ADHD TRAINING MORNING Programme What is ADHD Core





- Slides: 35

ADHD TRAINING MORNING
Programme What is ADHD? ¡ Core Symptoms ¡ Assessment Process ¡ Aetiology and Risk Factors ¡ Management ¡ Support strategies in the classroom ¡ Questions ¡
Multi-Disciplinary Team (MDT) Approach ¡ A MDT approach is key within the assessment, treatment and management of children with ADHD ¡ Key members of the team: Doctor Specialist Nurse Community Mental Health Worker Occupational Therapist Liaison with Educational Psychologist The children, parents and education staff are integral

What is ADHD? ¡ ¡ ¡ Medically diagnosed condition Neurodevelopmental condition 3 Core Features or Behaviours l Inattention l Impulsiveness l Hyperactivity 3 P’s: Pre-school/Pervasive/Persistent The symptoms must be having an impact on the child’s academic, psychological or social functioning
What is ADHD? ¡ Those affected often fail to achieve their potential and have many co-morbid difficulties… ¡ It is thought to affect 2 to 5% of the childhood population. ¡ More boys diagnosed (4: 1) ¡ ADHD is on a continuum and symptoms can vary from mild to severe ¡ 3 main types – individuals can be strongly influenced by external factors
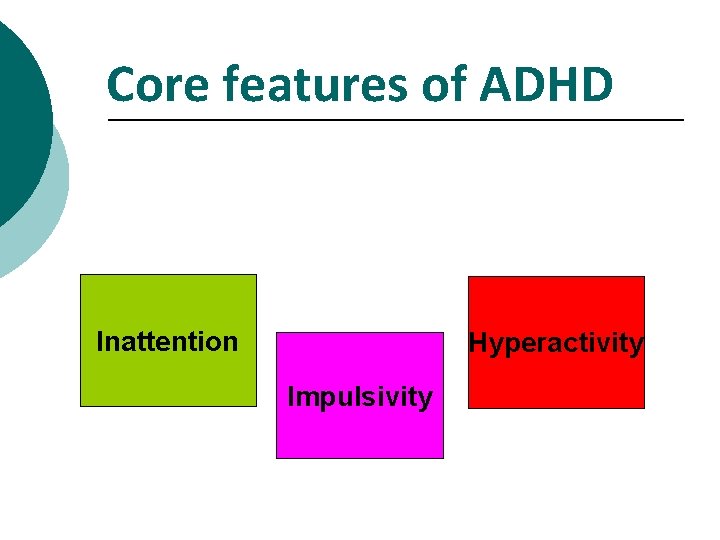
Core features of ADHD Inattention Hyperactivity Impulsivity
Inattention ¡ Difficulty sustaining attention, particularly boring, repetitive tasks, those which they are not interested in or require sustained mental effort. ¡ Poor attention to detail or makes careless mistakes ¡ Easily distracted ¡ Forgetful in daily activities ¡ Often does not seem to listen - even when spoken to directly ¡ Fails to follow directions ¡ Poor self-organisation-possessions/work ¡ STM
Impulsiveness ¡ Blurts out answers too soon ¡ Easily led ¡ Difficulty waiting turn ¡ Interrupts/intrudes on others’ activities ¡ Talks excessively without response to social constraints ¡ Does/says things without thinking of the consequences. ¡ Reacts quickly without thinking ¡ Completes activities quickly and without attention/care to detail ¡ Risk-taker
Think before you act…. .
