ADHD What is ADHD ADHD is a syndrome
- Slides: 26
ADHD
What is AD/HD? �AD/HD is a “syndrome of learning and behavioral problems characterized by difficulty in sustaining attention, impulsive behavior, and usually by excessive activity. ” (APA Style Guide, 7 th ed. ) �Point of some contention among psychologists: Whether AD/HD is a neurologically-based developmental disability or whether it’s a “fad diagnosis. ”
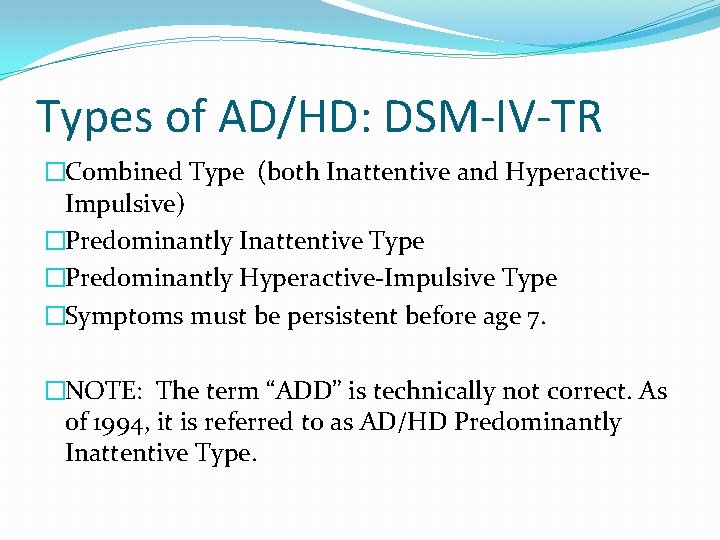
Types of AD/HD: DSM-IV-TR �Combined Type (both Inattentive and Hyperactive. Impulsive) �Predominantly Inattentive Type �Predominantly Hyperactive-Impulsive Type �Symptoms must be persistent before age 7. �NOTE: The term “ADD” is technically not correct. As of 1994, it is referred to as AD/HD Predominantly Inattentive Type.
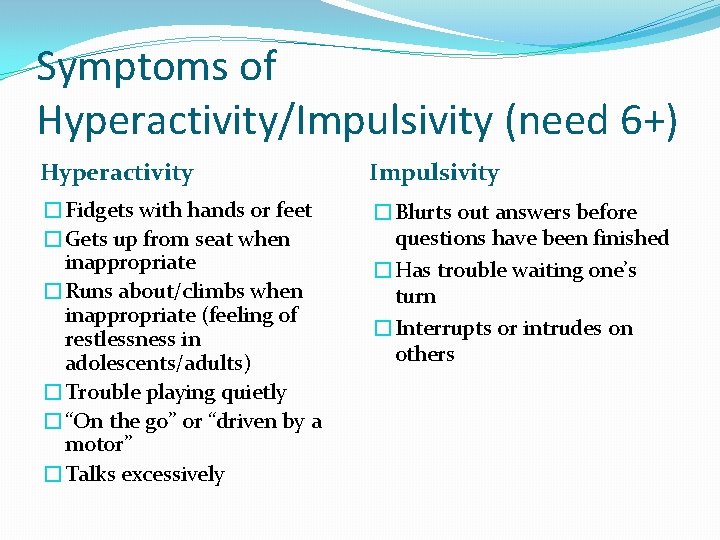
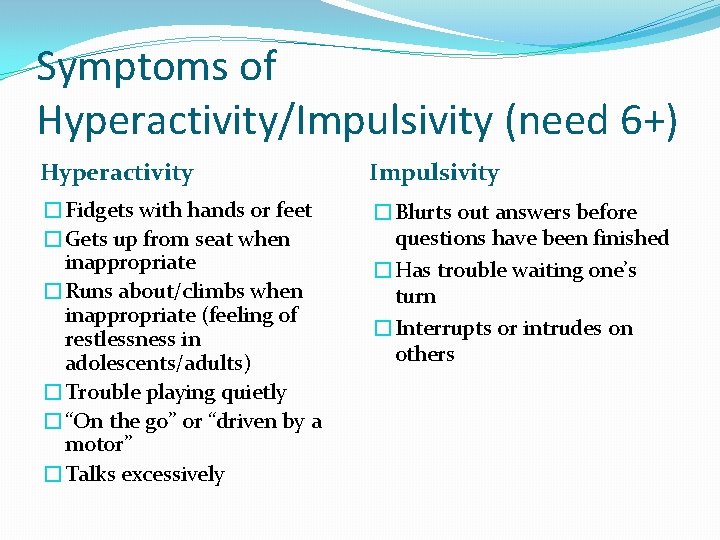
