Acute Respiratory Failure ARDS ABGs NURS 241 Chapter
Acute Respiratory Failure, ARDS, & ABGs NURS 241 Chapter 68 (p. 1744) Chapter 17 (p. 320 -324)
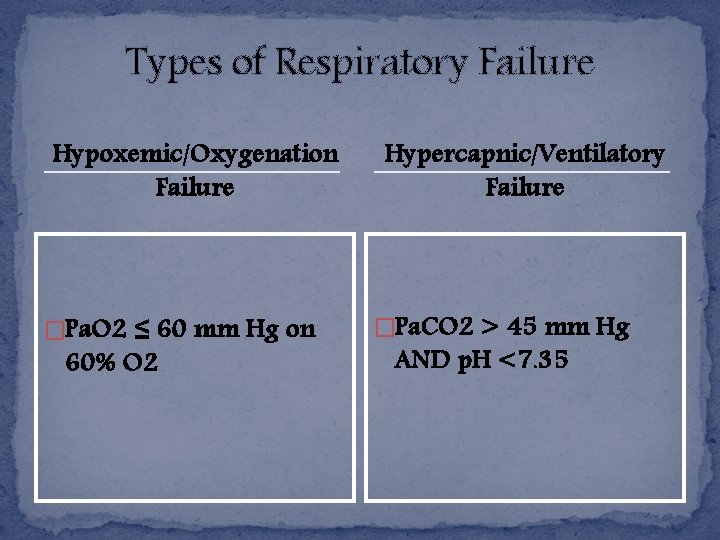
Types of Respiratory Failure Hypoxemic/Oxygenation Failure �Pa. O 2 ≤ 60 mm Hg on 60% O 2 Hypercapnic/Ventilatory Failure �Pa. CO 2 > 45 mm Hg AND p. H <7. 35
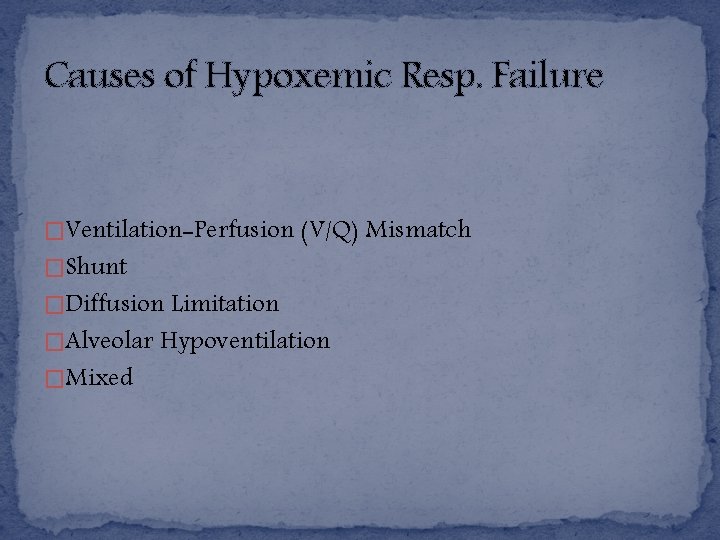
Causes of Hypoxemic Resp. Failure �Ventilation-Perfusion (V/Q) Mismatch �Shunt �Diffusion Limitation �Alveolar Hypoventilation �Mixed
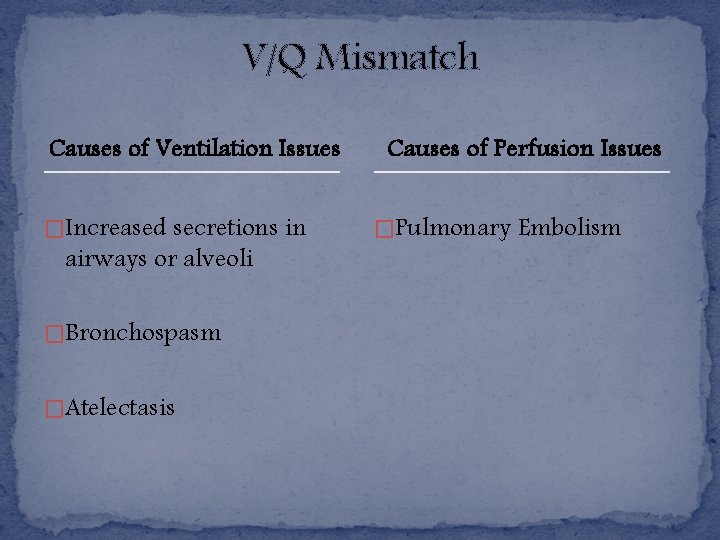
V/Q Mismatch Causes of Ventilation Issues �Increased secretions in airways or alveoli �Bronchospasm �Atelectasis Causes of Perfusion Issues �Pulmonary Embolism
Shunt �Essentially more extreme V/Q mismatch �Lack of gas exchange �Anatomic shunt- blood bypasses lungs (ventricular septal defect) �Intrapulmonary shunt- blood flows normally through lungs but no gas exchange (common w/ fluid in alveoli) �Typically very hypoxemic & require MV w/ high Fi. O 2
Diffusion Limitation �Gas exchange compromised d/t thickening and damage to alveolar-capillary membrane �Exacerbated by damage to pulmonary vascular bed (emphysema, recurrent PEs) �Hypoxemia worse w/ increased activity d/t rapid blood circulation & decreased time for O 2 diffusion
Alveolar Hypoventilation �Rise in Pa. CO 2 consequently results in lower Pa. O 2 levels �Result of restrictive lung diseases, CNS diseases, chest wall dysfunction, asthma, Neuromuscular diseases
