ACUTE VIRAL HEPATITIS IN CHILDREN Dr Shamshad Khan


- Slides: 59
ACUTE VIRAL HEPATITIS IN CHILDREN Dr. Shamshad Khan Deparment of Pediatrics. YENPOYA MEDICAL COLLEGE
Acute Viral Hepatitis A major health problem in both developing and developed countries Definition: An inflammatory disorder of the liver which is usually associated with a complete clinical and histological recovery within a period of 4 -6 weeks
Acute Viral Hepatitis Viruses affect liver in two ways directly – hepatotropic viruses Hepatitis A, B, C, D, E, G. as a part of systemic disease eg: Epstein Barr virus Herpes simplex virus Coxsackie B virus Cytomegalo virus
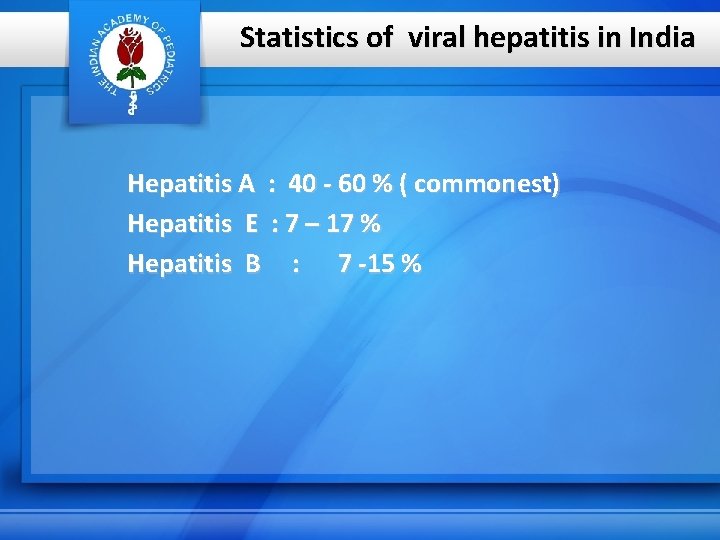
Statistics of viral hepatitis in India Hepatitis A : 40 - 60 % ( commonest) Hepatitis E : 7 – 17 % Hepatitis B : 7 -15 %
Hepatitis A • In India, > 90% of children are naturally exposed to HAV by the age of 10 years • HAV : entero virus of Picorna viridae • Causes 50 -80% of acute sporadic hepatitis in India • Relatively benign disease
Pathogenesis • Transmission by faeco- oral route • Reaches liver by portal vein • Replicates in the liver and excreted in the bile • Stool is the infective material (highest concentration in the stool 2 weeks prior to the onset of jaundice and decline rapidly after jaundice appears. )
