Acute Respiratory Distress Syndrome ARDS Done by Ammar
Acute Respiratory Distress Syndrome (ARDS) Done by: Ammar Masood Amareen and Mohammed Khaleel jaber. Supervised by: Dr. Samah shehata.
Contents General Considerations ● Etiology ● Pathogenesis ● Pathophysiology ● Pathology ● Clinical Presentation ● Diagnosis ● Treatment ● Prognosis ●
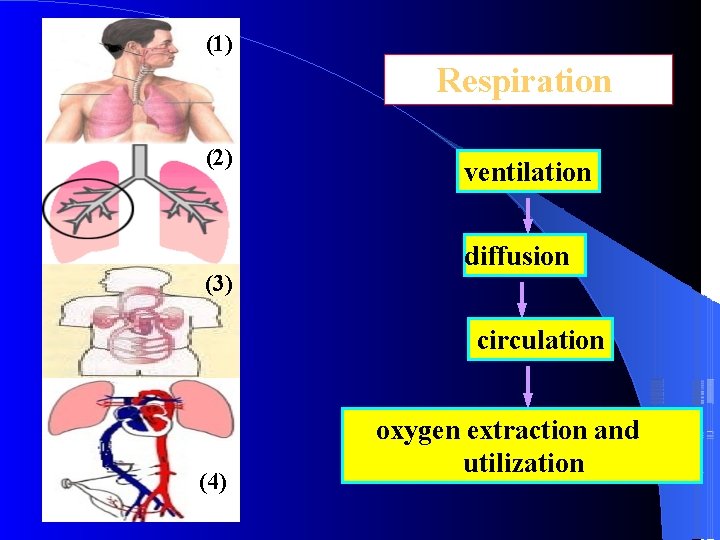
(1) Respiration (2) (3) ventilation diffusion circulation (4) oxygen extraction and utilization
General considerations Definitions Retrospect Incidence
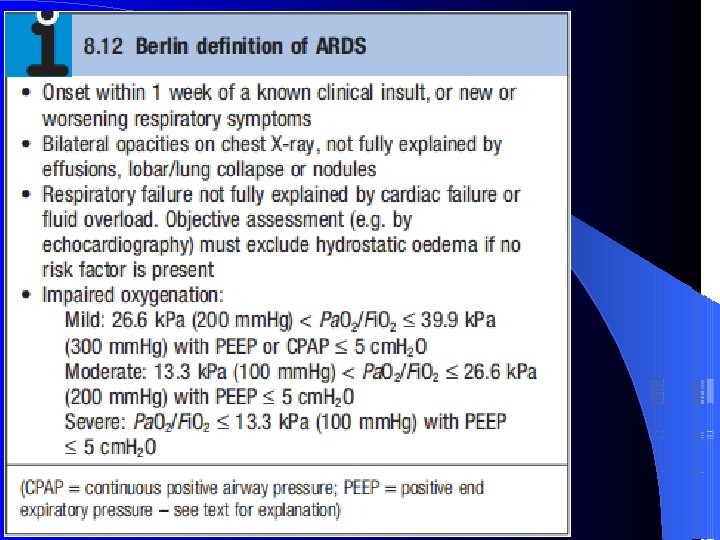
Definitions ARDS denotes acute hypoxemic respiratory failure following a systemic or pulmonary insult without evidence of heart failure. It is the most severe form of acute lung injury(ALI) and is characterized by bilateral, widespread radiographic pulmonary infiltrates, normal pulmonary capillary wedge pressure (PCWP) (<18 mm. Hg) and Pa 02/Fi 02 < 200 mm. Hg.