Hyperactivity ¡ Fidgets, squirms ¡ Noisy, can’t play or work quietly Persistent over-activity - not moderated by social demands - no ‘off switch’ ¡ Often leaves seat in classroom or in other situations where expected to remain seated ¡ ¡ Runs around or climbs excessively where it is inappropriate ¡ Talks excessively and goes off on tangents
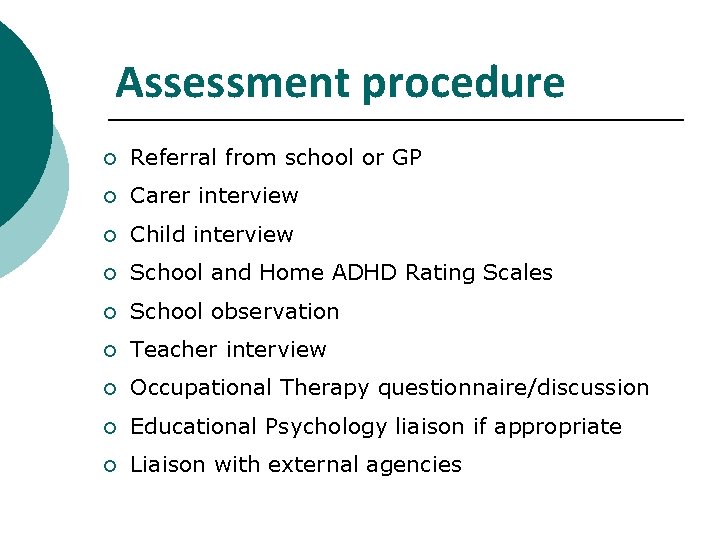
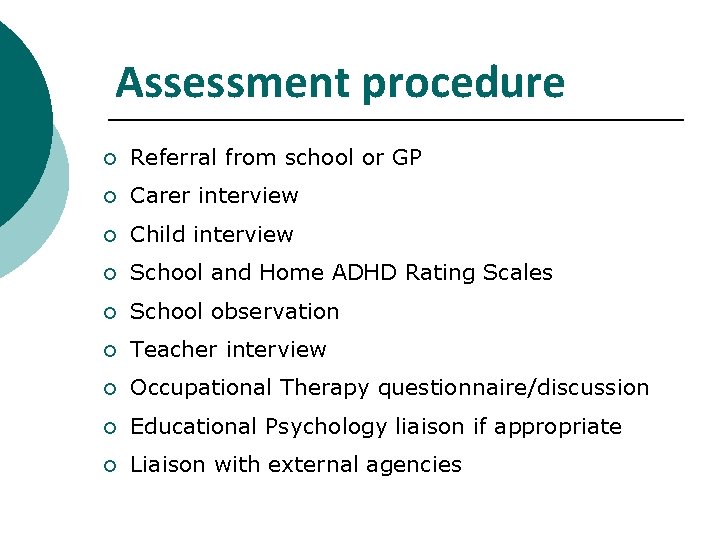
Assessment procedure ¡ Referral from school or GP ¡ Carer interview ¡ Child interview ¡ School and Home ADHD Rating Scales ¡ School observation ¡ Teacher interview ¡ Occupational Therapy questionnaire/discussion ¡ Educational Psychology liaison if appropriate ¡ Liaison with external agencies
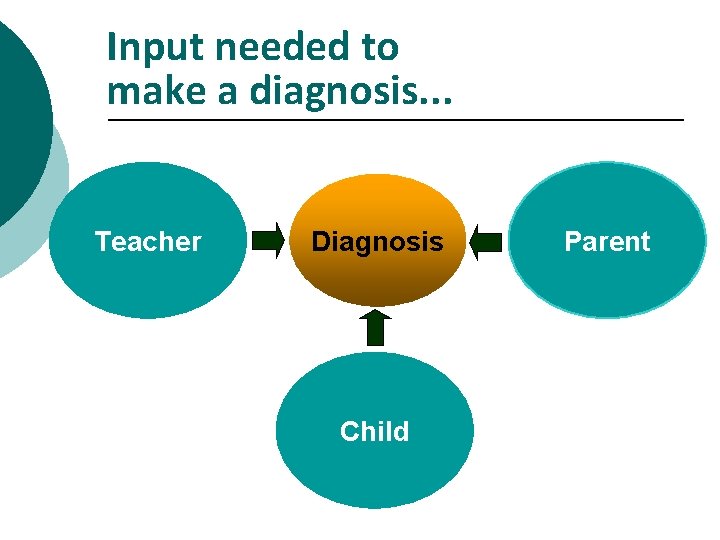
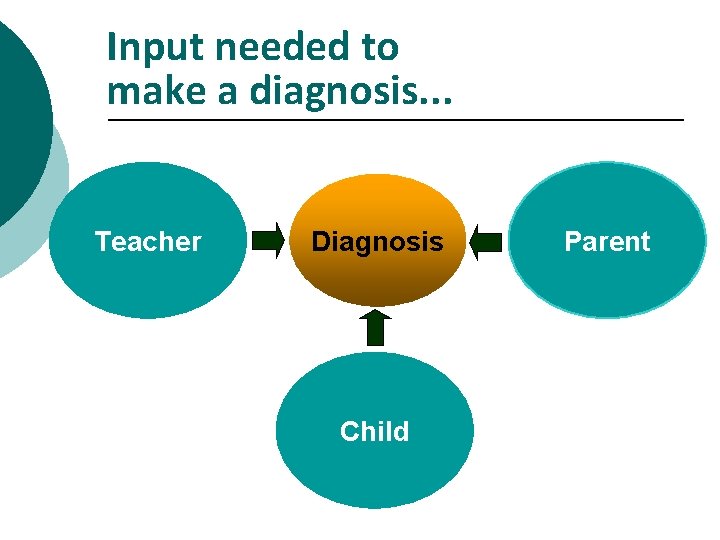
