Adaptive Defense System Third Line of Defense Immune
- Slides: 25
Adaptive Defense System Third Line of Defense • Immune response - response to a threat that targets specific antigens • 2 types of immunity: – Humoral immunity = antibody-mediated • Provided by antibodies present in body fluids – Cellular immunity = cell-mediated • Targets virus-infected cells, cancer cells, and cells of foreign grafts
• Antigens (nonself) – Any substance capable of exciting the immune system and provoking an immune response – Examples: • Foreign proteins (strongest) • • • Nucleic acids Large carbohydrates Some lipids Pollen grains Microorganisms restricts donors for transplants • Self-antigens – Your immune cells do not attack your own cell surface proteins
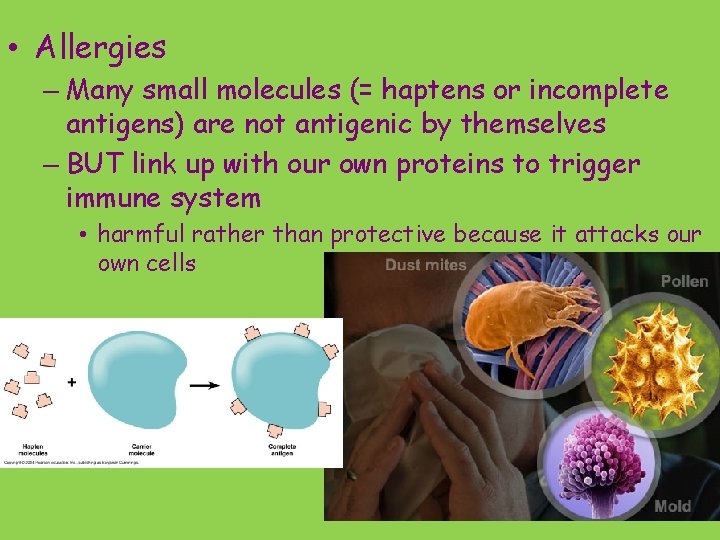
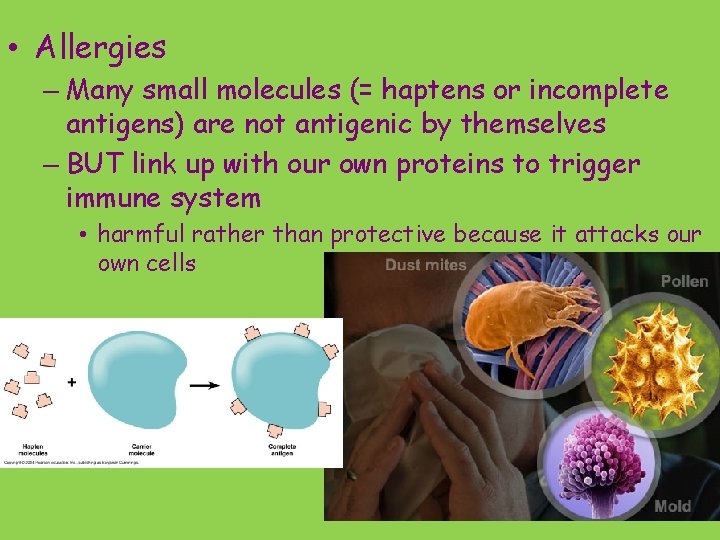
• Allergies – Many small molecules (= haptens or incomplete antigens) are not antigenic by themselves – BUT link up with our own proteins to trigger immune system • harmful rather than protective because it attacks our own cells
• Cells of the adaptive defense system: – Lymphocytes respond to specific antigens • What type of cell a hemocytoblast turns into depends on where it becomes immunocompetent – capable of responding to specific antigen by binding to it – B lymphocytes (B cells) – in bone marrow – T lymphocytes (T cells) – in thymus – Macrophages help lymphocytes • Arise from monocytes • In lymphoid organs • Secrete cytokines (= proteins important in the immune response)
