ADJUSTMENT DISORDER Dr shakeel Adjustment Disorder Short term



- Slides: 16
ADJUSTMENT DISORDER Dr shakeel
Adjustment Disorder Short term maladaptive reactions to psychological stressor Symptoms must appear within 3 months of a stressor’s onset Stressors are not specified, mostly everyday events (loss of loved one, change of employment, financial situation) Symptoms usually resolved within 6 months (may be longer if produced by a chronic stressor)
COMMON SYMPTOMS � � Anxiety, depression, deliberate self harm, worry, decreased concentration, aggression, irritability with substance abuse. ANS arousal symptoms such as palpitations , tremor. Gradual onset, prolonged course. Impairment in social , occupational functioning and intense distress.
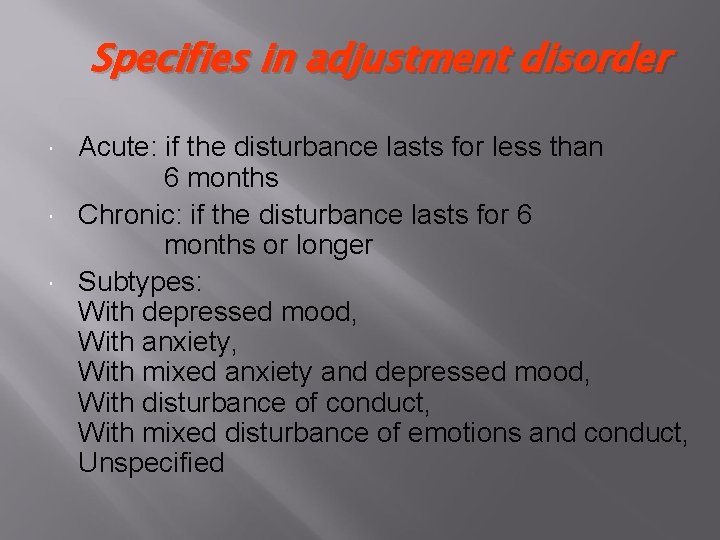
Specifies in adjustment disorder Acute: if the disturbance lasts for less than 6 months Chronic: if the disturbance lasts for 6 months or longer Subtypes: With depressed mood, With anxiety, With mixed anxiety and depressed mood, With disturbance of conduct, With mixed disturbance of emotions and conduct, Unspecified

Common causes � � � Sexual and physical abuse Divorce and separation Change of job, school shifting Migration or status change Birth of a handicap child. Terminal illness.