Symptoms of Hyperactivity/Impulsivity (need 6+) Hyperactivity Impulsivity �Fidgets with hands or feet �Gets up from seat when inappropriate �Runs about/climbs when inappropriate (feeling of restlessness in adolescents/adults) �Trouble playing quietly �“On the go” or “driven by a motor” �Talks excessively �Blurts out answers before questions have been finished �Has trouble waiting one’s turn �Interrupts or intrudes on others
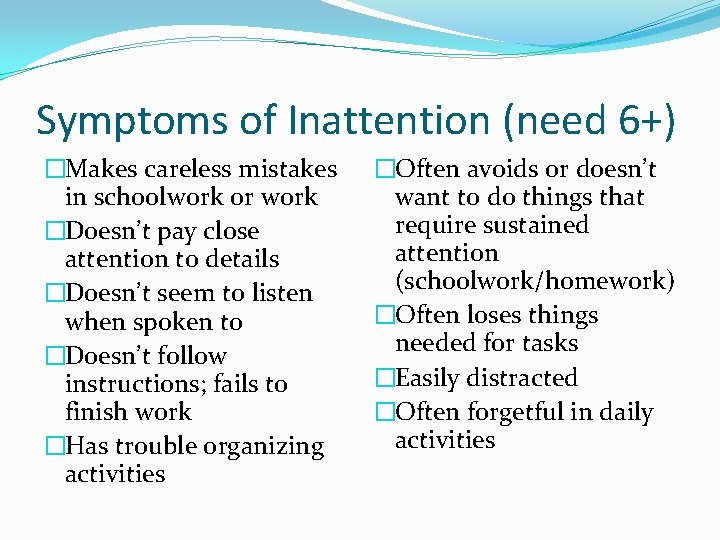
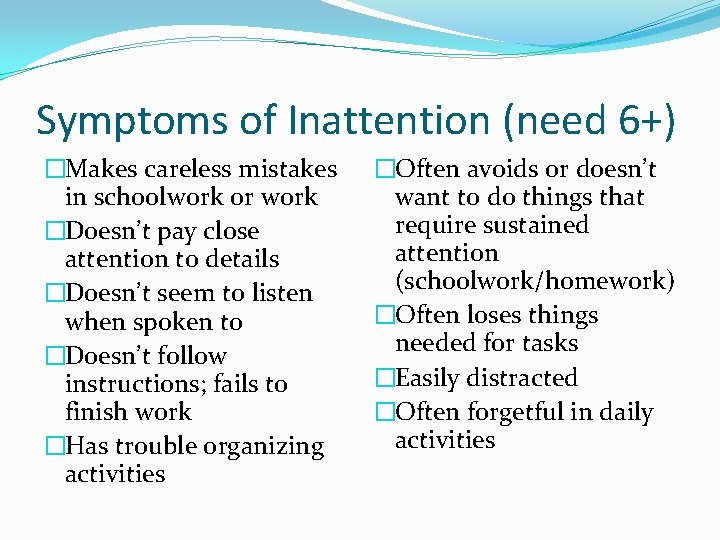
Symptoms of Inattention (need 6+) �Makes careless mistakes in schoolwork or work �Doesn’t pay close attention to details �Doesn’t seem to listen when spoken to �Doesn’t follow instructions; fails to finish work �Has trouble organizing activities �Often avoids or doesn’t want to do things that require sustained attention (schoolwork/homework) �Often loses things needed for tasks �Easily distracted �Often forgetful in daily activities
Children with AD/HD may have trouble controlling their impulses.