Causes of Hypercapnic Resp. Failure �Imbalance of ventilatory supply & demand caused by one or more of the following… �Airway & Alveolar abnormalities �CNS problems �Chest wall dysfunction �Neuromuscular conditions
Airway & Alveolar Abnormalities �Common w/ asthma, COPD, & Cystic Fibrosis �Impedance of airflow & air trapping �Muscle fatigue & ventilatory failure arise from increased inspiratory effort needed to achieve adequate tidal volumes
CNS Problems �CNS depressants reduce respiratory drive �Brainstem infarct or severe head injury = interference w/ normal function of respiratory center control of medulla �Metabolic or structural brain injuries affecting LOC �High-level spinal cord injuries- limit innervation of respiratory muscles & diaphragm
Chest Wall Dysfunction �Structural abnormalities impacting normal chest wall function → limited lung expansion → impaired gas exchange �Examples of causes: Flail chest, kyphoscoliosis, morbid obesity
Neuromuscular Conditions �Conditions like Guillain-Barre syndrome, muscular dystrophy, myasthenia gravis, muscular sclerosis �Issue is not w/ lungs themselves �Respiratory weakness and/or paralysis → inability to inspire adequate tidal volumes to remove sufficient CO 2 from lungs
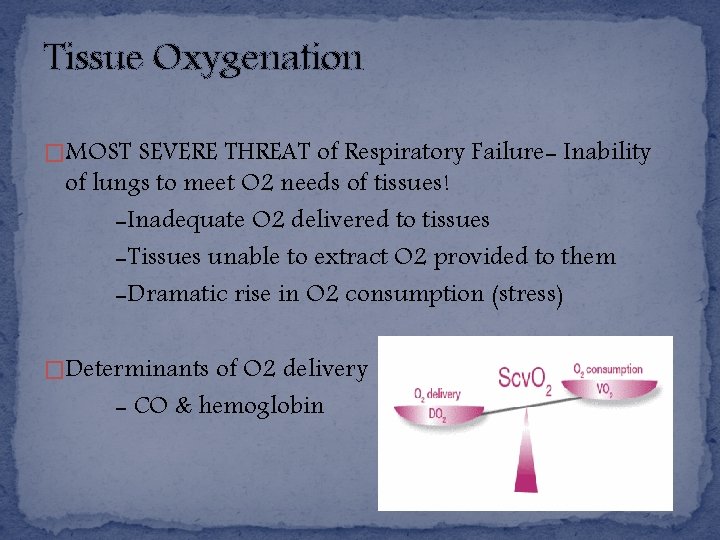
Tissue Oxygenation �MOST SEVERE THREAT of Respiratory Failure- Inability of lungs to meet O 2 needs of tissues! -Inadequate O 2 delivered to tissues -Tissues unable to extract O 2 provided to them -Dramatic rise in O 2 consumption (stress) �Determinants of O 2 delivery - CO & hemoglobin
