Addressing possible serious bacterial infection among sick young
Addressing possible serious bacterial infection among sick young infants in Kenya where referral is not feasible: Where are we now? Dr. Felicitas Makokha Paediatrician, Bungoma County Wilson Liambila and Timothy Abuya-Population Council Fred Were and Kezia K’Oduol- KEPRECON Jesse Gitaka –Mount Kenya University Kenya Paediatric Association 2019 Annual Scientific Conference Mombasa, 9 th to 12 th April 2019
Introduction • Kenya has high NNM rate (22 per 1000 live births) with sepsis contributing up to 20% of deaths • Poor care seeking, dysfunctional referral pathways and negative cultural beliefs worsen situation • Reducing this burden requires timely case identification & initiation of suitable antibiotic treatment • Clinical trials of simplified treatment regimens in Asia and Africa (2011 -2013) showed: ü high refusal rates for referral by caregivers (Kenya 89%) ü simplified antibiotic regimens for SYIs provided at PHC level when referral is not feasible are effective and can save lives.
WHO Guidelines Developed to Respond to Clinical Trial Results
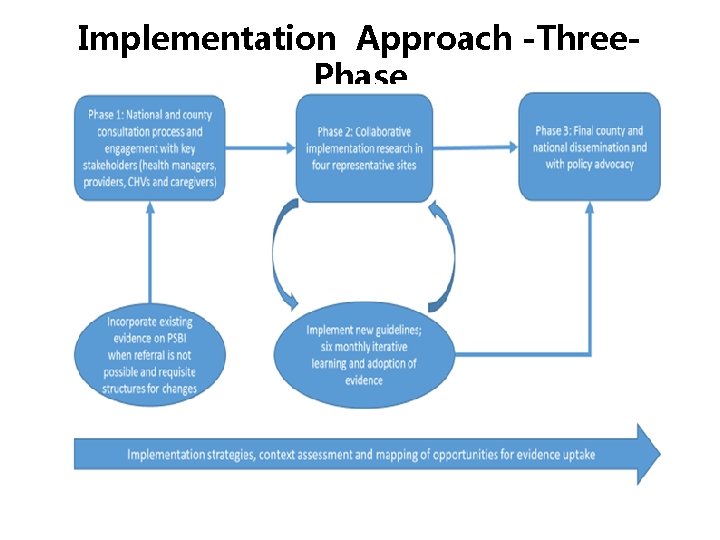
Implementation Approach -Three. Phase

PROJECT PROGRESS IN PAST ONE YEAR
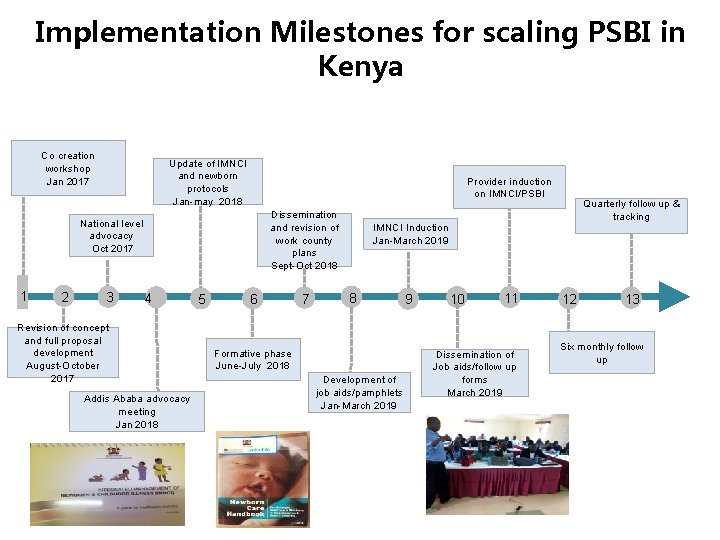
Implementation Milestones for scaling PSBI in Kenya Co creation workshop Jan 2017 Update of IMNCI and newborn protocols Jan-may 2018 Provider induction on IMNCI/PSBI Dissemination and revision of work county plans Sept-Oct 2018 National level advocacy Oct 2017 1 