Additional Content You might consider adding multimedia content



![Thank you! [Insert Contact Information] Visit the National Center for PTSD at: www. ptsd. Thank you! [Insert Contact Information] Visit the National Center for PTSD at: www. ptsd.](https://slidetodoc.com/presentation_image_h/a97d574f24c3d739ac17df3846892414/image-54.jpg)
- Slides: 54
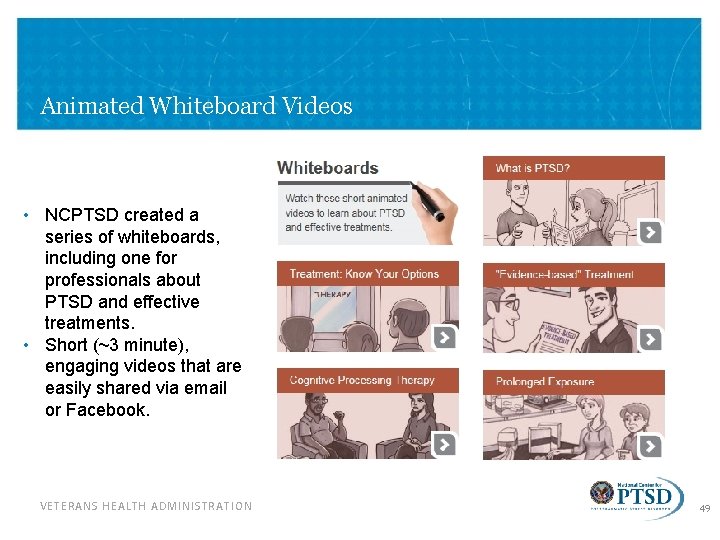
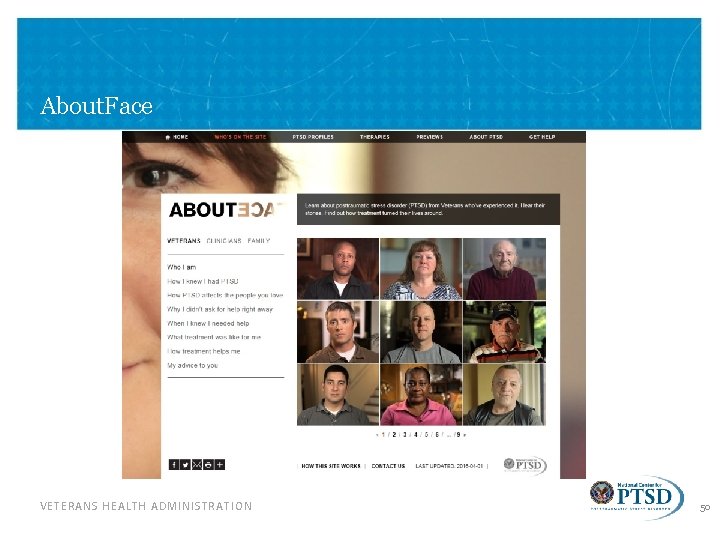
Additional Content You might consider adding multimedia content to the PPT, which we did not do to maintain file size of this PPT. In particular: • Download About. Face Previews: compilation of Veteran responses to key questions which overview symptoms and treatment experiences • Download Whiteboard Videos (Public): series of 5 animated whiteboard videos on PTSD and effective treatments • Download Whiteboard Video (Professional): animated whiteboard video for providers on best treatments for PTSD If you have questions or need more in-depth information for your presentation, contact: PTSDconsult@va. gov or rebecca. matteo@va. gov VETERANS HEALTH ADMINISTRATION 1
Posttraumatic Stress Disorder Overview and Treatment Alex L. Alexander MS, ND, LMHC March 2017
Overview • What is a traumatic stressor or: trauma, traumatic event? • How common are trauma and PTSD? • What are the symptoms of PTSD? • Why do some people develop PTSD and others do not? • What problems co-occur with PTSD? • How is PTSD treated? • National Center for PTSD (NCPTSD) Resources for Trauma Survivors & Clinicians VETERANS HEALTH ADMINISTRATION 3
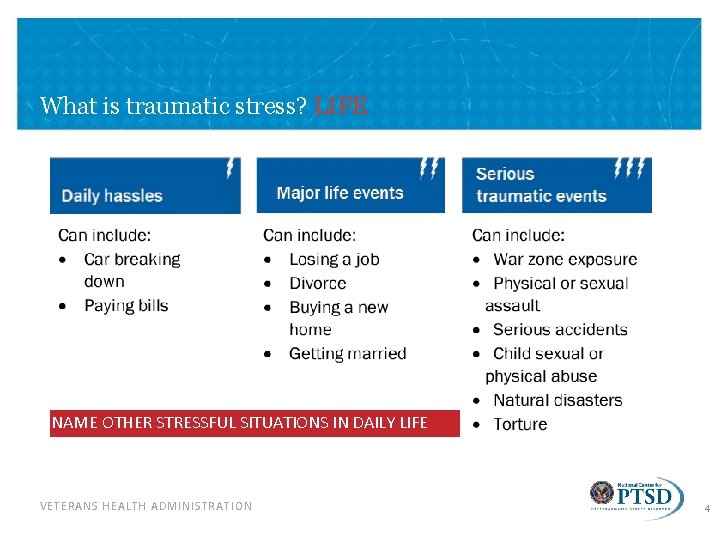
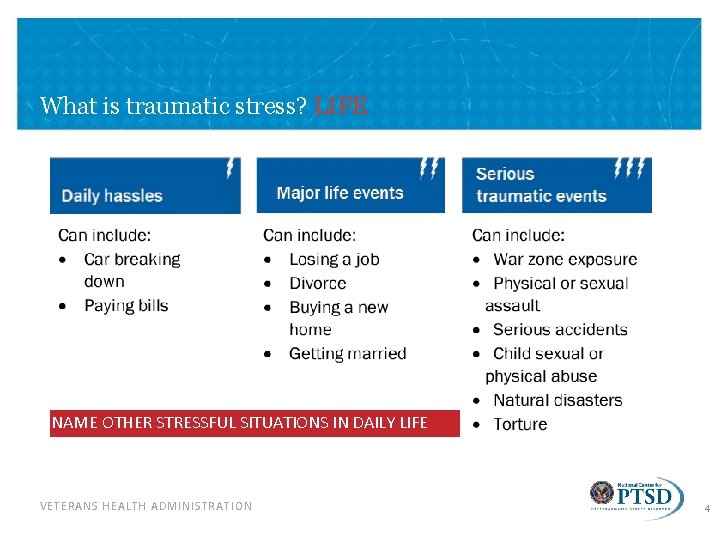
What is traumatic stress? LIFE NAME OTHER STRESSFUL SITUATIONS IN DAILY LIFE VETERANS HEALTH ADMINISTRATION 4
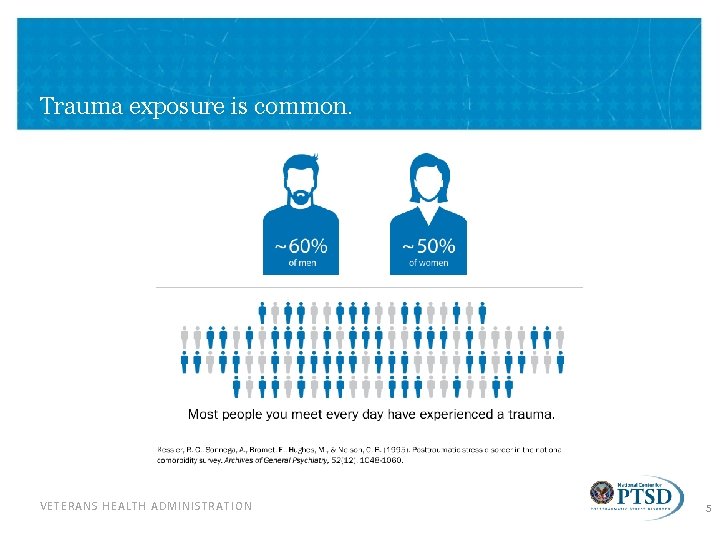
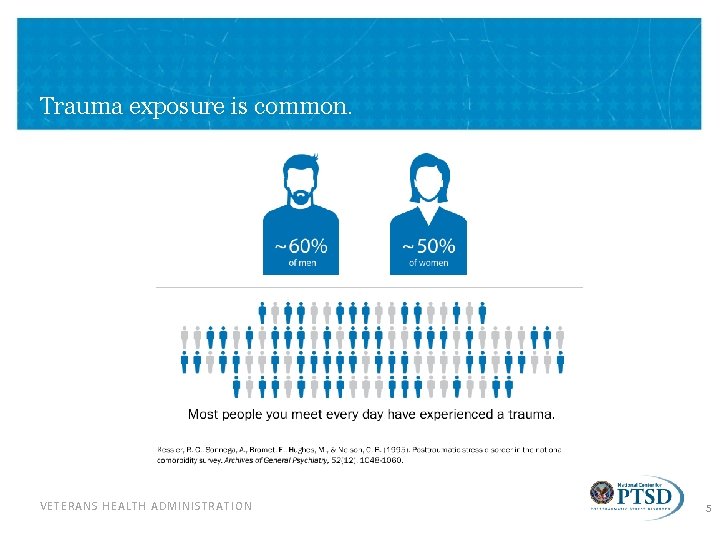
Trauma exposure is common. VETERANS HEALTH ADMINISTRATION 5
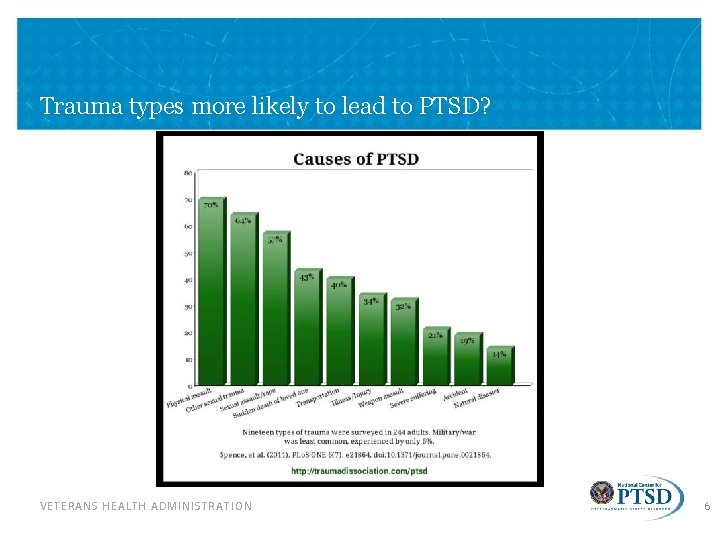
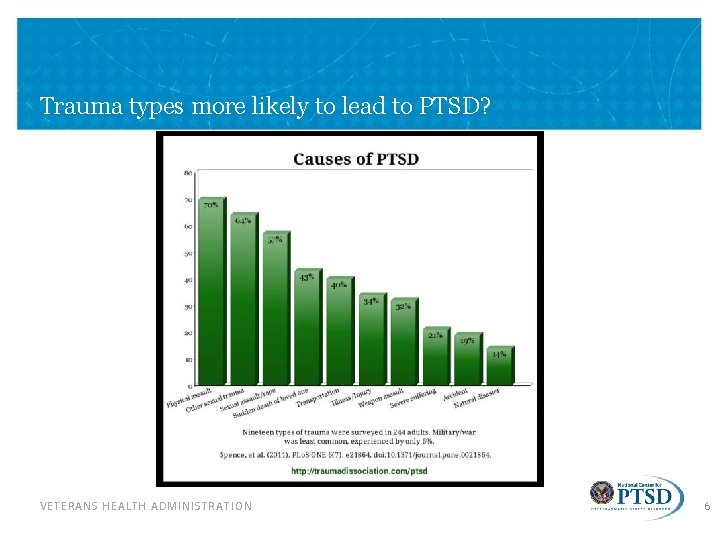
