ACUTE RENAL FAILURE Kidneys are the pair organs























- Slides: 71
ACUTE RENAL FAILURE
• Kidneys are the pair organs located in the retroperitoneum (at the level of 12 -th rib in the loin region). Their main function is elimination of the metabolic waists from the organism. They are supplied with blood by paired renal arteries, which are direct arterial branches of abdominal aorta. • Nephron is the basic functional unit of the kidneys. Its structure is quite complicated: it consists of renal corpuscle (Bowman-Shumlanski’s capsule and glomerulus), proximal convoluted tubule, loop of Henle, distal convoluted tubule and direct tubule. •
• Kidneys are exclusively “hard-working” organ. Their total weigh is hardly 0, 4% of the total body weight, however they receive 25 % of cardiac output. 10% of total inhaled oxygen are used for their metabolic needs. During the day nearly 150 liters of primary urine are ultrafiltrated out of the blood. Ultrafiltration is possible only when effective filtration pressure is not less than 12 mm Hg. It is defined as a difference between hydrostatic (47 mm Hg), oncotic (25 mm Hg) and intracapsular pressure (10 mm Hg). • EFP=Hp(47)-Op(25)-ICp(10)= 12 mm Hg • So when hydrostatic pressure (mean arterial pressure) is decreasing or when intracapsular pressure is reaching critical values filtration stops and renal failure appears.