Clinical Manifestations Hypoxemic Failure �Dyspnea, tachypnea, prolonged I: E ratio, intercostal retraction, use of accessory muscles, ↓ sp 02 �Agitation, delirium, ↓ LOC �Tachycardia, HTN, cool/clammy, diaphoretic skin, dysrhythmias �Fatigue Hypercapnic Failure � ↓ RR or rapid rate but shallow breaths, ↓ Tv, tripoding, pursed-lip breathing � Morning HA, disorientation, progressive somnolence, ↑ ICP � Dysrhythmias, HTN, Tachycardia � Muscle weakness, ↓ DTRs, later seizures
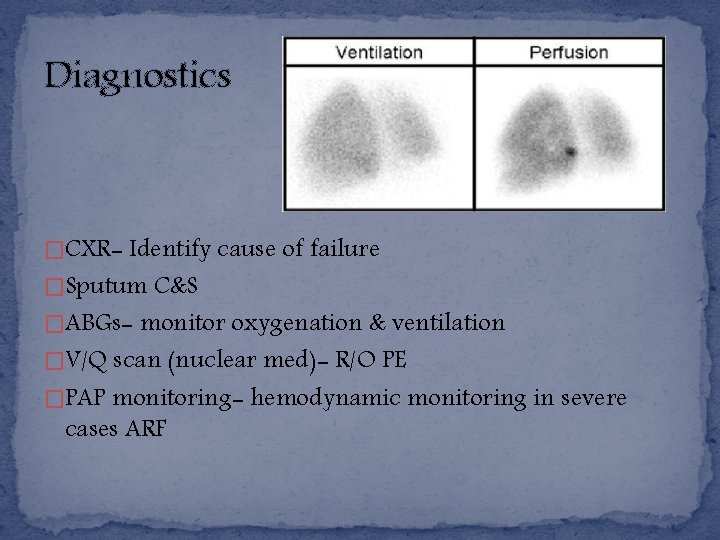
Diagnostics �CXR- Identify cause of failure �Sputum C&S �ABGs- monitor oxygenation & ventilation �V/Q scan (nuclear med)- R/O PE �PAP monitoring- hemodynamic monitoring in severe cases ARF
Treatment Interventions � O 2 therapy for hypoxemia- shunting requirements higher (complications- O 2 toxicity, CO 2 retainers) � Mobilize secretions - Pulmonary toilet -“good lung down”- improve V/Q mismatch, facilitate secretion draining -Hydrate and humidify -Chest PT -Suctioning � Positive pressure ventilation (NIPPV vs. invasive)
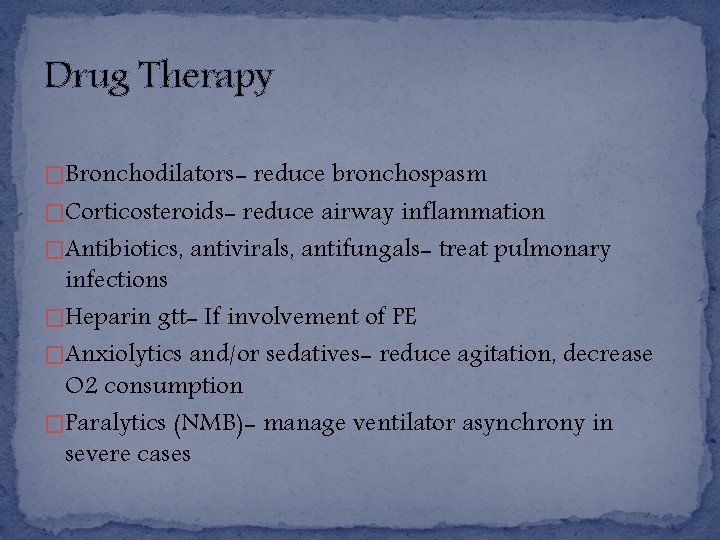
Drug Therapy �Bronchodilators- reduce bronchospasm �Corticosteroids- reduce airway inflammation �Antibiotics, antivirals, antifungals- treat pulmonary infections �Heparin gtt- If involvement of PE �Anxiolytics and/or sedatives- reduce agitation, decrease O 2 consumption �Paralytics (NMB)- manage ventilator asynchrony in severe cases
