Acute Respiratory Distress Paul D Simmons MD Faculty






- Slides: 37

Acute Respiratory Distress Paul D. Simmons, MD Faculty Physician St. Mary’s Family Medicine Residency Grand Junction, Colorado
Objectives • Approach to the patient in respiratory distress. • Review the physiology of O 2 and CO 2 in the context of dyspnea. • Pitfalls in evaluating the dyspneic patient.
The Patient • Bob D. is a 49 year old man with type I diabetes mellitus presenting via EMS to your rural ER with acute shortness of breath. • Came on suddenly, woke him from sleep. • Worsened throughout morning. • Now associated with chest tightness. • He is unable to speak in full sentences.
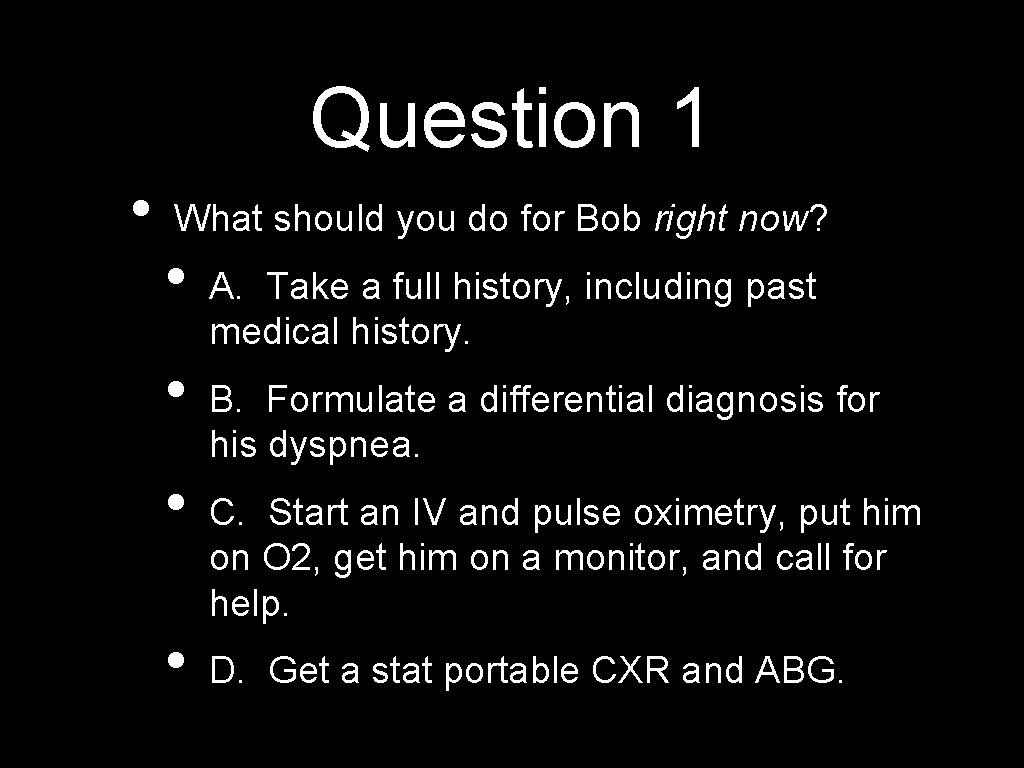
Question 1 • What should you do for Bob right now? • • A. Take a full history, including past medical history. B. Formulate a differential diagnosis for his dyspnea. C. Start an IV and pulse oximetry, put him on O 2, get him on a monitor, and call for help. D. Get a stat portable CXR and ABG.
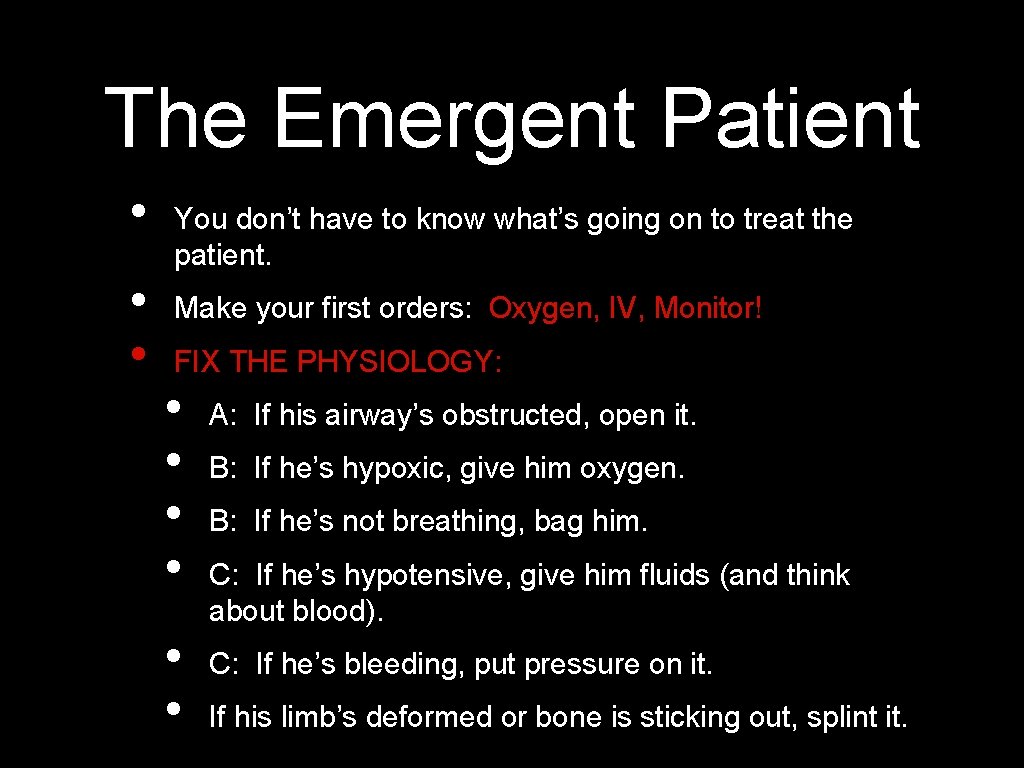
The Emergent Patient • • • You don’t have to know what’s going on to treat the patient. Make your first orders: Oxygen, IV, Monitor! FIX THE PHYSIOLOGY: • • • A: If his airway’s obstructed, open it. B: If he’s hypoxic, give him oxygen. B: If he’s not breathing, bag him. C: If he’s hypotensive, give him fluids (and think about blood). C: If he’s bleeding, put pressure on it. If his limb’s deformed or bone is sticking out, splint it.