Trauma types more likely to lead to PTSD? VETERANS HEALTH ADMINISTRATION 6
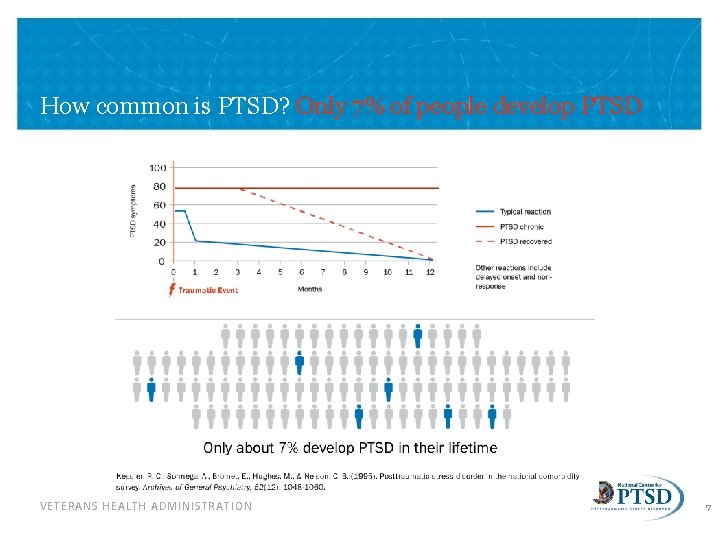
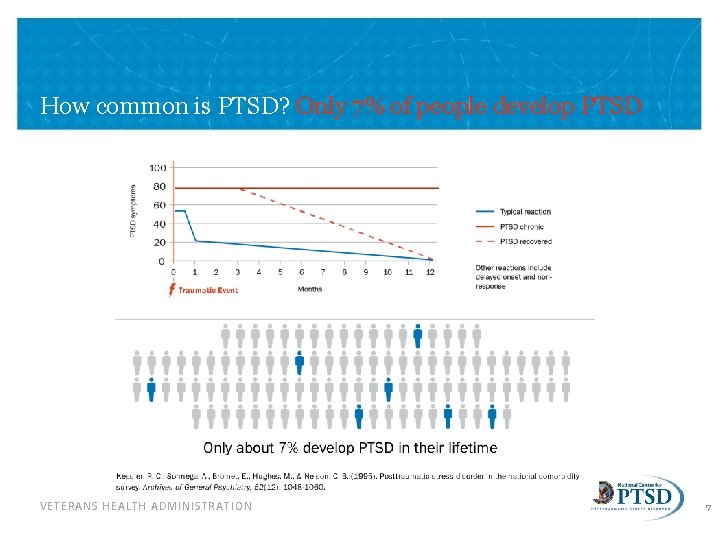
How common is PTSD? Only 7% of people develop PTSD VETERANS HEALTH ADMINISTRATION 7
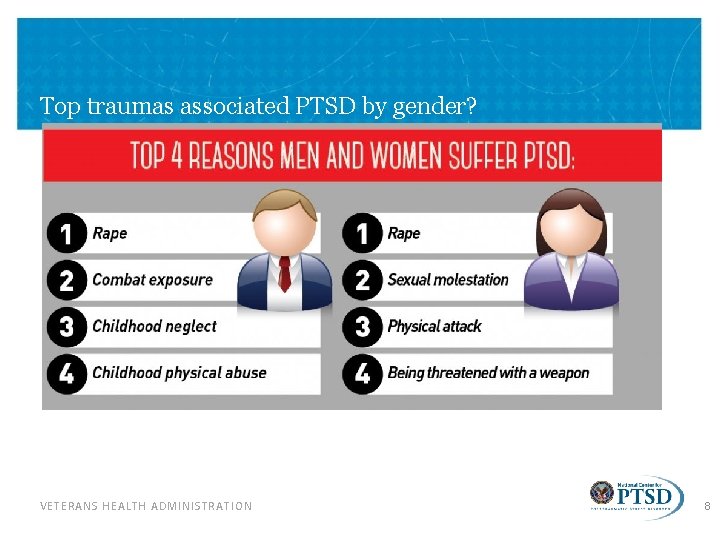
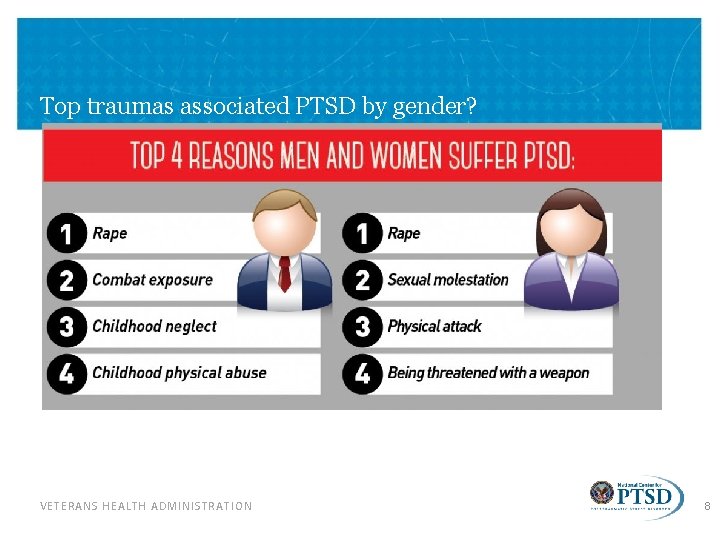
Top traumas associated PTSD by gender? VETERANS HEALTH ADMINISTRATION 8
What about repeated exposure to tragic events? Name as many news-media-reported events in the last 10 years as you can that were traumatic to hear about and process VETERANS HEALTH ADMINISTRATION 9
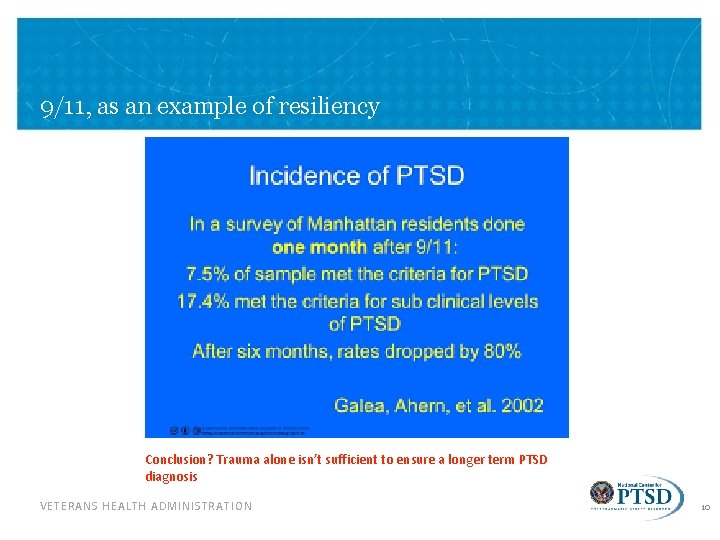
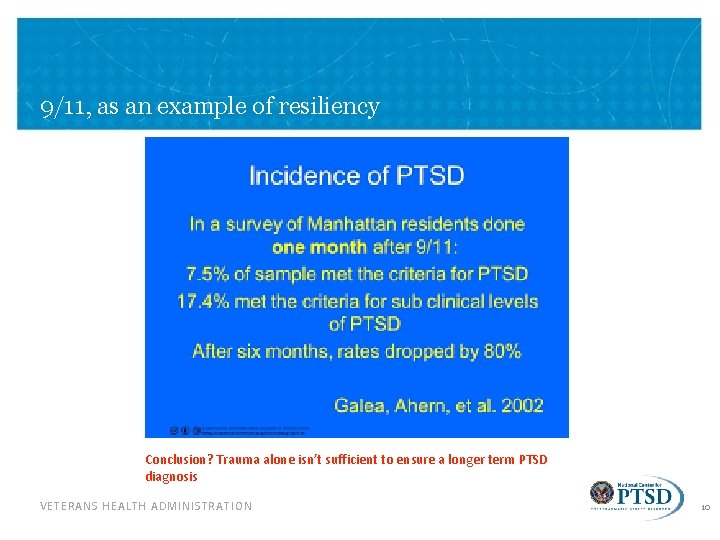
9/11, as an example of resiliency Conclusion? Trauma alone isn’t sufficient to ensure a longer term PTSD diagnosis VETERANS HEALTH ADMINISTRATION 10
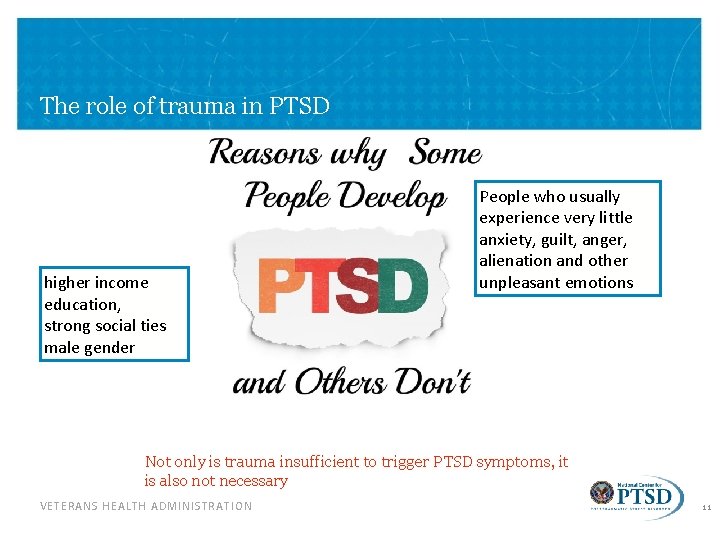
The role of trauma in PTSD higher income education, strong social ties male gender People who usually experience very little anxiety, guilt, anger, alienation and other unpleasant emotions Not only is trauma insufficient to trigger PTSD symptoms, it is also not necessary VETERANS HEALTH ADMINISTRATION 11
Emotional triggers. Although by definition clinicians cannot diagnose PTSD in the absence of trauma, recent work suggests that the disorder’s telltale symptom pattern can emerge from stressors that do not involve bodily peril. DSM V VETERANS HEALTH ADMINISTRATION 12
The emerging research In a 2005 study of 454 undergraduates, psychologist Sari Gold of Temple University and her colleagues revealed that students who had experienced nontraumatic stressors, such as serious illness in a loved one, divorce of their parents, relationship problems or imprisonment of someone close to them, reported even higher rates of PTSD symptoms than did students who had lived through bona fide trauma. Taken together, these findings call into question the long-standing belief that these symptoms are tied only to physical threat. PTSD symptoms can follow emotional upheavals VETERANS HEALTH ADMINISTRATION 13
