ACUTE RESPIRATORY FAILURE Definitions Hypoxemia is reduction in
- Slides: 36
ACUTE RESPIRATORY FAILURE Definitions Hypoxemia is reduction in the oxygen content in the arterial blood system. Tissue hypoxia is reduction in the oxygen delivery to the tissues, caused by reduction oxygen content and or reduction in cardiac output.
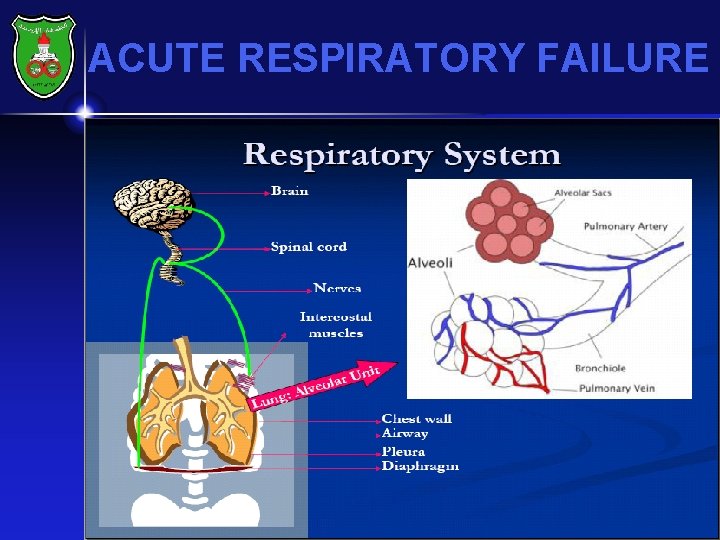
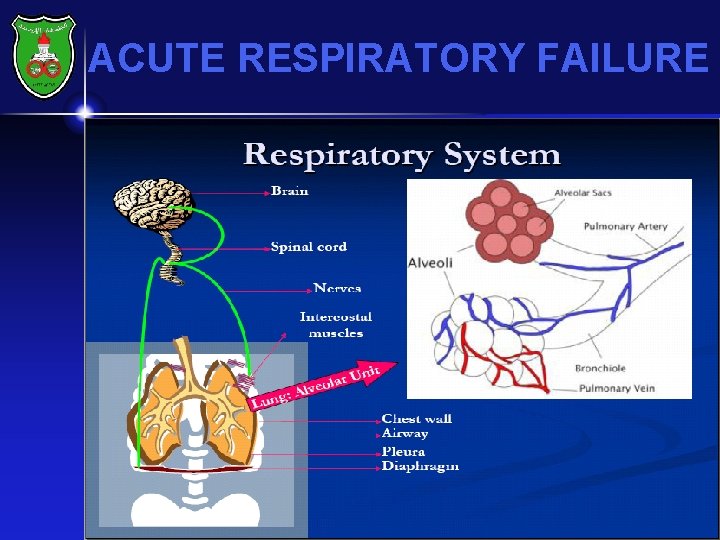
ACUTE RESPIRATORY FAILURE DEFINITION IT IS ASYNDROME OF INADEQUATE GAS EXCHANGE DUE TO DYSFUNCTION OF ONE OR MORE ESSENTIAL COMPONENTS OF RESPIRATORY SYSTEM.
ACUTE RESPIRATORY FAILURE
ACUTE RESPIRATORY FAILURE • CHEST WALL (INCLUDING PLEURA AND DIAFRAGM ) • AIRWAYS • PULMONARY CIRCULATION • NERVES • CNS OR BRAIN STEM
ACUTE RESPIRATORY FAILURE EPIDEMIOLOGY INCIDENCE : ABOUT 360. 000 /YR IN USA 36 DIE DURING HOSPITALIZATION MORTALITY AND MORBIDITY INCREASE WITH AGE COMORBIDITIES
ACUTE RESPIRATORY FAILURE • CLASIFICATION TYPE I OR HYPOXEMIC (Pa. O 2 < 60 at sea level) : FAILURE OF OXYGEN EXCHANGE INCREASED SHUNT FRACTION (QS/QT ) • DUE TO ALVEOLAR FLOODING • HYPOXEMIA REFRACTORY TO O 2 SUPPLEMNT TYPE II OR HYPERCAPNIC Pa. CO 2>50 FAILURE TO REMOVE OR TO EXCHANGE CO 2 DECREASE ALVEOLAR MIN. VENTIL. (VA) OFTEN ACCOMPANIED BY HYPOXEMIA THAT CORRECTED WITH SUPPLEMENTAL O 2