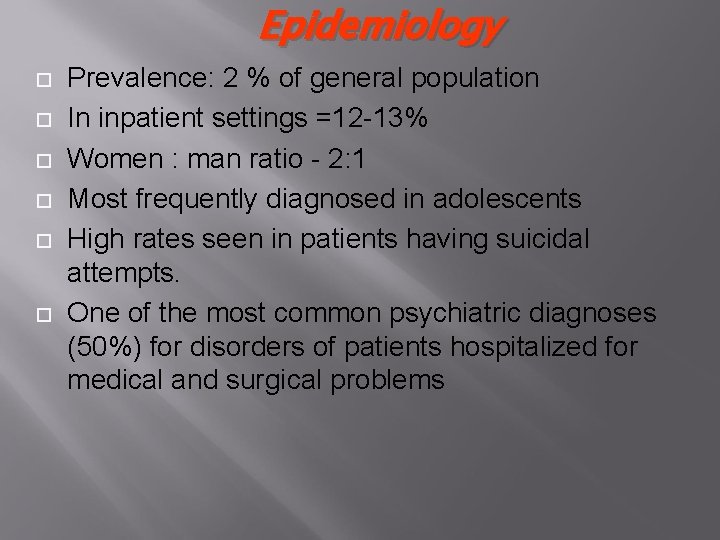
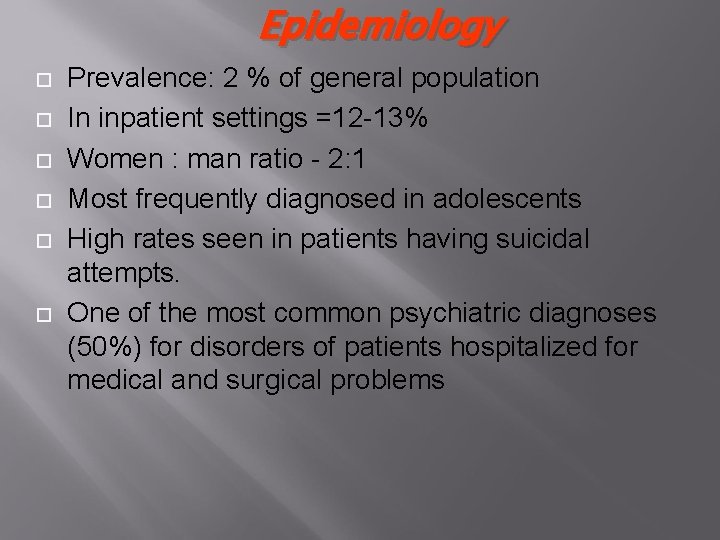
Epidemiology Prevalence: 2 % of general population In inpatient settings =12 -13% Women : man ratio - 2: 1 Most frequently diagnosed in adolescents High rates seen in patients having suicidal attempts. One of the most common psychiatric diagnoses (50%) for disorders of patients hospitalized for medical and surgical problems

Risk Factors � � � Individual social support system, marital status (unmarried) also predispose him vulnerable for a stressor. Medically ill children are more likely to acquire AD when their families are malfunctioning. A positive child-parent relationship has a protective value, while previous mental or physical disorders increase the risk.
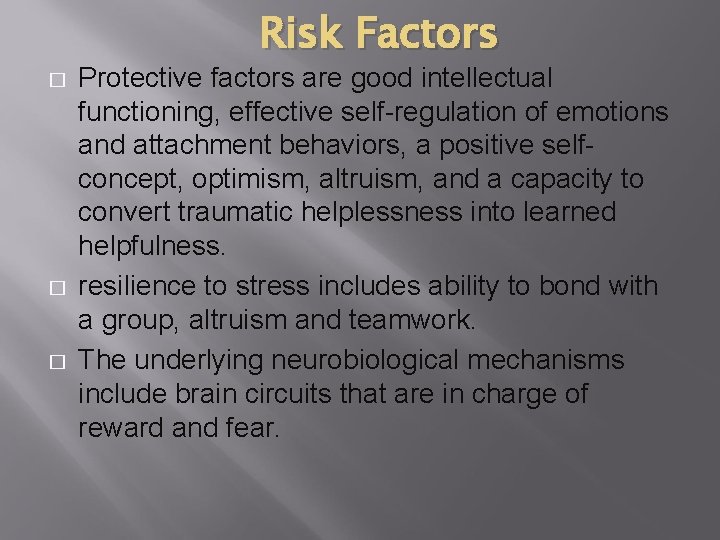
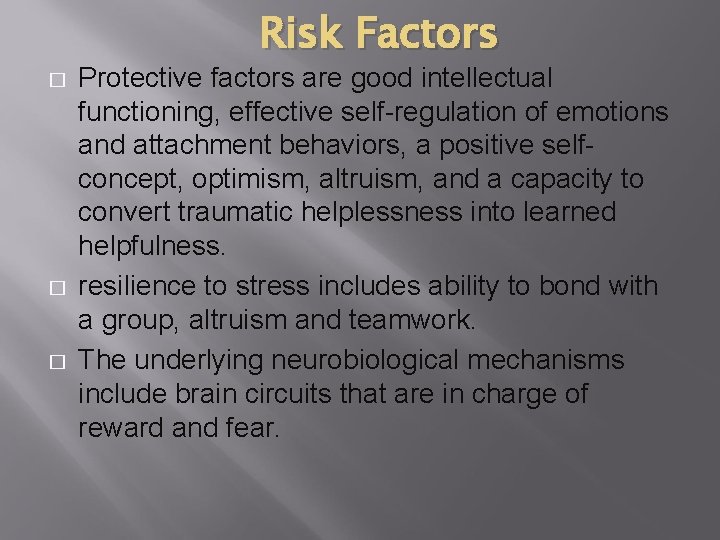
Risk Factors � � � Protective factors are good intellectual functioning, effective self-regulation of emotions and attachment behaviors, a positive selfconcept, optimism, altruism, and a capacity to convert traumatic helplessness into learned helpfulness. resilience to stress includes ability to bond with a group, altruism and teamwork. The underlying neurobiological mechanisms include brain circuits that are in charge of reward and fear.