ALI is a syndrome of inflammation and increased permeability that is associated with a constellation of clinical, radiologic, and physiologic abnormalities that cannot be explained by, but may coexist with, left atrial or pulmonary capillary hypertension. Exclusion of left atrial hypertension as the primary cause of hypoxemia is critical to this definition
The distinction between ALI and ARDS is the degree of hypoxemia ALI: Pa 02/Fi 02 < 300 mm. Hg ARDS: Pa 02/Fi 02 < 200 mm. Hg
Incidence Controversy still exists about the correct incidence because of differing criteria used to define ARDS Incidence: annually 12. 6 to 18 per 100, 000 persons
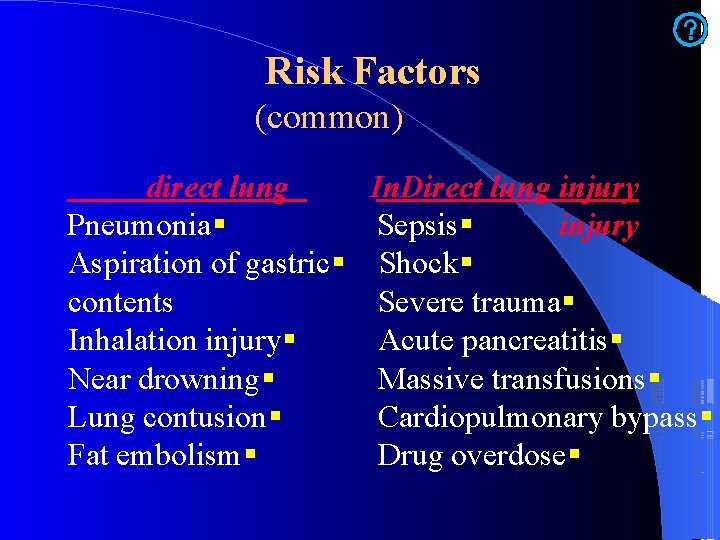
Risk Factors (common) direct lung In. Direct lung injury Pneumonia Sepsis Aspiration of gastric Shock contents Severe trauma Inhalation injury Acute pancreatitis Near drowning Massive transfusions Lung contusion Cardiopulmonary bypass Fat embolism Drug overdose
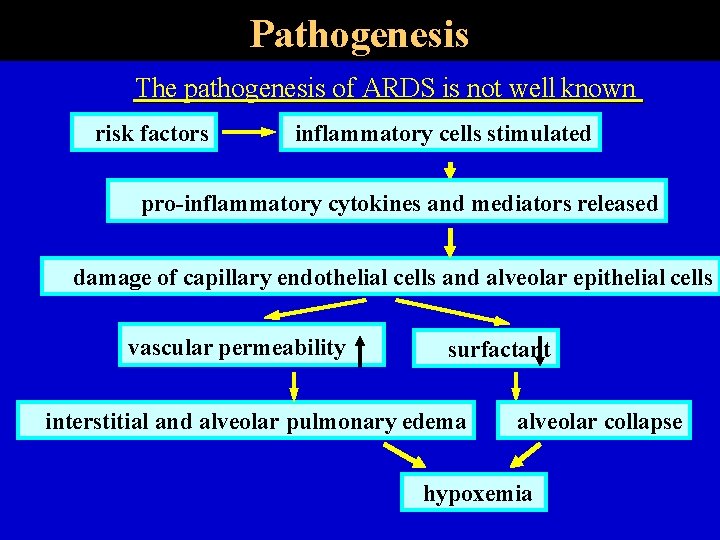
Pathogenesis The pathogenesis of ARDS is not well known risk factors inflammatory cells stimulated pro-inflammatory cytokines and mediators released damage of capillary endothelial cells and alveolar epithelial cells vascular permeability surfactant interstitial and alveolar pulmonary edema alveolar collapse hypoxemia
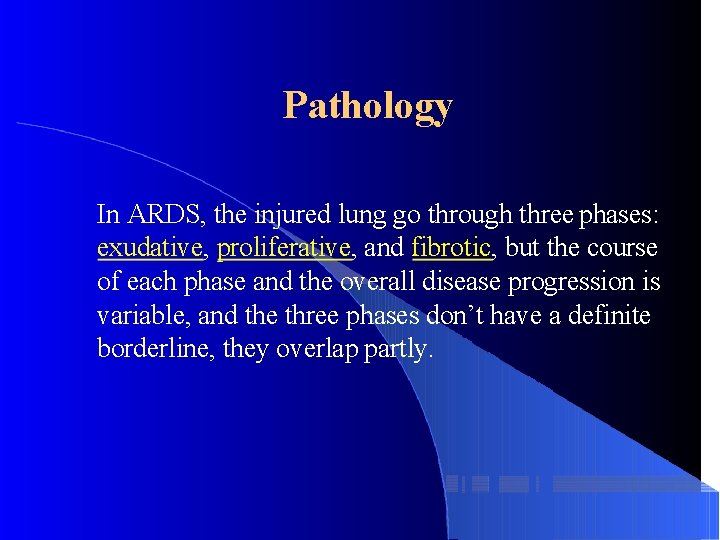
Pathology In ARDS, the injured lung go through three phases: exudative, proliferative, and fibrotic, but the course of each phase and the overall disease progression is variable, and the three phases don’t have a definite borderline, they overlap partly.
