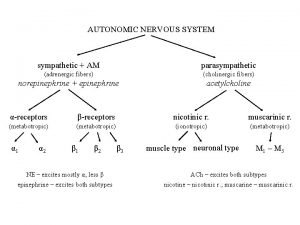
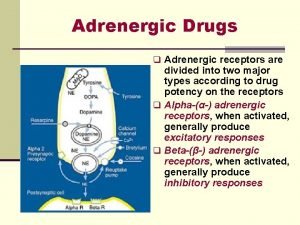
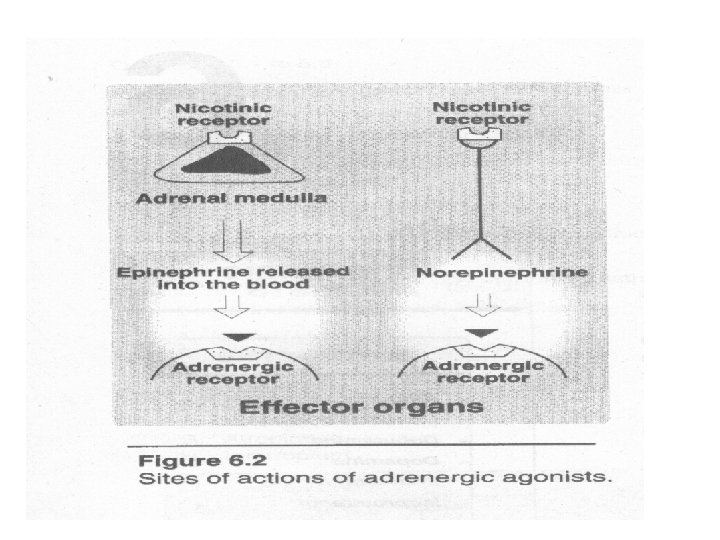
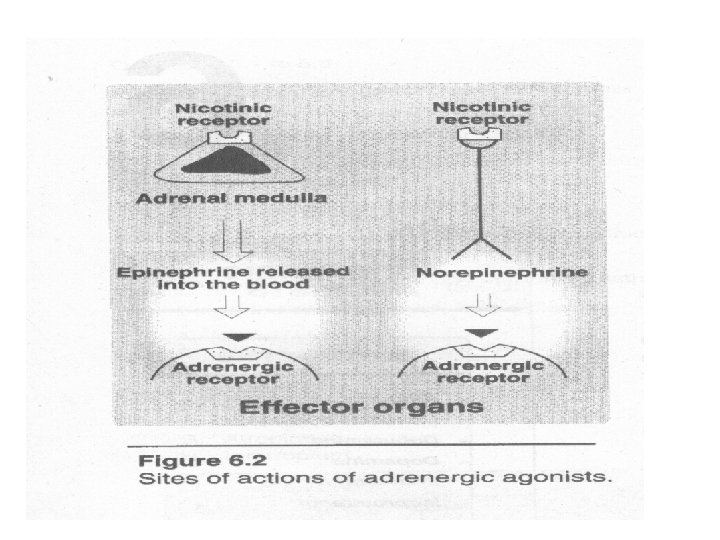
overview n The adrenergic drugs affect receptor that are stimulated by norepinephrine or epinephrine
The adrenergic neuron n n Adrenergic neurons release norepinephrine as the neurotransmitter. CNS, and between ganglia and the effector organs in sympathetic nervous system.
