Acute Respiratory Distress Syndrome ARDS Chapter 68 Copyright



- Slides: 73
Acute Respiratory Distress Syndrome (ARDS) Chapter 68 Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
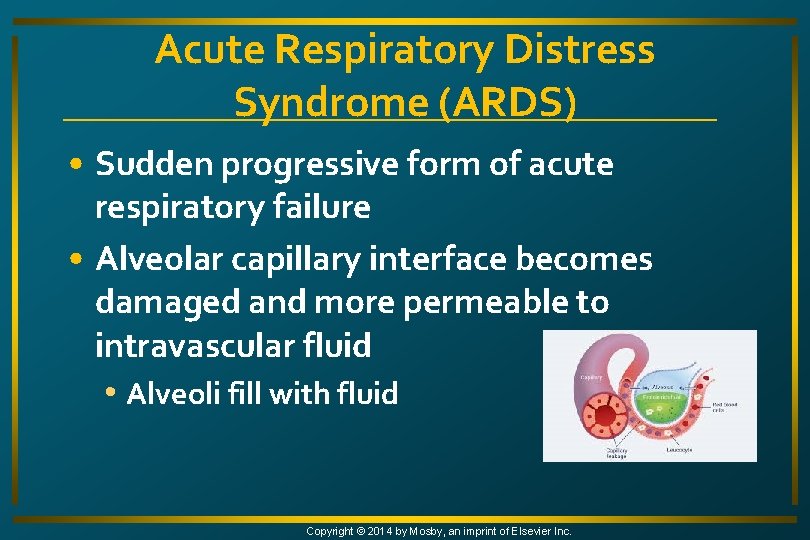
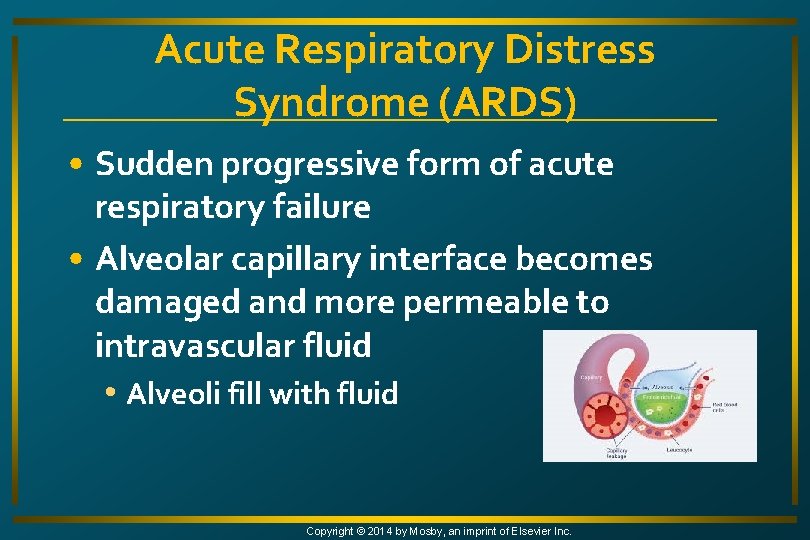
Acute Respiratory Distress Syndrome (ARDS) • Sudden progressive form of acute respiratory failure • Alveolar capillary interface becomes damaged and more permeable to intravascular fluid • Alveoli fill with fluid Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
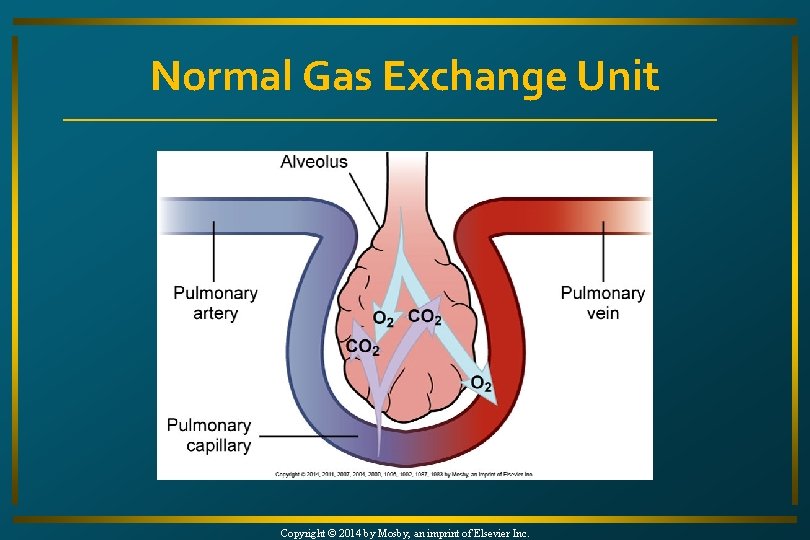
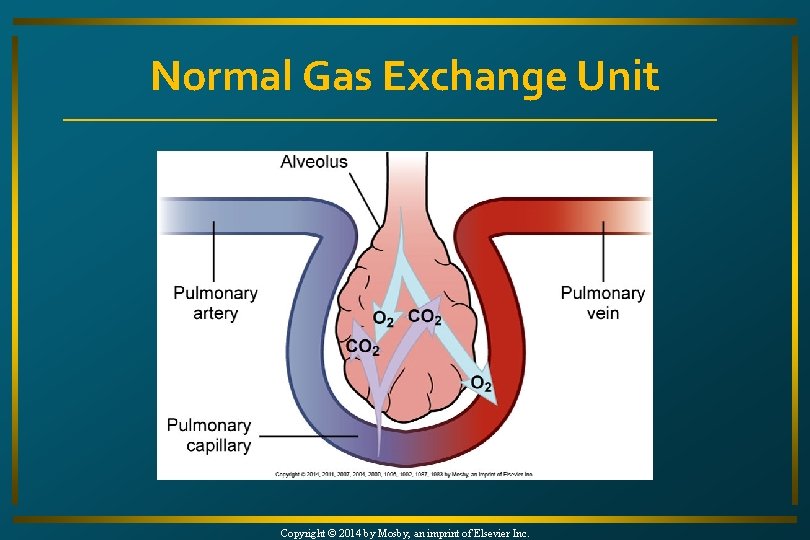
Normal Gas Exchange Unit Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
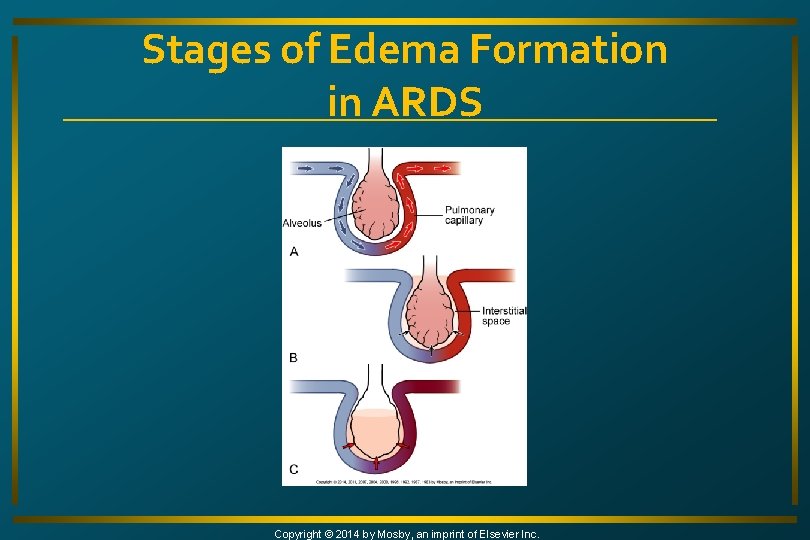
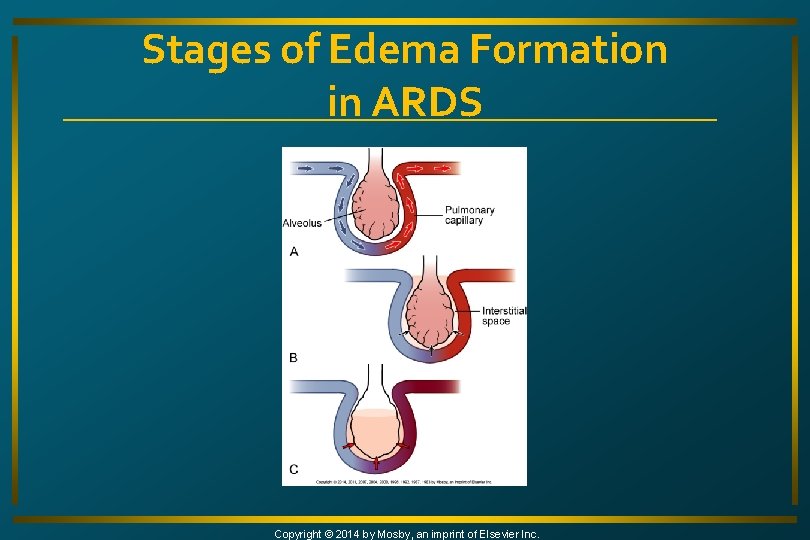
Stages of Edema Formation in ARDS Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

ARDS • Results • Severe dyspnea • Hypoxia • Decreased lung compliance • Diffuse pulmonary infiltrates • 150, 000 cases annually • 50% mortality rate Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • J. P. , an 82 -year-old woman, is brought to the ED from a long-term care facility. • 4 days ago, she aspirated her lunch. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study • The physician on call for the facility diagnosed her with aspiration pneumonia. • She was started on antibiotic therapy of azithromycin (Zithromax). i. Stockphoto/Thinkstock Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study • During the past 24 hours, J. P. has developed progressive dyspnea and restlessness. • On admission to the ED, she is confused and agitated. • At times she is gasping for air. • Chest x-ray shows diffuse infiltrates. Copyright © 2014 by Mosby, an imprint of Elsevier Inc. i. Stockphoto/Thinkstock
Case Study • What was the cause of J. P. ’s respiratory distress? • What are her risks for ARDS? • What is her priority of care? Copyright © 2014 by Mosby, an imprint of Elsevier Inc. i. Stockphoto/Thinkstock
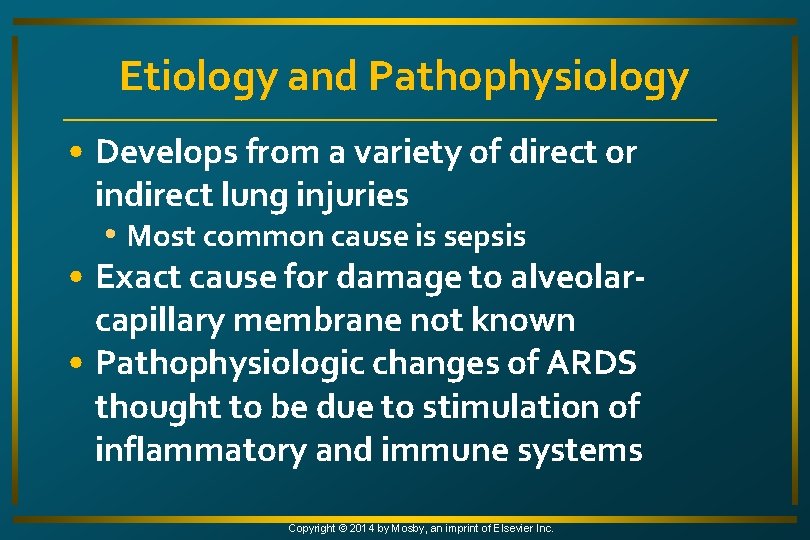
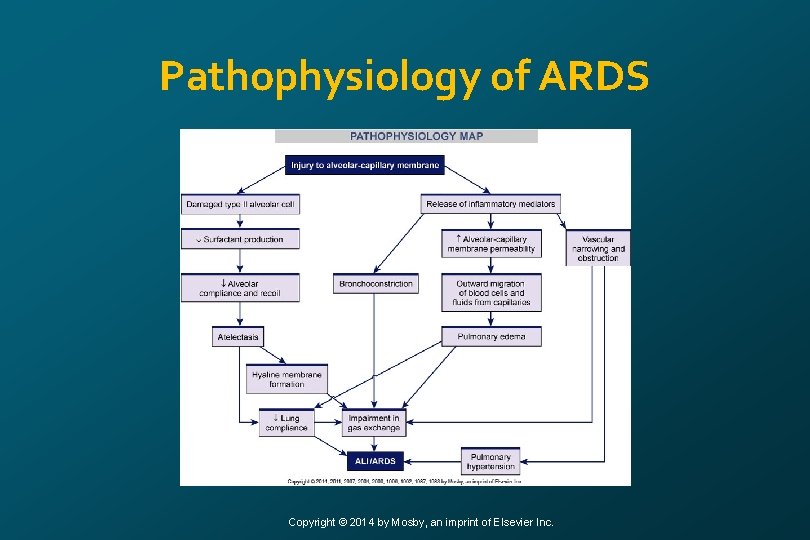
Etiology and Pathophysiology • Develops from a variety of direct or indirect lung injuries • Most common cause is sepsis • Exact cause for damage to alveolarcapillary membrane not known • Pathophysiologic changes of ARDS thought to be due to stimulation of inflammatory and immune systems Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
