Acute renal failure Intrinsic renal Prerenal Acute tubular


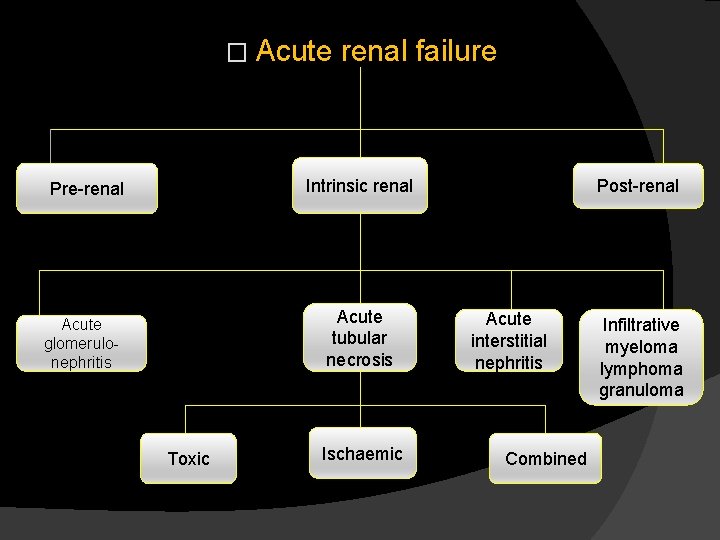
� Acute renal failure Intrinsic renal Pre-renal Acute tubular necrosis Acute glomerulonephritis Toxic Ischaemic Post-renal Acute interstitial nephritis Combined Infiltrative myeloma lymphoma granuloma
Different types of acute renal failure � In pre-renal failure the renal tissue is intact and kidney biopsy shows normal renal histology. Oliguria and high serum creatinin are due to functional impairment , since there is no sufficient blood reaching the kidney to be cleared of these toxins.
� In post-renal failure, the obstruction up to the nephron including the urinary space of the renal glomeruli. When this back pressure exceeds that of the filtration pressure in the renal glomeruli. , the process of urine formation will stop with progressive accumulation of wastes and increase of serum creatinine and blood urea
� In renal failure (intrinsic renal failure), there is a damage involving the glomeruli, renal tubules or tubulointrestitium with loss of their functions. Consequently wastes accumulate with increase in serum creatinine and blood urea.
1 -Pre-renal failure � Combination of hypotension, hypovolaemia resulting in diminshed renal perfusion is the most common cause of acute renal failure in hospitalized patients � Additional causes of pre-renal failure not necessarily associated with a decrease in GFR are conditions that increase urea production such as large protein intake and increased protein catabolism (fever, surgery, sever illness, steroids and tetracyclines).
� In patients with gastrointestinal bleeding the combination of high protein load (blood in gastrointestinal tract) and contracted circulating volume leads to an increase in blood urea concentration. � When renal hypoperfusion (due to hypotension and/or hypovolaemia)is not severe enough to cause renal tubular damage , it will manifest as pre-renal failure in the form of oliguria and a rise in serum creatinine and blood urea.