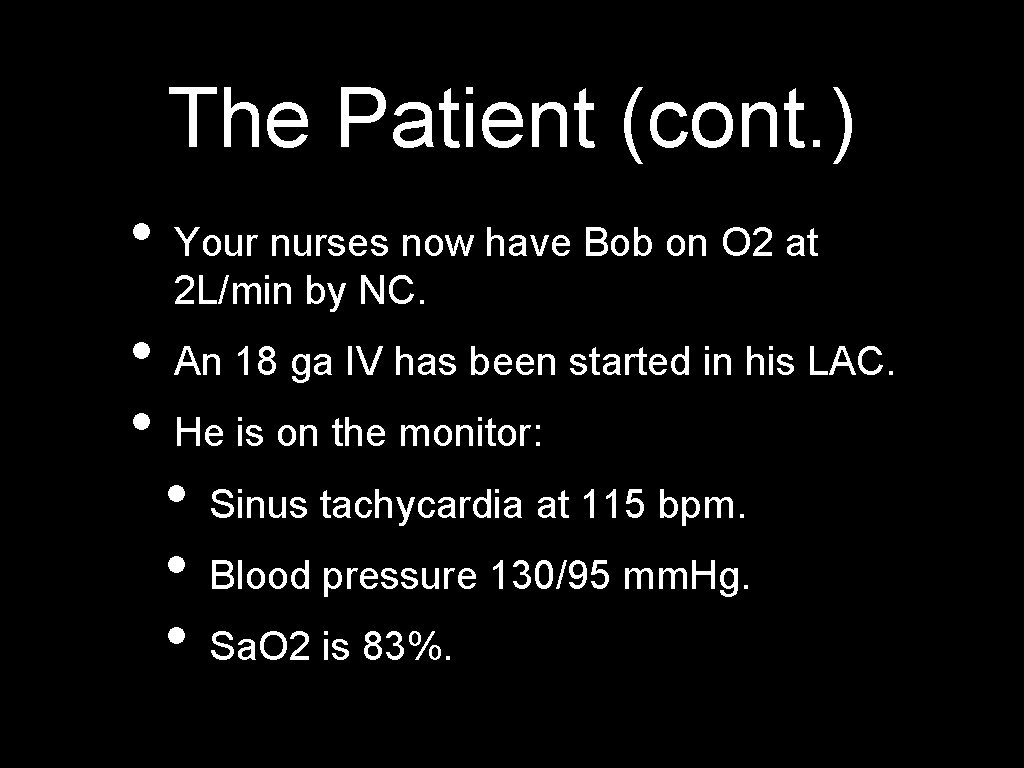
The Patient (cont. ) • • • Your nurses now have Bob on O 2 at 2 L/min by NC. An 18 ga IV has been started in his LAC. He is on the monitor: • • • Sinus tachycardia at 115 bpm. Blood pressure 130/95 mm. Hg. Sa. O 2 is 83%.

How To Give O 2 Route Max Fi. O 2 RA 21% NC 40% FM 60% NRB/reservoir 80% ETT/NIPPV 90 -100%
The Patient (cont. ) • • Now the nurses have Bob on the monitor, IV access established and O 2 via NRB at 10 L/min. • • • HR 95/min BP 152/90 mm. Hg Sa. O 2 97% So now you have a moment to think. . . and take more history.
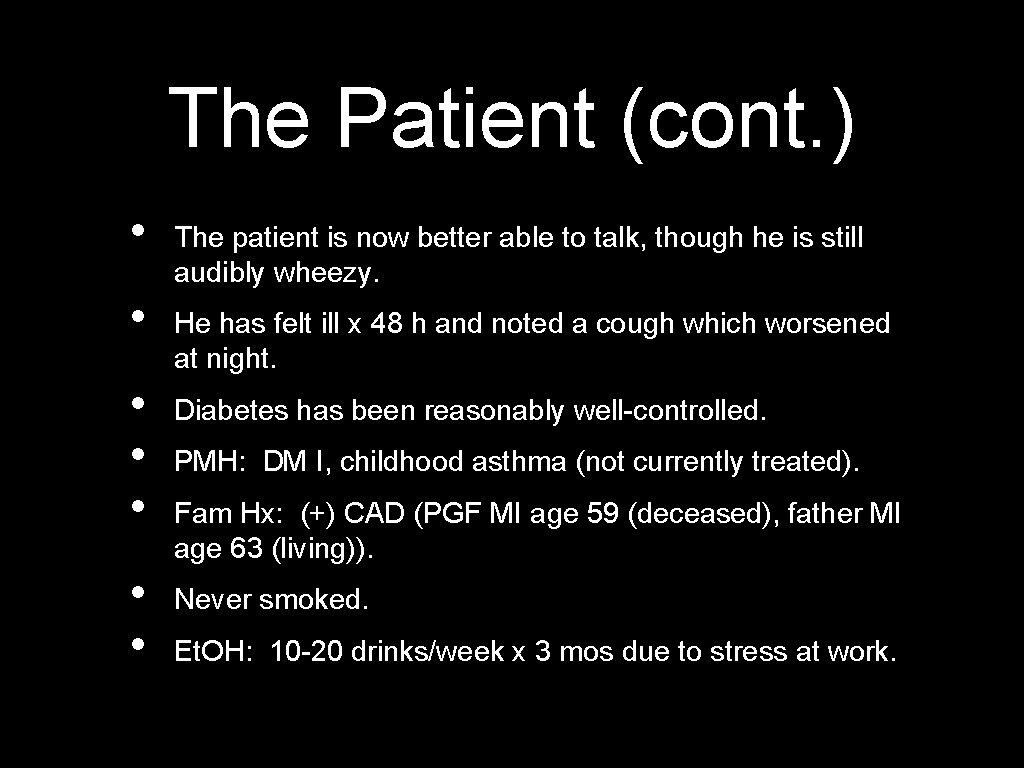
The Patient (cont. ) • • The patient is now better able to talk, though he is still audibly wheezy. He has felt ill x 48 h and noted a cough which worsened at night. Diabetes has been reasonably well-controlled. PMH: DM I, childhood asthma (not currently treated). Fam Hx: (+) CAD (PGF MI age 59 (deceased), father MI age 63 (living)). Never smoked. Et. OH: 10 -20 drinks/week x 3 mos due to stress at work.