ACUTE RESPIRATORY FAILURE TYPE III RESP. FAILURE : PERIOPERATIVE RESP FAILURE INCREASED ATELECTASIS DUE TO LOW (FRC) IN SITTING OR ABNORMAL ABD. MECHANICS RESLUT IN TYPE I OR II RESP FAILURE AMELIORATED BY ANESTHETICS , OP TECHNIQUE, POSTURE. INCENTIVE SPIROMETRY. ANALGESIA TYPE IV RESP FAILURE : IN SHOCK PATIENT VENTLATED , TO STABILIZE GAS EXCHANGE. TO LOWER RESP MUSCLE O 2 CONSUMPTION
ACUTE RESPIRATORY FAILURE CLASSIFICATION ACUTE CHRONIC ACUTE ON CHRONIC Ex. Acute Exacerbation of COPD
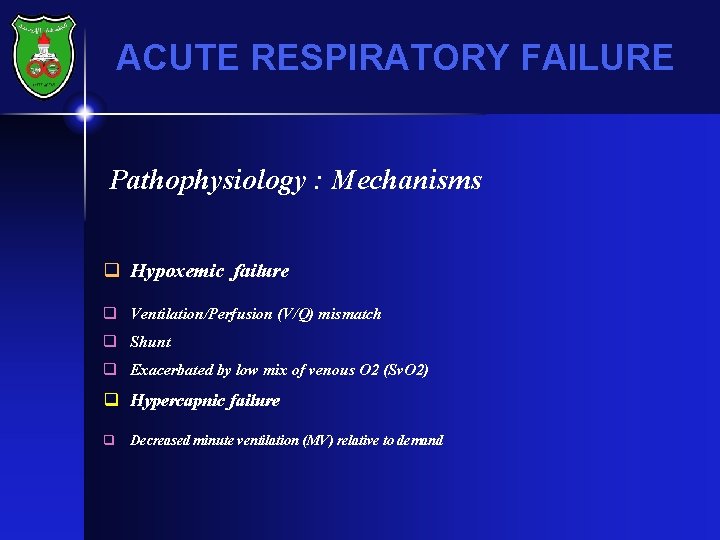
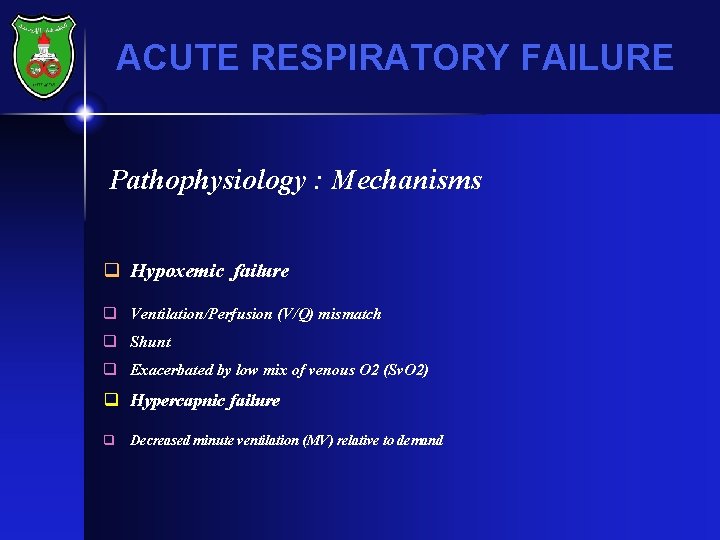
ACUTE RESPIRATORY FAILURE Pathophysiology : Mechanisms q Hypoxemic failure q Ventilation/Perfusion (V/Q) mismatch q Shunt q Exacerbated by low mix of venous O 2 (Sv. O 2) q Hypercapnic failure q Decreased minute ventilation (MV) relative to demand
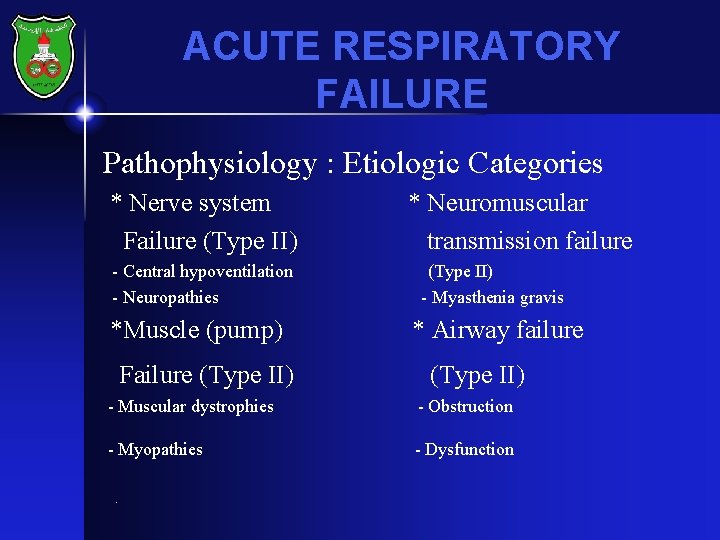
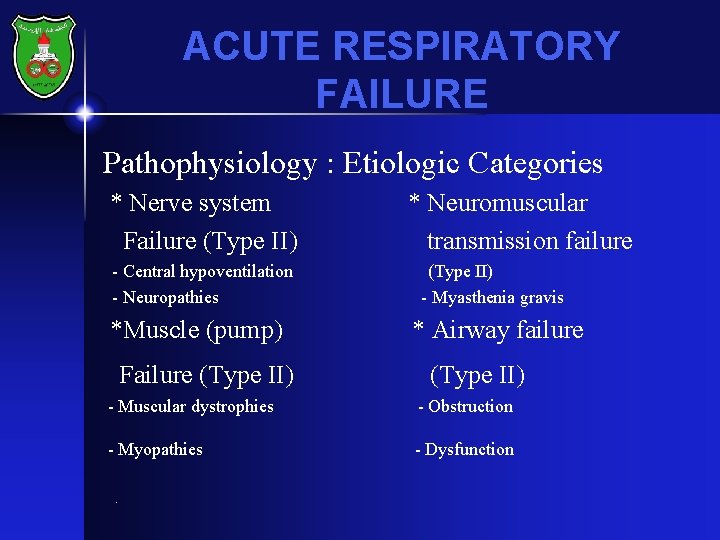
ACUTE RESPIRATORY FAILURE Pathophysiology : Etiologic Categories * Nerve system Failure (Type II) - Central hypoventilation - Neuropathies *Muscle (pump) Failure (Type II) * Neuromuscular transmission failure (Type II) - Myasthenia gravis * Airway failure (Type II) - Muscular dystrophies - Obstruction - Myopathies - Dysfunction .