� Since there is no structural renal damage , early diagnosis and correction of renal hypoperfusion result in immediate diuresis and rapid drop in serum creatinine and blood urea level. � If hypoperfusion is severe or neglected , renal compensatory mechanisms will fail and acute tubular necrosis occure. � In this new situation , correction of hypoperfusion will not be followed by diuresis or drop in serum creatinine. Few days or weeks(mean 2 -3 weeks) are needed for tubular regeneration and recovery of kidney function to occure.
2 -Acute intrinsic renal failure � This includes acute tubular necrosis (ATN), acute interstitial nephritis and acute glomerulonephritis.
Acute tubular necrosis � Acute tubular necrosis can be induced by renal hypoperfusion (ischemia) or exposure to nephrotoxins (exogenous or endogenous toxin) and frequently by a combination of both.
Causes of ischaemic ATN : A-Intravascular volume depletion � Major trauma , burn and crush injury. � Haemorrhage (post partum, surgical and gastrointestinal) � Pancreatitis, vomiting, diarrhea, peritonitis, dehydration. � Hypoalbuminemia � Fluid volume depletion secondary to renal losses (diabetic ketoacidosis, diuretic abuse and adrenal insufficiency)
B-Decreased cardiac output � Severe congestive heart failure or low cardiac output syndrome � Pulmonary hypertension and massive pulmonary embolism
Increased(renal/systemic)vascula r resistances ratio: � Renal vasoconstriction : - Alpha adrenergic agonists - Hypercalcemia, amphotericin. Systemic vasodilatation: -After load reduction - Antihypertensive medications - Anaphylactic shock - Anesthesia - Sepsis � Liver cell failure: - Results in both systemic VD and renal VC �
D-Renovascular obstruction: � Renal artery: -Atherosclerosis, embolism, thrombosis, vasculitis. � Renal vein: - Thrombosis, compression.
E- Increased blood viscosity � Multiple myeloma � Macroglobulinaemia � polycythaemia
F- Aggravation of renal hypoperfusion by interference with renal autoregulation � Prostaglandin synthesis inhibitors as NSAIDs � Angiotensin converting enzyme inhibition in patients with renal artery stenosis.
Causes of toxic ATN
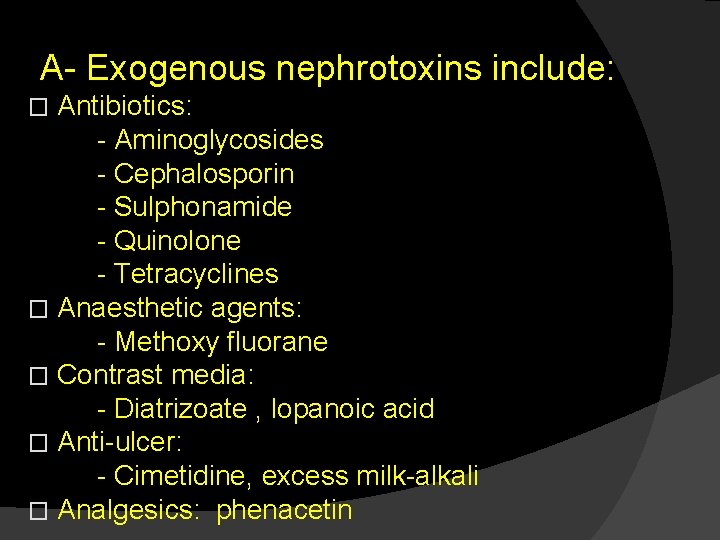
A- Exogenous nephrotoxins include: Antibiotics: - Aminoglycosides - Cephalosporin - Sulphonamide - Quinolone - Tetracyclines � Anaesthetic agents: - Methoxy fluorane � Contrast media: - Diatrizoate , lopanoic acid � Anti-ulcer: - Cimetidine, excess milk-alkali � Analgesics: phenacetin �
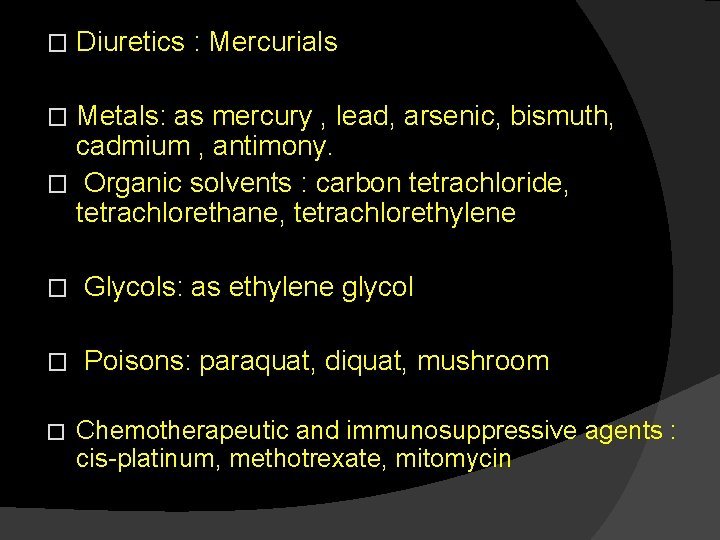
� Diuretics : Mercurials Metals: as mercury , lead, arsenic, bismuth, cadmium , antimony. � Organic solvents : carbon tetrachloride, tetrachlorethane, tetrachlorethylene � � Glycols: as ethylene glycol � Poisons: paraquat, diquat, mushroom � Chemotherapeutic and immunosuppressive agents : cis-platinum, methotrexate, mitomycin
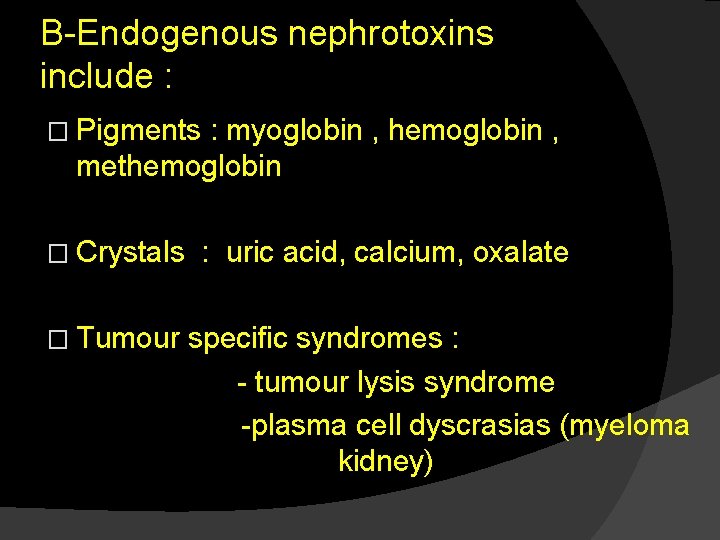
B-Endogenous nephrotoxins include : � Pigments : myoglobin , hemoglobin , methemoglobin � Crystals � Tumour : uric acid, calcium, oxalate specific syndromes : - tumour lysis syndrome -plasma cell dyscrasias (myeloma kidney)
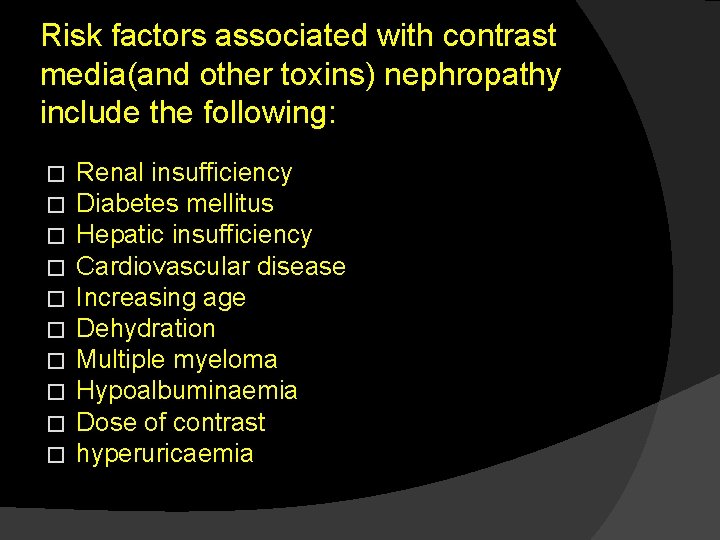
Risk factors associated with contrast media(and other toxins) nephropathy include the following: � � � � � Renal insufficiency Diabetes mellitus Hepatic insufficiency Cardiovascular disease Increasing age Dehydration Multiple myeloma Hypoalbuminaemia Dose of contrast hyperuricaemia
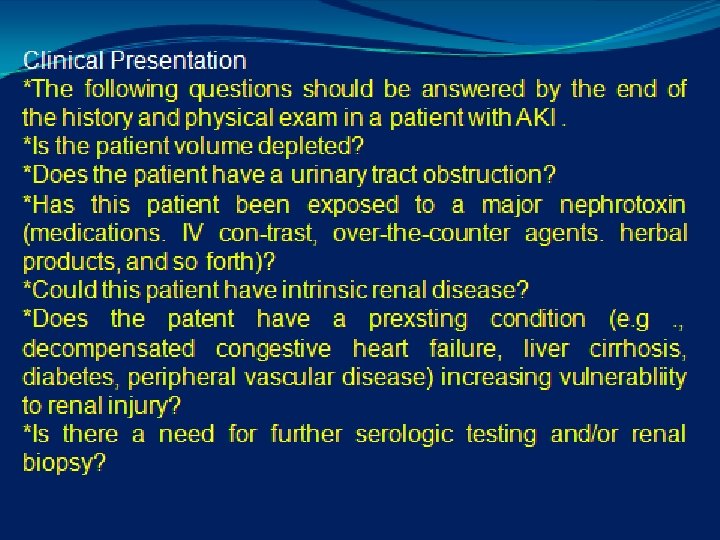

