ACUTE REJECTION Outline Epidemiology Stats Effects on Outcome

- Slides: 39
ACUTE REJECTION
Outline Epidemiology, Stats, Effects on Outcome Pathophysiology Presentation Diagnosis / Pathology Grading Prevention Treatment
Epidemiology Rejection epidemiology more developed in pediatrics since NAPRTCS collects info No multicenter adult database collects rejection data
Acute Rejection is Different in Kids
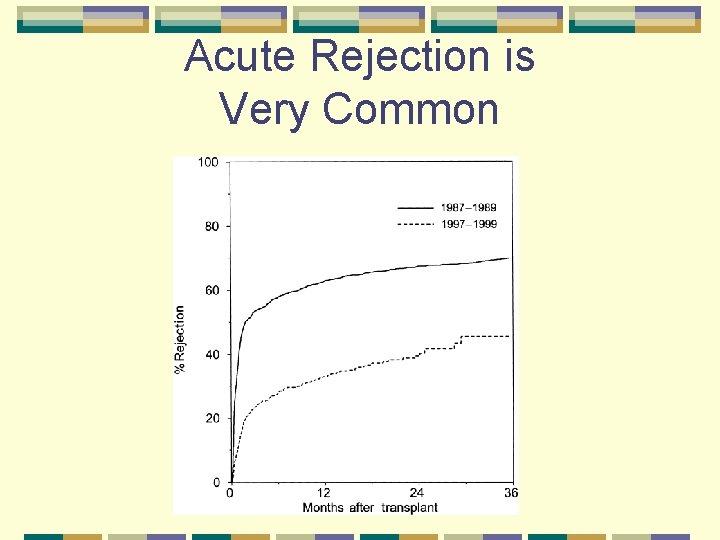
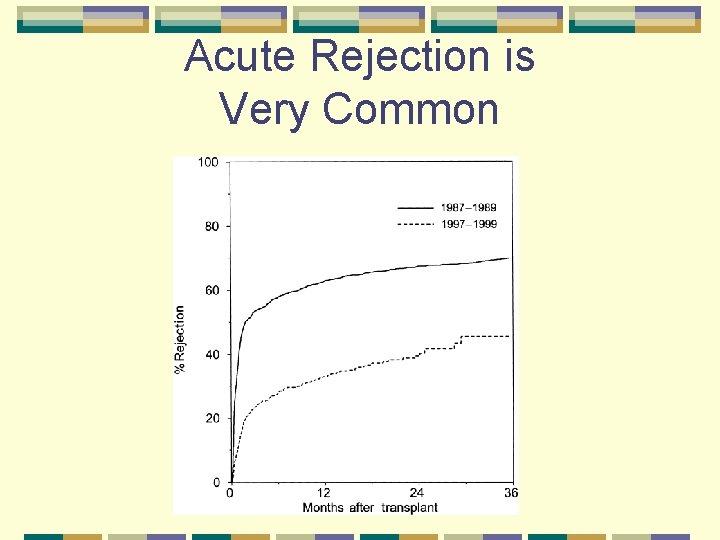
Acute Rejection is Very Common
Acute Rejection is More Frequent in Kids than Adults
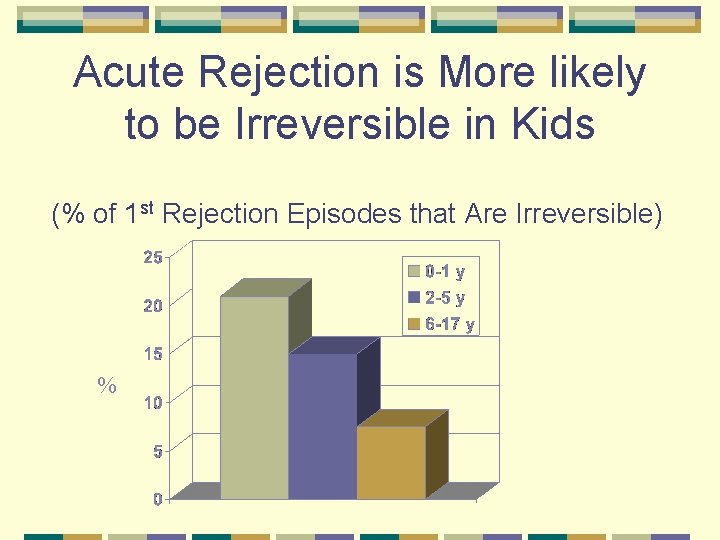
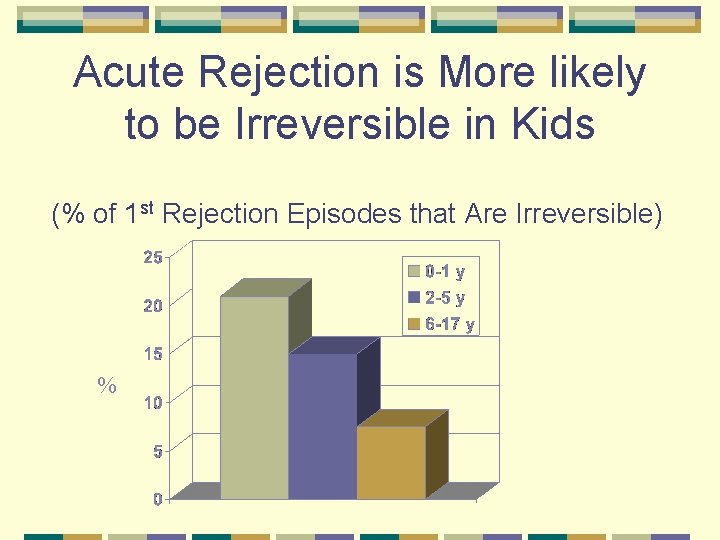
Acute Rejection is More likely to be Irreversible in Kids (% of 1 st Rejection Episodes that Are Irreversible) %