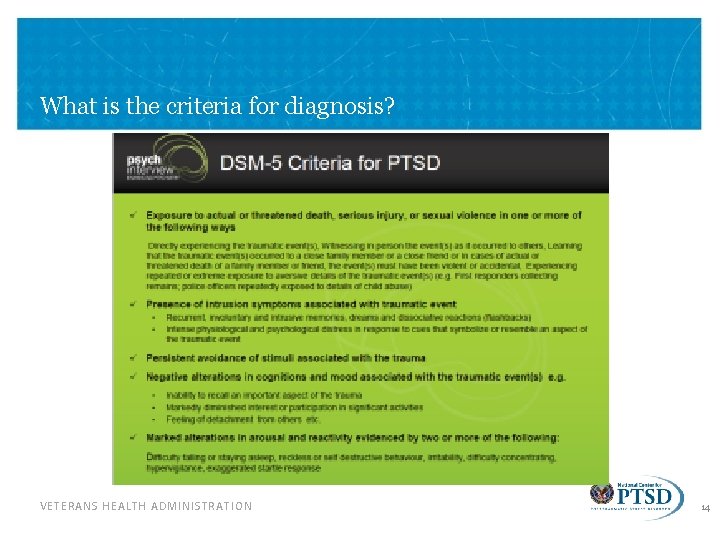
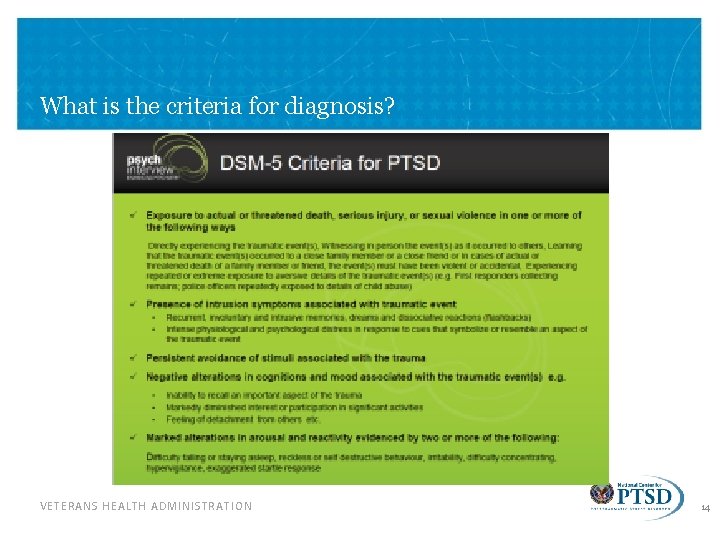
What is the criteria for diagnosis? VETERANS HEALTH ADMINISTRATION 14
Criterion A: Traumatic Event • Directly experiencing a traumatic event • Witnessing, in person, an event that happened to someone else • Learning about the violent or unexpected death of a friend of family member • Experiencing repeated or extreme exposure to aversive details of traumatic events VETERANS HEALTH ADMINISTRATION 15

Symptom Clusters VETERANS HEALTH ADMINISTRATION 16
Symptom Clusters 2 Cont. • Intrusion (or re-experiencing, “flashbacks”) – Recurrent distressing dreams of the event or acting/feeling as if the event is happening again VETERANS HEALTH ADMINISTRATION 17
Symptom Clusters 3 Cont. • Avoidance – Avoiding memories, thoughts, feelings, people, places or activities that are reminders of the event VETERANS HEALTH ADMINISTRATION 18
Symptom Clusters 4 Cont. • Negative alterations in cognitions and mood – Diminished interest in activities, feeling detached, inability to feel positive emotions, negative emotions, distorted blame of self or others VETERANS HEALTH ADMINISTRATION 19
Symptom Clusters 5 Cont. • Alterations in arousal and reactivity – Irritable behavior, outbursts of anger, reckless or self destructive behavior, problems concentrating, hypervigilance, exaggerated startle, sleep disturbance VETERANS HEALTH ADMINISTRATION 20
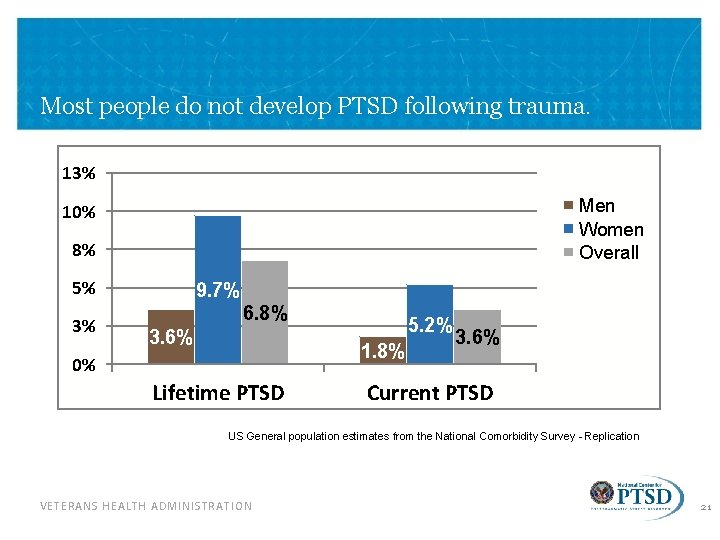
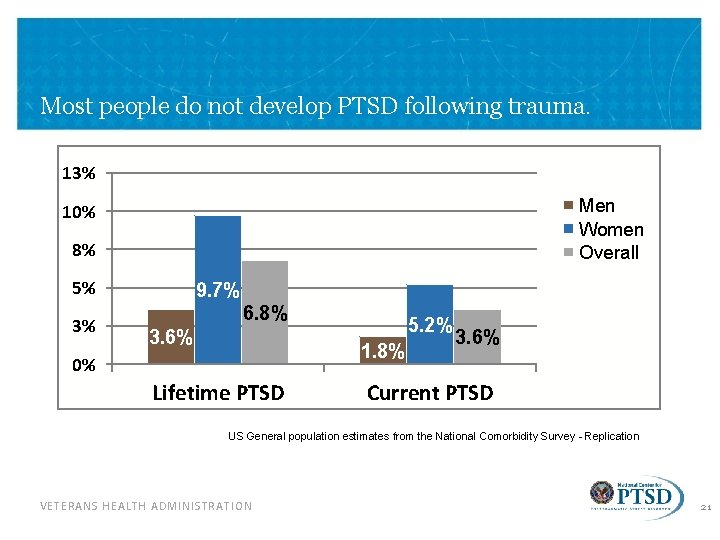
Most people do not develop PTSD following trauma. 13% Men Women Overall 10% 8% 5% 3% 9. 7% 6. 8% 3. 6% 5. 2% 1. 8% 0% Lifetime PTSD 3. 6% Current PTSD US General population estimates from the National Comorbidity Survey - Replication VETERANS HEALTH ADMINISTRATION 21
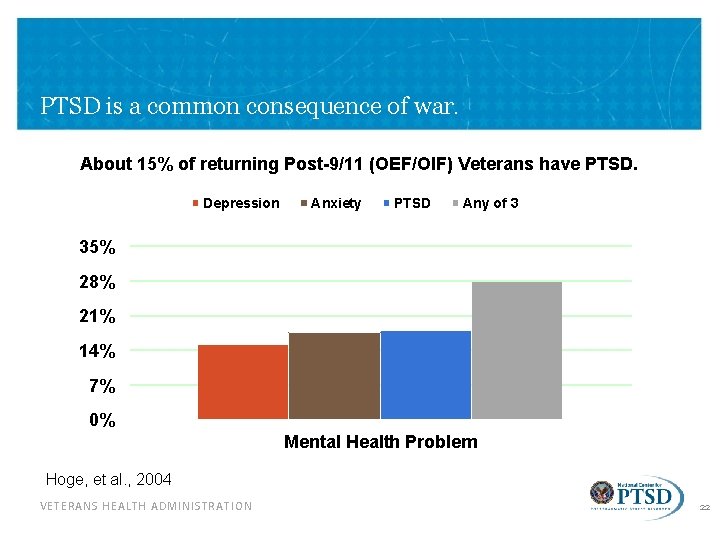