Routes of transmission Faeco oral: • Direct transmission (person to person) by contaminated hands or eating utensils • Through contaminated food or milk or water • Water-borne : more in developing countries, related to overcrowding, poor hygiene and poor sanitation • Food borne : more in developed countries through infected food handlers, uncooked foods Parenteral transmission ? very rare
Clinical manifestations • Incubation period : 2 -7 weeks • 85 % cases anicteric in children • Prodromal period mild, characterized by anorexia, nausea, vomiting, fever, abdominal pain, then jaundice. • Recovers in 7 – 14 days • Chronicity less
Lab. findings Liver function tests • S. bilirubin : increased ( usually < 10 mg /dl) • Enzymes : ALT AST elevated Alk. Phosphatase Prothrombin time : prolonged in severe liver damage
Ig M anti HAV antibodies : appears during late incubation period and reaches peak by 2 -3 weeks ; disappears by after 3 -4 months
Complications of Viral hepatitis A • Cholestatic hepatitis more in older children and adolescents lasts for 40 -110 days with severe itching good prognosis • Fulminant hepatitis rare ( < 0. 1%)
Complications contd…. . Relapsing hepatitis relapse 3 -90 days later occurs in 10% cases second episode 1 -4 months after the initial one may last for several months ultimate recovery is the rule
Complications contd…. . • Neurological complications G B syndrome, transverse myelitis • Renal nephritis, nephrotic syndrome • Haematological red cell aplasia • Acute pancreatitis