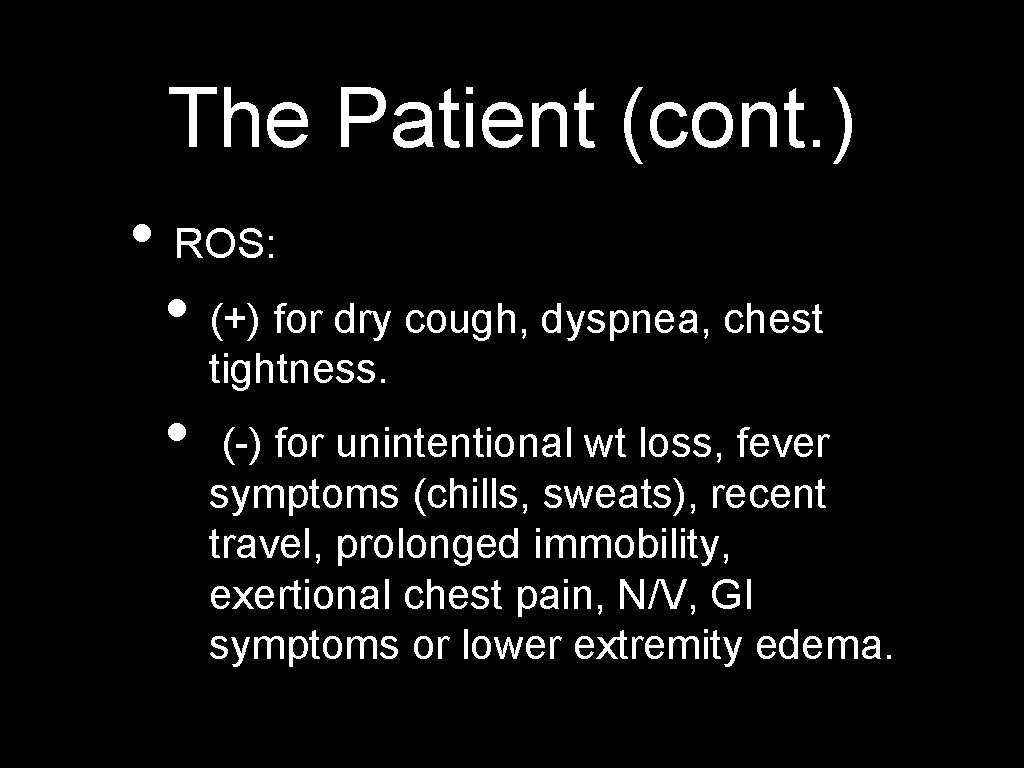
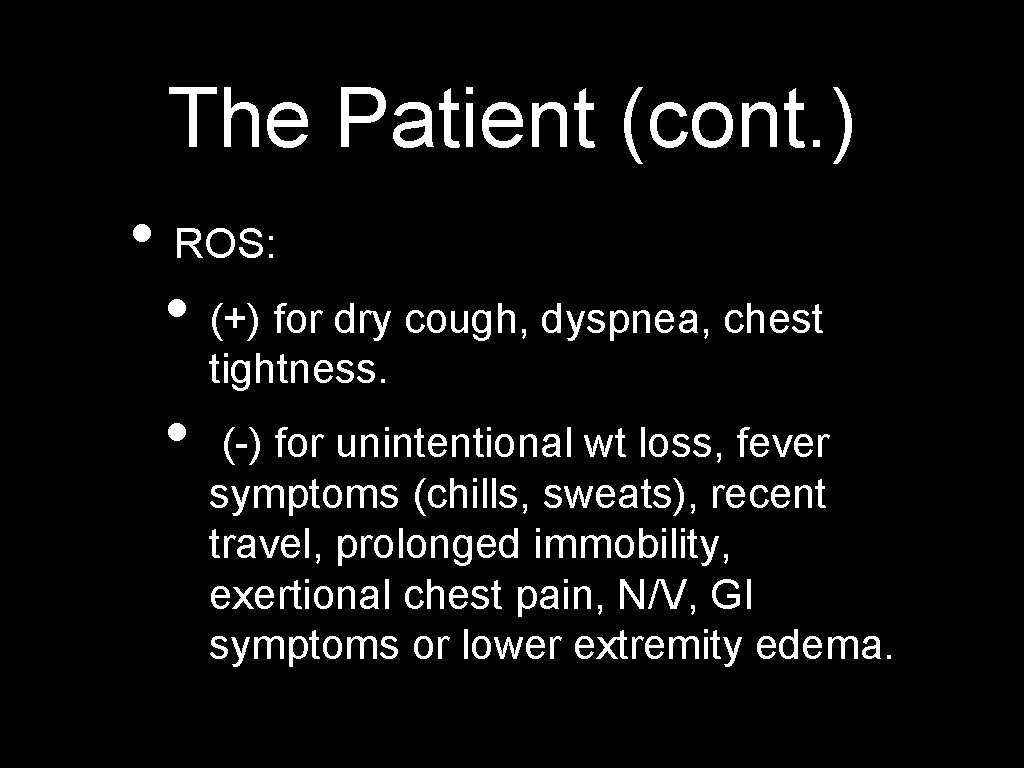
The Patient (cont. ) • ROS: • (+) for dry cough, dyspnea, chest tightness. • (-) for unintentional wt loss, fever symptoms (chills, sweats), recent travel, prolonged immobility, exertional chest pain, N/V, GI symptoms or lower extremity edema.
