ADDRESSING RACIAL ETHNIC HEALTH INEQUITIES THE ROLE OF



- Slides: 52
ADDRESSING RACIAL & ETHNIC HEALTH INEQUITIES: THE ROLE OF PUBLIC HEALTH SOCIAL WORK
Learning Objectives • Grasp the significance of racial and ethnic health disparities and inequities • Understand why social work and public health social work (PHSW) practitioners need to address health disparities and inequities • Define key terms and their meanings related to health disparities, health equity and social determinants of health • Utilize key resources and readings to enhance knowledge on this content • Understand possible strategies for PHSW to address racial and ethnic disparities/inequities • Apply knowledge of PHSW in actual racial and ethnic disparities/inequities
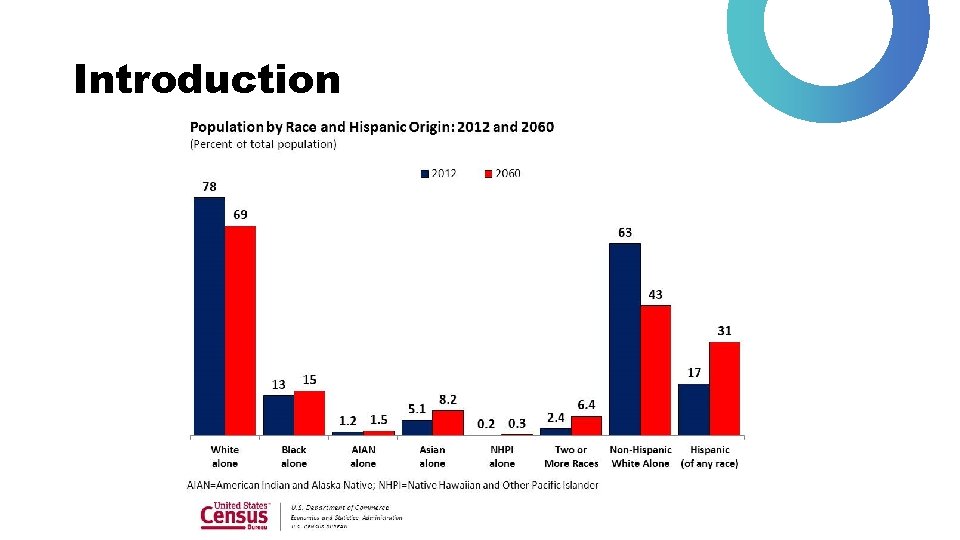
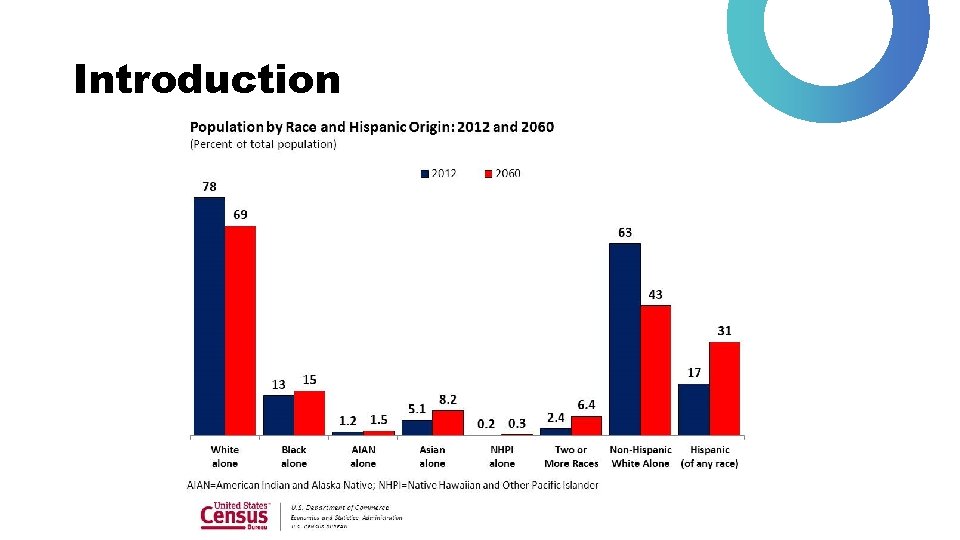
Introduction
Why Focus on Racial and Ethnic Health Disparities and Inequities • Race and ethnicity intersect with other key factors to produce inequities, including (but not limited to): • socioeconomic status, • geographic location, • immigration status and nationality • When studying health, many roads lead back to race and ethnicity • This does not mean other disparate groups based on sexual orientation, gender, homelessness, or disability status are less important, but that focus on race/ethnicity is a critical focus
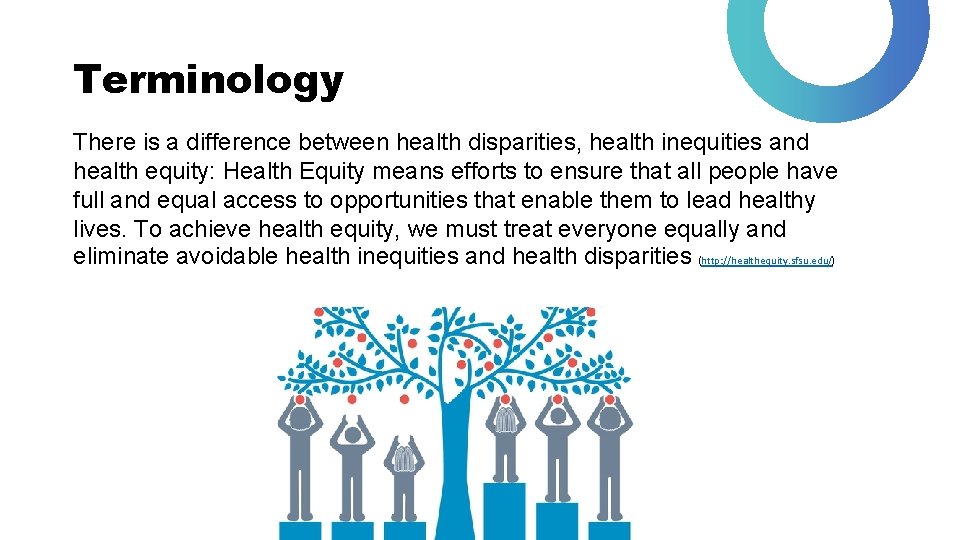
Terminology There is a difference between health disparities, health inequities and health equity: Health Equity means efforts to ensure that all people have full and equal access to opportunities that enable them to lead healthy lives. To achieve health equity, we must treat everyone equally and eliminate avoidable health inequities and health disparities (http: //healthequity. sfsu. edu/)

What is a Health Disparity? • A higher burden of illness, injury, disability or mortality experienced by one population group relative to another. • Differences between population groups in health insurance coverage, access to and use of care, quality of care. • Not all health disparities are unjust – some are just a part of life!
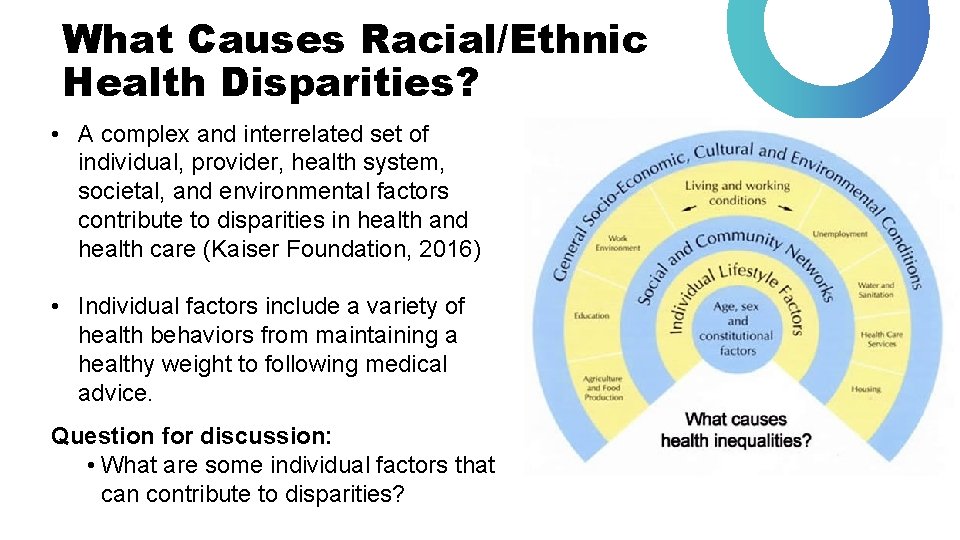
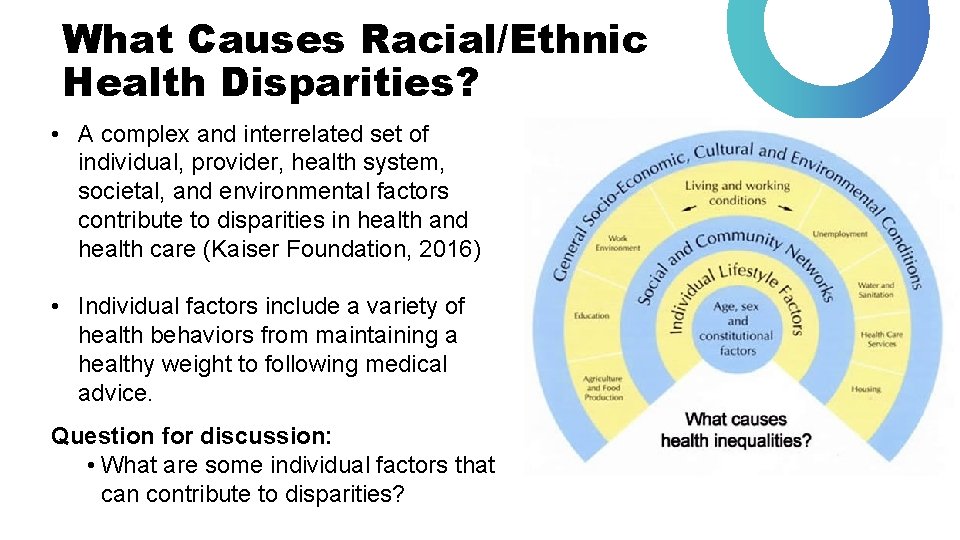
What Causes Racial/Ethnic Health Disparities? • A complex and interrelated set of individual, provider, health system, societal, and environmental factors contribute to disparities in health and health care (Kaiser Foundation, 2016) • Individual factors include a variety of health behaviors from maintaining a healthy weight to following medical advice. Question for discussion: • What are some individual factors that can contribute to disparities?