Management • No specific therapy ; disease self limited • Only supportive • No specific dietary restriction needed • Avoid hepatotoxic drugs • Specific antiviral agents not available
Prognosis • Excellent prognosis • Full recovery • Mortality less than 0. 1% • Does not cause chronic liver disease
Prevention • Isolation of the patient not very effective as the virus is already disseminated even before the diagnosis is made • Safe drinking water and proper disposal of sanitary waste
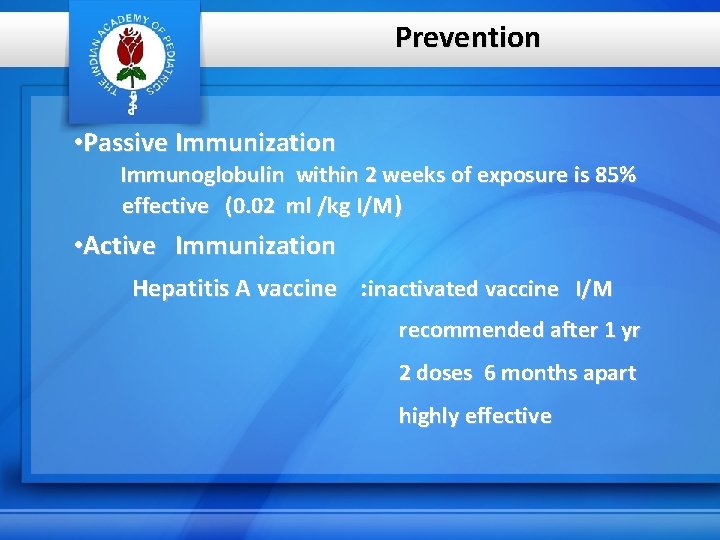
Prevention • Passive Immunization Immunoglobulin within 2 weeks of exposure is 85% effective (0. 02 ml /kg I/M) • Active Immunization Hepatitis A vaccine : inactivated vaccine I/M recommended after 1 yr 2 doses 6 months apart highly effective
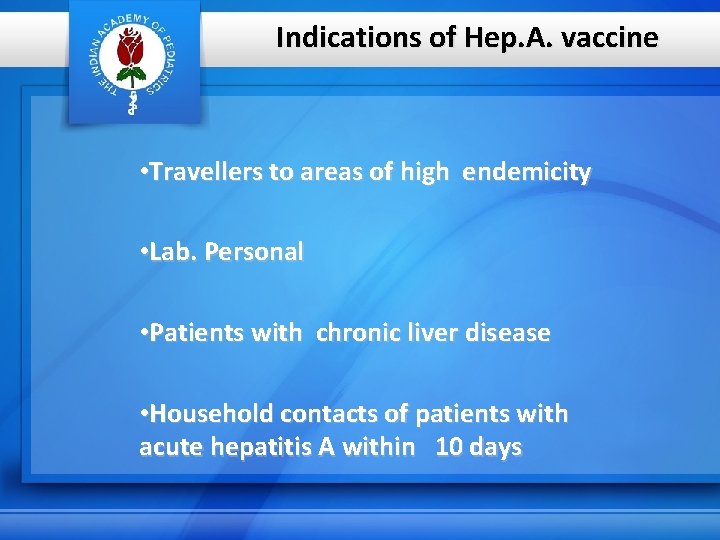
Indications of Hep. A. vaccine • Travellers to areas of high endemicity • Lab. Personal • Patients with chronic liver disease • Household contacts of patients with acute hepatitis A within 10 days
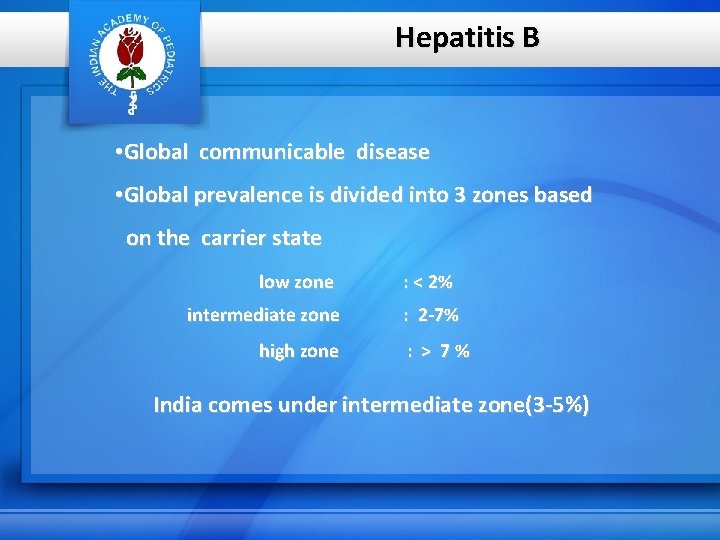
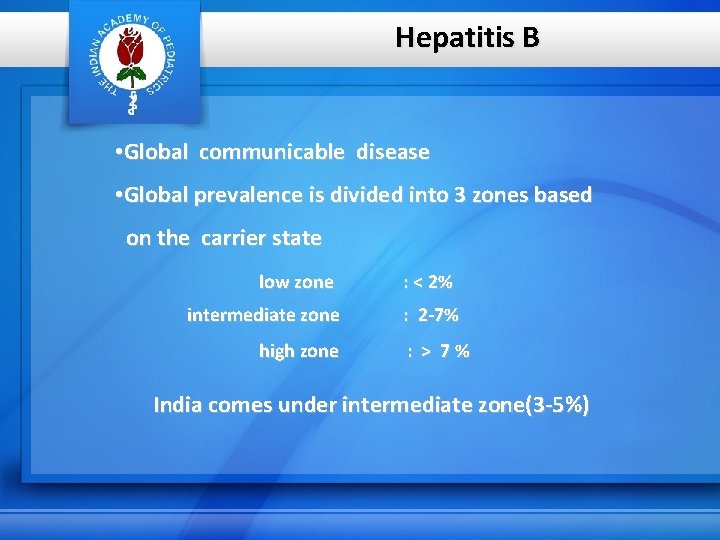
Hepatitis B • Global communicable disease • Global prevalence is divided into 3 zones based on the carrier state low zone intermediate zone high zone : < 2% : 2 -7% : > 7% India comes under intermediate zone(3 -5%)
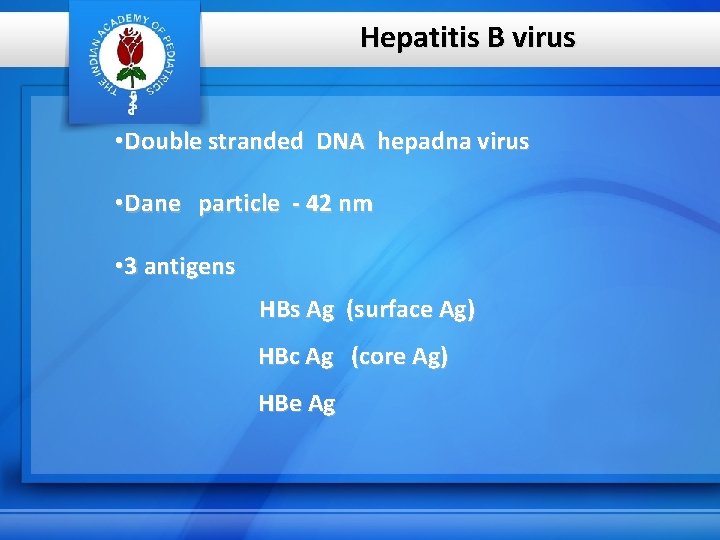
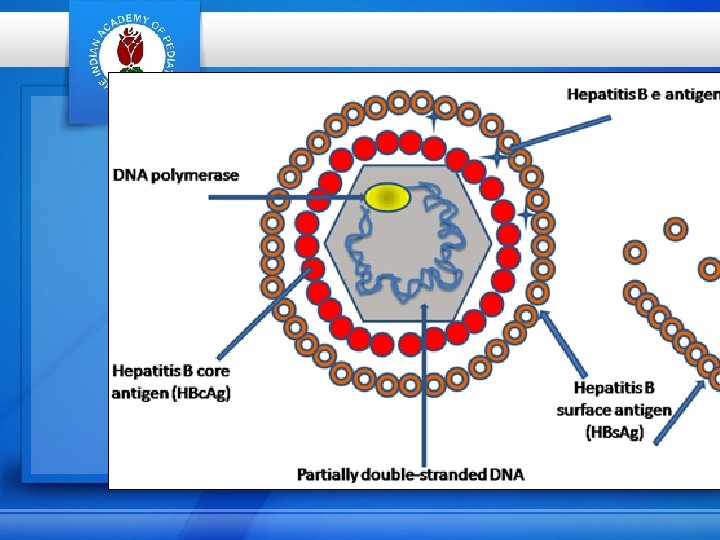
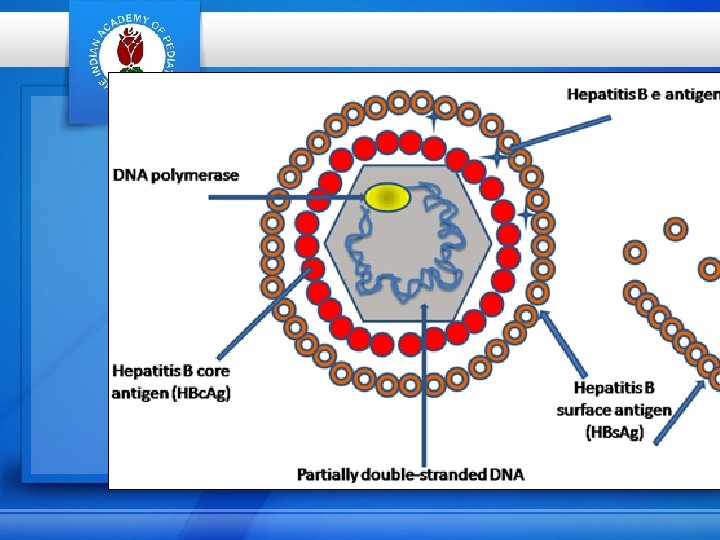
