ACUTE PANCREATITIS Dr Chirag Patel CLINICAL DEFINITION Acute

- Slides: 33
ACUTE PANCREATITIS Dr. Chirag Patel
CLINICAL DEFINITION Acute condition presenting with abdominal pain raised with blood and pancreatic enzymes as results of pancreatic inflammation PATHOLOGICAL DEFINITION Reversible pancreatic parenchymal injury associated with inflammation If underlying cause removed, no functional or morphological loss of gland If recurrent attack- chronic pancreatitis associated with irreversible injury
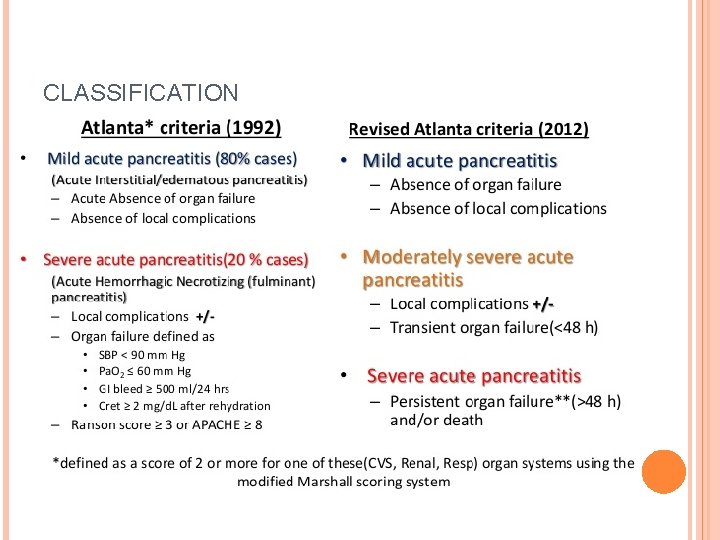
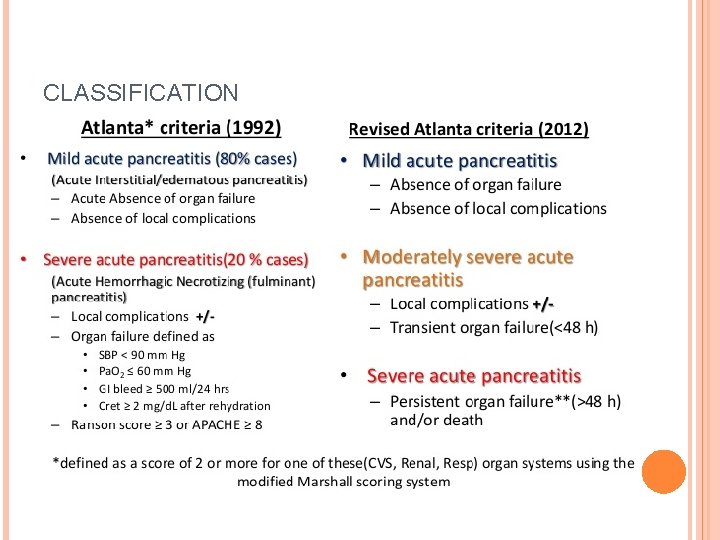
CLASSIFICATION