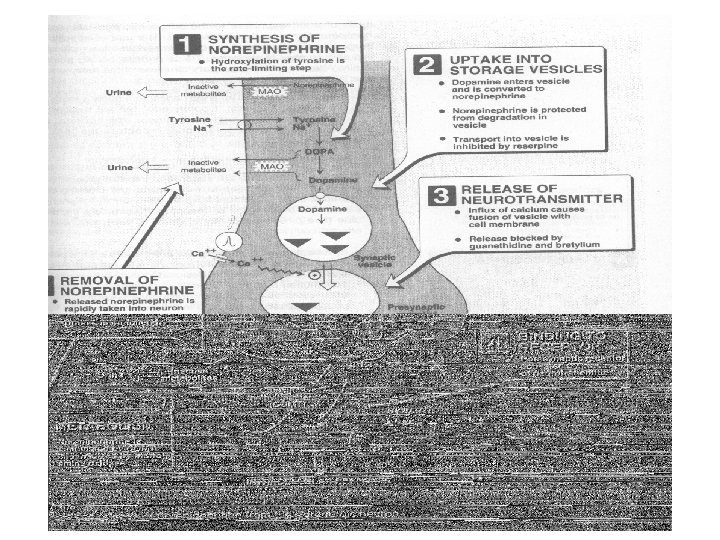
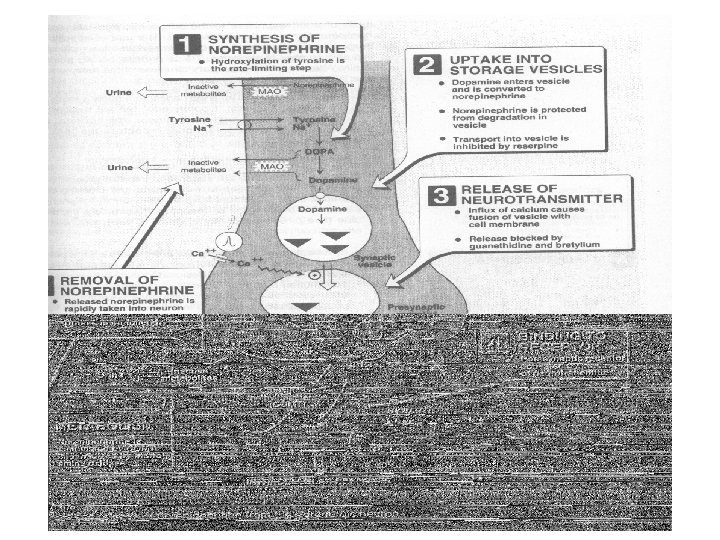
Neurotransmission at adrenergic neurons n n n Synthesis of norepiephrine Storage of norepiephrine in vesicles Release of norepiephrine Binding by receptor Removal of norepiephrine Potential fates of recaptured norepiephrine
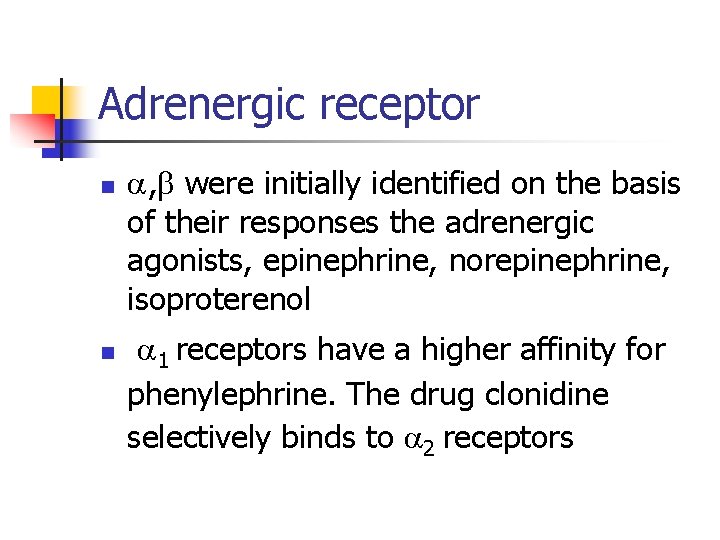
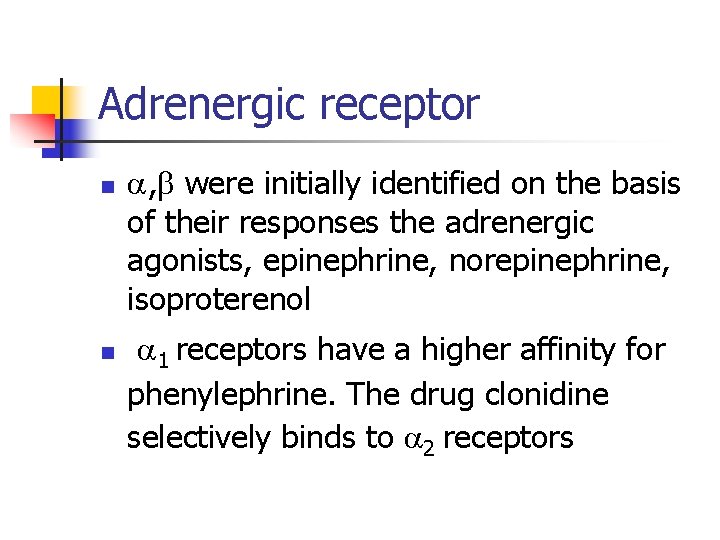
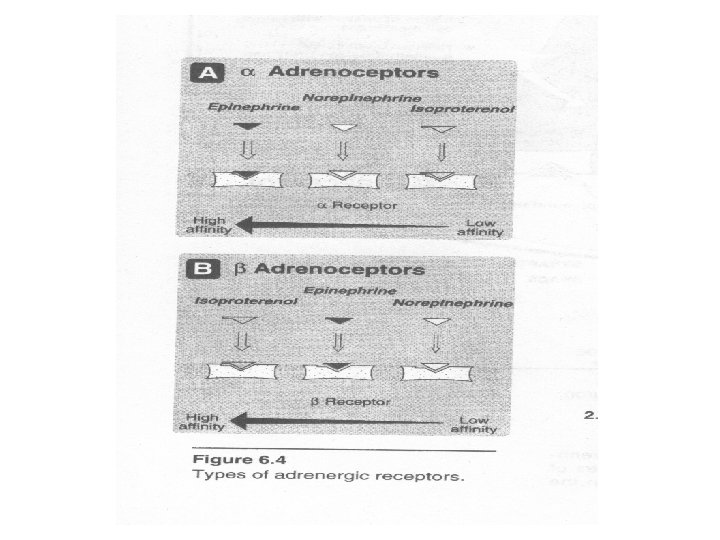
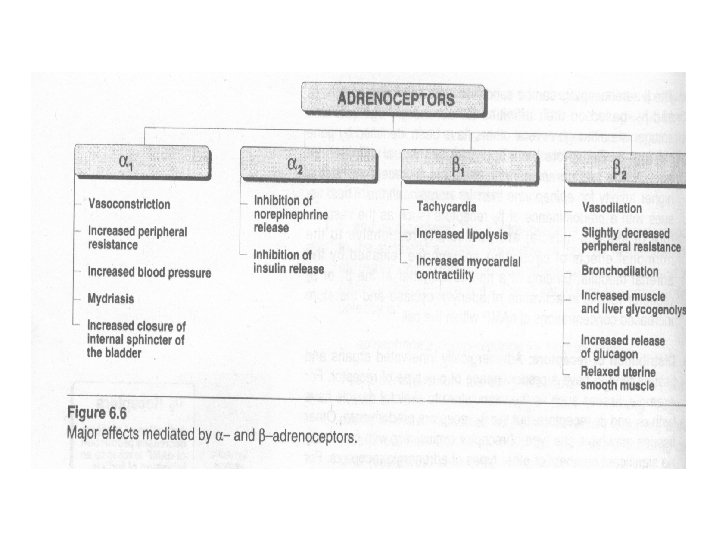
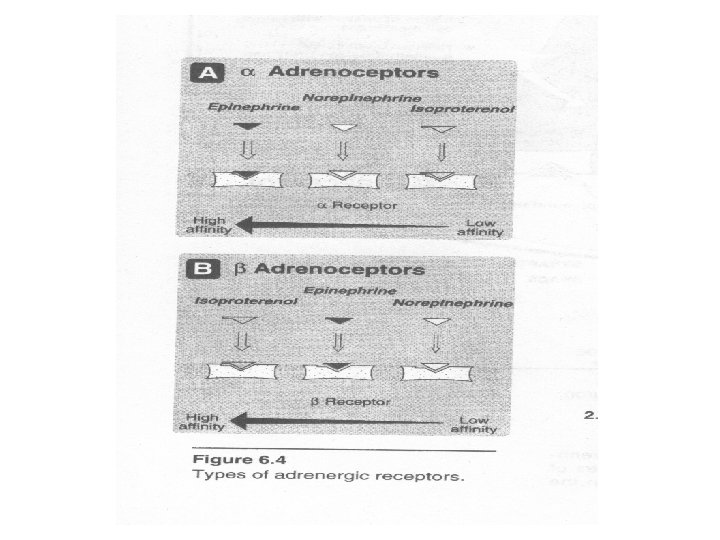
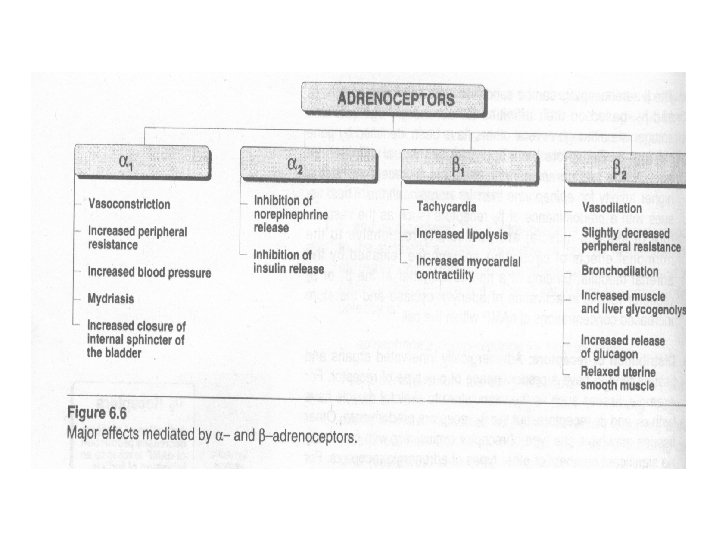
Adrenergic receptor n n , were initially identified on the basis of their responses the adrenergic agonists, epinephrine, norepinephrine, isoproterenol 1 receptors have a higher affinity for phenylephrine. The drug clonidine selectively binds to 2 receptors