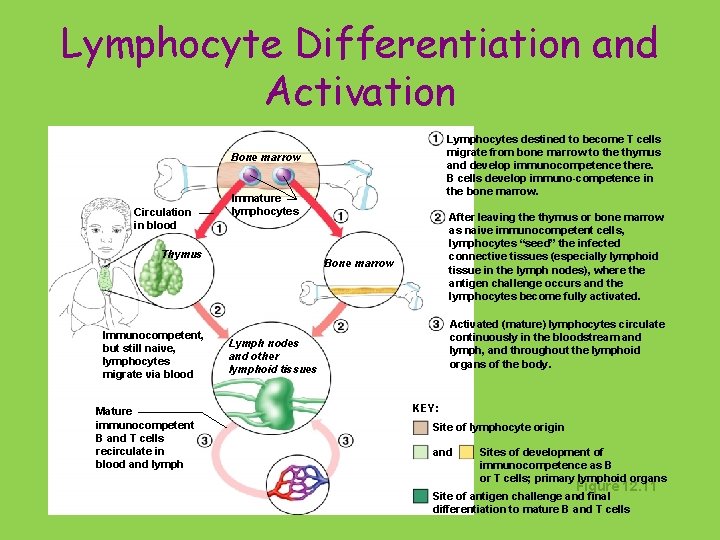
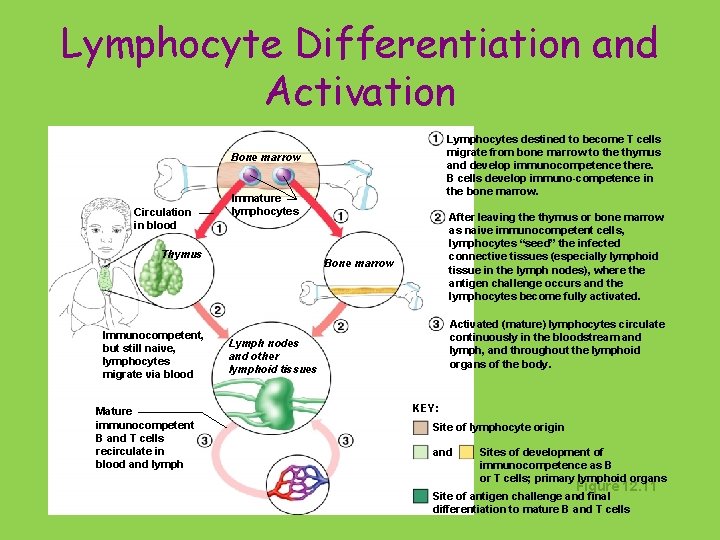
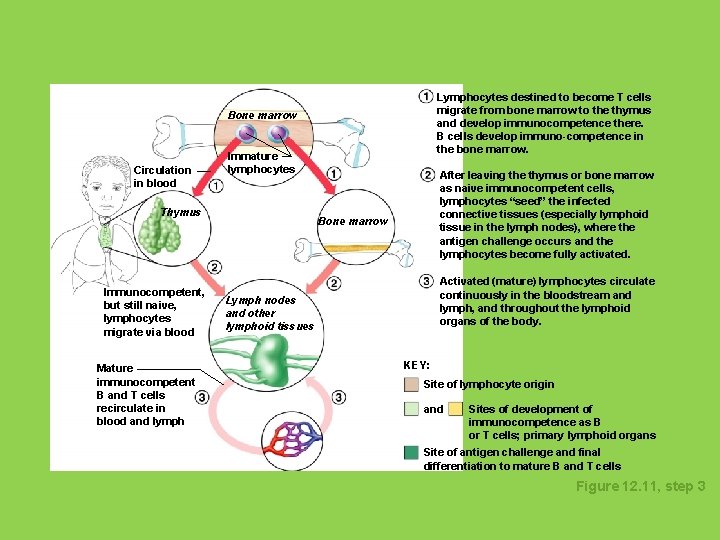
Lymphocyte Differentiation and Activation Lymphocytes destined to become T cells migrate from bone marrow to the thymus and develop immunocompetence there. B cells develop immuno-competence in the bone marrow. Bone marrow Circulation in blood Immature lymphocytes Thymus Immunocompetent, but still naive, lymphocytes migrate via blood Mature immunocompetent B and T cells recirculate in blood and lymph After leaving the thymus or bone marrow as naive immunocompetent cells, lymphocytes “seed” the infected connective tissues (especially lymphoid tissue in the lymph nodes), where the antigen challenge occurs and the lymphocytes become fully activated. Bone marrow Activated (mature) lymphocytes circulate continuously in the bloodstream and lymph, and throughout the lymphoid organs of the body. Lymph nodes and other lymphoid tissues KEY: Site of lymphocyte origin and Sites of development of immunocompetence as B or T cells; primary lymphoid organs Figure 12. 11 Site of antigen challenge and final differentiation to mature B and T cells
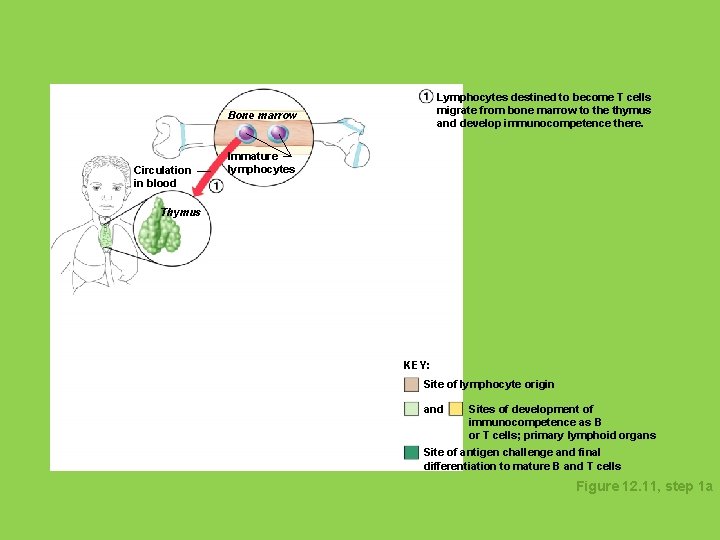
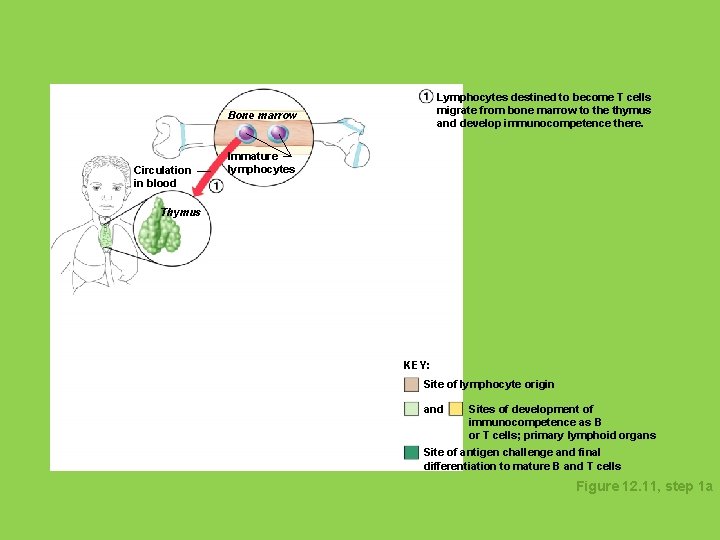