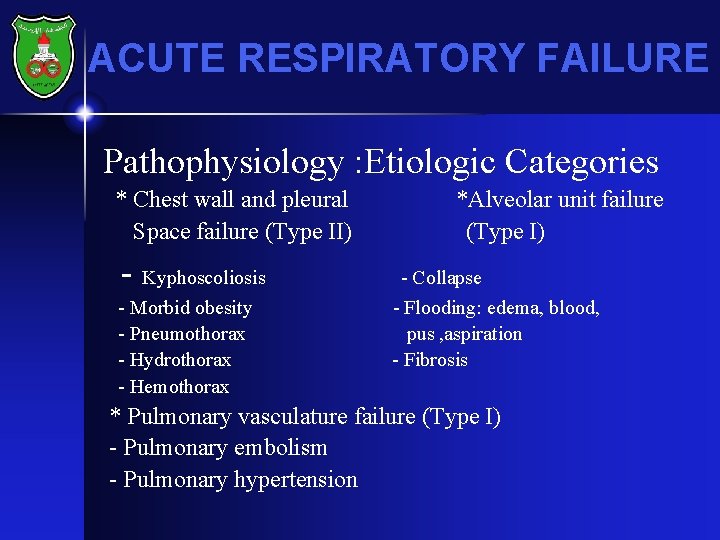
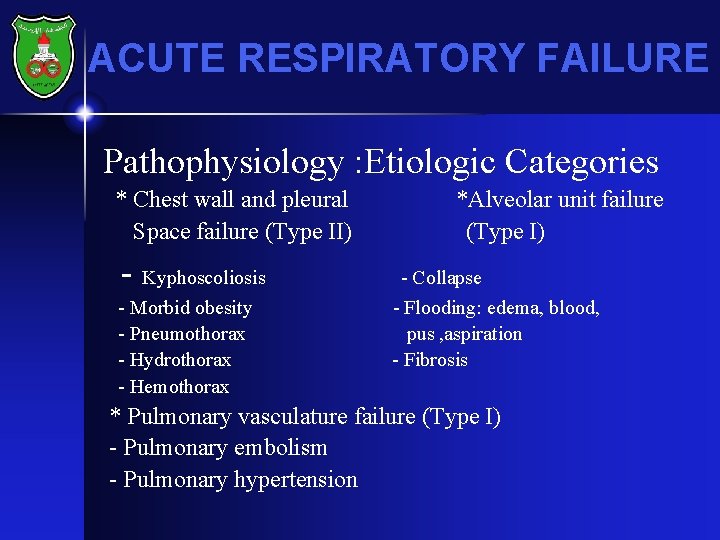
ACUTE RESPIRATORY FAILURE Pathophysiology : Etiologic Categories * Chest wall and pleural Space failure (Type II) - Kyphoscoliosis - Morbid obesity - Pneumothorax - Hydrothorax - Hemothorax *Alveolar unit failure (Type I) - Collapse - Flooding: edema, blood, pus , aspiration - Fibrosis * Pulmonary vasculature failure (Type I) - Pulmonary embolism - Pulmonary hypertension
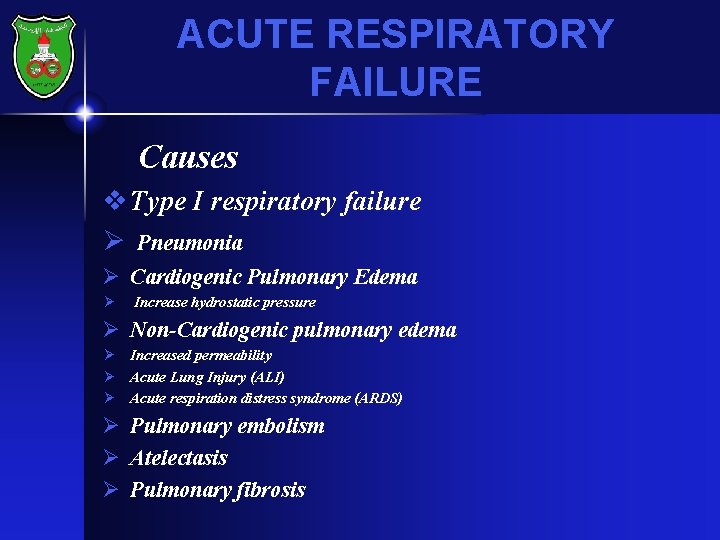
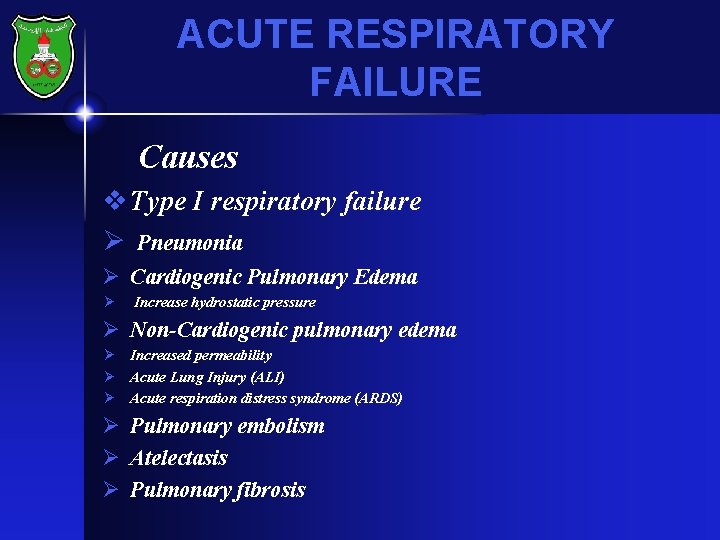
ACUTE RESPIRATORY FAILURE Causes v Type I respiratory failure Ø Pneumonia Ø Cardiogenic Pulmonary Edema Ø Increase hydrostatic pressure Ø Non-Cardiogenic pulmonary edema Ø Increased permeability Ø Acute Lung Injury (ALI) Ø Acute respiration distress syndrome (ARDS) Ø Pulmonary embolism Ø Atelectasis Ø Pulmonary fibrosis
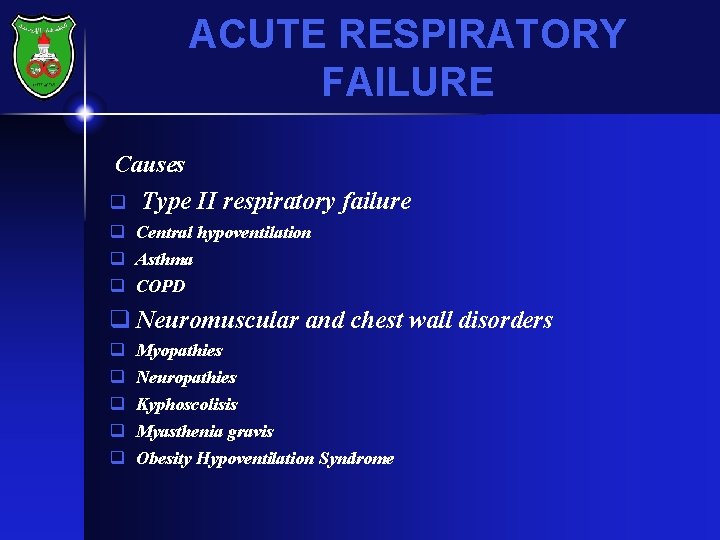
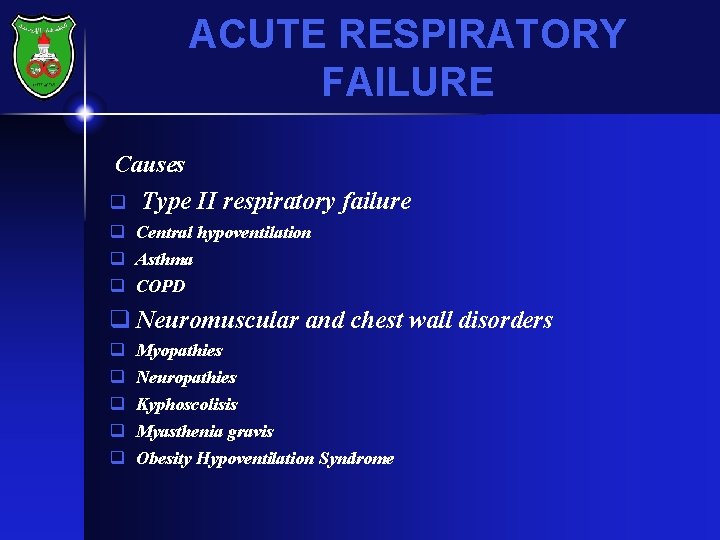