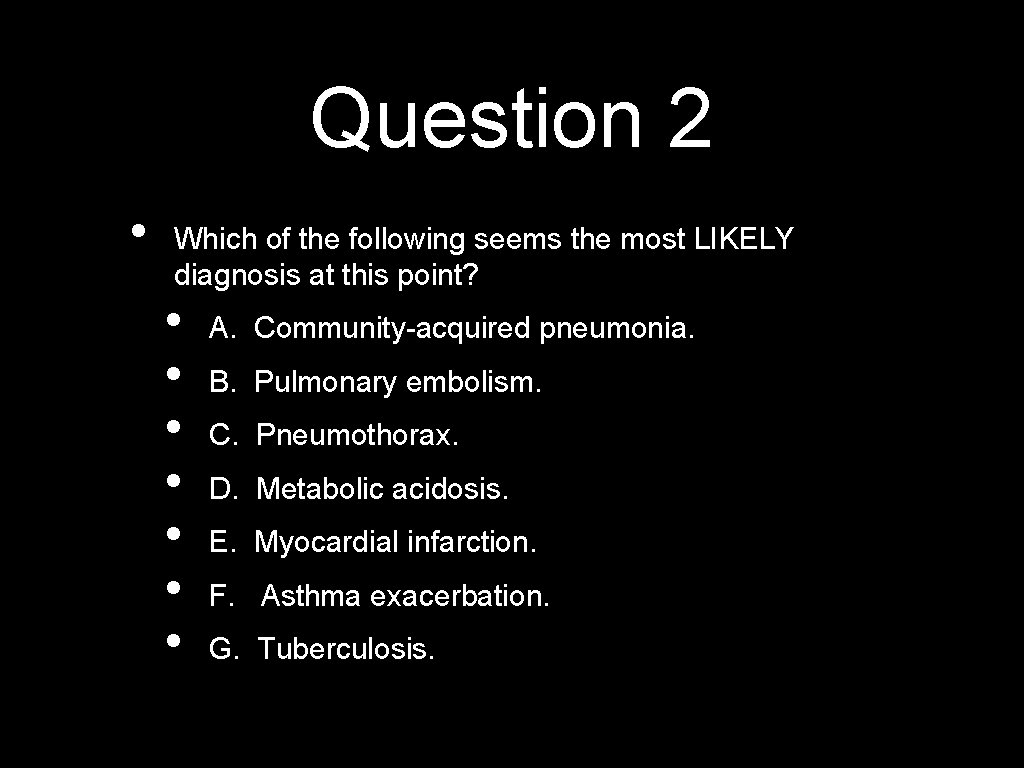
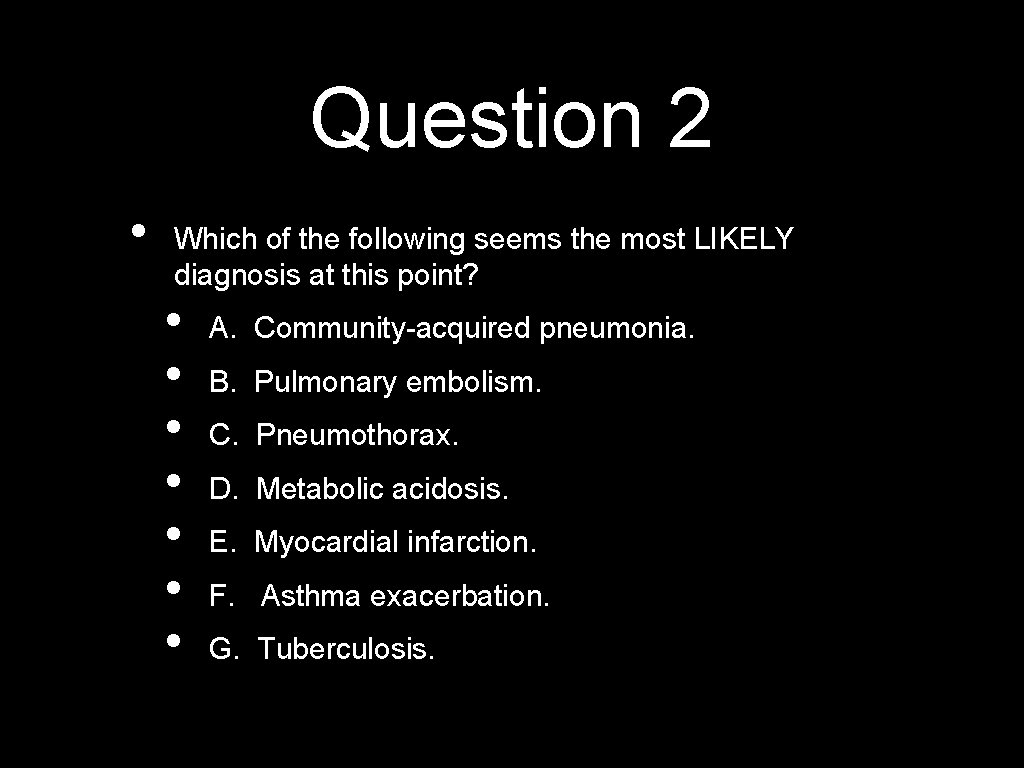
Question 2 • Which of the following seems the most LIKELY diagnosis at this point? • • A. Community-acquired pneumonia. B. Pulmonary embolism. C. Pneumothorax. D. Metabolic acidosis. E. Myocardial infarction. F. Asthma exacerbation. G. Tuberculosis.

Question 3 • Which of the following seems the most URGENT diagnosis to consider? • • A. Community-acquired pneumonia. B. Pulmonary embolism. C. Pneumothorax. D. Metabolic acidosis. E. Myocardial infarction. F. Asthma exacerbation. G. Tuberculosis.
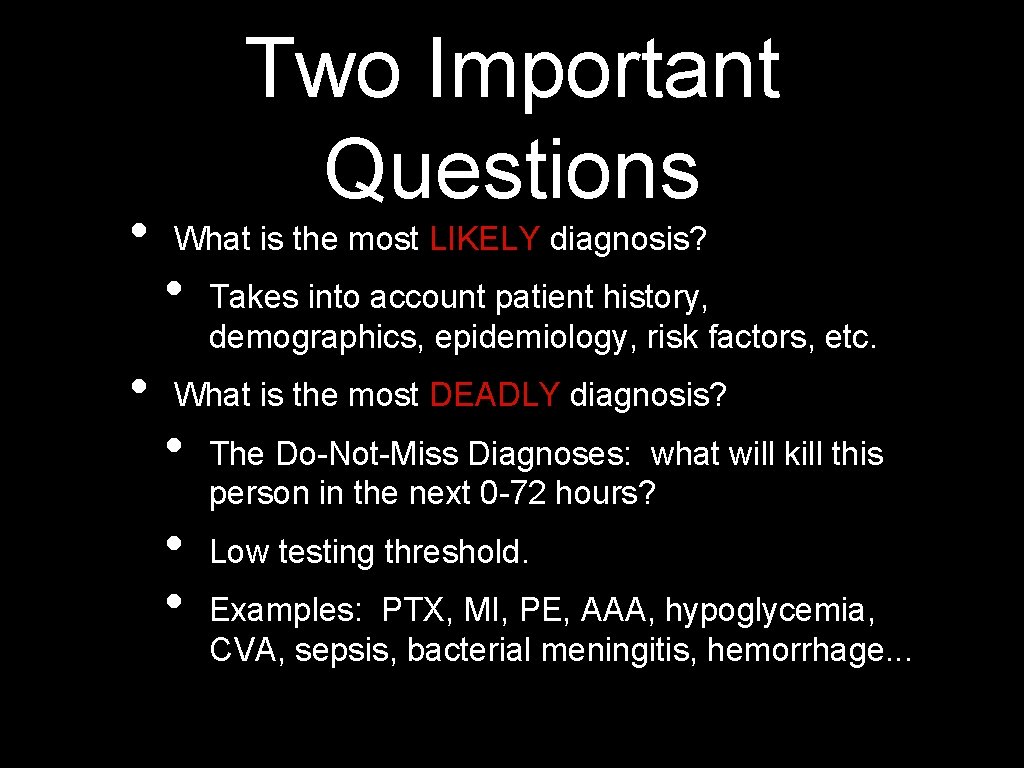
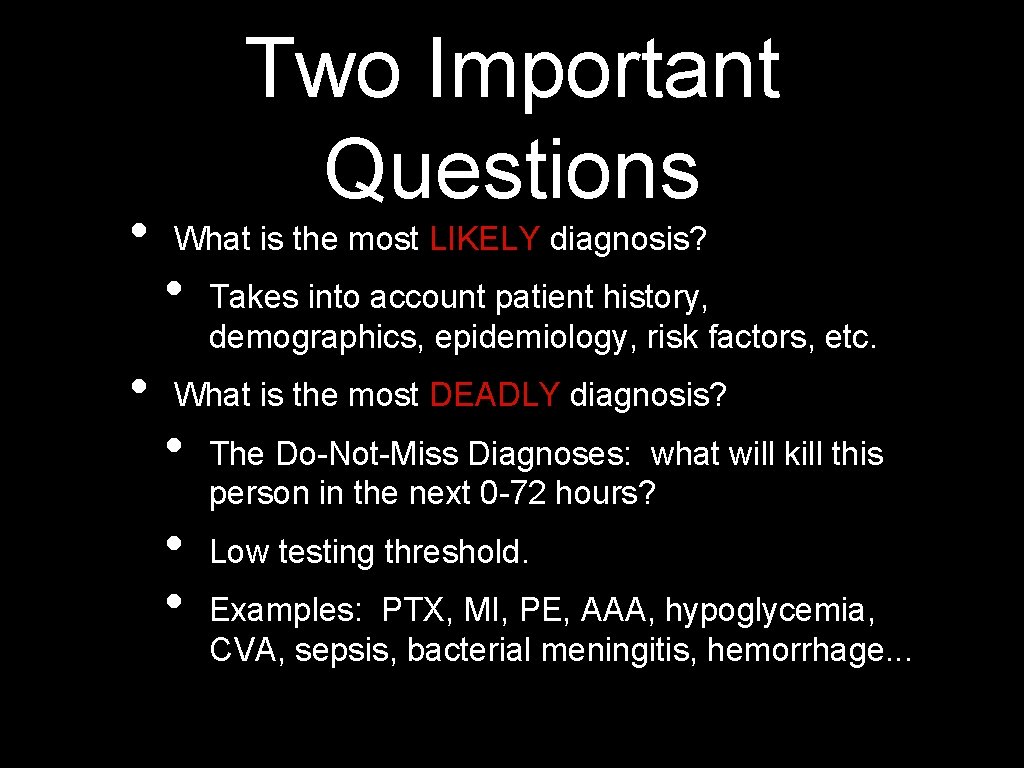
• • Two Important Questions What is the most LIKELY diagnosis? • Takes into account patient history, demographics, epidemiology, risk factors, etc. What is the most DEADLY diagnosis? • • • The Do-Not-Miss