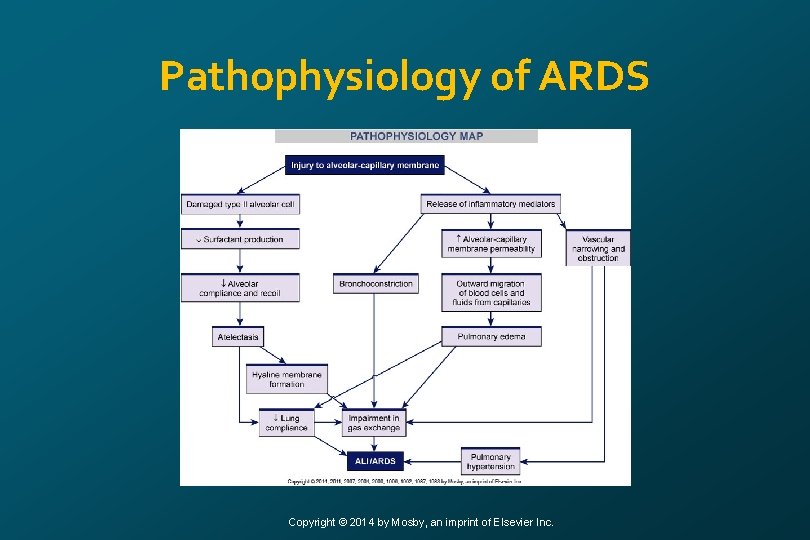
Pathophysiology of ARDS Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Neutrophils are attracted and release mediators, producing changes in lungs • ↑ Pulmonary capillary membrane permeability • Destruction of elastin and collagen • Formation of pulmonary microemboli • Pulmonary artery vasoconstriction Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
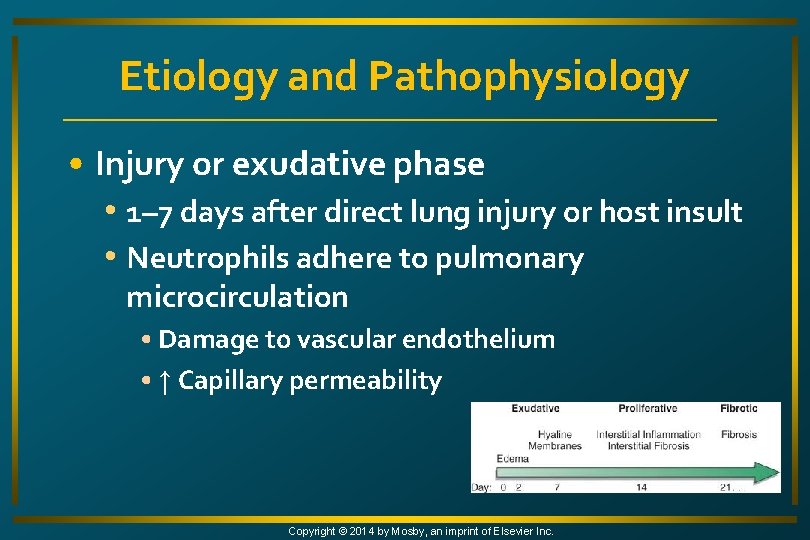
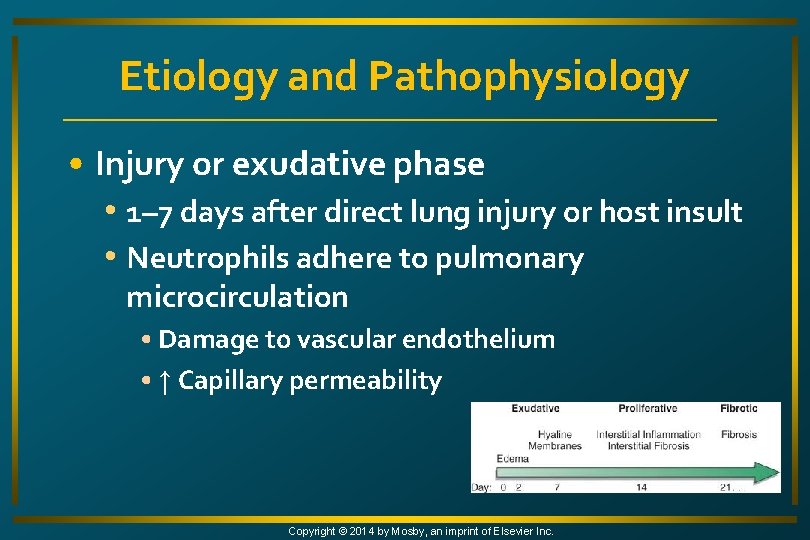
Etiology and Pathophysiology • Injury or exudative phase • 1– 7 days after direct lung injury or host insult • Neutrophils adhere to pulmonary microcirculation • Damage to vascular endothelium • ↑ Capillary permeability Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Injury or exudative phase • Engorgement of peribronchial and perivascular interstitial space • Fluid crosses into alveolar space • Intrapulmonary shunt develops as alveoli fill with fluid, and blood passing through cannot be oxygenated Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Injury or exudative phase • Alveolar cells type 1 and 2 are damaged • Surfactant dysfunction → atelectasis • Hyaline membranes line alveoli • Contribute to atelectasis and fibrosis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Injury or exudative phase • Severe V/Q mismatch and shunting of pulmonary capillary blood result in refractory hypoxemia • Unresponsive to increasing O 2 concentrations • Lungs become less compliant • Increased airway pressures must be generated Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Injury or exudative phase • ↑ Work of breathing (WOB) • ↑ Respiratory rate • ↓ Tidal volume • Produces respiratory alkalosis from increase in CO 2 removal • ↓ CO 2 and tissue perfusion Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Injury or exudative phase • Interstitial and alveolar edema (noncardiogenic pulmonary edema) • Atelectasis resulting in V/Q mismatch • Shunting of pulmonary capillary blood • Hypoxemia unresponsive to increasing concentrations of O 2 (refractory hypoxemia) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