Lymphocytes destined to become T cells migrate from bone marrow to the thymus and develop immunocompetence there. Bone marrow Circulation in blood Immature lymphocytes Thymus KEY: Site of lymphocyte origin and Sites of development of immunocompetence as B or T cells; primary lymphoid organs Site of antigen challenge and final differentiation to mature B and T cells Figure 12. 11, step 1 a
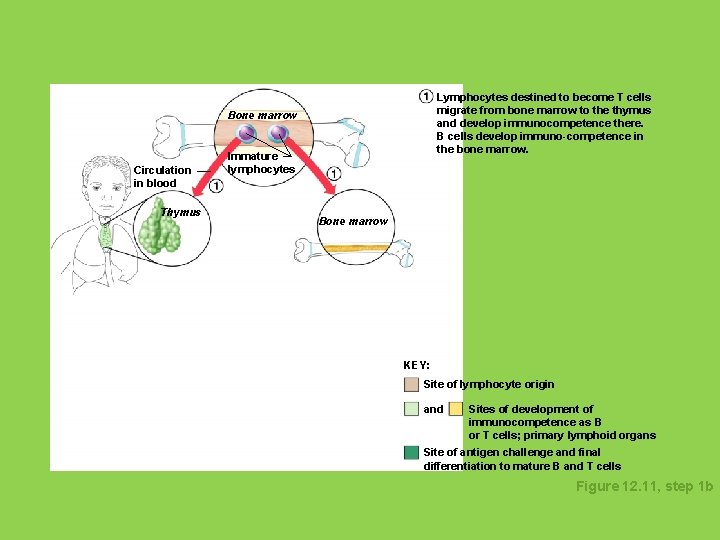
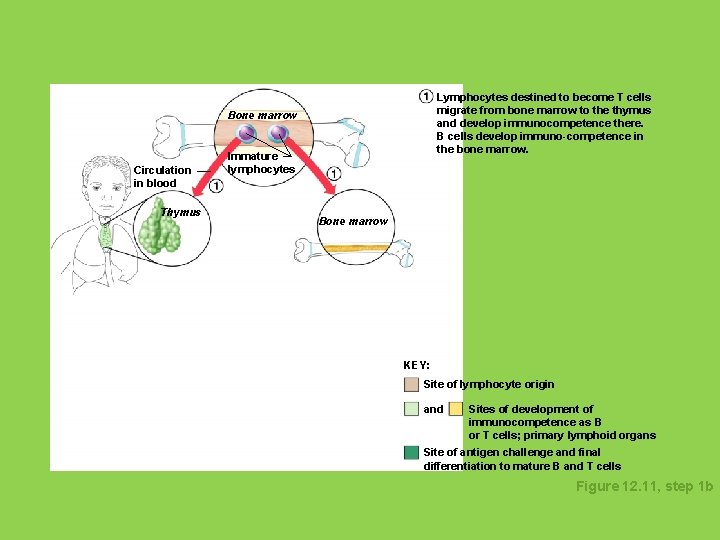
Lymphocytes destined to become T cells migrate from bone marrow to the thymus and develop immunocompetence there. B cells develop immuno-competence in the bone marrow. Bone marrow Circulation in blood Thymus Immature lymphocytes Bone marrow KEY: Site of lymphocyte origin and Sites of development of immunocompetence as B or T cells; primary lymphoid organs Site of antigen challenge and final differentiation to mature B and T cells Figure 12. 11, step 1 b
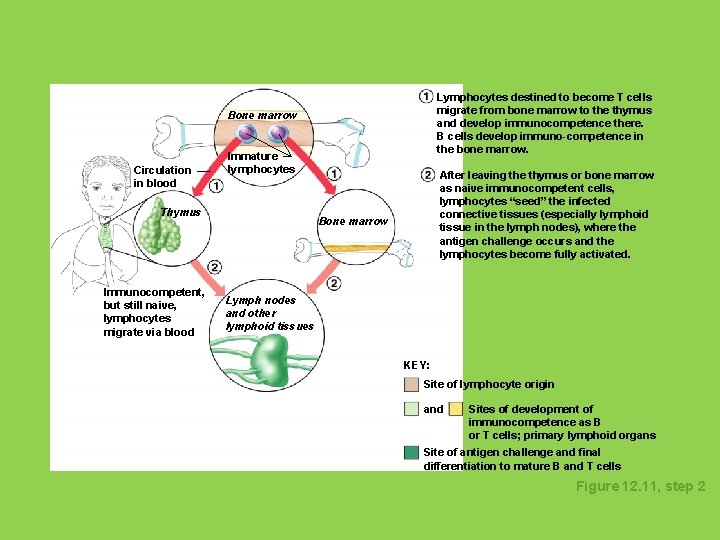
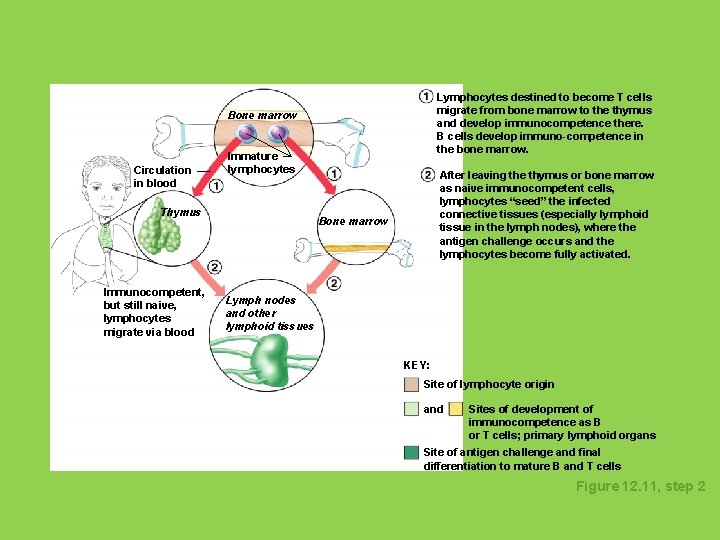
Lymphocytes destined to become T cells migrate from bone marrow to the thymus and develop immunocompetence there. B cells develop immuno-competence in the bone marrow. Bone marrow Circulation in blood Immature lymphocytes Thymus Immunocompetent, but still naive, lymphocytes migrate via blood After leaving the thymus or bone marrow as naive immunocompetent cells, lymphocytes “seed” the infected connective tissues (especially lymphoid tissue in the lymph