Acute Respiratory Distress Syndrome (ARDS) NURS 241 Chapter 68 (p. 1744)
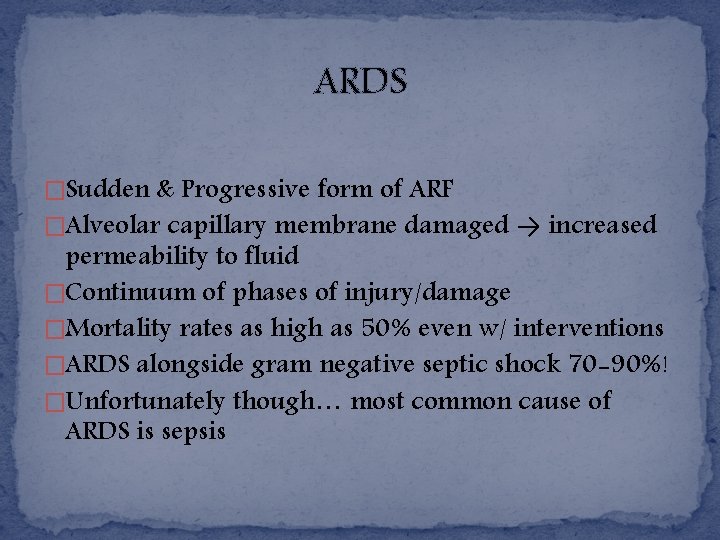
ARDS �Sudden & Progressive form of ARF �Alveolar capillary membrane damaged → increased permeability to fluid �Continuum of phases of injury/damage �Mortality rates as high as 50% even w/ interventions �ARDS alongside gram negative septic shock 70 -90%! �Unfortunately though… most common cause of ARDS is sepsis
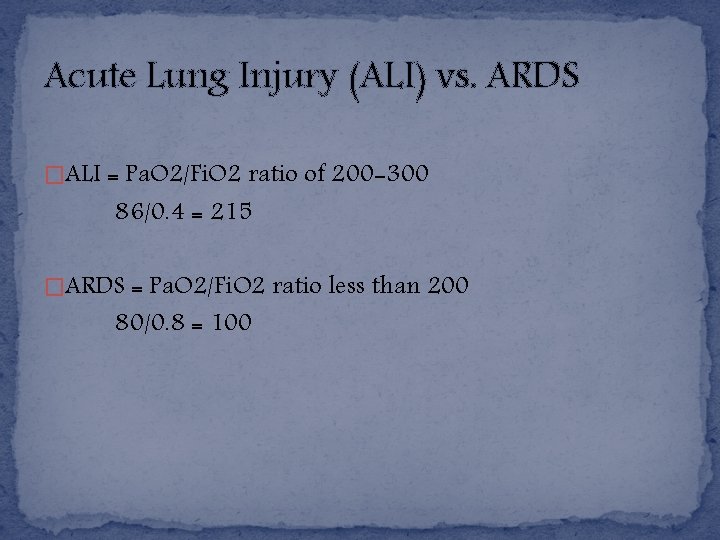
Acute Lung Injury (ALI) vs. ARDS �ALI = Pa. O 2/Fi. O 2 ratio of 200 -300 86/0. 4 = 215 �ARDS = Pa. O 2/Fi. O 2 ratio less than 200 80/0. 8 = 100
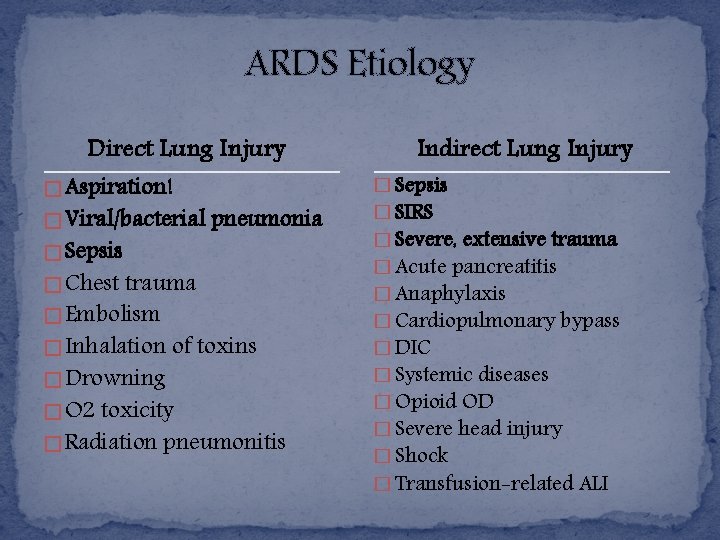
ARDS Etiology Direct Lung Injury � Aspiration! � Viral/bacterial pneumonia � Sepsis � Chest trauma � Embolism � Inhalation of toxins � Drowning � O 2 toxicity � Radiation pneumonitis Indirect Lung Injury � Sepsis � SIRS � Severe, extensive trauma � Acute pancreatitis � Anaphylaxis � Cardiopulmonary bypass � DIC � Systemic diseases � Opioid OD � Severe head injury � Shock � Transfusion-related ALI
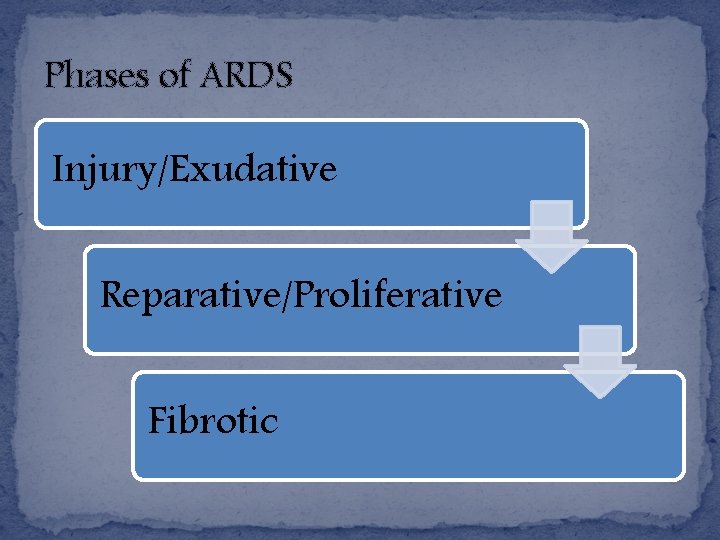
Phases of ARDS Injury/Exudative Reparative/Proliferative Fibrotic
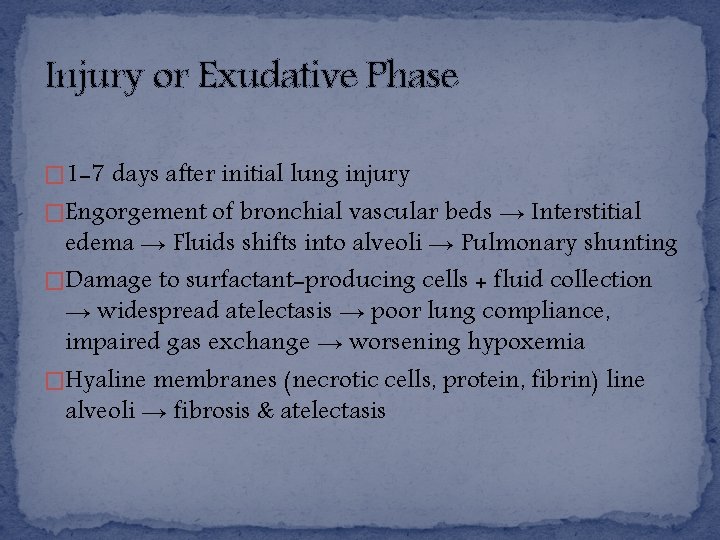