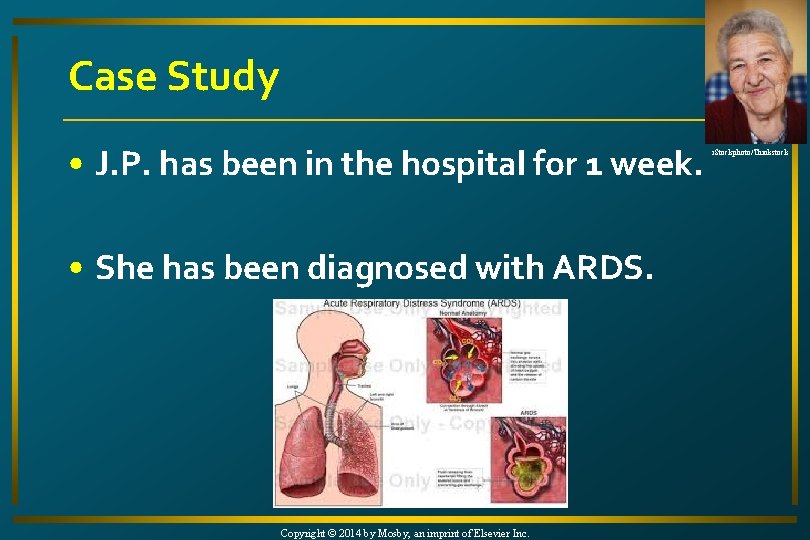
Case Study • J. P. has been in the hospital for 1 week. • She has been diagnosed with ARDS. Copyright © 2014 by Mosby, an imprint of Elsevier Inc. i. Stockphoto/Thinkstock
Case Study • She is on IV antibiotics and oxygen therapy, but continues to struggle to breath. i. Stockphoto/Thinkstock • Her oxygen saturation is 88% on 6 L via a face mask. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study • What is she experiencing clinically? • What is she at risk for in terms of ARDS progression? Copyright © 2014 by Mosby, an imprint of Elsevier Inc. i. Stockphoto/Thinkstock
Etiology and Pathophysiology • Reparative or proliferative phase • 1– 2 weeks after initial lung injury • Influx or neutrophils, monocytes, and lymphocytes • Fibroblast proliferation • Lung becomes dense and fibrous • Lung compliance continues to ↓ Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Reparative or proliferative phase • Hypoxemia worsens • Thickened alveolar membrane • Diffusion limitation and shunting • If reparative phase persists, widespread fibrosis results • If phase is arrested, lesions resolve Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
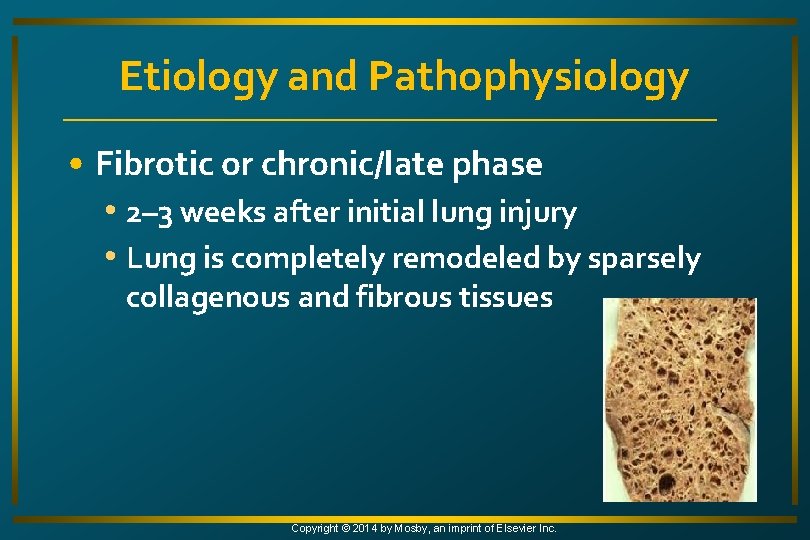
Etiology and Pathophysiology • Fibrotic or chronic/late phase • 2– 3 weeks after initial lung injury • Lung is completely remodeled by sparsely collagenous and fibrous tissues Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Etiology and Pathophysiology • Fibrotic or chronic/late phase • ↓ Lung compliance • ↓ Area for gas exchange • Hypoxemia continues • Pulmonary hypertension • Results from pulmonary vascular destruction and fibrosis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
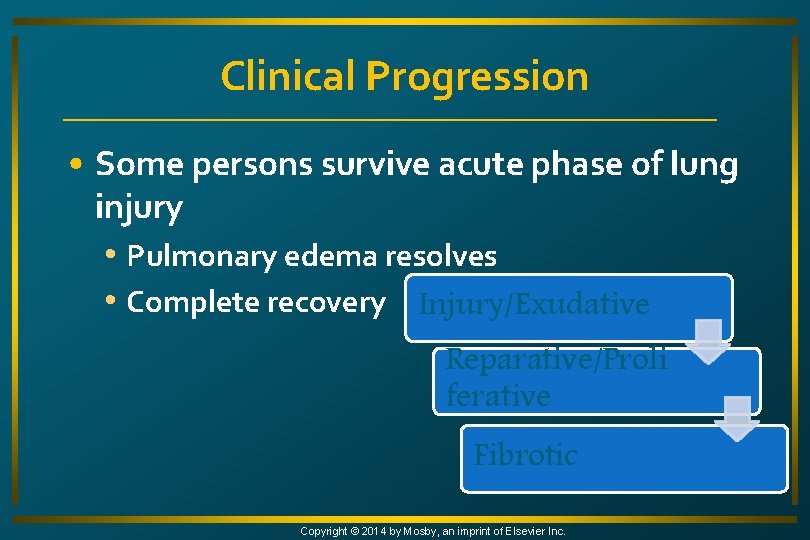
Clinical Progression • Some persons survive acute phase of lung injury • Pulmonary edema resolves • Complete recovery Injury/Exudative Reparative/Proli ferative Fibrotic Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Clinical Progression • Survival chances are poor for those who enter fibrotic phase • Requires long-term mechanical ventilation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Clinical Manifestations: Early • Dyspnea, tachypnea, cough, restlessness • Chest auscultation may be normal or may reveal fine, scattered crackles • ABGs • Mild hypoxemia and respiratory alkalosis caused by hyperventilation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Clinical Manifestations: Early • Chest x-ray may be normal or may show minimal scattered interstitial infiltrates • Edema may not show until 30% increase in lung fluid content Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
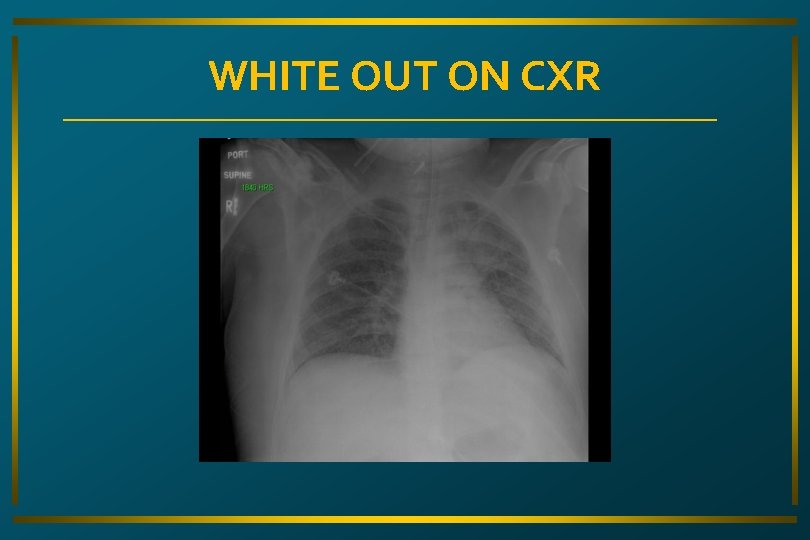
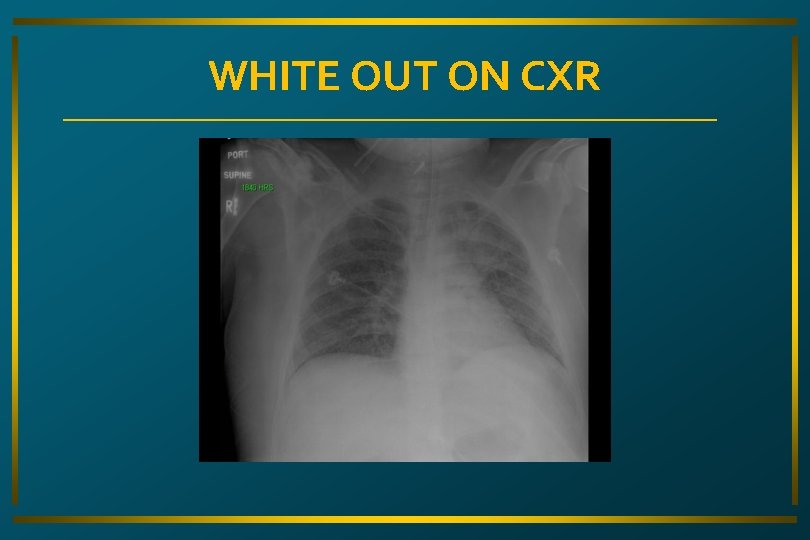
WHITE OUT ON CXR
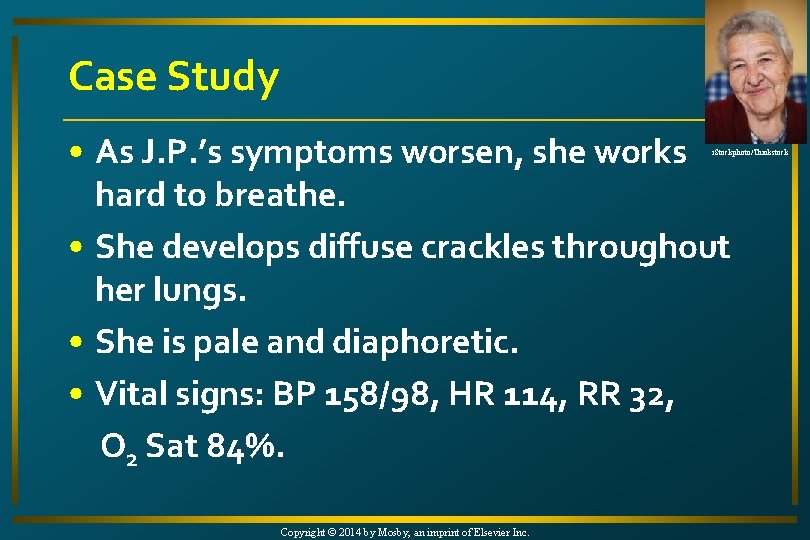
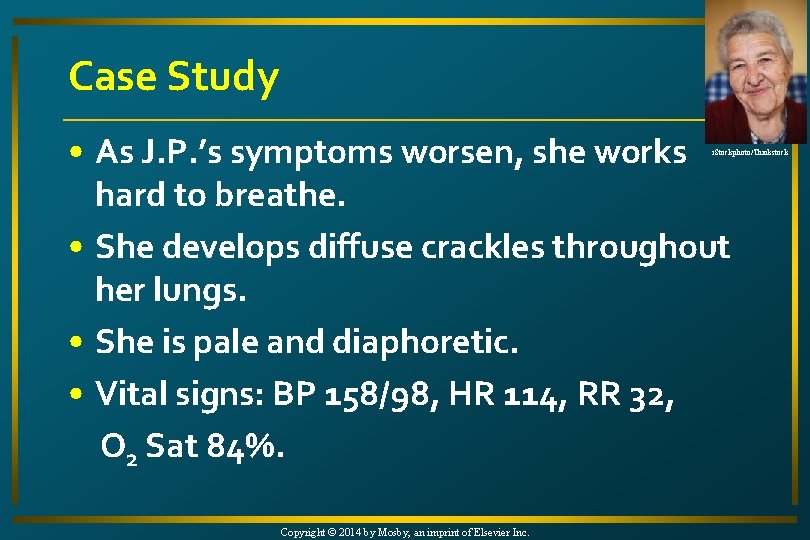
Case Study • As J. P. ’s symptoms worsen, she works hard to breathe. • She develops diffuse crackles throughout her lungs. • She is pale and diaphoretic. • Vital signs: BP 158/98, HR 114, RR 32, O 2 Sat 84%. i. Stockphoto/Thinkstock Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study i. Stockphoto/Thinkstock • What diagnostic tests would be indicated for J. P? • What is the next step in treatment for her? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Clinical Manifestations: Late • Symptoms worsen with progression of fluid accumulation and decreased lung compliance • Pulmonary function tests reveal decreased compliance, lung volumes, and functional residual capacity (FRC) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Clinical Manifestations: Late • Diffuse crackles and rhonchi • Tachycardia, diaphoresis, changes in sensorium with decreased mentation, cyanosis, and pallor • Hypoxemia and a Pa. O 2/FIO 2 ratio <200 despite increased FIO 2 Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Clinical Manifestations • As ARDS progresses, profound respiratory distress requires endotracheal intubation and positive-pressure ventilation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
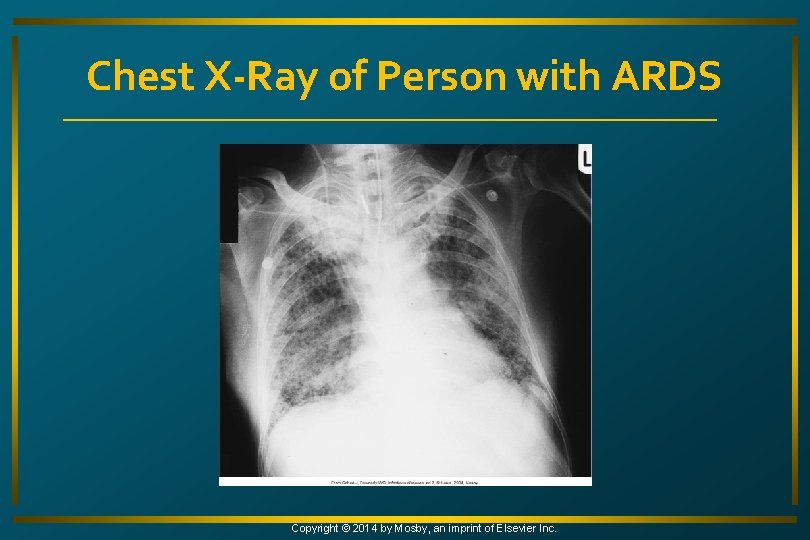
Clinical Manifestations • Chest x-ray termed whiteout or white lung because of consolidation and widespread infiltrates throughout lungs • Leaves few recognizable air spaces Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
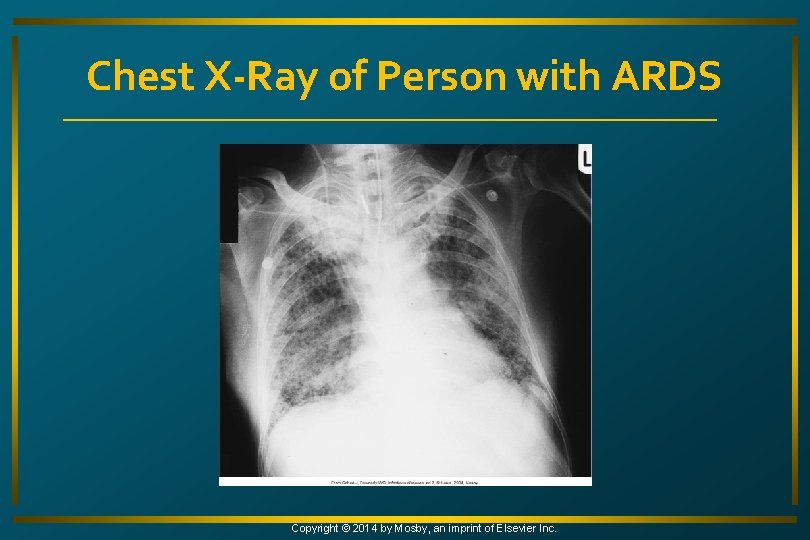
Chest X-Ray of Person with ARDS Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
