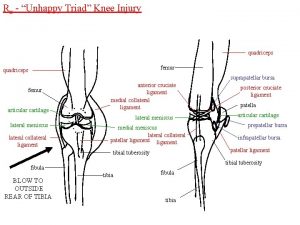
Acute Quadriceps Muscle Strains MRI features and prognosis








- Slides: 102
Acute Quadriceps Muscle Strains MRI features and prognosis Dr Tom Cross MBBS, FACSP, DCH The Stadium Orthopaedic and Sports Medicine Centre
Acute Quadriceps Muscle Strains: MRI features and prognosis Dr T Cross Dr N Gibbs Mr M Cameron Dr M Houang AJSM, April 2004
1. Introduction 2. Literature review 3. Methods 4. Results and Discussion 5. Conclusions 6. Questions? ?

Clinical Scenario e. g. . Anterior thigh pain 7 days before World Cup Final Can he play? ?
1. Introduction
Objective To describe the MRI findings of a series of acute quadriceps muscle strains
Objective To assess any relationship between the MRI findings and the time taken to return to sport

Setting l l Sydney Swans Football Club 1 of 16 clubs in the National competition

Design Prospective study over 3 years (1999 -2001): Both in-season and pre-season periods
Patients 40 professional footballers Consent from Club and individual players

Australian Rules Football “Athletes at risk” l l Repetitive sprinting efforts Repetitive kicking Repetitive jumping & landing Game time approximately 100 minutes
Australian Rules Football Ideal sport ( “outdoor laboratory”) to study muscle strain injury

Australian Rules Football Hamstring strain is the most significant injury in ARF (Quadriceps strain in top 10)
Motivation for research l To better understand/diagnose quadriceps muscle strains l To better manage/rehabilitate quadriceps muscle strains
Motivation for research l To make an EARLY ACCURATE PROGNOSIS (i. e. we were unable to clinically differentiate benign from serious quadriceps strains)
2. Literature Review
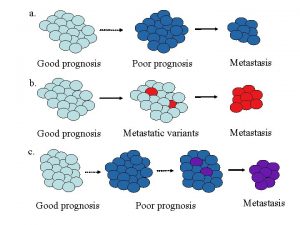
Literature review Pomeranz (1993) • Retrospective study of Hamstring strains • n=14 • Prognosis associated with size (cross-sectional area%) of muscle strain injury on MRI scan
Literature review No research (i. e. series of cases) on, Clinical behavior MRI findings of acute quadriceps strains
Literature review No mention of Vastus quadriceps muscle strains in the literature
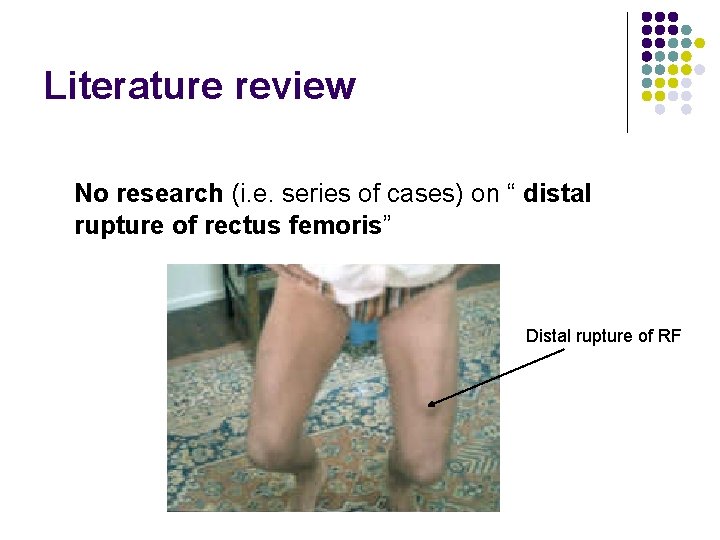
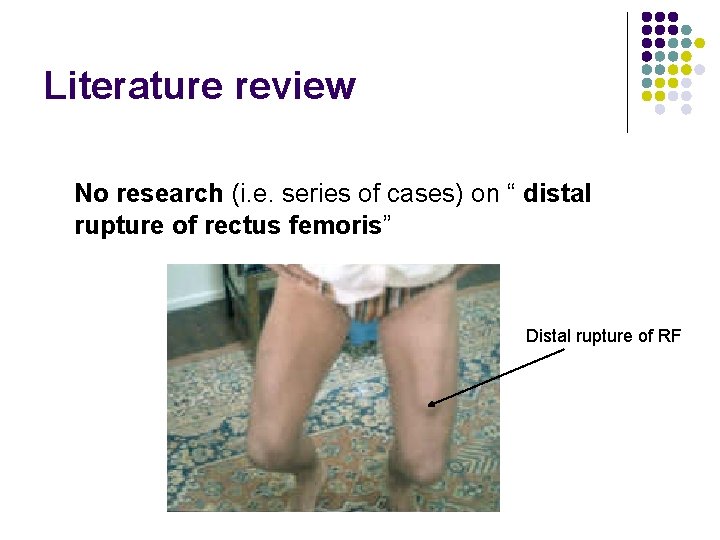
Literature review No research (i. e. series of cases) on “ distal rupture of rectus femoris” Distal rupture of RF
Literature review 3 retrospective studies on chronic muscle strain injuries of rectus femoris : all cases were “proximal injuries” 1. Rask and Lattig (1972) n=5 2. Hughes and Hasselman (1995) n=10 3. Temple et al (1998) n=7
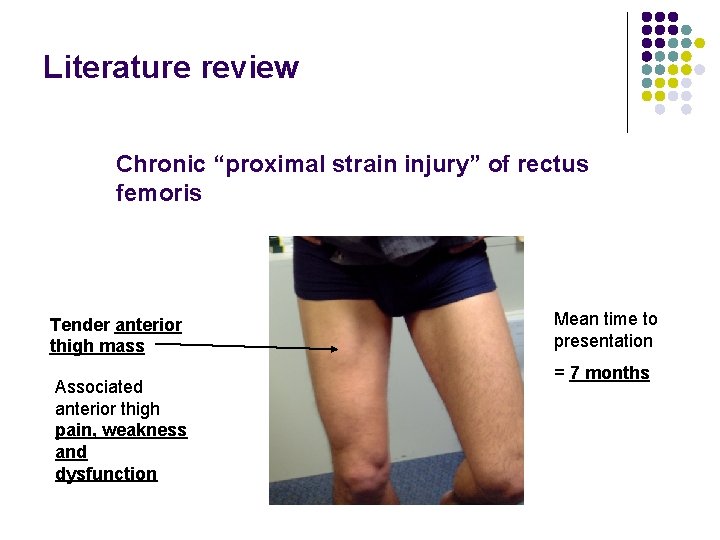
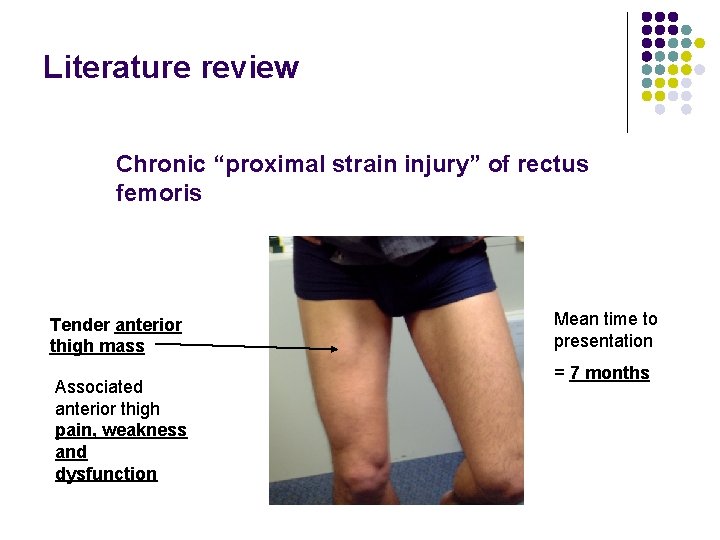
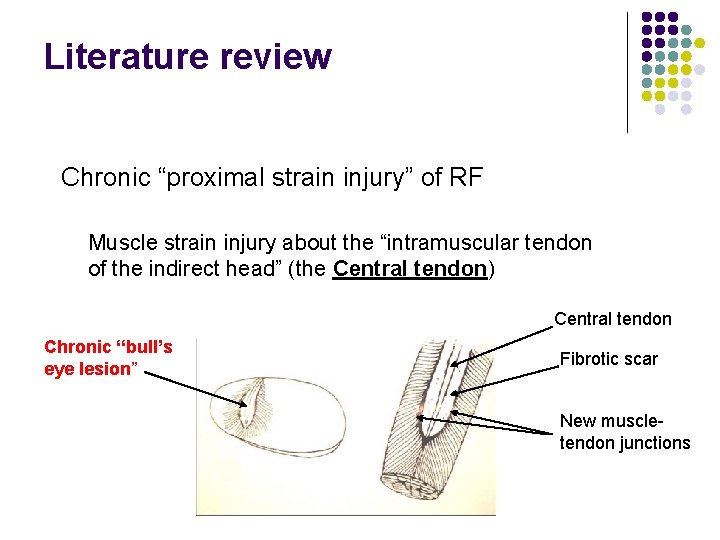
Literature review Chronic “proximal strain injury” of rectus femoris Tender anterior thigh mass Associated anterior thigh pain, weakness and dysfunction Mean time to presentation = 7 months
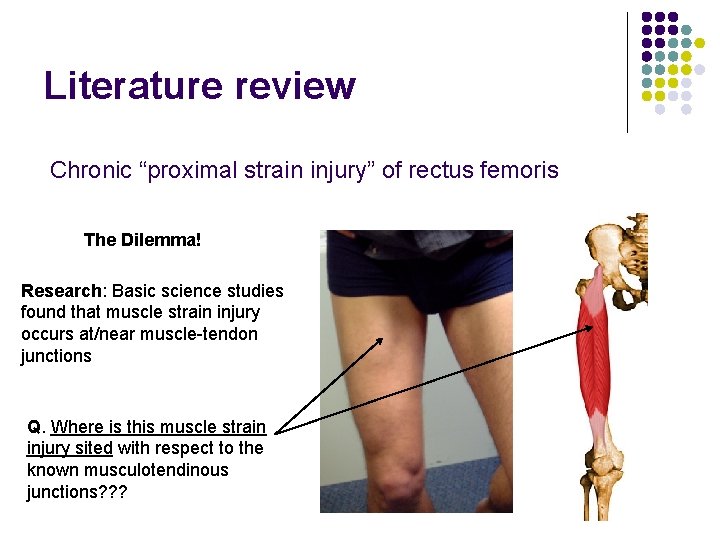
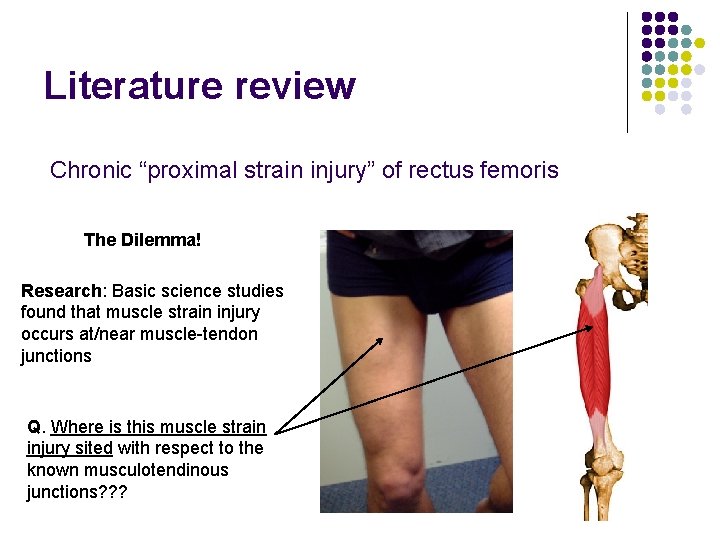
Literature review Chronic “proximal strain injury” of rectus femoris The Dilemma! Research: Basic science studies found that muscle strain injury occurs at/near muscle-tendon junctions Q. Where is this muscle strain injury sited with respect to the known musculotendinous junctions? ? ?
