ADHD Beyond the Basics Beth Bloom Emrick MD
ADHD: Beyond the Basics Beth Bloom Emrick, MD, FAAP Developmental Behavioral Pediatrician WV AAP Annual Meeting April 7, 2017
I have no financial interests or relationships to disclose
Objectives • Develop a treatment approach for a child with ADHD • Develop a treatment approach for the child with ADHD who has co-morbidities • Identify nonmedical management options for the child with ADHD
ADHD: The Basics Diagnosis
ADHD: The Basics
ADHD: The Basics • Most common neurobehavioral disorder in children – 8% • Consider the diagnosis in children who have: • Academic or behavioral problems • AND • Symptoms of inattention, hyperactivity, or impulsivity
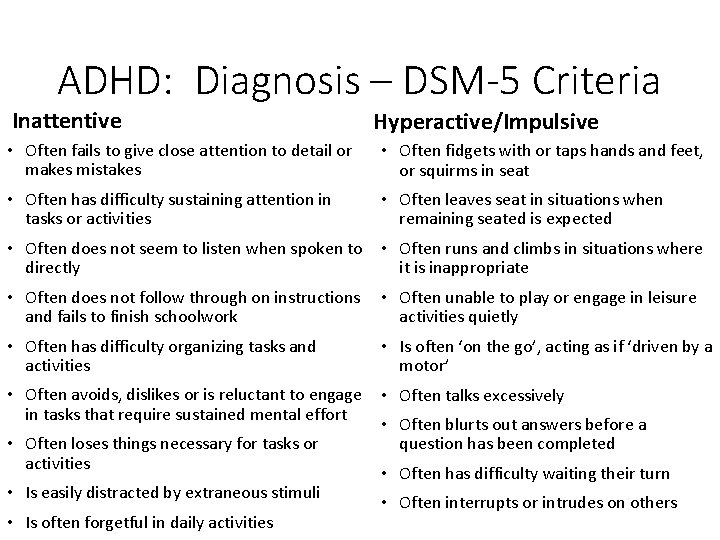
ADHD: Diagnosis – DSM-5 Criteria Inattentive Hyperactive/Impulsive • Often fails to give close attention to detail or makes mistakes • Often fidgets with or taps hands and feet, or squirms in seat • Often has difficulty sustaining attention in tasks or activities • Often leaves seat in situations when remaining seated is expected • Often does not seem to listen when spoken to directly • Often runs and climbs in situations where it is inappropriate • Often does not follow through on instructions and fails to finish schoolwork • Often unable to play or engage in leisure activities quietly • Often has difficulty organizing tasks and activities • Is often ‘on the go’, acting as if ‘driven by a motor’ • Often avoids, dislikes or is reluctant to engage in tasks that require sustained mental effort • Often talks excessively • Often loses things necessary for tasks or activities • Is easily distracted by extraneous stimuli • Is often forgetful in daily activities • Often blurts out answers before a question has been completed • Often has difficulty waiting their turn • Often interrupts or intrudes on others