Injury or Exudative Phase � 1 -7 days after initial lung injury �Engorgement of bronchial vascular beds → Interstitial edema → Fluids shifts into alveoli → Pulmonary shunting �Damage to surfactant-producing cells + fluid collection → widespread atelectasis → poor lung compliance, impaired gas exchange → worsening hypoxemia �Hyaline membranes (necrotic cells, protein, fibrin) line alveoli → fibrosis & atelectasis
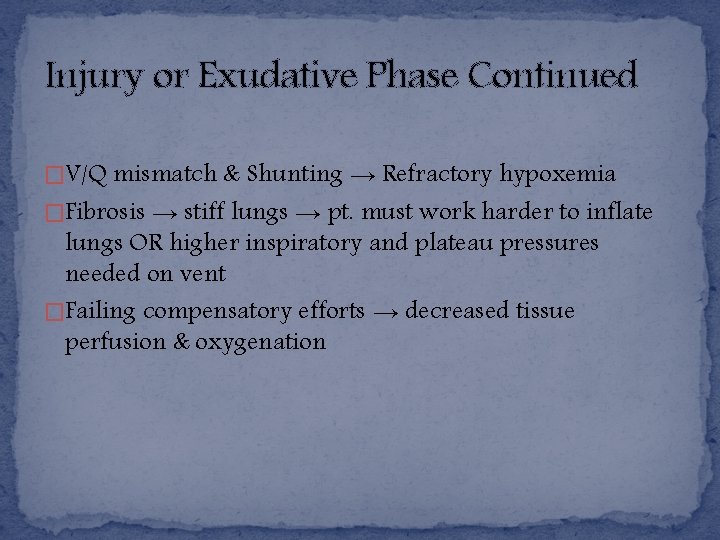
Injury or Exudative Phase Continued �V/Q mismatch & Shunting → Refractory hypoxemia �Fibrosis → stiff lungs → pt. must work harder to inflate lungs OR higher inspiratory and plateau pressures needed on vent �Failing compensatory efforts → decreased tissue perfusion & oxygenation
Reparative or Proliferative Phase � 1 -2 weeks after initial lung injury �Inflammatory response = flooding of lung tissue w/ inflammatory mediators = fibroblast proliferation �Phase ends w/ generalized fibrosis = decreased lung compliance �Worsening of hypoxemia d/t thickened alveolar membranes (shunting) �If phase stopped, lesions will resolve… if not, then…
Fibrotic Phase � 2 -3 weeks after initial lung injury �Chronic phase/irreversible damage �Lung tissue COMPLETELY remodeled by collagenous/fibrous tissues �Diffuse scaring/fibrosis = decreased lung compliance �Decreased surface area for gas exchange = continued hypoxemia �Fibrosis & pulmonary vascular destruction = pulmonary HTN
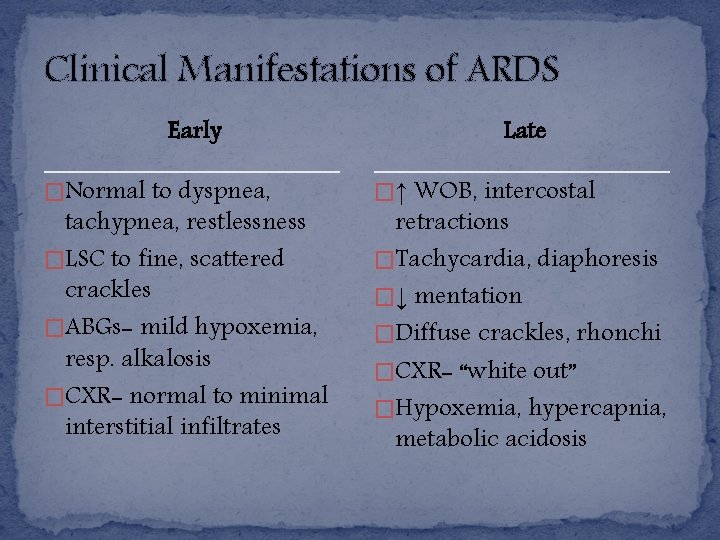
Clinical Manifestations of ARDS Early �Normal to dyspnea, tachypnea, restlessness �LSC to fine, scattered crackles �ABGs- mild hypoxemia, resp. alkalosis �CXR- normal to minimal interstitial infiltrates Late �↑ WOB, intercostal retractions �Tachycardia, diaphoresis �↓ mentation �Diffuse crackles, rhonchi �CXR- “white out” �Hypoxemia, hypercapnia, metabolic acidosis