Input needed to make a diagnosis. . . Teacher Diagnosis Child Parent
Aetiology ¡ NICE Guideline 2008 p 30 ¡ “… the presence of psychosocial adversity risk factors should not exclude a diagnosis of ADHD. The aetiology of ADHD involves the interplay of multiple genetic and environmental factors. ADHD is viewed as a heterogenous disorder with different sub-types resulting from different combinations of risk factors acting together. ”
Risk factors for ADHD? ¡ ¡ ¡ Strong genetic influences No single gene has been identified in ADHD Approximately 75% of cases of ADHD appear to have genetic links
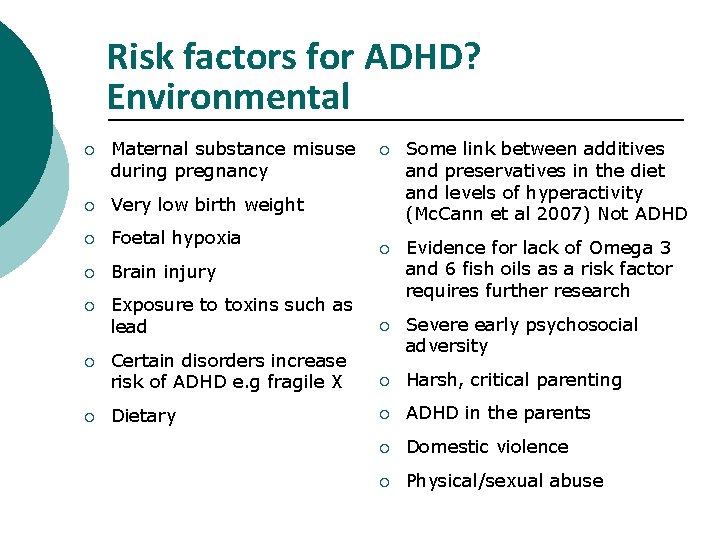
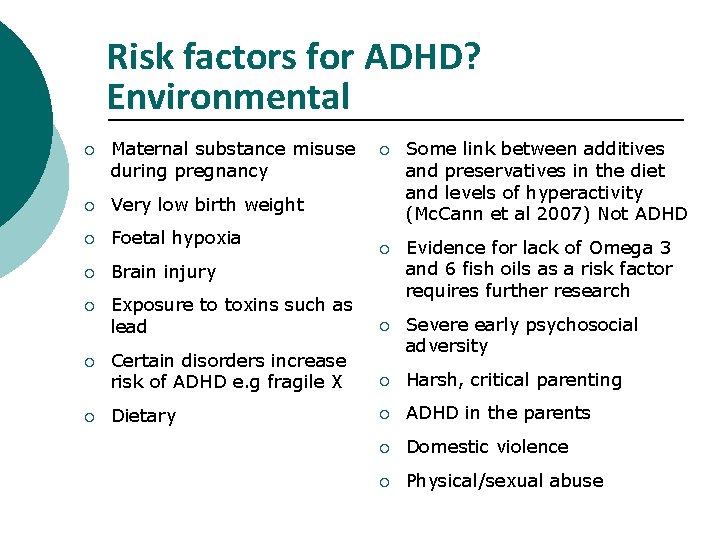
Risk factors for ADHD? Environmental ¡ Maternal substance misuse during pregnancy ¡ Very low birth weight ¡ Foetal hypoxia ¡ Brain injury ¡ ¡ Some link between additives and preservatives in the diet and levels of hyperactivity (Mc. Cann et al 2007) Not ADHD ¡ Exposure to toxins such as lead Evidence for lack of Omega 3 and 6 fish oils as a risk factor requires further research ¡ Certain disorders increase risk of ADHD e. g fragile X Severe early psychosocial adversity ¡ Harsh, critical parenting Dietary ¡ ADHD in the parents ¡ Domestic violence ¡ Physical/sexual abuse
Video ¡ ‘Kid in the Corner’ ¡ During the break, reflect on the implications of the child’s ADHD for: ¡ ¡ ¡ The child The parents Siblings COFFEE BREAK!
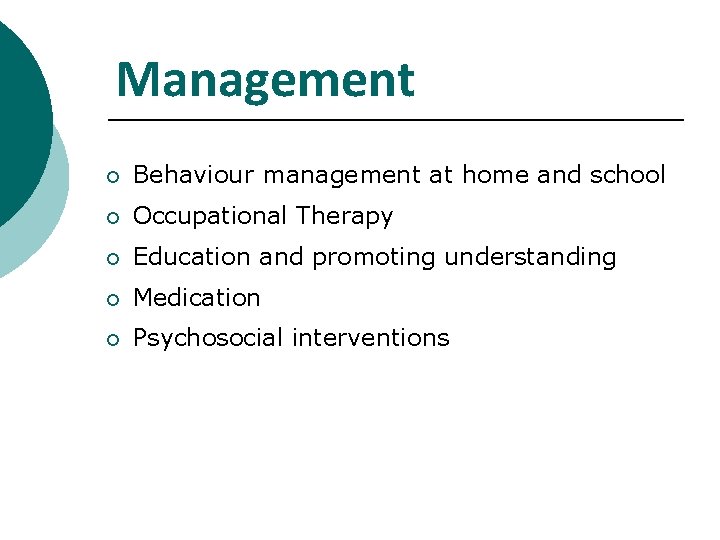
Management ¡ Behaviour management at home and school ¡ Occupational Therapy ¡ Education and promoting understanding ¡ Medication ¡ Psychosocial interventions

Top 10 tips….