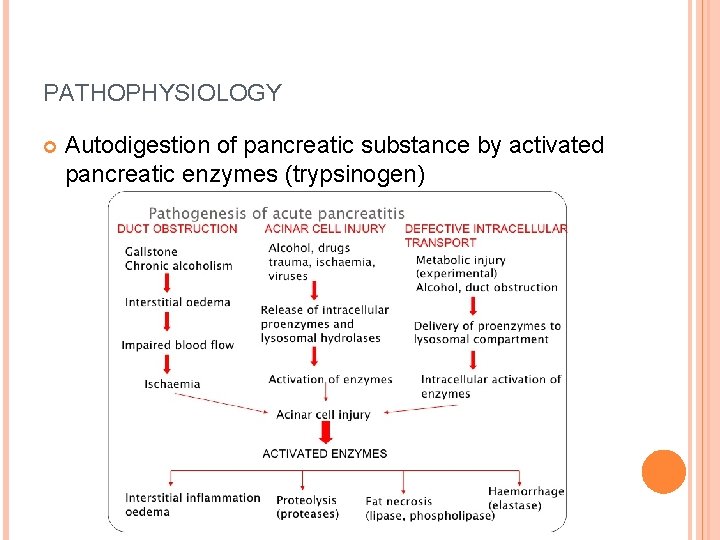
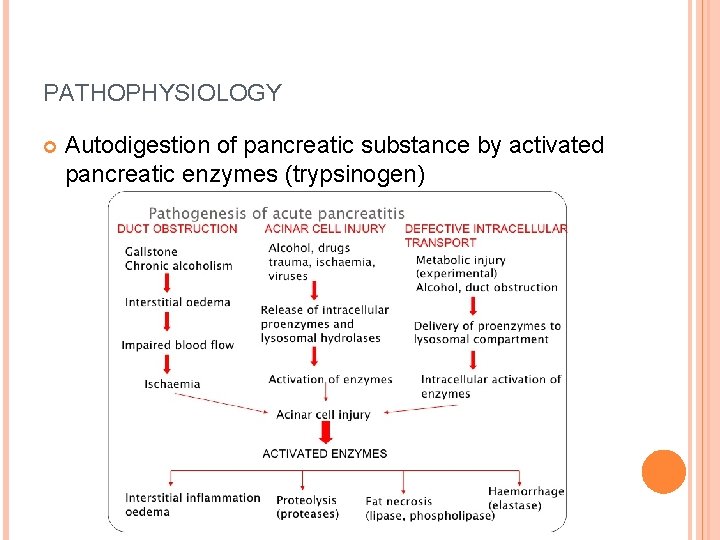
PATHOPHYSIOLOGY Autodigestion of pancreatic substance by activated pancreatic enzymes (trypsinogen)
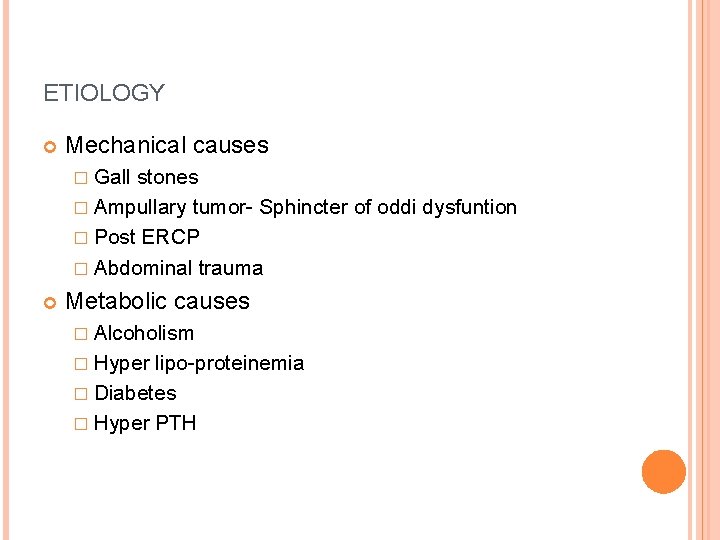
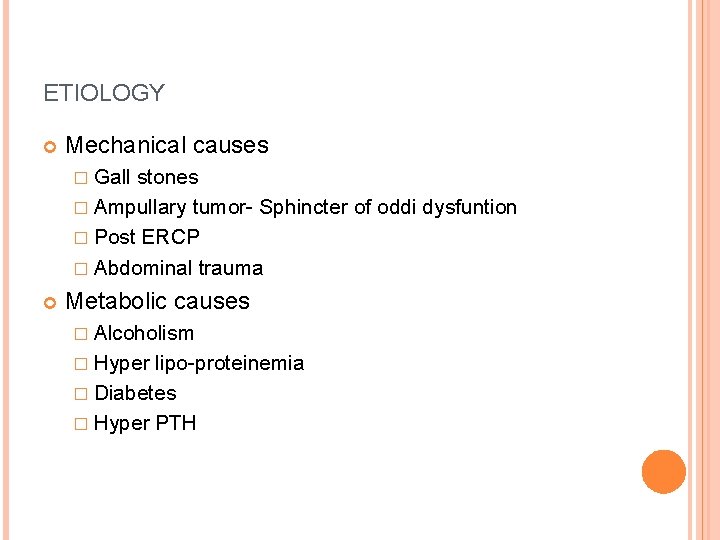
ETIOLOGY Mechanical causes � Gall stones � Ampullary tumor- Sphincter of oddi dysfuntion � Post ERCP � Abdominal trauma Metabolic causes � Alcoholism � Hyper lipo-proteinemia � Diabetes � Hyper PTH
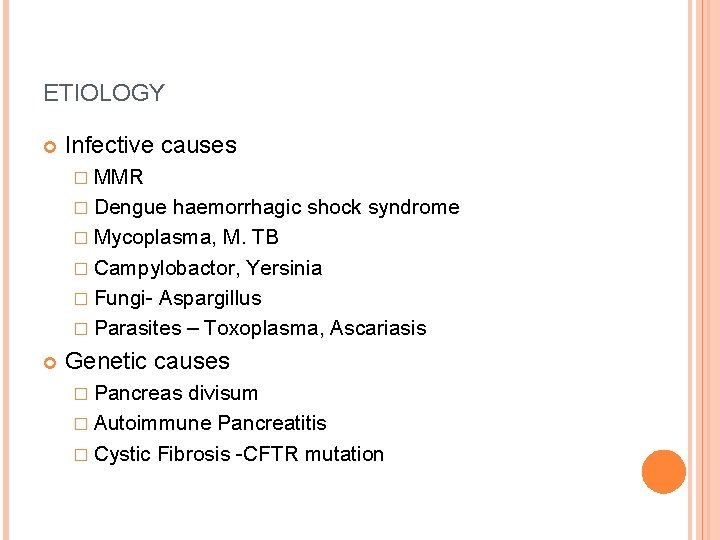
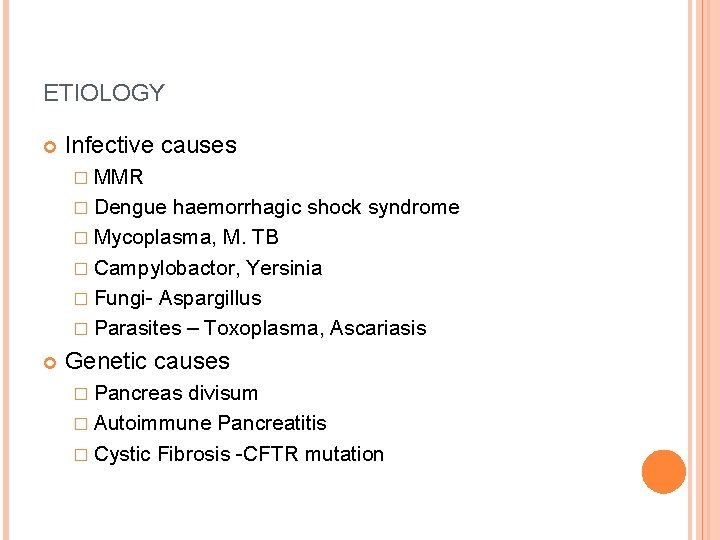