Provider Factors Provider bias and cultural/linguistic differences are another potential cause of racial/ethnic disparities: • Bias (or prejudice) against minorities • Greater clinical uncertainty when interacting with minority patients • Beliefs (or stereotypes) held by the provider about the behavior or health of minorities

Question: Provider Factors How might patient-provider communication impact care?
Systemic Factors That Contribute to Health Disparities • How health care is organized, financed, and delivered, including lack of access to care, inability to make it to appointments, high deductibles/copays, affects health outcomes and can produce disparities and differences in health outcomes among groups of people. • Social and environmental factors, such as poverty, education, proximity to care, lack of childcare, work considerations, and neighborhood safety affect ability to utilize health care system. Question for discussion: what are some other systemic factors that affect people you work with?
Relationship to Social Determinants of Health • Social determinants of health (SDOH) are systemic factors which affect health outcomes, defined as: “the circumstances in which people are born, grow up, live, work, and age. This also includes the systems in place to offer health care and services to a community. These circumstances are in turn shaped by a wider set of forces: economics, social policies, and politics. (Social Determinants of Health Key Concepts External, World Health Organization). • SDOH affect racial and ethnic groups through the following: poverty, inadequate housing, structural racism/discrimination, poor socioeconomic opportunities, food insecurity, quality of education, exposure to crime & violence, social norms and attitudes (e. g. discriminatory attitudes)
Summary of Disparities and Examples • Health disparities can be seen as persistent differences in health conditions and illness rates that cut across many illness categories and demographic groups • Disparities exist in different contexts and are rooted in the discriminatory and inequitable distribution of healthcare resources (Smedley et al. , 2003)
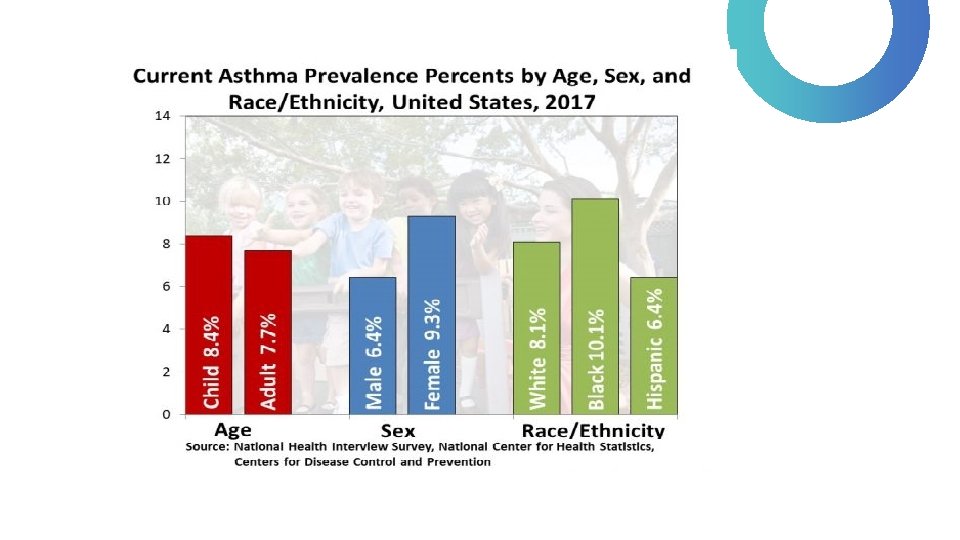
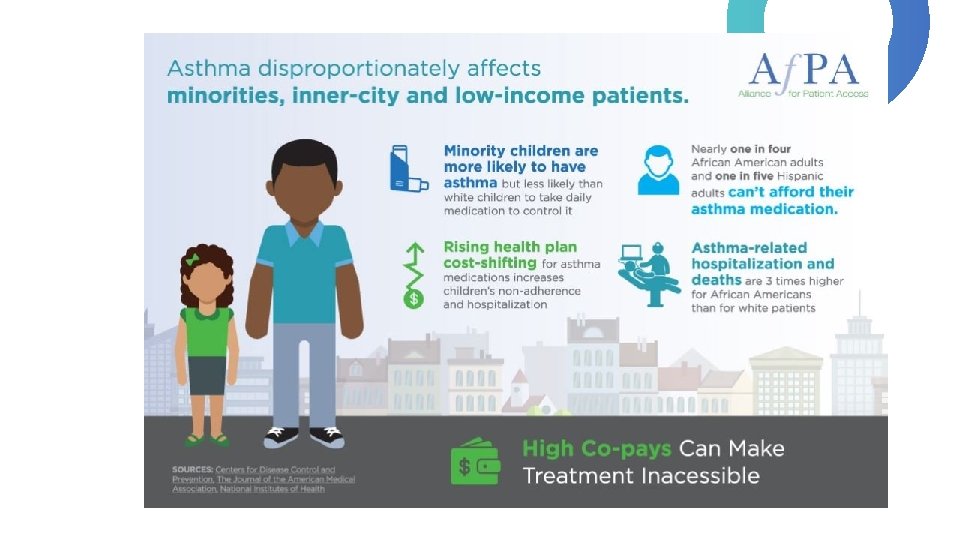
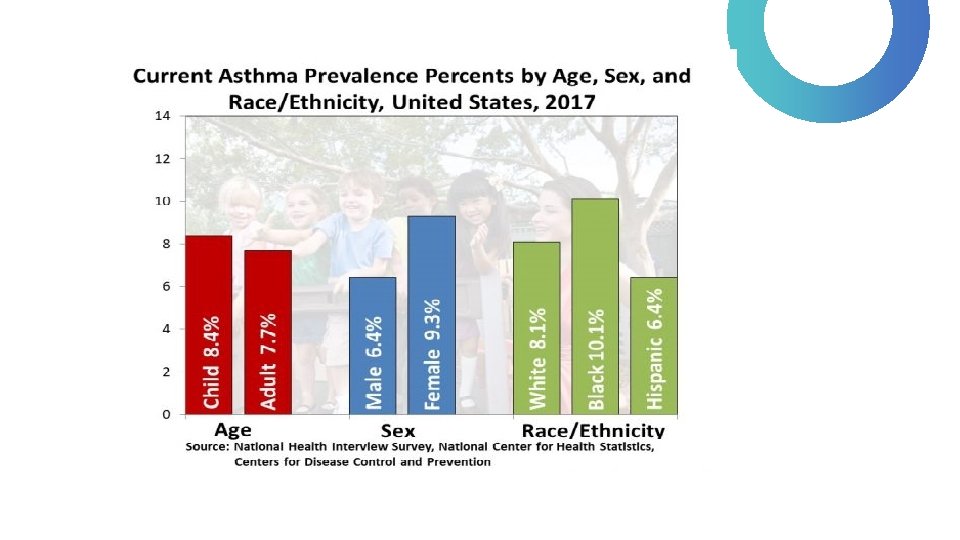
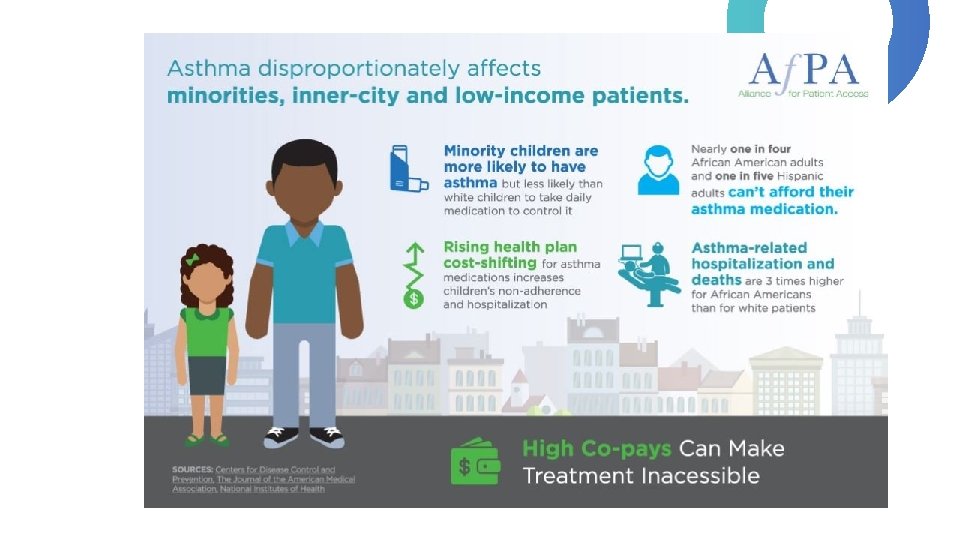
Example #1 African American children are more likely to die from asthma compared to non-Hispanic White children. Questions for discussion: • Why do we think this is? • What are possible individual factors? • What are possible provider factors? • What are possible systemic factors? • How can social work help?