Diagnoses: what will kill this person in the next 0 -72 hours? Low testing threshold. Examples: PTX, MI, PE, AAA, hypoglycemia, CVA, sepsis, bacterial meningitis, hemorrhage. . .

The Patient (cont. ) • Physical Examination: • • T 37. 1 C P 95 R 40 BP 152/90 Sa. O 2 97% 10 L NRB GEN: pale, clammy, sweaty, cool to touch. Neck: trachea midline, no JVD Heart: difficult to hear due to wheezing Chest: diffuse wheezing, no crackles, no dullness to percussion, equal breath sounds bilaterally Abdomen: benign, no pulsatile abdominal masses, no cirrhotic stigmata Extremities: no edema, clubbing or cyanosis
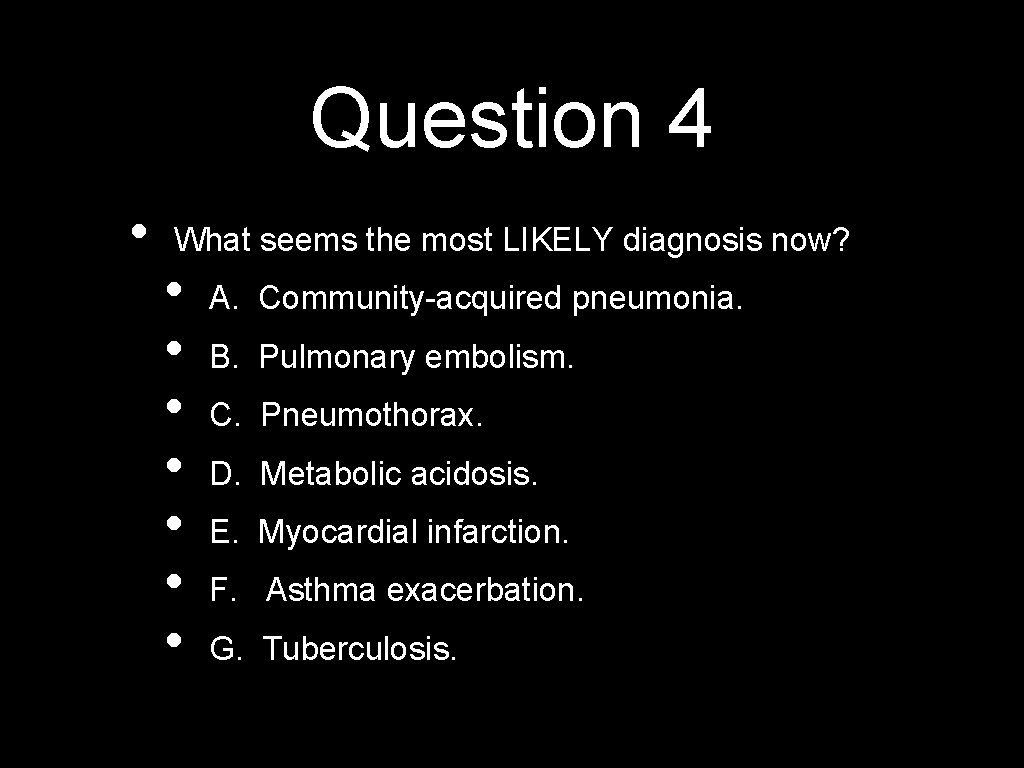
Question 4 • What seems the most LIKELY diagnosis now? • • A. Community-acquired pneumonia. B. Pulmonary embolism. C. Pneumothorax. D. Metabolic acidosis. E. Myocardial infarction. F. Asthma exacerbation. G. Tuberculosis.