nodes), where the antigen challenge occurs and the lymphocytes become fully activated. Bone marrow Lymph nodes and other lymphoid tissues KEY: Site of lymphocyte origin and Sites of development of immunocompetence as B or T cells; primary lymphoid organs Site of antigen challenge and final differentiation to mature B and T cells Figure 12. 11, step 2
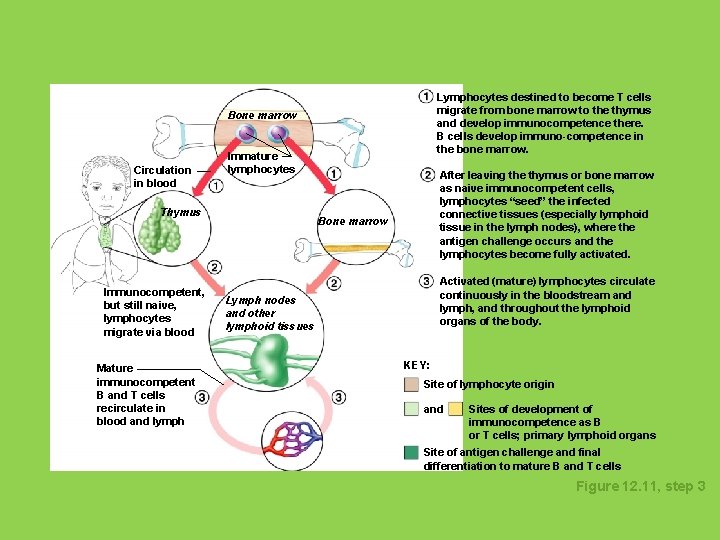
Lymphocytes destined to become T cells migrate from bone marrow to the thymus and develop immunocompetence there. B cells develop immuno-competence in the bone marrow. Bone marrow Circulation in blood Immature lymphocytes Thymus Immunocompetent, but still naive, lymphocytes migrate via blood Mature immunocompetent B and T cells recirculate in blood and lymph After leaving the thymus or bone marrow as naive immunocompetent cells, lymphocytes “seed” the infected connective tissues (especially lymphoid tissue in the lymph nodes), where the antigen challenge occurs and the lymphocytes become fully activated. Bone marrow Activated (mature) lymphocytes circulate continuously in the bloodstream and lymph, and throughout the lymphoid organs of the body. Lymph nodes and other lymphoid tissues KEY: Site of lymphocyte origin and Sites of development of immunocompetence as B or T cells; primary lymphoid organs Site of antigen challenge and final differentiation to mature B and T cells Figure 12. 11, step 3