2 3 4 Revision of concept and full proposal development August-October 2017 Addis Ababa advocacy meeting Jan 2018 5 6 7 Quarterly follow up & tracking IMNCI Induction Jan-March 2019 8 Formative phase June-July 2018 Development of job aids/pamphlets Jan-March 2019 9 10 11 Dissemination of Job aids/follow up forms March 2019 12 13 Six monthly follow up
USE OF EVIDENCE FOR IMPLEMENTATION
Project is using Implementation Research(IR) Approach to: • Create foundation for learning • Generate evidence for action • Develop a measurement framework through periodic monitoring of performance or implementation activities
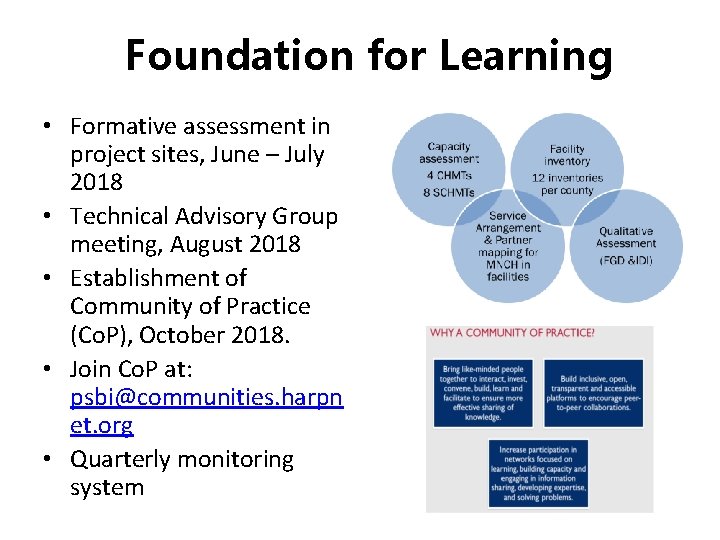
Foundation for Learning • Formative assessment in project sites, June – July 2018 • Technical Advisory Group meeting, August 2018 • Establishment of Community of Practice (Co. P), October 2018. • Join Co. P at: psbi@communities. harpn et. org • Quarterly monitoring system
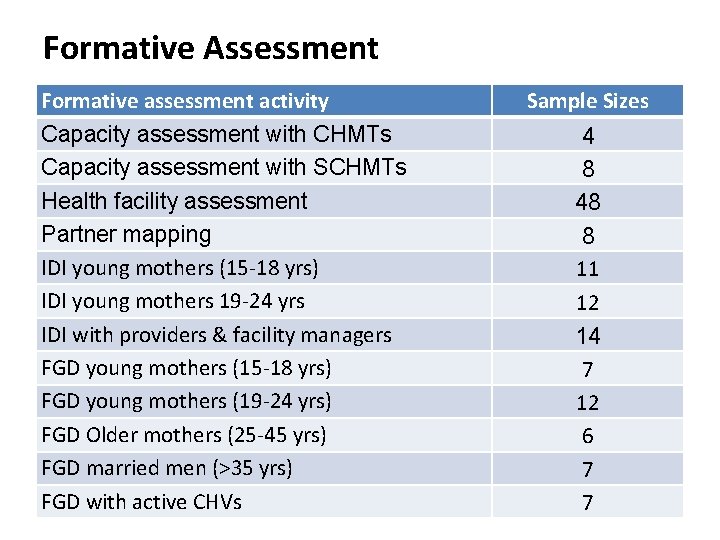
Formative Assessment Formative assessment activity Capacity assessment with CHMTs Capacity assessment with SCHMTs Health facility assessment Partner mapping IDI young mothers (15 -18 yrs) IDI young mothers 19 -24 yrs IDI with providers & facility managers FGD young mothers (15 -18 yrs) FGD young mothers (19 -24 yrs) FGD Older mothers (25 -45 yrs) FGD married men (>35 yrs) FGD with active CHVs Sample Sizes 4 8 48 8 11 12 14 7 12 6 7 7
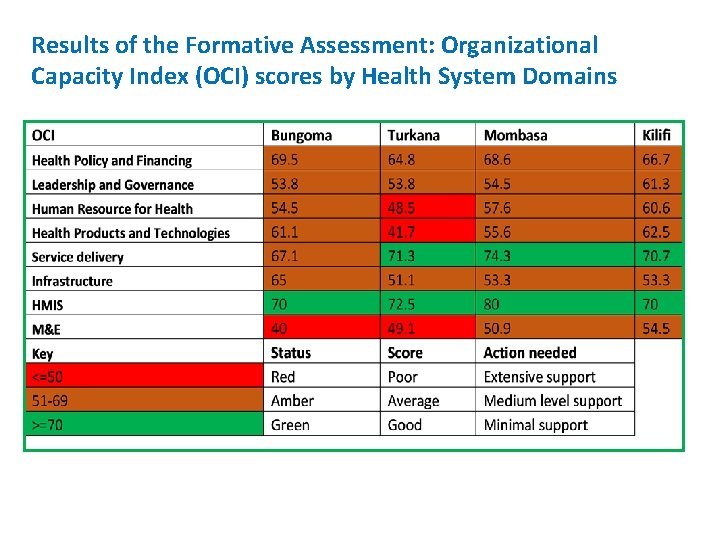
Results of the Formative Assessment: Organizational Capacity Index (OCI) scores by Health System Domains