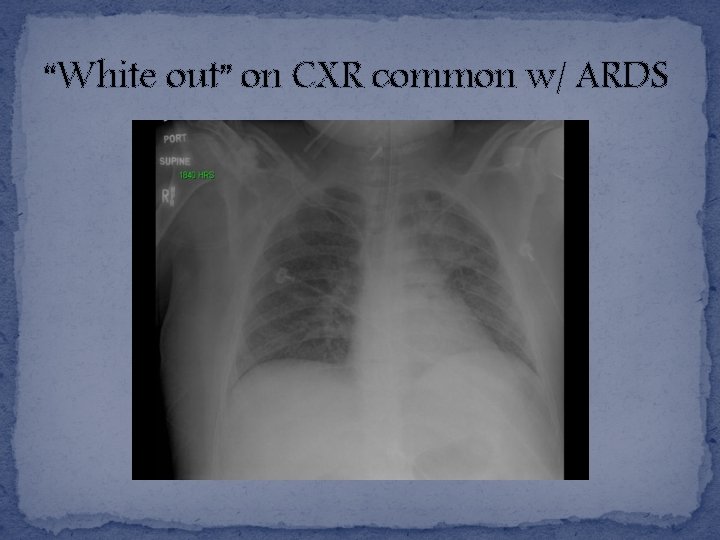
“White out” on CXR common w/ ARDS
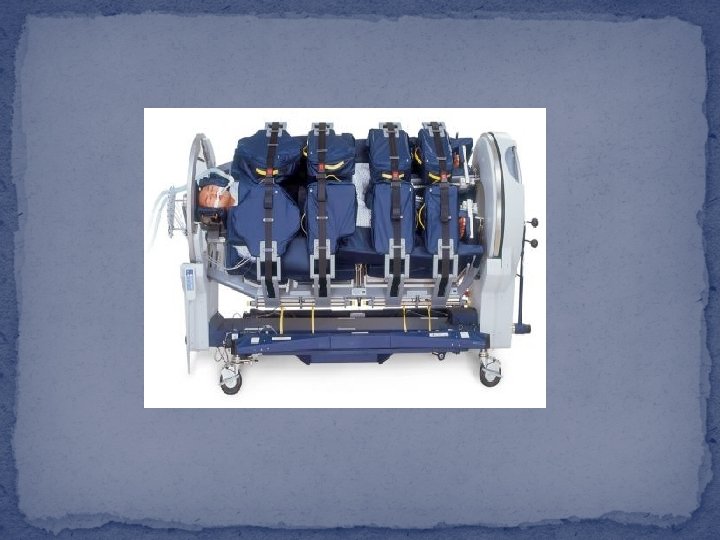
Treatment/Management of ARDS �Non-invasive positive pressure ventilation (CPAP & Bi. PAP) �Mechanical Ventilation (APRV- inverse ratio ventilation, longer inspiratory than expiratory time to increase alveolar recruitment) �Proning �Continuous lateral rotation therapy (CLRT) �Management of hemodynamic changes (PPV → decrease venous return → decrease preload → CO) �Nutrition therapy

Rotoprone Bed

Complications of ARDS/ Treatment � VAP � Barotrauma- rupture of alveoli d/t increased peak airway pressures -Minimize risk/damage- ventilate w/ lower Tv � Volutrauma- alveolar fracture & leaking of fluid into alveoli -Again minimized by use of lower Tv � Stress ulcers -Prevent or Tx w/ PPIs, H 2 antagonists, enteral nutrition � Renal Failure- damage from insufficient O 2 perfusion
Endotracheal Intubation & Mechanical Ventilation NURS 241 Chapter 66 (p. 1698 -1707)
Indications for Endotracheal Intubation �Upper airway obstruction �Apnea �High risk for aspiration �Ineffective secretion clearance �Respiratory distress or failure
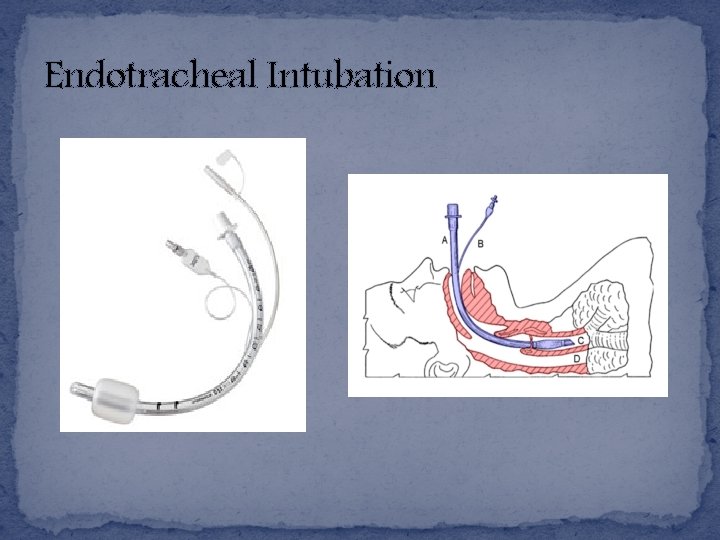
Endotracheal Intubation

What is the best immediate assessment to verify correct endotracheal tube placement?