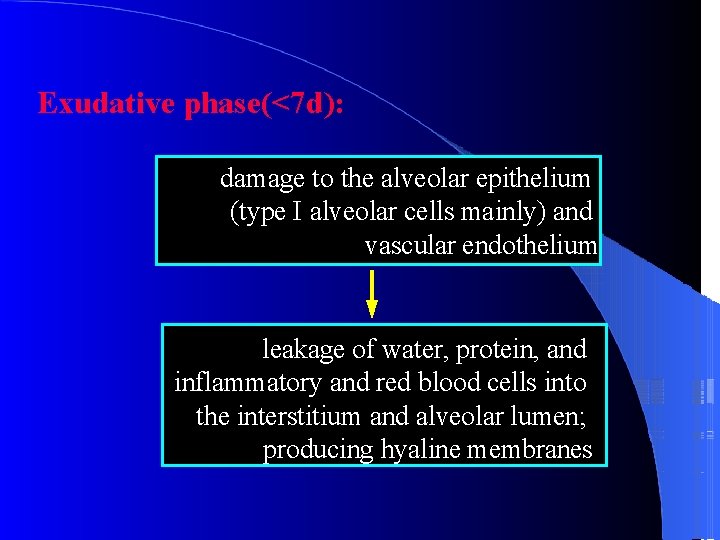
Exudative phase(<7 d): damage to the alveolar epithelium (type I alveolar cells mainly) and vascular endothelium leakage of water, protein, and inflammatory and red blood cells into the interstitium and alveolar lumen; producing hyaline membranes
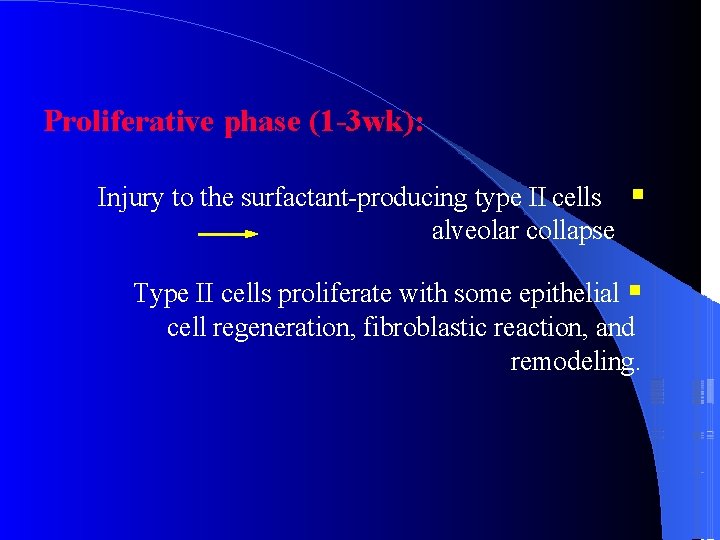
Proliferative phase (1 -3 wk): Injury to the surfactant-producing type II cells alveolar collapse Type II cells proliferate with some epithelial cell regeneration, fibroblastic reaction, and remodeling.