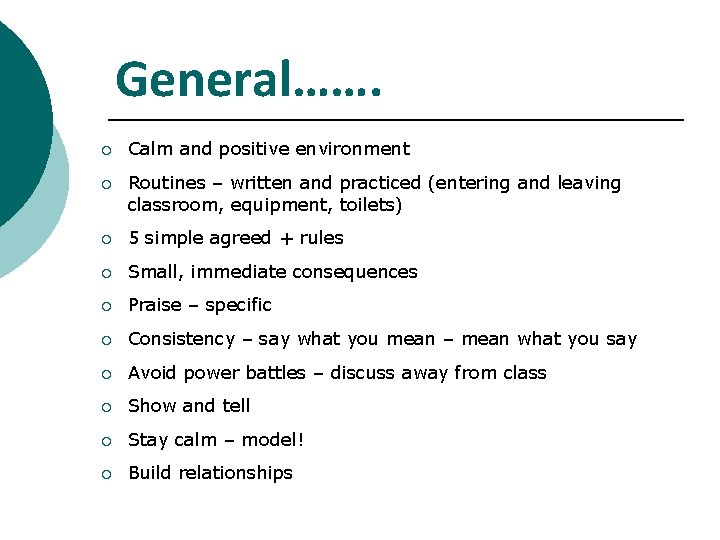
General……. ¡ Calm and positive environment ¡ Routines – written and practiced (entering and leaving classroom, equipment, toilets) ¡ 5 simple agreed + rules ¡ Small, immediate consequences ¡ Praise – specific ¡ Consistency – say what you mean – mean what you say ¡ Avoid power battles – discuss away from class ¡ Show and tell ¡ Stay calm – model! ¡ Build relationships
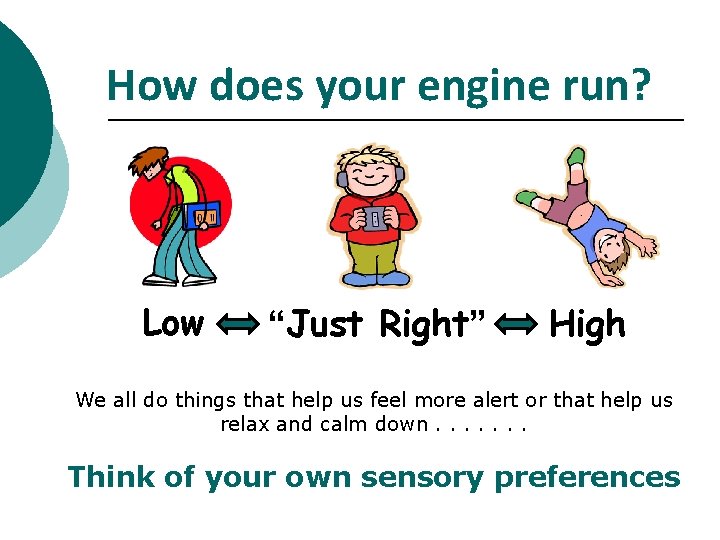
How does your engine run? Low “Just Right” High We all do things that help us feel more alert or that help us relax and calm down. . . . Think of your own sensory preferences
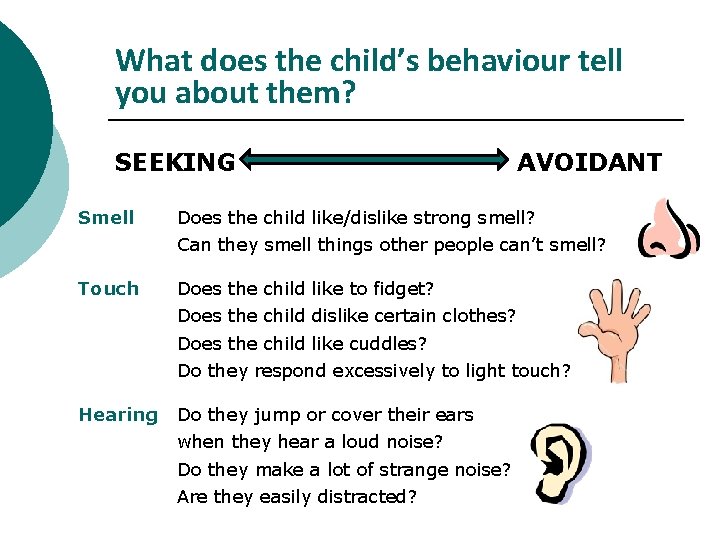
What does the child’s behaviour tell you about them? SEEKING Smell AVOIDANT Does the child like/dislike strong smell? Can they smell things other people can’t smell? Touch Does the child like to fidget? Does the child dislike certain clothes? Does the child like cuddles? Do they respond excessively to light touch? Hearing Do they jump or cover their ears when they hear a loud noise? Do they make a lot of strange noise? Are they easily distracted?