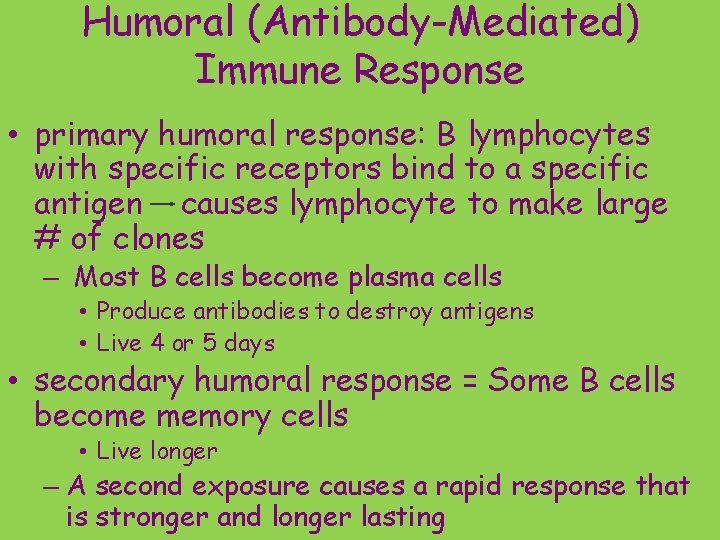
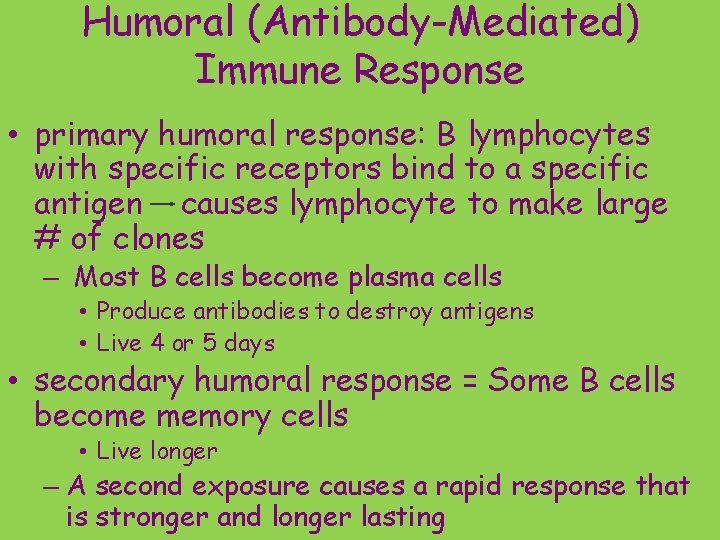
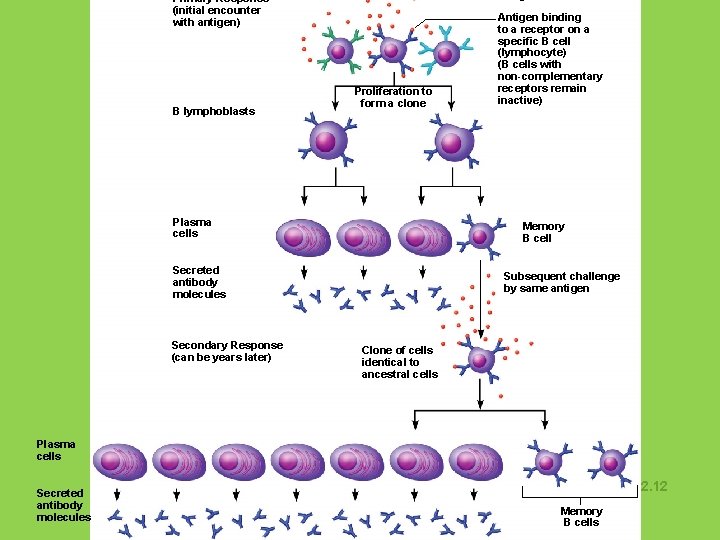
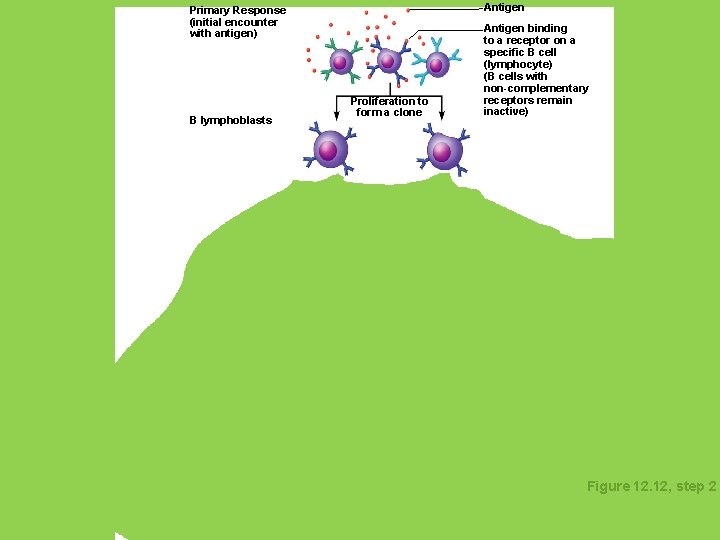
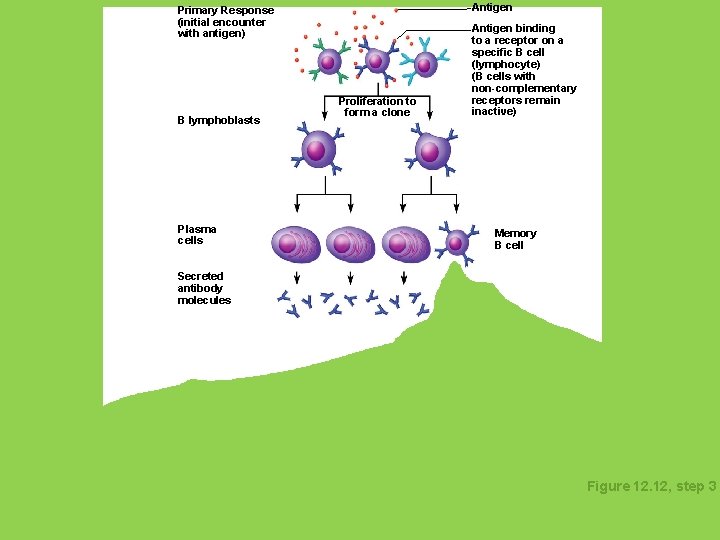
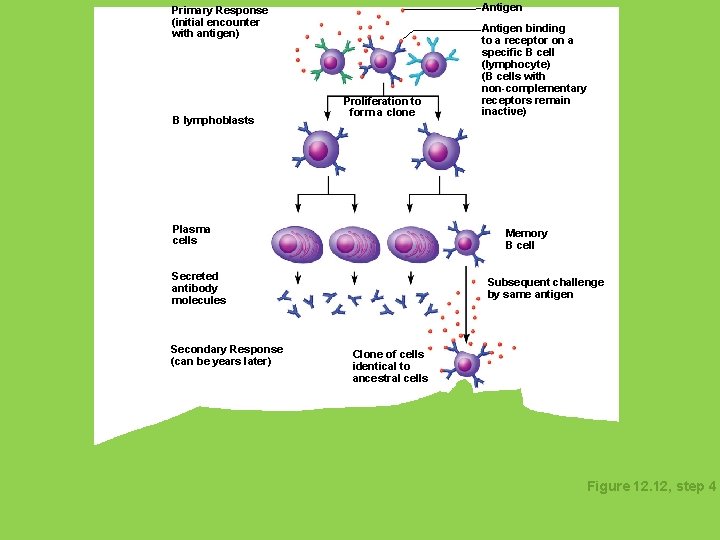
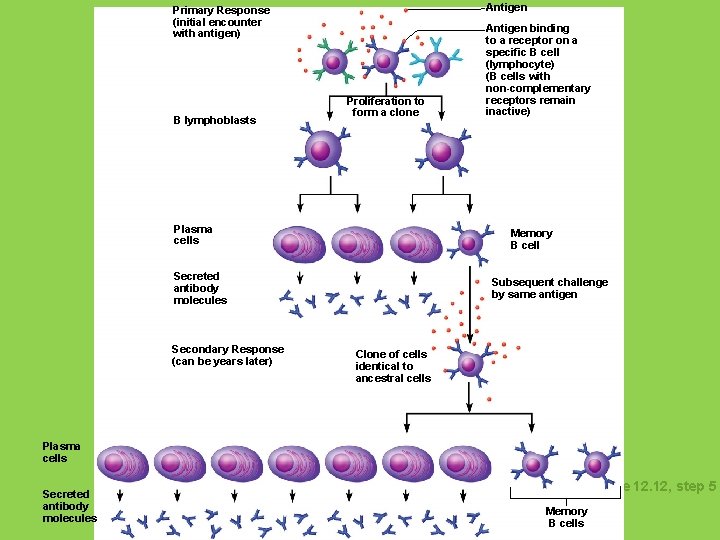
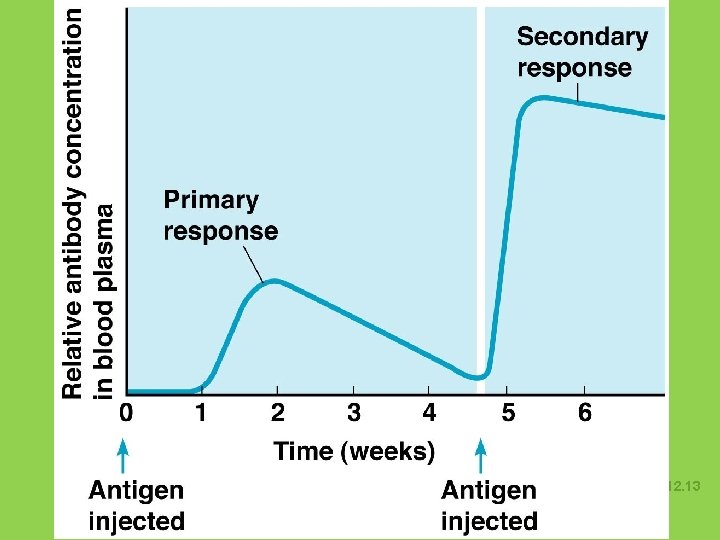
Humoral (Antibody-Mediated) Immune Response • primary humoral response: B lymphocytes with specific receptors bind to a specific antigen causes lymphocyte to make large # of clones – Most B cells become plasma cells • Produce antibodies to destroy antigens • Live 4 or 5 days • secondary humoral response = Some B cells become memory cells • Live longer – A second exposure causes a rapid response that is stronger and longer lasting
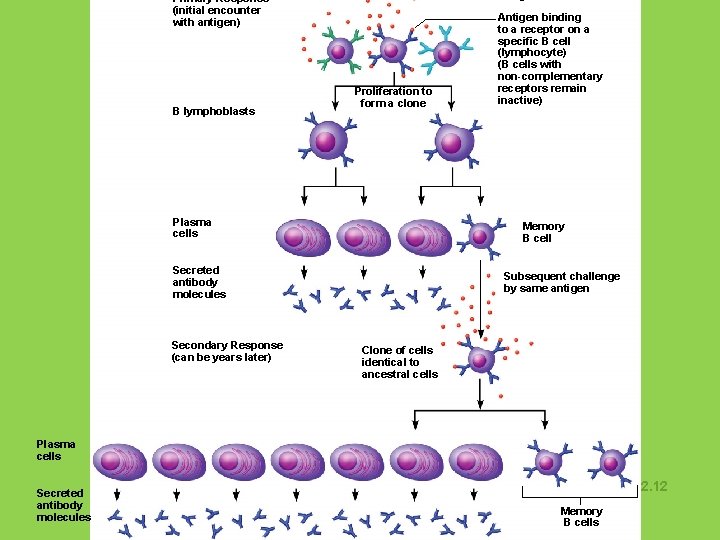
Primary Response (initial encounter with antigen) B lymphoblasts Proliferation to form a clone Plasma cells Memory B cell Secreted antibody molecules Secondary Response (can be years later) Antigen binding to a receptor on a specific B cell (lymphocyte) (B cells with non-complementary receptors remain inactive) Subsequent challenge by same antigen Clone of cells identical to ancestral cells Plasma cells Secreted antibody molecules Figure 12. 12 Memory B cells
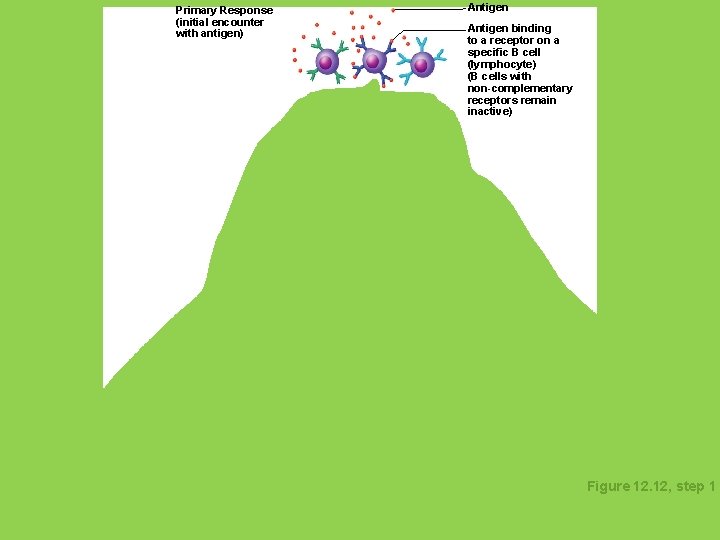
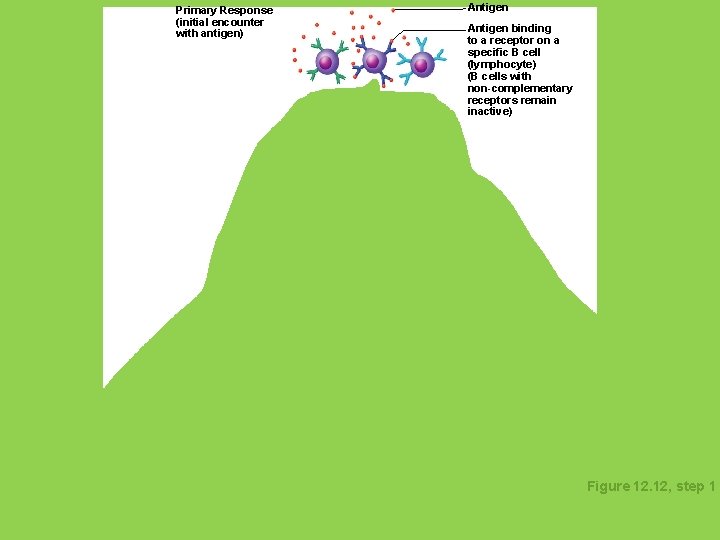