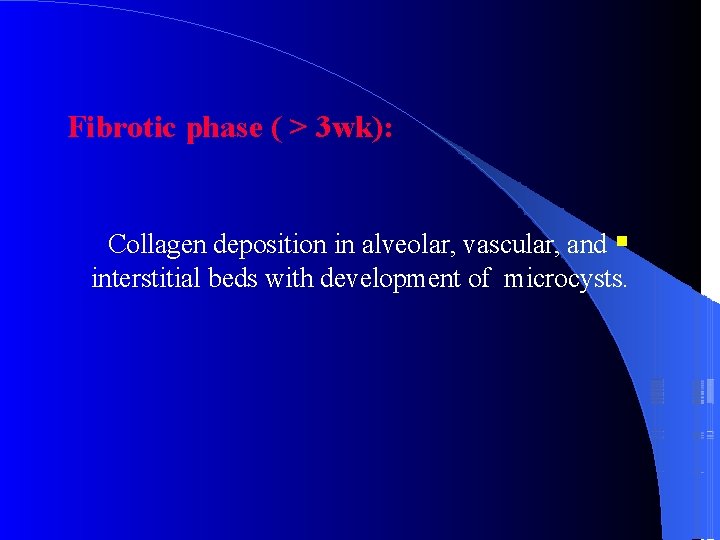
Fibrotic phase ( > 3 wk): Collagen deposition in alveolar, vascular, and interstitial beds with development of microcysts.
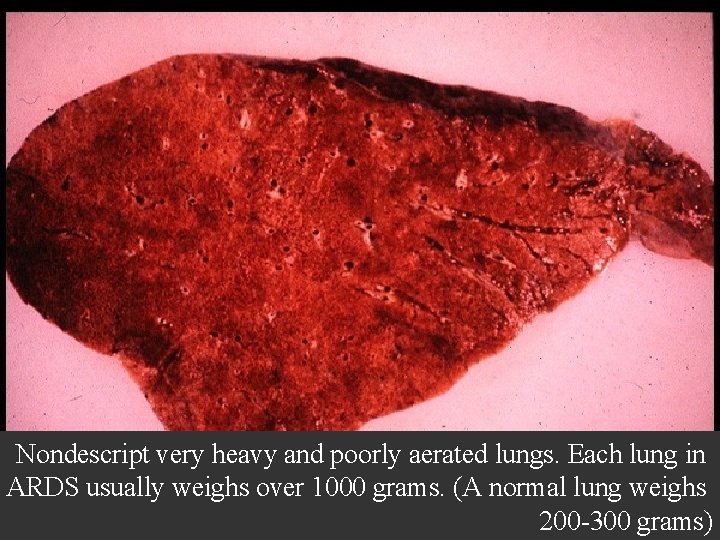
Nondescript very heavy and poorly aerated lungs. Each lung in ARDS usually weighs over 1000 grams. (A normal lung weighs 200 -300 grams)
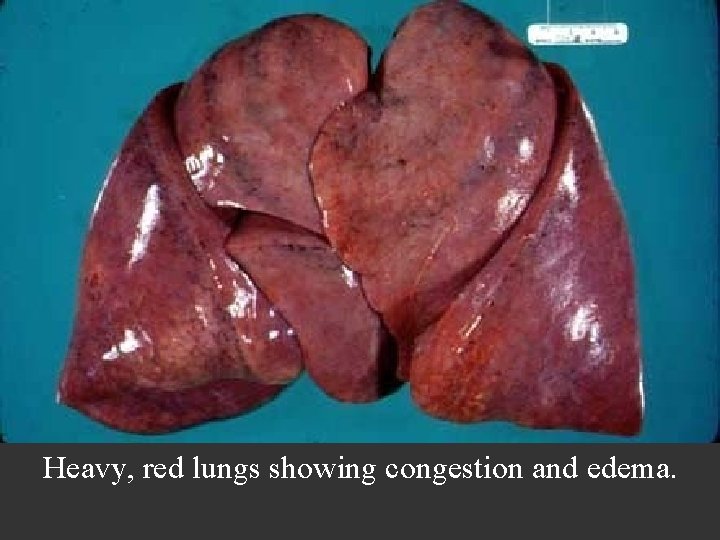
Heavy, red lungs showing congestion and edema.