ADHD: Diagnosis – DSM-5 Criteria • Must be present in 2 or more settings • Must interfere with social, academic, or occupational functioning • “The symptoms do not occur exclusively during the course of schizophrenia or another psychotic disorder and are not better explained by another mental disorder”
ADHD: Diagnosis – DSM-5 Changes • Age of onset • Adolescent/adult criteria


ADHD: Common Coexisting Conditions • Learning problems • Language disorder • Disruptive behavior • Anxiety • Mood disorders • Tic disorders • Seizures • Developmental coordination disorder • Sleep disorders

ADHD: Beyond the Basics

ADHD Case: Abigail • 12 years old, 5 th grade • Did fairly well in school kindergarten through 3 rd grade • No behavior problems • Difficulty with organization • 4 th grade • Worsening difficulty with organization • Struggles completing assignments and turning them in on time • 5 th grade • Harder for her to get her work done • Teacher has to remind her to stay on task • Grades dropping
ADHD Case: Abigail • Sleeps well • No other symptoms – anxiety, depression, etc • Medical history and physical exam normal

ADHD Case: Abigail Vanderbilt Behavior Rating Scales Parent Teacher Inattention 8 of 9 7 of 9 Hyperactivity/Impulsivity 2 of 9 3 of 9 Oppositional Defiant 0 of 8 Conduct Disorder 0 of 15 Anxiety/Depression 0 of 7 Performance Problematic in • All academic areas • Peer relationships • Assignment completion • Organization skills

ADHD Case: Abigail Vanderbilt Behavior Rating Scales Parent Teacher Inattention 8 of 9 7 of 9 Hyperactivity/Impulsivity 2 of 9 3 of 9 Oppositional Defiant 0 of 8 Conduct Disorder 0 of 15 Anxiety/Depression 0 of 7 Performance Problematic in • All academic areas • Peer relationships • Assignment completion • Organization skills
ADHD Case: Treatment Options • Medication • Behavior Therapy • Classroom Management
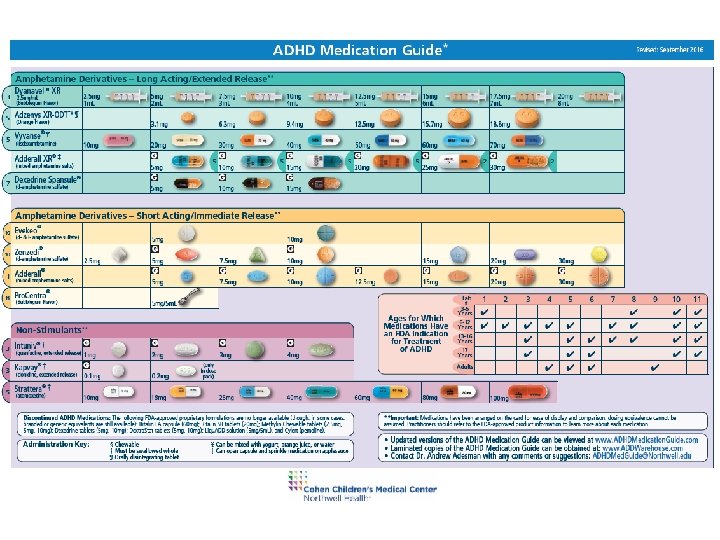
Starting ADHD Medications: Factors to Consider • Swallow pills? • Delivery system • • • Capsule Beads Liquid – flavor ODT Duration of action Dosing schedule Preferred drug list Cost Adverse effects Family preference