• In tubules water, electrolytes and glucose are reabsorbed and metabolic wastes are secreted to the urine. Eventually during one day only 1 % of primary urine is evacuated from the organism in the form of secondary urine with high concentration of toxic substances. • Kidneys participate in haematopoiesis, regulation of fluid balance, electrolytes metabolism and acid-base balance. • Kidneys are also organs of secretion: their parenchyma produces rennin – substance very important for vascular tone regulation. • 6. 2 Etiology and pathogenesis of acute renal failure (acute kidney injury). • Acute kidney injury is a syndrome appearing due to sudden and progressive affection of nephrones, which causes violation of renal function and induces life-threatening homoeostasis disorders.
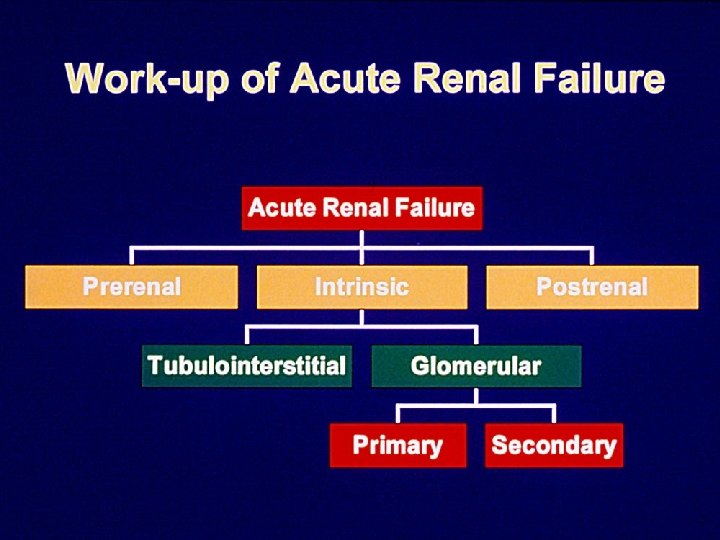
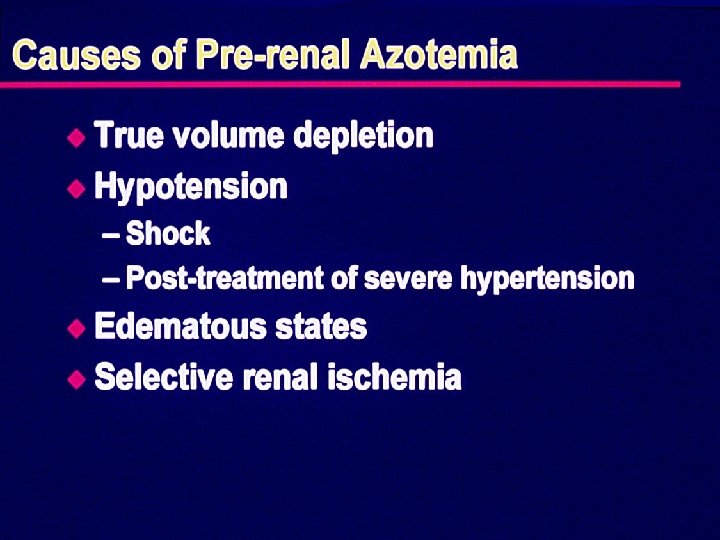
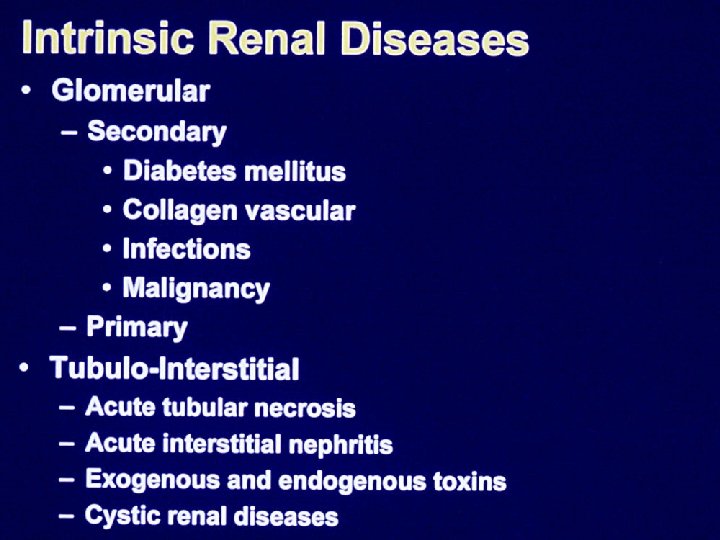
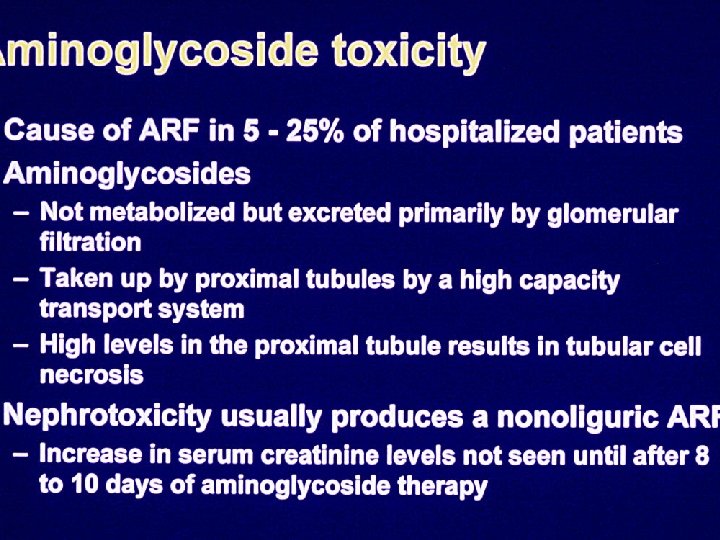
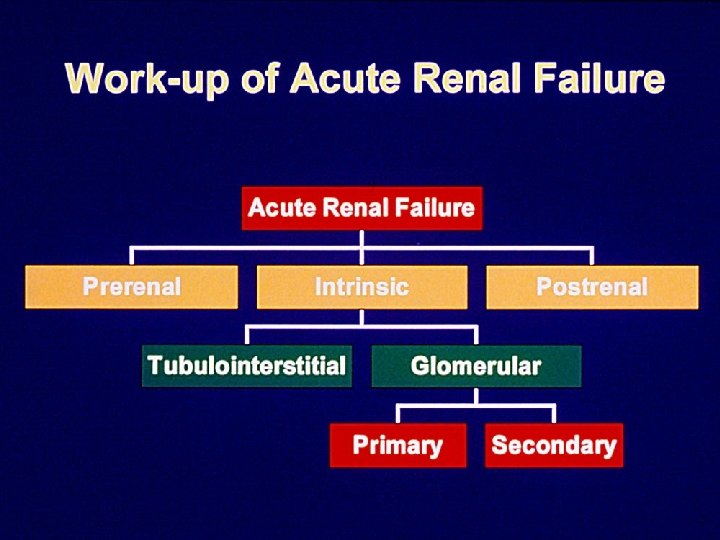
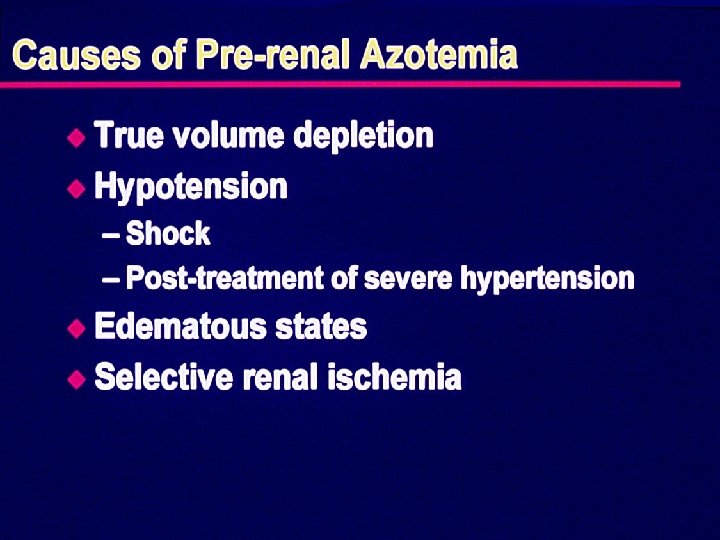
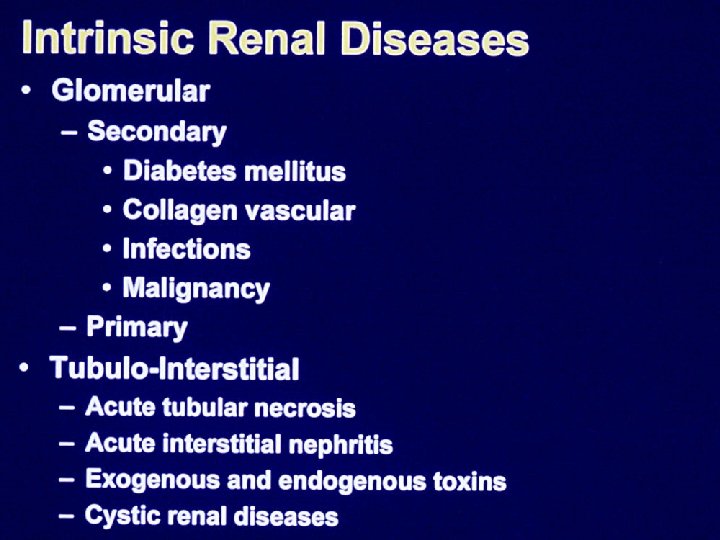
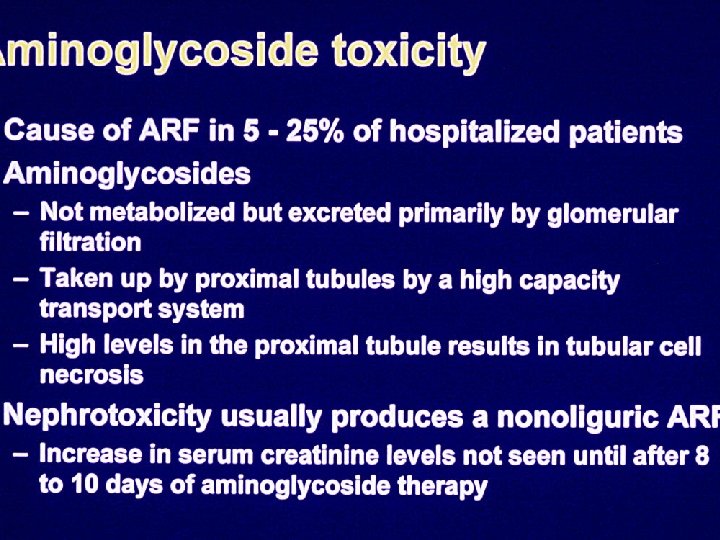
• The reasons of acute kidney injury are divided into 3 gorups: • 1. Prerenal: pathological conditions, which lower renal blood flow, such as hypovolemia, hypotension, thrombosis, renal artery embolism, renal artery spasm, haemolysis, myolysis (muscle desintegration). Thus the prerenal failure can be connected with the massive blood loss, shock (traumatic, anaphylactic, cardiac), dehydration (burns, pancreatitis, peritonitis, vomiting, diarrhoea), crush-syndrome, transfusion of incompatible blood, acute respiratory failure. • 2. Intrinsic: the primary damage is caused to the renal parenchyma by exogenous toxins (alcohol surrogates, acetic acid, ethylene glycol, heavy metal salts), nephrotoxic antibiotics (aminoglycosides), bacterial toxins (in case of sepsis), acute glomerulonephritis, eclampsia.