Question 5 • Which of the following labs or studies would be most helpful now? • • • A. Arterial blood gas. B. EKG and troponins. C. CXR PA/lateral D. BNP (brain natriuretic peptide) F. All of the above. G. None of the above.
The Patient (cont. ) • You pick all of the above, and… • ABG: p. H 7. 50 / p. CO 2 20 / HCO 3 15 / p. O 2 110 • Troponins: 1. 6 ng/m. L (<0. 4) • BNP: 1300 pg/m. L (<100)
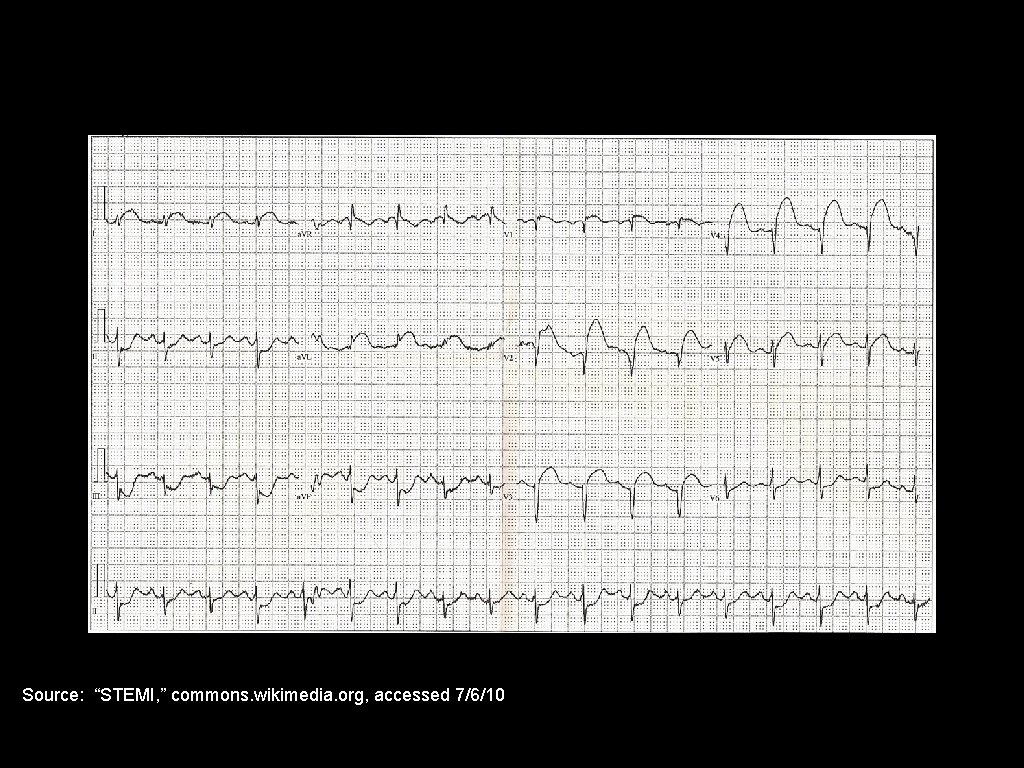
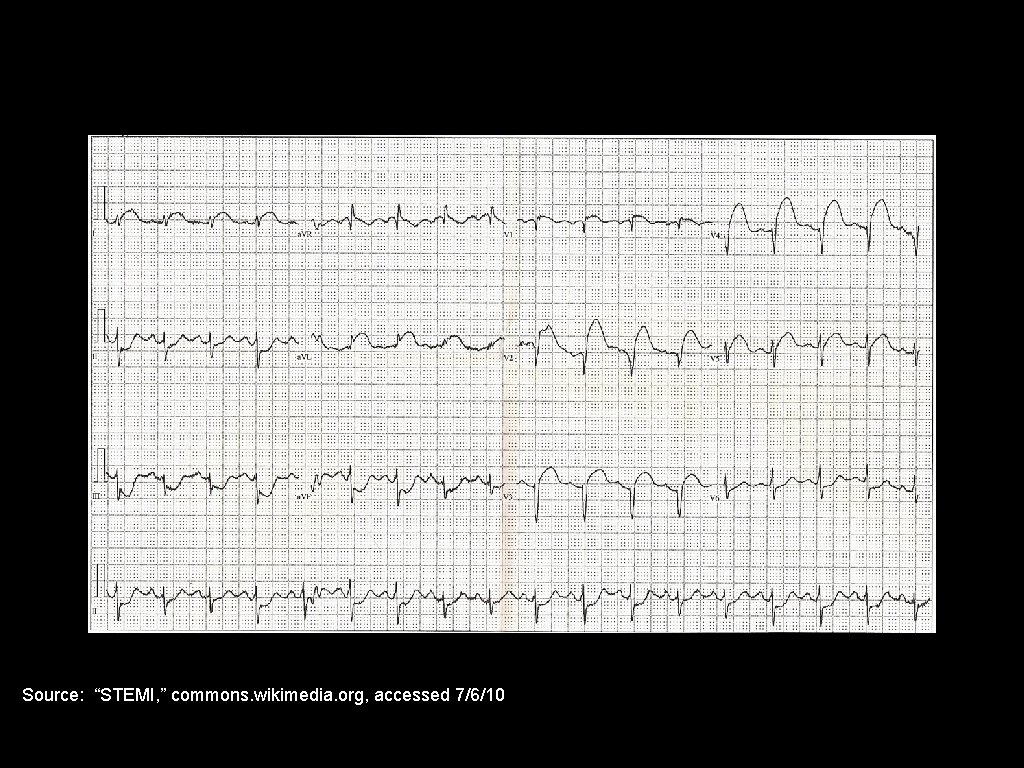
Source: “STEMI, ” commons. wikimedia. org, accessed 7/6/10

Source, Up. To. Date, accessed 7/6/10.
Question 6 • What is your final diagnosis? • • • A. Community-acquired pneumonia. B. Pulmonary embolism. C. Pulmonary edema due to LV dysfunction. D. Pneumothorax from ruptured bleb. E. Asthma exacerbation.