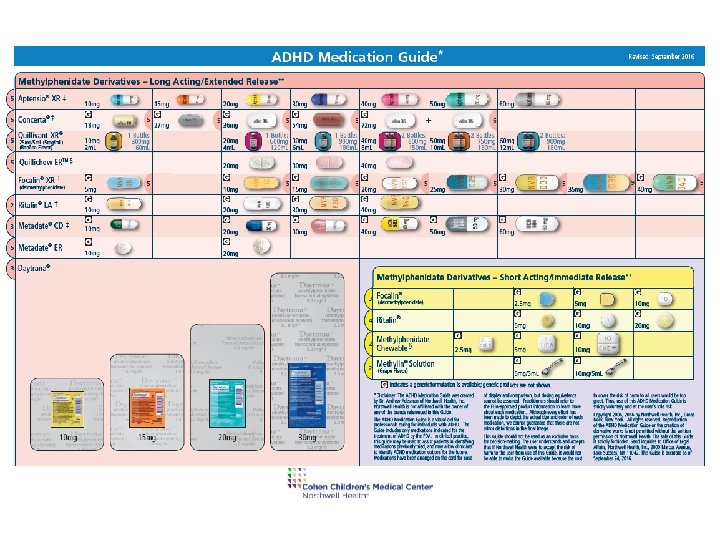
ADHD Medications: Methylphenidates • Titration • Increase 5 -10 mg/day every 1 -2 weeks if limited benefits and no adverse effects • Can add short acting afternoon dose if needed • To short acting BID dosing • To long acting qam dosing
ADHD Medications: Methylphenidates • Other considerations: • Many long acting forms can be opened and sprinkled on applesauce or pudding • Metadate CD®, Ritalin LA®, Focalin XR®, Aptensio XR® • Concerta® capsule cannot be opened due to delivery system • Daytrana® • Patch is applied at the hip; may cause skin irritation • Quillivant XR® is an extended release liquid preparation • Quillichew ERTM is an extended release chewable
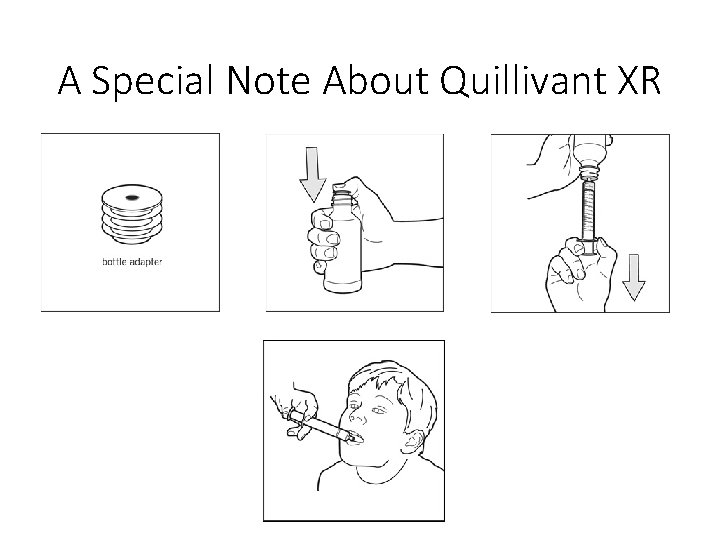
A Special Note About Quillivant XR
ADHD Medications: Amphetamines • Amphetamine titration • Increase 5 -10 mg/day every 1 -2 weeks if limited benefits and no adverse effects • Can add short acting afternoon dose if needed • To short acting BID dosing • To long acting qam dosing
ADHD Medications: Amphetamines • Other considerations: • Adderall XR® and Dexedrine spansule® can be opened and sprinkled • Vyvanse® capsule can be opened and contents dissolved in small amount of water (1 -2 tsp) • Vyvanse® may have decreased abuse potential due to pro-drug delivery system • Dyanavel XRTM is an extended release liquid preparation • Adzenys XR-ODTTM is an extended release oral dissolvable tablet
ADHD Medications: Stimulants • Contraindication • Mania • Psychosis • Precautions • • Anxiety Parental substance abuse Tics? Seizures?
ADHD Medications: Stimulants • Adverse event monitoring • • Aggression Irritability Social withdrawal Hypertension, tachycardia Appetite suppression Sleep disturbance Exacerbation of Tics?
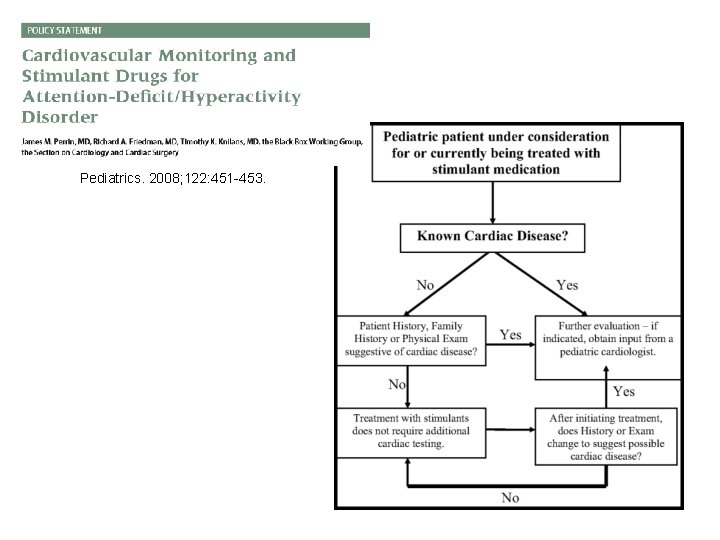
Pediatrics. 2008; 122: 451 -453.