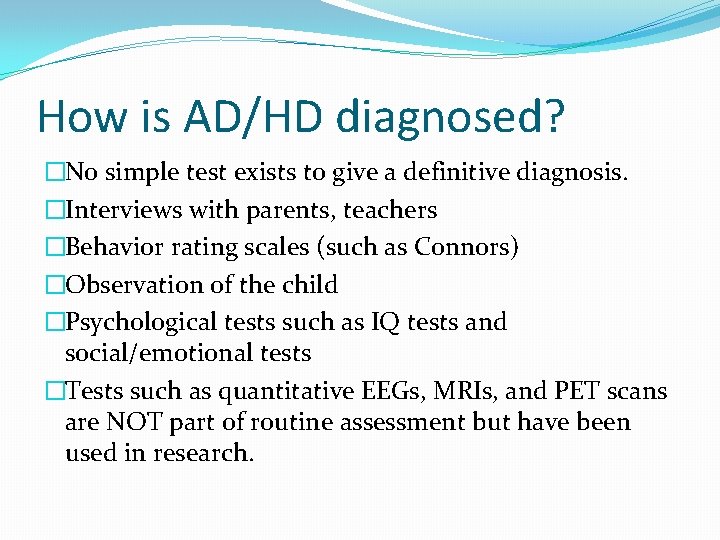
How is AD/HD diagnosed? �No simple test exists to give a definitive diagnosis. �Interviews with parents, teachers �Behavior rating scales (such as Connors) �Observation of the child �Psychological tests such as IQ tests and social/emotional tests �Tests such as quantitative EEGs, MRIs, and PET scans are NOT part of routine assessment but have been used in research.
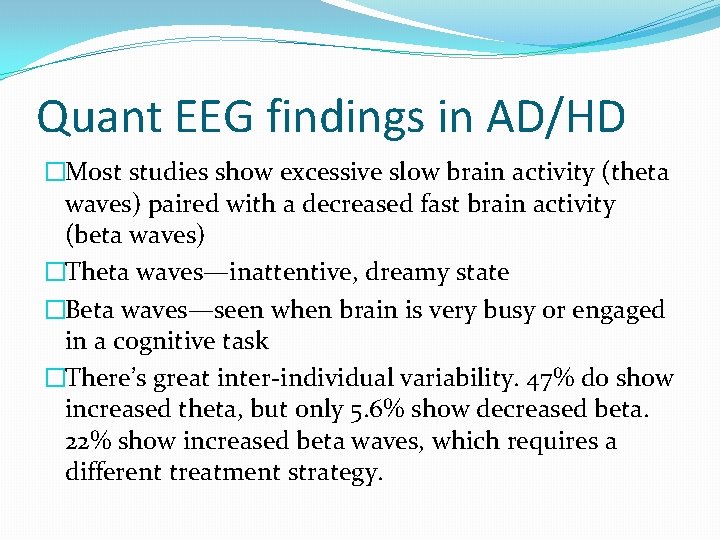
Quant EEG findings in AD/HD �Most studies show excessive slow brain activity (theta waves) paired with a decreased fast brain activity (beta waves) �Theta waves—inattentive, dreamy state �Beta waves—seen when brain is very busy or engaged in a cognitive task �There’s great inter-individual variability. 47% do show increased theta, but only 5. 6% show decreased beta. 22% show increased beta waves, which requires a different treatment strategy.
Other brain differences �Children with AD/HD show decreased electrical and blood-flow activity in the frontal lobe and in other areas involved in attention, behavior inhibition, and motor control. �The brain volume of children with AD/HD is roughly 3% smaller than average.
Do children grow out of AD/HD? �Study by the NIMH in 2007 found that parts of the cortex mature more slowly in children with ADHD. �The lateral prefrontal cortex reaches maximum thickness at age 10. 5 in AD/HD children compared with age 7. 5 in children without it. �Some children do appear to “grow out of it, ” but some do not. It’s not understood why.
What causes AD/HD? �Presently unknown �There is a genetic predisposition. Genes involving neural communication have been implicated. �September 2009: An article in JAMA with adults with AD/HD showed lower dopamine receptor levels in the midbrain & accumbens (key dopamine receptor pathways) compared to controls. Low dopamine receptors were linked to inattention. �Prenatal exposure to alcohol, nicotine, or other drugs may increase the risk of ADHD. �Exposure to lead may increase the risk.
Stimulant medications �Stimulants such as Ritalin/Concerta are effective in 70 -80% of children with AD/HD. �Children with increased Beta activity as shown in QEEGs do not respond well to stimulants. �In general, children whose AD/HD involves frontal lobe inactivity respond to stimulants because the drugs appear to increase activity in the frontal lobe.