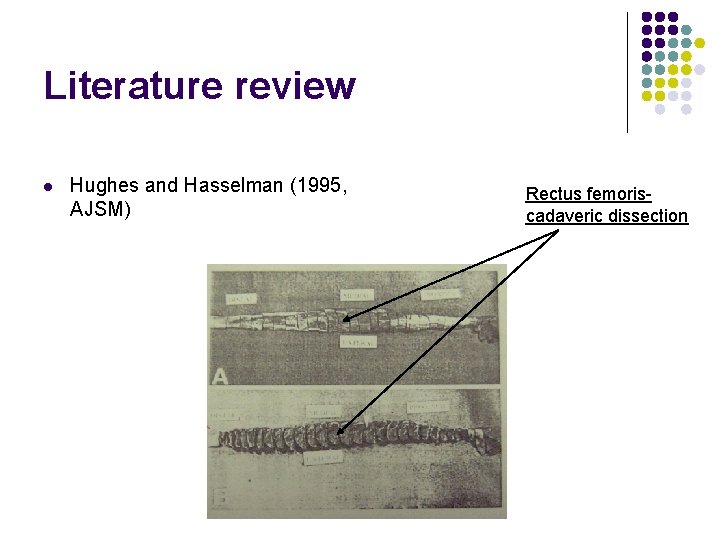
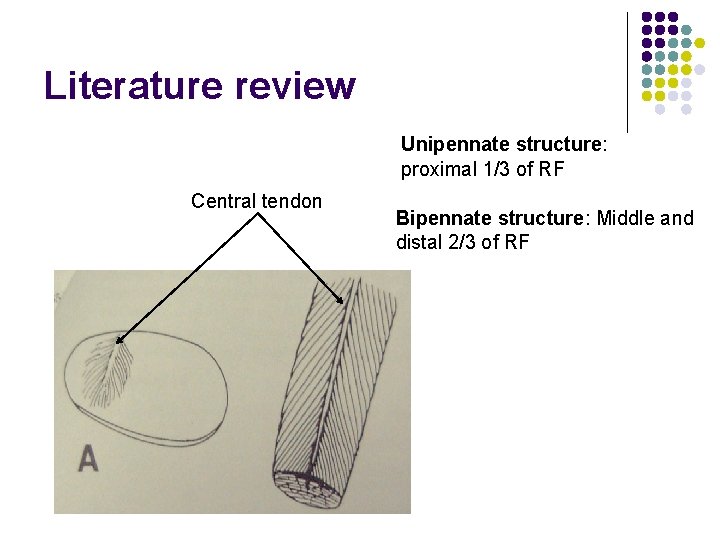
Literature review l Hughes and Hasselman (1995, AJSM) Rectus femoriscadaveric dissection
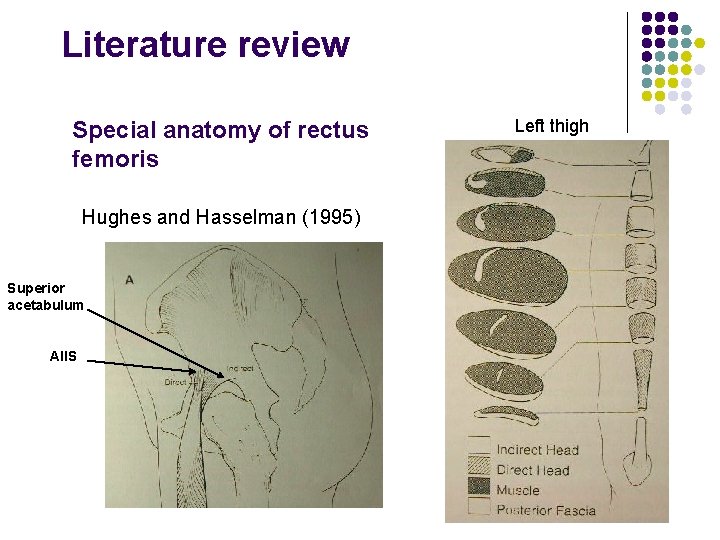
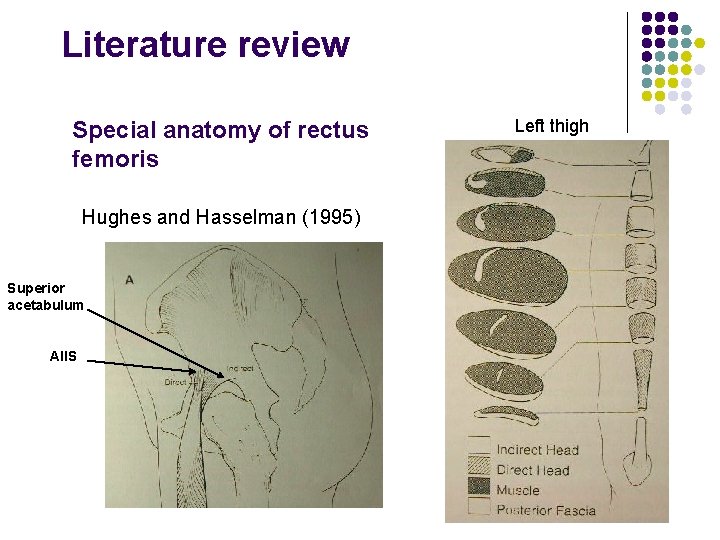
Literature review Special anatomy of rectus femoris Hughes and Hasselman (1995) Superior acetabulum AIIS Left thigh
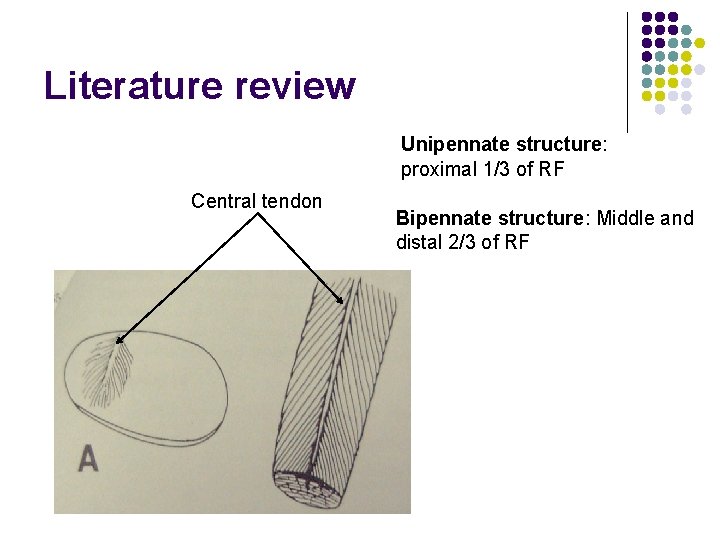
Literature review Unipennate structure: proximal 1/3 of RF Central tendon Bipennate structure: Middle and distal 2/3 of RF
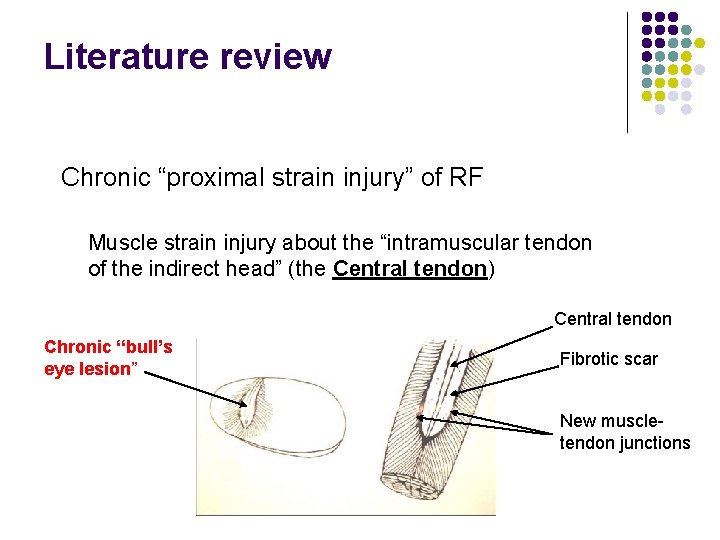
Literature review Chronic “proximal strain injury” of RF Muscle strain injury about the “intramuscular tendon of the indirect head” (the Central tendon) Central tendon Chronic “bull’s eye lesion” Fibrotic scar New muscletendon junctions
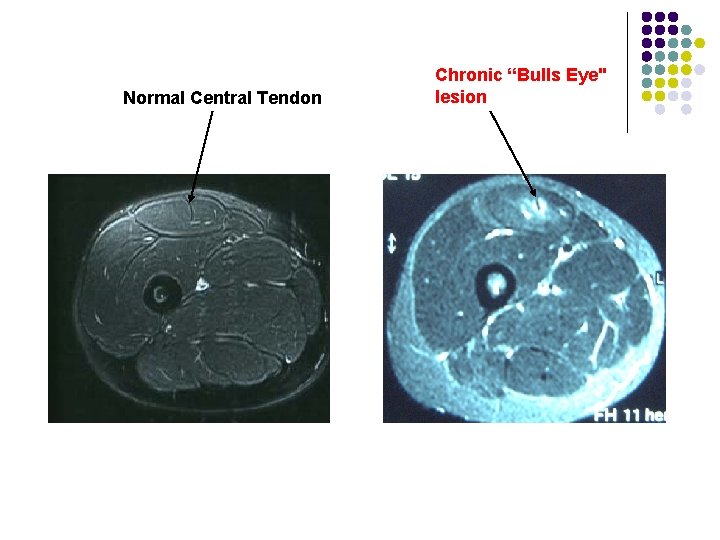
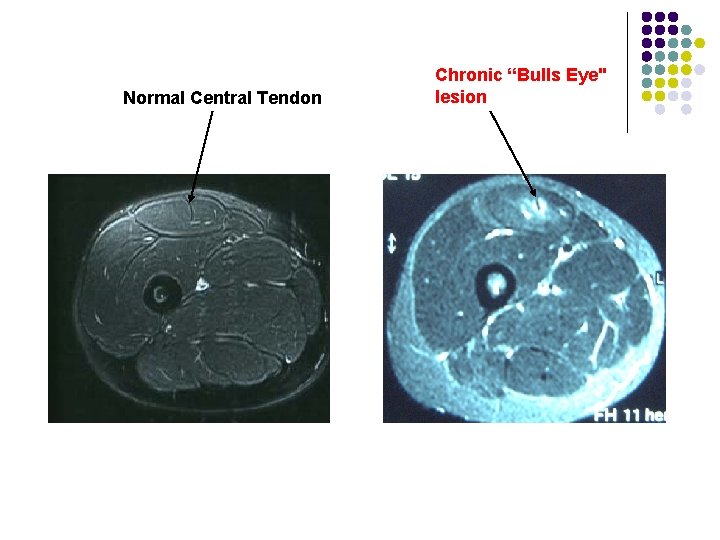
Normal Central Tendon Chronic “Bulls Eye" lesion
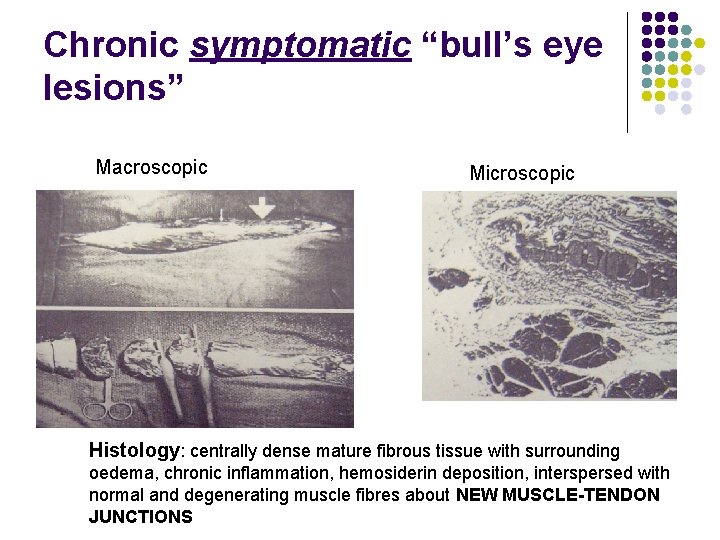
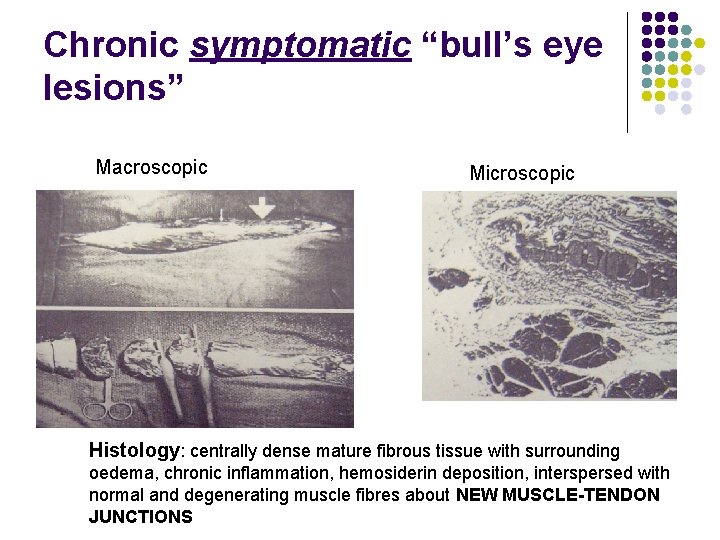
Chronic symptomatic “bull’s eye lesions” Macroscopic Microscopic Histology: centrally dense mature fibrous tissue with surrounding oedema, chronic inflammation, hemosiderin deposition, interspersed with normal and degenerating muscle fibres about NEW MUSCLE-TENDON JUNCTIONS
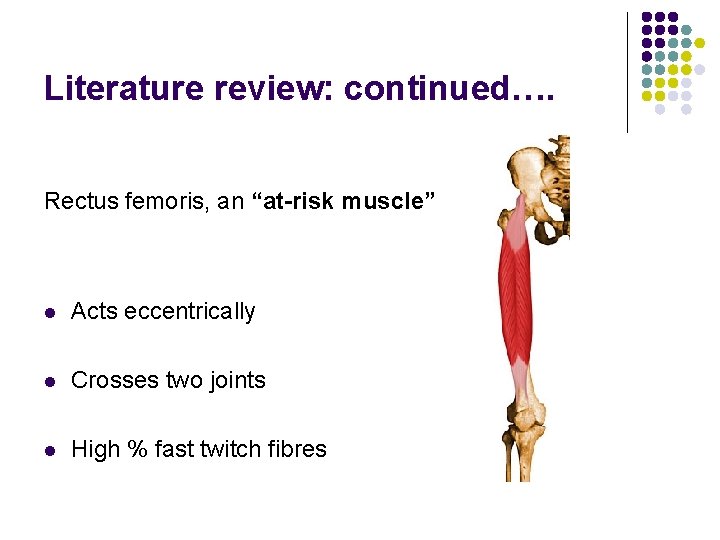
Literature review: continued…. Rectus femoris, an “at-risk muscle” l Acts eccentrically l Crosses two joints l High % fast twitch fibres
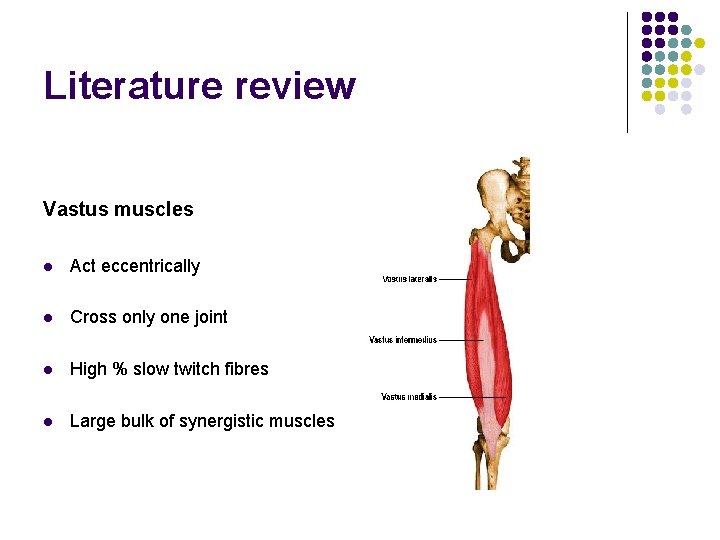
Literature review Vastus muscles l Act eccentrically l Cross only one joint l High % slow twitch fibres l Large bulk of synergistic muscles
3. Methods
Methods Inclusion criteria 1. 2. History 1. acute or gradual onset of anterior thigh pain while training or playing 1. Mechanism of injury documented (running, kicking, jumping/landing): if onset of symptoms were acute 2. Preferred kicking leg was correlated with the side injured Examination : tenderness over the anterior thigh : other signs elicited but not the subject of this study
Methods Exclusion criteria 1. History of trauma to anterior thigh (Contusion) 2. Delayed onset of anterior thigh pain (DOMS)
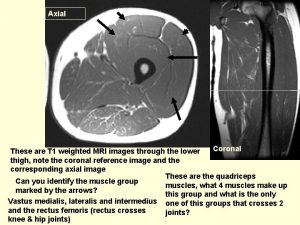
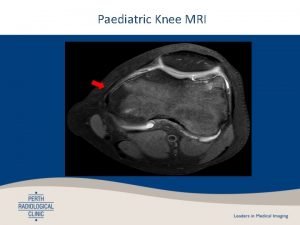
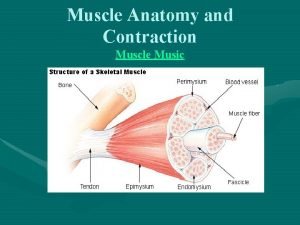