Primary Response (initial encounter with antigen) Antigen binding to a receptor on a specific B cell (lymphocyte) (B cells with non-complementary receptors remain inactive) Figure 12. 12, step 1
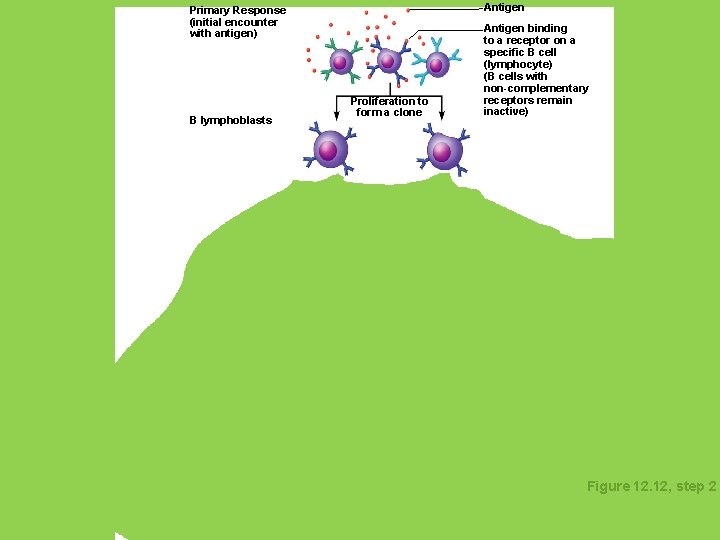
Antigen Primary Response (initial encounter with antigen) B lymphoblasts Proliferation to form a clone Antigen binding to a receptor on a specific B cell (lymphocyte) (B cells with non-complementary receptors remain inactive) Figure 12. 12, step 2
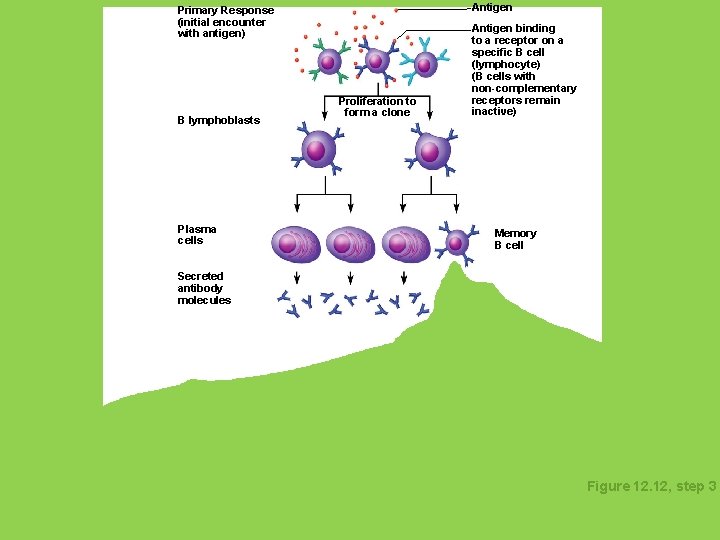
Antigen Primary Response (initial encounter with antigen) B lymphoblasts Plasma cells Proliferation to form a clone Antigen binding to a receptor on a specific B cell (lymphocyte) (B cells with non-complementary receptors remain inactive) Memory B cell Secreted antibody molecules Figure 12. 12, step 3
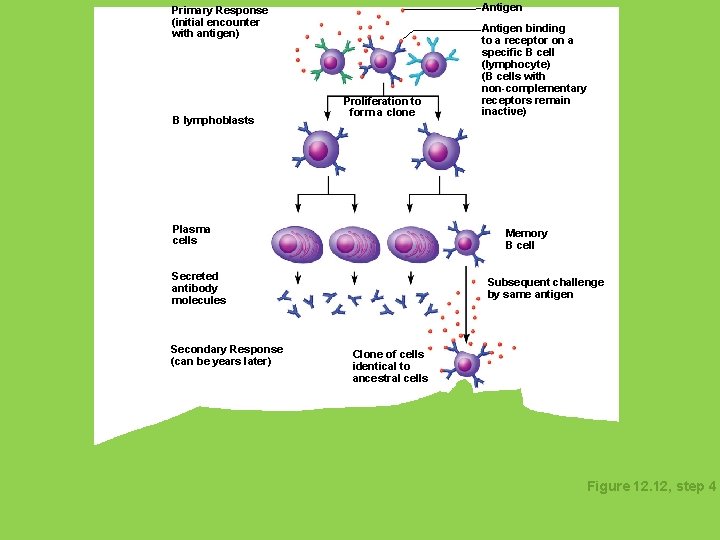
Antigen Primary Response (initial encounter with antigen) B lymphoblasts Proliferation to form a clone Plasma cells Memory B cell Secreted antibody molecules Secondary Response (can be years later) Antigen binding to a receptor on a specific B cell (lymphocyte) (B cells with non-complementary receptors remain inactive) Subsequent challenge by same antigen Clone of cells identical to ancestral cells Figure 12. 12, step 4
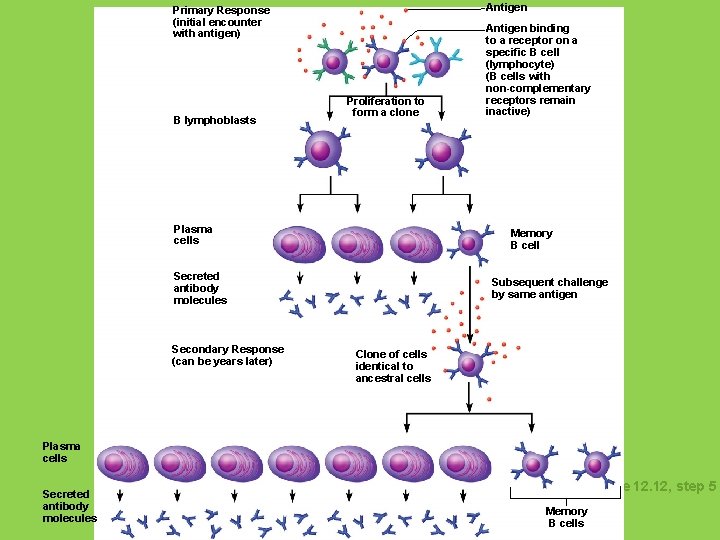