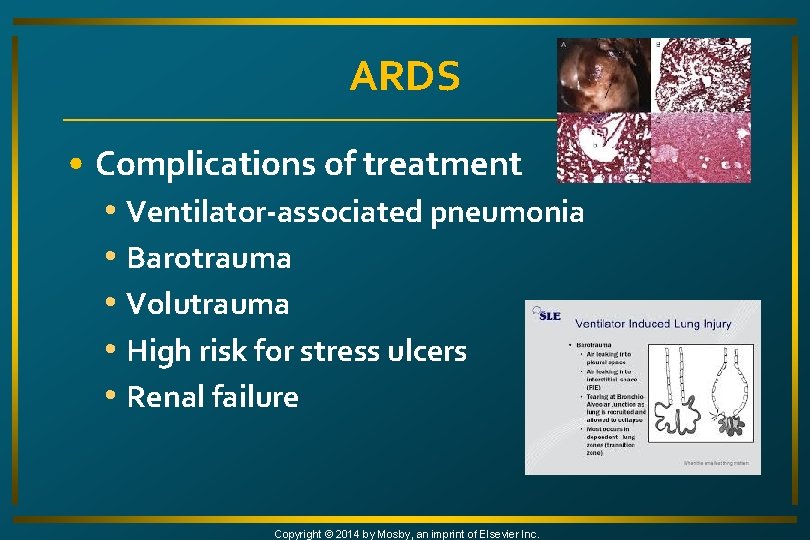
ARDS • Complications of treatment • Ventilator-associated pneumonia • Barotrauma • Volutrauma • High risk for stress ulcers • Renal failure Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Complications • Ventilator-associated pneumonia • Strategies for prevention of ventilatorassociated pneumonia • Strict infection control measures • Elevate HOB 45 degrees or more to prevent aspiration Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Complications • Barotrauma • Rupture of overdistended alveoli during mechanical ventilation • To avoid, ventilate with smaller tidal volumes • Higher Pa. CO 2 • Permissive hypercapnia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Complications • Volutrauma • Occurs when large tidal volumes are used to ventilate noncompliant lungs • Alveolar fracture and movement of fluids and proteins into alveolar spaces • Avoid by using smaller tidal volumes or pressure-control ventilation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Complications • Stress ulcers • Bleeding from stress ulcers occurs in 30% of patients with ARDS on mechanical ventilation • Management strategies • Correction of predisposing conditions • Prophylactic antiulcer agents • Early initiation of enteral nutrition Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Complications • Renal failure • Occurs from decreased renal tissue oxygenation from hypotension, hypoxemia, or hypercapnia • May also be caused by nephrotoxic drugs used for infection associated with ARDS Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study • J. P. ’s daughter arrives to be with her. • She shares that her mother had smoked for over 30 years, but quit 20 years ago. • She asks you if smoking contributed to her respiratory problems now. i. Stockphoto/Thinkstock Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Assessment • History of lung disease • Exposures to lung toxins • Tobacco use • Related hospitalizations • Spinal cord trauma • Extreme obesity Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Assessment • Use of O 2, inhalers, nebulizers, immunosuppressant therapy • Previous intubation • Thoracic or abdominal surgery • Exercise • Immunizations Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Assessment • Anorexia • Weight gain/loss • Diaphoresis • Dizziness • Dyspnea, wheezing, cough, sputum, palpitations, swollen feet • Changes in sleep pattern • Fatigue Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Assessment • Headache • Chest pain • Anxiety • Restlessness • Agitation • Pale, cool, clammy or warm, flushed skin • Use of accessory muscles Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Assessment • Shallow breathing with increased respiratory rate • Tachycardia progressing to bradycardia • Extra heart sounds • Abnormal breath sounds • Hypertension progressing to hypotension Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Assessment • Abdominal distention, ascites • Somnolence, confusion, delirium • Changes in p. H, Pa. CO 2, Pa. O 2, Sa. O 2 Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Assessment • Decreased tidal volume, FVC • Abnormal x-ray • Normal pulmonary artery wedge pressure (noncardiogenic pulmonary edema) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study • J. P. is now on mechanical ventilation, sedated to allow her to rest, and beginning to improve slowly. • Her O 2 saturation is now 92% and her blood gases are slowly returning to normal. Copyright © 2014 by Mosby, an imprint of Elsevier Inc. i. Stockphoto/Thinkstock
Nursing Diagnoses • Ineffective airway clearance • Ineffective breathing pattern • Risk for imbalanced fluid volume • Anxiety • Impaired gas exchange • Imbalanced nutrition: less than body requirements Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Planning • Following recovery • Pa. O 2 within normal limits or at baseline • Sa. O 2 >90% • Patent airway • Clear lungs on auscultation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Respiratory Therapy • Oxygen • High-flow systems used to maximize O 2 delivery • Sp. O 2 continuously monitored • Give lowest concentration that results in Pa. O 2 60 mm Hg or greater Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Respiratory Therapy • Risk for O 2 toxicity increases when FIO 2 exceeds 60% for >48 hours • Patients will commonly need intubation with mechanical ventilation because Pa. O 2 cannot be maintained at acceptable levels Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Respiratory