Methods MRI within 24 -72 hours • T 1, T 2 with fat suppression, STIR • Axial, coronal planes (both thighs imaged) (Axial T 2 with fat suppression most useful images)
Methods Muscle strain injury= high signal on T 2 weighted images
Methods MRI diagnosis Location (MRI category) 1. 2. Which quadriceps muscle (s) injured Location of injury with respect to known musculotendinous junctions
Methods MRI diagnosis Size 1. Cross sectional area % (CSA) 2. Length (cm)
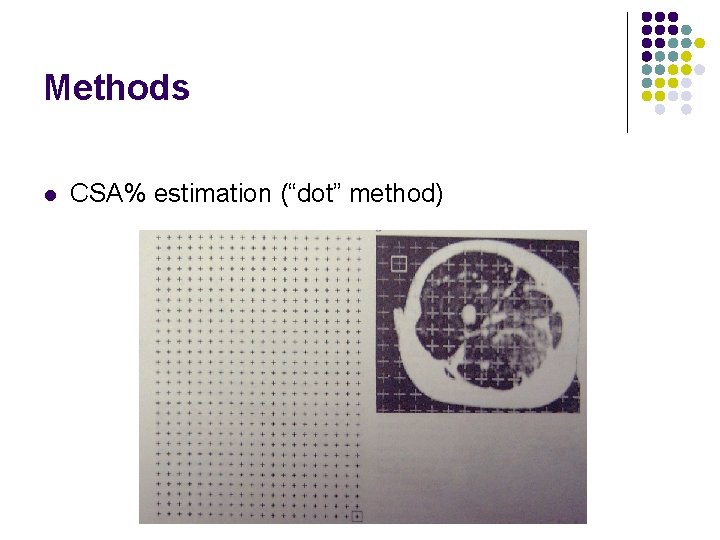
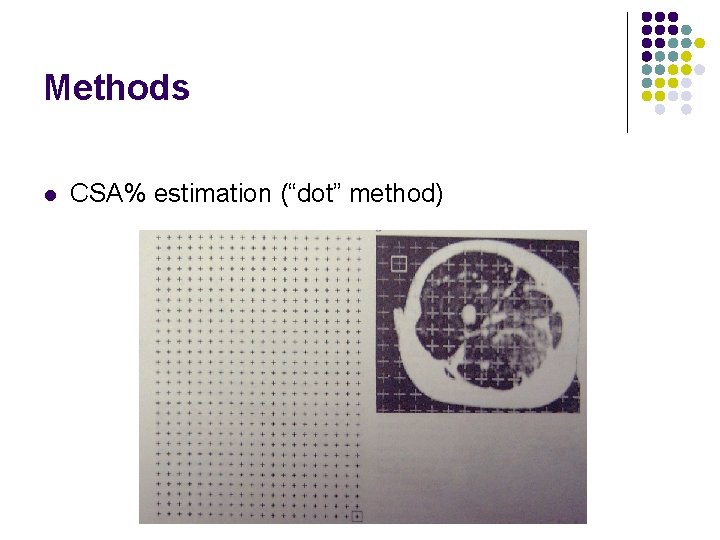
Methods l CSA% estimation (“dot” method)
Methods MRI diagnosis: miscellaneous features… • T 2 hyper intensity • muscle fibre disruption • Perifascial fluid • Scarring/fibrosis
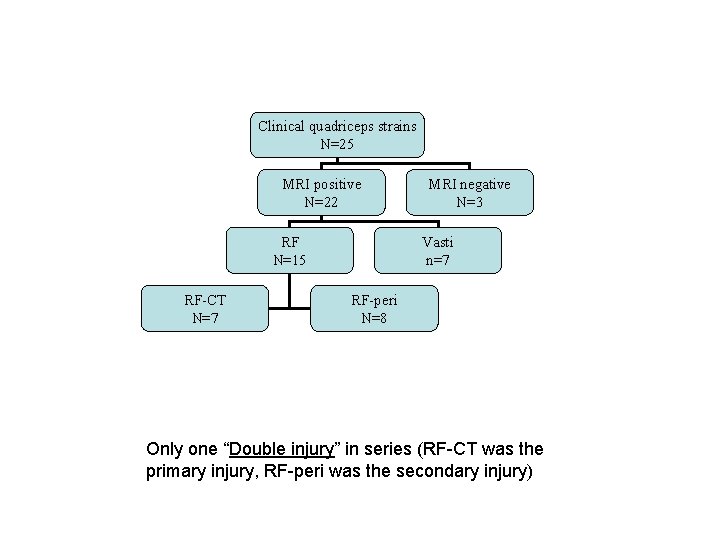
Methods What if more than one muscle injured? (i. e. double injury etc. ) 1. Primary muscle injured= greatest CSA% 2. Secondary muscle injury= smaller CSA%
Results of acute MRI images l 25 acute clinical quadriceps strains were imaged l Authors were not blinded to these MRI’s
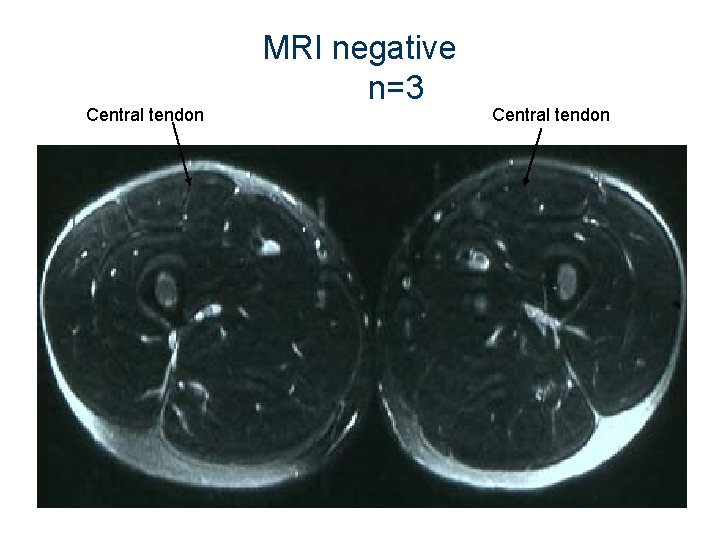
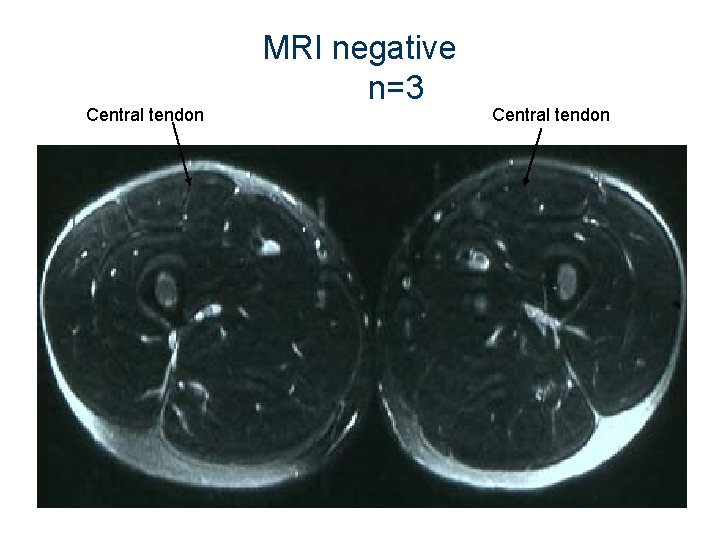
Central tendon MRI negative n=3 Central tendon
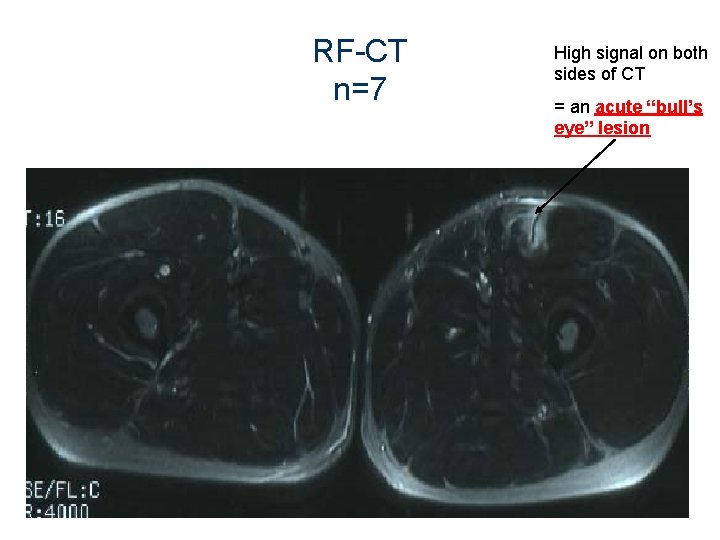
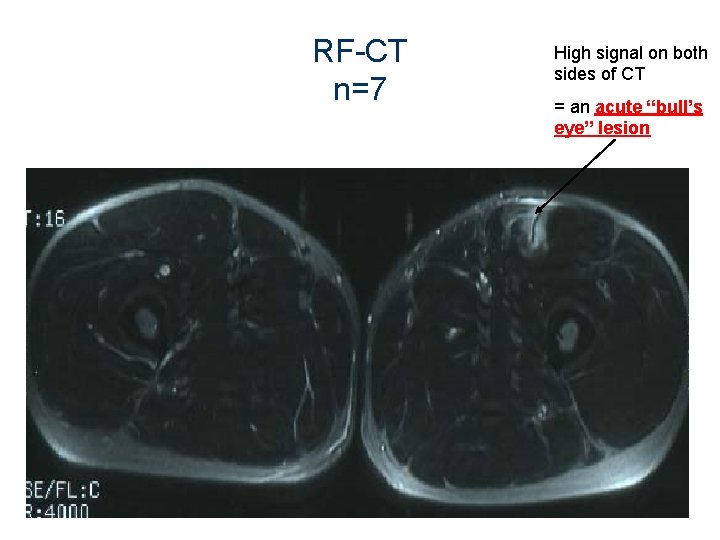
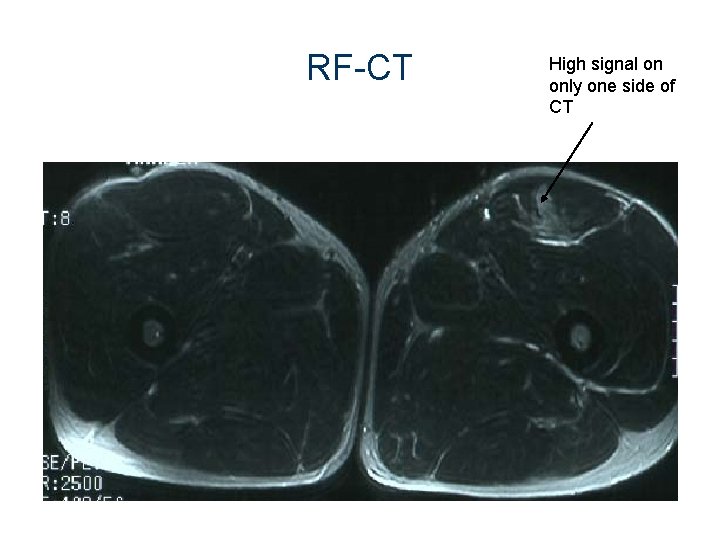
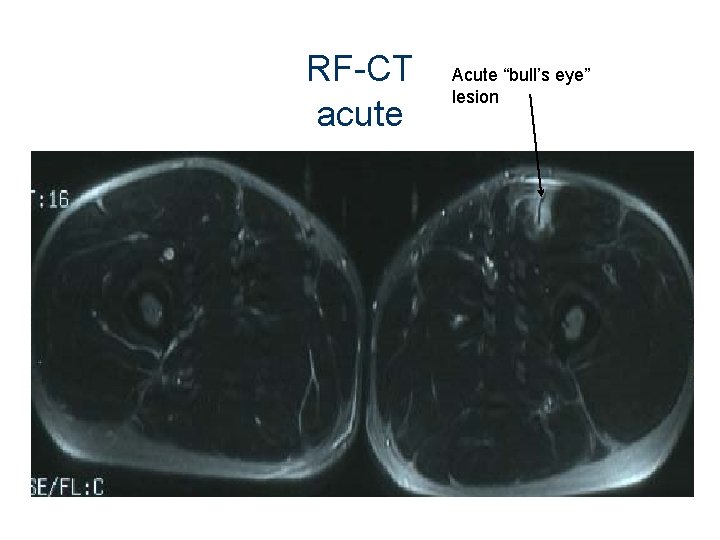
RF-CT n=7 High signal on both sides of CT = an acute “bull’s eye” lesion
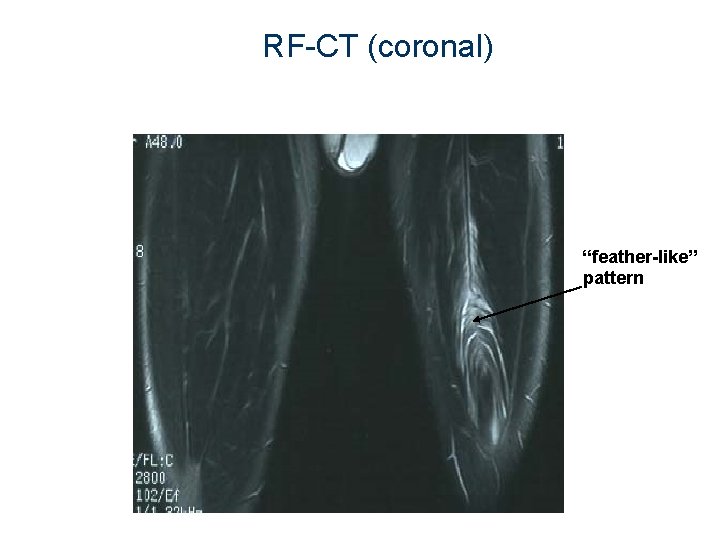
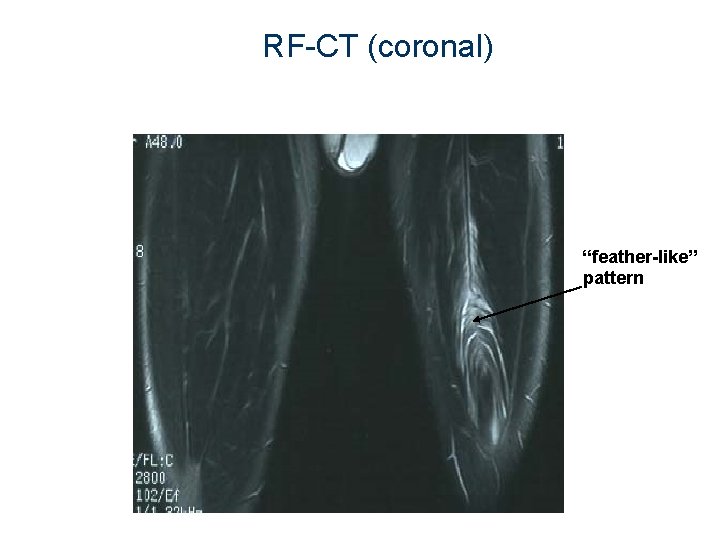
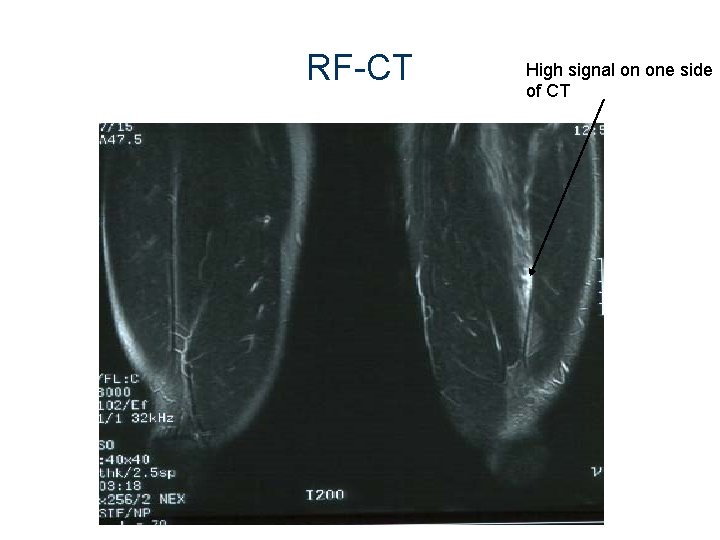
RF-CT (coronal) “feather-like” pattern
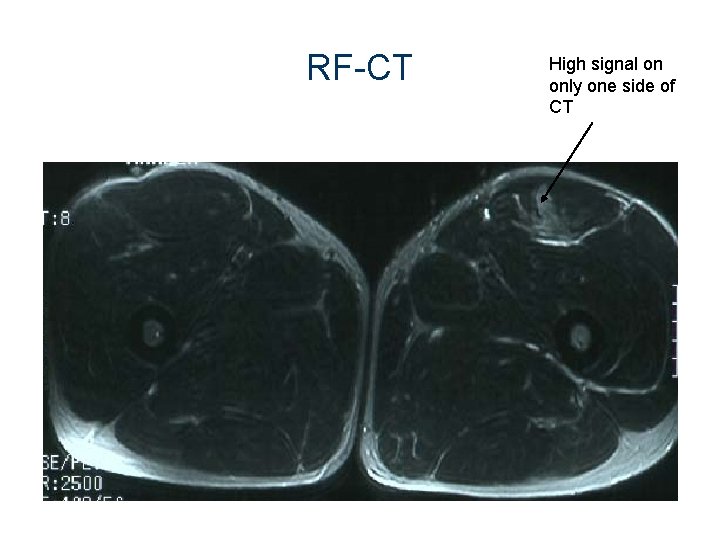
RF-CT High signal on only one side of CT
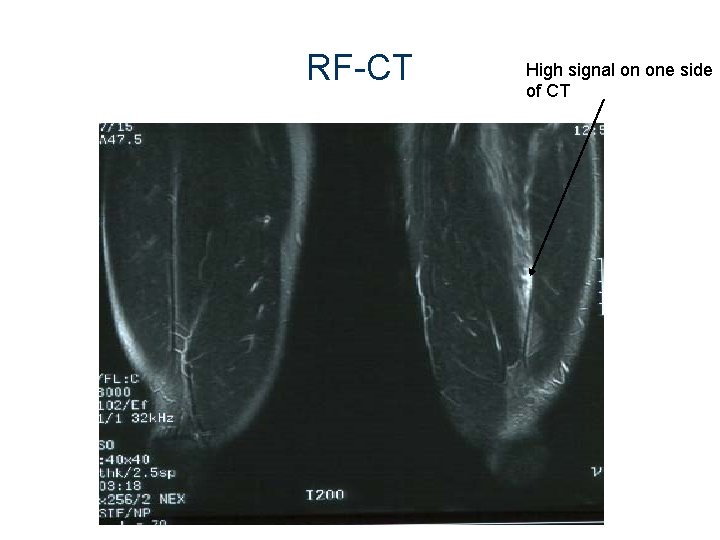
RF-CT High signal on one side of CT
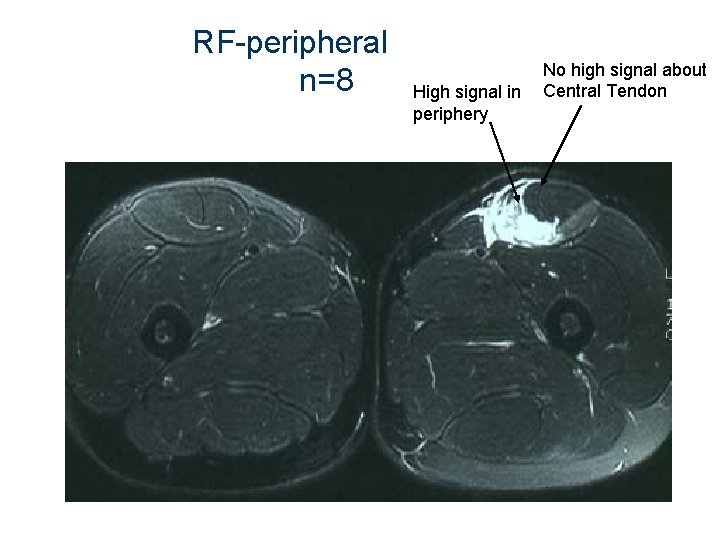
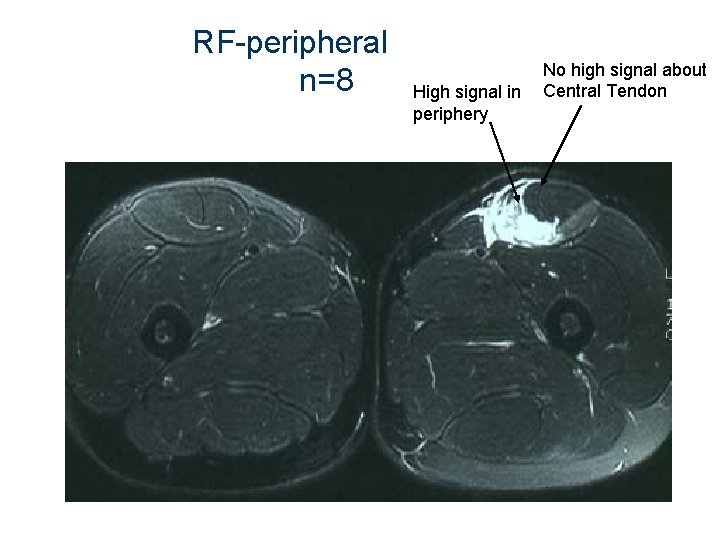
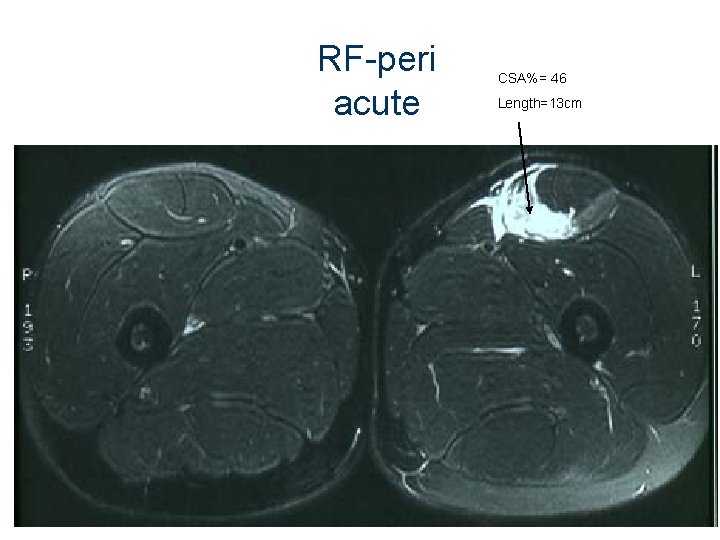
RF-peripheral n=8 High signal in periphery No high signal about Central Tendon
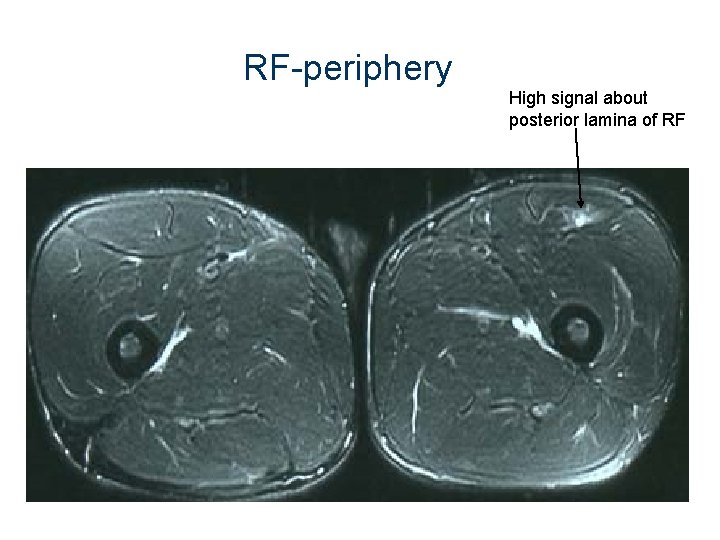
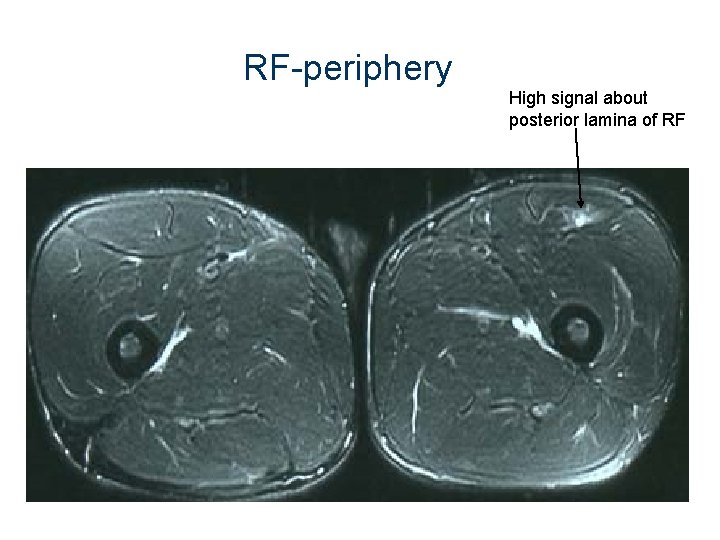
RF-periphery High signal about posterior lamina of RF
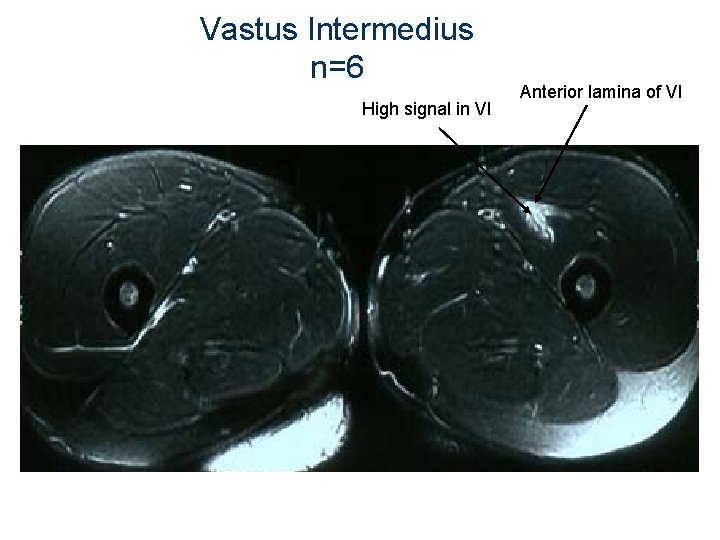
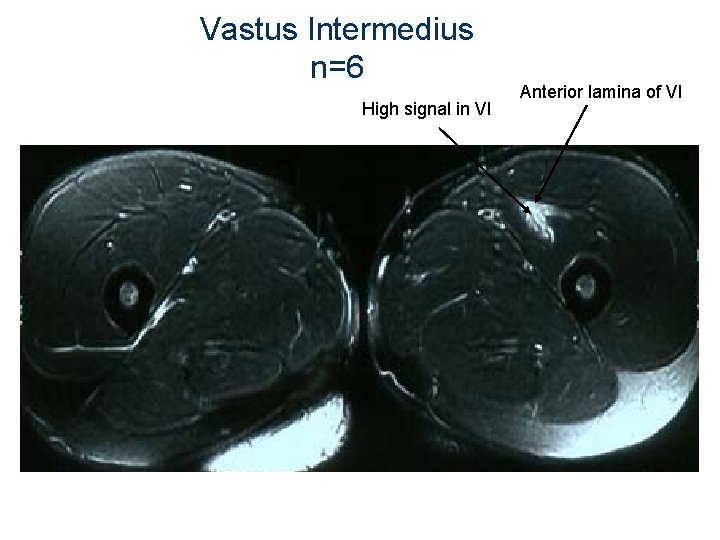
Vastus Intermedius n=6 High signal in VI Anterior lamina of VI
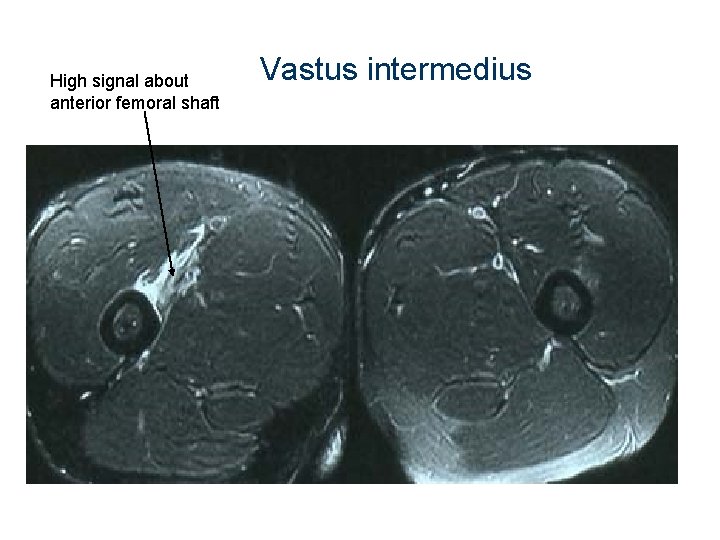
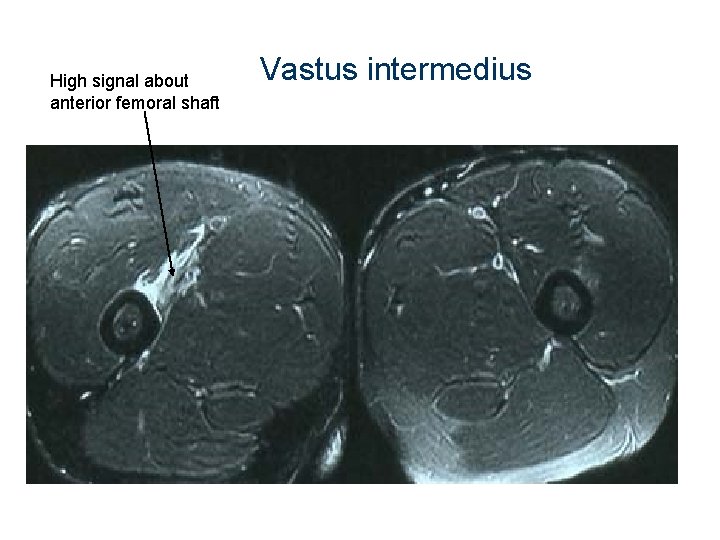
High signal about anterior femoral shaft Vastus intermedius
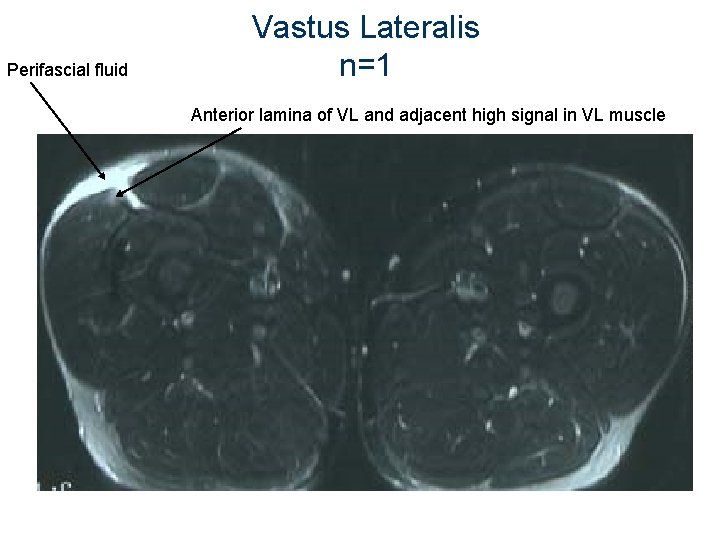
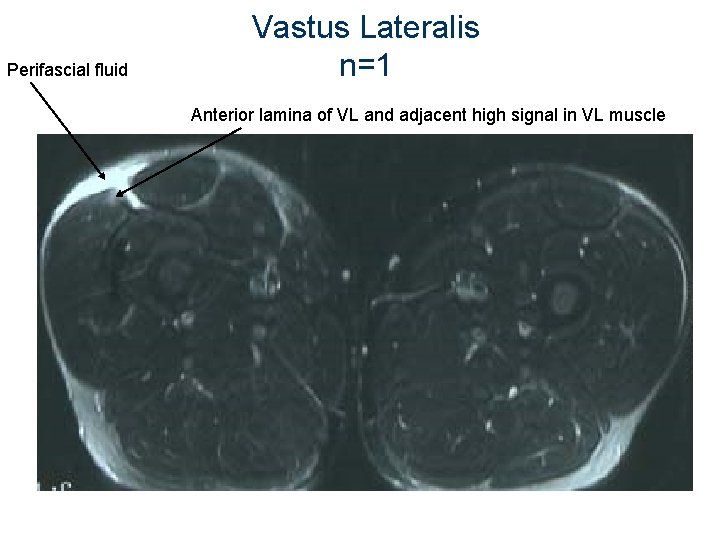