ETIOLOGY Infective causes � MMR � Dengue haemorrhagic shock syndrome � Mycoplasma, M. TB � Campylobactor, Yersinia � Fungi- Aspargillus � Parasites – Toxoplasma, Ascariasis Genetic causes � Pancreas divisum � Autoimmune Pancreatitis � Cystic Fibrosis -CFTR mutation
ETIOLOGY Vascular Causes � Shock � Hypothermia � Athero-embolism � Vasculitis
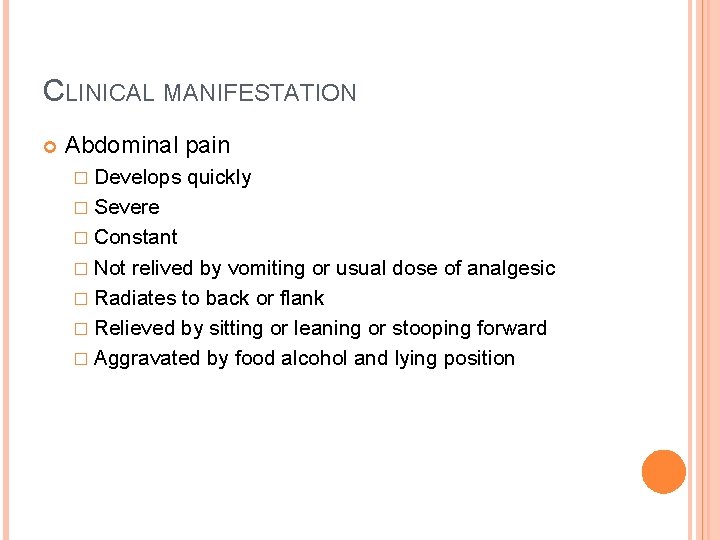
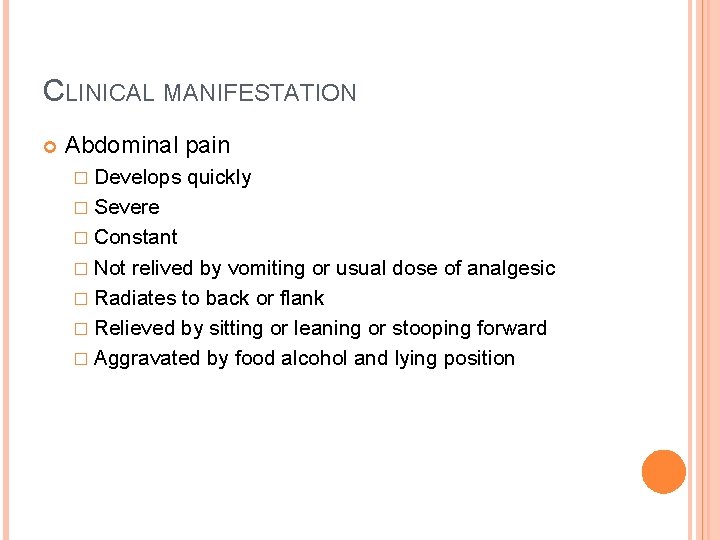
CLINICAL MANIFESTATION Abdominal pain � Develops quickly � Severe � Constant � Not relived by vomiting or usual dose of analgesic � Radiates to back or flank � Relieved by sitting or leaning or stooping forward � Aggravated by food alcohol and lying position