• 3. Postrenal: acute renal failure appears due to complications of urine outflow (tumours and calculi of renal pelvis and ureter, prostate, accidental ligation of the ureters during operation). • In 70% of the cases acute renal injury appears as a result of prerenal cause. In stress conditions (massive blood loss, multiple injuries) adrenals intensively produce catecholamines: arterioles of skin, smooth muscles, intestines and kidneys spasm. As you probably remember this helps to save the brain and heart (additional blood for circulating blood volume), however for the rest organs this situation, lasting over 3 -4 hours will bring ischemia and even necrosis.
• Another mechanism for acute renal failure is connected with the acute vascular insufficiency (collapse, endotoxicosis). Hydrostatic pressure decreases and thus filtration of the blood lowers. • The mechanism of this pathological process is next: hypoperfusion-renal ischemia-hypoxia-coagulation of blood in glomerular vessels-termination of plasma filtration-affection of tubules membranes- compression of the nephron and capillaries-renal necrosis. • Death of over 75% of nephrons finds its clinical manifestation in acute kidneys injury. All the functions of the kidneys- ultrafiltration, reabsorption, secretion, bioactive substances production – are violated.
• Clinically in acute kidneys injury we differentiate 5 stages: • I. First stage (initial) is the stage of shock: depends on the initial aggressive agent and duration of its influence. It can last several hours or several days (2 -3). Clinic also depends on the causing factor, however first of all you should observe carefully the haemodynamics and urine output, because correct evaluation of patient’s condition and proper treatment may prevent the development of next stages. • Warring symptoms are: • - arterial hypotension (systolic blood pressure less than 70 mm Hg if it stays during few hours); • - decrease of urine output; • - hyposthenuria (low specific gravity- less than 1006 -1008)
Background • Common in Hospitalized patients • Associated with high Morbidity and Mortality • Often Multifactorial • Identifiable risk factors.

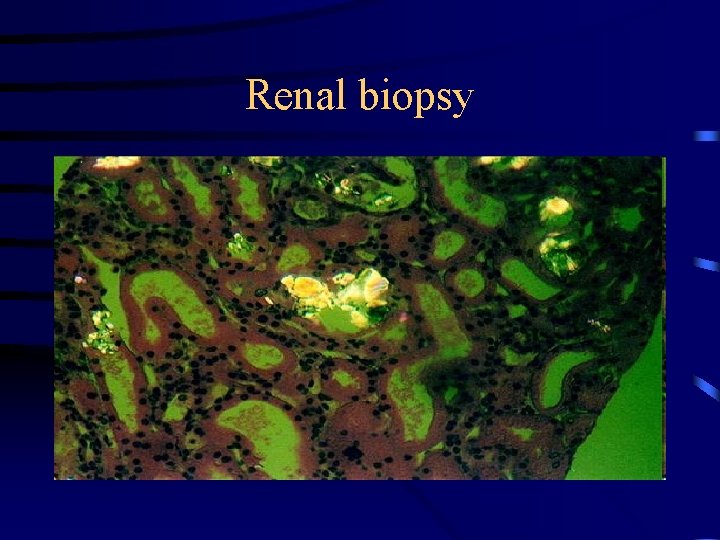
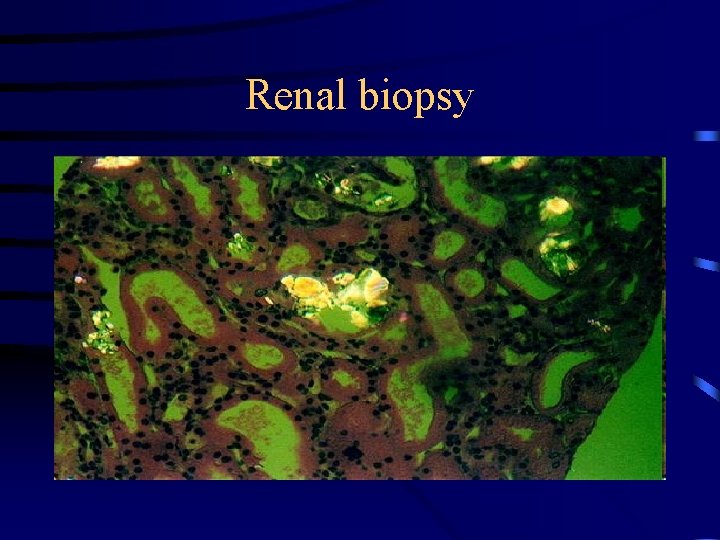
Renal biopsy
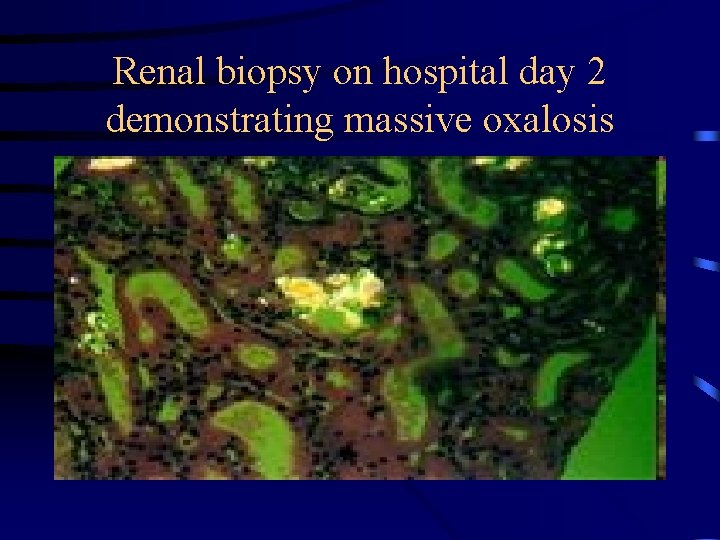
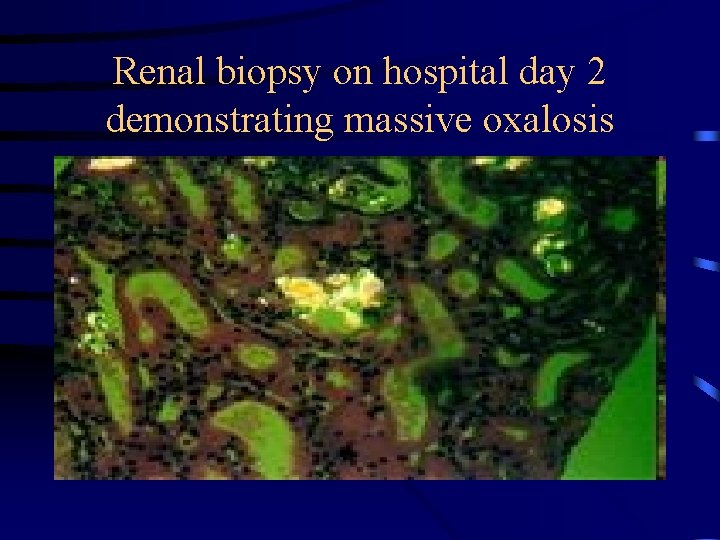
Renal biopsy on hospital day 2 demonstrating massive oxalosis
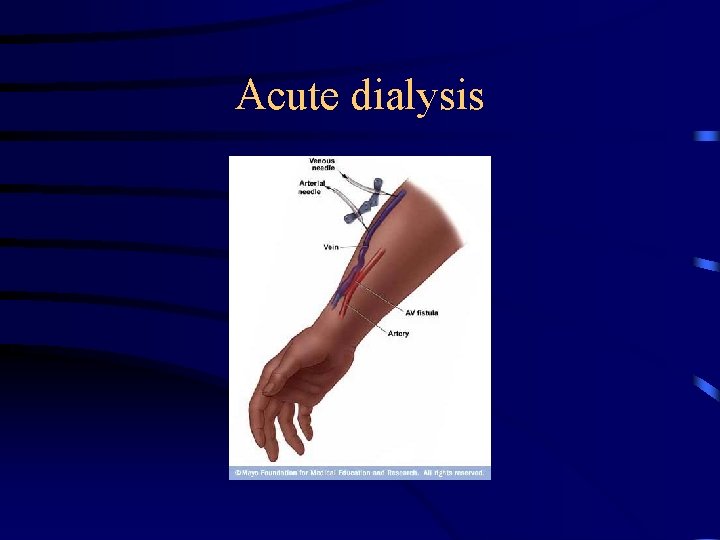
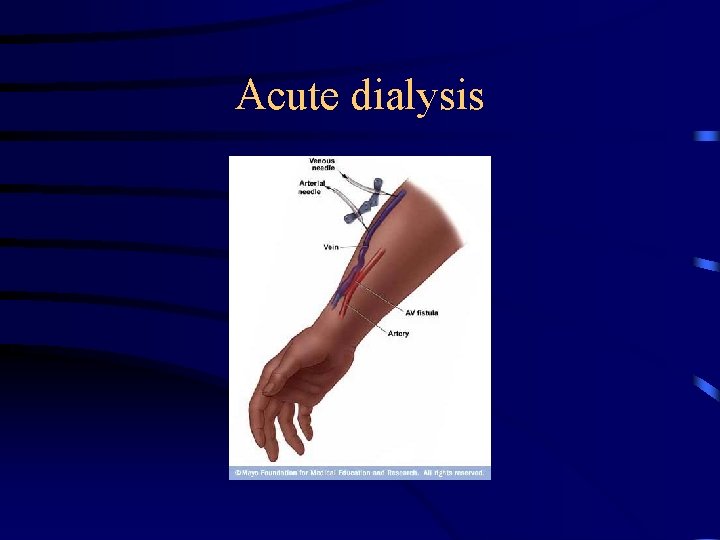
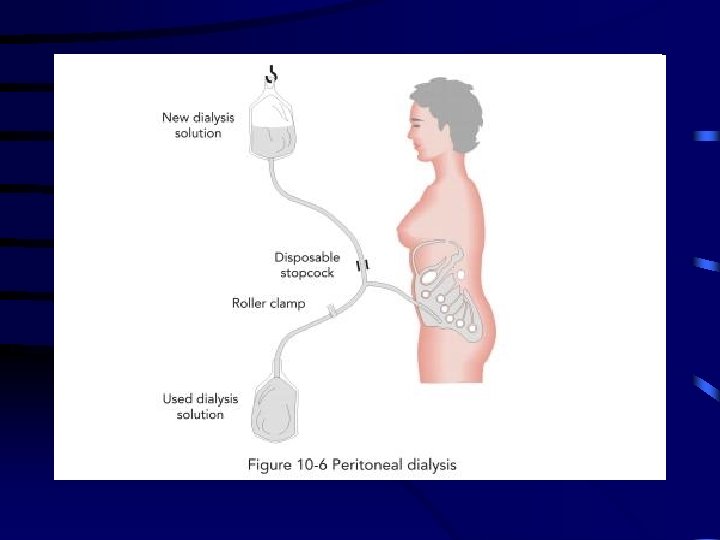
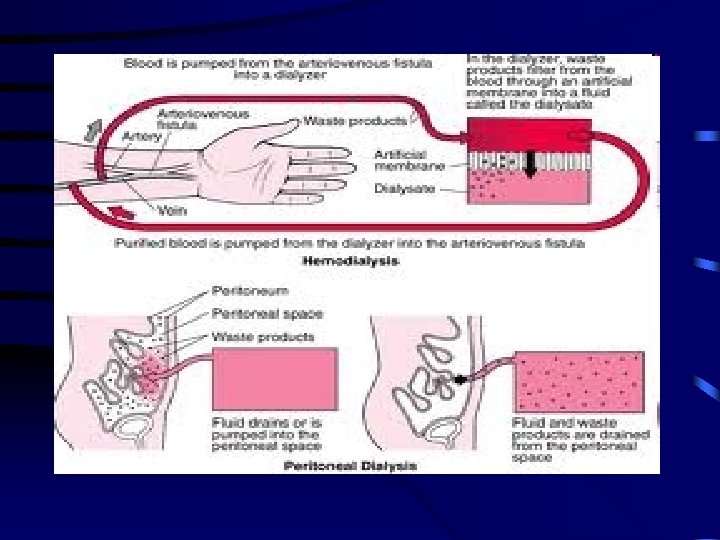
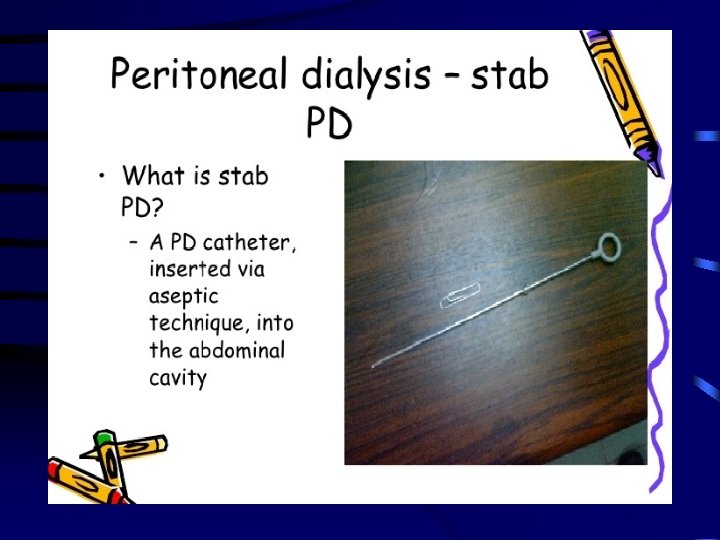
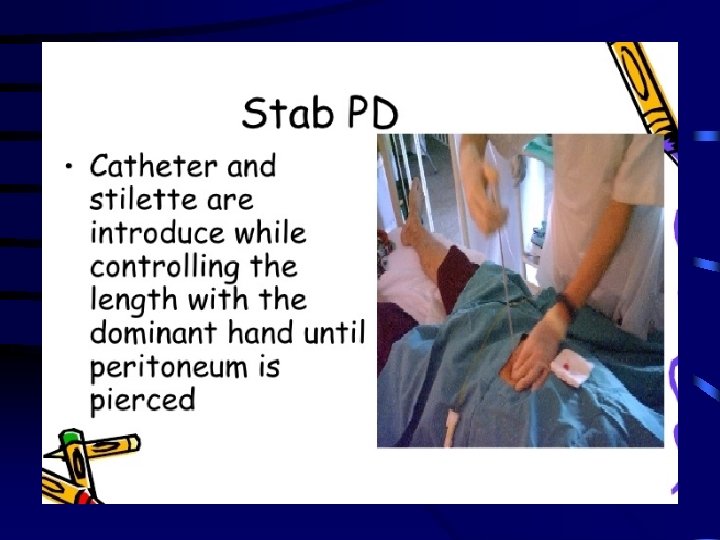
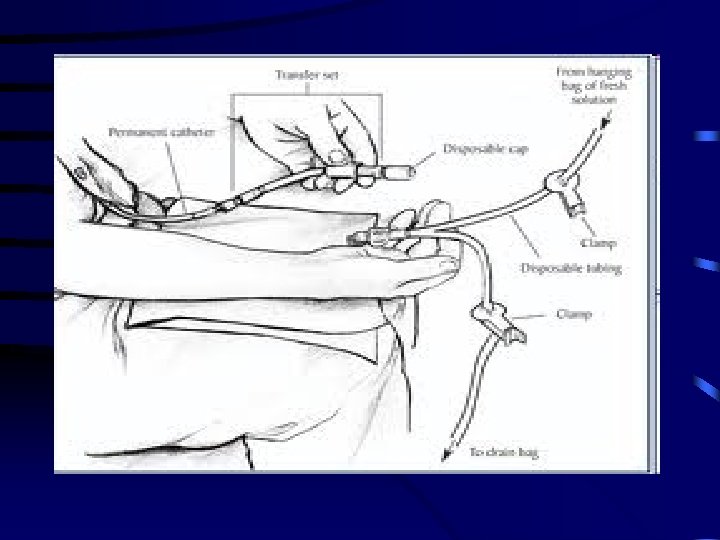
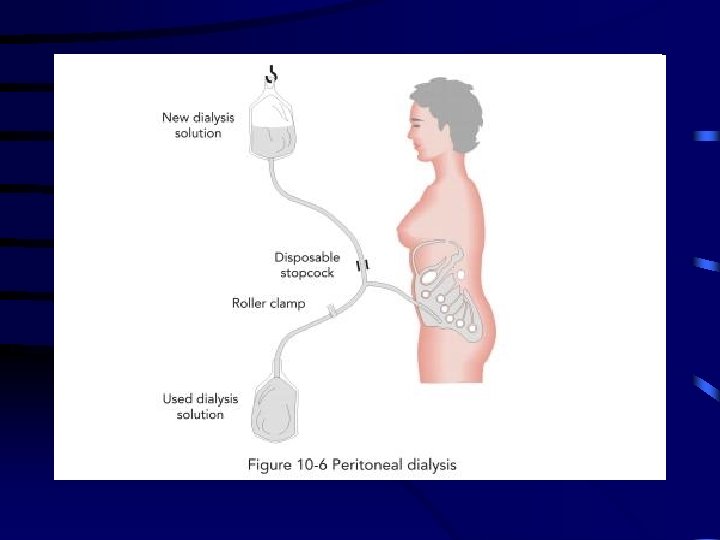
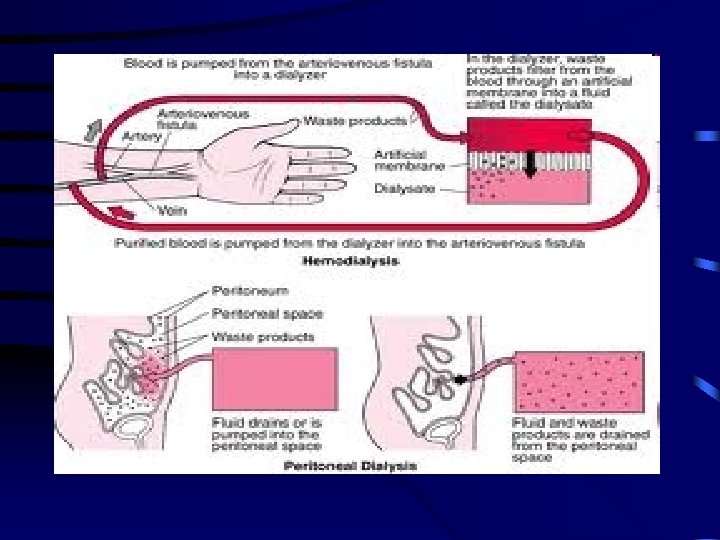
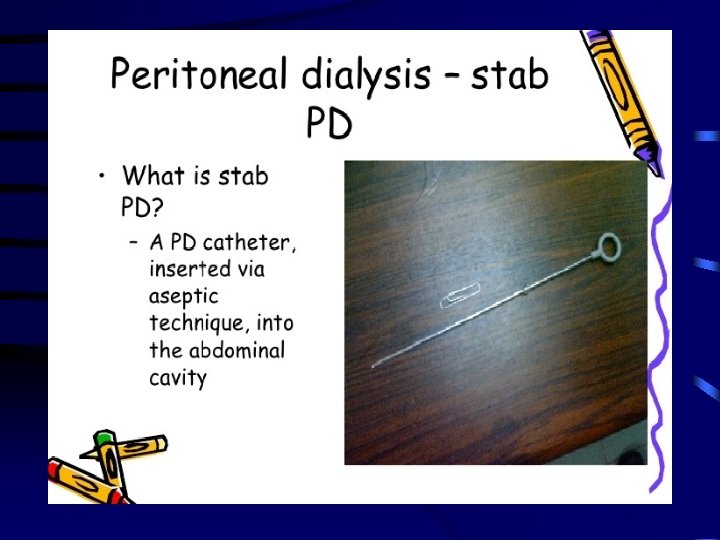
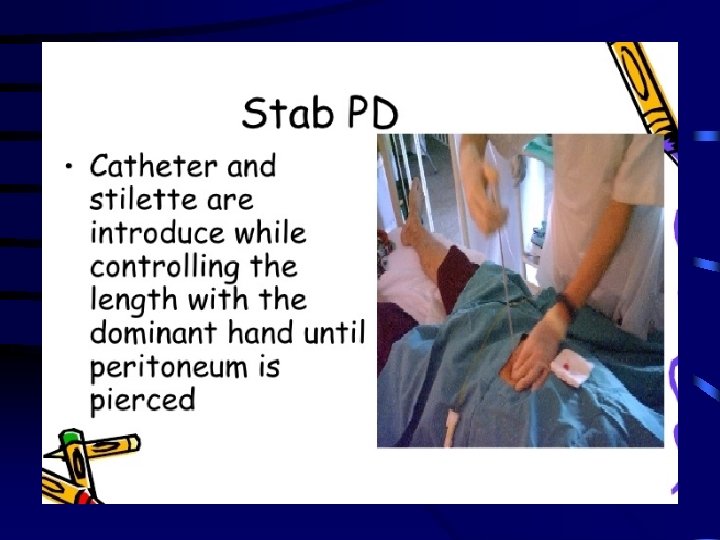
Acute dialysis




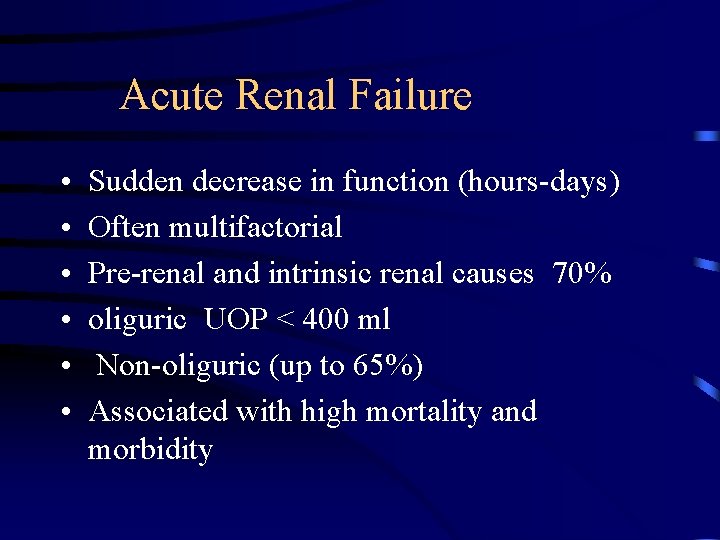