Therapy • Mechanical ventilation • PEEP at 5 cm H 2 O compensates for loss of glottic formation • Opens collapsed alveoli Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Respiratory Therapy • Mechanical ventilation • Higher levels of PEEP are often needed to maintain Pa. O 2 at 60 mm Hg or greater • High levels of PEEP can compromise venous return • ↓ Preload, CO, and BP Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Respiratory Therapy • Alternative modes of mechanical ventilation if hypoxemia persists • Pressure support ventilation • Pressure release ventilation • Pressure control ventilation • Inverse ratio ventilation • High-frequency ventilation • Permissive hypercapnia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
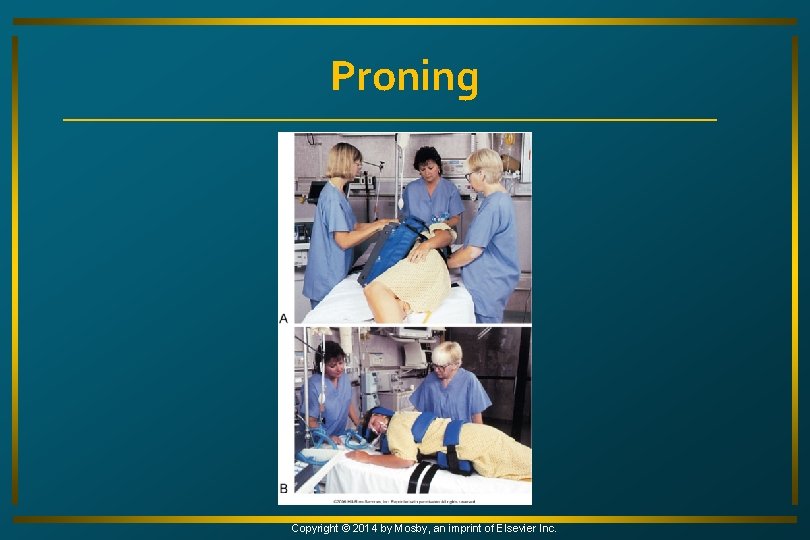
Respiratory Therapy • Positioning strategies • Turn from supine to prone position • May be sufficient to reduce inspired O 2 or PEEP • Mediastinal and heart contents place more pressure on lungs when in supine position than when in prone • Predisposes to atelectasis • Fluid pools in dependent regions of lung Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
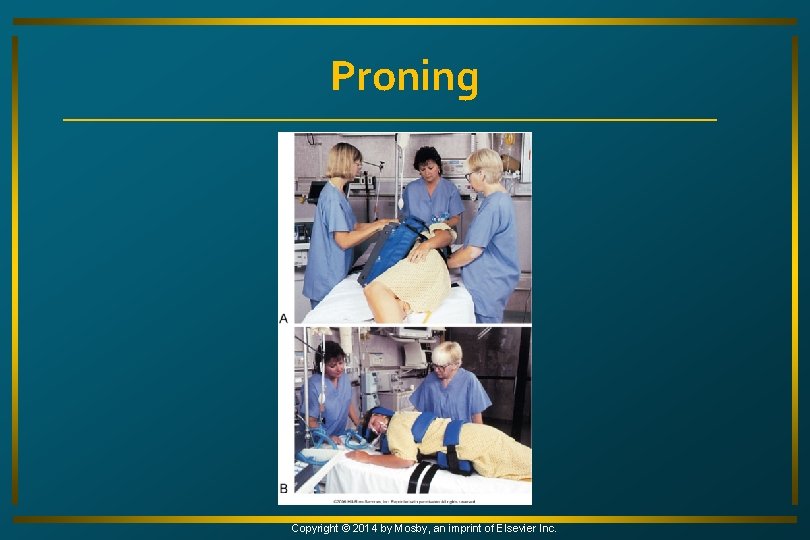
Proning Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Respiratory Therapy • Proning typically reserved for refractory hypoxemia not responding to otherapies • Plan for immediate repositioning for CPR Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Respiratory Therapy • Other positioning strategies • Continuous lateral rotation therapy (CLRT) • Kinetic therapy Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

ROTOPRONE BED
Continuous Lateral Rotation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Medical Supportive Therapy • Maintenance of cardiac output and tissue perfusion • Hemodynamic monitoring via a central venous or pulmonary artery catheter Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Medical Supportive Therapy • Maintenance of fluid balance • May be volume depleted and prone to hypertension and decreased CO from mechanical ventilation and PEEP • Monitor PAWP, daily weights, and I&O to assess fluid status Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Evaluation • No abnormal breath sounds • Effective