Hepatitis B virus • Double stranded DNA hepadna virus • Dane particle - 42 nm • 3 antigens HBs Ag (surface Ag) HBc Ag (core Ag) HBe Ag
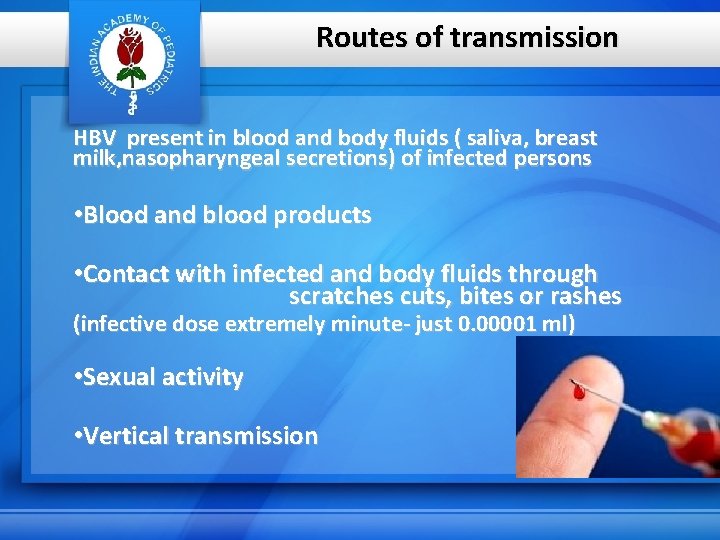
Routes of transmission HBV present in blood and body fluids ( saliva, breast milk, nasopharyngeal secretions) of infected persons • Blood and blood products • Contact with infected and body fluids through scratches cuts, bites or rashes (infective dose extremely minute- just 0. 00001 ml) • Sexual activity • Vertical transmission
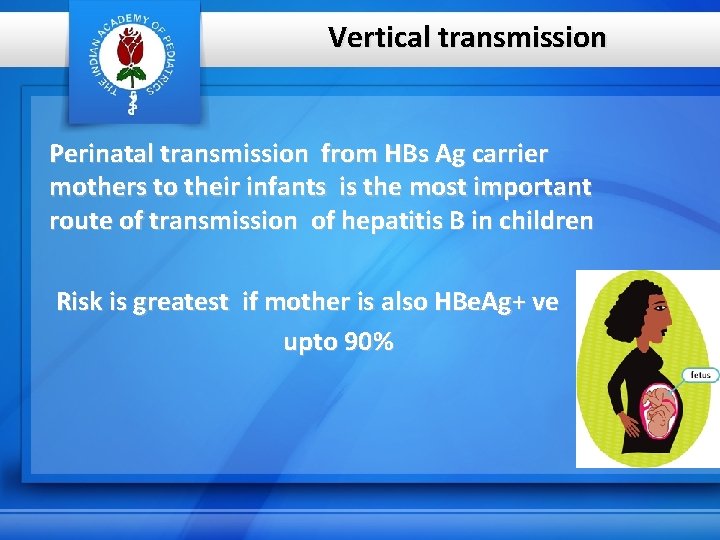
Vertical transmission Perinatal transmission from HBs Ag carrier mothers to their infants is the most important route of transmission of hepatitis B in children Risk is greatest if mother is also HBe. Ag+ ve upto 90%
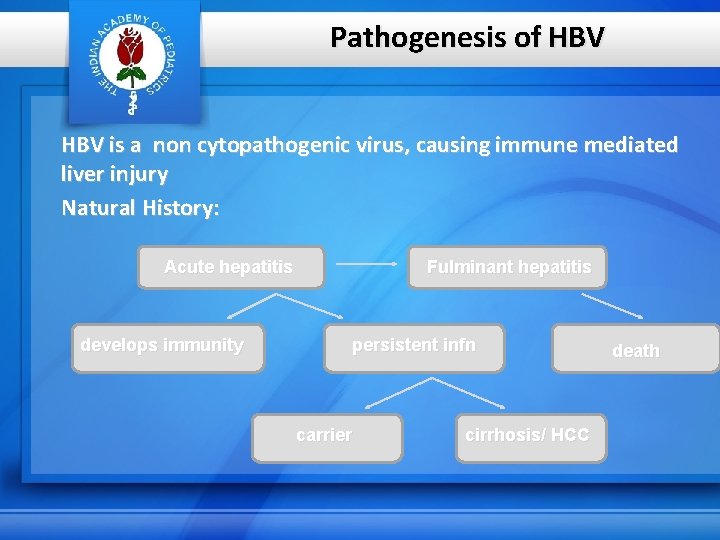
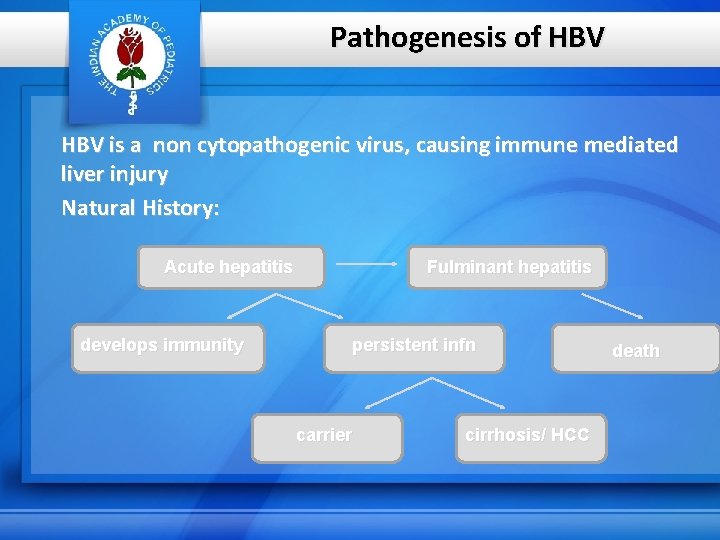
Pathogenesis of HBV is a non cytopathogenic virus, causing immune mediated liver injury Natural History: Acute hepatitis develops immunity Fulminant hepatitis persistent infn carrier cirrhosis/ HCC death
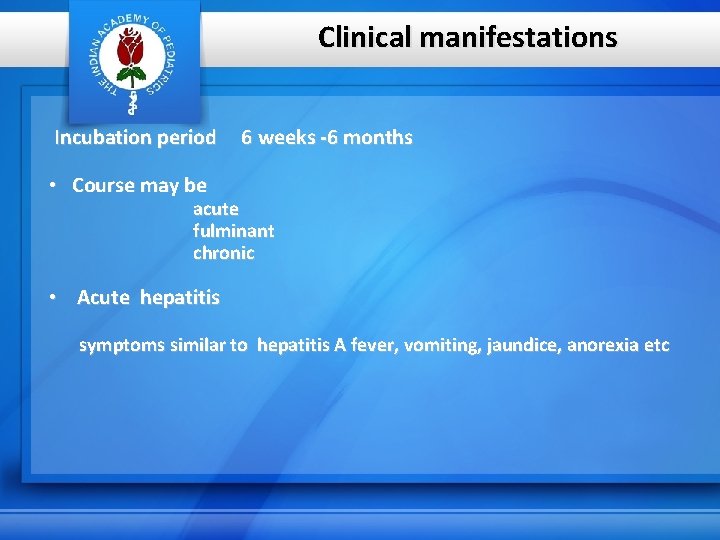
Clinical manifestations Incubation period 6 weeks -6 months • Course may be acute fulminant chronic • Acute hepatitis symptoms similar to hepatitis A fever, vomiting, jaundice, anorexia etc
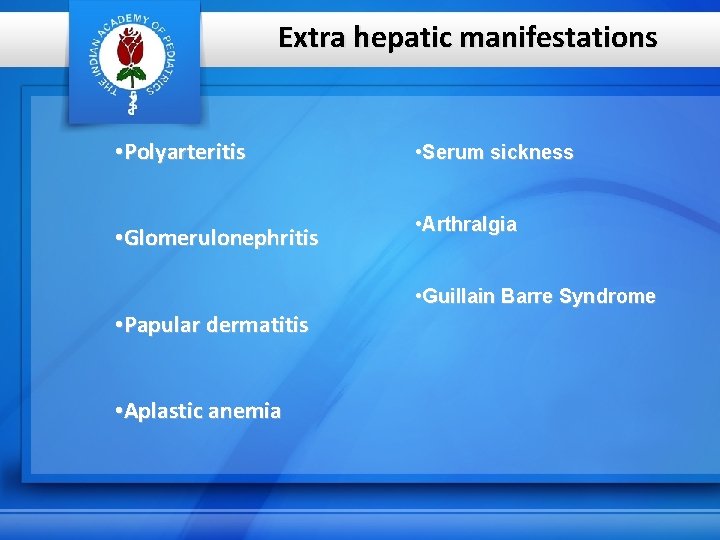
Extra hepatic manifestations • Polyarteritis • Serum sickness • Glomerulonephritis • Arthralgia • Guillain Barre Syndrome • Papular dermatitis • Aplastic anemia