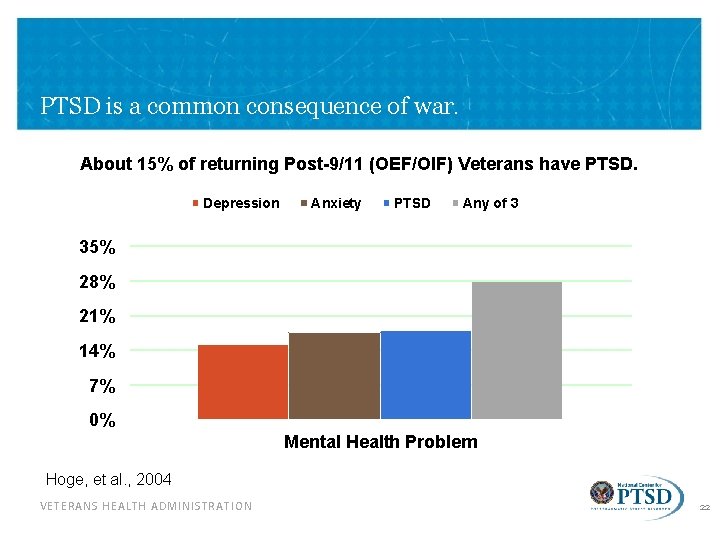
PTSD is a common consequence of war. About 15% of returning Post-9/11 (OEF/OIF) Veterans have PTSD. Depression Anxiety PTSD Any of 3 35% 28% 21% 14% 7% 0% Mental Health Problem Hoge, et al. , 2004 VETERANS HEALTH ADMINISTRATION 22
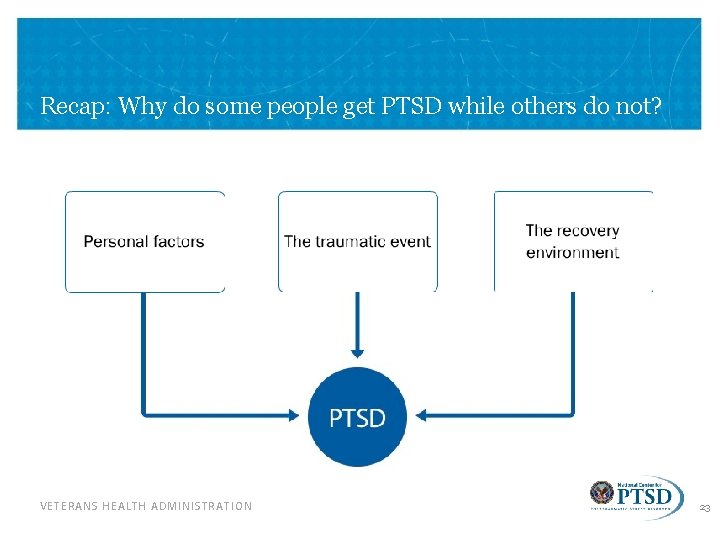
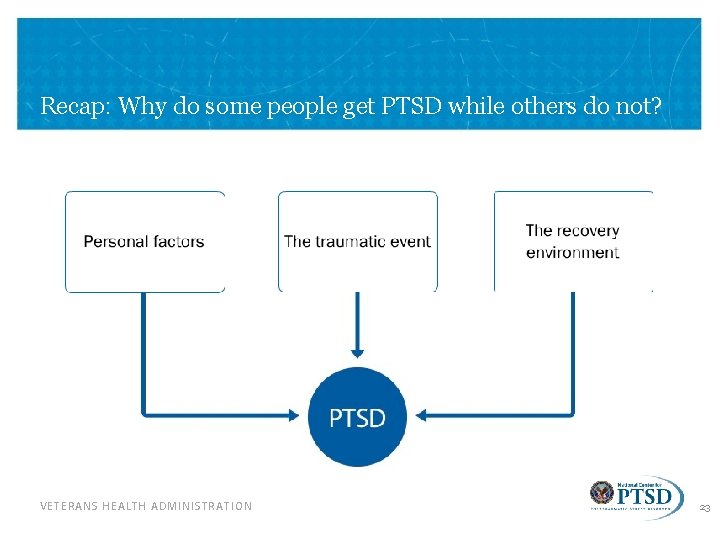
Recap: Why do some people get PTSD while others do not? VETERANS HEALTH ADMINISTRATION 23
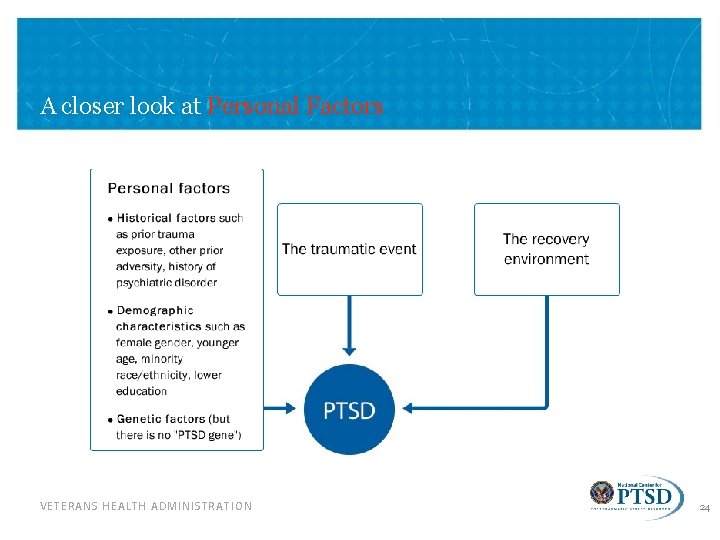
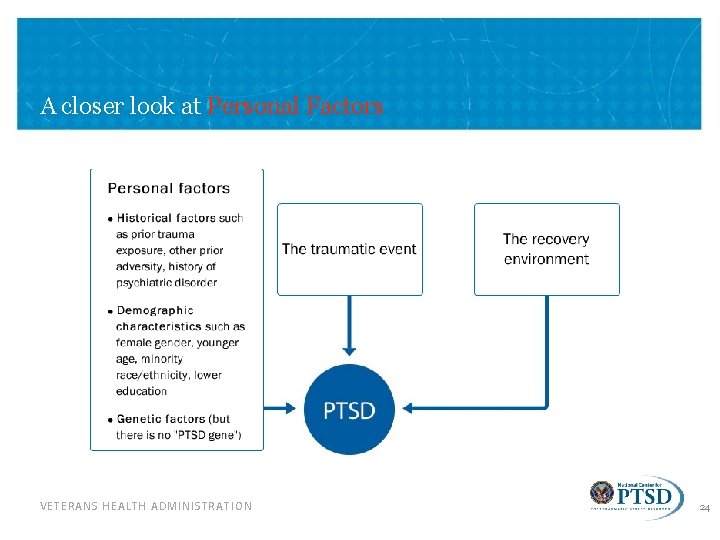
A closer look at Personal Factors VETERANS HEALTH ADMINISTRATION 24
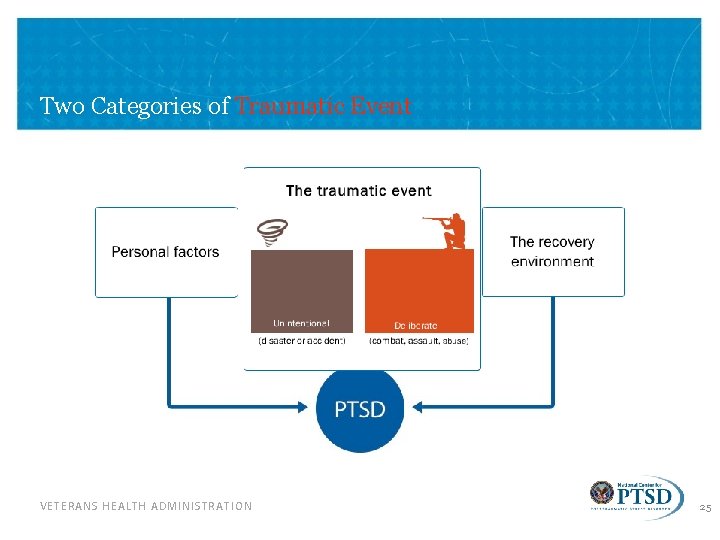
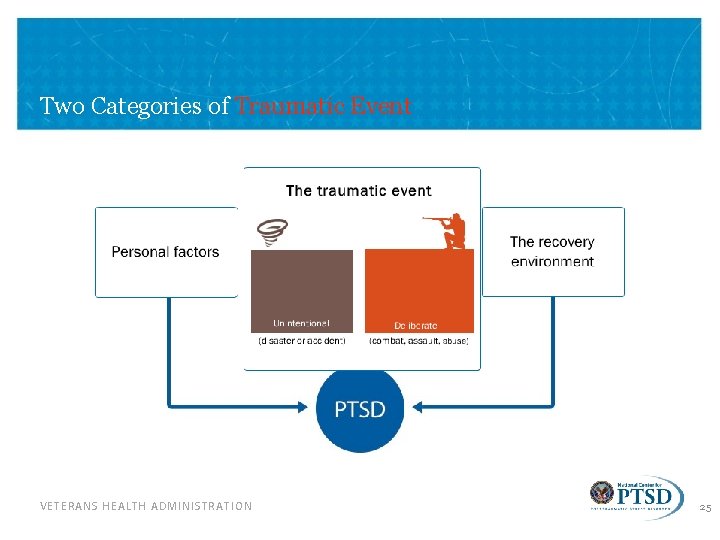
Two Categories of Traumatic Event VETERANS HEALTH ADMINISTRATION 25
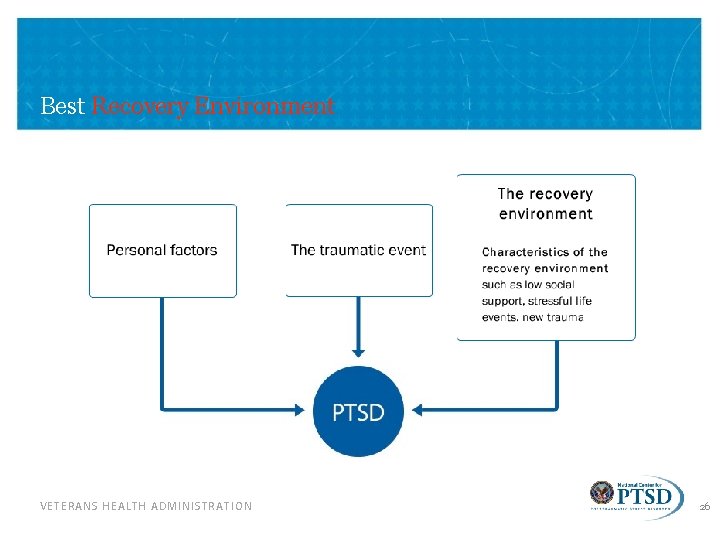
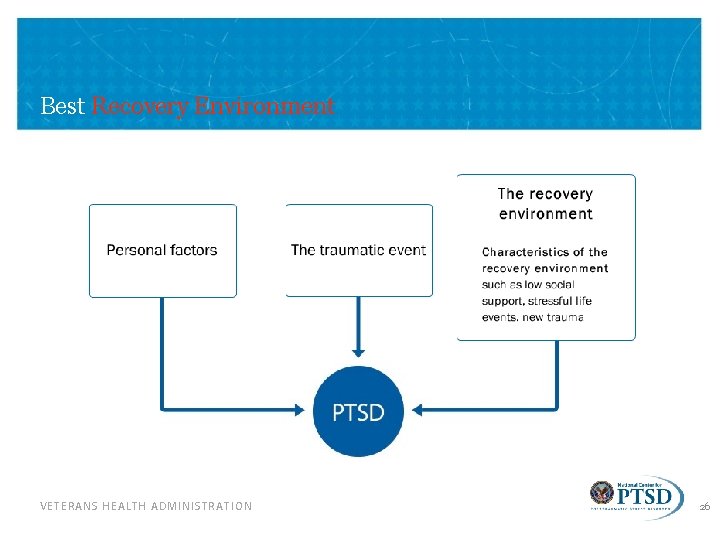
Best Recovery Environment VETERANS HEALTH ADMINISTRATION 26
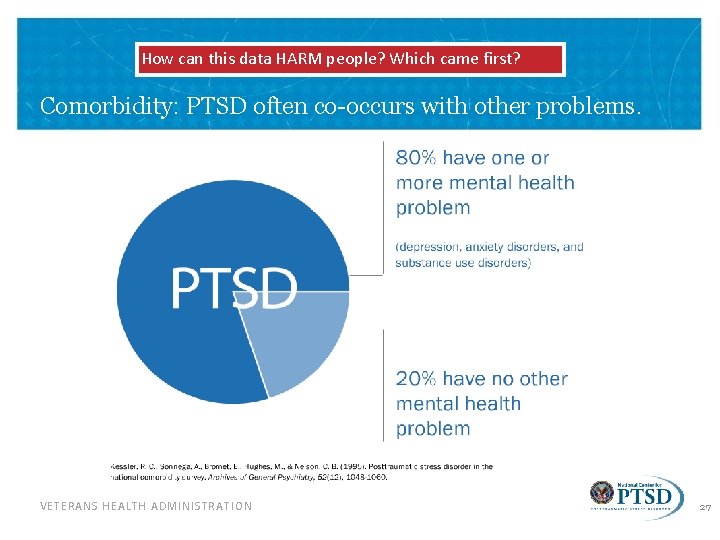
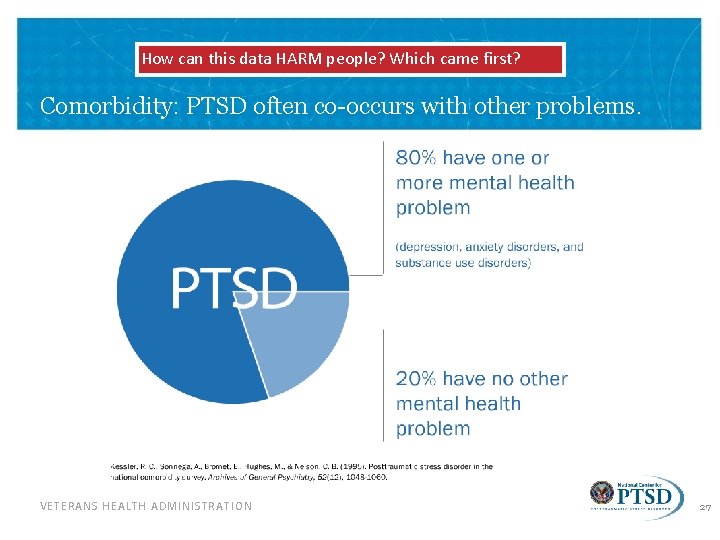
How can this data HARM people? Which came first? Comorbidity: PTSD often co-occurs with other problems. VETERANS HEALTH ADMINISTRATION 27
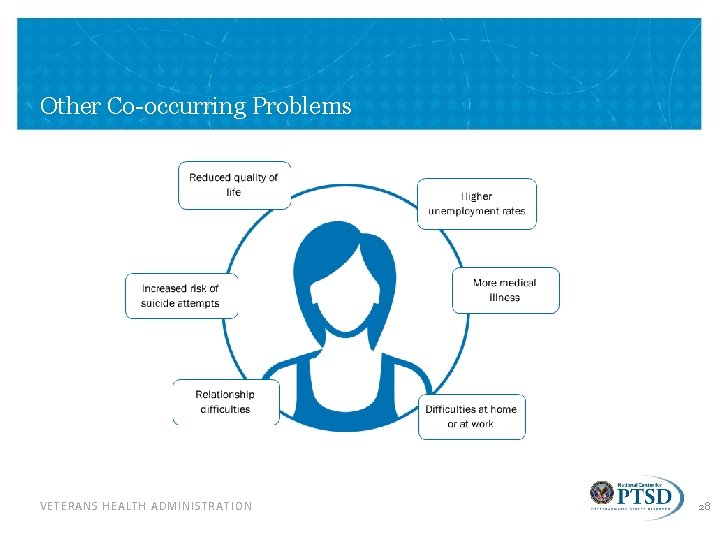
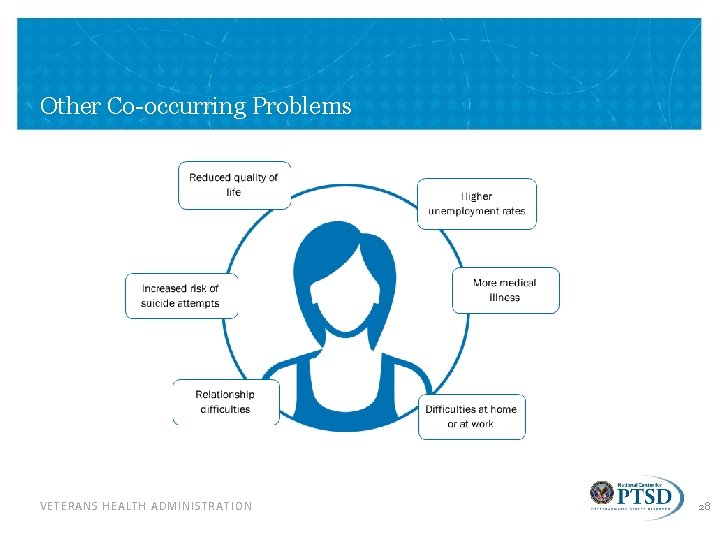
Other Co-occurring Problems VETERANS HEALTH ADMINISTRATION 28
How to Recognize PTSD in Patients https: //www. ptsd. va. gov/professional/materials/videos/index. asp VETERANS HEALTH ADMINISTRATION 29

Civilians and PTSD - It’s not just a veteran disorder https: //youtu. be/SNVATLHBVh. Y VETERANS HEALTH ADMINISTRATION 30
Diagnosing- The scales https: //www. ptsd. va. gov/professional/assessment/adult-sr/ptsd-checklist. asp Download the PTSD Checklist for DSM-5 (PCL-5): • PCL-5 (PDF) • PCL-5 with Criterion A (PDF) • PCL-5 with LEC-5 and Criterion A (PDF) • Using the PTSD Checklist for DSM-5 (PCL-5) (PDF) VETERANS HEALTH ADMINISTRATION 31
Treatment Options VETERANS HEALTH ADMINISTRATION 32
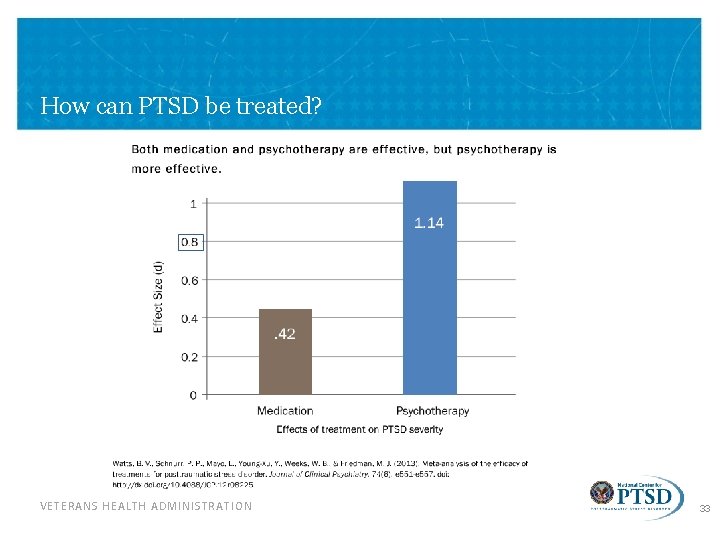
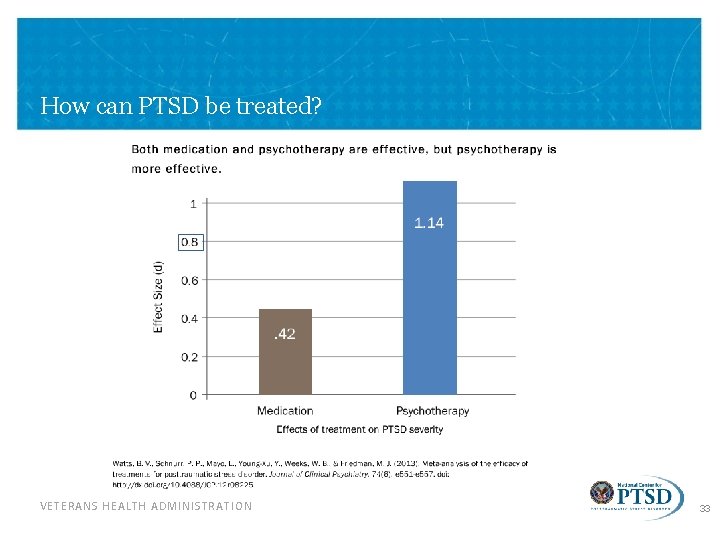