ACUTE RESPIRATORY FAILURE Causes q Type II respiratory failure q Central hypoventilation q Asthma q COPD q Neuromuscular and chest wall disorders q q q Myopathies Neuropathies Kyphoscolisis Myasthenia gravis Obesity Hypoventilation Syndrome
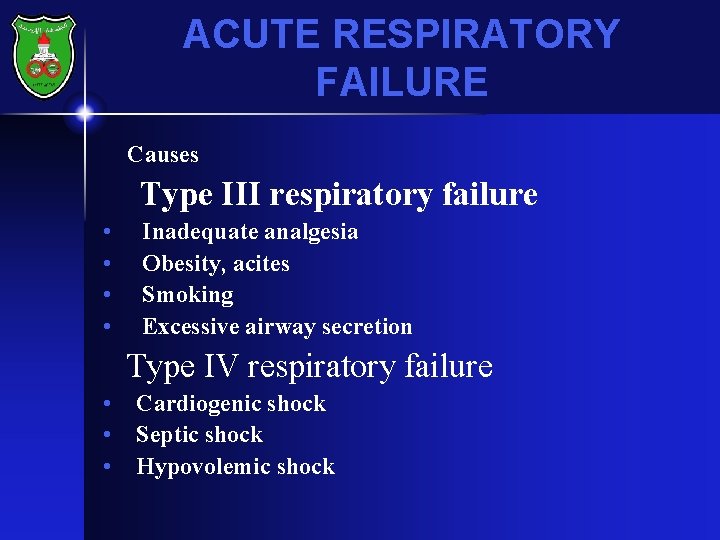
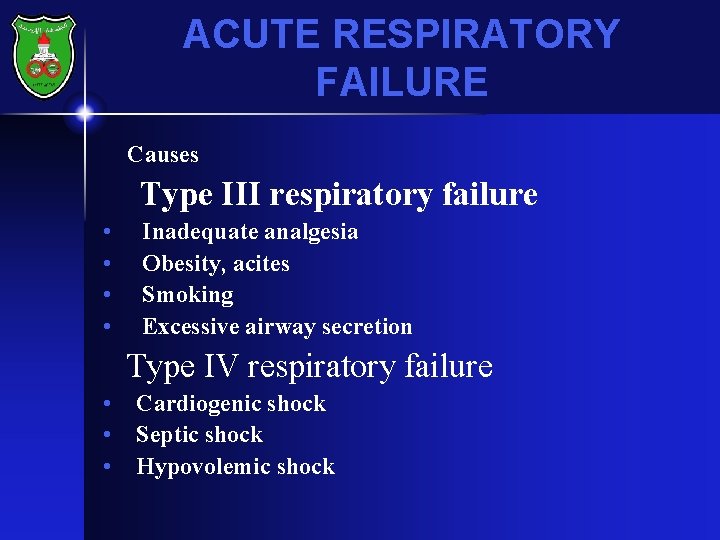
ACUTE RESPIRATORY FAILURE Causes Type III respiratory failure • • Inadequate analgesia Obesity, acites Smoking Excessive airway secretion Type IV respiratory failure • Cardiogenic shock • Septic shock • Hypovolemic shock
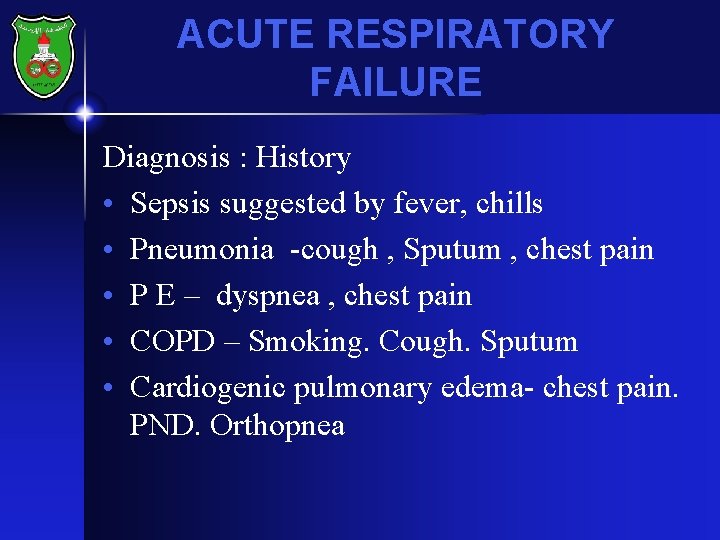
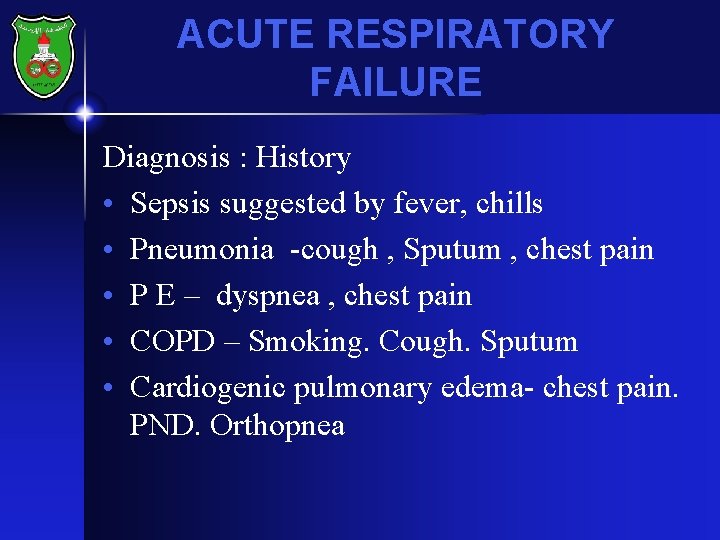
ACUTE RESPIRATORY FAILURE Diagnosis : History • Sepsis suggested by fever, chills • Pneumonia -cough , Sputum , chest pain • P E – dyspnea , chest pain • COPD – Smoking. Cough. Sputum • Cardiogenic pulmonary edema- chest pain. PND. Orthopnea
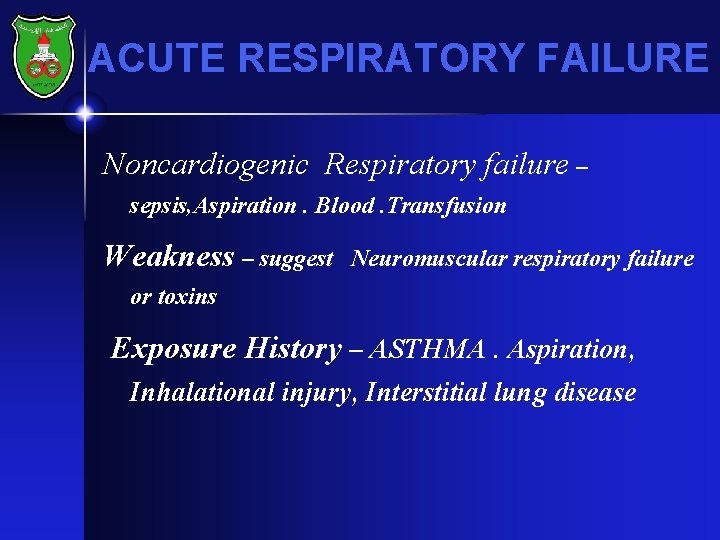
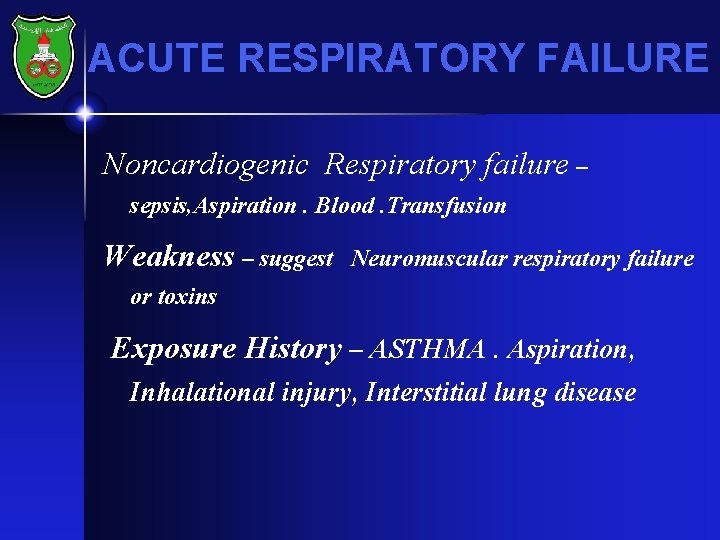