cough and expectoration • Normal respiratory rate, rhythm, and depth • Synchronous thoracoabdominal movement • Appropriate use of accessory muscles Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Evaluation • Decreased or absent peripheral edema • Normal pulmonary artery or pulmonary artery wedge pressures • Decreased anxiety • Verbalization of positive attitude toward outcome Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Evaluation • Pa. O 2 and Pa. CO 2 within normal ranges or at baseline • Maintenance of weight or weight gain • Serum albumin and protein within normal ranges Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
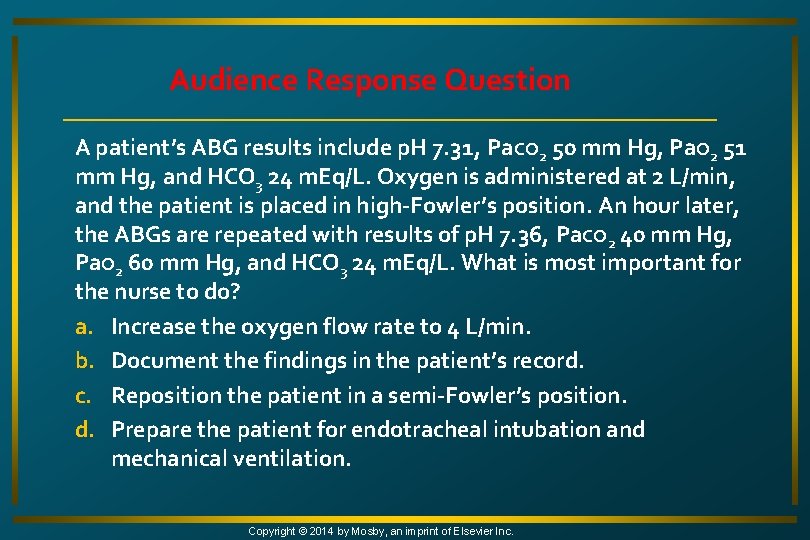
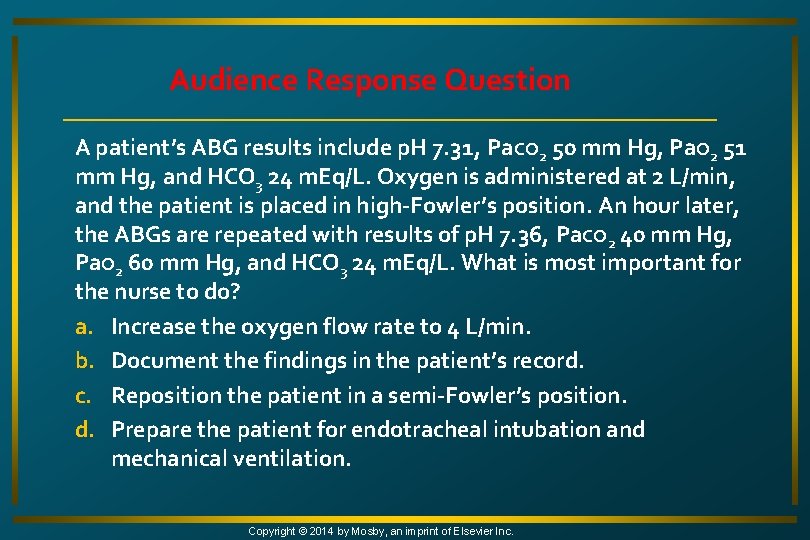
Audience Response Question A patient’s ABG results include p. H 7. 31, Pa. CO 2 50 mm Hg, Pa. O 2 51 mm Hg, and HCO 3 24 m. Eq/L. Oxygen is administered at 2 L/min, and the patient is placed in high-Fowler’s position. An hour later, the ABGs are repeated with results of p. H 7. 36, Pa. CO 2 40 mm Hg, Pa. O 2 60 mm Hg, and HCO 3 24 m. Eq/L. What is most important for the nurse to do? a. Increase the oxygen flow rate to 4 L/min. b. Document the findings in the patient’s record. c. Reposition the patient in a semi-Fowler’s position. d. Prepare the patient for endotracheal intubation and mechanical ventilation. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
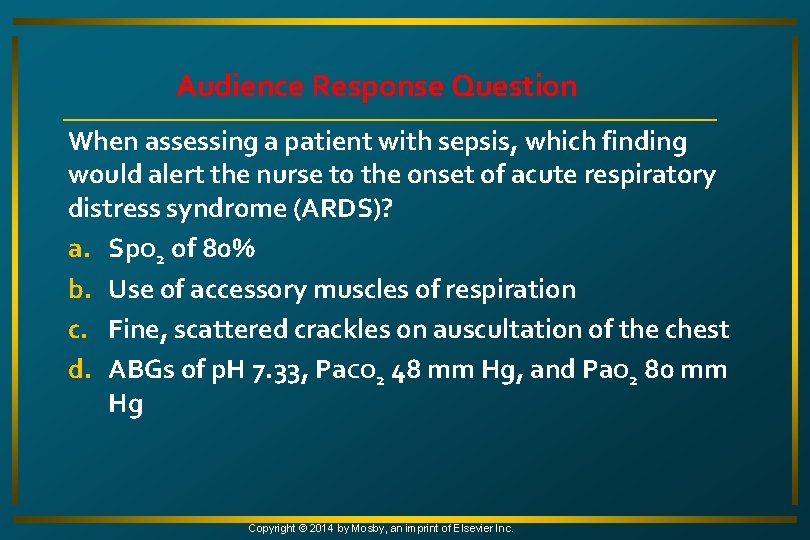
Audience Response Question When assessing a patient with sepsis, which finding would alert the nurse to the onset of acute respiratory distress syndrome (ARDS)? a. Sp. O 2 of 80% b. Use of accessory muscles of respiration c. Fine, scattered crackles on auscultation of the chest d. ABGs of p. H 7. 33, Pa. CO 2 48 mm Hg, and Pa. O 2 80 mm Hg Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
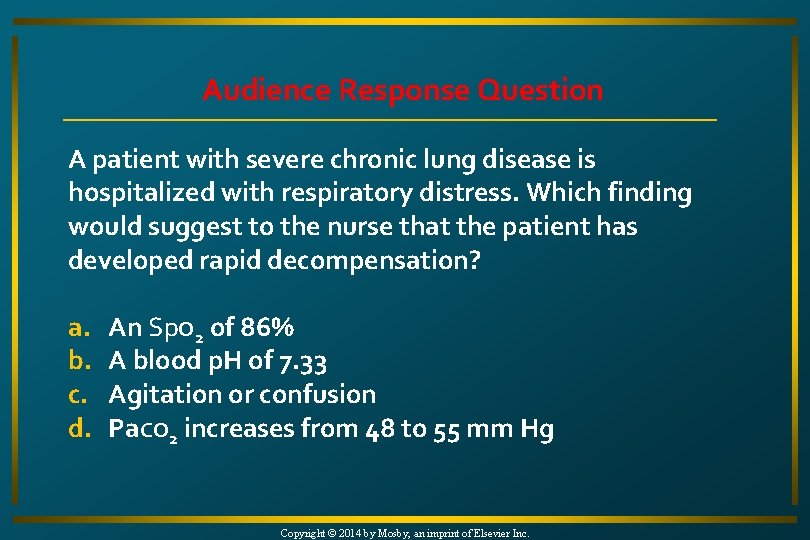
Audience Response Question A patient with severe chronic lung disease is hospitalized with respiratory distress. Which finding would suggest to the nurse that the patient has developed rapid decompensation? a. b. c. d. An Sp. O 2 of 86% A blood p. H of 7. 33 Agitation or confusion Pa. CO 2 increases from 48 to 55 mm Hg Copyright © 2014 by Mosby, an imprint of Elsevier Inc.