Antigen Primary Response (initial encounter with antigen) B lymphoblasts Proliferation to form a clone Plasma cells Memory B cell Secreted antibody molecules Secondary Response (can be years later) Antigen binding to a receptor on a specific B cell (lymphocyte) (B cells with non-complementary receptors remain inactive) Subsequent challenge by same antigen Clone of cells identical to ancestral cells Plasma cells Secreted antibody molecules Figure 12. 12, step 5 Memory B cells
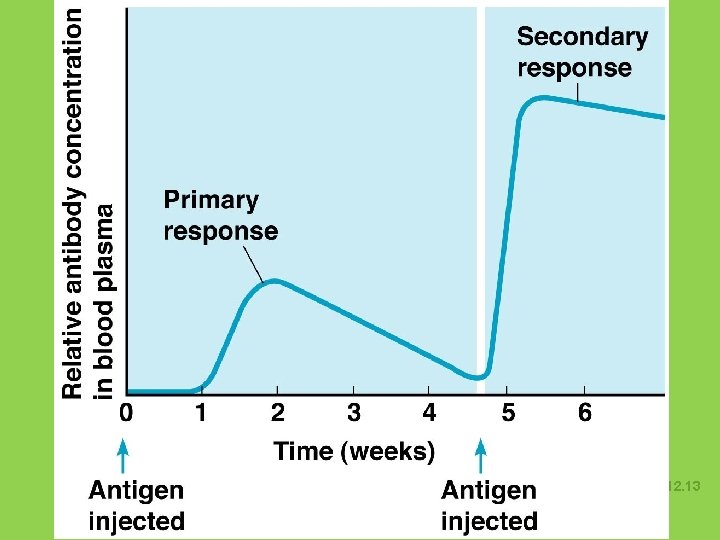
Humoral Immune Response Figure 12. 13
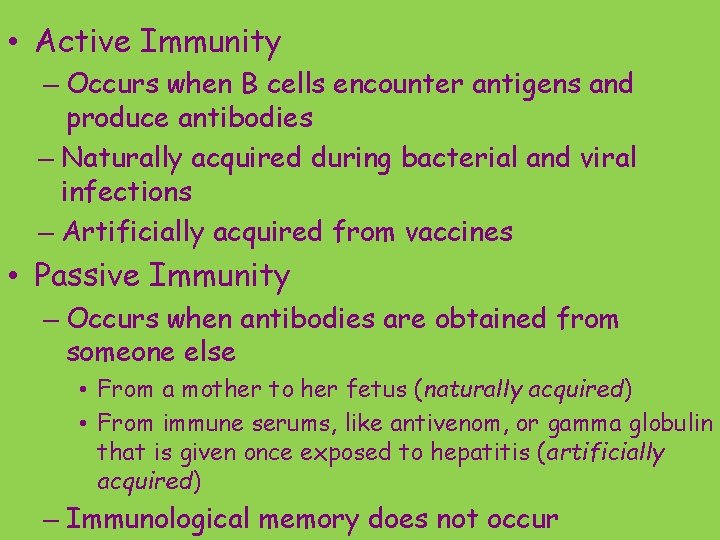
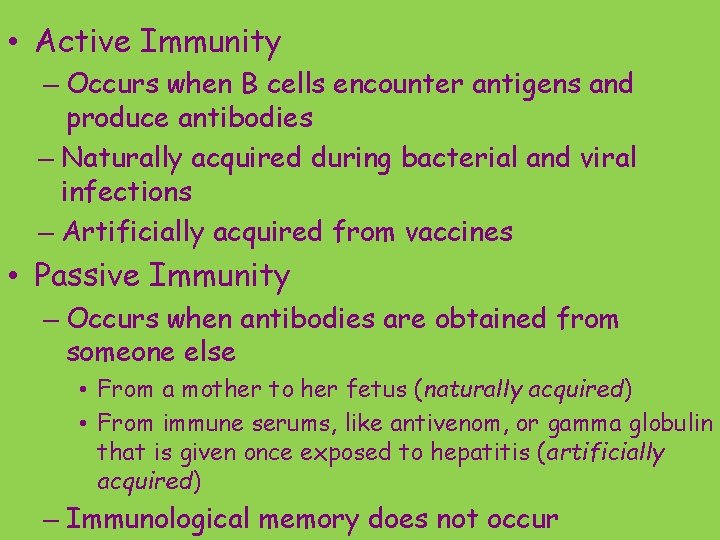
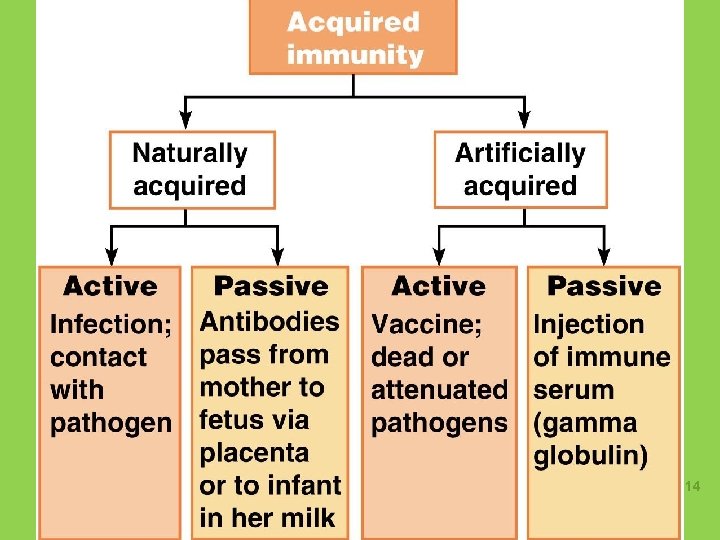
• Active Immunity – Occurs when B cells encounter antigens and produce antibodies – Naturally acquired during bacterial and viral infections – Artificially acquired from vaccines • Passive Immunity – Occurs when antibodies are obtained from someone else • From a mother to her fetus (naturally acquired) • From immune serums, like antivenom, or gamma globulin that is given once exposed to hepatitis (artificially acquired) – Immunological memory does not occur
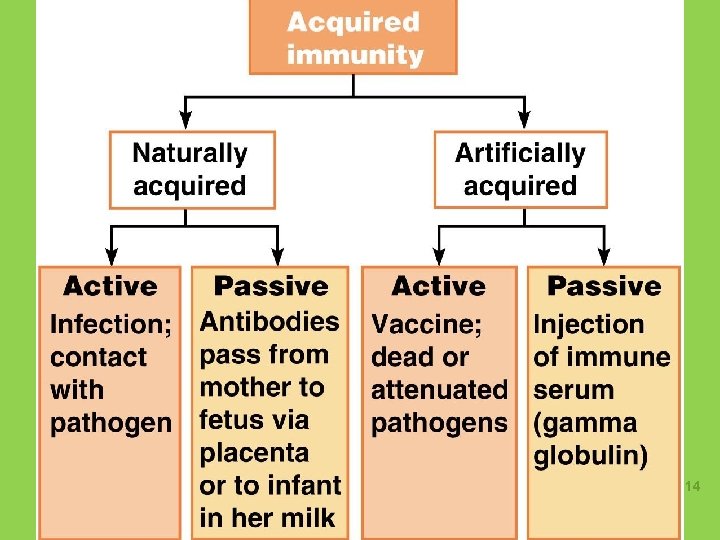
Types of Acquired Immunity Figure 12. 14
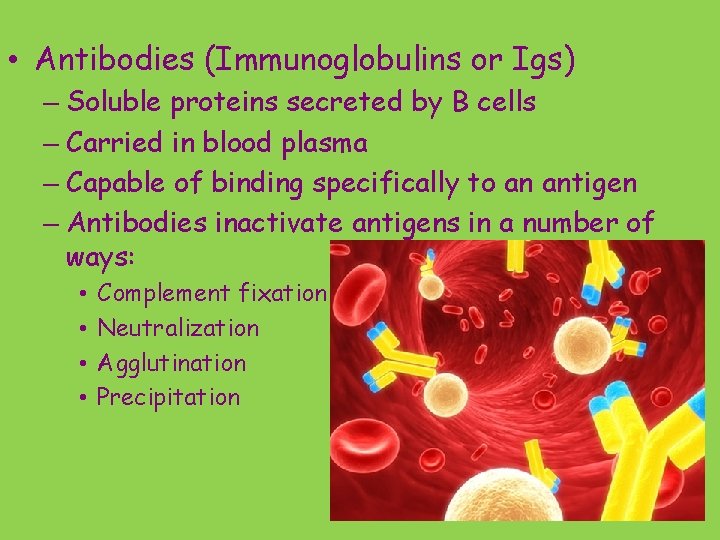
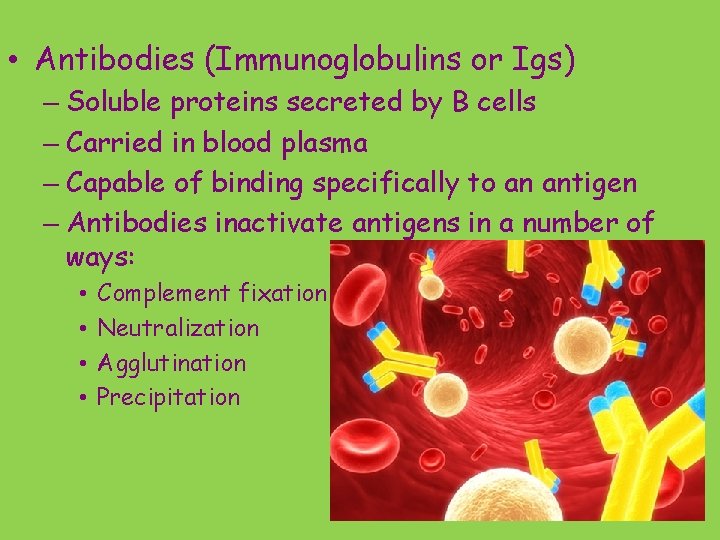
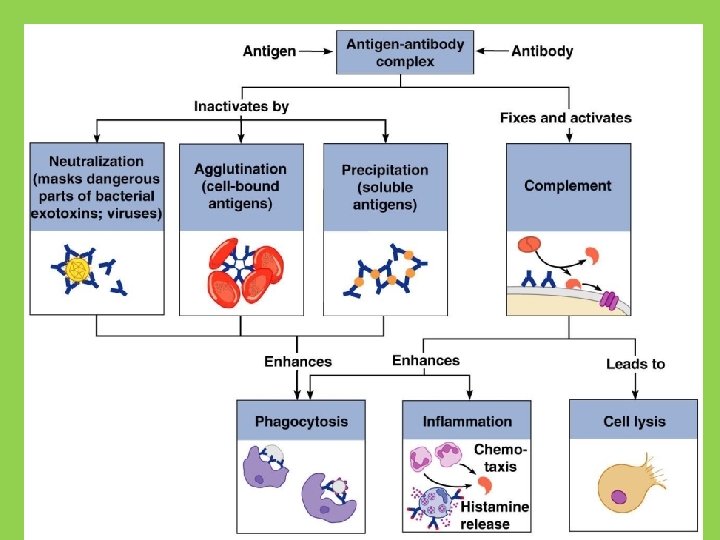
• Antibodies (Immunoglobulins or Igs) – Soluble proteins secreted by B cells – Carried in blood plasma – Capable of binding specifically to an antigen – Antibodies inactivate antigens in a number of ways: • • Complement fixation Neutralization Agglutination Precipitation