Acute Renal Failure • • • Sudden decrease in function (hours-days) Often multifactorial Pre-renal and intrinsic renal causes 70% oliguric UOP < 400 ml Non-oliguric (up to 65%) Associated with high mortality and morbidity

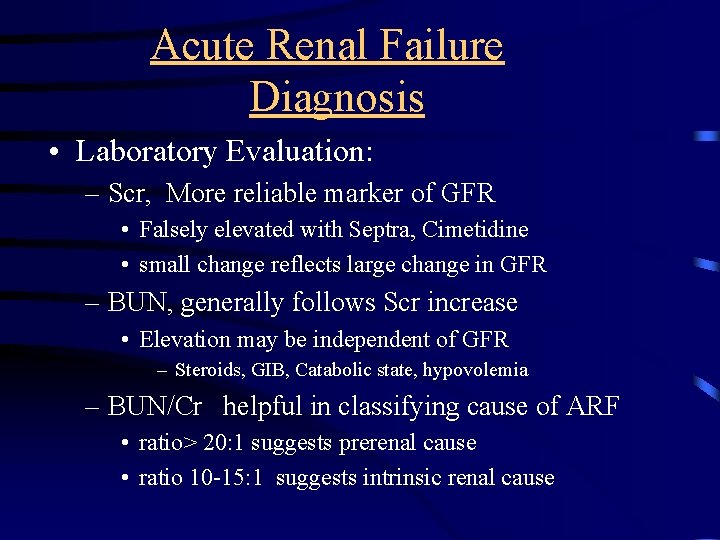
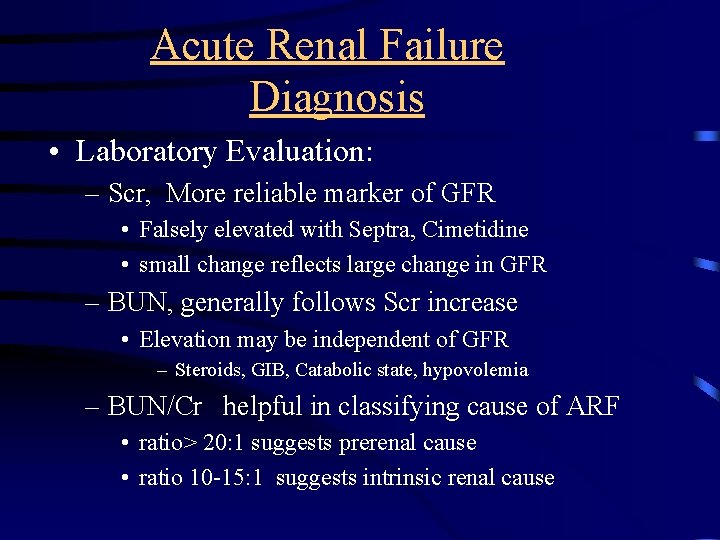
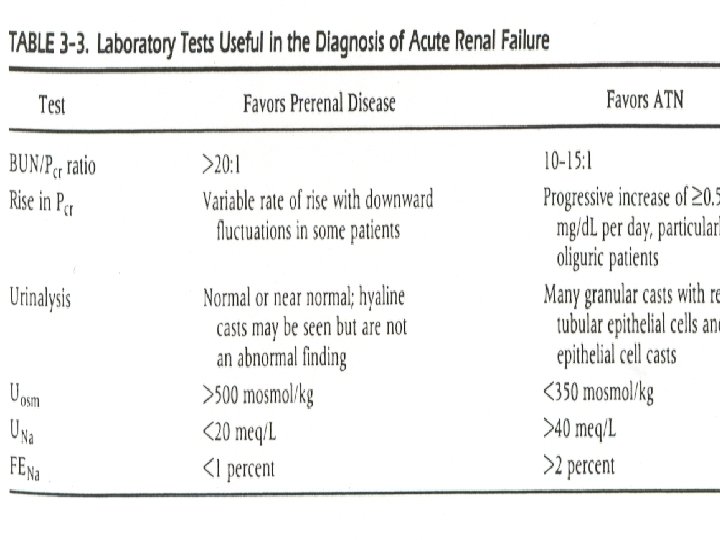
Acute Renal Failure Diagnosis • Laboratory Evaluation: – Scr, More reliable marker of GFR • Falsely elevated with Septra, Cimetidine • small change reflects large change in GFR – BUN, generally follows Scr increase • Elevation may be independent of GFR – Steroids, GIB, Catabolic state, hypovolemia – BUN/Cr helpful in classifying cause of ARF • ratio> 20: 1 suggests prerenal cause • ratio 10 -15: 1 suggests intrinsic renal cause











Acute Renal Failure Diagnosis (cont’d) • Urinalysis – Unremarkable in pre and post renal causes – Differentiates ATN vs. AIN. vs. AGN • Muddy brown casts in ATN • WBC casts in AIN – Hansel stain for Eosinophils
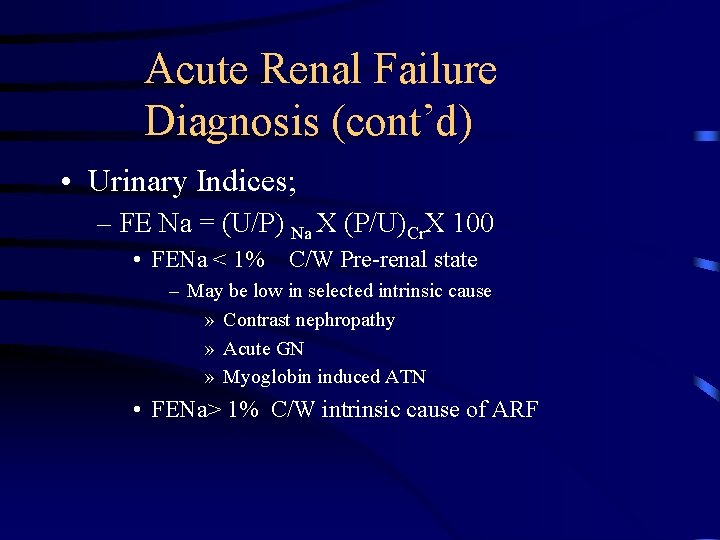
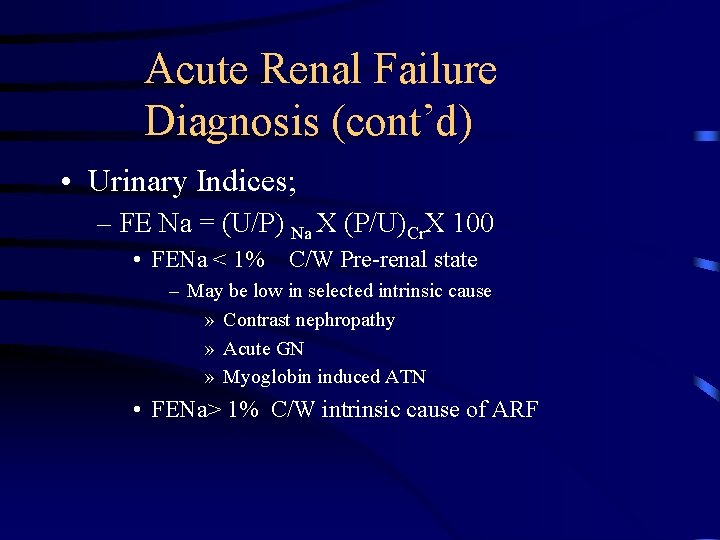
Acute Renal Failure Diagnosis (cont’d) • Urinary Indices; – FE Na = (U/P) Na X (P/U)Cr. X 100 • FENa < 1% C/W Pre-renal state – May be low in selected intrinsic cause » Contrast nephropathy » Acute GN » Myoglobin induced ATN • FENa> 1% C/W intrinsic cause of ARF



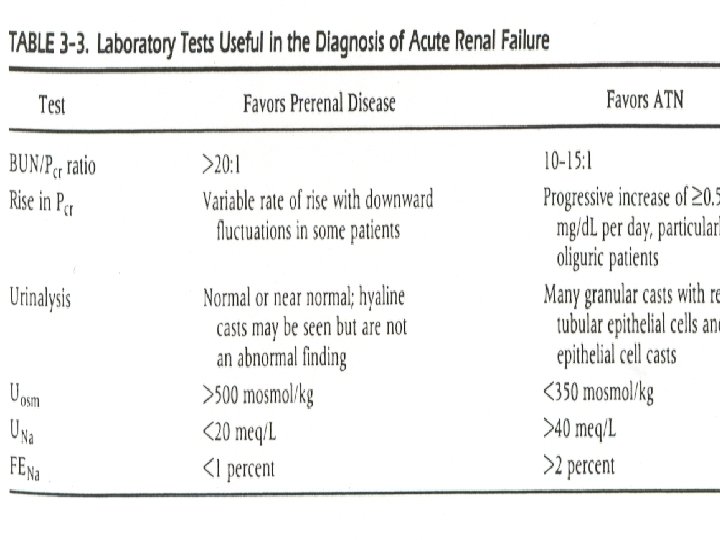
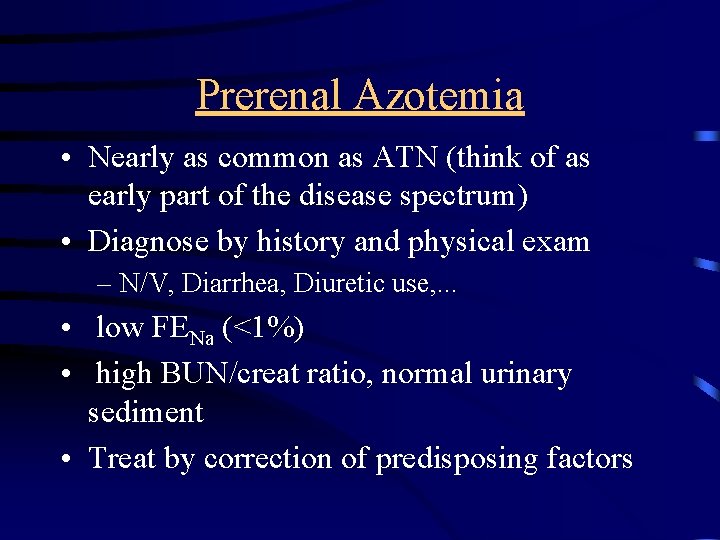
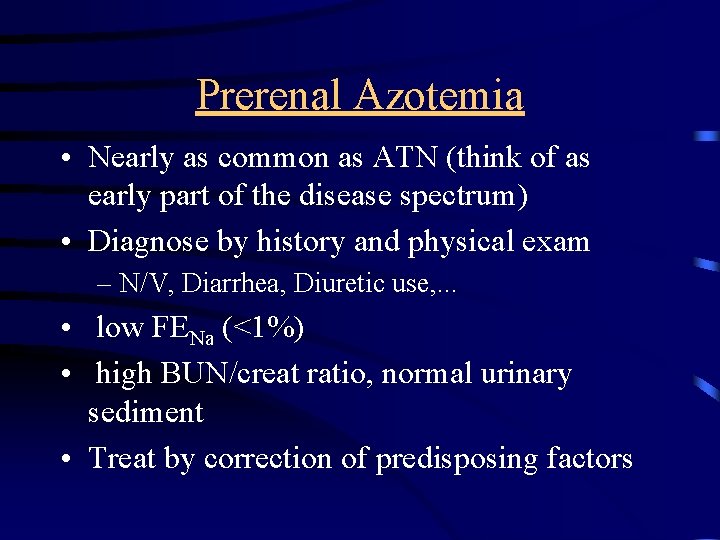
Prerenal Azotemia • Nearly as common as ATN (think of as early part of the disease spectrum) • Diagnose by history and physical exam – N/V, Diarrhea, Diuretic use, . . . • low FENa (<1%) • high BUN/creat ratio, normal urinary sediment • Treat by correction of predisposing factors