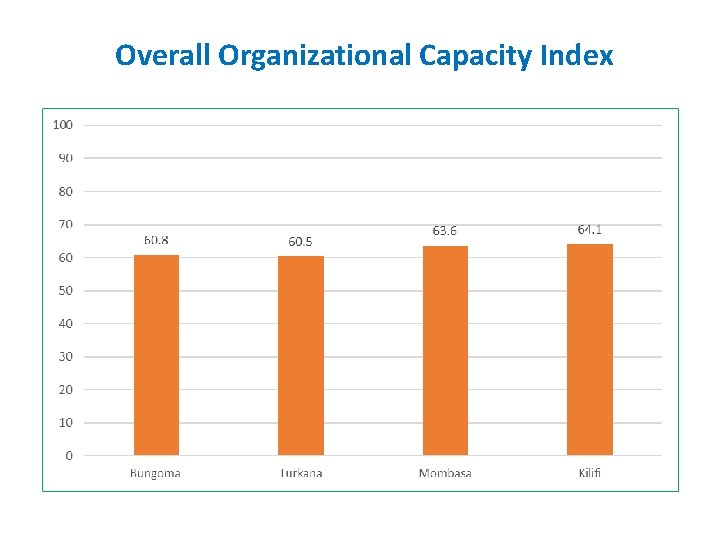
Overall Organizational Capacity Index
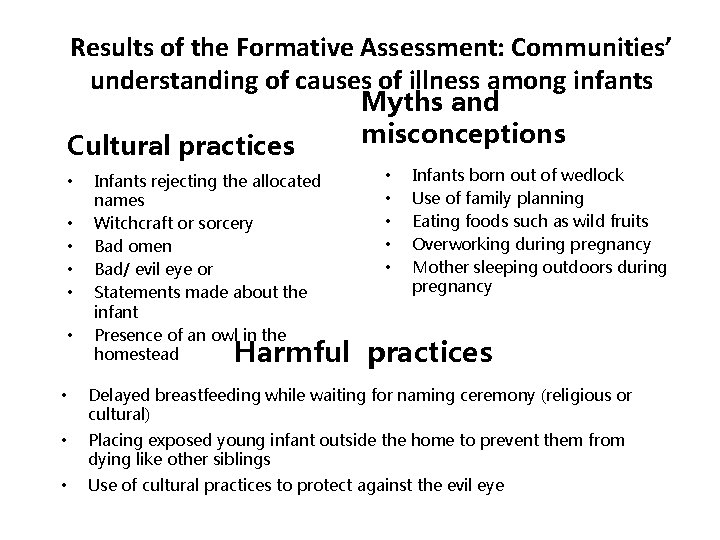
Results of the Formative Assessment: Communities’ understanding of causes of illness among infants Cultural practices • • • Infants rejecting the allocated names Witchcraft or sorcery Bad omen Bad/ evil eye or Statements made about the infant Presence of an owl in the homestead Myths and misconceptions • • • Infants born out of wedlock Use of family planning Eating foods such as wild fruits Overworking during pregnancy Mother sleeping outdoors during pregnancy Harmful practices • Delayed breastfeeding while waiting for naming ceremony (religious or cultural) • Placing exposed young infant outside the home to prevent them from dying like other siblings • Use of cultural practices to protect against the evil eye
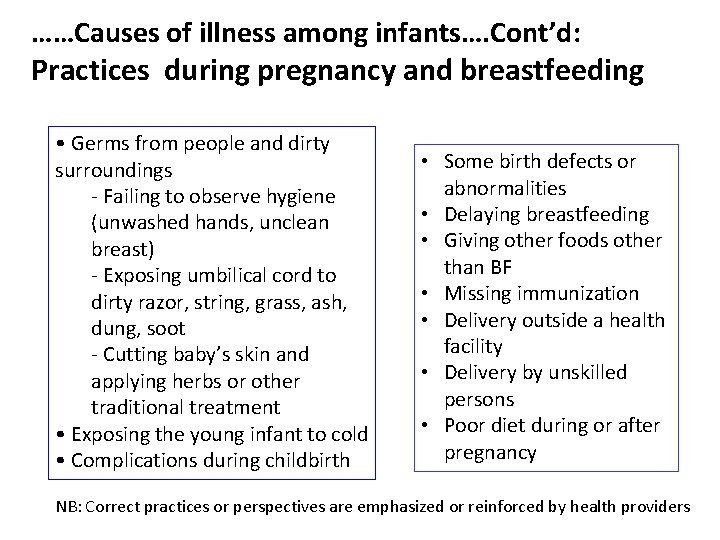
……Causes of illness among infants…. Cont’d: Practices during pregnancy and breastfeeding • Germs from people and dirty surroundings - Failing to observe hygiene (unwashed hands, unclean breast) - Exposing umbilical cord to dirty razor, string, grass, ash, dung, soot - Cutting baby’s skin and applying herbs or other traditional treatment • Exposing the young infant to cold • Complications during childbirth • Some birth defects or abnormalities • Delaying breastfeeding • Giving other foods other than BF • Missing immunization • Delivery outside a health facility • Delivery by unskilled persons • Poor diet during or after pregnancy NB: Correct practices or perspectives are emphasized or reinforced by health providers