Clinical features of ARF � 1 - Usually the patient gives history of the etiologic cause such as trauma, shock, haemolysis, drug intake, infection, or stone disease � 2 - Patient may notice a change in urine volume and character , oliguria is common, but in 10 -50% of cases urine volume will be normal or even higher (as toxic ATN) this is called polyuric ATN. Absolute anuria is highly suggestive of obstructive ARF (post-renal) or very severe form of ATN (cortical necrosis).

� 3 - Manifestation of salt and water retention (oedema, puffiness, hypertension and even heart failure). � 4 -By time manifestation of uraemia appear as acidotic breathing, dyspnea, nausea, vomiting, headache, muscle twitches and even frank encephalopathy and coma. � 5 -Patient may present as well with any of the following complications:

-Complications of acute renal failure: � Cardiovascular - pulmonary odema - hypertension - myocardial infarction - arrhythemias - pericardial effusion - pulmonary embolism
� Metabolic: - hyponatremia - acidosis - hyperphosphatemia - hyperkalemia - hypocalcemia � Neurologic : - coma - seizures � Gastrointestinal : - gastritis - gastroduodenal ulcers
� Infections : - pneumonia - UTI - septicemia
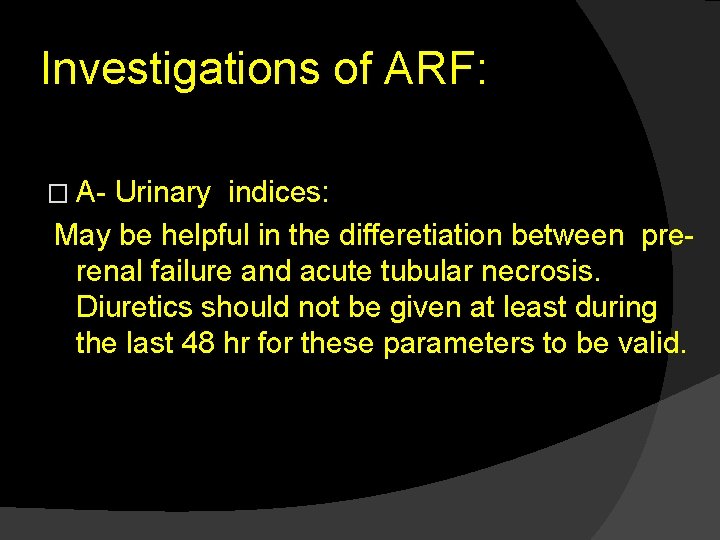
Investigations of ARF: � A- Urinary indices: May be helpful in the differetiation between prerenal failure and acute tubular necrosis. Diuretics should not be given at least during the last 48 hr for these parameters to be valid.
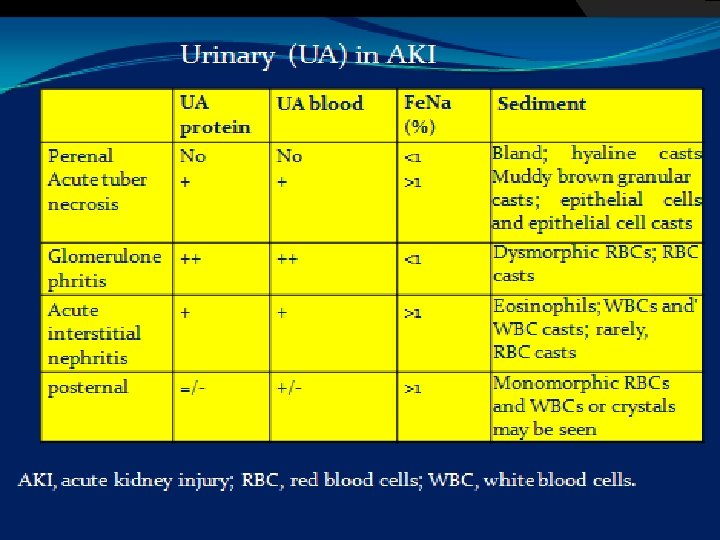