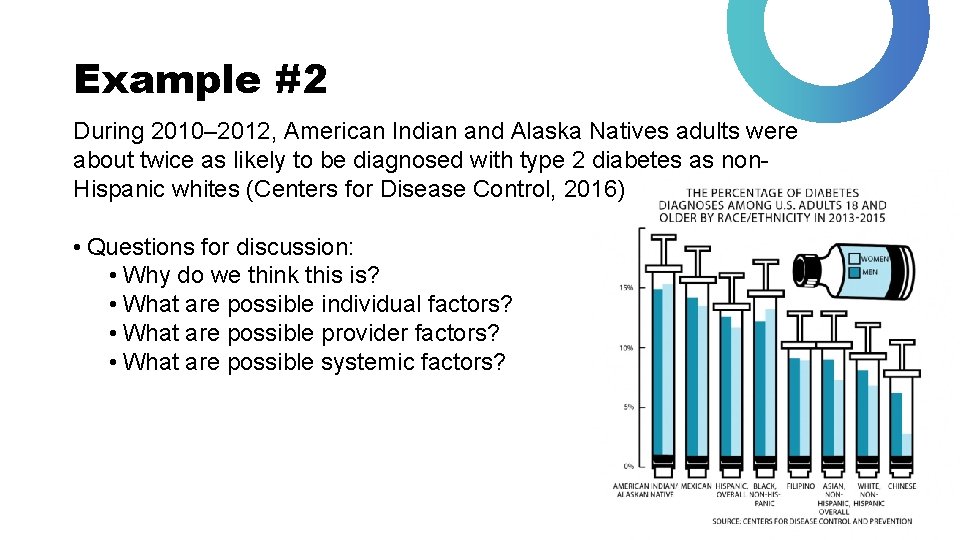
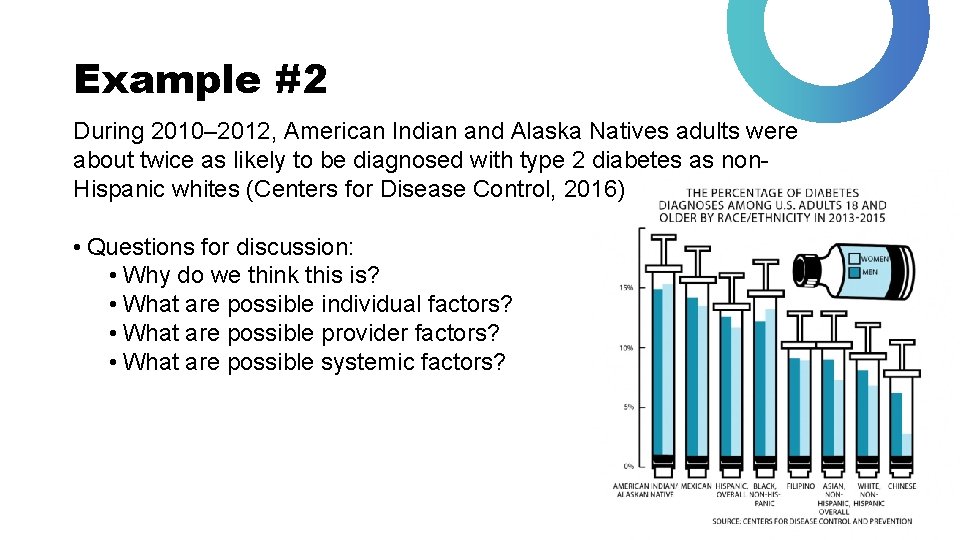
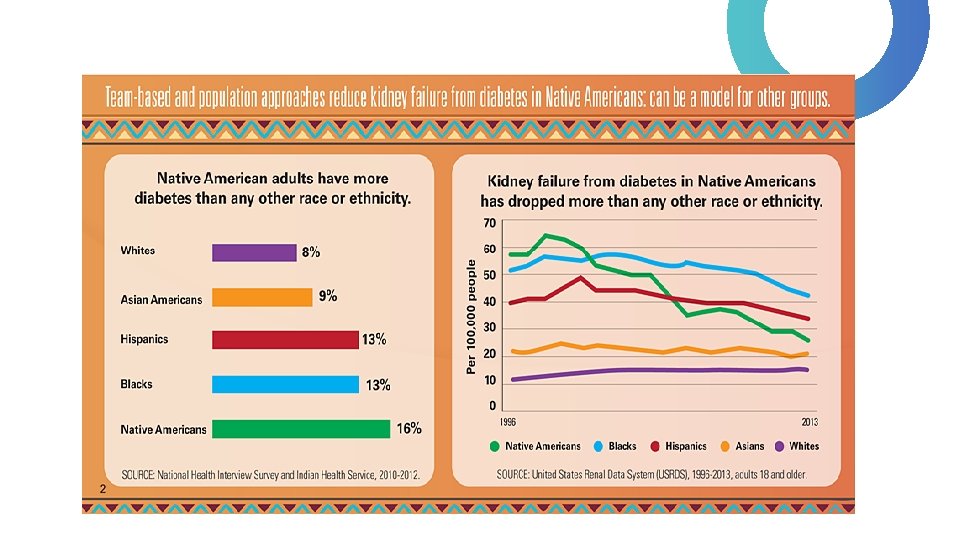
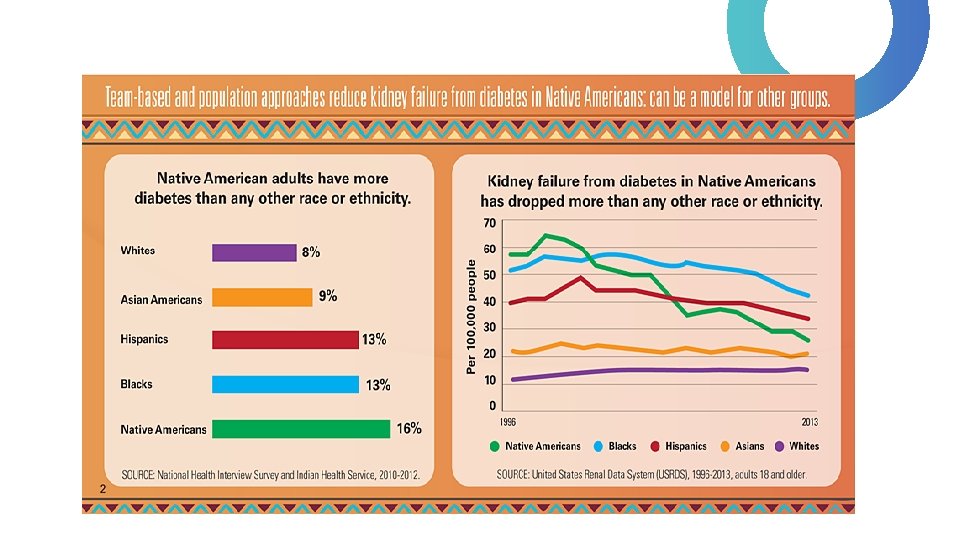
Example #2 During 2010– 2012, American Indian and Alaska Natives adults were about twice as likely to be diagnosed with type 2 diabetes as non. Hispanic whites (Centers for Disease Control, 2016) • Questions for discussion: • Why do we think this is? • What are possible individual factors? • What are possible provider factors? • What are possible systemic factors?
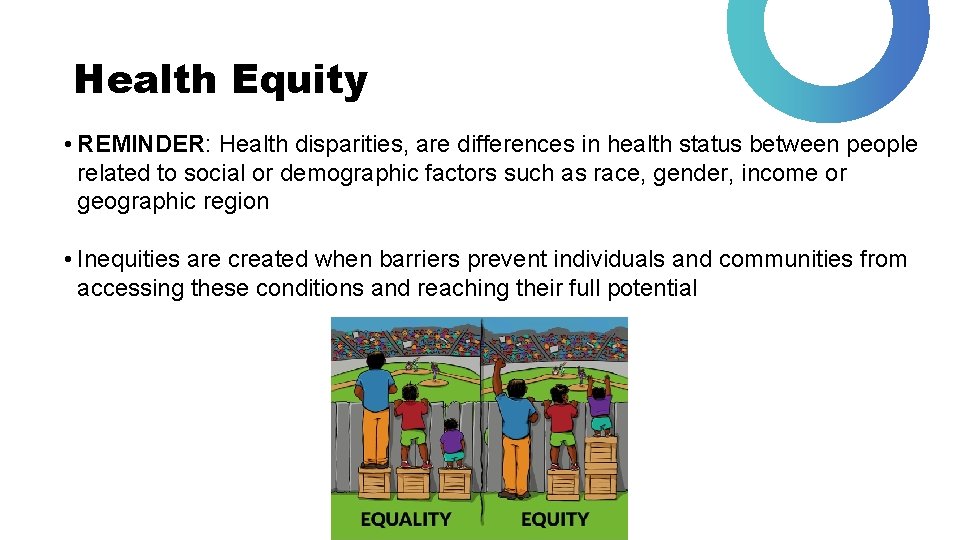
Health Equity • REMINDER: Health disparities, are differences in health status between people related to social or demographic factors such as race, gender, income or geographic region • Inequities are created when barriers prevent individuals and communities from accessing these conditions and reaching their full potential
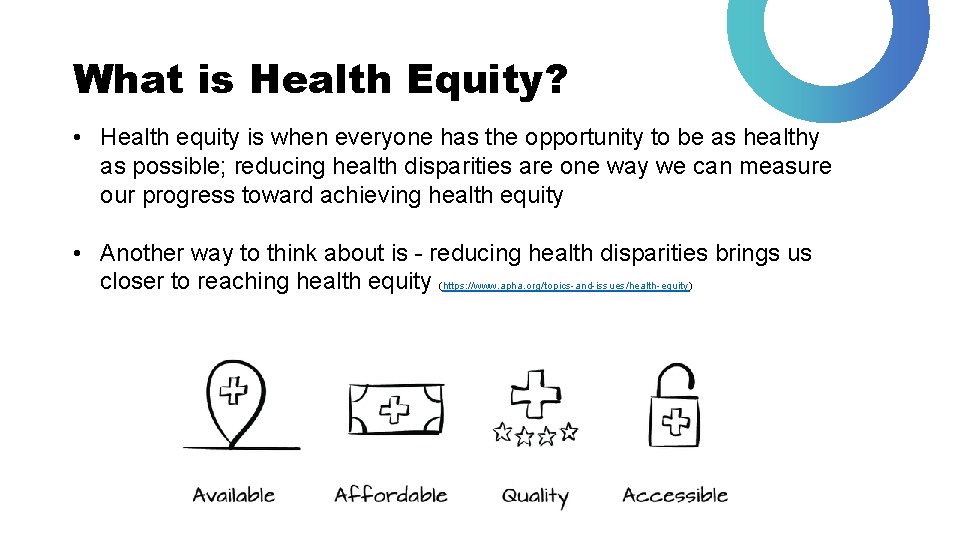
What is Health Equity? • Health equity is when everyone has the opportunity to be as healthy as possible; reducing health disparities are one way we can measure our progress toward achieving health equity • Another way to think about is - reducing health disparities brings us closer to reaching health equity (https: //www. apha. org/topics-and-issues/health-equity)
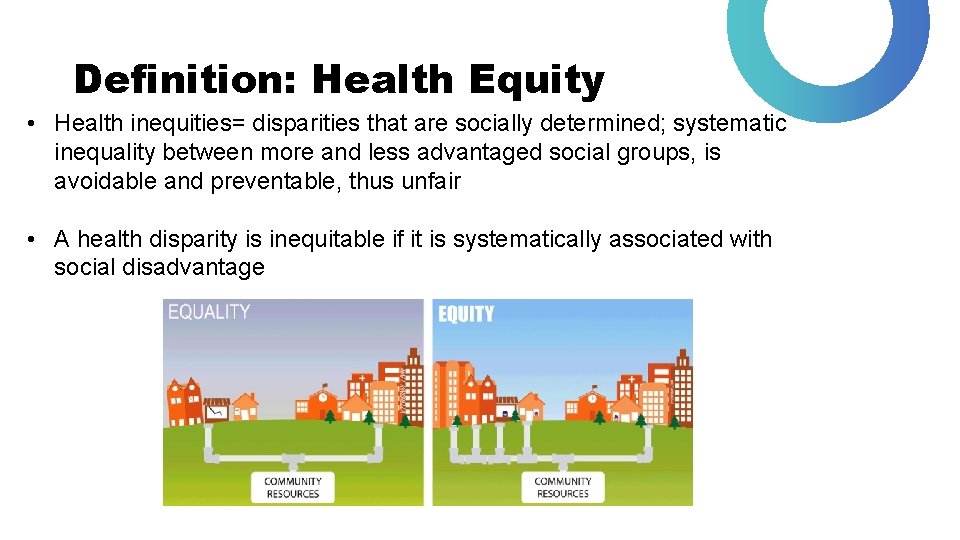
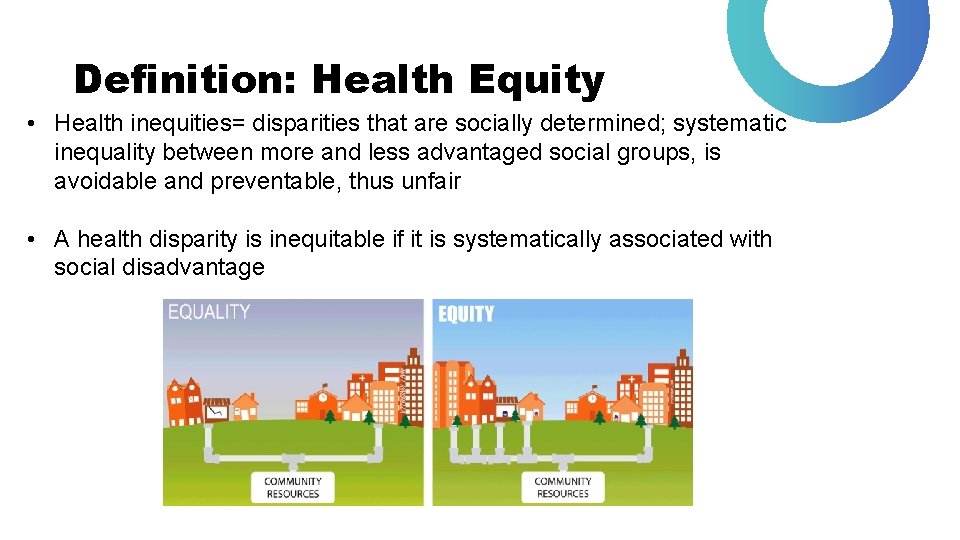
Definition: Health Equity • Health inequities= disparities that are socially determined; systematic inequality between more and less advantaged social groups, is avoidable and preventable, thus unfair • A health disparity is inequitable if it is systematically associated with social disadvantage