What does the child’s behaviour tell you about them? SEEKING AVOIDANT Movement Does the child find it hard to sit still? Does the child rock on their chair? Do they like or strongly dislike roundabouts/rollercoasters? Do they get travel sick? Taste Does the child have a restricted diet? Does the child like strong tastes, different textured food? Does the child like to chew? Sight Is the child easily distracted by moving objects? Do they notice all movement in the room? Do they like/dislike bright lights?
So what is next? . . . What can we do next? ¡ Provide opportunity for your child to get the sensory experience they like (and that changes their level of alertness) in an appropriate way! Creating a sensory diet ¡ Reduce the sensations they don’t like or that distracts them ¡ Warn your child in advance of any situations which might include a sensory experience they dislike i. e. a loud noise

Top 5 tips….
Classroom Management In three groups come up with TOP FIVE tips for: l Over activity l Impulsiveness l Inattention
Overactivity ¡ Movement breaks ¡ Creative seating ¡ Allowing fidgeting ¡ Stimulus through activity
Impulsivity: Positive Expectations Stop / Start When / Then ¡ ¡ Redirection I need you to. . .
Impulsivity ¡ Visual symbols and non-verbal cues to avoid over use of name ¡ Give them a job ¡ Pick your battles
Inattention ¡ ¡ Use of small post-its between words Breaking tasks down sentence by sentence ¡ Task list on post-its ¡ Half tennis ball under chair leg ¡ Use a cushion ¡ Concentration station
Medication ¡ ¡ Stimulants (Affect Dopamine and Noradrenalin) l Methylphenidate (Ritalin, Equasym, Concerta XL, Equasym XL, Medikinet XL) l Dexamphetamine (Dexedrine) Noradrenergic agents l Atomoxetine (Strattera)
Thank you. . . Any questions?

Reading list: ¡ Atwood, T. ADD. The Parent’s Handbook. ISBN 1860831427. ¡ Barkley RA (1995) Taking charge of ADHD: The complete Authoritative guide for Parents. New York: The Guilford Press. ¡ Brown, T. E (2005) Attention Deficit disorder: The unfocused mind in Children and Adults. Yale: University Press. ¡ Casey, Nigg and Durston (2007) New potential leads in the biology and treatment of attention deficit hyperactivity disorder. Current Opinion In Neurology (20) p 119 -124 ¡ Chu S (2003 a) Attention Deficit Hyperactivity Disorder (ADHD) part one: a review of literature. International Journal of Therapy and Rehabilitation, 10(5), 218 -227.
¡ Dunn W and Bennett D (2002) Patterns of sensory processing in children with attention deficit hyperactivity disorder. The Occupational Therapy Journal of Research, 22(1), 4 -15. ¡ Green C, Chee K. (1997) Understanding ADHD: A Parents Guide to Attention Deficit Hyperactivity Disorder in Children. London: Vermillion. ¡ Goldman LS et al (1998) Diagnosis and treatment of ADHD in Children and Adolescents. JAMA; 279: 1100 -1107. ¡ Hartmann T. (2000) Complete Guide to ADHD. Underwood Books. ¡ “Kid In the Corner” Channel 4
¡ National Institute for Health and Clinical Excellence (NICE) 2006 Guideline on the use of methylphenidate for Attention Deficit Hyperactivity Disorder (ADHD) in Childhood. London: National Institute For Clinical Excellence. ¡ National Institute for Health and Clinical Excellence (NICE) 2008 Attention Deficit Hyperactivity Disorder (Full Guideline). www. nice. org. uk/Guidance/CG 72 ¡ SIGN Guidelines 2009, Number 112 (www. sign. ac. uk/guidelines/fulltext/112/index. html) ¡ Steer C R (2005) Managing attention deficit/hyperactivity disorder: unmet needs and future directions. Archives of Disease in Childhood 90(suppl 1): i 19 -i 25.
References ¡ Tharpar, Langley, Asherson and Gill (2007) geneenvironment interplay in attention-deficit hyperactivity disorder and the importance of a developmental perspective. British Journal of Psychiatry, 190, P 1 -3.