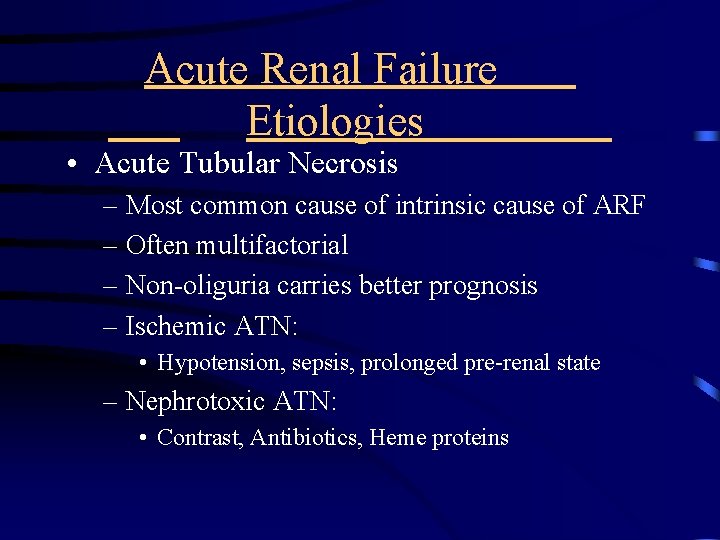
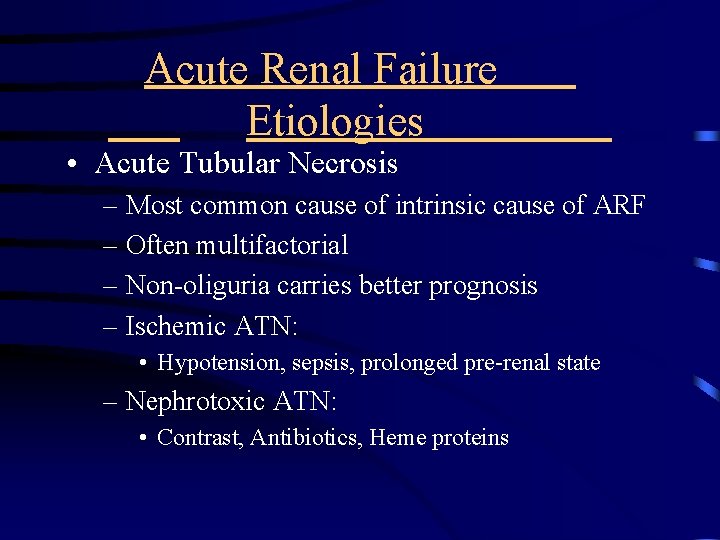
Acute Renal Failure Etiologies • Acute Tubular Necrosis – Most common cause of intrinsic cause of ARF – Often multifactorial – Non-oliguria carries better prognosis – Ischemic ATN: • Hypotension, sepsis, prolonged pre-renal state – Nephrotoxic ATN: • Contrast, Antibiotics, Heme proteins
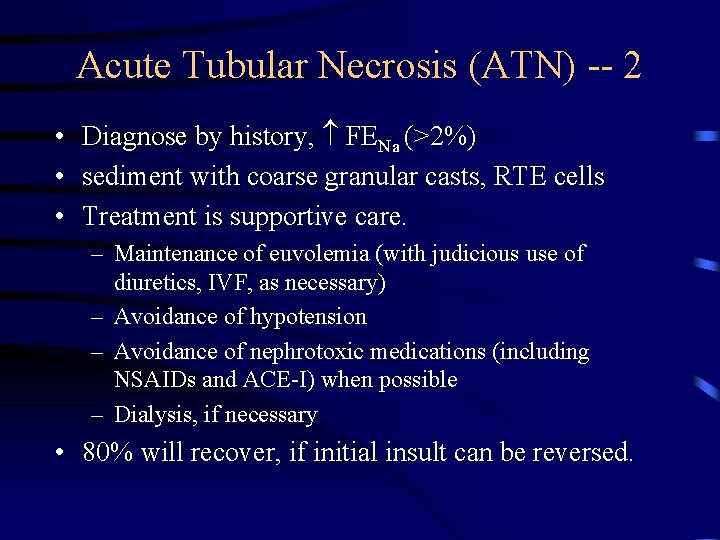
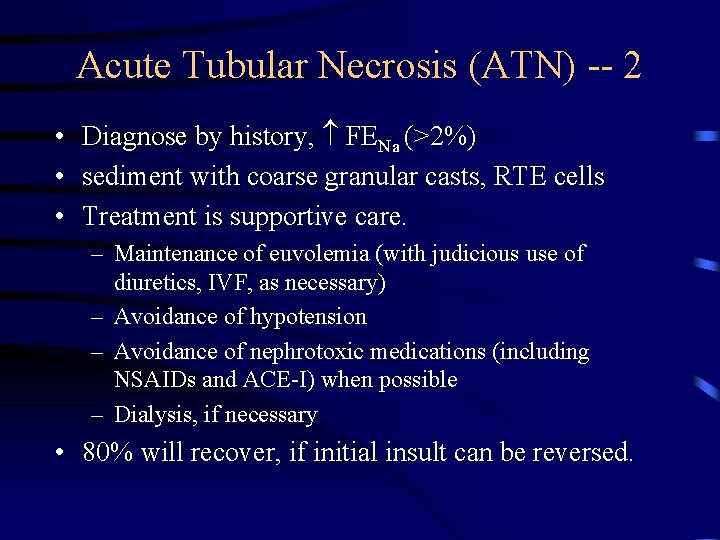
Acute Tubular Necrosis (ATN) -- 2 • Diagnose by history, FENa (>2%) • sediment with coarse granular casts, RTE cells • Treatment is supportive care. – Maintenance of euvolemia (with judicious use of diuretics, IVF, as necessary) – Avoidance of hypotension – Avoidance of nephrotoxic medications (including NSAIDs and ACE-I) when possible – Dialysis, if necessary • 80% will recover, if initial insult can be reversed.
Contrast nephropathy • 12 -24 hours post exposure, peaks in 3 -5 days • Non-oliguric, FE Na <1% !! • RX/Prevention: 1/2 NS 1 cc/kg/hr 12 hours pre/post • Mucomyst 600 BID pre/post (4 doses) • Risk Factors: CRF, Hypovolemia.
Rhabdomyolytic ARF • Diagnose with serum CPK (usu. > 10, 000), urine dipstick (+) for blood, without RBCs on microscopy, pigmented granular casts • Common after trauma (“crush injuries”), seizures, burns, limb ischemia occasionally after IABP or cardiopulmonary bypass • Treatment is largely supportive care. • Alkalinization of urine.