How can PTSD be treated? VETERANS HEALTH ADMINISTRATION 33
Evidence-based Pharmacological Treatments • First line medications – Selective Serotonin Reuptake Inhibitors (SSRIs) • E. g. , paroxetine (Paxil), sertraline (Zoloft) – Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) • E. g. , venlafaxine (Effexor) • Warning: Benzodiazepines (e. g. , Xanax, Valium, Klonopin) – Limited efficacy – Increased safety concerns – Not recommended for PTSD VETERANS HEALTH ADMINISTRATION 34
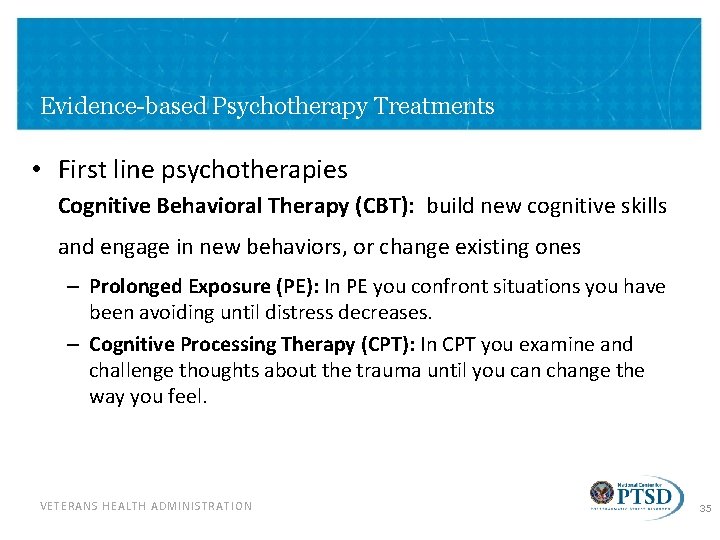
Evidence-based Psychotherapy Treatments • First line psychotherapies Cognitive Behavioral Therapy (CBT): build new cognitive skills and engage in new behaviors, or change existing ones – Prolonged Exposure (PE): In PE you confront situations you have been avoiding until distress decreases. – Cognitive Processing Therapy (CPT): In CPT you examine and challenge thoughts about the trauma until you can change the way you feel. VETERANS HEALTH ADMINISTRATION 35
CBT works with our thoughts, feelings and behaviors. CBT therapists understand that by changing the way we think and act in the here-and-now, we can affect the way we feel. CBT can also be applied longitudinally to explore the origin of beliefs, rules and assumptions which shape an individual's world-view: this knowledge can then be used to drive change in the present. There are evidence-based CBT models (and associated treatment protocols) for a wide range of disorders, but CBT can also be used to formulate (conceptualize) cases individually. VETERANS HEALTH ADMINISTRATION 36
Psychology Tools • • • https: //psychologytools. com/ptsd. html Free Easy Lots of Handouts Evidence Based VETERANS HEALTH ADMINISTRATION 37
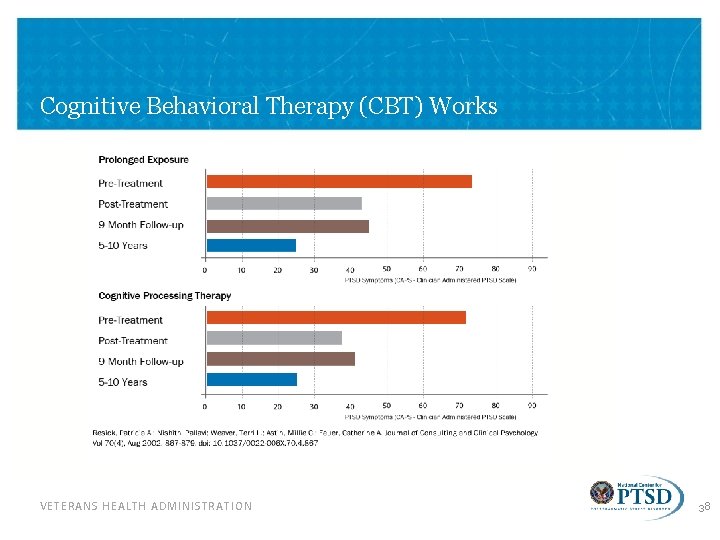
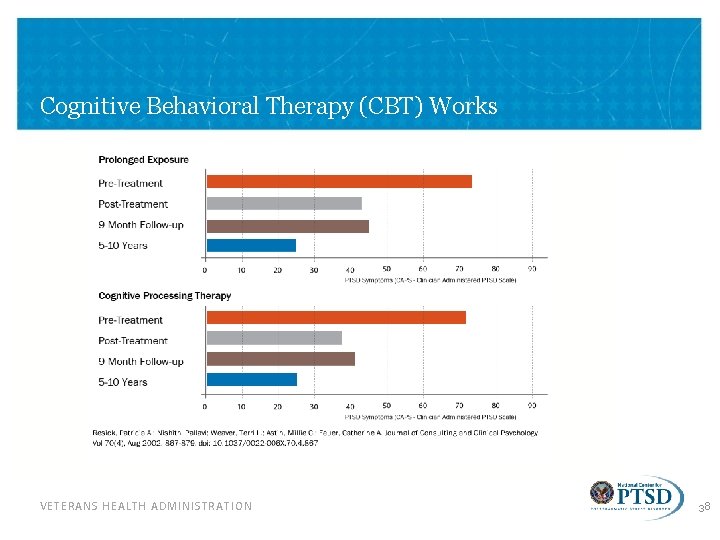
Cognitive Behavioral Therapy (CBT) Works VETERANS HEALTH ADMINISTRATION 38