Statement by American Public Health Association • “By health equity, we mean everyone has the opportunity to attain their highest level of health. Inequities are created when barriers prevent individuals and communities from accessing these conditions and reaching their full potential. Inequities differ from health disparities, which are differences in health status between people related to social or demographic factors such as race, gender, income or geographic region. Health disparities are one way we can measure our progress toward achieving health equity. • How do we achieve health equity? We value all people equally. We optimize the conditions in which people are born, grow, live, work, learn and age. We work with other sectors to address the factors that influence health, including employment, housing, education, health care, public safety and food access. 1 We name racism as a force in determining how these social determinants are distributed. ”
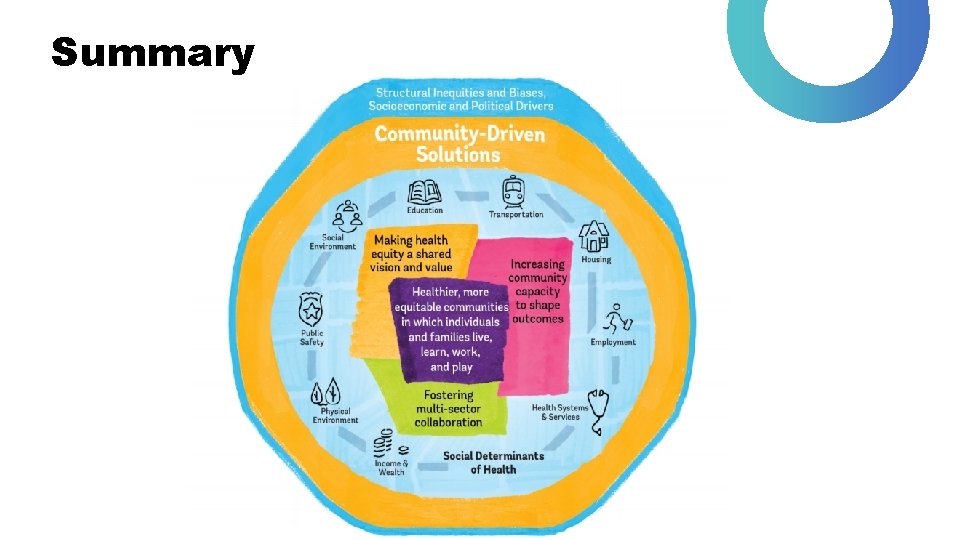
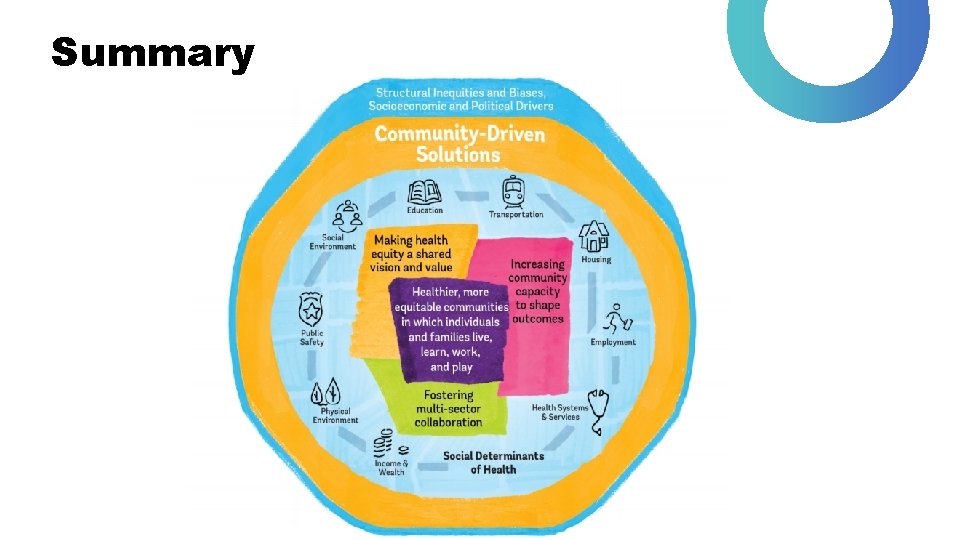
Summary
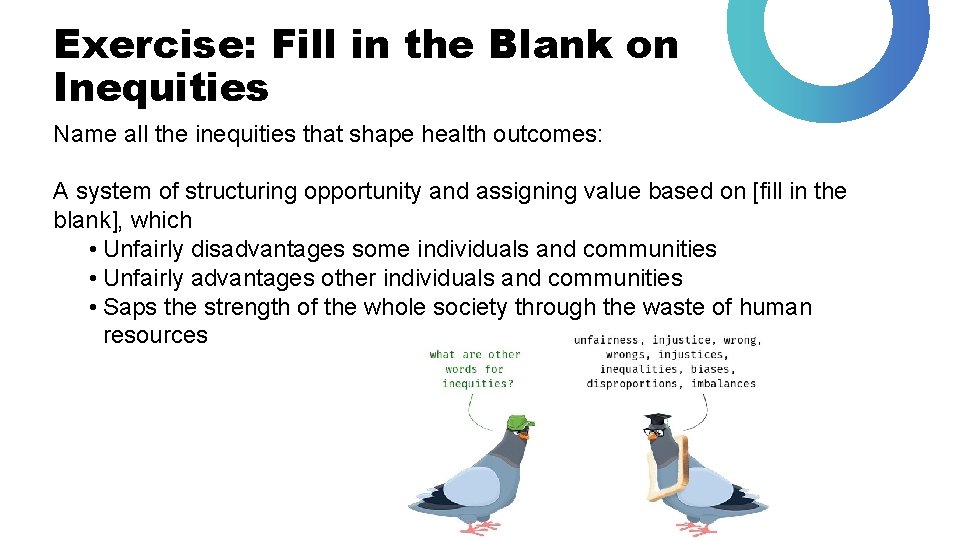
Exercise: Fill in the Blank on Inequities Name all the inequities that shape health outcomes: A system of structuring opportunity and assigning value based on [fill in the blank], which • Unfairly disadvantages some individuals and communities • Unfairly advantages other individuals and communities • Saps the strength of the whole society through the waste of human resources
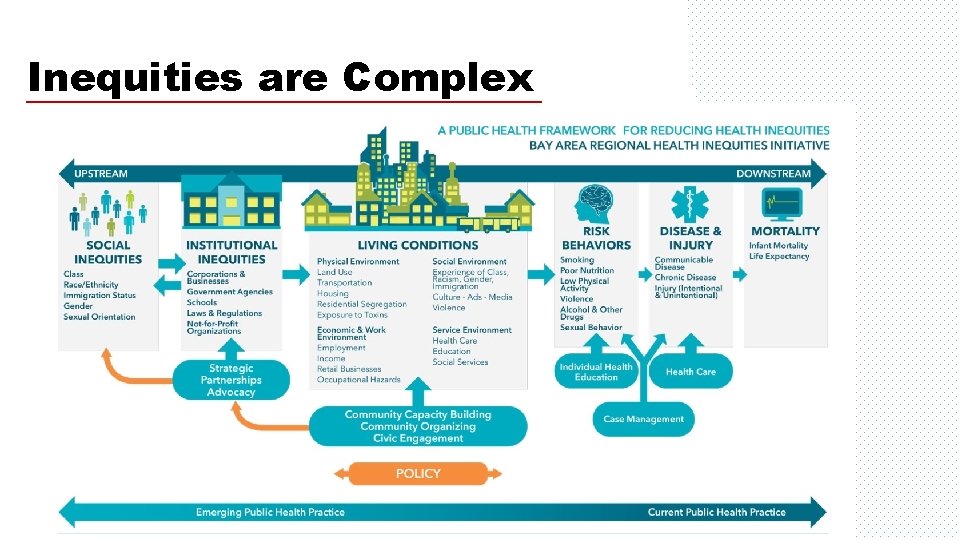
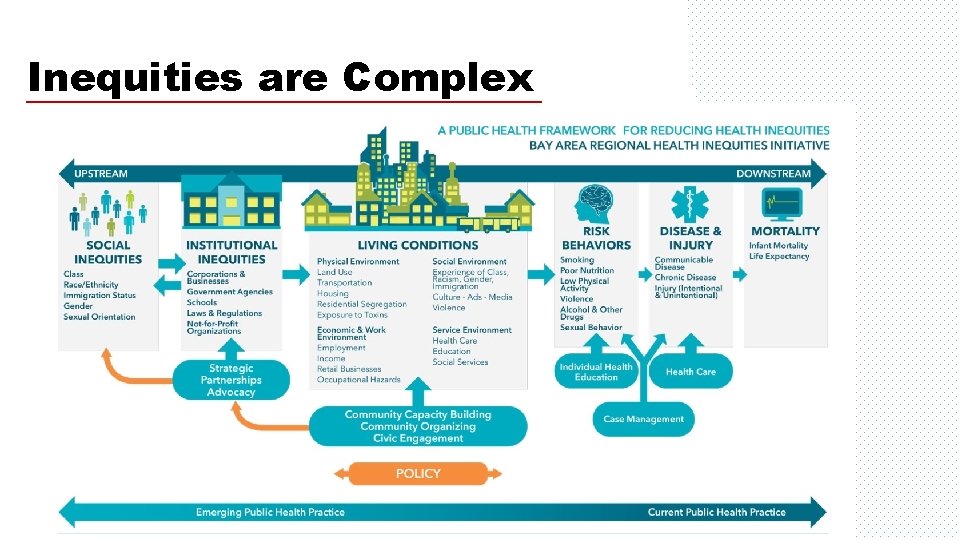
Inequities are Complex
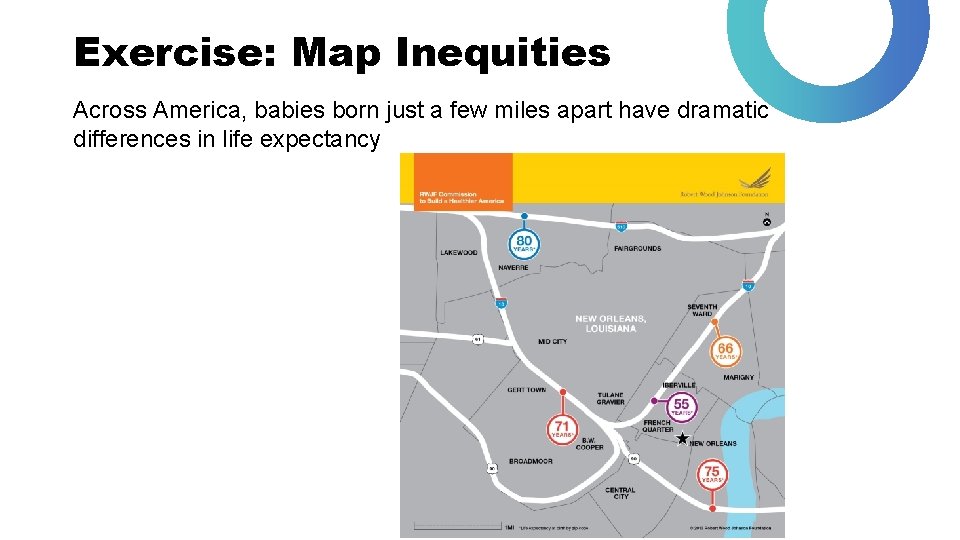
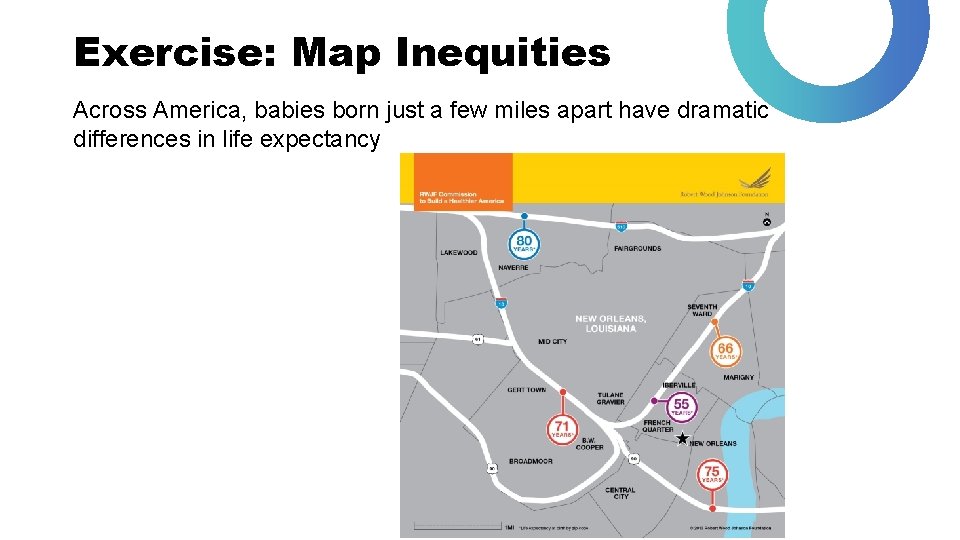
Exercise: Map Inequities Across America, babies born just a few miles apart have dramatic differences in life expectancy
Return to the Question: “Why Focus on Race and Ethnicity? ” • Racial/ethnic inequities are widespread, longstanding, and profound. • Blacks and Hispanics are more likely to experience poverty, low educational levels, poor neighborhood conditions. • Example: African Americans are far more likely than whites to experience the following hardships, even after