Acute Glomerulonephritis • Rare in the hospitalized patient • Most common types: acute post-infectious GN, “crescentic” RPGN • Diagnose by history, hematuria, RBC casts, proteinuria (usually non-nephrotic range), low serum complement in post-infectious GN), RPGN often associated with anti. GBM or ANCA • Usually will need to perform renal biopsy
Acute Glomerulonephritis (2) • If diagnosis is post-infectious, disease is usually self-limited, and supportive care is usually all that is necessary. • For RPGN, may need immunosuppressive therapy with steroids ± Cytoxan, plasmapheresis (if assoc. with anti-GBM)
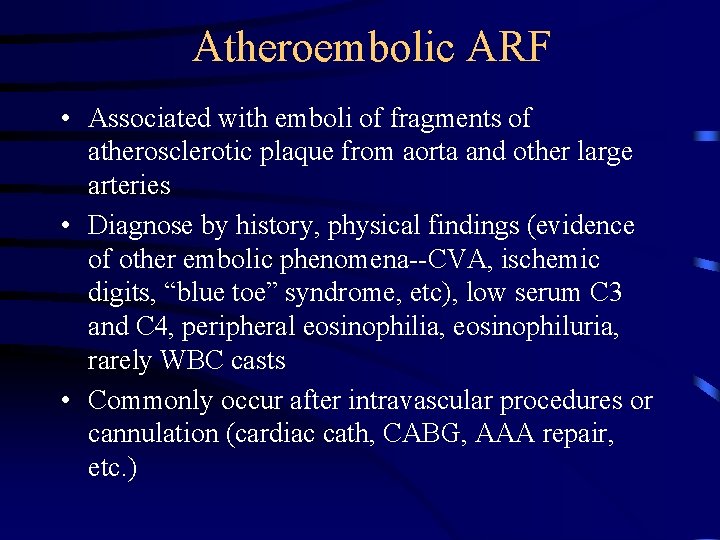
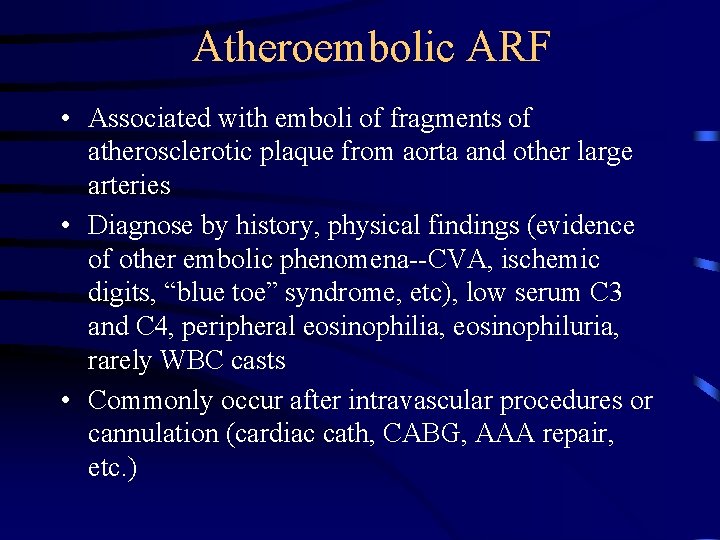
Atheroembolic ARF • Associated with emboli of fragments of atherosclerotic plaque from aorta and other large arteries • Diagnose by history, physical findings (evidence of other embolic phenomena--CVA, ischemic digits, “blue toe” syndrome, etc), low serum C 3 and C 4, peripheral eosinophilia, eosinophiluria, rarely WBC casts • Commonly occur after intravascular procedures or cannulation (cardiac cath, CABG, AAA repair, etc. )
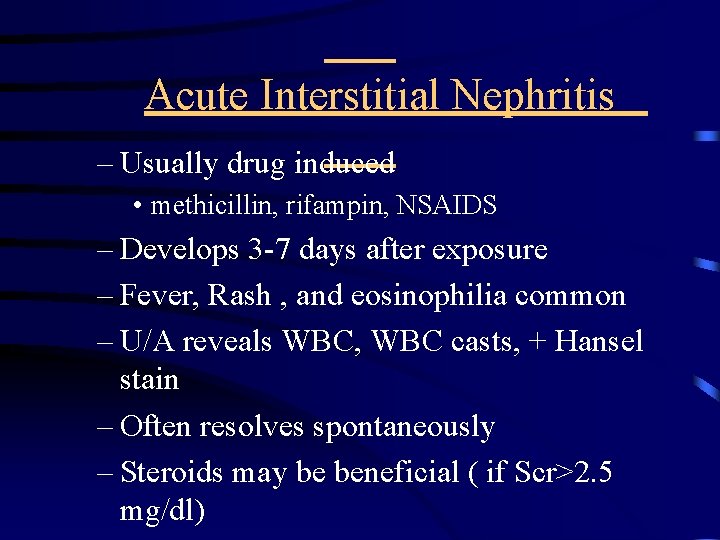
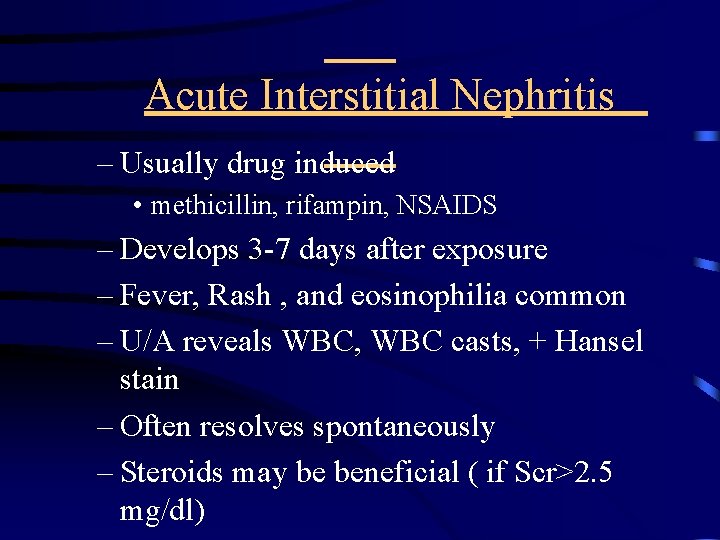
Acute Interstitial Nephritis – Usually drug induced • methicillin, rifampin, NSAIDS – Develops 3 -7 days after exposure – Fever, Rash , and eosinophilia common – U/A reveals WBC, WBC casts, + Hansel stain – Often resolves spontaneously – Steroids may be beneficial ( if Scr>2. 5 mg/dl)
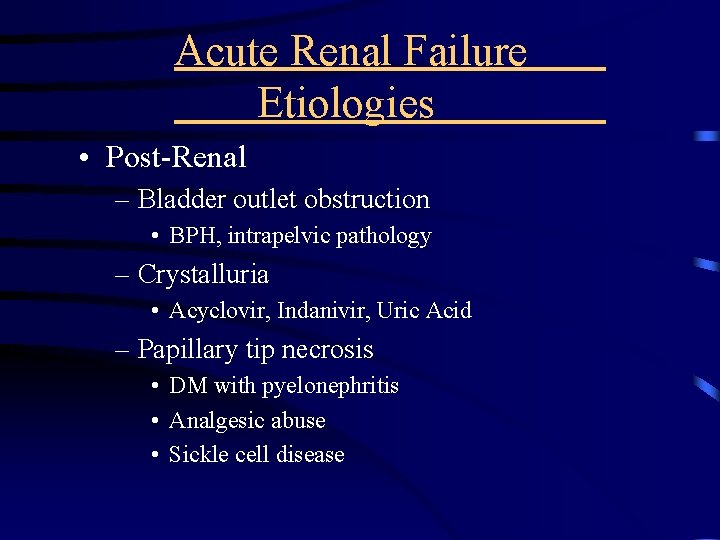
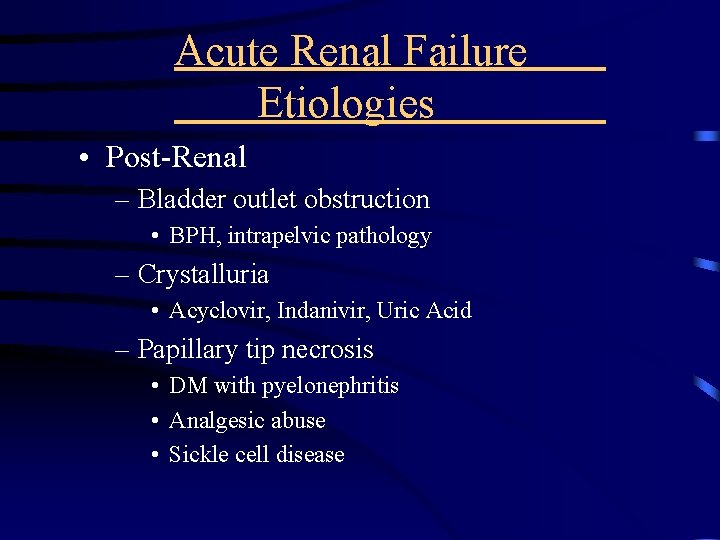