1 receptors n these receptors are present on the postsynaptic membrane of the effector organs. G-protein coupling
2 receptors n n Located primarily on the presynaptic nerve endings and on other cells. The stimulation of the 2 receptors causes feedback inhibition of the ongoing release of norepinephrine from the stimulated adrenergic neuron
receptor n n n Characterized by a strong response to isoproterenol. 1 receptor and 2 receptor Results in activation of adenylyl cyclase and therefore increased concentration of c. AMP within the cell
Distribution of receptors n Vasculature to skeletal muscle have both 1 and 2 receptors, but the 2 receptors predominate. The heart contains predominantly 1 receptors
Desensitization of receptors n Prolonged exposure to the catecholamines reduces the responsivity of these receptors.
Characteristics of adrenergic agonists n n n Derivatives of -phenylethylamine Catecholamines: sympathomimetic amines that contain the 3, 4 dihydroxybenzene group Non- catecholamines: lacking the catechol hydroxyl groups have longer half-lives.
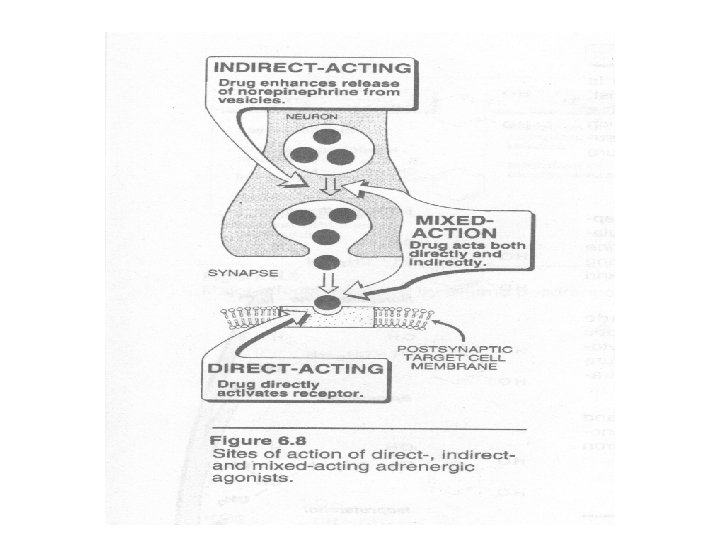
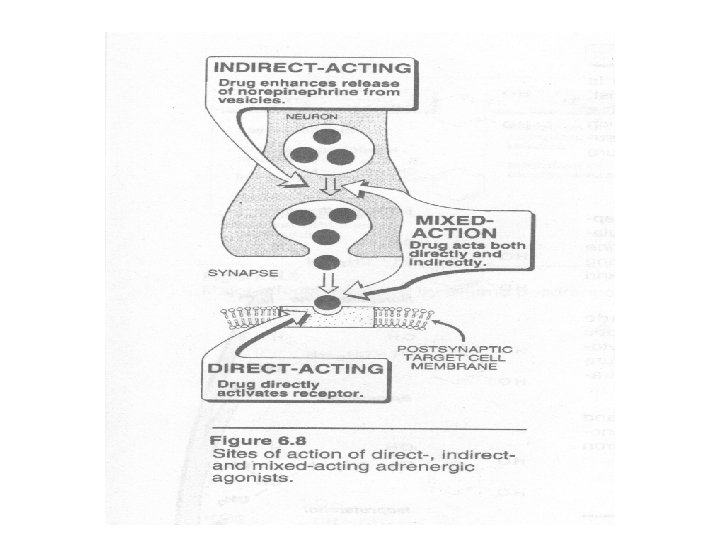
Mechanism of action of adrenergic agonists n n n Direct-acting agonists indirect-acting agonists Mixed-action agonists
Direct-acting adrenergic agonists n n Epinephrine is synthesized from tyrosine in the adrenal medulla and released. Interacts with both and receptors. At low doses, effects(vasodilation) on the vascular system predominate, whereas at high doses, effects(vasoconstriction) are strongest.