Perifascial fluid Vastus Lateralis n=1 Anterior lamina of VL and adjacent high signal in VL muscle
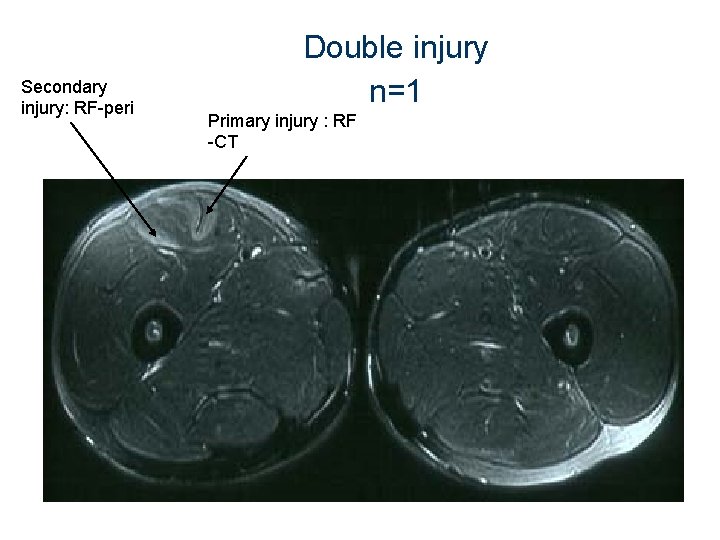
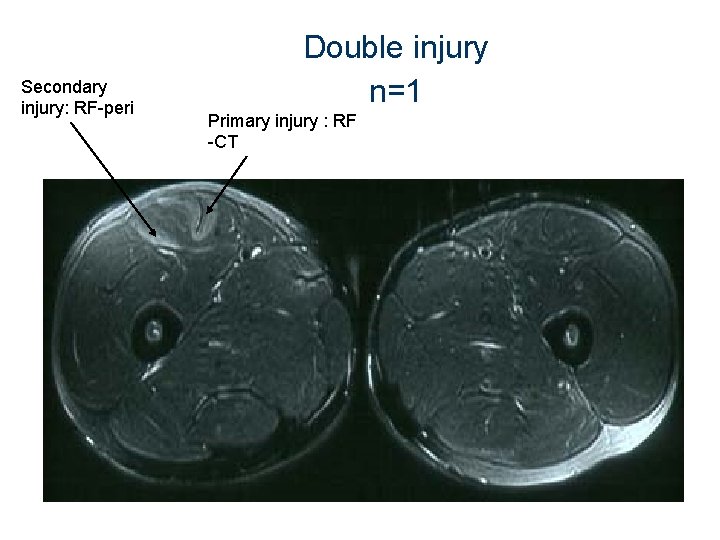
Secondary injury: RF-peri Double injury n=1 Primary injury : RF -CT
MRI “look-alikes” l l DOMS and muscle contusions: similar MRI appearance to muscle strain injuries Inclusion and exclusion criteria were strictly adhered to
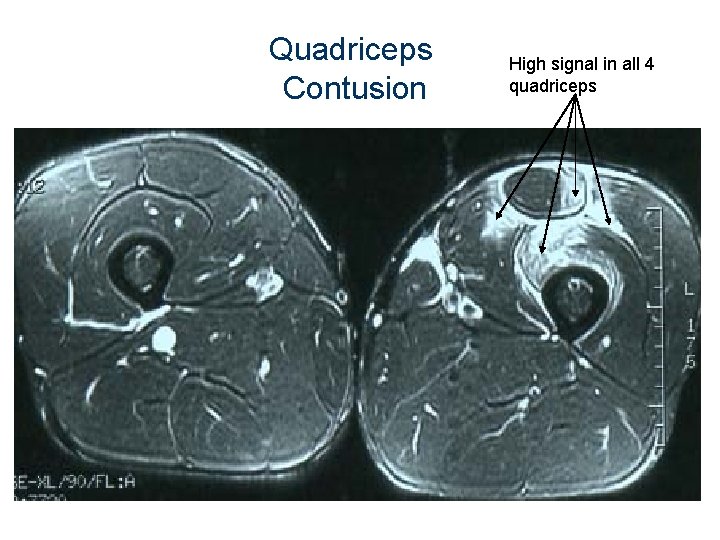
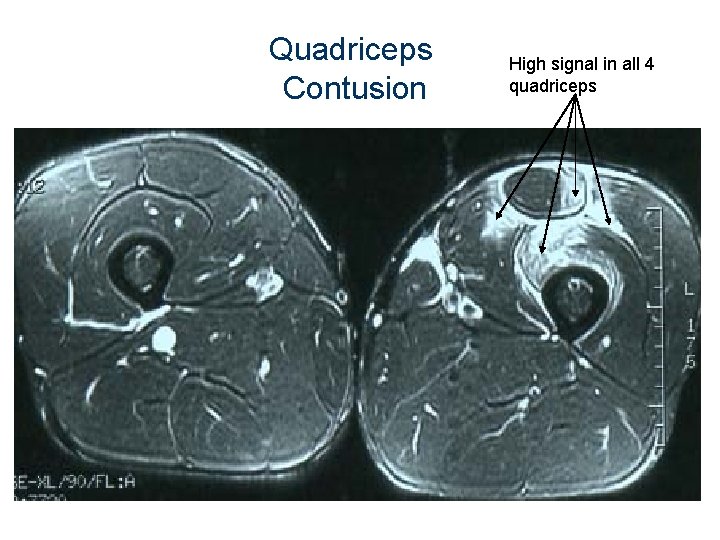
Quadriceps Contusion High signal in all 4 quadriceps
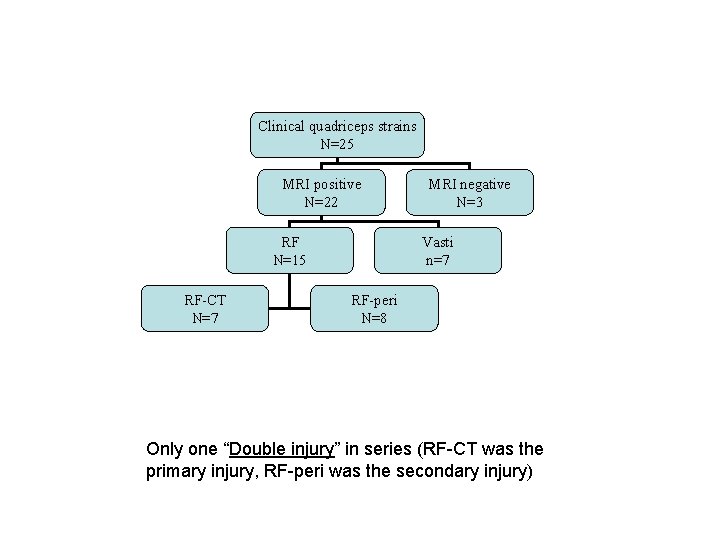
Clinical quadriceps strains N=25 MRI positive N=22 RF N=15 RF-CT N=7 MRI negative N=3 Vasti n=7 RF-peri N=8 Only one “Double injury” in series (RF-CT was the primary injury, RF-peri was the secondary injury)
Methods (rehabilitation phase) l No universally accepted rehabilitation regimen exists for muscle strain injuries
Methods (rehabilitation phase) Rehabilitation was standardised Phase 1 : Acute management l RICE/crutches first 48 hours l Intensive Physiotherapy • • • soft tissue therapy flexibility strengthening
Methods (rehabilitation phase) Phase 2: Remodeling phase l l Eligible to start running program when, l Full pain free ROM (prone knee flexion) l Complete 3 x 10 repetitions of single leg hops pain free 4 Stage running/kicking program (sport specific to ARF) was designed at beginning of study
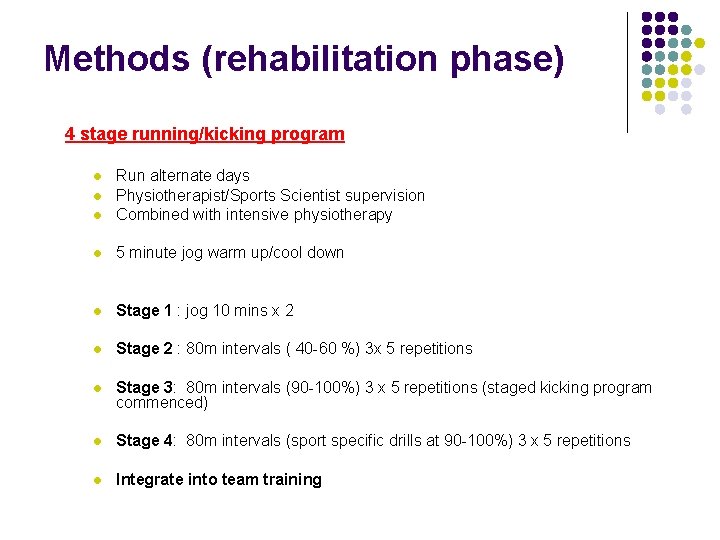
Methods (rehabilitation phase) 4 stage running/kicking program l Run alternate days Physiotherapist/Sports Scientist supervision Combined with intensive physiotherapy l 5 minute jog warm up/cool down l Stage 1 : jog 10 mins x 2 l Stage 2 : 80 m intervals ( 40 -60 %) 3 x 5 repetitions l Stage 3: 80 m intervals (90 -100%) 3 x 5 repetitions (staged kicking program commenced) l Stage 4: 80 m intervals (sport specific drills at 90 -100%) 3 x 5 repetitions l Integrate into team training l l
Methods (rehabilitation phase) 4 stage running/kicking programs • Some advanced rapidly • Others delayed by symptoms of high grade anterior thigh pain, weakness and dysfunction Decision to return to Full Training : Collaborative
Rehabilitation interval (RI) RI= time from the injury to the return to full training (measured in days)
4. Results & Discussion
Statistical analysis Statistician analyzed data § t-tests independent samples (dependent vs. independent variables) § Two-way analysis of variance