Evidence-based Psychotherapy Treatments Cont. • Other VA/Do. D Clinical Practice Guideline first line psychotherapies include: – Stress Inoculation Training (SIT): By teaching coping skills, SIT can help you find new ways to deal with PTSD symptoms. These skills can also help you manage other stressful situations or event in your life. – Eye Movement Desensitization and Reprocessing (EMDR): EMDR helps you process upsetting memories, thoughts, and feelings related to trauma. In EMDR, you’ll pay attention to a back-and-forth movement or sound while you think about the upsetting memory long enough for it to become less distressing. VETERANS HEALTH ADMINISTRATION 39
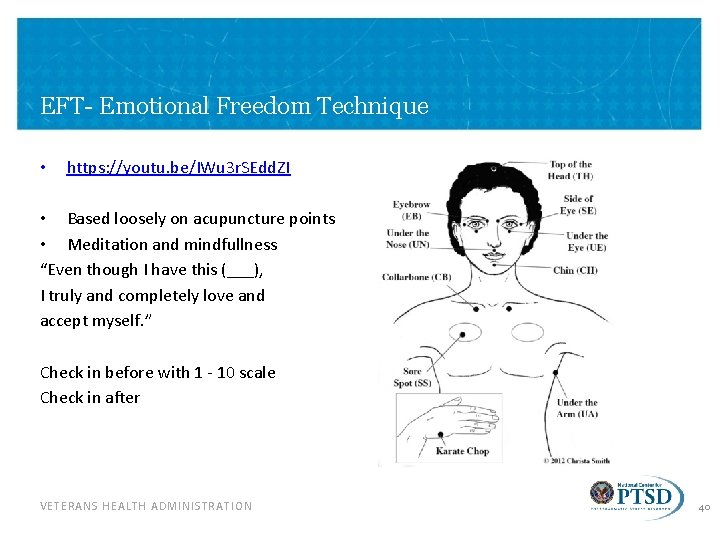
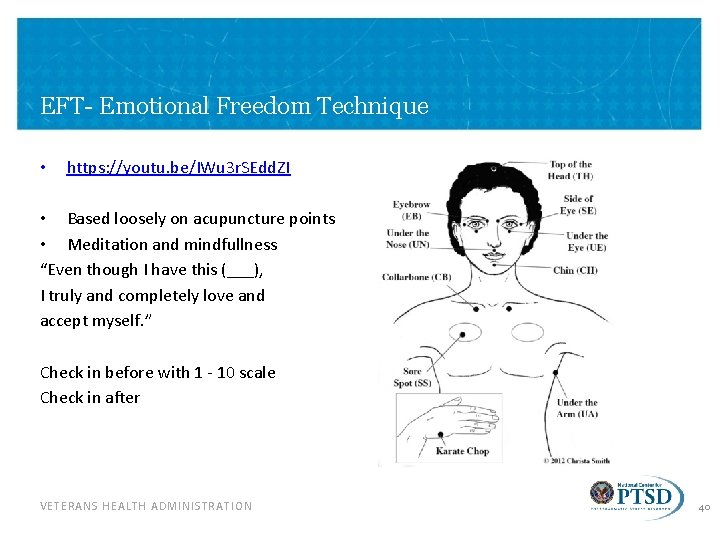
EFT- Emotional Freedom Technique • https: //youtu. be/IWu 3 r. SEdd. ZI • Based loosely on acupuncture points • Meditation and mindfullness “Even though I have this (___), I truly and completely love and accept myself. ” Check in before with 1 - 10 scale Check in after VETERANS HEALTH ADMINISTRATION 40
Resources and Tools for Professionals VETERANS HEALTH ADMINISTRATION 41
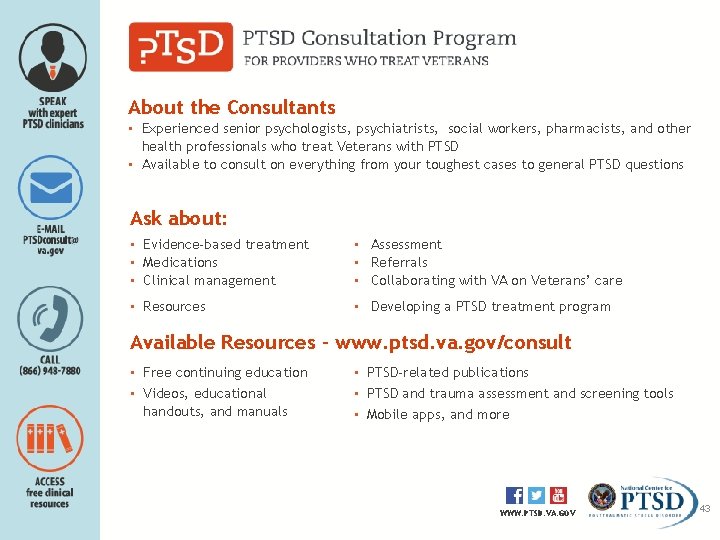
PTSDconsult@va. gov (866) 948 -7880 www. ptsd. va. gov/consult 42
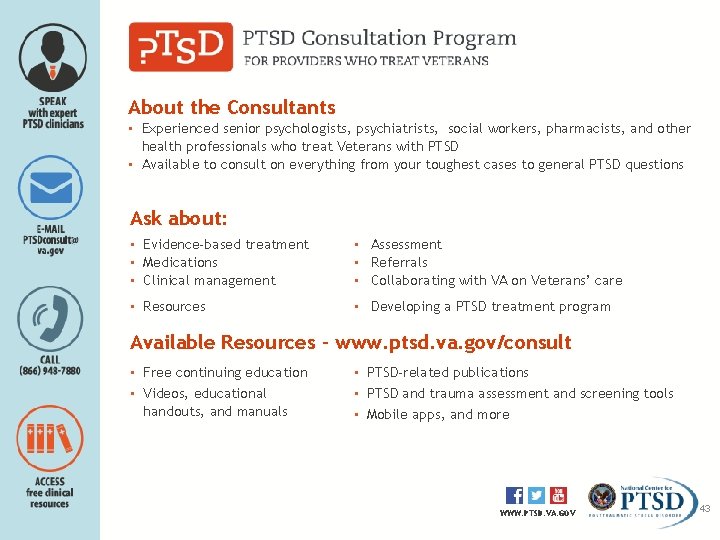
About the Consultants ▪ Experienced senior psychologists, psychiatrists, social workers, pharmacists, and other health professionals who treat Veterans with PTSD ▪ Available to consult on everything from your toughest cases to general PTSD questions Ask about: ▪ Evidence-based treatment ▪ Medications ▪ Clinical management ▪ Assessment ▪ Referrals ▪ Collaborating with VA on Veterans’ care ▪ Resources ▪ Developing a PTSD treatment program Available Resources - www. ptsd. va. gov/consult ▪ Free continuing education ▪ Videos, educational handouts, and manuals ▪ PTSD-related publications ▪ PTSD and trauma assessment and screening tools ▪ Mobile apps, and more WWW. PTSD. VA. GOV 43
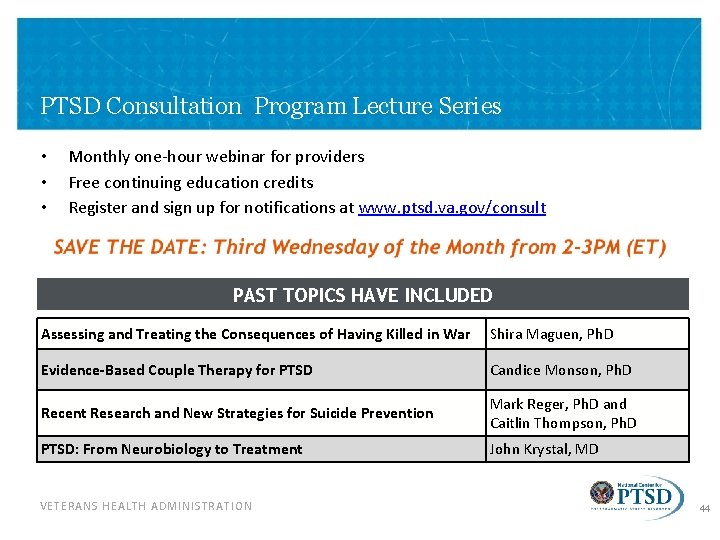
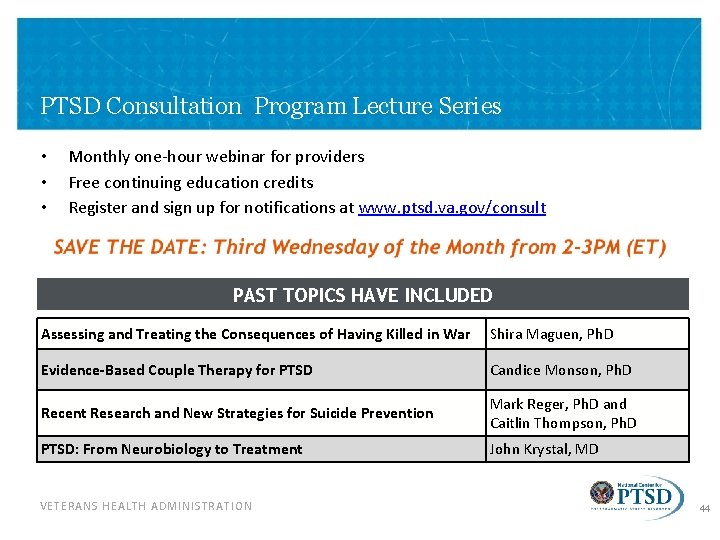