actions n n Cardiovascular: strengthen the contractility of the myocardium( 1 effect) Respiratory: causes powerful bronchodilation( 2 effect) Hyperglycemia: lipolysis
Therapeutic uses n n n Bronchospasm: emergency treatment of any condition of the respiratory tract where the presence of bronchoconstriction has resulted in diminished respiratory exchange. Acute asthma Anaphylactic shock
Therapeutic uses n n n Glaucoma: epinephrine solution reduce intraocular pressure in open-angle glaucoma. Anaphylactic shock: for the treatment of Type I hypersensitivity reaction in response to allergens In anesthetics: increase the duration of the local anesthesia
Pharmacokinetics n n n Intravenously for the most rapid onset of action Subcutaneously, by endotracheal tube, by inhalation, or topically to the eye Oral administration is ineffective
Adverse effects n n n CNS disturbance: anxiety, fear, tension, headache, and tremor Hemorrhage: induce cerebral hemorrhage Cardiac arrhythmias:
norepinephrine n a. b. c. Cardiovascular actions Vasoconstriction Baroreceptor reflex Effect of atropine pretreatment:
Therapeutic uses n n Is uses to treat shock because it increases vascular resistance Other actions of norepinephrine are not considered clinically significant. It is never used for asthma.
Isoproterenol n n Isoproterenol is a direct-acting synthetic catecholamine. Stimulates both beta 1 and beta 2 adrenergic receptors.
actions n n n Cardiovascular: increase heart rate and force of contraction, cause increased cardiac output. Beta 2 on arterioles of skeletal muscle result in a decreased peripheral resistance May increase systolic blood pressure slightly
pulmonary n n A profound and rapid bronchodilation is produced by the drug Other effects: other actions on beta receptor, such as increases in blood sugar and increased lipolysis
Therapeutic uses n n Stimulate heart in emergency situations Rarely used as bronchodilator in asthma
dopamine n n Dopamine, the immediate metabolic precursor of norepinephrine Can activate alpha and beta adrenergic receptors
Actions n n Cardiovascular: stimulatory effect on the beta 1 receptors of the heart, having both inotropic and chronotropic effects. At high doses, vasoconstriction Renal and visceral: dopamine dilates renal arterioles by activating dopaminergic receptors, thus increases blood flow to the kidneys and other viscera
Therapeutic uses n Shock: dopamine is the drug of choice for shock. It raises the blood pressure by stimulating the heart(beta 1 action). Dopamine is far superior to norepinephrine.
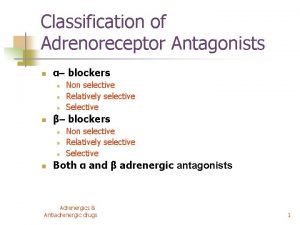
Adrenergic antagonists n Overview: bind to adrenoceptors but do not trigger the usual receptor-mediated intracellular effects
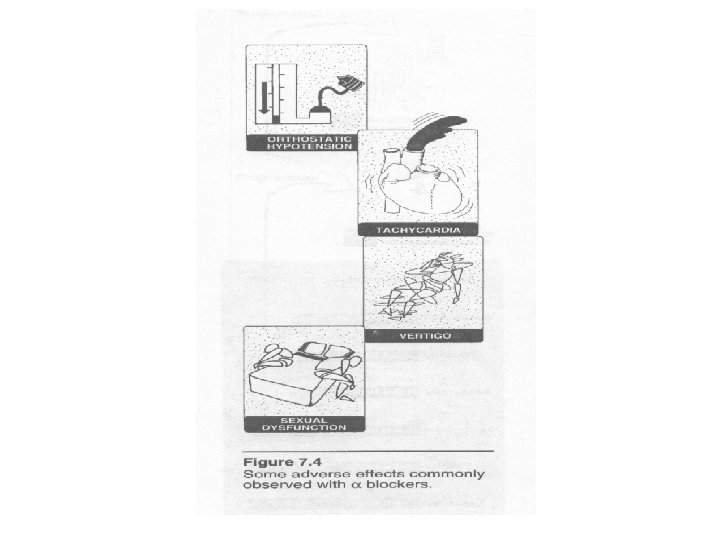
Alpha adrenergic blocking agents n Reduces the sympathetic tone of the blood vessels, resulting in decreased peripheral vascular resistance.