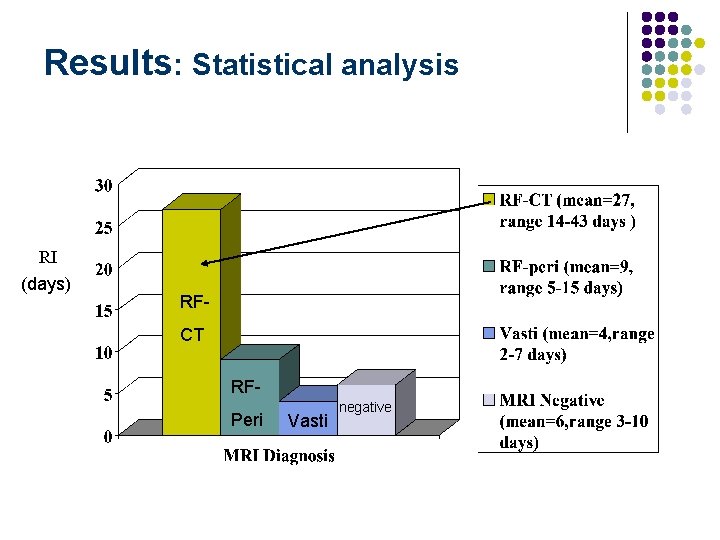
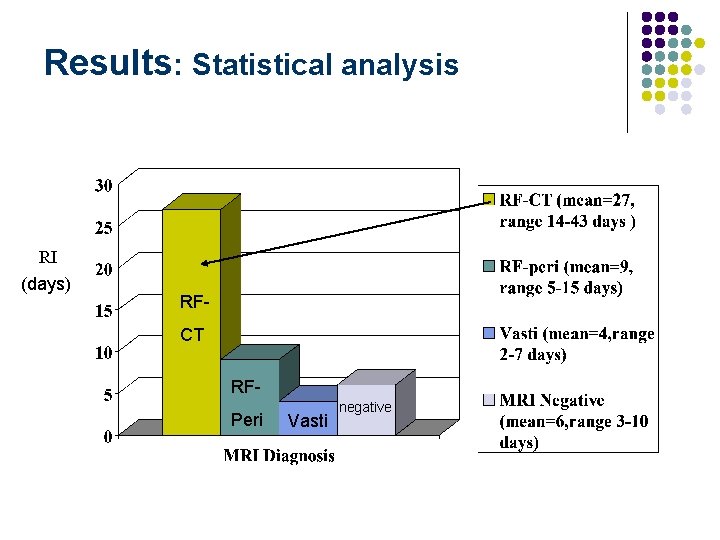
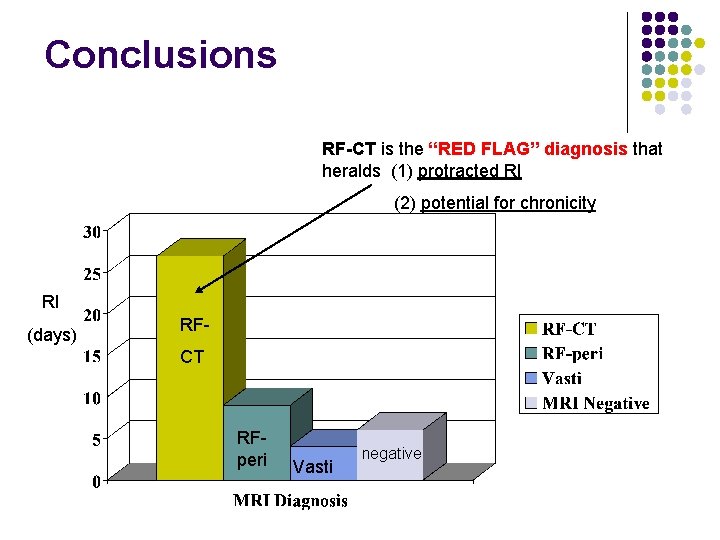
Results: Statistical analysis RI (days) RFCT RFPeri Vasti negative

RF-CT: “acute bull’s eye lesion” l n=7 l Mean RI=27 days l significantly longer RI (p=0. 001)
RF-CT: “acute bull’s eye lesion” Is the RED FLAG diagnosis that heralds a protracted rehabilitation
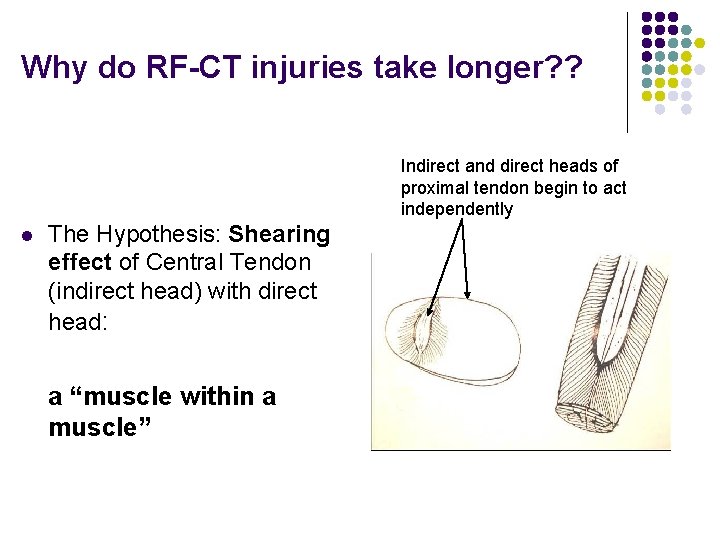
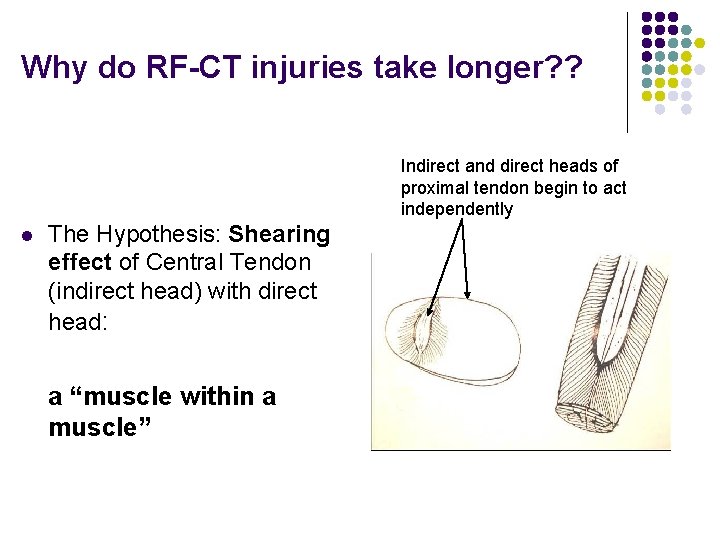
Why do RF-CT injuries take longer? ? Indirect and direct heads of proximal tendon begin to act independently l The Hypothesis: Shearing effect of Central Tendon (indirect head) with direct head: a “muscle within a muscle”
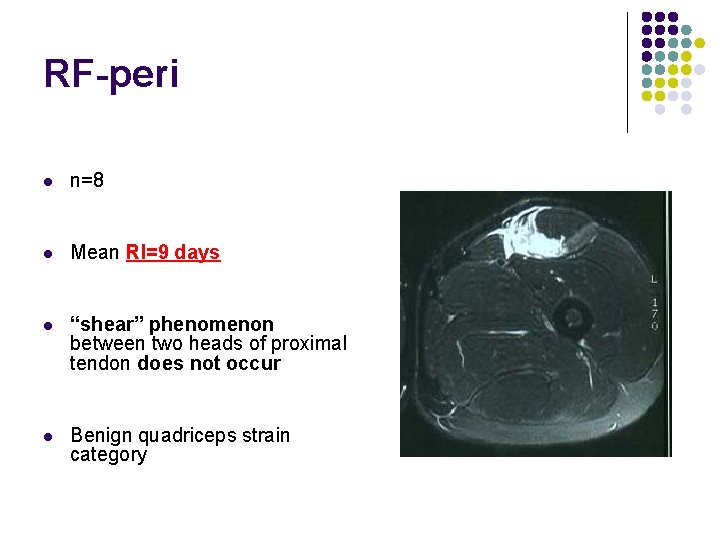
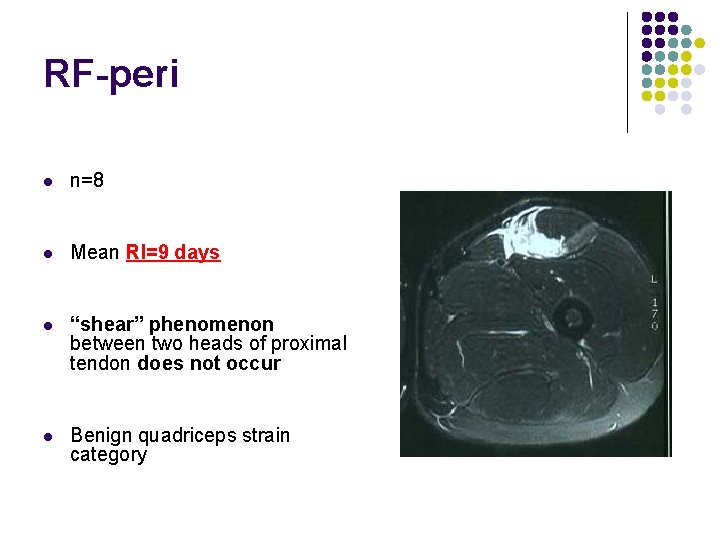
RF-peri l n=8 l Mean RI=9 days l “shear” phenomenon between two heads of proximal tendon does not occur l Benign quadriceps strain category
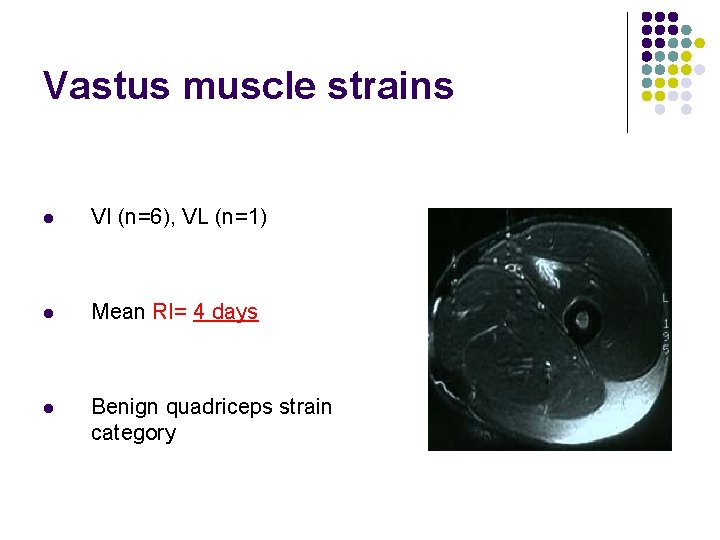
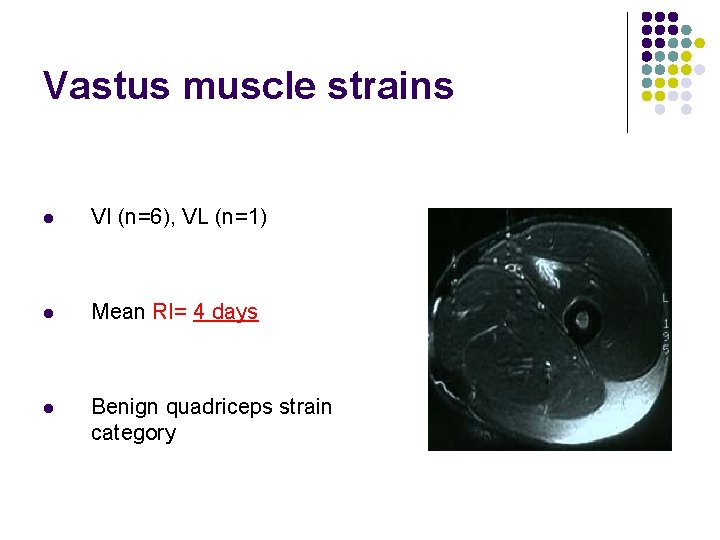
Vastus muscle strains l VI (n=6), VL (n=1) l Mean RI= 4 days l Benign quadriceps strain category
Vastus muscle strains l Hypothesis 1. Slow twitch muscle 2. Crosses only one joint 3. Large bulk of synergistic muscles
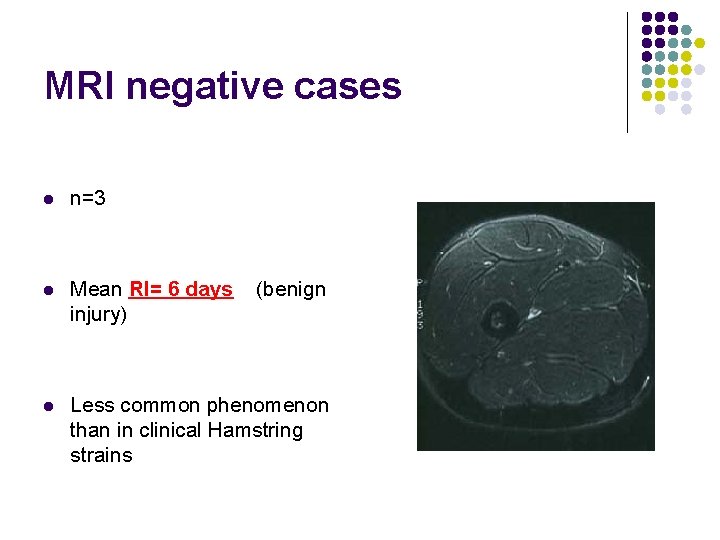
MRI negative cases l n=3 l Mean RI= 6 days injury) l Less common phenomenon than in clinical Hamstring strains (benign
MRI negative cases Hypotheses l MRI done too early l Strain injury too small to resolve l Pain mediated by neuro-meningeal structures (e. g. femoral nerve)
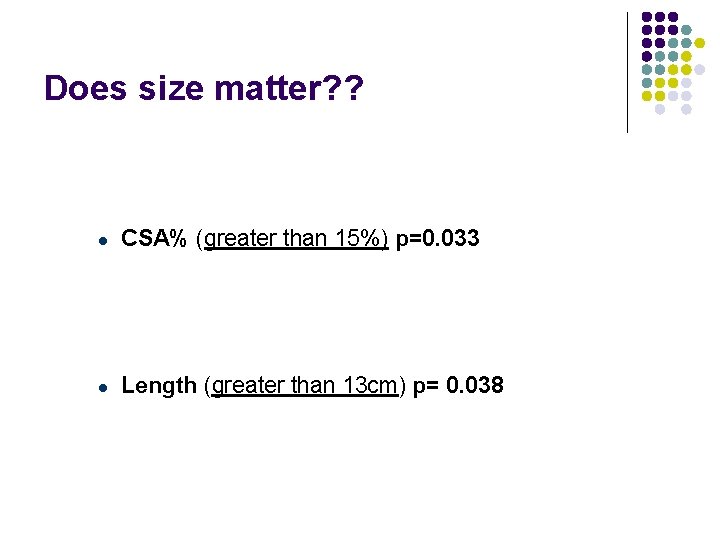
Does size matter? ? l CSA% (greater than 15%) p=0. 033 l Length (greater than 13 cm) p= 0. 038
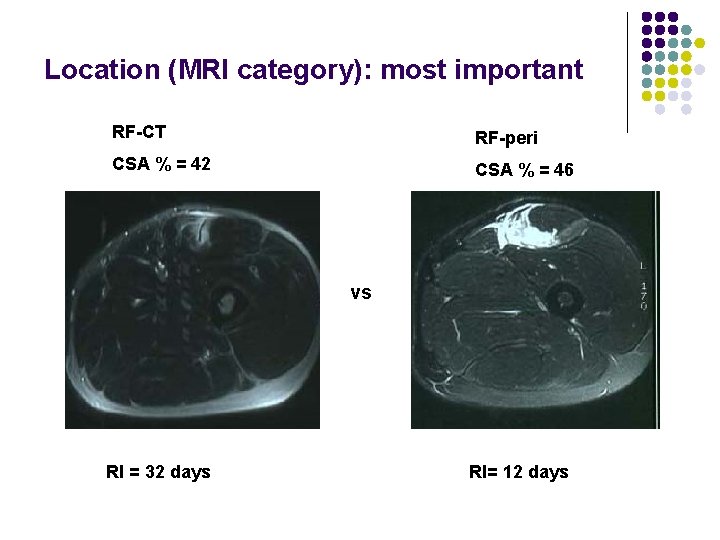
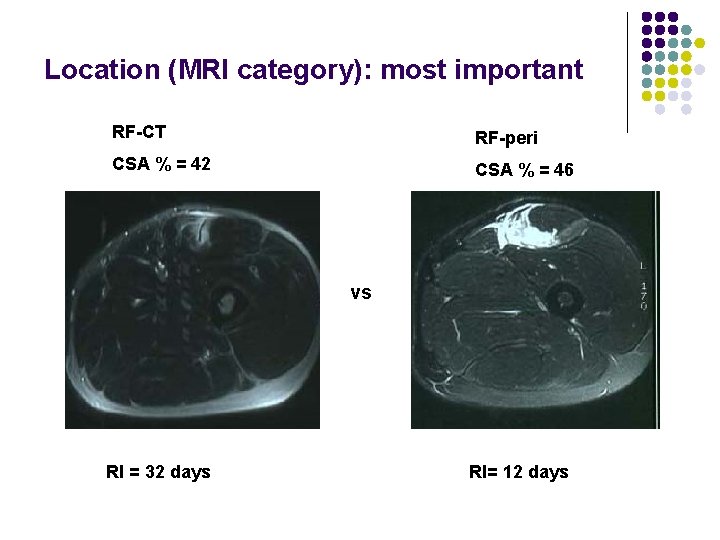
Location (MRI category): most important RF-CT RF-peri CSA % = 42 CSA % = 46 vs RI = 32 days RI= 12 days
Clinical evaluation l History (onset, mechanism, preferred kicking leg) is unhelpful l Examination- not analyzed
? ? Recurrent strains l No recurrences l 5 players had more than one quadriceps strain in the study period (different sites) l Why? l l One on one Physiotherapy Graded running/kicking program
Were any follow-up MRI done? l Yes l N=11 available for study • • l 4 out of interest when player considered rehabilitated 7 incidental Not routinely done, no statistical analysis