PTSD Consultation Program Lecture Series • • • Monthly one-hour webinar for providers Free continuing education credits Register and sign up for notifications at www. ptsd. va. gov/consult PAST TOPICS HAVE INCLUDED Assessing and Treating the Consequences of Having Killed in War Shira Maguen, Ph. D Evidence-Based Couple Therapy for PTSD Candice Monson, Ph. D Recent Research and New Strategies for Suicide Prevention Mark Reger, Ph. D and Caitlin Thompson, Ph. D PTSD: From Neurobiology to Treatment John Krystal, MD VETERANS HEALTH ADMINISTRATION 44
Continuing Education Courses • NCPTSD offers well over 50 hours of web-based courses for professionals. • • All courses are free. Most offer continuing education for multiple disciplines. Available to Anyone For VA Staff VETERANS HEALTH ADMINISTRATION 45
Trauma and PTSD: Stay Up-To-Date • NCPTSD works to bring the most current research on trauma and PTSD to professionals. • Each of our publications are free e-subscriptions. VETERANS HEALTH ADMINISTRATION 46
PTSD Awareness in Health Care Settings VETERANS HEALTH ADMINISTRATION • PTSD Awareness is a 15 -minute video that shares the stories of three Veterans being seen at VA for PTSD care. • Models strategies to improve interactions in health care settings with Veterans who have PTSD and trauma histories. • A Facilitator Guide is also available for those offering a training to medical staff. 47
PTSD Assessment VETERANS HEALTH ADMINISTRATION • We provide information on a variety of measures assessing trauma and PTSD. • We also offer online courses about best practices. • Most NCPTSD authored measures are available for direct download by qualified mental health professionals on our website. 48
Animated Whiteboard Videos • NCPTSD created a series of whiteboards, including one for professionals about PTSD and effective treatments. • Short (~3 minute), engaging videos that are easily shared via email or Facebook. VETERANS HEALTH ADMINISTRATION 49