Acute Rejection a Strong Predictor of Graft Failure • 32 % of all pediatric graft losses • 1 st episode increases risk by 3. 6 x • 2 d episode increases risk by 4. 2 x Tejani, NAPRTCS, 2002
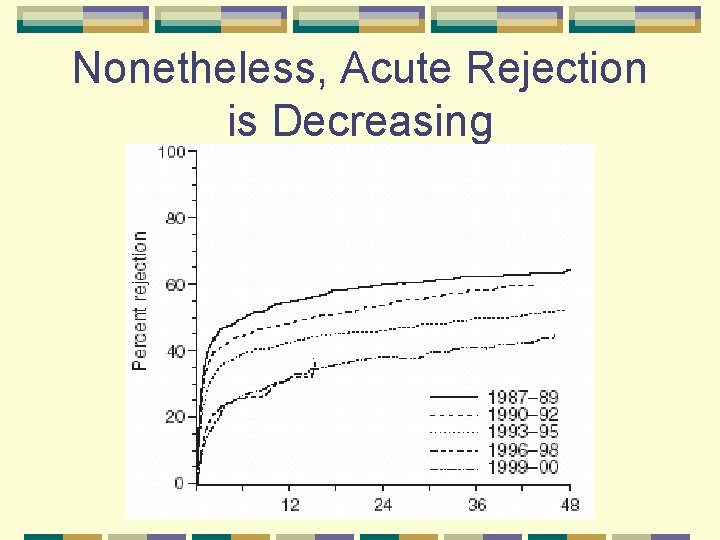
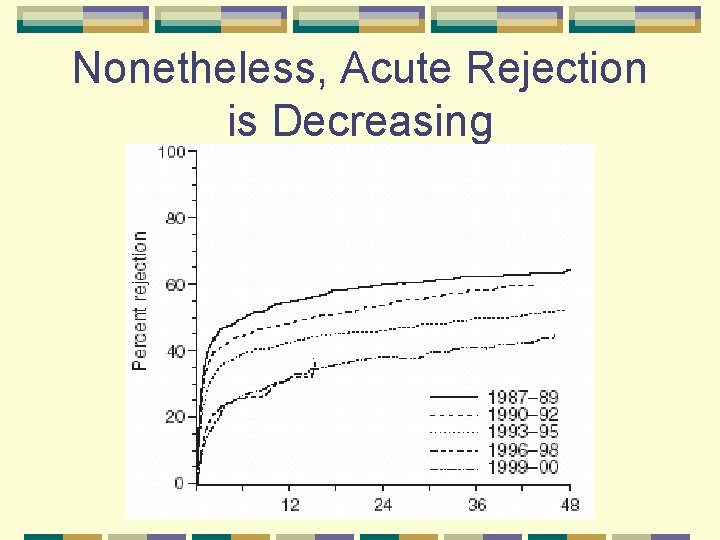
Nonetheless, Acute Rejection is Decreasing
Risks for Acute Cellular Rejection DGF Re-transplantation High PRA Low immunosuppressive dosing Poor compliance African-American
Types of Rejection Hyperacute / Accelerated Acute Cellular / Vascular Chronic Late Antibody Mediated
Hyperacute Uncommon due to screening Time: minutes Symptoms: None; seen in OR Signs: Purple, clotted graft; may rupture Pathogenesis: Anti-Donor HLA Abs, present before transplant; attack endothelium Histology: thrombosis, necrosis