Special Diets and AD/HD �Research has shown that sugar is not related to AD/HD. �Restricted diets such as the Feingold Diet help about 5% of children with AD/HD. Most of these are very young children or those with food allergies.
Other Facts about AD/HD �Boys are 3 -9 times more likely to be diagnosed than girls are. �Children with AD/HD tend to score 7 -15 points lower on IQ tests than other children do, but this might reflect their inability to stay focused rather than a true intellectual difference. �About 10 -30% of gifted children have AD/HD, compared to 3 -5% in the general population.
Comorbidities and AD/HD �AD/HD is often seen in combination with other disorders, such as the following: �Depression �Anxiety �Obsessive-compulsive disorder �Oppositional defiant disorder �Drug and alcohol abuse: About 1/3 of children with AD/HD end up abusing drugs and alcohol during adolescence and adulthood.
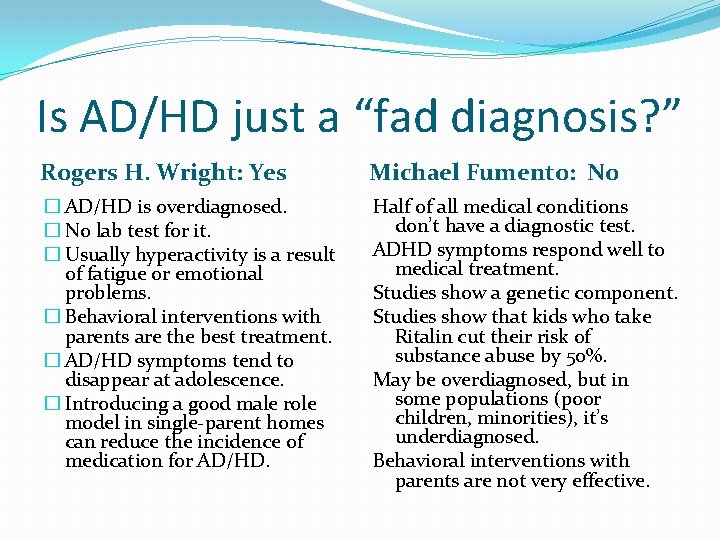
Is AD/HD just a “fad diagnosis? ” Rogers H. Wright: Yes Michael Fumento: No � AD/HD is overdiagnosed. � No lab test for it. � Usually hyperactivity is a result of fatigue or emotional problems. � Behavioral interventions with parents are the best treatment. � AD/HD symptoms tend to disappear at adolescence. � Introducing a good male role model in single-parent homes can reduce the incidence of medication for AD/HD. Half of all medical conditions don’t have a diagnostic test. ADHD symptoms respond well to medical treatment. Studies show a genetic component. Studies show that kids who take Ritalin cut their risk of substance abuse by 50%. May be overdiagnosed, but in some populations (poor children, minorities), it’s underdiagnosed. Behavioral interventions with parents are not very effective.
Coping with a Child with AD/HD
Spanking It may feel like the right thing to do, but physical punishment and aggression do not work well with children with AD/HD.
AD/HD and “Spirit” �Children with AD/HD present with challenging behavior: explosive tantrums, inflexibility, hyperactivity, and intensity. �Lots of overlap between children with a spirited temperament and those with true AD/HD (Kurcinka, 1998) �Children with AD/HD would often be considered “difficult” children in Thomas & Chess’s model. �Medication alone is not sufficient. Effective parenting strategies are crucial.
Thomas & Chess’s Goodness of Fit model (1977) �Parents can change child’s temperament somewhat by using different parenting styles. �Difficult children need warm, sensitive, and consistent parents who are gentle but who make firm & reasonable demands. �Harsh parenting leads to conduct problems in difficult children. �Parents must respond sensitively and consistently to their difficult children’s needs to avoid behavior problems.