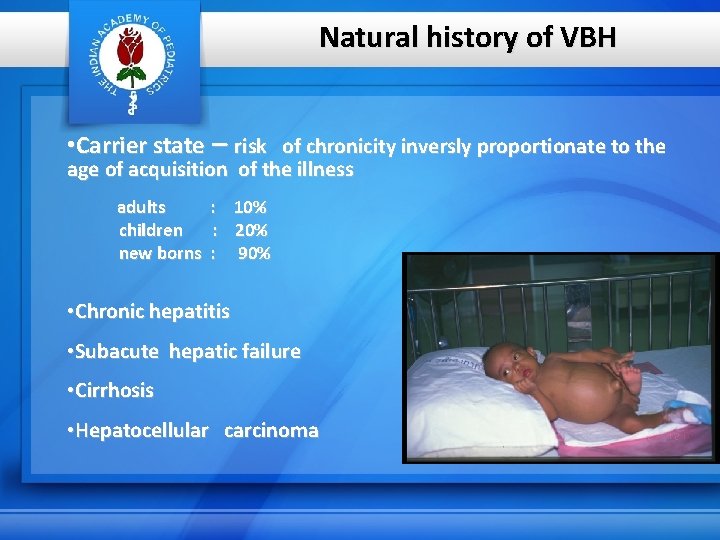
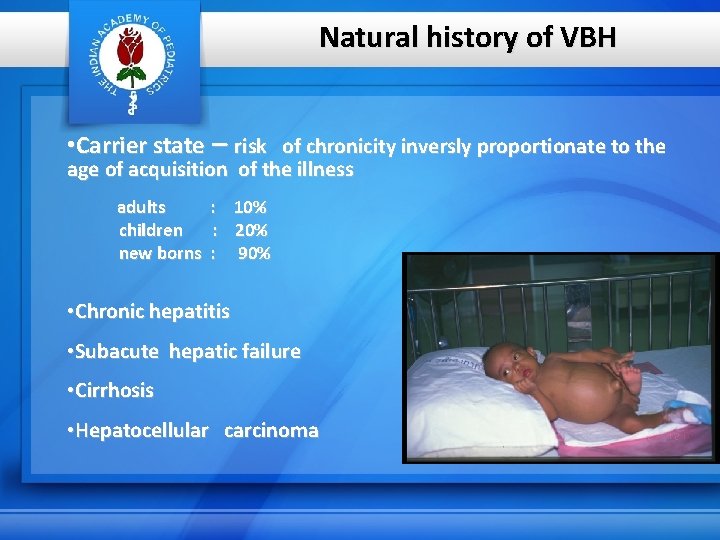
Natural history of VBH • Carrier state – risk of chronicity inversly proportionate to the age of acquisition of the illness adults children new borns : 10% : 20% : 90% • Chronic hepatitis • Subacute hepatic failure • Cirrhosis • Hepatocellular carcinoma
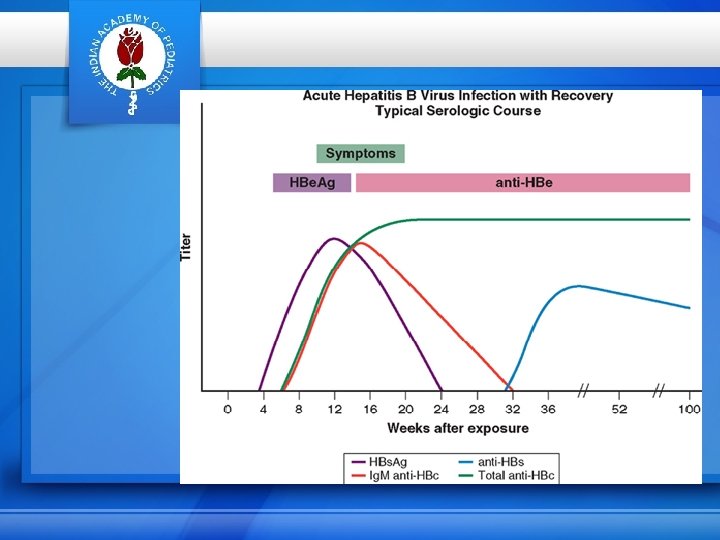
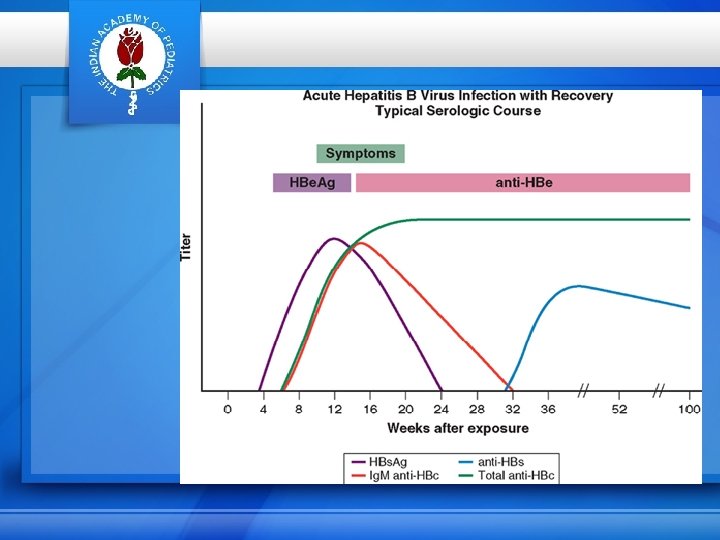
HBV serology • HBs Ag : appears by 6 weeks after infection(even before the onset of symptoms) disappears by 3 -6 months if persists > 6 months- carrier state (marker both in acute and chronic infection) • Anti HBs : protective antibody appears disappearance of HBs Ag shortly after the
Serology contd…. • HBe Ag : marker of active viral replication appears soon after HBs Ag disappears by 6 weeks if persists after 6 weeks indicate progression to chronicity • Anti HBe antibody : appears after the disappearance of HBe Ag not a protective antibody
Serology contd… • HBc Ag ( core antigen) : not present in blood • Ig M anti HBc antibody: appears 1 -2 weeks after the appearance of HBs. Ag (first antibody to appear even before anti HBe or anti HBs) • Ig G anti HBc antibody: appears after 6 months • HBV DNA : marker of replication and infectivity