Dyspnea • The subjective feeling of being “short of breath” or “winded, ” an increased awareness of one’s own breathing. • Not a synonym for “chest tightness, ” though it can be concurrent. • Dyspnea is what you feel after running a sprint.
Tachypnea • • The objective finding of an increased respiratory rate: >19 breaths/min. In studies of young, healthy men - mean resting RR was 13/min in the AM, 15/min after lunch, never >19/min. However, RR > 20 often seen in elderly NH patients without other active disease, probably due to position, kyphosis, decreased vital capacity. Nevertheless, EVERYONE in the hospital seems to have either RR 12 or RR 22! Rarely an odd number.
Bradypnea • RR < 8/min • Usually only seen in intoxicated or narcotized patients.
Orthopnea • Dyspnea that occurs or worsens in the recumbent position. • From Greek “orthos” (upright) and “pneo” (breathing). • Although 95% of orthopnea is due to cardiac disease, it can be observed in lung disease, since sitting upright improves vital capacity and lung compliance.

Platypnea • • Dyspnea that occurs or worsens with an upright posture. From Greek “platus” (flat) and “pneo” (breathing). Often associated with orthodeoxia - Hb desaturation upon sitting upright. DDx: R-to-L shunt - multiple PE, pleural effusions, cirrhosis, AV malformations, intracardiac R-to-L shunt (eg, ASD).
Trepopnea • • • Dyspnea that occurs or worsens in the prone or the supine position. Patient breathes best with the good lung down. From Greek “trepo” (twisted) and “pneo” (breathing). Putting the good lung in dependent position improves blood flow and lessens V/Q mismatch (eg, massive unilateral effusion, endobronchial obstruction).
• • • Respiratory Failure Any situation in which the cardiopulmonary system cannot maintain OXYGENATION and/or VENTILATION to meet the needs of the tissues. Oxygenation: measured by end-organ function (eg, mental status), Sa. O 2 monitor and ABG. Ventilation: measured by end-organ function, ETCO 2 monitor and ABG (or VBG).
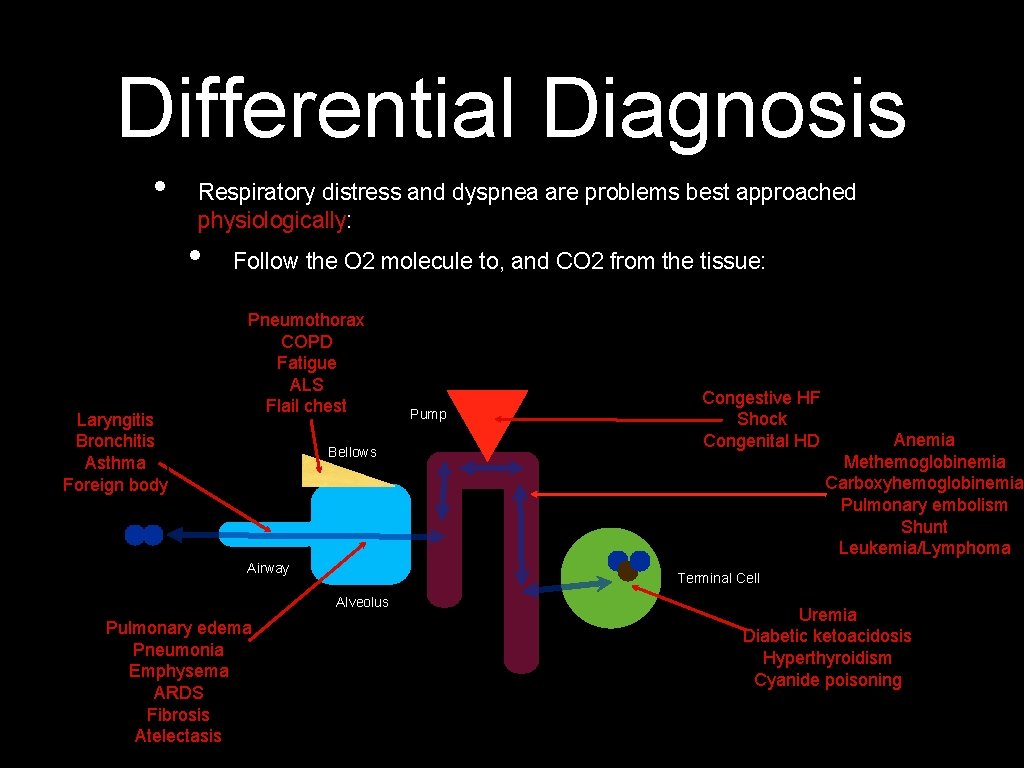
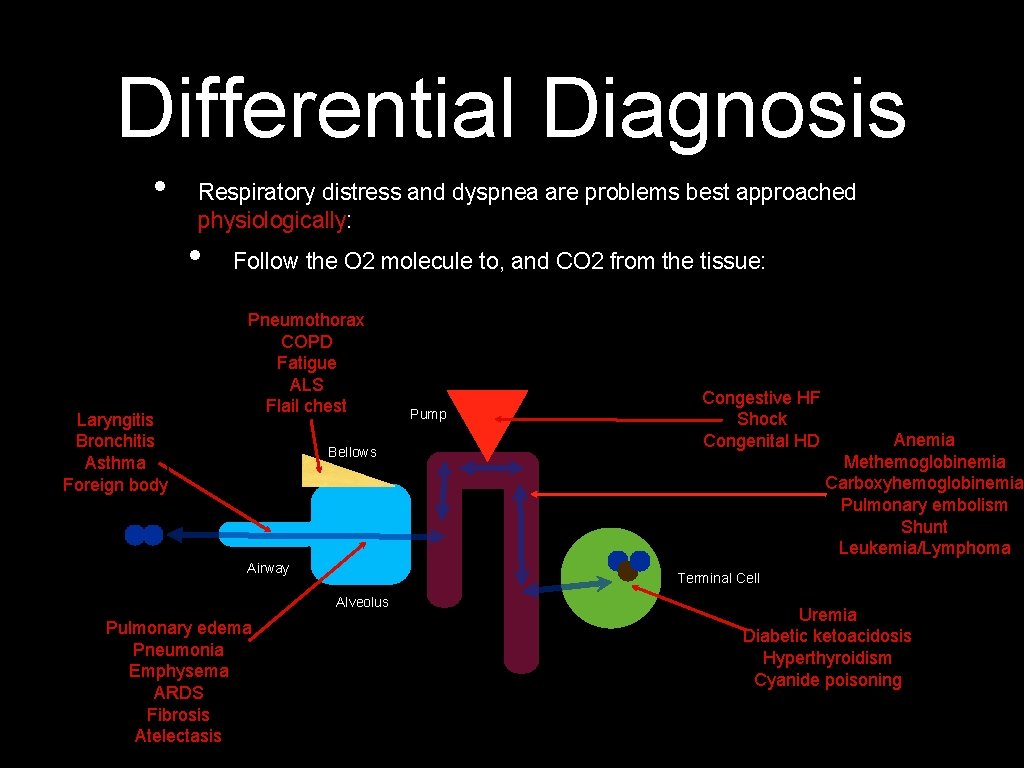
Differential Diagnosis • Respiratory distress and dyspnea are problems best approached physiologically: • Laryngitis Bronchitis Asthma Foreign body Follow the O 2 molecule to, and CO 2 from the tissue: Pneumothorax COPD Fatigue ALS Flail chest Bellows Airway Anemia Methemoglobinemia Carboxyhemoglobinemia Pulmonary embolism Shunt Leukemia/Lymphoma Terminal Cell Alveolus Pulmonary edema Pneumonia Emphysema ARDS Fibrosis Atelectasis Pump Congestive HF Shock Congenital HD Uremia Diabetic ketoacidosis Hyperthyroidism Cyanide poisoning
Pitfalls in Respiratory Distress • Pitfall 1: Relying on a normal physical exam to exclude disease. • • • Ex: sensitivity of auscultation for PTX is only 50 -84% (remember Sn. NOut). Ex: physical exam findings for PNA have sensitivity of 47 -69%, specificity of 58 -75%. NOTE: Positive findings ARE suggestive, just don’t depend on negative findings for “rule out. ” Pitfalls adapted from “Emergency Medicine: Avoiding the Pitfalls and Improving the Outcomes, ” Amal Mattu and Deepi Goyal, eds. , Blackwell, 2007.