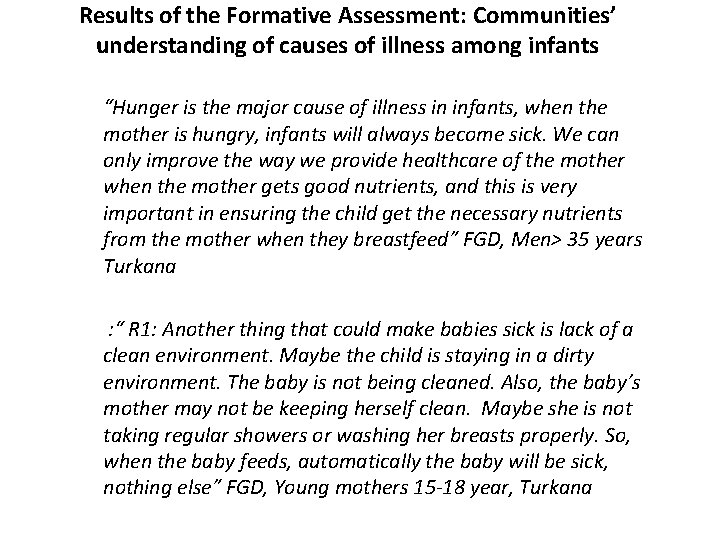
Results of the Formative Assessment: Communities’ understanding of causes of illness among infants “Hunger is the major cause of illness in infants, when the mother is hungry, infants will always become sick. We can only improve the way we provide healthcare of the mother when the mother gets good nutrients, and this is very important in ensuring the child get the necessary nutrients from the mother when they breastfeed” FGD, Men> 35 years Turkana : “ R 1: Another thing that could make babies sick is lack of a clean environment. Maybe the child is staying in a dirty environment. The baby is not being cleaned. Also, the baby’s mother may not be keeping herself clean. Maybe she is not taking regular showers or washing her breasts properly. So, when the baby feeds, automatically the baby will be sick, nothing else” FGD, Young mothers 15 -18 year, Turkana
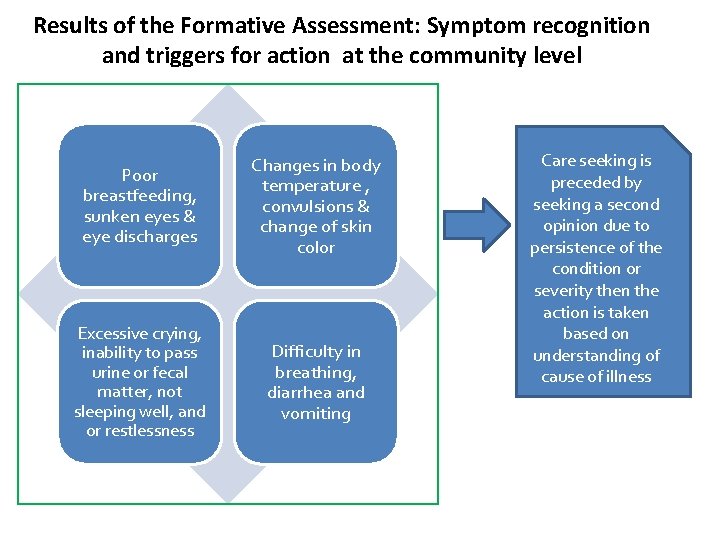
Results of the Formative Assessment: Symptom recognition and triggers for action at the community level Poor breastfeeding, sunken eyes & eye discharges Changes in body temperature , convulsions & change of skin color Excessive crying, inability to pass urine or fecal matter, not sleeping well, and or restlessness Difficulty in breathing, diarrhea and vomiting Care seeking is preceded by seeking a second opinion due to persistence of the condition or severity then the action is taken based on understanding of cause of illness