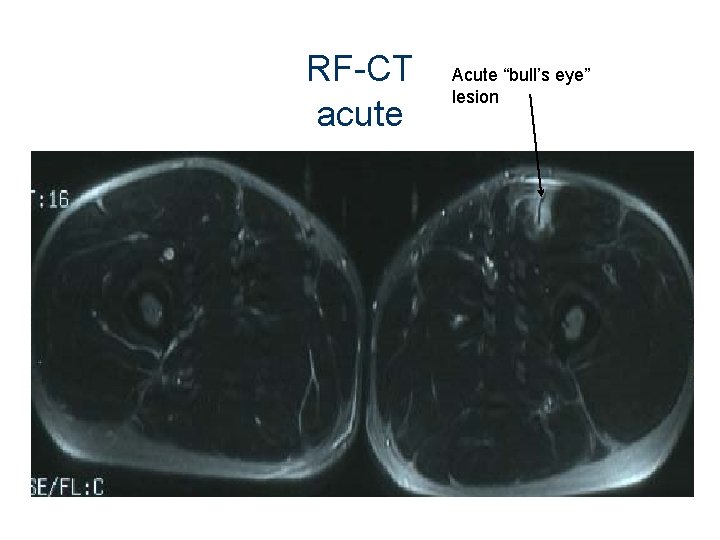
RF-CT acute Acute “bull’s eye” lesion
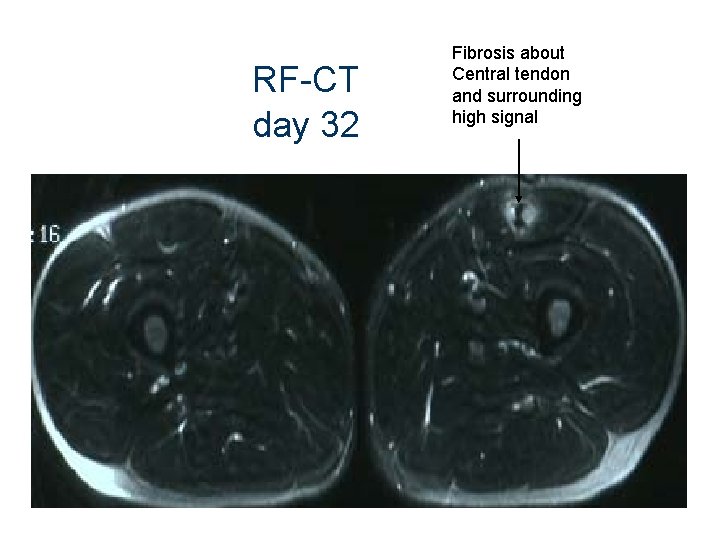
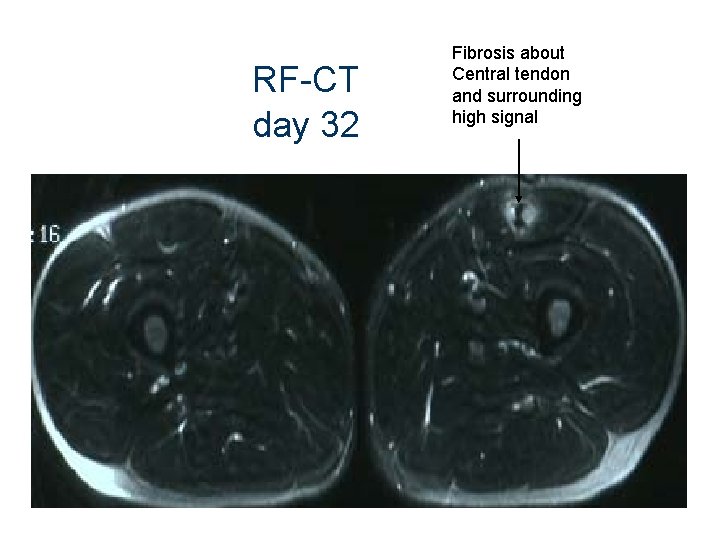
RF-CT day 32 Fibrosis about Central tendon and surrounding high signal
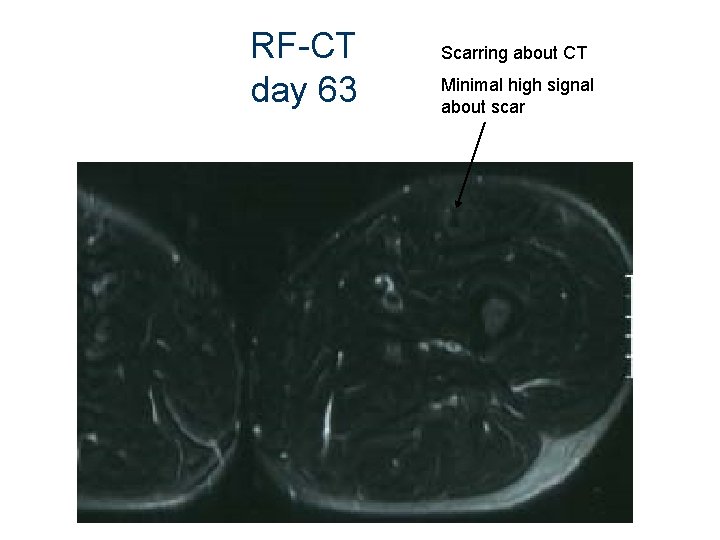
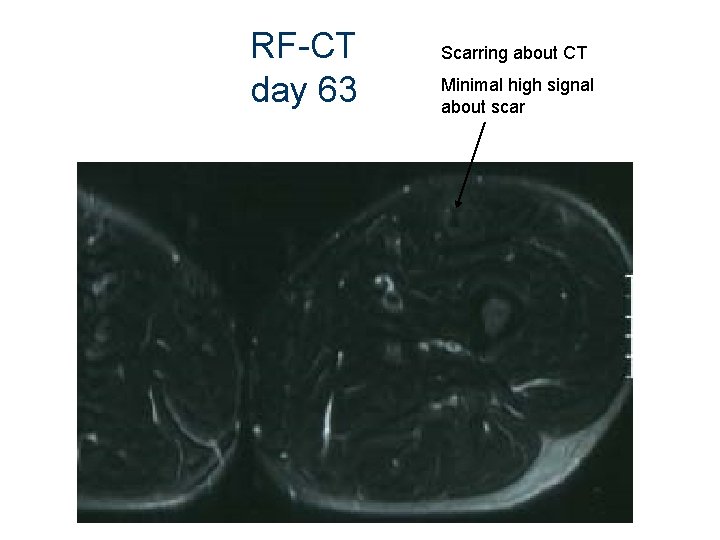
RF-CT day 63 Scarring about CT Minimal high signal about scar
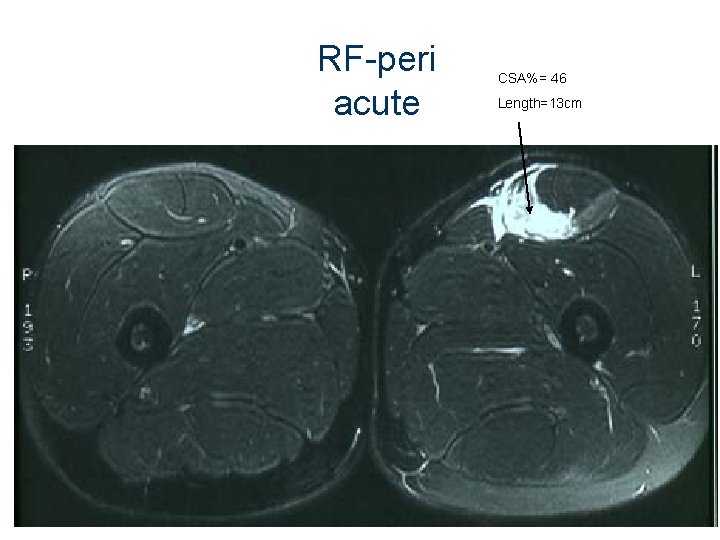
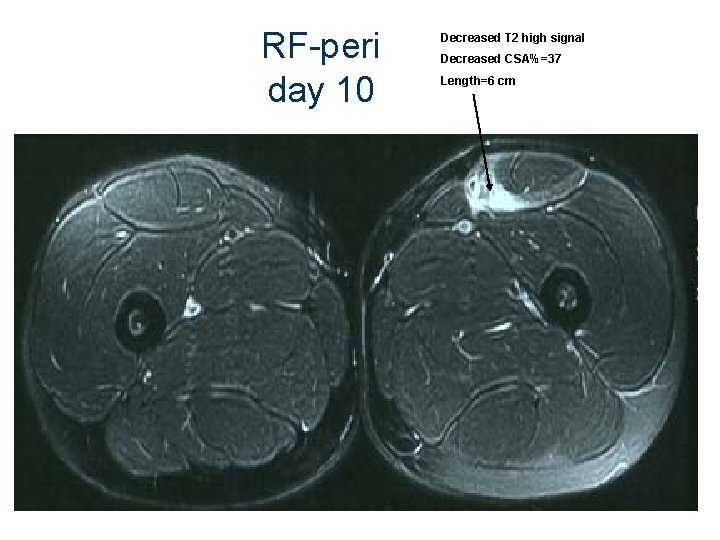
RF-peri acute CSA%= 46 Length=13 cm
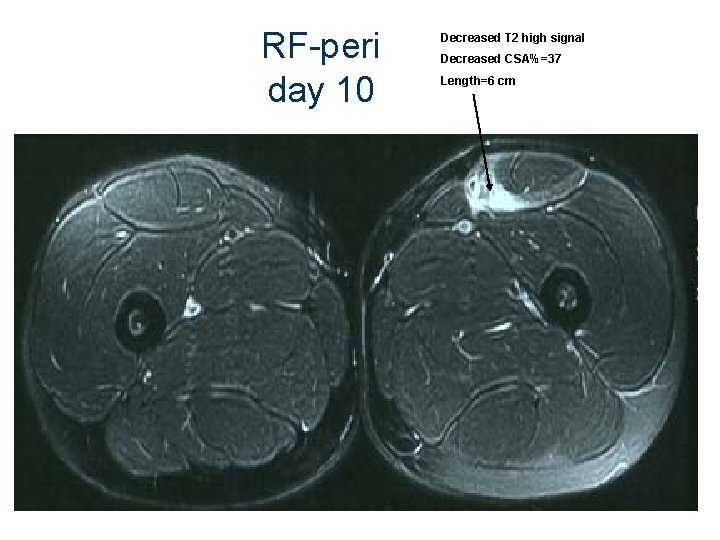
RF-peri day 10 Decreased T 2 high signal Decreased CSA%=37 Length=6 cm
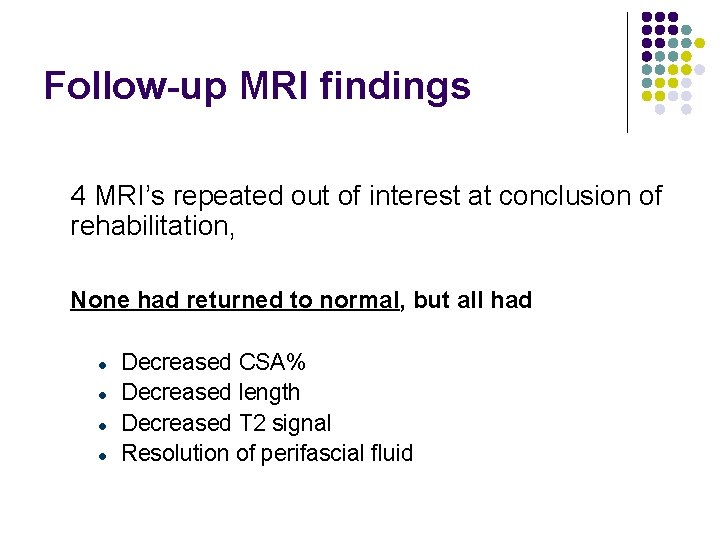
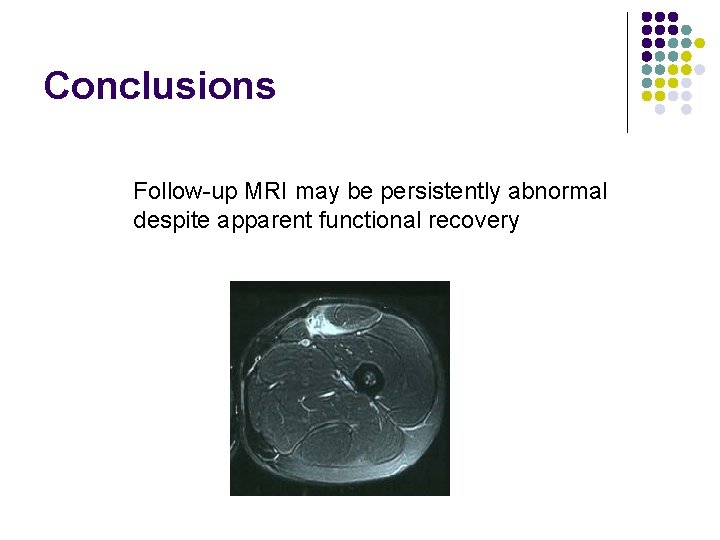
Follow-up MRI findings 4 MRI’s repeated out of interest at conclusion of rehabilitation, None had returned to normal, but all had l l Decreased CSA% Decreased length Decreased T 2 signal Resolution of perifascial fluid
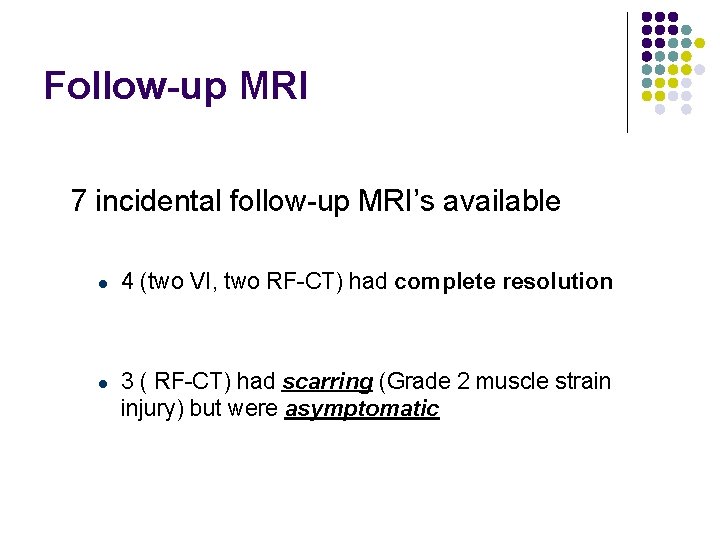
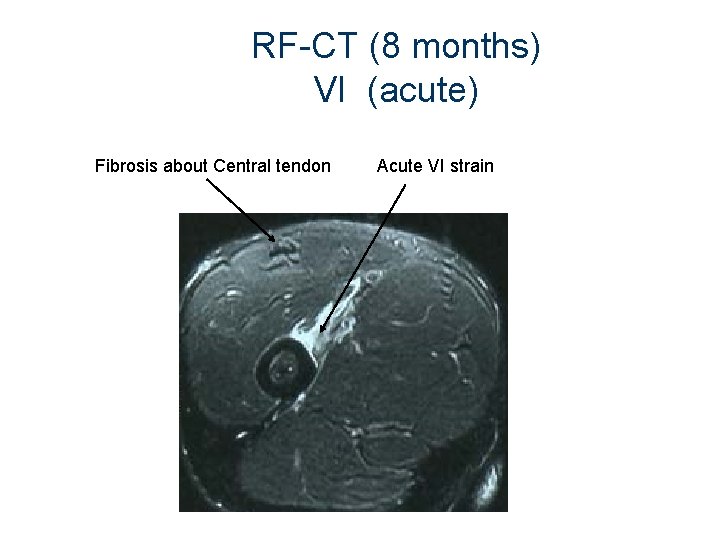
Follow-up MRI 7 incidental follow-up MRI’s available l l 4 (two VI, two RF-CT) had complete resolution 3 ( RF-CT) had scarring (Grade 2 muscle strain injury) but were asymptomatic
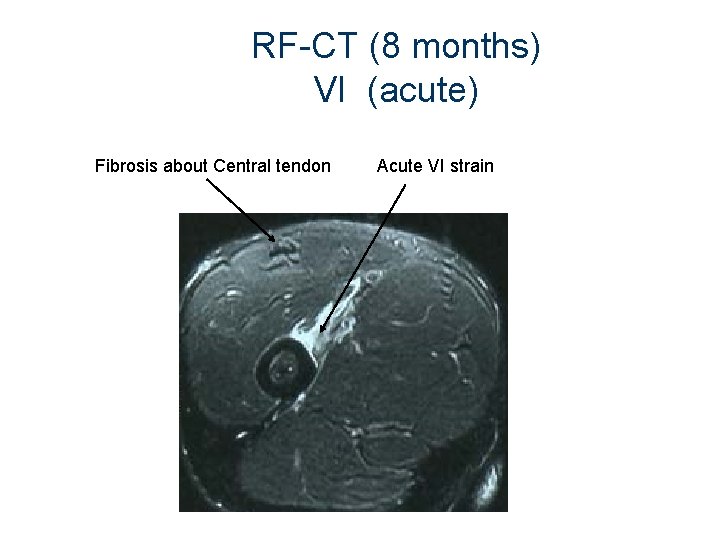
RF-CT (8 months) VI (acute) Fibrosis about Central tendon Acute VI strain
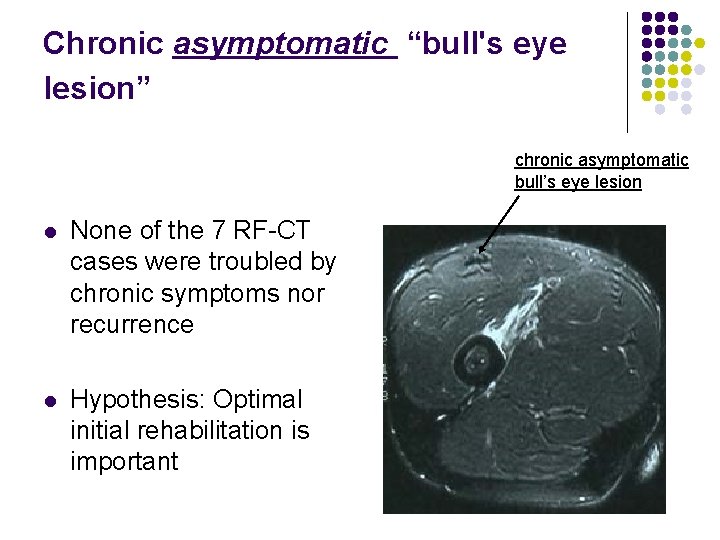
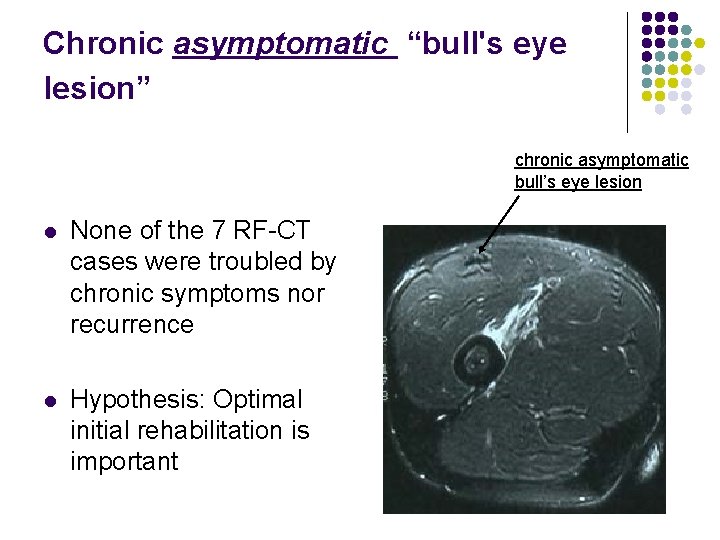
Chronic asymptomatic “bull's eye lesion” chronic asymptomatic bull’s eye lesion l None of the 7 RF-CT cases were troubled by chronic symptoms nor recurrence l Hypothesis: Optimal initial rehabilitation is important
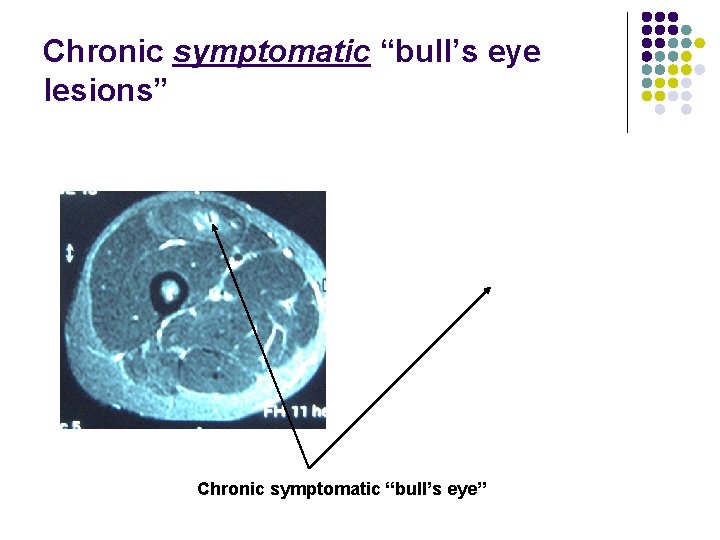
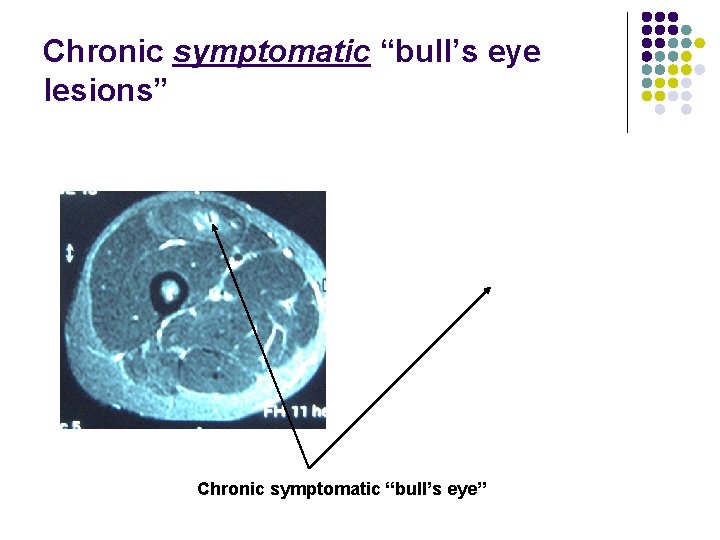
Chronic symptomatic “bull’s eye lesions” Chronic symptomatic “bull’s eye”

CONCLUSIONS
Conclusions MRI defines muscle strain injury objectively: “probe beneath the surface of the skin”
Conclusions All 22 MRI positive cases of muscle strain injury occurred about known muscle-tendon junctions (This concurs with basic science studies)
Conclusions The rectus femoris was the most commonly injured muscle (15/22 cases)
Conclusions Tenderness over the anterior thigh does not always = rectus femoris muscle strain (could be Vastus muscle strain or MRI negative)
Conclusions No cases of “distal rupture of RF”