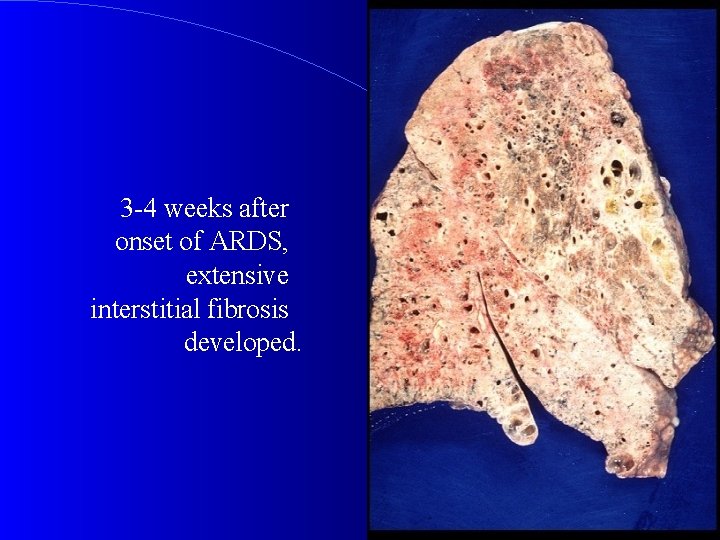
3 -4 weeks after onset of ARDS, extensive interstitial fibrosis developed.
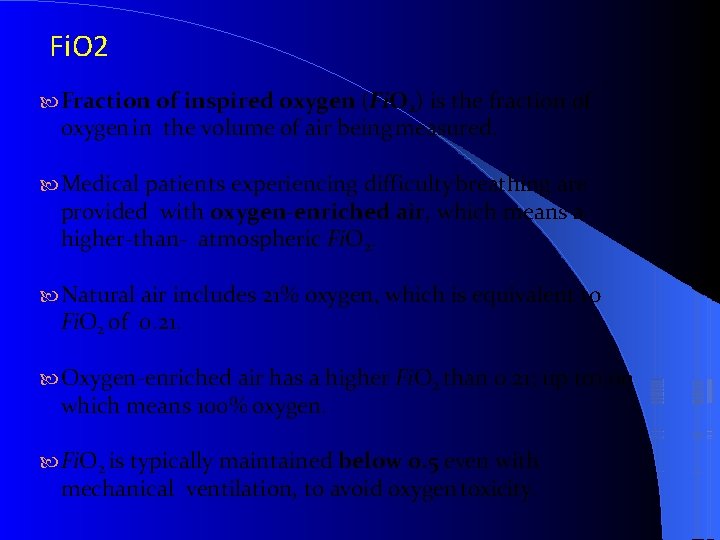
Fi. O 2 Fraction of inspired oxygen (Fi. O 2) is the fraction of oxygen in the volume of air being measured. Medical patients experiencing difficulty breathing are provided with oxygen-enriched air, which means a higher-than- atmospheric Fi. O 2. Natural air includes 21% oxygen, which is equivalent to Fi. O 2 of 0. 21. Oxygen-enriched air has a higher Fi. O 2 than 0. 21; up to 1. 00 which means 100% oxygen. Fi. O 2 is typically maintained below 0. 5 even with mechanical ventilation, to avoid oxygen toxicity.

P o s i t i v e e n d e x p i PEEP
CXR Chest radiographic findings are non-specific and resemble those of typical pulmonary edema or pulmonary hemorrhage. There are diffuse bilateral coalescent opacities (the only radiological criterion defined by the Consensus Conference). The time course of ARDS may help in differentiating it from typical pulmonary edema. Chest x-ray features usually develop 12 -24 hours after initial lung insult as a result of proteinaceous interstitial edema. Within one week, alveolar pulmonary edema (hyaline membrane) occurs due to type 1 pneumocyte damage. In contrast to cardiogenic pulmonary edema, which clears in response to diuretic therapy, ARDS persists for days to weeks.
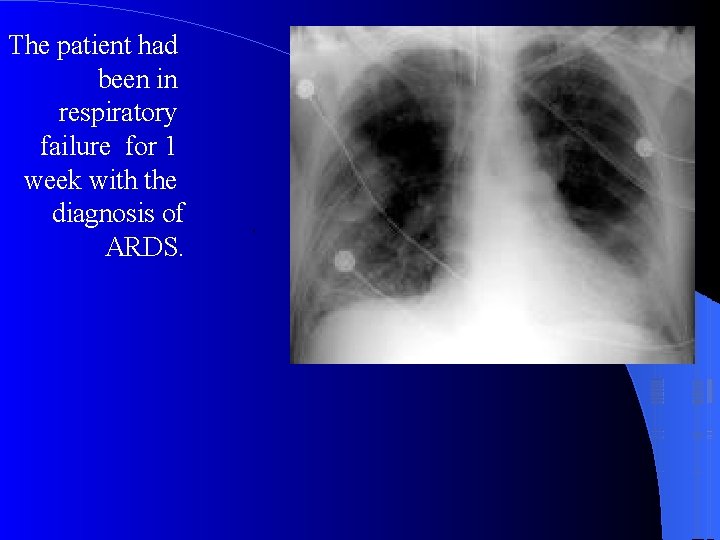
The patient had been in respiratory failure for 1 week with the diagnosis of ARDS. .