Mechanical Ventilation (MV) Settings �Ventilator Mode (CMV, SIMV, APRV) �Fi. O 2 - fraction of inspired O 2 �Tidal Volume- volume delivered w/ each breath, 6 -10 ml/kg �Respiratory rate �PEEP (positive end expiratory pressure)- keep alveoli expanded
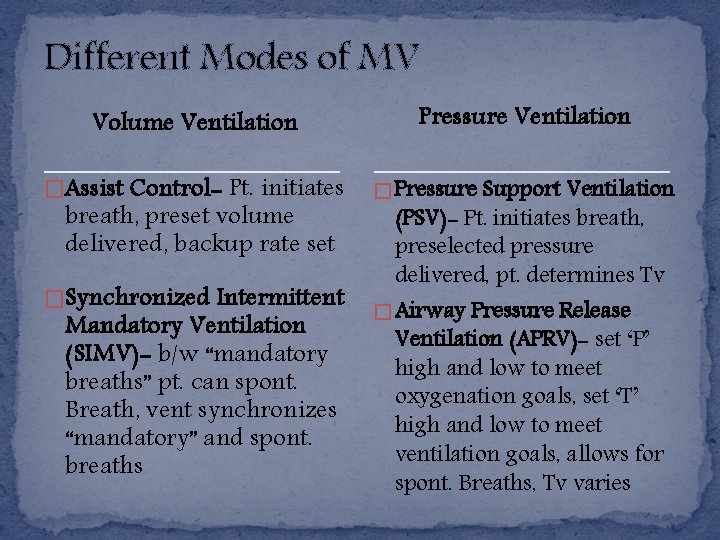
Different Modes of MV Volume Ventilation Pressure Ventilation �Assist Control- Pt. initiates � Pressure Support Ventilation breath, preset volume delivered, backup rate set �Synchronized Intermittent Mandatory Ventilation (SIMV)- b/w “mandatory breaths” pt. can spont. Breath, vent synchronizes “mandatory” and spont. breaths (PSV)- Pt. initiates breath, preselected pressure delivered, pt. determines Tv � Airway Pressure Release Ventilation (APRV)- set ‘P’ high and low to meet oxygenation goals, set ‘T’ high and low to meet ventilation goals, allows for spont. Breaths, Tv varies
Also common �Continuous Mandatory Ventilation (CMV) -Present Tv, rate, PEEP -Preset Tv delivered for each preset breath
MV Complications � Barotrauma � Volutrauma � Alveolar hypoventilation- inappropriate vent settings, leakage in circuit or cuff, increased secretions, low V/Q ratio � Alveolar hyperventilation- Tv set too high � VAP � PPV → decreased venous return → compromised CO , increased ICP � Gastric ulcers → GIBs � Musculoskeletal problems- contractures, pressure ulcers, foot drop