Conclusions This research complements the research on chronic symptomatic RF-CT injuries regarding: 1. How acute RF-CT injuries may behave 2. How acute RF-CT injuries may look
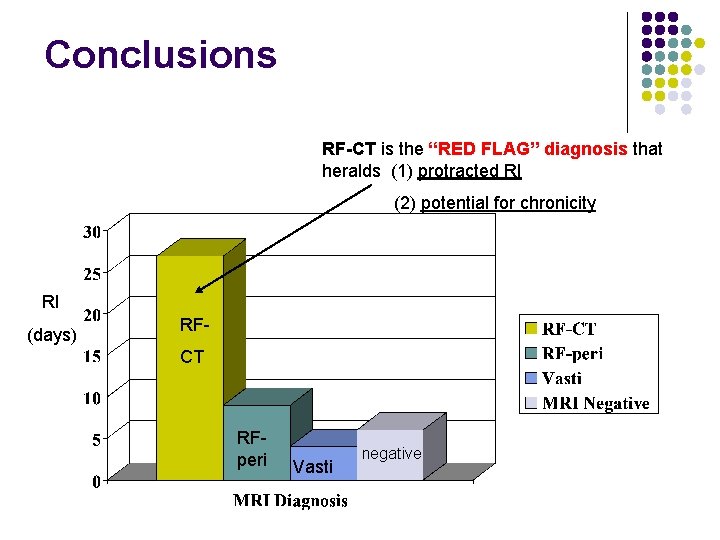
Conclusions RF-CT is the “RED FLAG” diagnosis that heralds (1) protracted RI (2) potential for chronicity RI (days) RFCT RFperi Vasti negative
Conclusions l Size ( CSA % and length) of muscle strain injury is also predictive of RI
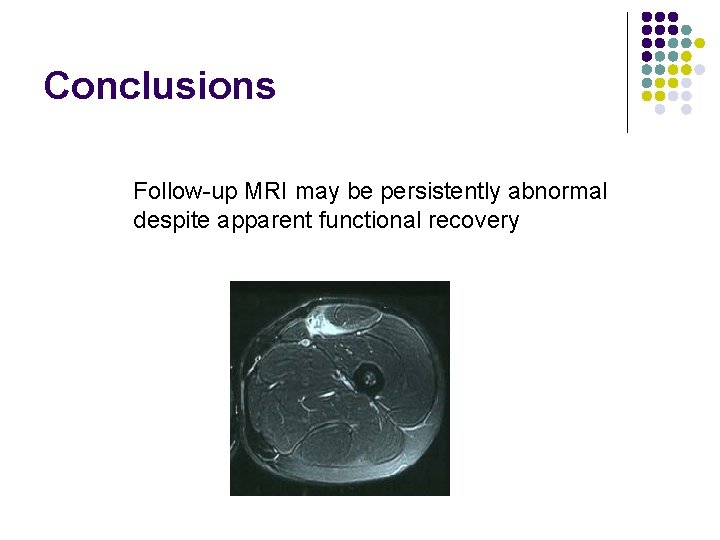
Conclusions Follow-up MRI may be persistently abnormal despite apparent functional recovery
Conclusions Indications for MRI Acute MRI for elite athletes Soccer World Cup 2002
e. g. Anterior thigh pain 7 days before Final Can he play? ? YES : if Benign MRI NO: if RF-CT (acute “bull’s eye)
Conclusions Indications for MRI If no MRI available? Suspect RF-CT if troubled by high grade anterior thigh pain in rehabilitation All athletes : consider MRI for chronic anterior thigh pain

Thank-you Questions?
 What are the greatest strains on walter and ruth's marriage
What are the greatest strains on walter and ruth's marriage Sprains and strains
Sprains and strains Pure shear
Pure shear Gracilis muscle mri
Gracilis muscle mri Orleans hanna algebra prognosis test
Orleans hanna algebra prognosis test Ejemplos de prognosis en trabajo social
Ejemplos de prognosis en trabajo social Ich score prognosis
Ich score prognosis Helllp syndrome
Helllp syndrome Autism prognosis
Autism prognosis Splinter skills
Splinter skills Autism prognosis
Autism prognosis Kanner syndrome
Kanner syndrome Autism prognosis
Autism prognosis Static-99
Static-99 What is prognosis
What is prognosis Prognosis
Prognosis Child-pugh score prognosis
Child-pugh score prognosis Cholangitis prognosis
Cholangitis prognosis Good prognosis
Good prognosis Prognosis of cystic fibrosis
Prognosis of cystic fibrosis Pyloric adenoma
Pyloric adenoma Good prognosis
Good prognosis Acute cholecystitis clinical features
Acute cholecystitis clinical features Acute inflammation
Acute inflammation Periodontitis acuta serosa
Periodontitis acuta serosa Obliques muscles
Obliques muscles Biceps triceps and quadriceps
Biceps triceps and quadriceps Refractory period cardiac
Refractory period cardiac What muscle fibers run in circles around your eye
What muscle fibers run in circles around your eye Qceps
Qceps Leg muscles
Leg muscles M. sartorius origo insertio
M. sartorius origo insertio Atteches