Acute Cellular 90% of early histologically proven rejection Time: 7 -30 days Symptoms: Uusally none, but fever, chills, sweats, myalgia, graft tenderness, decreased UO, HTN Signs: increasing Cr, Increased RIs, Swollen kidney without CM differentiation, thickened uroepithelium, Pathogenesis: Graft infiltration with recipient T -Cells Histology: tubulitis, vasculitis
Ab Mediated 5 -10% of biopsy rejections Hours to weeks Symptoms: none, or fever and graft tenderness Histology: Little tubulitis, prominent vasculitis, C 4 d staining in peritubular capillaries (PTCs)
Chronic Rejection Added by Banff in 1993 CAN
Diagnosis Symptoms Traditional Labs “New” Lab Tests Imaging Biopsies
Symptoms Stable s. Cr, but new HTN or fever > 5 d (Bunchman) Fever, Myalgias, Graft tenderness, Decreased Urine Output
Labs Increase in s. Cr
Imaging Large swollen kidneys High Resistive Indices on US
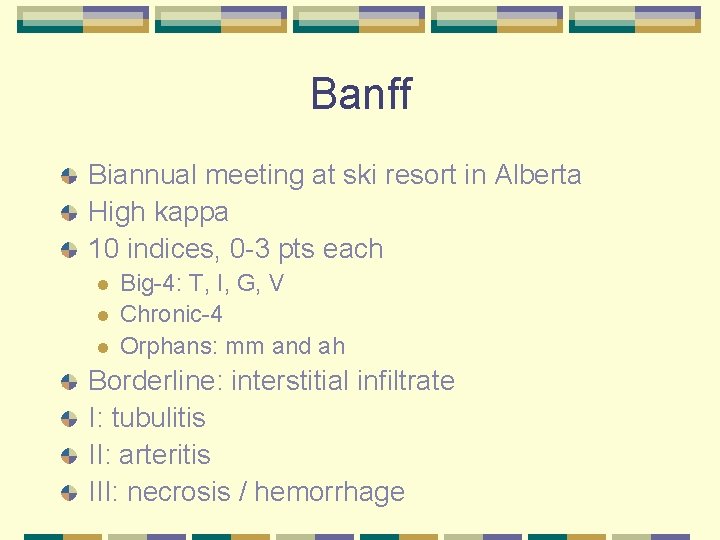
Banff Biannual meeting at ski resort in Alberta High kappa 10 indices, 0 -3 pts each l l l Big-4: T, I, G, V Chronic-4 Orphans: mm and ah Borderline: interstitial infiltrate I: tubulitis II: arteritis III: necrosis / hemorrhage
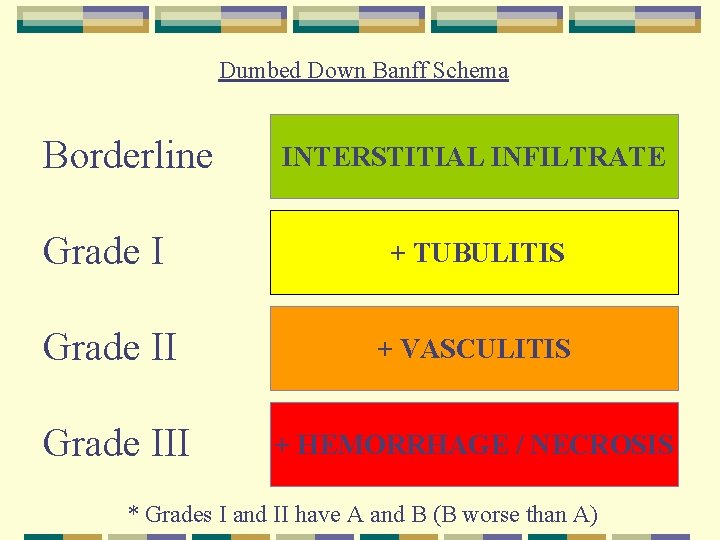
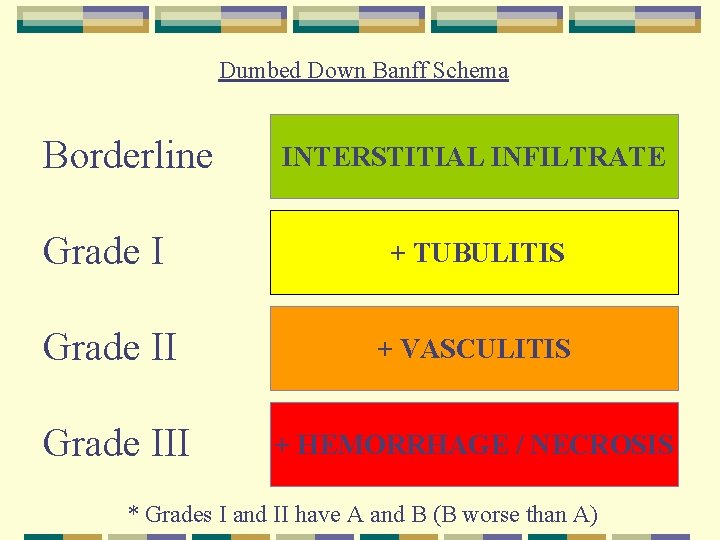
Dumbed Down Banff Schema Borderline INTERSTITIAL INFILTRATE Grade I + TUBULITIS Grade II + VASCULITIS Grade III + HEMORRHAGE / NECROSIS * Grades I and II have A and B (B worse than A)