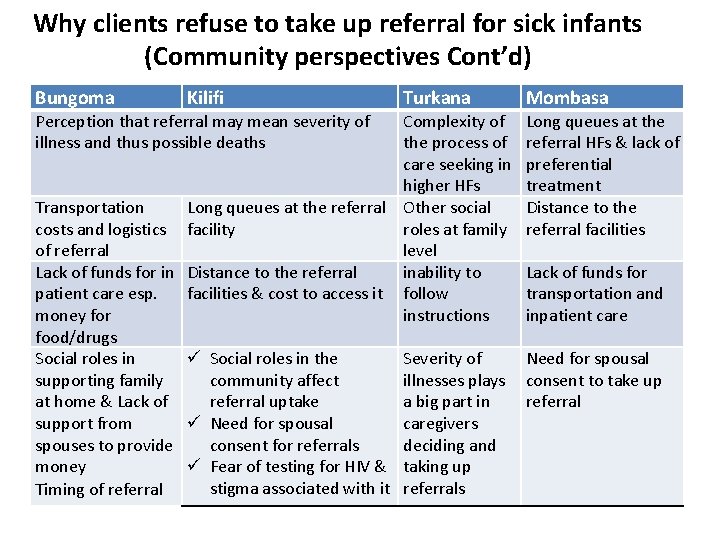
Why clients refuse to take up referral for sick infants (Community perspectives Cont’d) Bungoma Kilifi Perception that referral may mean severity of illness and thus possible deaths Turkana Complexity of the process of care seeking in higher HFs Transportation Long queues at the referral Other social costs and logistics facility roles at family of referral level Lack of funds for in Distance to the referral inability to patient care esp. facilities & cost to access it follow money for instructions food/drugs Social roles in ü Social roles in the Severity of supporting family community affect illnesses plays at home & Lack of referral uptake a big part in support from ü Need for spousal caregivers spouses to provide consent for referrals deciding and money ü Fear of testing for HIV & taking up stigma associated with it referrals Timing of referral Mombasa Long queues at the referral HFs & lack of preferential treatment Distance to the referral facilities Lack of funds for transportation and inpatient care Need for spousal consent to take up referral
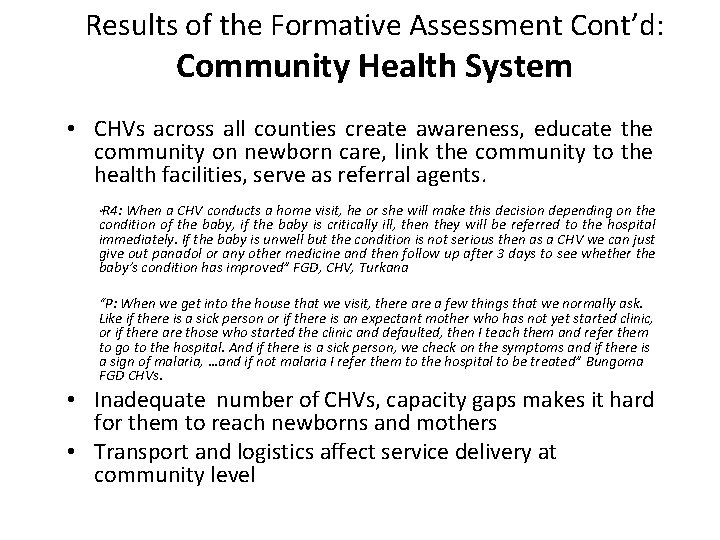
Results of the Formative Assessment Cont’d: Community Health System • CHVs across all counties create awareness, educate the community on newborn care, link the community to the health facilities, serve as referral agents. R 4: When a CHV conducts a home visit, he or she will make this decision depending on the condition of the baby, if the baby is critically ill, then they will be referred to the hospital