Acute peritonitis with or without abscess Definition Inflammation
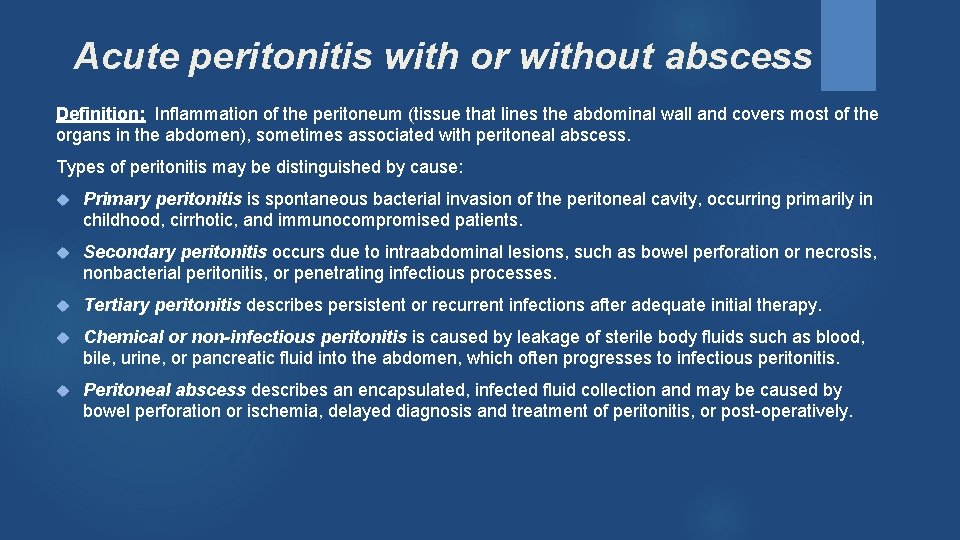
Acute peritonitis with or without abscess Definition: Inflammation of the peritoneum (tissue that lines the abdominal wall and covers most of the organs in the abdomen), sometimes associated with peritoneal abscess. Types of peritonitis may be distinguished by cause: Primary peritonitis is spontaneous bacterial invasion of the peritoneal cavity, occurring primarily in childhood, cirrhotic, and immunocompromised patients. Secondary peritonitis occurs due to intraabdominal lesions, such as bowel perforation or necrosis, nonbacterial peritonitis, or penetrating infectious processes. Tertiary peritonitis describes persistent or recurrent infections after adequate initial therapy. Chemical or non-infectious peritonitis is caused by leakage of sterile body fluids such as blood, bile, urine, or pancreatic fluid into the abdomen, which often progresses to infectious peritonitis. Peritoneal abscess describes an encapsulated, infected fluid collection and may be caused by bowel perforation or ischemia, delayed diagnosis and treatment of peritonitis, or post-operatively.

Acute peritonitis with or without abscess Clinical Indicators Abdominal pain or tenderness Bloating or distention of the abdomen, Guarding / Rebound tenderness on exam. Rigidity, Nausea and vomiting Fever Inability to pass stool or gas or Diarrhea fatigue. Low urine output Nausea and vomiting Thirst Treatment: Antibiotics – the type and duration of antibiotic therapy depends on the severity of the condition and the kind of peritonitis. Surgery – may be warranted to remove infected tissue, treat the underlying cause of the infection, and prevent the infection from spreading, especially if peritonitis is due to a ruptured appendix, stomach, or colon. Other treatments – depending on signs and symptoms, treatment while in the hospital may include pain medications, IV fluids, supplemental oxygen, and in some cases a blood transfusion.

Acute peritonitis with or without abscess Documentation Tips: ü Acute peritonitis should be documented when your patient has the clinical manifestations and a cause for peritoneal inflammation. ü Include a “DUE TO” link to the etiologies to include a ruptured appendix, perforated colon, gastric ulcer or bile leak, diverticulitis, pancreatitis, or trauma, etc. ü If there is an associated abscess, DO NOT forget to document "peritoneal abscess. ” ü If one is uncertain as to the etiology of the peritonitis, it is acceptable and encouraged to use terms such as “probable, ” “possible, ” or “suspected, ” etc. to describe this diagnosis (or any other diagnosis). To qualify, these terms must end up in the discharge summary, so attaching them to the diagnosis in the detail section of the problem list is very important.

Acute peritonitis with or without abscess Documentation Tips: ü If the patient’s presentation of symptoms are that of a systemic response of the infection, consider sepsis. ü Document all co-morbid conditions treated during this hospitalization. ü Include the “DUE TO” to link the causal condition. ü Even if cultures are negative, remember that your suspicion of the causative organism should be documented based on the history, clinical presentation and your choice of antibiotics. ü Coders can only code what is written and MUST follow coding guidelines. ü Coders can not interpret abnormal lab or x-ray findings or assume a link if the physician does not document it. Telling the clinical truth will lead to accurate coding and appropriate risk-adjusted scores will follow. Think in ink!
- Slides: 4