parameter prerenal ATN Concentration of urine Urine specific gravity > 1. 020 Urine osmolarity (mosm/lit) > 500 < 1. 010 <350 GFR and overall tubular reabsorption Creatinine clearance > 20 < 20 Urine/plasma urea >8 <3 > 40 < 20 Urine/plasma creatinine Tubular handling of solutes UNa (m. Eq/L) Fe. Na(%) <20 <1 >40 >1

B- Urinary sediment � Centrifugation of fresh urine sample and examination of the urinary sediment may be helpful in diagnosing different causes of ARF. C- Renal imaging: 1 - Plain film of the abdomen 2 - Renal ultrasonography and echo- Doppler of renal vessels 3 - Retograde and antegrade pyelography 4 - Radionuclide studies(Renogram) 5 - Angiography 6 - CT. studies 7 -Magnetic resonance urography

D- Renal biopsy: The indication of renal biopsy 1 - Equivocal case history 2 - Renal signs suggesting glomerular, vascular or interstitial lesions. 3 - Extrarenal manifestation in patients in whom a systemic disease identifiable by biopsy is suggested. 4 - Prolonged renal failure (more than 3 weeks)

In case of contrast media, the following additional points should be adopted, these are : � Avoid unnecessary contrast procedures. � Avoid multiple contrast exposure within a few days. � Avoid contrast exposure in high risk patient. � Use the smallest dose possible. � Use of non-ionic contrast is to somewhat safer. � In high risk patient with renal impairment web can manage to wash the contrast out immediately after the technique (e. g. coronary angiography) by haemodialysis � MRU is good alternative for visualization of the urinary tract obstruction. �
� Fluid requirement will increase with the increase in the body surface area and the atmospheric temperature and humidity (leading to increase in sweating). Fluids could be given orally or (if not possible ) it could be given intravenously. 2 -Electrolytes and acid –base balance: - Prevent and treat hyperkalemia. - Avoid hyponatremia. - Keep serum bicarbonate above 16 mmol/L - Minimize hyperphosphatemia by giving phosphate binders (e. g. Ca Co 3) with meals. - Treat hypocalcaemia. �
3 - Nutritional � Restrict protein (to 0. 5 gm/kg/day) but maintain sufficient caloric intake. � Carbohydrate intake should be at least 100 gm/day to minimize ketosis and endogenous protein catabolism. 4 - Drugs: - Review all medications. - Stop magnesium-containing medications. - Adjust dosage for renal failure.
5 - Treatment of hyperkalemia: � Calcium gluconate I. V. � Na Hco 3 I. V. � K-exchange resins (e. g. resonium) � Avoid diets and drugs causing hyperkalaemia � Glucose 50%+ insulin � Salbutamol � dialysis
6 - Dialysis: The indications of dialysis in ARF are: a- Clinical : � Poor clinical state, nausea, confusion. � Fluid overload, pulmonary oedema. � Preoperatively b- Biochemical : � Plasma K+ > 7 mmol/L. � Plasma bicarbonate < 12 mmol/L � Arterial Ph < 7. 15.
Prognosis of AFR: � The mortality of AFR remains high, ranging between 50 -80% in surgical and post – traumatic cases. It is generally lower in ARF due to drug and toxins. About 75% of deaths occur in the first week of ARF, and 25 -50% of these deaths are due to the underlying disease. The overall prognosis is better in non-oliguric than in oliguric renal failure.

The factors influencing patient survival in acute renal failure include the following: � Aetiology of ARF � Severity of ARF � Number and severity of coexisting illness. � Patient ’s age � Presence of complications

- Slides: 50