Adopting the TeachBack Method of Patient Education The
Adopting the Teach-Back Method of Patient Education The program is required for all St. Luke’s RNs who perform any patient/family education. Review the entire Power. Point© program which will take approximately 20 minutes. Open the program as “Slide Show”. When finished, close the program and “Take Test. ” You will receive 0. 5 CE for successful completion. Completion of this program should occur by September 1, 2013. 1
Objectives At the conclusion of this program, the learner will be able to: List barriers to teaching/learning Identify patient learning needs Use the Teach-Back method of communication with patients and families to provide meaningful patient education 2
Did you know that… … 90, 000 American adults are illiterate … 40, 000 immigrants speak a language other than English …the average reading level is 8 th or 9 th grade Krames On-Demand patient are Most educational materials areeducation written formaterials a 10 th grade understanding. generally writtenlevel at a of 5 th-8 th grade reading level and are available in many languages. 3
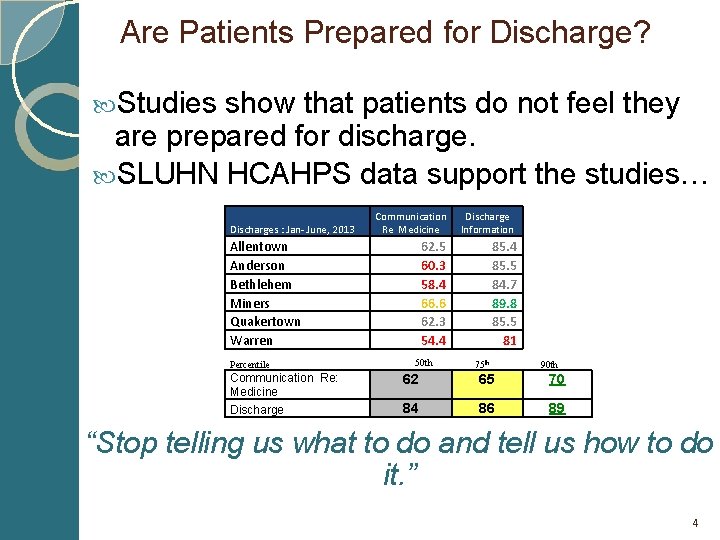
Are Patients Prepared for Discharge? Studies show that patients do not feel they are prepared for discharge. SLUHN HCAHPS data support the studies… Discharges : Jan- June, 2013 Communication Re Medicine Allentown Anderson Bethlehem Miners Quakertown Warren Percentile Communication Re: Medicine Discharge Information 62. 5 60. 3 58. 4 66. 6 62. 3 54. 4 50 th 85. 4 85. 5 84. 7 89. 8 85. 5 81 75 th 90 th 62 65 70 84 86 89 “Stop telling us what to do and tell us how to do it. ” 4
Barriers to Effective Patient Education Nurse Barriers Patient Barriers Environmental Barriers 5
Environmental Barriers The hospital is a stressful environment for patients, families Sometimes our and focusstaff. is on getting it done, not fragmented the patient GETTING Teaching can be and it! incomplete. We often focus on what we need to teach, not always what the patient needs or wants to know. 6
Patient Barriers Patients ◦ ◦ ◦ are: I need to tell you about your new medications. sick stressed in pain medicated unable to understand often overwhelmed Your diagnosis is going… I am afraid your prognosis is not very good… You need to watch your diet… You need to go for a test … This is how you change your dressing. . . Patients may have visual, hearing or cognitive deficits Patients may be resistant to change 7
Patient Barriers Other barriers which may contribute to whether a patient complies or attempts to comply with treatment plans: Socioeconomics (i. e. no insurance, not enough insurance coverage, inability to afford medications or treatments) Cultural differences regarding health and disease (belief systems vary) Understanding the health care system (i. e. how to navigate the system and get what they need) Disease processes and complex treatments (i. e. medical terms, prognosis, consequences) 8
Nurse Barriers Confidence/knowledge subject about the (i. e. disease process, medication, treatment, etc. ) Lack of practice teaching Little patient continuity (i. e. knowing the patient and needs) Time 9
Get Past the Barriers! Acknowledge that there are barriers Accept that it is your responsibility Make the most of the time you have Use simple techniques Teach then document the teaching 10
What you do and say make a difference! Nurses are the most effective and meaningful providers of patient education. Why? Time spent with patients providing care Trust “Nurses maintained their dominance atop Gallup's annual poll on trustworthy professions, topping the list for the 12 th time in the 13 years they have been included as an option. The survey was conducted …among a random sample of 1, 012 adults representing all 50 states. . When asked to rate the honesty and ethical standards of nurses, 84% responded with "very high" or "high, " while 15% responded "average" and only 1% responded "low" or "very low. “ … The only year nurses did not finish first in the survey since their inclusion was 2001, when firefighters took the top spot in the wake of the Sept. 11 terrorist attacks. ” http: //news. nurse. com/article/20111213/NATIONAL 02/112190001/1003 11