ACUTE RESPIRATORY FAILURE Noncardiogenic Respiratory failure – sepsis, Aspiration. Blood. Transfusion Weakness – suggest Neuromuscular respiratory failure or toxins Exposure History – ASTHMA. Aspiration, Inhalational injury, Interstitial lung disease
ACUTE RESPIRATORY FAILURE • DIAGNOSIS- PHYSICAL FINDING • Hypotension- poor perfusion –in sepsis , embolus • Hypertension –with poor perfusion in Cardiogenic pulmonary edema • Wheezing – Suggest A/W obstruction : Bronchospasm upper or lower airway pathology Secretion Pulmonary edema
ACUTE RESPIRATORY FAILURE • Stridor suggests upper airway obstruction • Elevated jugular venous pressure suggests right ventricular dysfunction due to accompanying pulmonary hypertension • Tachycardia and arrhythmias may be the cause of cardiogenic pulmonary edema
ACUTE RESPIRATORY FAILURE • • • Labortary ABG CBC Cardiac serologic markers Troponin , (CK-MB) Microbiology Cultures, Sputum , tracheal aspirate Blood , urine and body fluid
ACUTE RESPIRATORY FAILURE • • • Chest X-ray ECG Echocardiography Pulmonary function tests Bronchoscopy
ACUTE RESPIRATORY FAILURE • Management • ABC’s • Ensure airway is adequate • Oxygen therapy and assisted ventilation if needed • Support circulation
ACUTE RESPIRATORY FAILURE • Treatment of a specific cause when possible • Infection • Airway obstruction • Improve cardiac function Positive airway pressure, diuretics, inotropy
ACUTE RESPIRATORY FAILURE • Mechanical ventilation • Non-invasive (if patient a/w is protected and hemodynamically stable) • Mask • Invasive (Endotracheal tube)
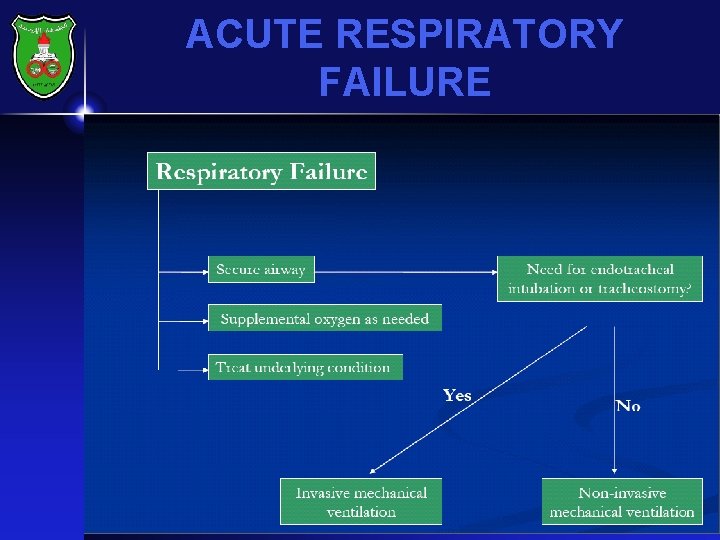
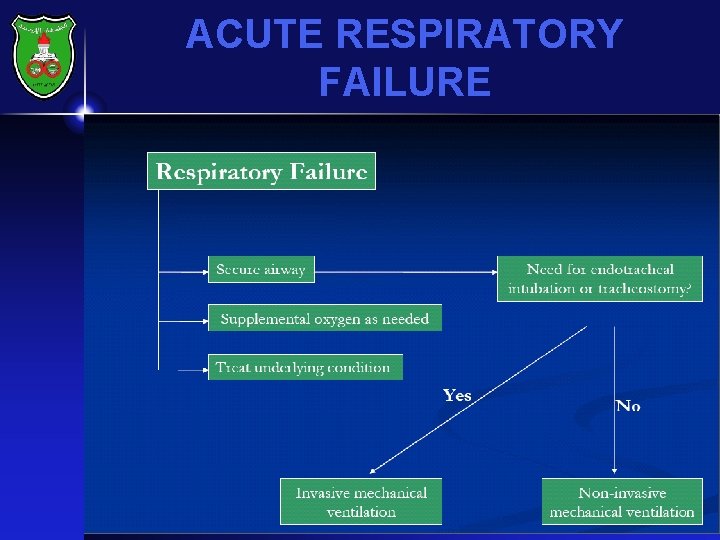
ACUTE RESPIRATORY FAILURE
ACUTE RESPIRATORY FAILURE • Indication for mechanical ventilation • Cardiac or respiratory arrest • Tachy/bradypnea • Respiratory acidosis • Refractory hypoxemia • Depressed level of consciousness • Shock • Inability to excrete secretions
ACUTE RESPIRATORY FAILURE • Neuromuscular disease with V/C less than 10 -15 ML/kg • Increased ICP