Atteches Quadriceps kası
Quadriceps kası Lumbal ekstansör ne demek
Lumbal ekstansör ne demek Pp
Pp Quadriceps femoris group of muscles
Quadriceps femoris group of muscles Isquiocrural
Isquiocrural Supracrestal plane
Supracrestal plane Sidération quadriceps
Sidération quadriceps Weak quadriceps
Weak quadriceps Policeman tip hand
Policeman tip hand Quadriceps femoral
Quadriceps femoral Quadriceps knee flexion
Quadriceps knee flexion Relaksasyon egzersizleri
Relaksasyon egzersizleri Subkutan enjeksiyon
Subkutan enjeksiyon Gait
Gait Determinants of gait
Determinants of gait Features of smooth muscle
Features of smooth muscle Mri surf2surf
Mri surf2surf Gp mri indications
Gp mri indications Ax t2 propeller mri
Ax t2 propeller mri Mri image formation
Mri image formation Type 1 acromion
Type 1 acromion How mri works
How mri works Mri hydrogen atoms
Mri hydrogen atoms Fourier transform mri
Fourier transform mri Translate
Translate Hoglund brain imaging center
Hoglund brain imaging center Function of putamen
Function of putamen Mri energy consumption
Mri energy consumption Haghighat mri center
Haghighat mri center Nomics mri
Nomics mri Pregnancy mri
Pregnancy mri Mamdouh mahfouz
Mamdouh mahfouz First mri image 1973
First mri image 1973 Bingabr
Bingabr Mri ap psychology
Mri ap psychology First mri image 1973
First mri image 1973 Vertical mri
Vertical mri Cerebellum ct anatomy
Cerebellum ct anatomy Entry slice phenomenon mri
Entry slice phenomenon mri Foramen rotundum ct
Foramen rotundum ct Mri k space
Mri k space Block imaging
Block imaging Angular momentum mri
Angular momentum mri Atriclip mri safety
Atriclip mri safety Mri scanner
Mri scanner Scan image to text
Scan image to text Mri scanner
Mri scanner Gp mri indications
Gp mri indications Disadvantage of mri
Disadvantage of mri Nmr kolena
Nmr kolena Mri scanner
Mri scanner Fgatir ge mri
Fgatir ge mri Mri question
Mri question Siemens mri safety video
Siemens mri safety video Romberg test positive causes
Romberg test positive causes Dr zsigmond ildikó
Dr zsigmond ildikó Nsf mri
Nsf mri Andy rekito
Andy rekito Cnr mri
Cnr mri Cnr mri
Cnr mri Mri brain
Mri brain Mri safety signage
Mri safety signage Unwarping turners
Unwarping turners Advances in mri
Advances in mri Mri scoliosis protocol
Mri scoliosis protocol Mri safety
Mri safety Mri
Mri Mri
Mri Nmv mri
Nmv mri Carasil mri
Carasil mri