About. Face VETERANS HEALTH ADMINISTRATION 50
About. Face: Product Goals • Knowing about PTSD does not necessarily mean that someone recognizes PTSD in themselves. • Goal: Present real stories to help users identify if they have PTSD and break down barriers to seeking care. – Present testimonials of how bad it can get with PTSD (e. g. , family, functioning, co-occurring conditions, etc. ). – Highlight that treatment helps. – Offer advice from Veterans and family members who have been there and turned their lives around with treatment. – Offer videos of VA clinicians talking in plain language about their experiencing treating Veterans with PTSD. – Link to fact sheets on the NCPTSD website. VETERANS HEALTH ADMINISTRATION 51

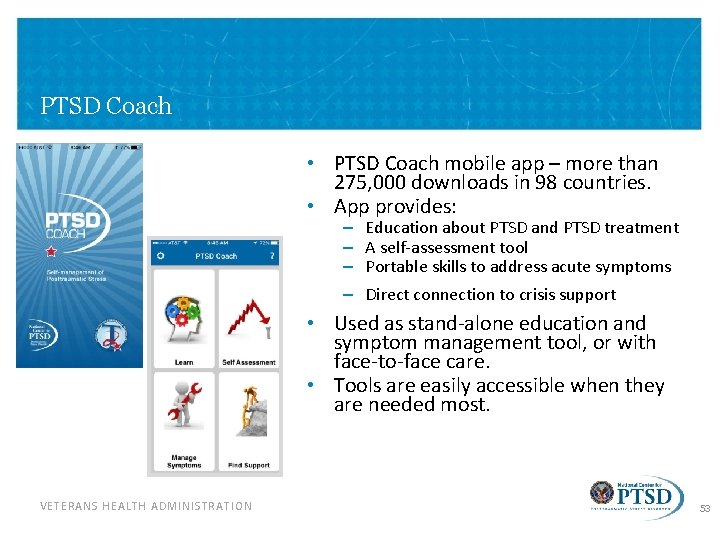
Mobile Apps • NCPTSD has partnered with a number of organizations to develop a variety of mobile apps. • Apps are focused on PTSD, related health problems (e. g. , insomnia, alcohol use, etc. ), or general wellbeing. • There apps for patients, providers, and for use with patient -provider dyads. VETERANS HEALTH ADMINISTRATION 52
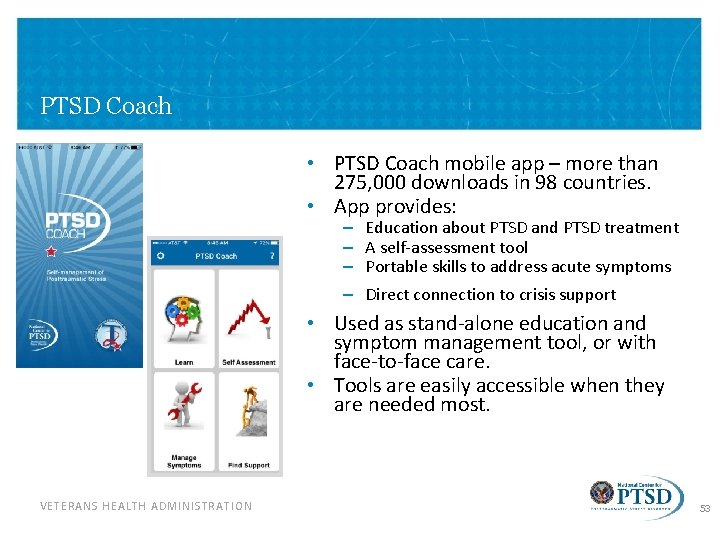
PTSD Coach • PTSD Coach mobile app – more than 275, 000 downloads in 98 countries. • App provides: – – Education about PTSD and PTSD treatment A self-assessment tool Portable skills to address acute symptoms Direct connection to crisis support • Used as stand-alone education and symptom management tool, or with face-to-face care. • Tools are easily accessible when they are needed most. VETERANS HEALTH ADMINISTRATION 53
![Thank you Insert Contact Information Visit the National Center for PTSD at www ptsd Thank you! [Insert Contact Information] Visit the National Center for PTSD at: www. ptsd.](https://slidetodoc.com/presentation_image_h/a97d574f24c3d739ac17df3846892414/image-54.jpg)
Thank you! [Insert Contact Information] Visit the National Center for PTSD at: www. ptsd. va. gov VETERANS HEALTH ADMINISTRATION 54