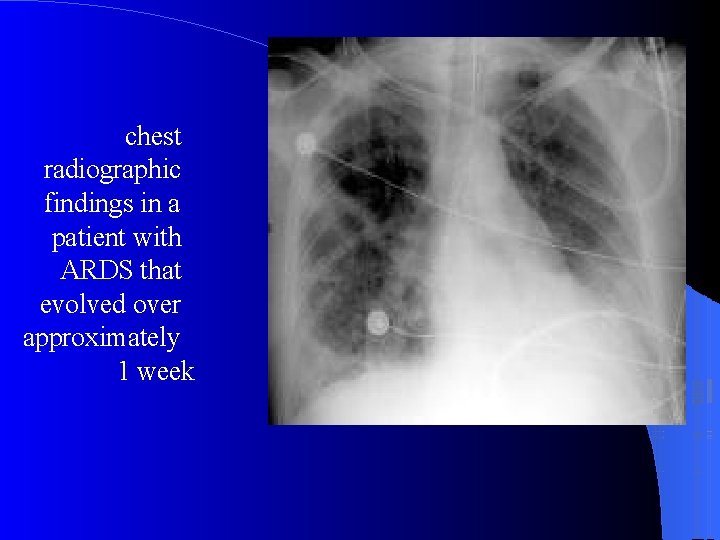
chest radiographic findings in a patient with ARDS that evolved over approximately 1 week
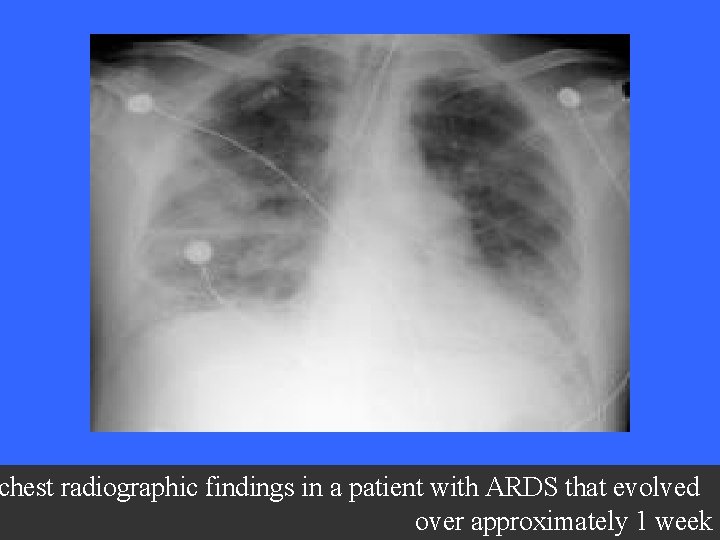
chest radiographic findings in a patient with ARDS that evolved over approximately 1 week
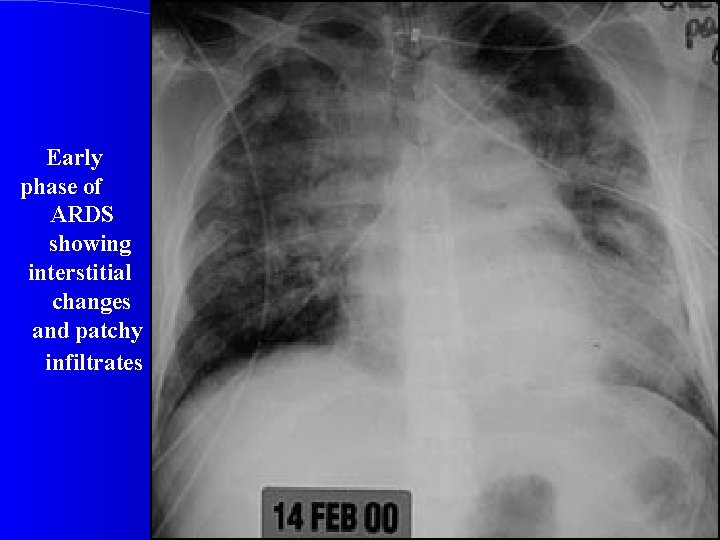
Early phase of ARDS showing interstitial changes and patchy infiltrates
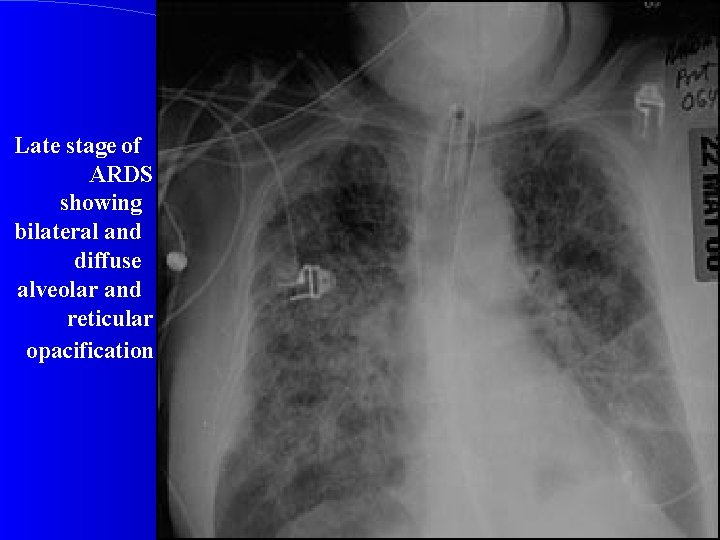
Late stage of ARDS showing bilateral and diffuse alveolar and reticular opacification

Arterial Blood Gas (ABG) Sputum, Blood, Urine culture : To look for underlying infection Amylase and Lipase : To rule out Acute pancreatitis
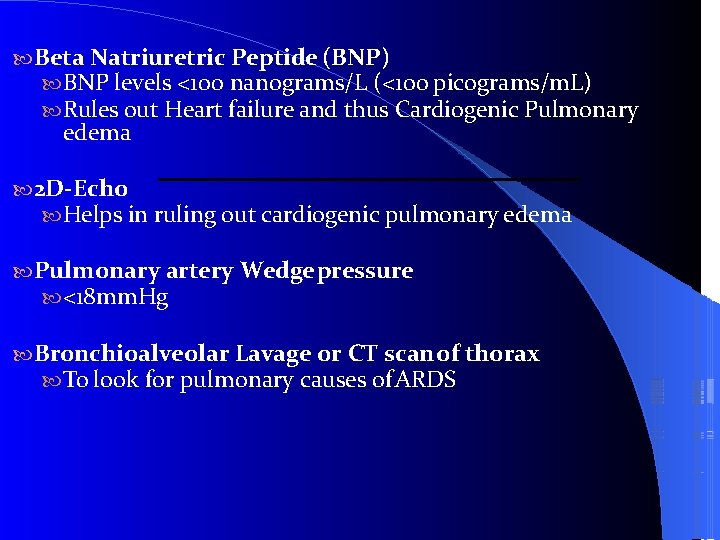
Beta Natriuretric Peptide (BNP) BNP levels <100 nanograms/L (<100 picograms/m. L) Rules out Heart failure and thus Cardiogenic Pulmonary edema 2 D-Echo Helps in ruling out cardiogenic pulmonary edema Pulmonary artery Wedge pressure <18 mm. Hg Bronchioalveolar Lavage or CT scan of thorax To look for pulmonary causes of ARDS

Treatment Oxygenation and Ventilation Prone positioning Intravenous fluids Antimicrobials + identification and treatment of source of infection Supportive care
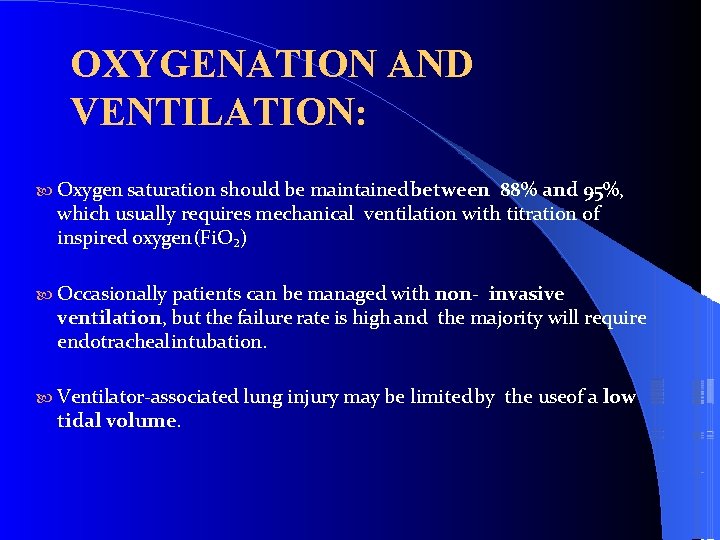
OXYGENATION AND VENTILATION: Oxygen saturation should be maintained between 88% and 95%, which usually requires mechanical ventilation with titration of inspired oxygen (Fi. O₂) Occasionally patients can be managed with non- invasive ventilation, but the failure rate is high and the majority will require endotracheal intubation. Ventilator-associated lung injury may be limited by the useof a low tidal volume.