ACUTE RESPIRATORY FAILURE • Invasive vs. Non-Invasive ventilation • Non-invasive in : COPD Cardiogenic pulmonary edema Obesity hypoventilation syndrome Asthma
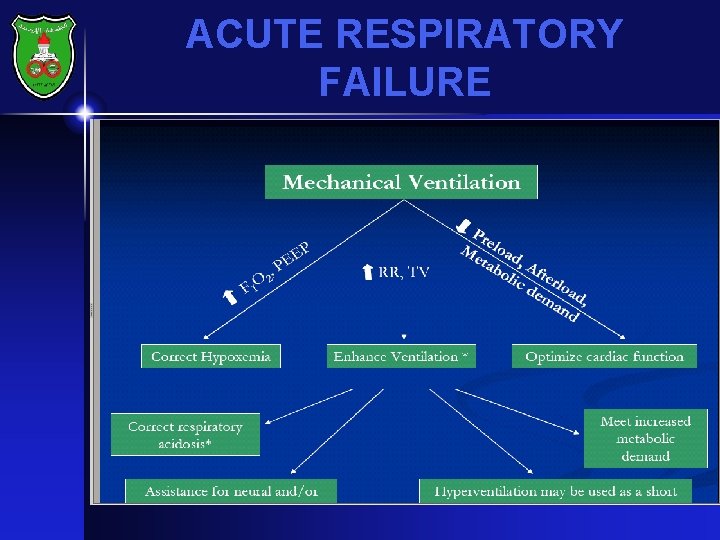
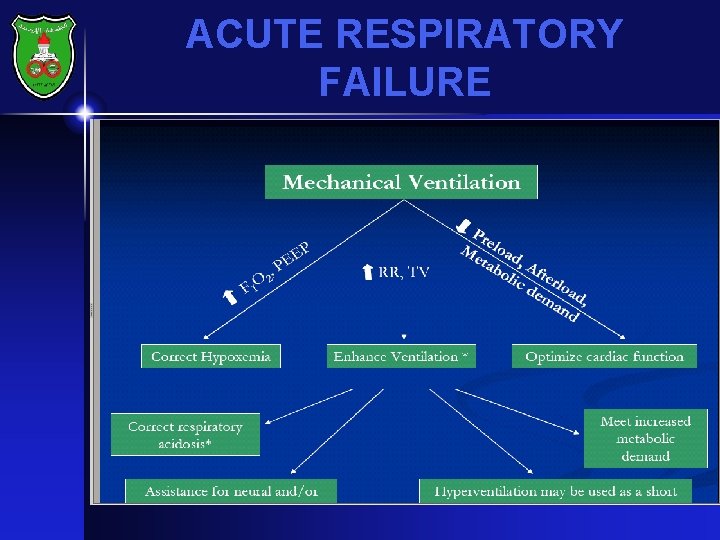
ACUTE RESPIRATORY FAILURE • Goals of Mechanical Ventilation • Improve ventilation by augmenting respiratory rate and tidal volume • Assistant for neural or muscle dysfunction • Sedated, paralyzed or comatose patient • Neuropathy • Intra-operative ventilation • Correct respiratory acidosis • Match respiratory demand • Rest respiratory muscles
ACUTE RESPIRATORY FAILURE • Correct hypoxemia High FIO 2 PEEP • Improve cardiac function Decrease preload Decrease afterload Decrease metabolic demand
ACUTE RESPIRATORY FAILURE • Permissive Hypercapnia Strategy that allows Pa. CO 2 to rise by accepting lower alveolar minute ventilation to avoid specific risks: Dynamic hyperinflation (Auto-PEEP) and barotrauma in patients with asthma Ventilator associated with lung injury in ARDS Contraindicated in ICP