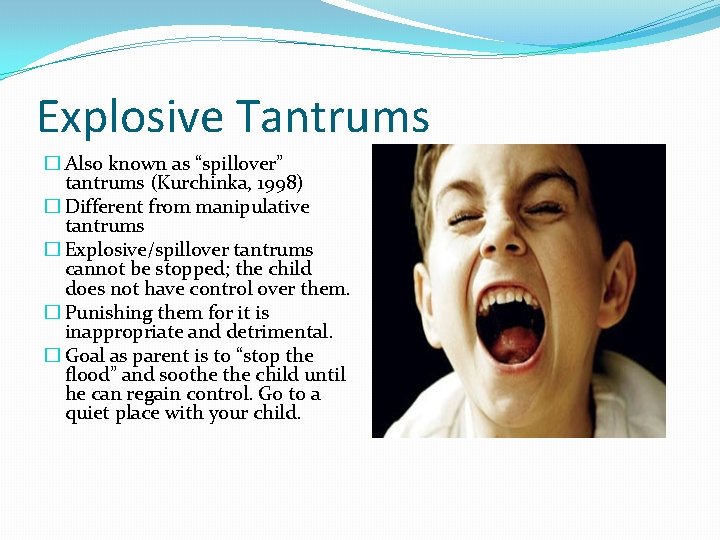
Explosive Tantrums � Also known as “spillover” tantrums (Kurchinka, 1998) � Different from manipulative tantrums � Explosive/spillover tantrums cannot be stopped; the child does not have control over them. � Punishing them for it is inappropriate and detrimental. � Goal as parent is to “stop the flood” and soothe child until he can regain control. Go to a quiet place with your child.
Greene’s “Explosive Child” �Explosive child is basically the same as a spirited child. �Greene says that “children do well if they can. ” �An explosive outburst occurs when cognitive demands being placed on a person outstrip his ability to cope. �Explosive kids lack certain “executive skills” (organizing, planning, separating emotional reactions from the thinking you need to do, controlling impulses, etc. ) �Common in children with ADHD, autism, and other developmental disorders.
Parents’ role (Greene’s model) �Parents have to function as their child’s executive center during explosive tantrums. �First: Avoid triggers for the tantrum if possible, even if it means “giving in” to the child. �Standard “behavioral management approach” (like Dr. Phil’s “going commando”) does NOT work with explosive children. Need a gentler approach. �Inflexibilty + inflexibility = explosion. Child can’t be flexible, so parent has to be until child learns those executive skills.
Greene’s Plans A, C, and B �Plan A: telling child “You must” or “You will. ” “Do what I said because I said so. ” Works with easy children but not difficult ones. �Plan C: opposite from Plan A; dropping the expectation completely, at least temporarily. E. g. , Don’t take explosive child to the grocery store. �Plan B: “Collaborative Problem Solving. ” Present problem to the child and ask for his input in how it should be solved. (Surrogate frontal lobe)
Keys to Success �Empathy—you must be able to see the world from the child’s perspective and have empathy for how he’s feeling. (Refer to Kochanska’s article about MRO: empathy in mothers played a key role in establishing MRO. ) �Another key—staying calm as much as you can. A reactive tantrum from the parent just makes the child’s tantrum worse.
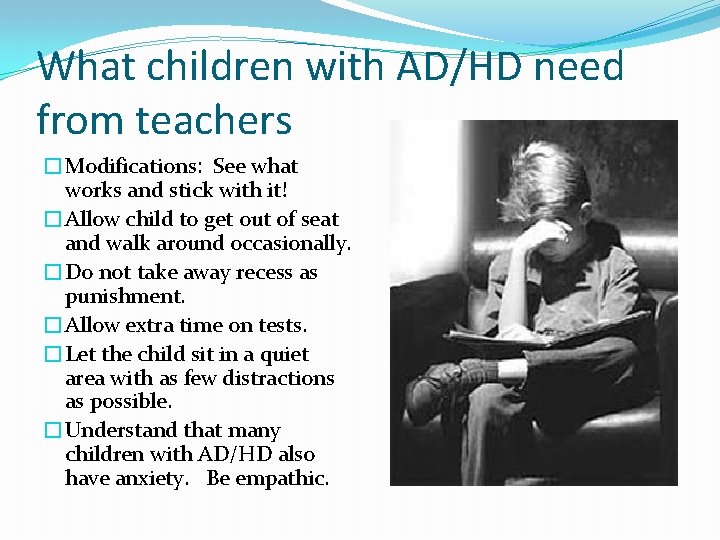
What children with AD/HD need from teachers �Modifications: See what works and stick with it! �Allow child to get out of seat and walk around occasionally. �Do not take away recess as punishment. �Allow extra time on tests. �Let the child sit in a quiet area with as few distractions as possible. �Understand that many children with AD/HD also have anxiety. Be empathic.