Phenoxybenzamine n n Non-selective, alpha 1 postsynaptic and alpha 2 presynaptic receptors Last about 24 h after a single administration
Actions n n Cardiovascular effects: the decreased peripheral resistance provokes a reflex tachycardia Epinephrine reversal: reverse the alpha agonist actions of epinephrine
Therapeutic uses n Is used in the treatment of pheochromocytoma, a catecholaminesecreting tumor of cells derived from the adrenal medulla.
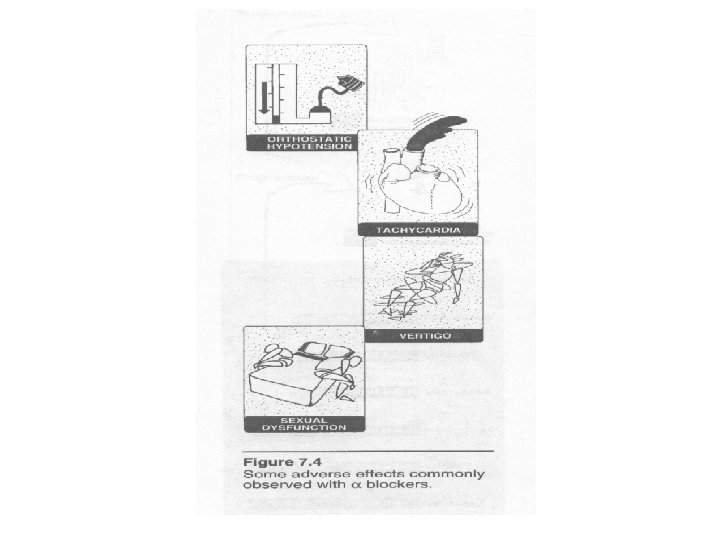
Adverse effects n Can cause postural hypotension, nasal stuffiness, and nausea and vomiting.
Prazosin, terazosin and doxazosin n Cardiovascular effects: prazosin and terazosin decrease peripheral resistance and lower arterial blood pressure
Therapeutic uses n n The “first dose” effects as an alternative to surgery in patients with symptomatic benign prostatic hypertrophy. Decreases tone in the smooth muscle of the bladder neck and prostate and improve urine flow.
Adverse effects n Prazosin and terazosin may cause dizziness, a lack of energy, nasal congestion, headache, and orthostatic hypotension
 Sympathomimetic drugs
Sympathomimetic drugs Antihypertensive drugs classification
Antihypertensive drugs classification Dopamine agonists
Dopamine agonists Indirect acting cholinergic drugs
Indirect acting cholinergic drugs Direct vs. indirect cholinergic agonists
Direct vs. indirect cholinergic agonists Drugs that affect basic driving skills are
Drugs that affect basic driving skills are Adrenergic receptors
Adrenergic receptors Alpha 2 agonist
Alpha 2 agonist Sympathomimetic drugs
Sympathomimetic drugs Sar of adrenergic antagonist
Sar of adrenergic antagonist Cholinergic vs adrenergic
Cholinergic vs adrenergic Opposite of adrenergic
Opposite of adrenergic Adrenergic neuron blockers
Adrenergic neuron blockers Alpha vs beta receptors
Alpha vs beta receptors Adrenergic and cholinergic difference
Adrenergic and cholinergic difference Beta blockers moa
Beta blockers moa Non selective alpha blockers
Non selective alpha blockers Blocking muscarinic receptors would
Blocking muscarinic receptors would Pentolamine
Pentolamine Adrenergic agonist
Adrenergic agonist Alpha-adrenergic antagonist
Alpha-adrenergic antagonist Preganglionic parasympathetic fibres
Preganglionic parasympathetic fibres Lp html
Lp html So nguyen to
So nguyen to đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thang điểm glasgow
Thang điểm glasgow Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Chúa yêu trần thế
Chúa yêu trần thế Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con Diễn thế sinh thái là
Diễn thế sinh thái là