immediately. If the baby is unwell but the condition is not serious then as a CHV we can just give out panadol or any other medicine and then follow up after 3 days to see whether the baby’s condition has improved” FGD, CHV, Turkana “ “P: When we get into the house that we visit, there a few things that we normally ask. Like if there is a sick person or if there is an expectant mother who has not yet started clinic, or if there are those who started the clinic and defaulted, then I teach them and refer them to go to the hospital. And if there is a sick person, we check on the symptoms and if there is a sign of malaria, …and if not malaria I refer them to the hospital to be treated” Bungoma FGD CHVs. • Inadequate number of CHVs, capacity gaps makes it hard for them to reach newborns and mothers • Transport and logistics affect service delivery at community level
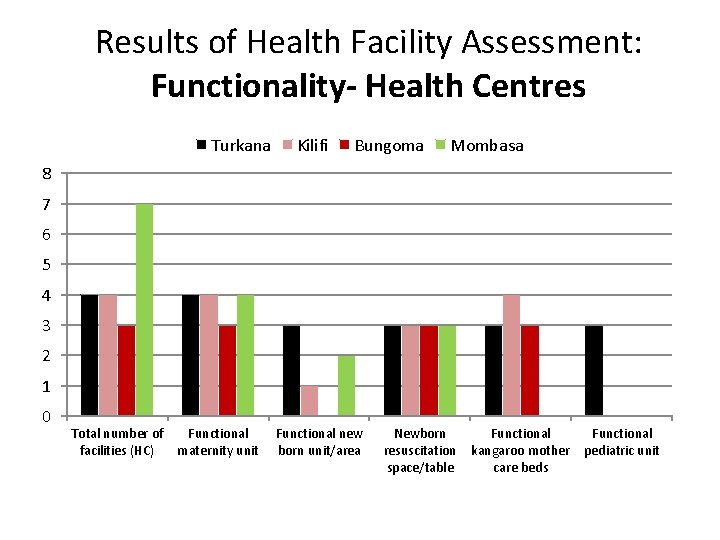
Results of Health Facility Assessment: Functionality- Health Centres Turkana Kilifi Bungoma Mombasa 8 7 6 5 4 3 2 1 0 Total number of facilities (HC) Functional maternity unit Functional new born unit/area Newborn resuscitation space/table Functional kangaroo mother pediatric unit care beds
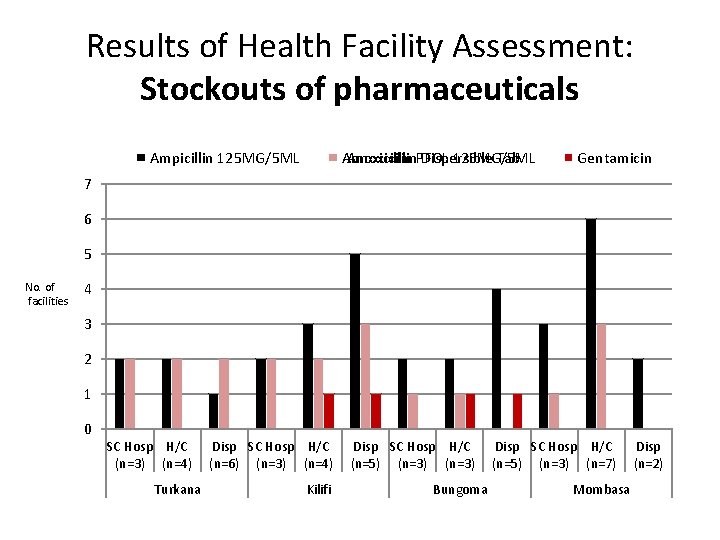
Results of Health Facility Assessment: Stockouts of pharmaceuticals Amoxicillin. PFOL Dispersible Tab Amoxicillin 125 MG/5 ML Ampicillin 125 MG/5 ML Gentamicin 7 6 5 No. of facilities 4 3 2 1 0 SC Hosp H/C (n=3) (n=4) Turkana Disp SC Hosp H/C (n=6) (n=3) (n=4) Kilifi Disp SC Hosp H/C (n=5) (n=3) Bungoma Disp SC Hosp H/C (n=5) (n=3) (n=7) Mombasa Disp (n=2)