adjusting for income, education, employment status, transfer payments, home ownership, gender, marital status, children, disability, health insurance and residential mobility: Inability to meet essential expenses, unable to pay full rent on mortgage, unable to pay full utility bill, more likely to have utilities shut off, more likely to experience eviction
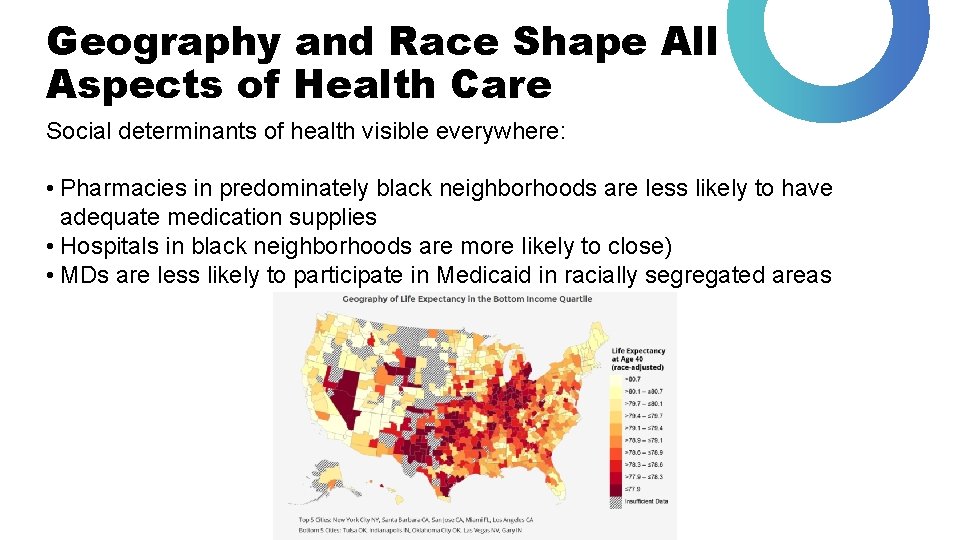
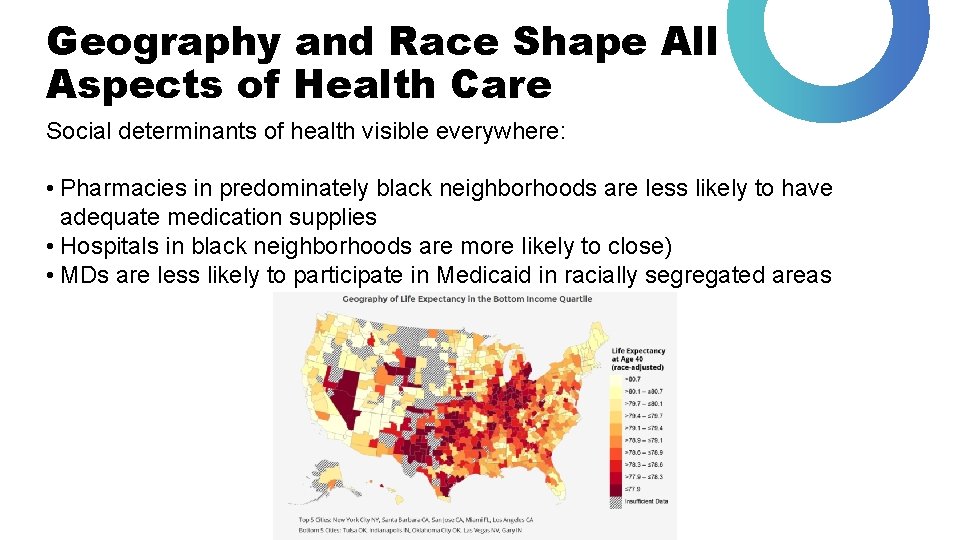
Geography and Race Shape All Aspects of Health Care Social determinants of health visible everywhere: • Pharmacies in predominately black neighborhoods are less likely to have adequate medication supplies • Hospitals in black neighborhoods are more likely to close) • MDs are less likely to participate in Medicaid in racially segregated areas
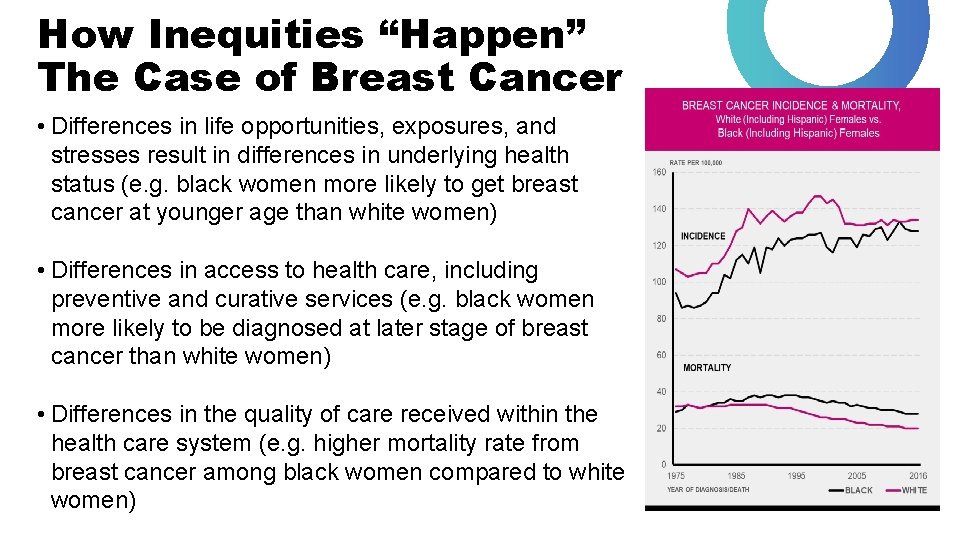
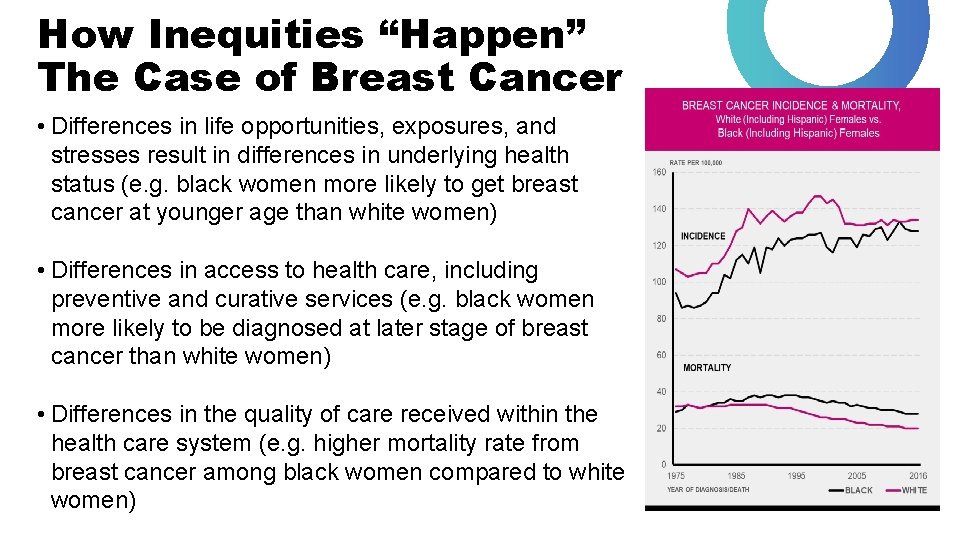
How Inequities “Happen” The Case of Breast Cancer • Differences in life opportunities, exposures, and stresses result in differences in underlying health status (e. g. black women more likely to get breast cancer at younger age than white women) • Differences in access to health care, including preventive and curative services (e. g. black women more likely to be diagnosed at later stage of breast cancer than white women) • Differences in the quality of care received within the health care system (e. g. higher mortality rate from breast cancer among black women compared to white women)

We Seemingly Have Tried: The Persistence of Racial/Ethnic Disparities Despite broad efforts, we have largely FAILED! In spite of: • A War on Poverty • A Civil Rights Revolution • Medicare and Medicaid • The Hill-Burton Act • Major advances in medical research & technology We have made little progress in reducing the elevated death rates of Blacks in particular and other minorities (Williams, Priest, & Anderson, 2016)
The Case of COVID-19