ACUTE RESPIRATORY FAILURE
ACUTE RESPIRATORY FAILURE Other issues to consider when initiating Mechanical Ventilation • • • Don’t wait respiratory acidosis with evidence of : Inability to protect airway RR > 35 /minute Respiratory muscle fatigue Consider risks and benefits of mechanical vetilation
ACUTE RESPIRATORY FAILURE Other issues in intubated and Ventilated patients • Elevate head > 30 degree • Ulcer and DVT prophylaxis • In patient with ALI use small TV (6 ml/kg and pressure of 30 cm. H 2 O • Modify ventilation according to the patient
ACUTE RESPIRATORY FAILURE • Monitoring Routine Monitoring ECG Blood Pressure Pulse Oximetry Temperature Capnography Blood gases
ACUTE RESPIRATORY FAILURE • • CARE OF VENTILATED PATIENTS SEDATION ANALGESIA NURSING CARE MUSCLE RELAXANTS ? ? ? WEAKNESS. MYOPATHY AND (POST PARALYTIC SNDROME)
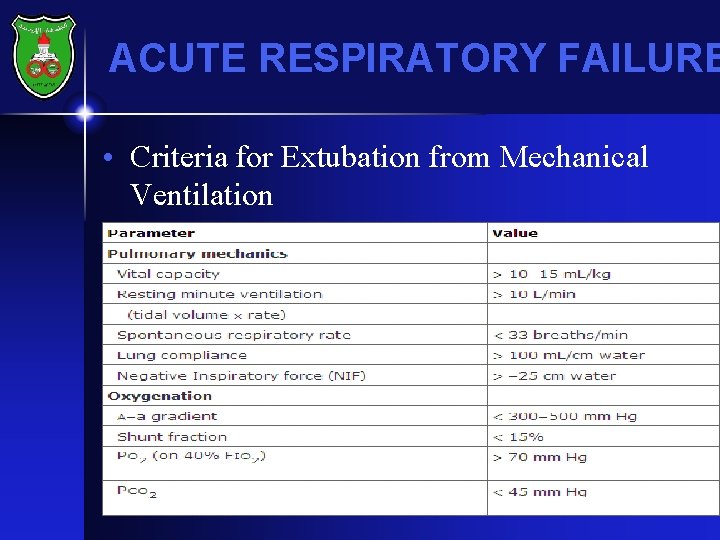
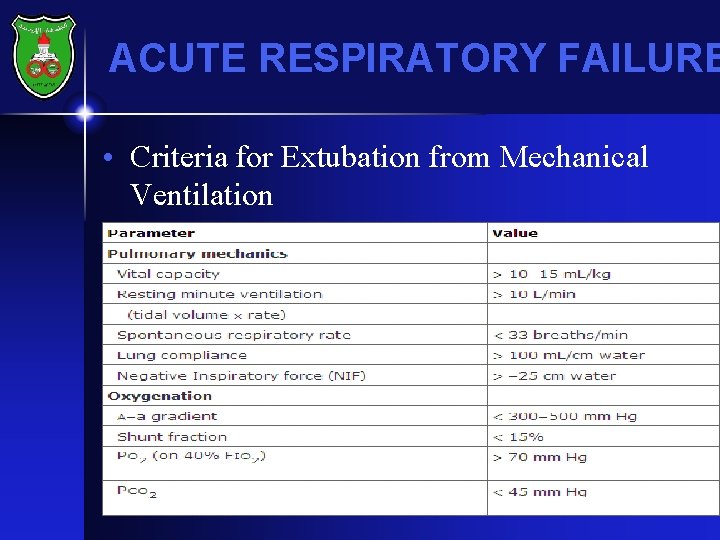
ACUTE RESPIRATORY FAILURE • Criteria for Extubation from Mechanical Ventilation •