ADHD Medications: Common Stimulant Pitfalls • “Abigail gets really emotional at the end of the day. It’s worse than when she’s not on medicine. ” • Manage rebound symptoms: • Behavioral intervention • Long acting formulations • Small dose of short acting medication in the afternoon
ADHD Medications: Common Stimulant Pitfalls • Abigail’s mother expresses frustration about dose changes. • “It feels like you’re just experimenting…” • Advise parents at the onset of treatment about medication titration
ADHD Medications: Common Stimulant Pitfalls • “Abigail’s medication is working well but she isn’t eating much. What can we do? ” • Switch to another formulation • Encourage high calorie, healthy foods and afternoon/evening snacks • Consider weekend breaks for stimulants (if clinically appropriate) • Review other considerations for weight loss
ADHD Medications: Atomoxetine • Mechanism of action • Selective norepinephrine reuptake inhibitor • May take up to 12 weeks for full effect
ADHD Medications: Atomoxetine • Other considerations: • • Pills cannot be opened or split Can divide dose BID to minimize side effects Must give daily Dose adjustment in patients with impaired liver function
ADHD Medications: Alpha-agonists • Mechanism of action • Theoretically acts on post-synaptic receptors in the prefrontal cortex • Other considerations • Sedation: Clonidine >> Guanfacine • Rebound hypertension may occur if dose stopped abruptly • Pills cannot be opened or split Stahl SM. The Prescriber’s Guide. 3 rd ed. New York, NY: Cambridge Press; 2009: 103 -104, 233 -235.
ADHD Medications: Alpha-agonists • Dosing • Guanfacine ER (Intuniv®) • Long acting: start at 1 mg qd • Increase weekly to 4 mg maximum dose • Clonidine ER (Kapvay®) • Long acting: start at 0. 1 mg q. HS • Increase weekly by 0. 1 mg divided BID to 0. 4 mg/day maximum dose
ADHD Medications • Atomoxetine • • • Norepinephrine reuptake inhibitor Suicidal ideation Hypertension, tachycardia GI upset Behavioral activation • Alpha-agonists • Hypotension, bradycardia • Sedation
ADHD and Comorbidities • Screening • History • Tools • SCARED - Self-Report for Childhood Anxiety Related Disorders • Center for Epidemiological Studies Depression Scale for Children (CES-DC) • Patient Health Questionnaire – 9 (PHQ-9)
ADHD and Comorbidities • Which one do you treat first? • Will treatment of one worsen the other?
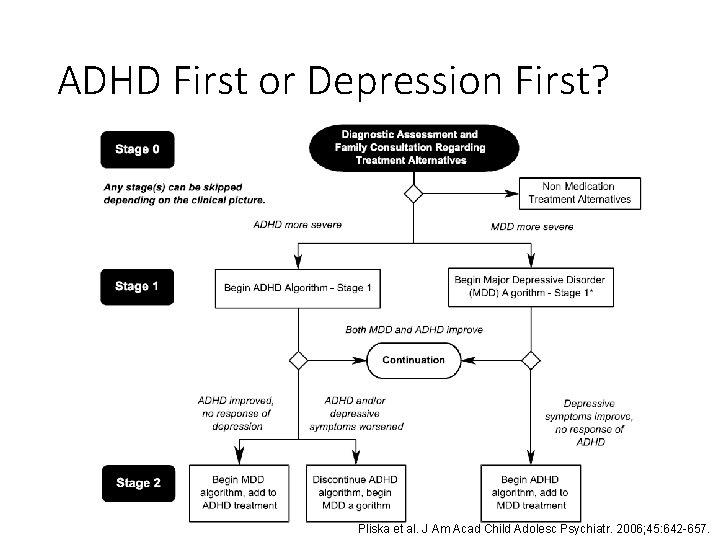
ADHD First or Depression First? Pliska et al. J Am Acad Child Adolesc Psychiatr. 2006; 45: 642 -657.
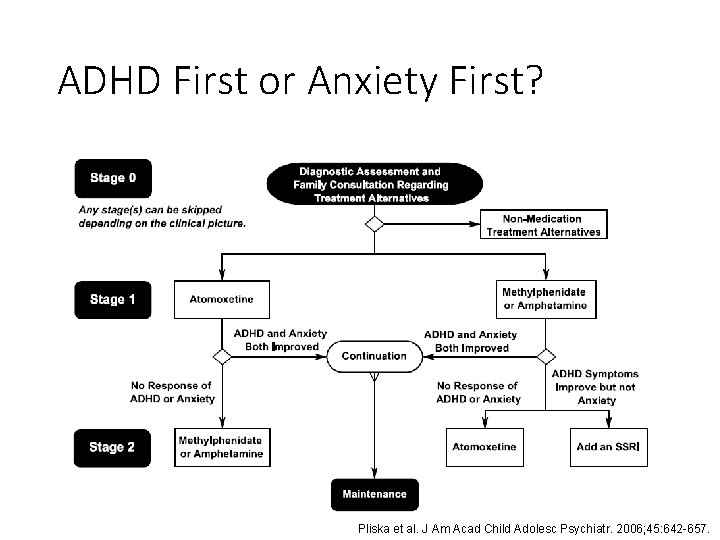
ADHD First or Anxiety First? Pliska et al. J Am Acad Child Adolesc Psychiatr. 2006; 45: 642 -657.