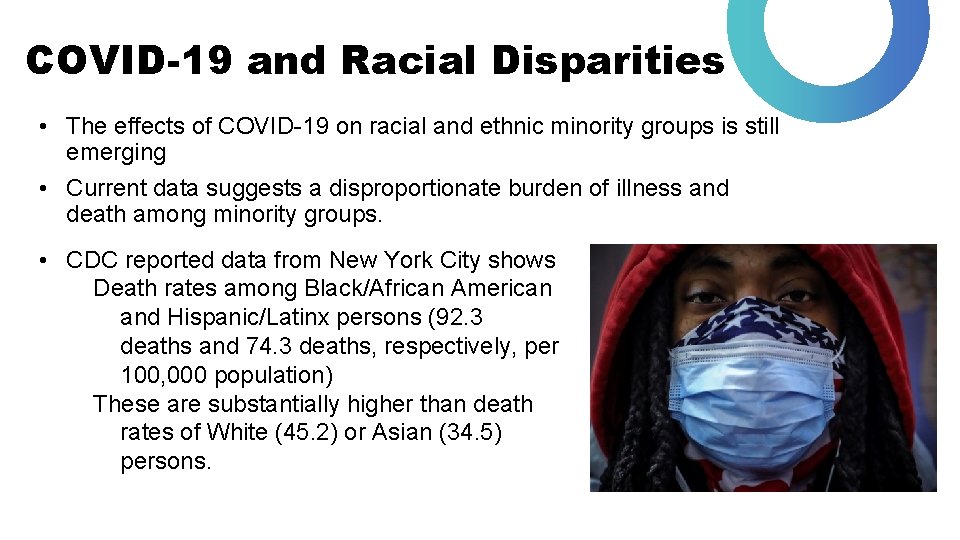
COVID-19 and Racial Disparities • The effects of COVID-19 on racial and ethnic minority groups is still emerging • Current data suggests a disproportionate burden of illness and death among minority groups. • CDC reported data from New York City shows Death rates among Black/African American and Hispanic/Latinx persons (92. 3 deaths and 74. 3 deaths, respectively, per 100, 000 population) These are substantially higher than death rates of White (45. 2) or Asian (34. 5) persons.
Structural Racism • The policies, programs, and institutional practices that facilitate the well-being of some while creating barriers to others results in inequalities in access to health and health promotion that drive COVID-19 inequities • Factors to consider: • • Employment Education The Wealth Gap Employer-based Health Insurance
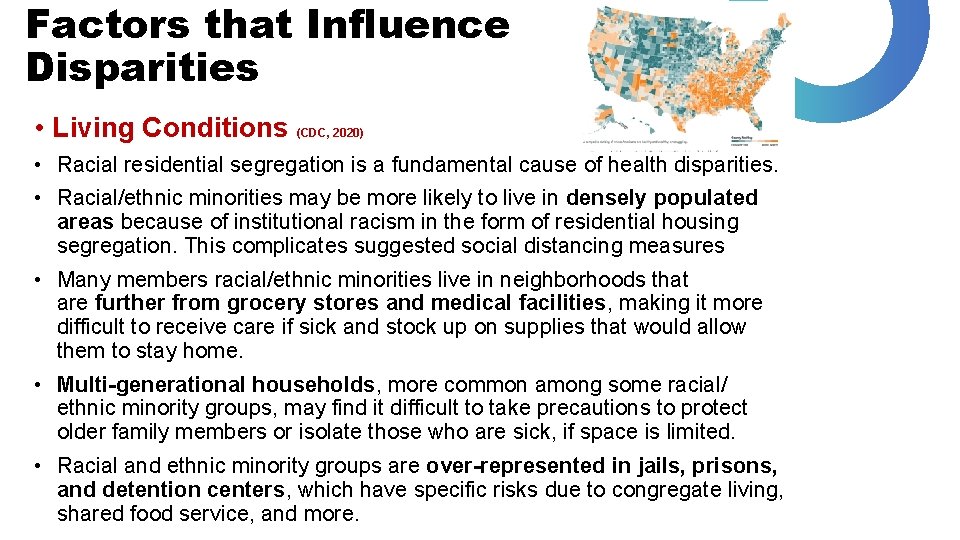
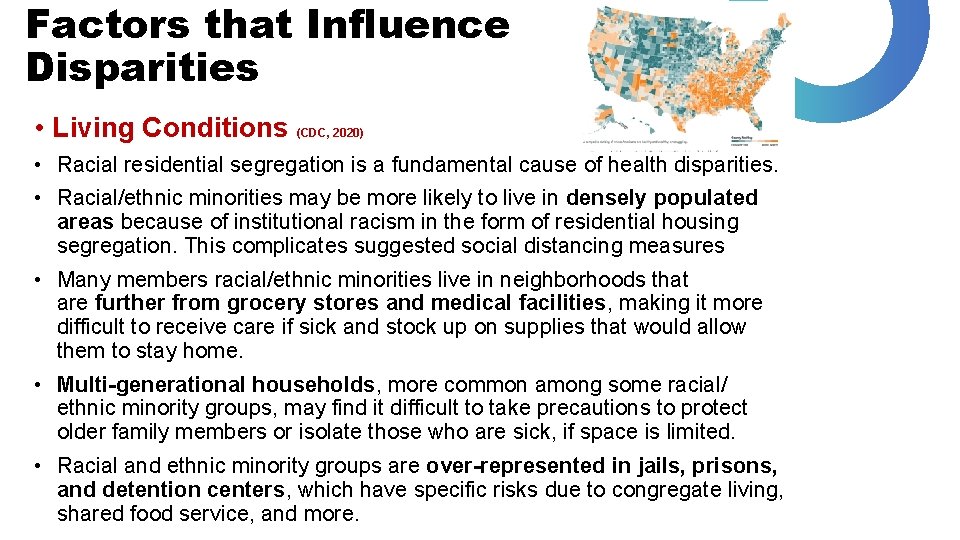
Factors that Influence Disparities • Living Conditions (CDC, 2020) • Racial residential segregation is a fundamental cause of health disparities. • Racial/ethnic minorities may be more likely to live in densely populated areas because of institutional racism in the form of residential housing segregation. This complicates suggested social distancing measures • Many members racial/ethnic minorities live in neighborhoods that are further from grocery stores and medical facilities, making it more difficult to receive care if sick and stock up on supplies that would allow them to stay home. • Multi-generational households, more common among some racial/ ethnic minority groups, may find it difficult to take precautions to protect older family members or isolate those who are sick, if space is limited. • Racial and ethnic minority groups are over-represented in jails, prisons, and detention centers, which have specific risks due to congregate living, shared food service, and more.