PRONE POSITIONING: Prone positioning can improve oxygenation in patients with ARDS and has been shown to reduce mortality in patients with severe ARDS (Pa. O₂/Fi. O₂ <150). Complications of prone positioning, includes : facial oedema, pressure sores, and dislodgement of catheters and endotracheal tubes, prone positioning should only be considered in patients with severe ARDS (Pa. O₂/Fi. O₂ <150).
IV FLUIDS: The patient's fluid balance should be maintained as slightly negative or neutral (providing the patient is not in shock). A central line is recommended to measure the central venous pressure (CVP), with regular assessments of fluid status. The goal is to keep the CVP <4 cm H₂O.
IDENTIFICATION OF SOURCE OF INFECTION+ANTI-MICROBIAL THERAPTY In patients who have an infectious cause for ARDS (e. g. , pneumonia or sepsis), the prompt initiation of antimicrobials is important. Empirical antibiotics targeted at the suspected underlying infection should be used as soon as possible after obtaining appropriate cultures including blood, sputum, and urine cultures. Once culture results are available, the antimicrobial regimen can be tailored for the identified organism.
SUPPORATIVE CARE: Prevention of deep vein thrombosis Blood glucose control Prophylaxis against stress-induced gastrointestinal Bleeding Haemodynamic support to maintain a mean arterial pressure >60 mm. Hg Transfusion of packed red blood cells in patients with Hb <70 g/L (<7 g/d. L).