Genetic factors � One study found a slightly greater prevalence of AD in monozygotic twins than dizygotic twins.
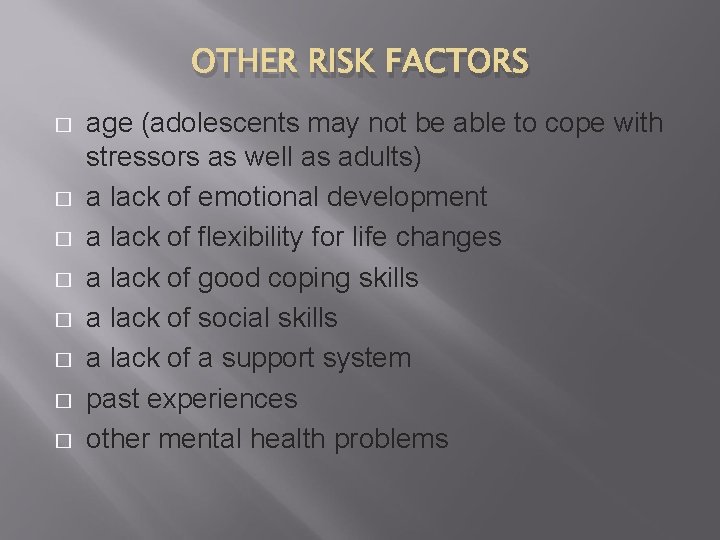
OTHER RISK FACTORS � � � � age (adolescents may not be able to cope with stressors as well as adults) a lack of emotional development a lack of flexibility for life changes a lack of good coping skills a lack of social skills a lack of a support system past experiences other mental health problems
Neurotransmitters � � � In adjustment disorder main principle is complex feedback between the various mediators including cortisol, corticotropin-releasing hormone, norepinephrine, serotonin, and gonadal steroids.
Differential Diagnosis Grief reaction Acute stress reaction/disorder GAD/panic attack PTSD Acute and transient psychotic disorder Conversion/dissociation. Substance-related disorder Somatization disorder depressive illness Personality disorder
Co-morbidity � � � 70% patients have another co morbid disorder. substance abuse and dependence. personality disorders.
Course and Prognosis Generally favorable prognosis Symptoms of AD usually disappear within 6 months. one-third of patients do not remit after 6 months, and one-fourth still have the disorder after a year. Recovery seen in more than 90% patients, Some patients (30 -40%) receive later a diagnosis of mood disorder, antisocial personality or substance related disorder. 30% have suicidal thoughts and 20% have completed suicide.

Treatment (psychotherapy) M Carta BMC-2009 Psychotherapy – the treatment of choice solution-focused therapy, that help the individual deal more effectively with the specific life problem solving therapy. Dynamic supportive therapy, cognitive-behavioral therapy, hypnosis and relaxation techniques.
Pharmacological treatment � � The recommended pharmacologic treatment period is shorter than 3 months. Occasionally an anxiolytic or hypnotic is used for few days and tricyclic antidepressants and methylphenidate have efficacy in medically ill patients
 Long and short
Long and short Nadia shakeel
Nadia shakeel Komal shakeel
Komal shakeel Long term plan and short term plan
Long term plan and short term plan Long term memory vs short term memory
Long term memory vs short term memory Example of short term human resources
Example of short term human resources Difference between long term and short term liabilities
Difference between long term and short term liabilities Long term liabilities
Long term liabilities Short term goals examples for students
Short term goals examples for students Short term and long term cash forecasting
Short term and long term cash forecasting Adjustment disorder nursing diagnosis
Adjustment disorder nursing diagnosis Adjustment disorder
Adjustment disorder Dsm 5 munchausen by proxy
Dsm 5 munchausen by proxy In my understanding
In my understanding Nth term of a quadratic sequence
Nth term of a quadratic sequence Position-to-term rule
Position-to-term rule Expand a+bc'+abd'+abcd to minterms and maxterms
Expand a+bc'+abd'+abcd to minterms and maxterms