ADHD and Comorbidities • Initial management of ADHD does not change • Doses are the same • Consider Cognitive Behavioral Therapy • May end up needing >1 medication to treat both
What if anxiety gets worse with stimulants? • No real benefit for attention and focus!! • More irritable and intense rebound! • Trial of a different ADHD medication • Stimulant vs. non-stimulant • Cognitive Behavioral Therapy
ADHD and Comorbidities • “I noticed Abigail is having tics. They may have been there before she started Concerta®. What should we do? ” • Consider the severity of the tics • • • Continue stimulant Change stimulant class Change to non-stimulant Add alpha-agonist Cognitive Behavioral Intervention for Tics (CBIT) Pliska et al. J Am Acad Child Adolesc Psychiatr. 2006; 45: 642 -657.
ADHD: Behavioral Interventions for Parents • Goal: Train the parents in techniques • Improve their ability to shape child’s behavior • Improve child’s ability to regulate own behavior • Positive reinforcement • Planned ignoring • Appropriate consequences • Gradually increase expectations as tasks are mastered
ADHD: Behavioral Interventions in the Classroom • Clear, simple rules and expectations • Predictability of events and activities through establishing routines • Cues and signals about transitions and changes • Frequent use of praise • Seating arrangements • Brisk pace of instruction • Sequence of activities
ADHD: Child-specific accommodations • Preferential seating • Modified assignments • Test modifications • Cues for staying on task • Assignment notebook that teacher checks • Positive behavior plan with reward system • Using a timer • Written and oral directions • Have student repeat instructions
Summary • Consider the risks and benefits of medication • Discuss openly with patients and families • Develop a process for monitoring • Medications can be an effective component of a comprehensive treatment plan
Resources • www. chadd. org • www. additudemag. com • www. timemanagement. org • Center for Mental Health Services in Pediatric Primary Care • http: //web. jhu. edu/pedmentalhealth/ • A Guide to Psychopharmacology for Pediatricians • http: //web. jhu. edu/pedmentalhealth/Psychopharmacolog%20 use. html
References • American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with Attention-Deficit Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatr. 2007; 46: 894 -921. • American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with oppositional defiant disorder. J Am Acad Child Adolesc Psychiatr. 2007; 46: 126 -141. • Cheung AH, Zuckerbrot RA, Jensen PS et al. Guidelines for the Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and Ongoing Management. Pediatrics. 2007; 120: e 1313 -e 326. • Gibbons RD, Brown CH, Hur K, et al. Early Evidence on the Effects of Regulators’ Suicidality Warnings on SSRI Prescriptions and Suicide in Children and Adolescents. Am J Psychiatry 2007; 164: 1356– 1363. • Hammad TA. Review and evaluation of clinical data. Washington, DC, Food and Drug Administration, Aug 16, 2004 (http: //www. fda. gov/ohrms/dockets/ac/04/briefing/2004 -4065 b 1 -10 -TAB 08 -Hammads-Review. pdf ). Accessed October 22, 2012. • Pappadopulos E, Mac. Intyre JC, Crismon ML et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. J Am Acad Child Adolesc Psychiatr. 2003; 42: 145 -161. • Pliszka SR, Crismon ML, Hughes CW, et al. The Texas Children’s Medication Algorithm Project: Revision of the algorithm for pharmacotherapy of Attention-Deficit-Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatr. 2006; 46: 642 -657. • Subcommittee on Attention-Deficit/Hyperactivity Disorder and the Committee on Quality Improvement. Clinical practice guideline: treatment of the school-aged child with Attention-Deficit/Hyperactivity Disorder. Pediatrics. 2001; 108(4): 10331044. • Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of Attention. Deficit/Hyperactivity Disorder in children and adolescents. Pediatrics. 2011; 128: 1007 -1022. • Practice Parameter for the Assessment and Treatment of Children and Adolescents with Oppositional Defiant Disorder. J. American Academy of Child and Adolescent Psychiatry. 2007; 46(1): 126 -141
- Slides: 50