Complications Acute liver cell failure coagulopathy, encephalopathy, cerebral odema more frequently seen with HBV infection than with any other hepatotropic viruses mortality due to acute liver cell failure is 30%
Treatment of Hepatitis B • Only symptomatic and supportive for acute hepatitis • IFN- Alpha and Lamivudine approved for chronic cases
Prevention Active immunization (Hepatitis B vaccine) Passive prophylaxis ( HBIG -hepatitis B immunoglobulin)
Hepatitis B Vaccine • Universal immunization is now recommended by AAP & IAP. Newborn period is targeted. • Recombinant vaccine • 3 doses • Dosage shedule 0, 6 and 10 weeks or 6, 10 and 14 weeks or 0, 1 and 6 months • No booster dose needed
Immunoprophylaxis (HBIG) For providing immediate protection of people acutely exposed to HBs. Ag +ve blood Dose : 1000 – 2000 IU( adult) 32 – 48 IU/kg ( children)
Prophylaxis contd…… For newborn of HBV infected women HBIG 0. 5 ml I/M – 100 – 200 units to be given within 12 hours of birth concurrently with HBV - first dose Combination of HBIG and HBVaccine prevent transmission in 95% cases
Hepatitis D A defective virus which cannot produce infection without a concurrent HBV infection Co- infection as acute hepatitis and more severe or Super infection in HBV carriers as chronic infection and more common
Hepatitis D contd… • Diagnosis : Ig M anti HDV antibodies • Treatment : supportive only • Prevention : by preventing HBV infection
Hepatitis C • Previously known as transfusion related Non A Non B hepatitis • Single stranded RNA virus • 6 major genotypes • Type 3 common in India