Factors that Influence Disparities Work Circumstances (CDC, 2020) • The types of work and policies in the work environments where some racial/ethnic minority groups are overrepresented can contribute to their risk for COVID-19. • Examples include: • Critical workers: The risk of infection may be greater for workers in essential industries who continue to work outside the home despite outbreaks in their communities • Nearly a quarter of employed Hispanic & Black workers are employed in service industry jobs compared to 16% of non-Hispanic whites. • Hispanic workers account for 17% of total employment but constitute 53% of agricultural workers; Black workers make up 12% of all employed workers, but account for 30% of licensed practical and licensed vocational nurses. 7 • A lack of paid sick leave: Workers without paid sick leave might be more likely to continue to work even when they are sick for any reason. This can increase workers exposure to other workers who may have COVID-19, or, in turn, expose others
Factors that Influence Disparities Underlying Health Conditions and Low Access to Care (CDC, 2020) • Existing health disparities (i. e. poorer underlying health & barriers to care) might make members of many racial/ethnic minority groups especially vulnerable in public health emergencies like COVID-19. • Lack of health insurance: Compared to Whites, Hispanics are almost 3 times as likely to be uninsured, and African Americans are almost twice as likely to be uninsured. • Inadequate access to care is also driven by a long-standing distrust of the health care system, language barriers, and financial implications associated with missing work to receive care. • Serious underlying medical conditions: Compared to Whites, Black Americans experience higher death rates, and higher prevalence rates of chronic conditions • Stigma and systemic inequalities may undermine prevention efforts, increase levels of chronic and toxic stress, and ultimately sustain health and health care disparities.
COVID-19 in the African American Community • COVID-19 is disproportionately impacting the African American community across the U. S. • Example Chicago: ½ of those diagnosed have been black, while African Americans only make up 1/3 rd of the population. • Example Louisiana: 70% of fatalities linked to COVID-19 have been among Black people, while this community makes up ~ 1/3 rd the overall population • Higher rates of infection and fatality are linked to existing health inequities (i. e. higher rates of diabetes and hypertension, and barriers to care) • Differences in access to high quality jobs and economic stability, quality education, health care services, and quality neighborhoods—contribute to these
Why Social Workers Should Care Our commitments to service, social justice, cultural competence, and diversity • Thinking about/doing something about situations that are discriminatory, that constrain people’s ability to exercise self-determination, or that limit individuals’ capacity to participate fully in society is what health disparities are about
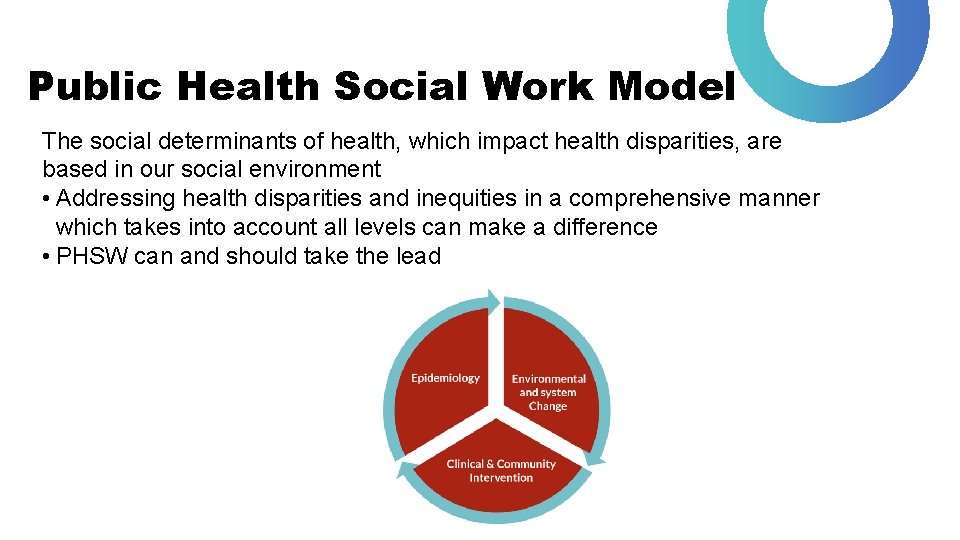
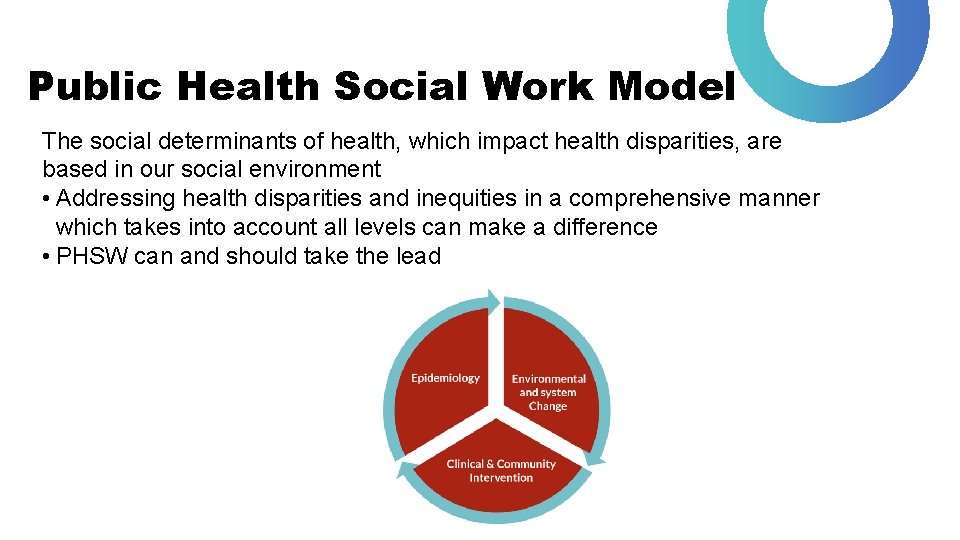
Public Health Social Work Model The social determinants of health, which impact health disparities, are based in our social environment • Addressing health disparities and inequities in a comprehensive manner which takes into account all levels can make a difference • PHSW can and should take the lead
We Are and Have Been Health Social Workers! Long history of involvement in health concerns, dating back to the turn of the 20 th century (Ruth & Marshall, 2017) Half of all social workers work within health, and the remaining social workers are employed addressing social determinants of health such as housing, child welfare, education, etc. (Ruth & Marshall, 2017) NASW, 2016 has specified standards for social work in health settings: these include the importance of prevention, the need to address health disparities, and recognition of the importance and complexity of this field of practice and the profession’s “leadership role in the psychosocial aspects of health care” (https: //www. socialworkers. org/Link. Click. aspx? fileticket=f. Fns. RHX-4 HE%3 D&portalid=0 )
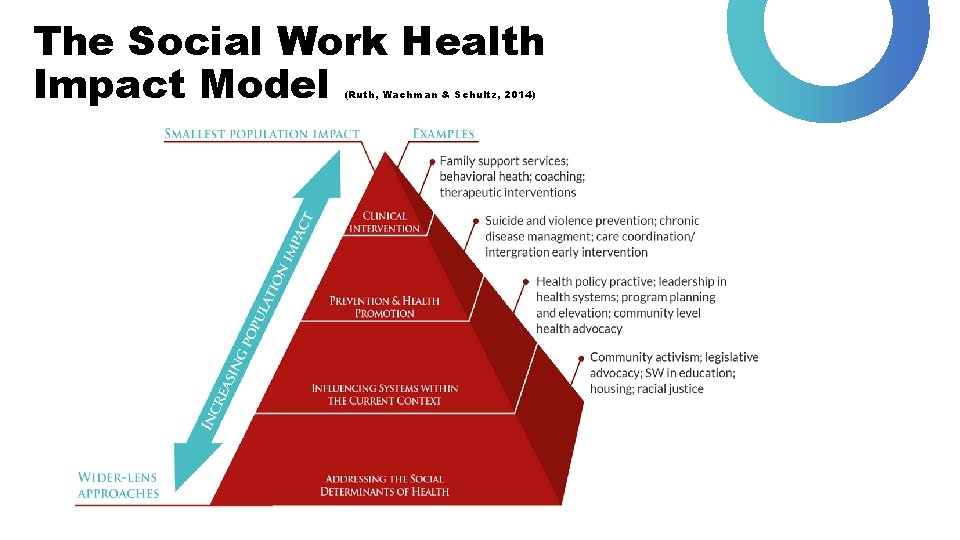
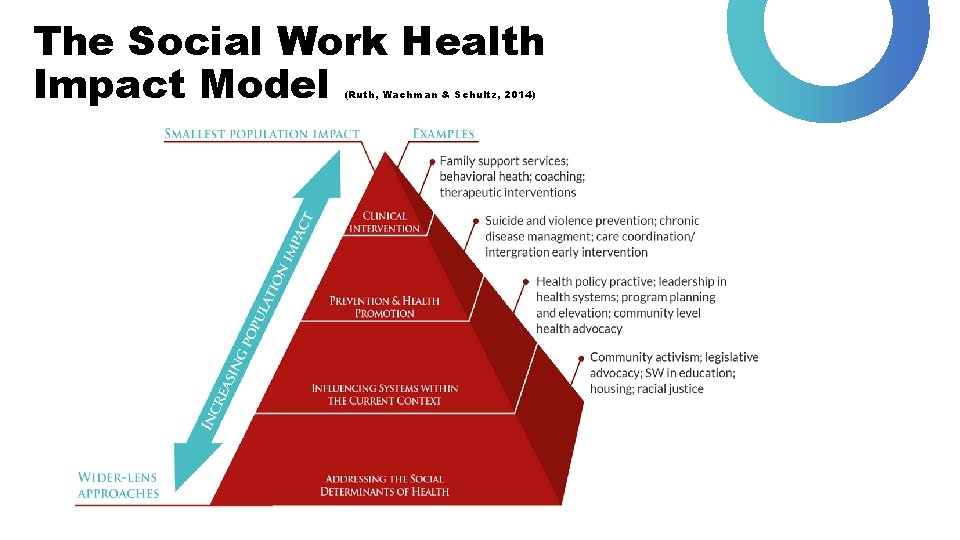
The Social Work Health Impact Model (Ruth, Wachman & Schultz, 2014)
PHSW Strategies to Address Ethnic & Racial Health Disparities/Inequities • Promoting techniques for self-managing health conditions (Mc. Pheeters et al. , 2012) • Connecting patients to the healthcare system through navigation and warm handoffs (Chin et al. , 2012; Quiñones et al. , 2011) • Ensuring that patients that require interpreters get them (University of Wisconsin, 2010)
COVID-19: What Can be Done? Federal Level • Collecting data to monitor and track disparities in the number of COVID-19 cases, complications, and deaths • Data translation into information to improve the clinical management of patients, allocation of resources, and targeted public health information. • Supporting partnerships between scientific researchers, professional organizations, community organizations, and community members to address need for information to prevent COVID-19 in racial and ethnic minority communities. • Providing clinical guidance and guidance to support actions to slow the spread of COVID-19 in schools, workplaces and community settings, including those serving racial and ethnic minorities.