IMPLEMENTATION ACTIONS BASED ON FORMATIVE DATA
Developed provider and caregiver Pamphlets
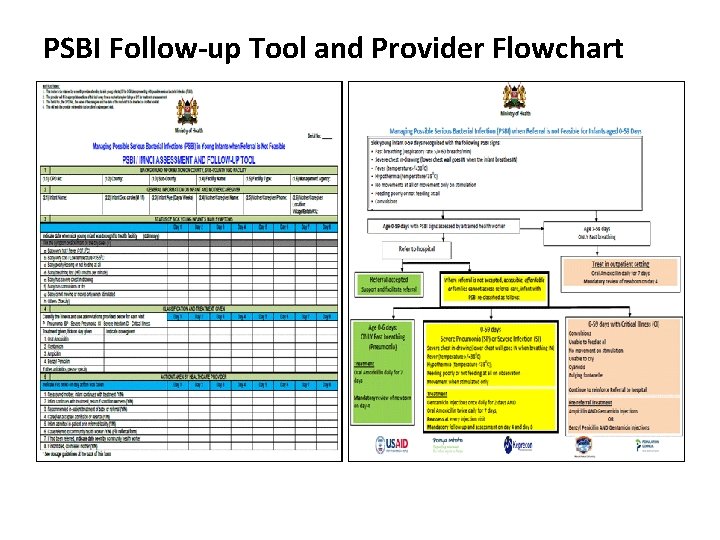
PSBI Follow-up Tool and Provider Flowchart
IMNCI Training/Updates • IMNCI training materials have been revised/ updated to incorporate PSBI • In Mombasa and Kilifi counties, majority of providers have received updates on the revised IMNCI/PSBI materials • In Bungoma-IMNCI training for TOTs has just been completed and plans are underway to train the providers • Providers in a few subcounties in Turkana including Turkana Central have received updates on IMNCI/PSBI
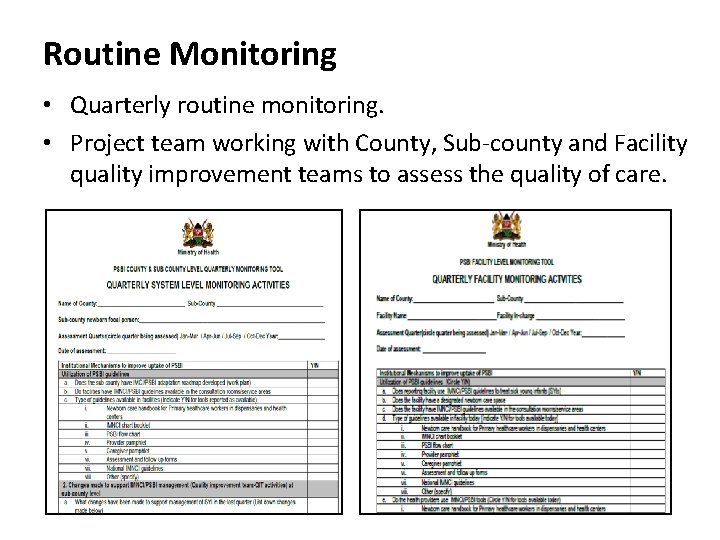
Routine Monitoring • Quarterly routine monitoring. • Project team working with County, Sub-county and Facility quality improvement teams to assess the quality of care.
Periodic Iterative Data Collection • IR data collection cycles involve conducting case narratives with women who use PSBI and those referred from the community by CHVs, and in-depth interviews with active CHVs and frontline providers. • Project team will continuously document the number of PSBI cases seen and the treatment given as well as referral practices for purposes of generating additional evidence to guide scale up and future revisions of national IMNCI/PSBI guidelines.