Arterial Blood Gases & Acid/Base Imbalances NURS 241 Chapter 17 (p. 320 -324)
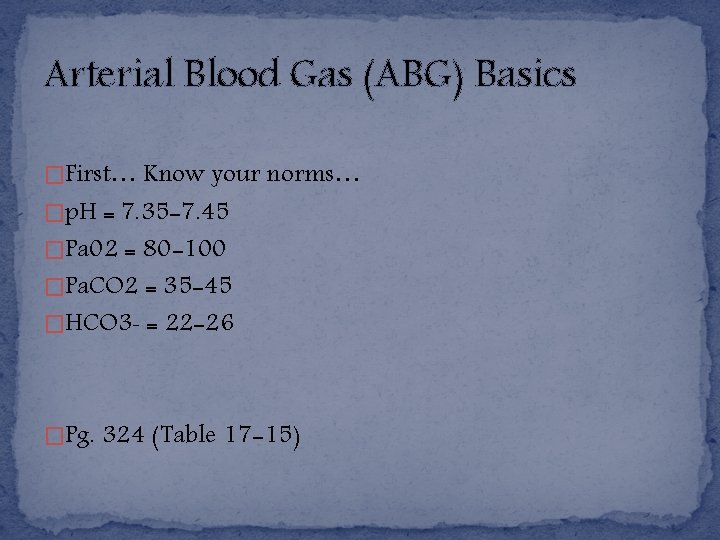
Arterial Blood Gas (ABG) Basics �First… Know your norms… �p. H = 7. 35 -7. 45 �Pa 02 = 80 -100 �Pa. CO 2 = 35 -45 �HCO 3 - = 22 -26 �Pg. 324 (Table 17 -15)
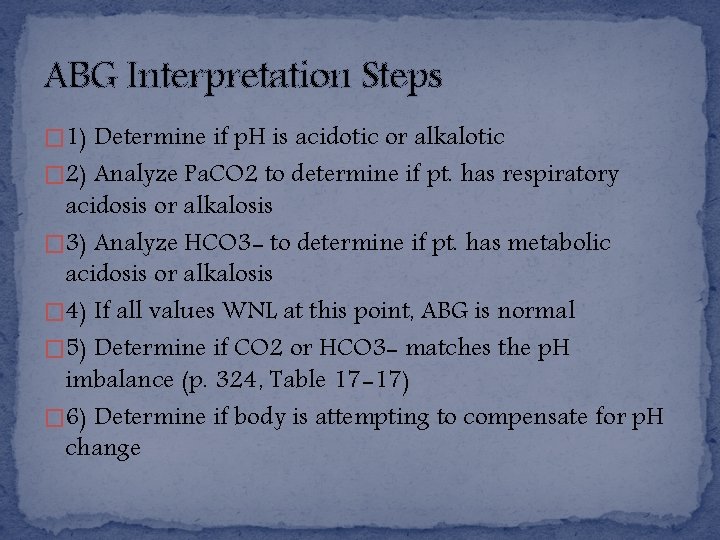
ABG Interpretation Steps � 1) Determine if p. H is acidotic or alkalotic � 2) Analyze Pa. CO 2 to determine if pt. has respiratory acidosis or alkalosis � 3) Analyze HCO 3 - to determine if pt. has metabolic acidosis or alkalosis � 4) If all values WNL at this point, ABG is normal � 5) Determine if CO 2 or HCO 3 - matches the p. H imbalance (p. 324, Table 17 -17) � 6) Determine if body is attempting to compensate for p. H change
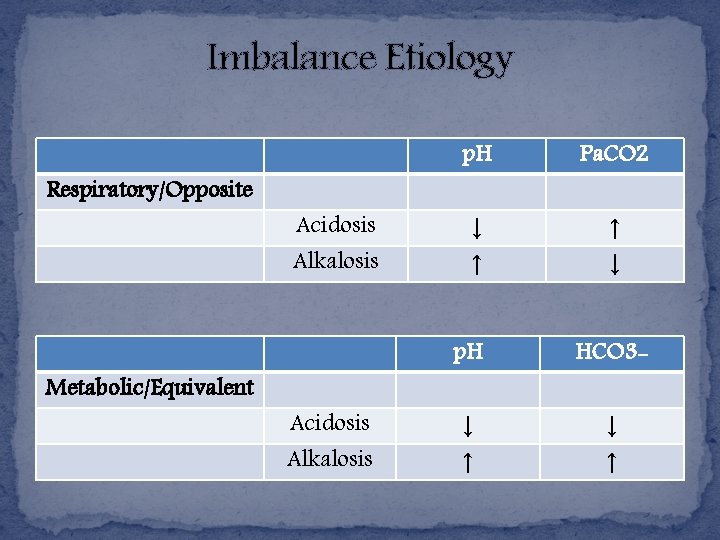
Imbalance Etiology Respiratory/Opposite Metabolic/Equivalent Acidosis Alkalosis p. H Pa. CO 2 ↓ ↑ ↑ ↓ p. H HCO 3 - ↓ ↑
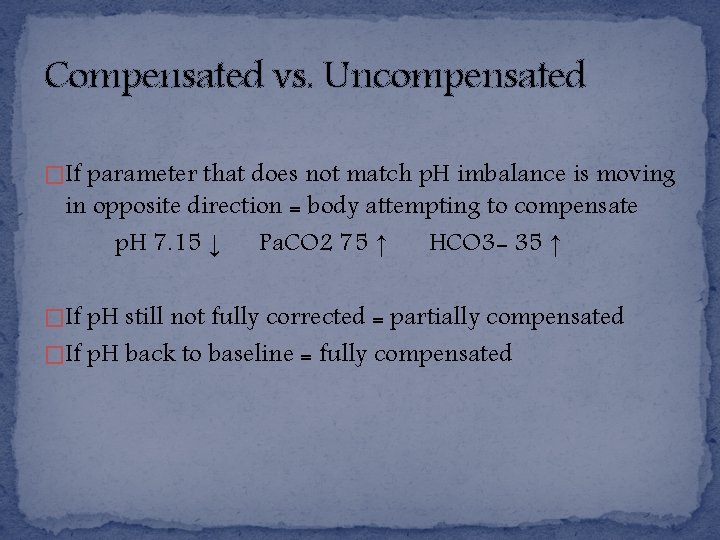
Compensated vs. Uncompensated �If parameter that does not match p. H imbalance is moving in opposite direction = body attempting to compensate p. H 7. 15 ↓ Pa. CO 2 75 ↑ HCO 3 - 35 ↑ �If p. H still not fully corrected = partially compensated �If p. H back to baseline = fully compensated
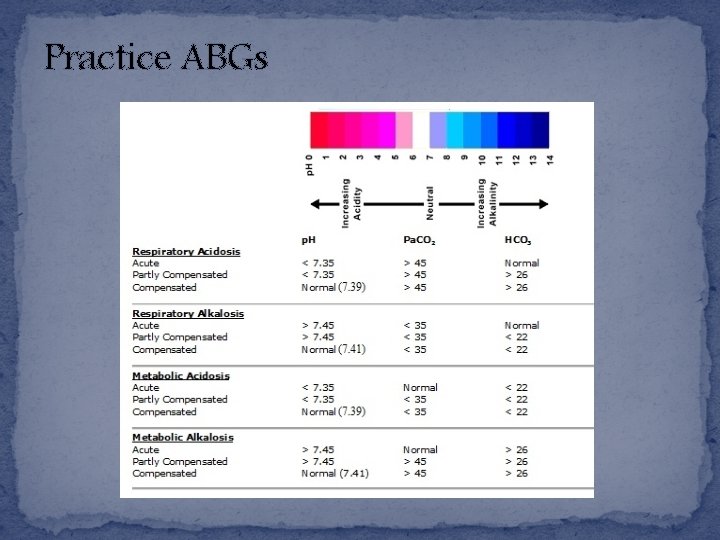
Practice ABGs
- Slides: 47