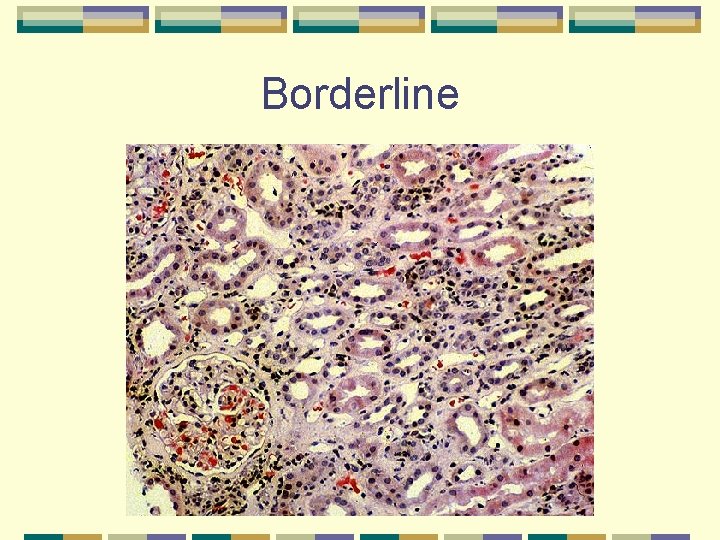
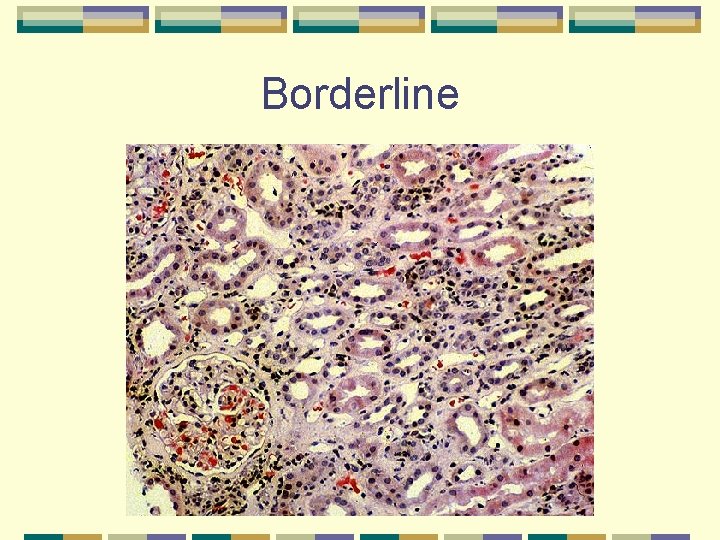
Borderline
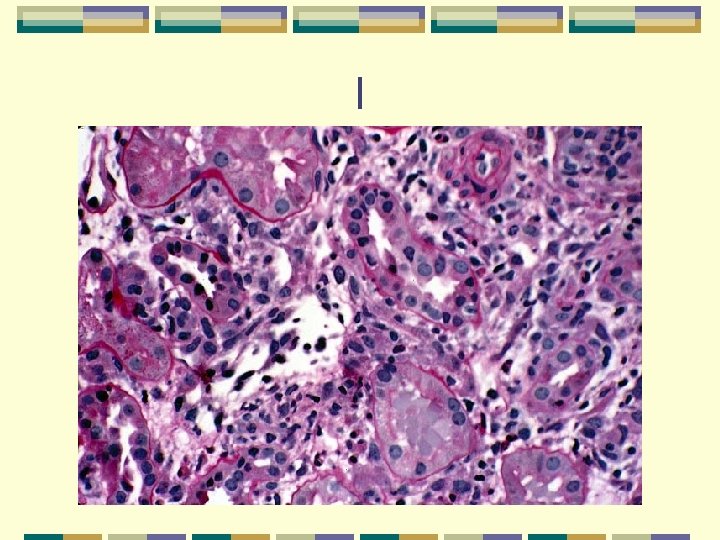
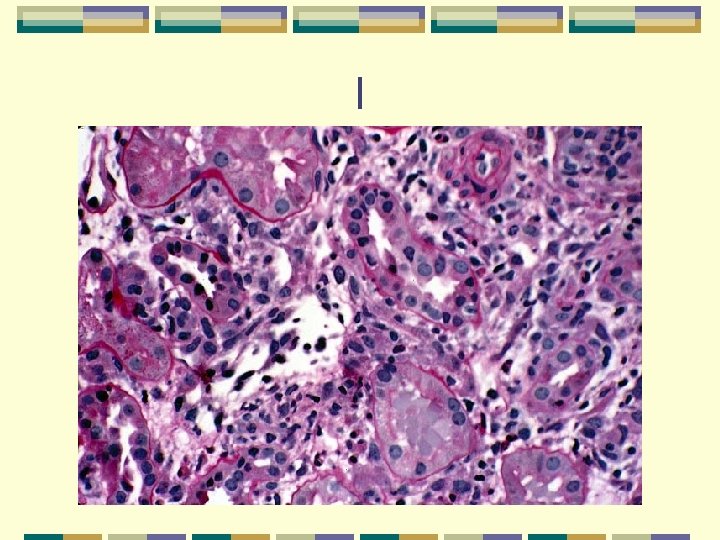
I
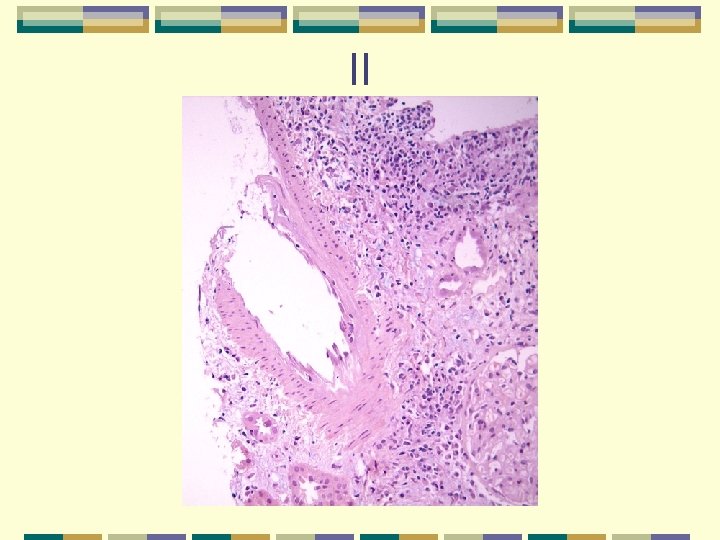
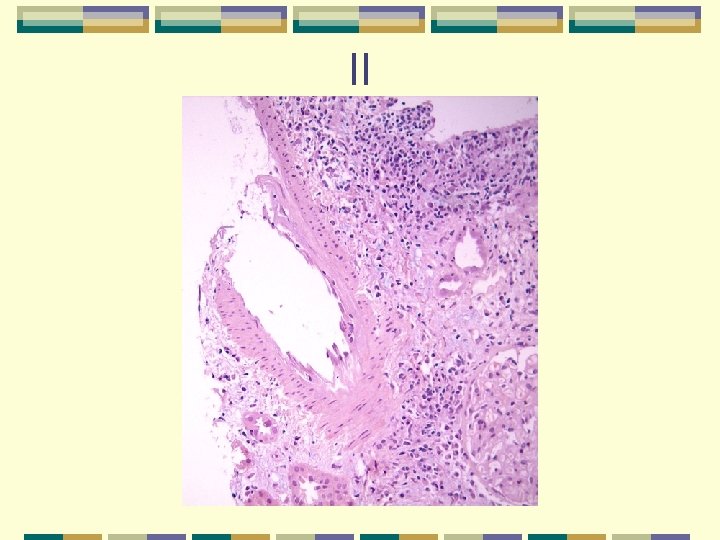
II
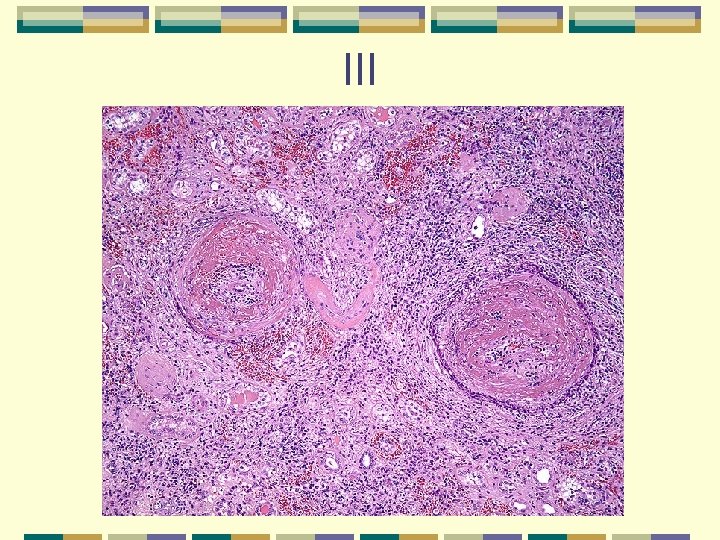
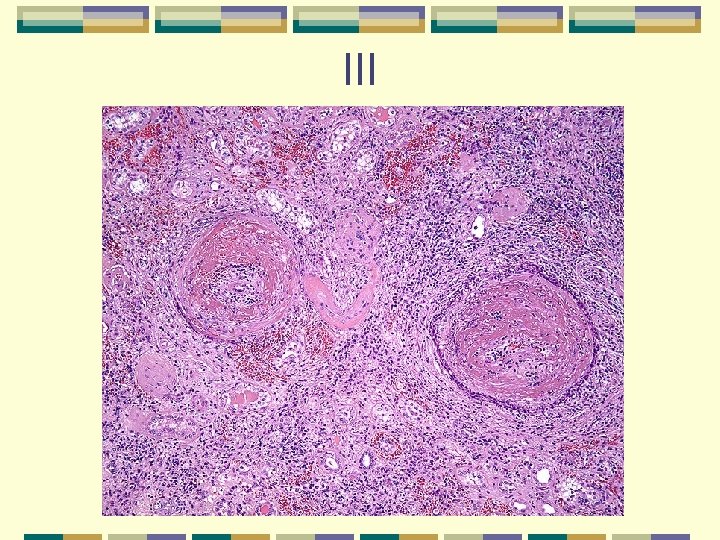
III

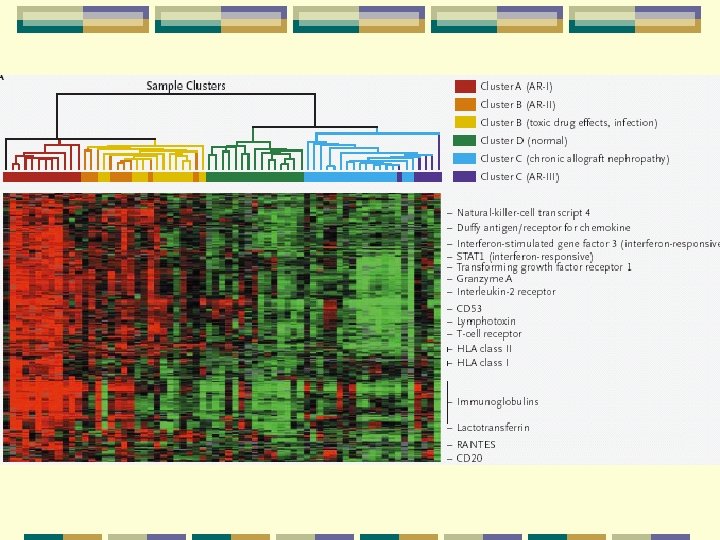
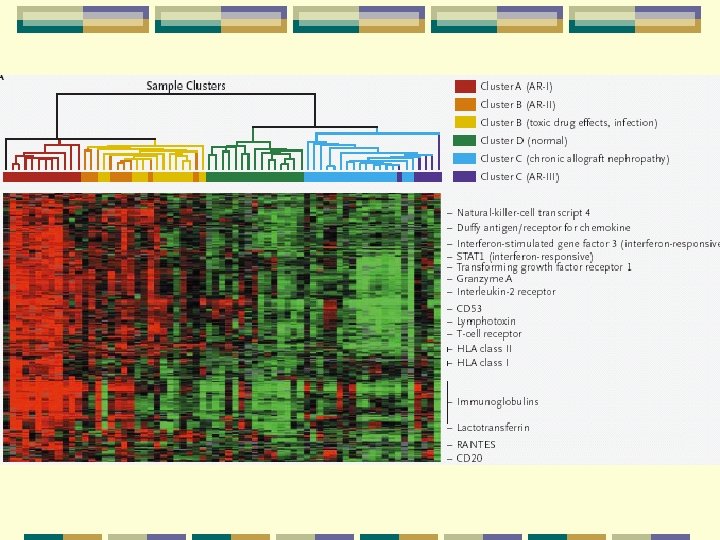
New Labs Urine microarrays Urine enzymes
Prevention Immunosuppressive Monitoring Protocol Biopsies Anti-IL 2 R Induction
Anti-IL-2 Induction Basiliximab (3 RCTs) Daclizumab (8 RCTs) Decrease AR in 1 st yr by 50%; 25% by 5 yrs l No difference in graft survival or complications l