SUPPORATIVE CARE: Nutrition should be provided enterally where possible. Inhaled or intravenous beta-adrenergic agonists to promote alveolar fluid clearance and resolution of pulmonary oedema are not recommended. Neither early nor late administration of corticosteroids has been shown to improve mortality in patients with ARDS, and their routine use is not recommended
Prognosis Mortality rate: greater than 50% between 1979 and 1994, more recent studies show a decline in mortality to be 35%~40% If ARDS is accompanied by sepsis, the mortality rate may reach 90%. The major causes of death in ARDS are the primary illness and secondary complications such as organ failure sepsis. Most survivors of ARDS are left with some pulmonary symptoms (cough, dyspnea, sputum production), which tend to improve over time
Summarization ARDS denotes acute hypoxemic respiratory failure following a systemic or pulmonary insult without evidence of HF, and is the most severe form of ALI. It is characterized by dyspnea, profound hypoxemia, decreased lung compliance, and diffuse bilateral infiltrates on chest radiography. Provision of supplemental oxygen, lung rest, and supportive care the fundamentals of therapy, endotracheal intubation and mechanical ventilation are frequently required, Timely correction of the inciting clinical condition is essential for preventing further injury.
Emphases Definition of ARDS Pathophysiology Clinical presentation & diagnosis of ARDS The principles of treatment of ARDS

- Slides: 41