COVID-19: What Can be Done? Community Level • Utilization of shared faith, family, and cultural institutions as sources of social support. • Preparation of community health workers in underserved racial/ethnic minority communities to educate and link people to free or low-cost services. • Prioritize resources for clinics, private practices, and other organizations that serve minority populations. • Leverage effective health promotion programs in community, work, school, and home settings • Work across sectors to connect people with services, such as grocery delivery or temporary housing, that help with social distancing practices • Help combat the spread of rumors and misinformation by providing credible information from official sources.
COVID-19: What Public Health Social Workers Can Do • Promote precautions to protect individuals in your community • Ensure that communications about COVID-19 is frequent, clear, transparent, and credible (from official sources). • Work with other sectors, such as faith and community education, business, transportation, and housing organizations, to share information and implement strategies to slow the spread of COVID-19. • Link more people to healthcare services for serious underlying medical conditions • Provide information to healthcare professionals and health systems to understand cultural differences among patients and how patients interact with providers and the healthcare system • Use evidence-based strategies to reduce health disparities
Activity: Disparities in Context What does it mean to recognize and address health disparities in the context of public health social work practice? Read the Equity Stories (https: //www. apha. org/~/media/files/pdf/topics/equity_stories. ashx) from the American Public Health Association and choose one as your focus. In small groups or on your own, answer the following: • How would you summarize the health disparity in this story? What specific factors contributed to this issue? • What was done to improve outcomes for the population affected? In particular, how did public health social work leaders partner with the population affected? • What lessons could you take away to use in your own context or with your population of interest?
Takeaway You can provide services but you are also responsible, as a social worker, for helping to ensure the availability, accessibility, quality and acceptability to and for the services; that means putting racial and ethnic inequities “on the table” In-class Exercise or Group Assignment: Let’s work through some examples by examining common health conditions associated with health disparities/health inequities: • Heart disease and stroke • Diabetes • Maternal and infant and child health
A Call to Action: How Social Workers Can Work Towards Health Equity • Maintain focus and commitment to social justice, particularly racial/ethnic justice • Use your advocacy skills to target health issues that disproportionately affect socially disadvantaged clients and groups • Infuse public health approaches into practice and educate colleagues about health inequities, emphasizing the need to address SDOH by helping clients: • Find safe housing • Secure employment • Enroll self or children in school or preschool • Link to health and social services • Know their rights
Selected Resources • American Public Health Association. (2015). Better health through equity – Case studies in reframing public health work. Retrieved from https: //www. apha. org/~/media/files/pdf/topics/equity_stories. ashx • Keefe, R. H. (2010). Health disparities: A primer for public health social workers. Social Work in Public Health, 25(3 -4), 237 -257. • Mitchell, F. M. (2015). Racial and ethnic health disparities in an era of health care reform. Health & Social Work, 40(3), e 66 -e 74. • Social Work in Illness Prevention and Health Promotion. Retrieved from https: //us. sagepub. com/sites/default/files/upm-binaries/44223_6. pdf • Unnatural causes. Retrieved from http: //www. pbs. org/unnaturalcauses/explore_learn. htm • Walters, K. L. , Spencer, M. S. , Smukler, M. , Allen, H. L. , Andrews, C. , Browne, T. , Maramaldi, P. , Wheeler, D. , Zebrack, B. & Uehara, E. (2016). Health equity: Eradicating health inequalities for future generations (Grand Challenges for Social Work Initiative Working Paper No. 19). Cleveland: American Academy of Social Work and Social Welfare. Retrieved from http: //aaswsw. org/wp-content/uploads/2016/01/WP 19 -with-cover 2. pdf
Bibliography • American Public Health Association. (2018). Health Equity. Retrieved from https: //www. apha. org/topics-and-issues/healthequity • Centers for Disease Control. (2006). The state of childhood asthma, United States, 1980 -2005. Retrieved from http: //www. cdc. gov/nchs/data/ad/ad 381. pdf • Balfour, P. C. , Ruiz, J. M. , Talavera, G. A. , Allison, M. A. , & Rodriguez, C. J. (2016). Cardiovascular Disease in Hispanics/Latinos in the United States. Journal of Latina/o Psychology, 4(2), 98– 113. • Centers for Disease Control. (2014). African Americans Heart Disease and Stroke Fact Sheet. Retrieved from https: //www. cdc. gov/dhdsp/data_statistics/fact_sheets/fs_aa. ht m • Boston’s Community Asthma Initiative, http: //www. childrenshospital. org/Centers-and. Services/Programs/A-_-E/community-asthma-initiative-program • Centers for Disease Control (2016). Selected CDC-Sponsored Interventions, United States, 2016. Retrieved from https: //www. cdc. gov/minorityhealth/strategies 2016/ • Braveman, P. (2006). Health disparities and health equity: concepts and measurement. Annu. Rev. Public Health, 27, 167194. • Chin, M. H. , Clarke, A. R. , Nocon, R. S. , Casey, A. A. , Goddu, A. P. , Keesecker, N. M. , & Cook, S. C. (2012). A Roadmap and Best Practices for Organizations to Reduce Racial and Ethnic Disparities in Health Care. Journal of General Internal Medicine, 27(8), 992– 1000. http: //doi. org/10. 1007/s 11606 -0122082 -9 • Buchmueller, T. C. , Jacobson, M. , & Wold, C. (2006). How far to the hospital? : The effect of hospital closures on access to care. Journal of health economics, 25(4), 740 -761.
Bibliography • Council on Social Work Education. (2018). Results of the nationwide survey of 2017 social work graduates – The National social workforce study. Retrieved from https: //www. socialworkers. org/Link. Click. aspx? fileticket=C 0 r 5 P 1 zk. Mb. Q%3 d&portalid=0 • Morrison, R. S. , Wallenstein, S. , Natale, D. K. , Senzel, R. S. , & Huang, L. L. (2000). “We don't carry that”—failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. New England Journal of Medicine, 342(14), 1023 -1026. • Greene, J. , Blustein, J. , & Weitzman, B. C. (2006). Race, Segregation, and Physicians’ Participation in Medicaid. The Milbank Quarterly, 84(2), 239– 272. http: //doi. org/10. 1111/j. 1468 -0009. 2006. 00447. x • National Association of Social Workers. (2016). NASW standards for social work practice in health care settings. Retrieved from http: //www. socialworkers. org/practice/standards/Health. C are. Standards_SW%20 Practice_Final. pdf • Henry J. Kaiser Foundation. (2016). Disparities in Health and Health Care: Five Key Questions and Answers. Retrieved from http: //files. kff. org/attachment/Issue-Brief-Disparities-in-Healthand-Health-Care-Five-Key-Questions-and-Answers • Mc. Pheeters, M. L. , Kripalani, S. , Peterson, N. B. , Idowu, R. T. , Jerome, R. N. , Potter, S. A. , & Andrews, J. C. (2012). Quality Improvement Interventions to Address Health Disparities: Closing the Quality Gap: Revisiting the State of the Science. Vanderbilt University Evidence-based Practice Center • National Healthcare Quality and Disparities Reports. Data Query: Table 6_4_1_5_1. 2 b. Retrieved from http: //nhqrnet. ahrq. gov/inhqrdr/data/query • Quiñones, A. R. , O’Neil, M. , Saha, S. , Freeman, M. , Henry, S. R. , & Kansagara, D. (2011). Interventions to improve minority health care and reduce racial and ethnic disparities. Washington, DC: Department of Veterans Affairs.
Bibliography • Smedley, B. D. , Stith, A. Y. , & Nelson, A. R. (2003). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academic Press. • US Census (2015). Retrieved from https: //census. gov/content/dam/Census/library/publications/ 2015/demo/p 25 -1143. pdf • University of Wisconsin Population Health Institute. (2010). Professionally trained medical interpreters. Retrieved from http: //whatworksforhealth. wisc. edu/program. php? t 1=22&t 2= 17&t 3=28&id=637 • Williams, D. R. , Priest, N. , & Anderson, N. (2016). Understanding associations between race, socioeconomic status and health: Patterns and Prospects. Health Psychology, 35(4), 407– 411.
Acknowledgements • This slide deck was a project of the Advancing Leadership in Public Health Social Work Education project at Boston University School of Social Work (BUSSW-ALPS), made possible by a cooperative agreement from the Health Resources and Services Administration (HRSA) of the U. S. Department of Health and Human Services (HHS) under grant number G 05 HP 31425. We wish to acknowledge our project officer, Miryam Gerdine, MPH. Thanks also to Sara S. Bachman, BUSSW Center for Innovation in Social Work and Health, and the Group for Public Health Social Work Initiatives. • Author: Tamara J. Cadet, Ph. D. , LICSW, MPH The ALPS Team: • Betty J. Ruth, Principal Investigator • Madi Wachman, Co-Principal Investigator • Alexis Marbach Co-Principal Investigator • Nandini Choudhury, Research Assistant • Jamie Wyatt Marshall, Principal Consultant COVID Updates • Public Health Social Work Section of the American Public Health Association