Patient-centered Teaching Focus on what the patient or family needs. Example: The patient needs to do daily weights. For effectiveness, what does the RN need to know? Does the patient have a scale? Does the patient understand why weight is important? Does the patient know what to do with the weight data? 12
Patient-centered Teaching Mr. Smith is a heart failure patient and has been instructed to follow a low sodium diet. When asked, Mr. Smith reports he usually has toast and coffee for breakfast, a ham and cheese sandwich with soup for lunch and macaroni and cheese for supper. He says his wife hid the salt shaker so he cannot use it anymore. How can you evaluate whether or not Mr. & Mrs. Smith understand what a low sodium diet means? Does the patient know that low sodium is the same as salt? Does the patient know how to look for the sodium content in packaged and processed foods? 13
Patient-centered Teaching…HOW? By using the evidence-based method called “Teach-back Process” 14
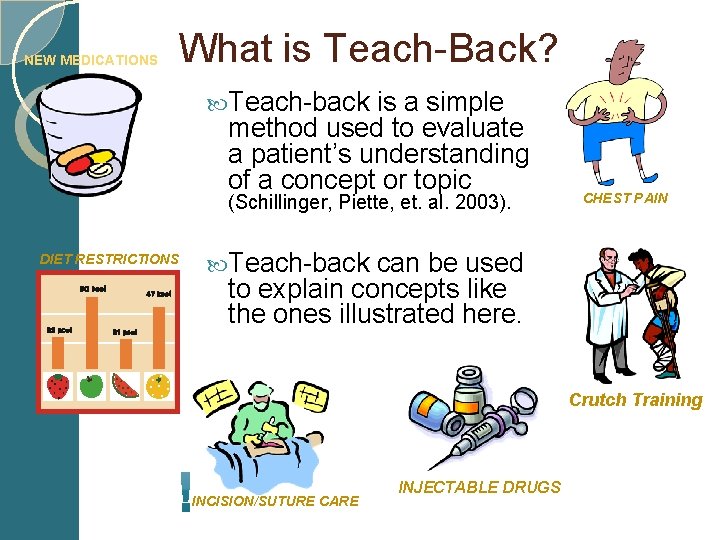
NEW MEDICATIONS What is Teach-Back? Teach-back is a simple method used to evaluate a patient’s understanding of a concept or topic (Schillinger, Piette, et. al. 2003). DIET RESTRICTIONS CHEST PAIN Teach-back can be used to explain concepts like the ones illustrated here. Crutch Training INCISION/SUTURE CARE INJECTABLE DRUGS
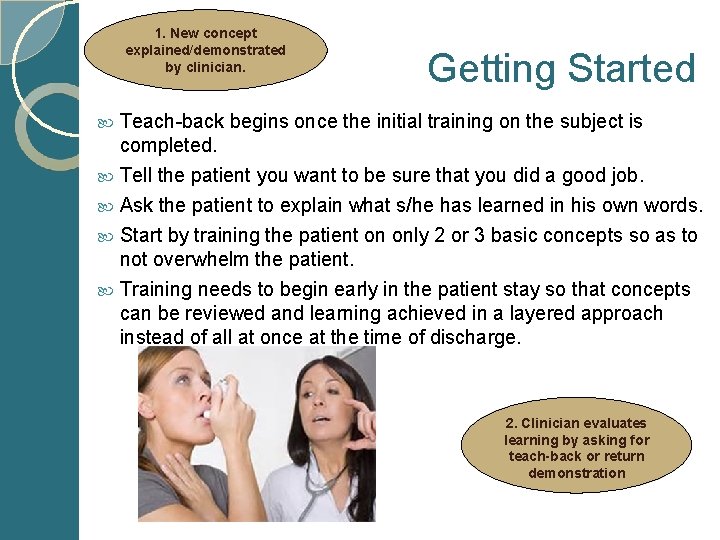
1. New concept explained/demonstrated by clinician. Getting Started Teach-back begins once the initial training on the subject is completed. Tell the patient you want to be sure that you did a good job. Ask the patient to explain what s/he has learned in his own words. Start by training the patient on only 2 or 3 basic concepts so as to not overwhelm the patient. Training needs to begin early in the patient stay so that concepts can be reviewed and learning achieved in a layered approach instead of all at once at the time of discharge. 2. Clinician evaluates learning by asking for teach-back or return demonstration
Teach-Back Process The teach-back process can help you evaluate what the patient understands or does not understand so you know where to focus your teaching. Example: “Mr. Smith, I want to make sure I did a good job in teaching you about the foods that you should avoid. Can you repeat to me what kinds of foods you should avoid? ” 17
3. Clinician clarifies & tailors explanation. Encourage Learning Avoid questions that require yes/no answers Ask open ended questions (encourages the patient to explain what has been learned) Give the patient the time s/he needs to explain. (Rushing raises the anxiety level in the room and interferes with learning) Use simple terms - 5 th grade level or less - without being patronizing Avoid medical jargon/technical terms & abbreviations
Ask the patient the “I” questions: When passing medication the nurse can say: “I want to make sure you know what your medicines are and what they are for. What is the name of your water pill? ” This can be followed with validation and another short question. “We talked about your Lasix yesterday. What do you remember about what it does? ” The nurse may also ask: “I teach people about this everyday and sometimes I may not make myself clear. I want to make sure you know the important things to watch for. Tell me what signs and symptoms of heart failure you need to call your doctor about. ” 19
4. Clinician re-evaluates learning by asking for teach-back or return demonstration Keep Encourage Learning your body language relaxed, your tone cheerful and encouraging and sit so that you are eye level with the patient. Reward the patient with positive feedback. Clarify any misunderstandings. Ask open-ended teach-back questions to assure understanding. Document your evaluation as well as 5. Patient recalls & progress/plan of care for concepts which comprehends; demonstrates mastery still need to be covered.