Pitfalls in Respiratory Distress • Pitfall 2: Over-reliance on normal pulse ox measurement. • • • Pulse ox tells you ONLY about hypoxia but nothing about ventilatory or CO 2 status! This pitfall becomes more dangerous when patients are on supplemental O 2. Patients can die with O 2 sats of 94 -96% while p. H is 6. 65 and Pa. CO 2 of 265! (Reported in Mayo Clin Proc 1998; 73(1): 51 -54. )
Pitfalls in Respiratory Distress • Pitfall 3: Mistaking dyspnea for anxiety. • Remember: the elderly experiencing an MI are more likely to have dyspnea, dizziness, nausea, syncope and psychiatric symptoms! • Even crazy people get PEs, PTX, pneumonia, and so on.
Pitfalls in Respiratory Distress • Pitfall 4: Not considering PE in your differential diagnosis. • • • The most important step in making a diagnosis of PE is to consider it. Dyspnea is the most common symptom of PE. Use the Wells Criteria! (www. mdcalc. com/wells-criteria-forpulmonary-embolism-pe)
Pitfalls in Respiratory Distress • Pitfall 5: Relying on a normal CXR to rule out cardiopulmonary disease. • In patients with unexplained dyspnea, a normal CXR should increase your suspicion for PE!
Pitfalls in Respiratory Distress • Pitfall 6: Under- or over-administration of O 2 in COPD patients. • • • Yes, excessive O 2 will decrease the minute ventilation in end-stage COPD. However--hypoxia is a greater threat that hypercarbia to these patients (who have chronic, compensated respiratory acidosis). Aim for a Sa. O 2 90% or greater and a Pa. O 2 of 60 -70 mm. Hg. Higher values add no benefit.
Pitfalls in Respiratory Distress • Pitfall 7: Failing to consider NIPPV (CPAP/Bi. PAP) as an alternative to ETT intubation. • • Strongest data is in COPD exacerbations. Increasing data in hypoxic respiratory failure, cardiogenic pulmonary edema, pneumonia and asthma. NOT suitable if patient needs emergent intubation! The earlier NIPPV used, the better. Give it only 1 -2 hours to work and monitor closely.
Take Home Points • • O 2, IV, monitor and the ABCs. Fix the deranged physiology as you find it. Start with a NRB - simplifies your intubation decision. Think physiologically - follow the O 2 and CO 2. Think about likely, but don’t forget URGENT possibilities: PE, pulm edema and PTX, especially. Pulse ox only measures oxygenation, not ventilation. Don’t be too reassured by normal physical exam and X-ray findings.
Thanks for Listening!
 Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Respiratory distress nasal flaring
Respiratory distress nasal flaring Protective reflexes
Protective reflexes Respiratory zone
Respiratory zone Georgia simmons barclays
Georgia simmons barclays Kristi fischer
Kristi fischer Epoxidacion de alquenos
Epoxidacion de alquenos Debora simmons
Debora simmons Kristi fischer
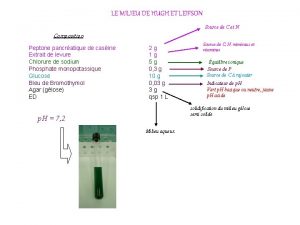
Kristi fischer épreuve de hugh et leifson
épreuve de hugh et leifson Reid simmons
Reid simmons Aarc simmons
Aarc simmons Kristi simmons
Kristi simmons Simmons
Simmons Shelby simmons parents
Shelby simmons parents Dee simmons young
Dee simmons young Roper vs simmons case
Roper vs simmons case Chris simmons md
Chris simmons md Baines simmons jobs
Baines simmons jobs Laurie simmons walking house
Laurie simmons walking house University of akron financial aid office
University of akron financial aid office Dr shannon simmons
Dr shannon simmons Dr chris walton
Dr chris walton Oyez roper v simmons
Oyez roper v simmons Polimerizacion cationica del isobutileno
Polimerizacion cationica del isobutileno Emma v simmons
Emma v simmons Andrew chapman simmons
Andrew chapman simmons Gabriel simmons
Gabriel simmons Write a short note on stress management
Write a short note on stress management Meconium grade 1 2 3
Meconium grade 1 2 3 Financial distress costs
Financial distress costs Batasan dan ruang lingkup psikologi klinis
Batasan dan ruang lingkup psikologi klinis Crisis survival kit dbt
Crisis survival kit dbt Nursing management of fetal distress
Nursing management of fetal distress Moral distress and burnout
Moral distress and burnout Konsep spiritual dalam keperawatan
Konsep spiritual dalam keperawatan The damsel in distress archetype
The damsel in distress archetype