Commonest mode of transfusion is through blood and blood products (more common in patients with thalassemia, hemophilia etc)
Clinical presentation Incubation period 7 -8 weeks Insidious onset and mild Often asymptomatic and jaundice seen only in 25% cases Progression to acute liver cell failure is rare Aminotransferase levels typically fluctuate during HCV infection and donot correlate with the degree of liver cell fibrosis Vertical transmission is rare
Hepatitis C contd… • Diagnosis Ig M Anti HCV antibodies or HCV RNA • Treatment chronic cases require interferon and ribavirin • Prevention no vaccine available only screening of blood
Hepatitis E • HEV virus - a single stranded RNA virus transmitted from person to person via fecal- oral route (often through contaminated drinking water) • Causes acute sporadic and epidemic viral hepatitis • Common in older children and young adults
Hepatitis E contd… Clinical presentation incubation period : 3 -8 weeks features similar to HAV infection increased risk of fulminant hepatitis in pregnant women
Diagnosis Ig M Anti HEV antibodies No specific therapy Prevention no vaccine good personal hygiene
Hepatitis G HGV – flavi like virus related to post transufusion hepatitis, chronic hepatitis and cirrhosis TTV (Transfusion transmitted virus) new virus related to transfusion.
Summary • Hep. A : commonest cause of viral hepatitis in children. • Hep. B, C, D : responsible for transfusion related hepatitis • Hep A & E are waterborne infections • Hepatitis A is generally mild and associated with few complications
• Hepatitis B is associated with chronicity and acute liver all failure • Hep. C is often asymptomatic and associated with chronicity • Vaccine available for Hepatitis A and B • Perinatal transmission from HBs Ag carrier mothers to their newborns can be prevented by combined HBIG and HBvaccine

Questions
QUESTIONS 1) Discuss Clinical Features & Complications Of Hepatitis B.
QUESTIONS 2)Discuss Etiology, transmission, Clinical manifestations , and preventive measures for Hepatitis A Infection.
SHORT NOTES 1) Hepatitis B Immunisation 2)Australia Antigen 3)Treatment Stategy for Hepatitis B 4) Hepatotrophic viruses.
MCQ 1) In Hepatatis A infection , a) Most patients achieve full recovery. b) Most patients develop complications. c) Chronicity is common
MCQ 2) One of the following Drugs is not used in the mangement of Hepatitis B. a) Lamivudine b) Acyclovir C) Adefovir
MCQ 3) Rate of Vertical Transmission of Hepatitis B is a) 10% b) 50% c) 90% d) 100%
MCQ 4) Baby born to Hepatitis B positive mother should rececive Hepatitis B (HBIG) Immunogloblins a)Within 24 hrs b) Within 12 hrs. c) within a week.
MCQ 5) Chronic Hepatitis Risk is highest in a) Hep A b)Hep B c) Hep C d) Hep E

Thank you