Acute Renal Failure Etiologies • Post-Renal – Bladder outlet obstruction • BPH, intrapelvic pathology – Crystalluria • Acyclovir, Indanivir, Uric Acid – Papillary tip necrosis • DM with pyelonephritis • Analgesic abuse • Sickle cell disease
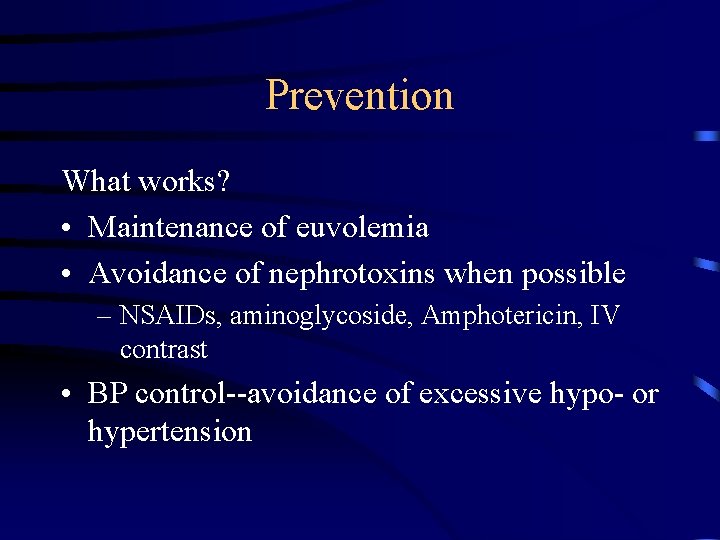
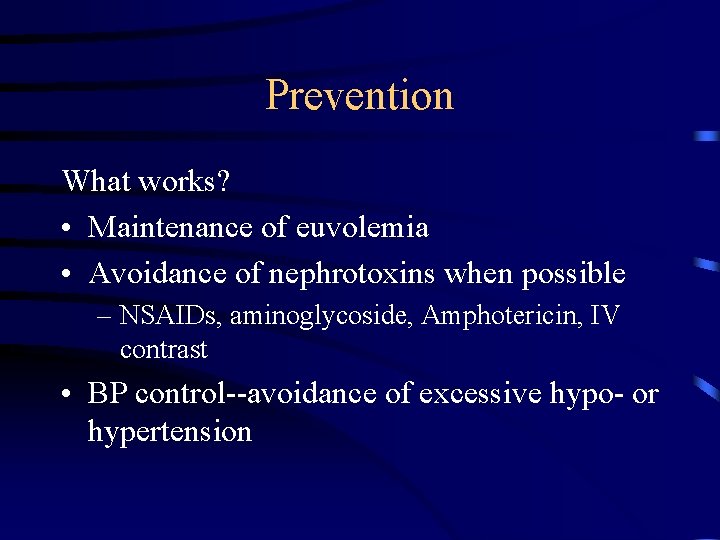
Prevention What works? • Maintenance of euvolemia • Avoidance of nephrotoxins when possible – NSAIDs, aminoglycoside, Amphotericin, IV contrast • BP control--avoidance of excessive hypo- or hypertension
Prevention What doesn’t work? • Empiric use of: – Diuretics (i. e. , Furosemide, Mannitol) – Dopamine (or Dopamine agonists such as Fenoldopam) – Calcium-channel blockers
Acute Renal Failure Treatment • • • Water and sodium restriction Protein restriction Potassium and phosphate restriction Adjust medication dosages Avoidance of further insults – BP support – Nephrotoxins
Hyperkalemia • Highly Arrhythmogenic – Usually with progressive EKG changes • Peaked T waves ---> Widened QRS--> Sinus wave – K> 5. 5 meq/L needs evaluation/intervention – Usually in setting of Decrease GFR but: • medication also a common cause – ACEI – NSAIDS – Septra, Heparin

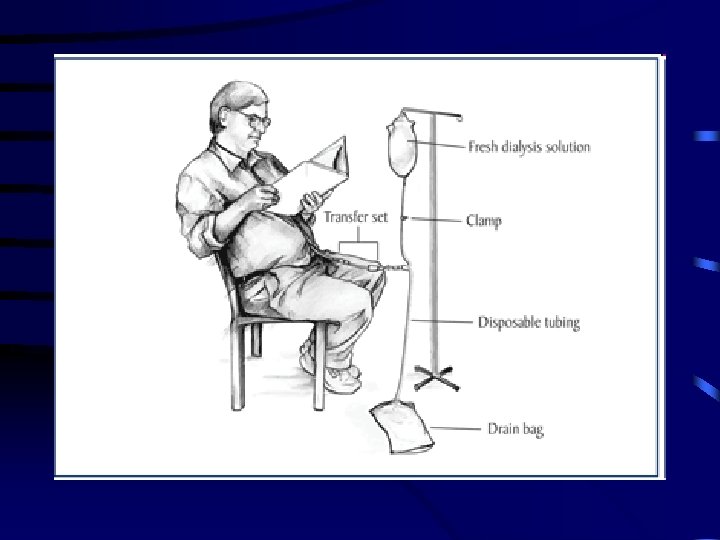
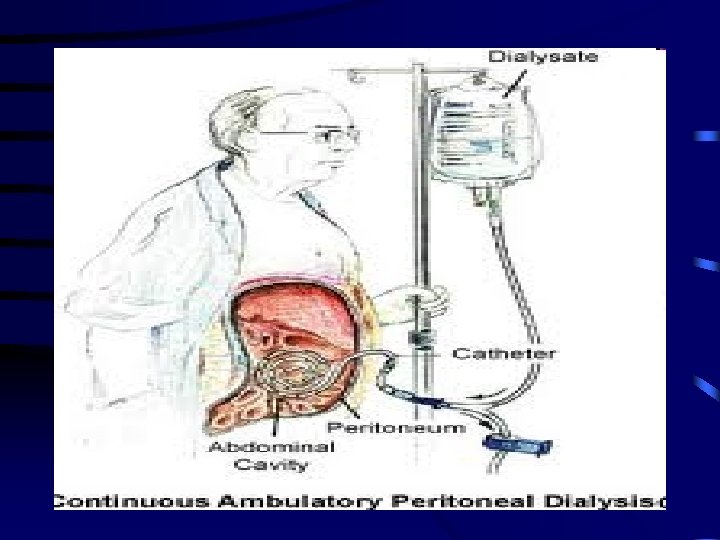
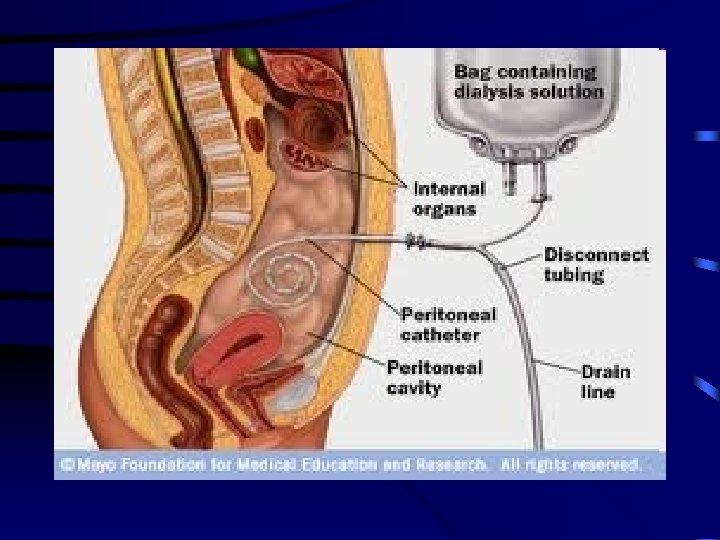
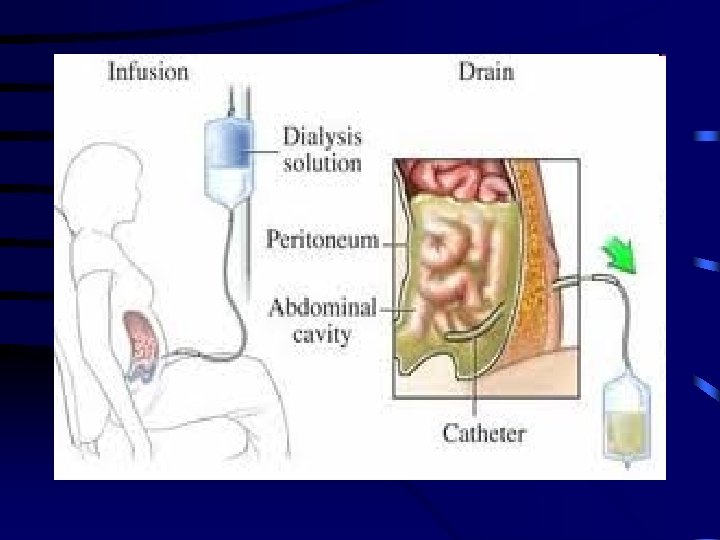
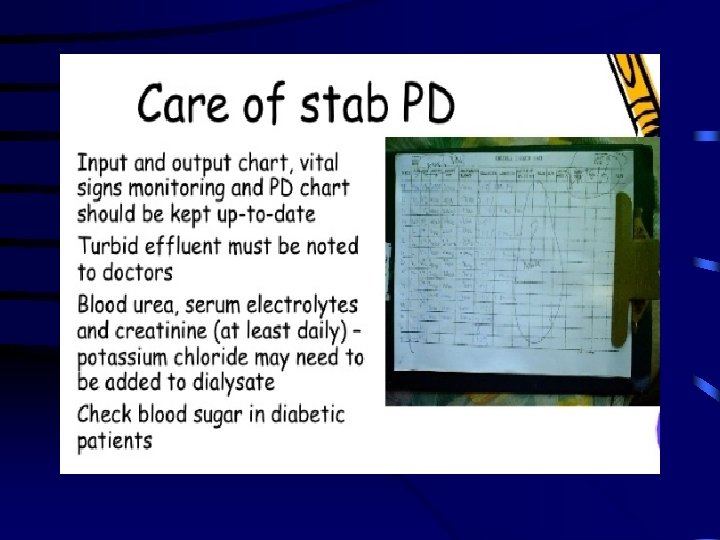
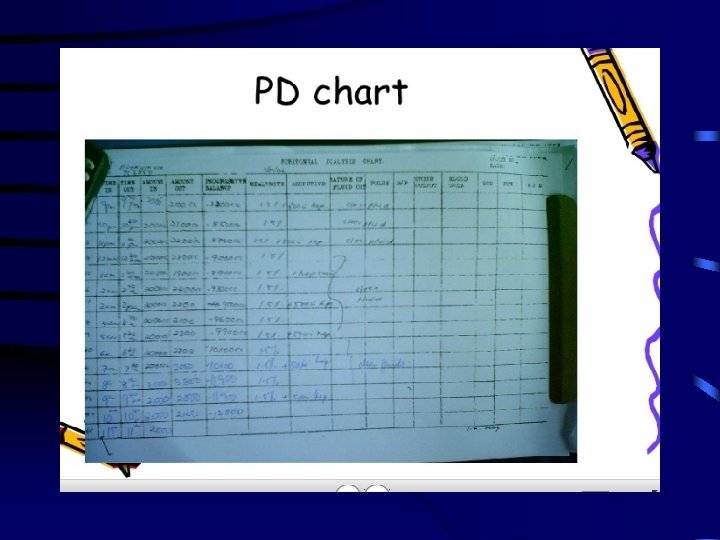
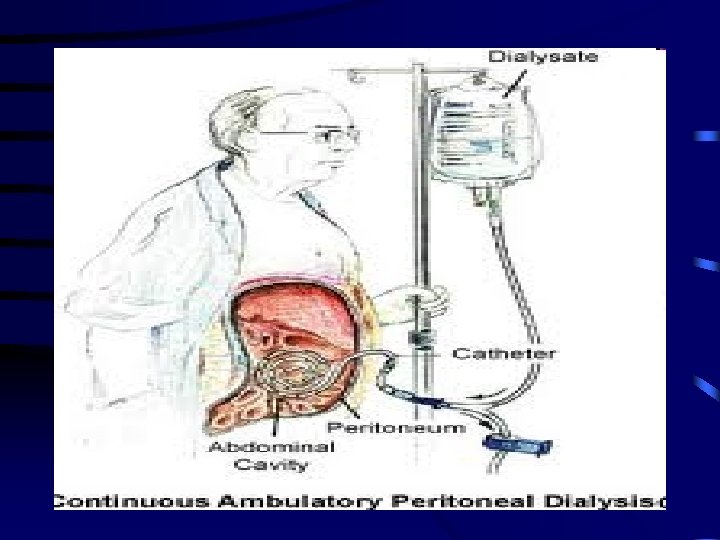
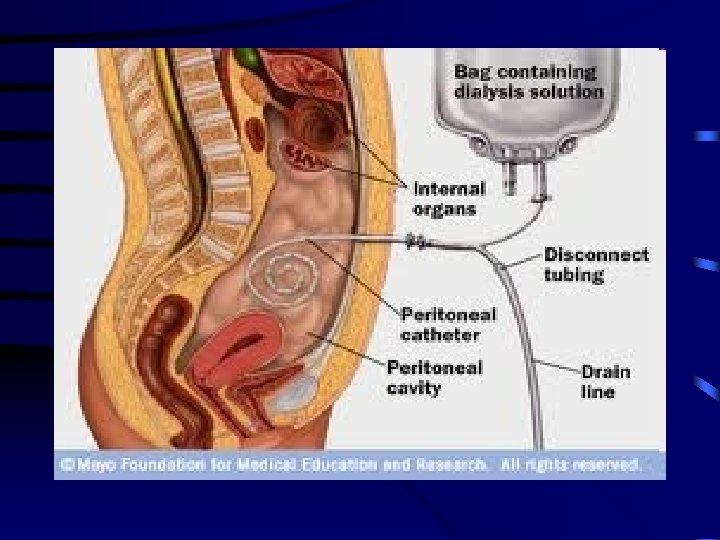
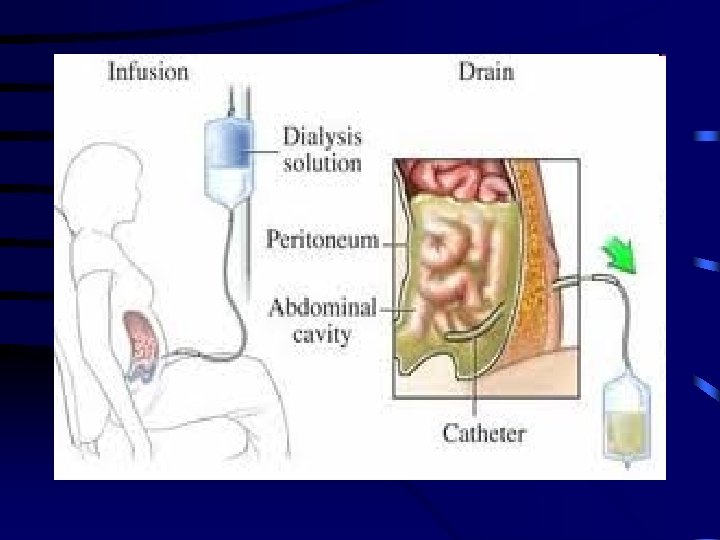
Dialysis Indications • Refractory hyperkalemia • Metabolic acidosis • Volume overload • Mental status changes