Protocol Biopsies Picks up “Subclinical AR” l 1 -6 mo: 20 -50% SAR Most SARs Banff I SAR may help determine risk of CAN (Nakivell, NEJM 2003)
Treatment Maintenance immunosuppression has changed over time. Acute Rejection treatment has changed relatively little
Treatment AR is fully reversed in 50% of 1 st rejection, 28% of 4 th rejections (NAPRTCS, Kohau 96 Ped Neph) Graft loss due to as 1 st AR more common in younger kids Corey tx of kids with AR Borderline: Pulse Me. Pred l More steroid resistant as Banff increases l
Treatment for Acute Cellular: Steroids • 250 -1000 mg/d IV for 3 -5 days, OR • 250 mg/d PO • Histologic/clinical response within 6 days • 60 -75% response; higher the earlier it’s diagnosed
Treatment of Acute Cellular: Antilymph Abs OKT 3 (Mouse anti-CD 3) 5 mg/day for 7 -14 days 90% response of early, 70% if caught late Thymo: polyclonal anti-T cell, 1. 5 mg/kg for 7 -14 days
Treatment for Acute Cellular: Radiation If medication resistant, 400 Gy over 3 -5 days
Treatment of Acute Cellular: Other Increase Baseline Immunosuppression : If on CSA, add FK IVIG: 2 g/kg over 18 hrs, repeat if needed in 30 days
Treatment of Acute Vascular Steroids not as effective as in acute cellular Anti-lymph Abs: more commonly used as 1 st line
Treatment of Acute Humoral Pheresis & IVIG are 1 st line Rituximab: anti-CD 20, 375 mg/m 2/week for 4 weeks