Implementation Challenges • Shortage of staff especially in lower HFs • Barriers such as negative cultural practices contribute to delays in care seeking for SYIs with PSBI • Weak linkage between HFs/providers & CHV activities contribute to poor follow up of SYIs with PSBI • Some HFs do not have community health units (CUs) - hence no active CHVs to assist in following up SYIs. • Erratic supply of some key antibiotics such as Gentamycin, Amoxicillin dispersible tablets, etc NB: There is need for the MOH/C&sub county teams to involve the private sector providers in the training of IMNCI/PSBI
What support are we seeking from pediatricians in scaling up PSPBI? • County pediatricians to support roll out in their respective counties • Advocate for IMNCI implementation – Training and induction of providers – Documentation of management • Enhance role out of PSBI guidelines in the private sector – Middle class population increasingly refusing referral – Inclusion of private sector providers in updates and training on IMNCI
Acknowledgements Population Council Wilson Liambila Timothy Abuya Charity Ndwiga George Odwe Charlotte Warren • • • Kenya Paediatric Research Consortium • • • Fred Were David Githanga Joe Mbuthia Doris Kinuthia Kezia K’Oduol Mount Kenya University • • • Jesse Gitaka Alice Natecho Samuel Mungai Peter Mwaura Jackline Nyaberi Institutions • • Newborn, Child & Adolescent Health Unit - MOH County and Sub-County Health Management Teams – Bungoma County and Sub-County Health Management Teams – Turkana County and Sub-County Health Management Teams – Mombasa County and Sub-County Health Management Teams – Kilifi Health Facility Management Teams – Project Counties USAID-for providing financial resources
- Slides: 31