“I” Questions By starting the teaching session with “I”, you take the pressure off of the patient. Avoid asking “Yes/No” questions like: “Do you understand? ” “Do you have any questions? ” This puts the patient on the spot and may make them feel intimidated. How many patients say, “Yes, I have a question”? 21
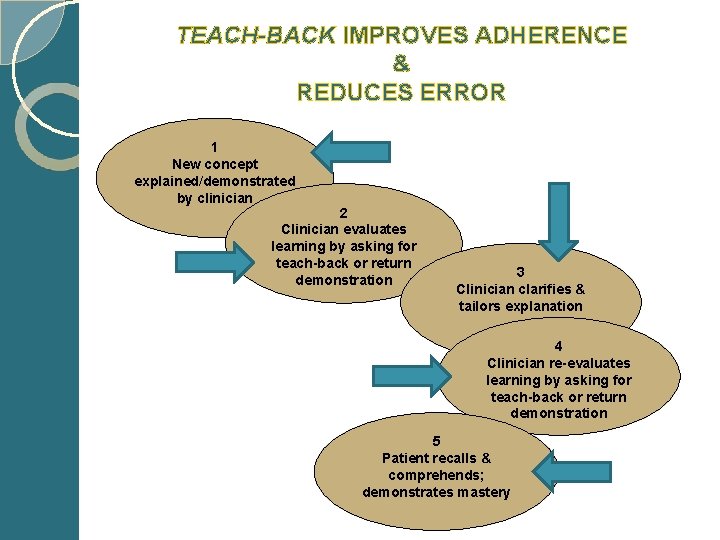
TEACH-BACK IMPROVES ADHERENCE & REDUCES ERROR 1 New concept explained/demonstrated by clinician 2 Clinician evaluates learning by asking for teach-back or return demonstration 3 Clinician clarifies & tailors explanation 4 Clinician re-evaluates learning by asking for teach-back or return demonstration 5 Patient recalls & comprehends; demonstrates mastery
Teach-Back Process Patients who are asked to teach-back may have a better recall and understanding of their instructions and are more likely to follow them. True or False? The process also provides the perfect opportunity to correct misinformation, add relevant details, and reinforce key points. True or False? 23
Putting It All Together http: //www. youtube. com/watch? v=4 r 9 NRb. K 9 MRk 24
Teach-Back Process St. Luke’s University Health Network is adopting the Teach-Back Process for ALL patient education. “Every Patient, Every Time” Start Now…begin using this simple process immediately. 25
Coming Soon An addition to the Teaching section of the Mc. Kesson computer documentation system: □Teach-Back Method WATCH for IT! 26
Summary Why is using the Teach-Back Method key to successful patient/family education? Improves patient outcomes Improves ability to manage care/self-care after discharge Reduces re-admissions Improves patient satisfaction Complies with accreditation standards It is evidence-based Tell me and I’ll forget; It is the right thing to do! Show me and I may remember; Involve me and I’ll understand. ~Chinese Proverb 27
Thank you! Exit the Power. Point program and “Take Test”. This program provides 0. 5 CE. Print and retain a copy of the certificate for your records. Go forth and Teach Back! 28
Special thanks to the following individuals who helped create this program: Amanda Miller, BSN, RN - Miners Campus Wanda Reitz, BS, RN - Bethlehem Campus Cathy Rehnert, MSN, RN and Pam Miles, ACNSBC – Allentown Campus 29
References Burkhead, V. , Jones, E. , Von. Cannon, L. & Hu, J. (2003). ENTER: A care guide for successfully educating patients. Journal for Nurses in Staff Development, 19(3), 143 -146. Gerber & Finn. (1998). Learning document skills at school and at work. Journal of Adolescent & Adult Literacy, 42(1), 32 -44. Help your patients succeed: Tips for improving communication with your patients. (2008). Pfizer Clear Health Communication Initiative. Retrieved, October 30, 2012 from http: //pfizerhealthliteracy. com/public-health Teach-Back: A tool for improving provider-patient communication (2006). Department of Veterans Affairs. Retrieved, October 30, 2012 from http: //www. ethics. va. gov/docs/infocus/In. Focus_20060401_Teach_Back. pdf. Resources: http: //www. nchealthliteracy. org/toolkit/tool 5. pdf www. nchealthliteracy, org www. pfizerhealthliteracy. com www. ethics. va. gov 30
- Slides: 30