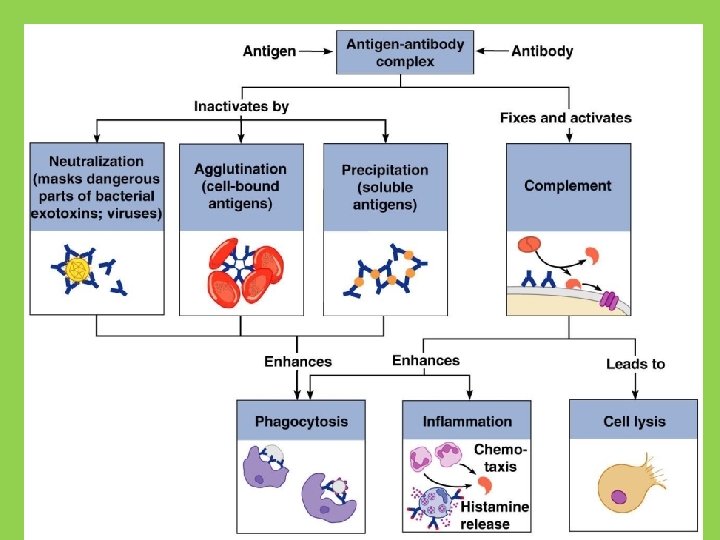
Antibody Function Figure 12. 16
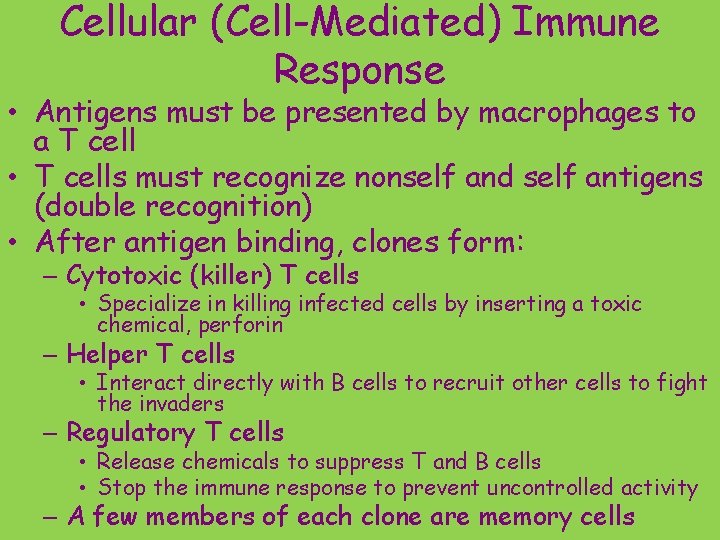
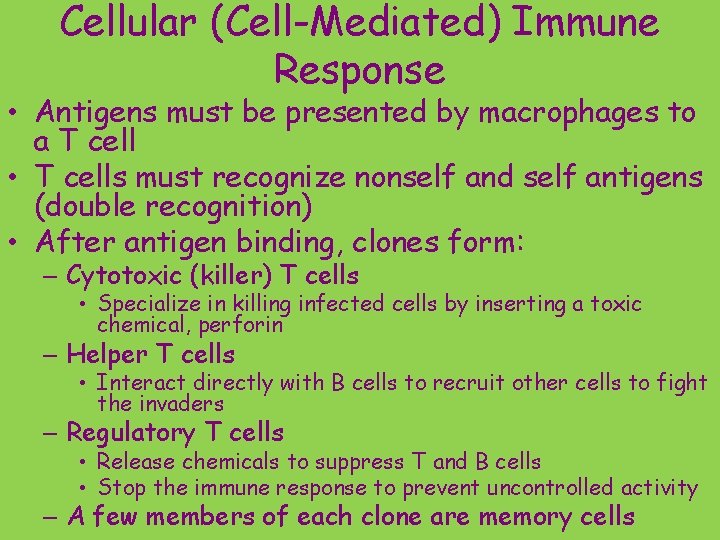
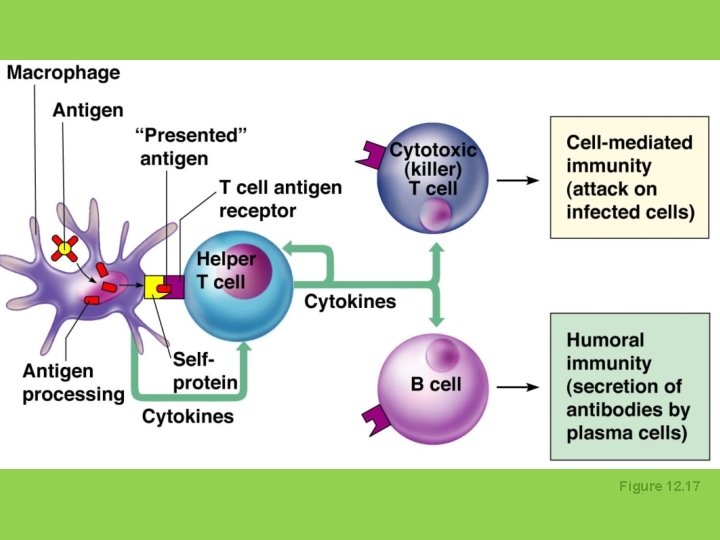
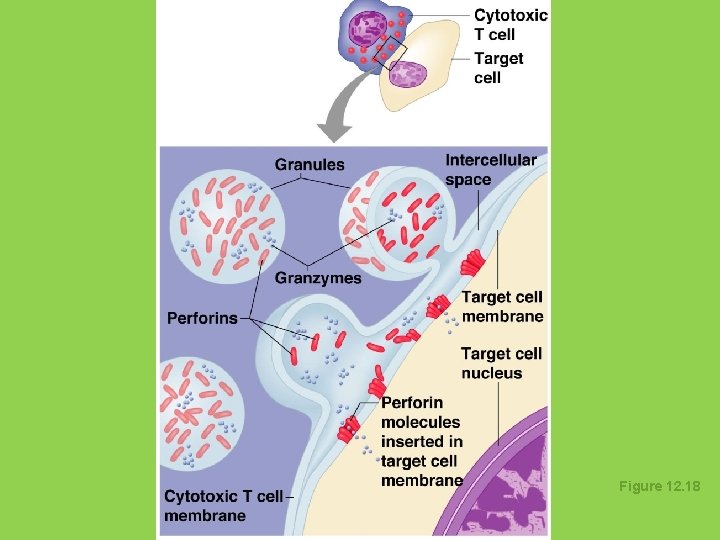
Cellular (Cell-Mediated) Immune Response • Antigens must be presented by macrophages to a T cell • T cells must recognize nonself and self antigens (double recognition) • After antigen binding, clones form: – Cytotoxic (killer) T cells • Specialize in killing infected cells by inserting a toxic chemical, perforin – Helper T cells • Interact directly with B cells to recruit other cells to fight the invaders – Regulatory T cells • Release chemicals to suppress T and B cells • Stop the immune response to prevent uncontrolled activity – A few members of each clone are memory cells
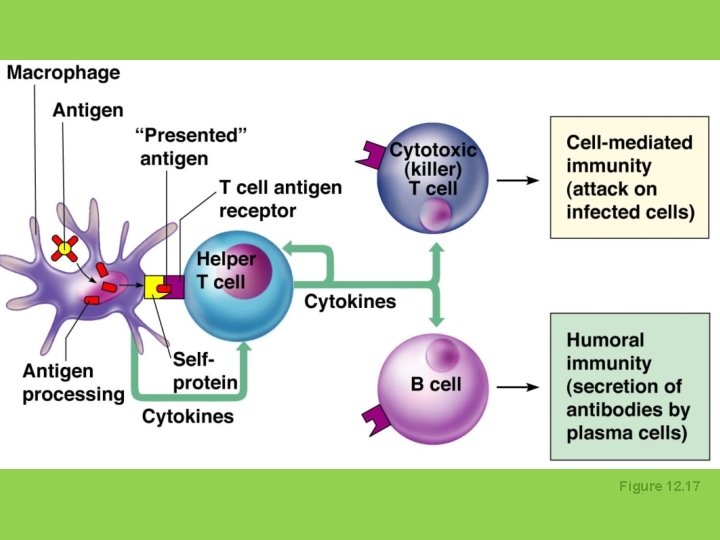
Figure 12. 17
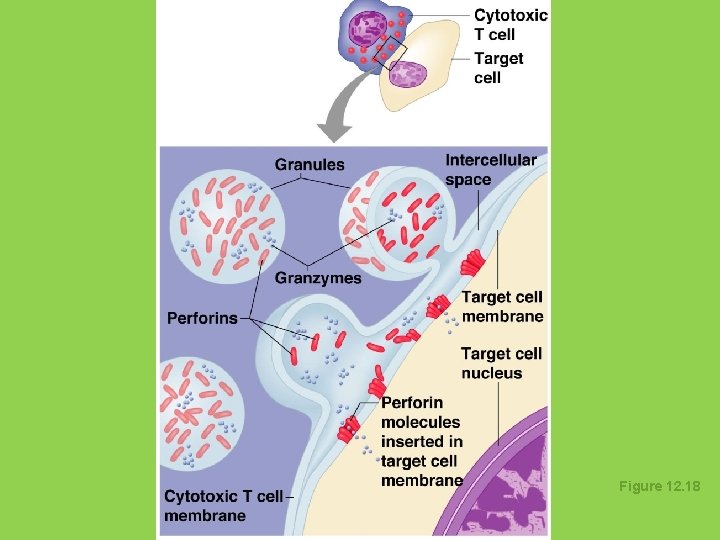
Figure 12. 18
Organ Transplants and Rejection • Major types of grafts 1. Autografts—tissue transplanted from one site to another on the same person 2. Isografts—tissue from an identical twin • Autografts and isografts are most ideal donors 3. Allografts—tissue from an unrelated person • Most commonly used (from cadaver) 4. Xenografts—tissue from a different animal • Whole organs are never successful but can use pig heart valves in humans