CLINICAL MANIFESTATION Nausea Due to reflex pylorospasm Vomiting and intense necrotizing Anorexia pancreatitis Diarrhoea Hiccups due to Gastric distension Low grade fever Poly Arthritis
PHYSICAL EXAMINATION Tachyapnea Tachycardia Hypotension Pyrexia/ fever Icterus – due to gall stone pancreatitis Cyanosis Pallor, cold clammy skin
ABDOMINAL EXAMINATION Tenderness in upper abdomen Abdominal distension Grey turner’s signs � Haemorrhagic spots/ ecchymosis in flanks Cullen’s sign � Bluish discoloration around umbilicus
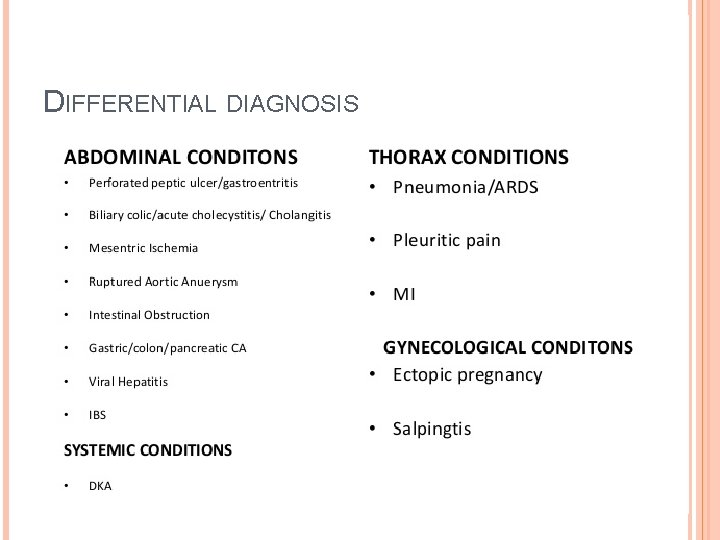
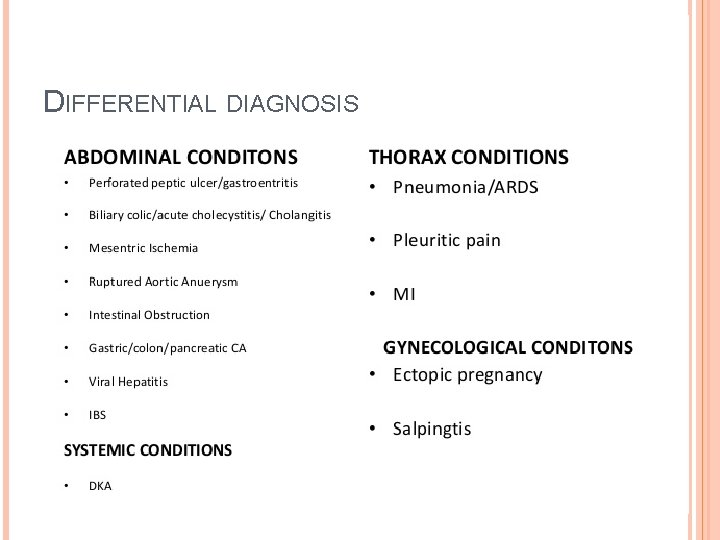
DIFFERENTIAL DIAGNOSIS
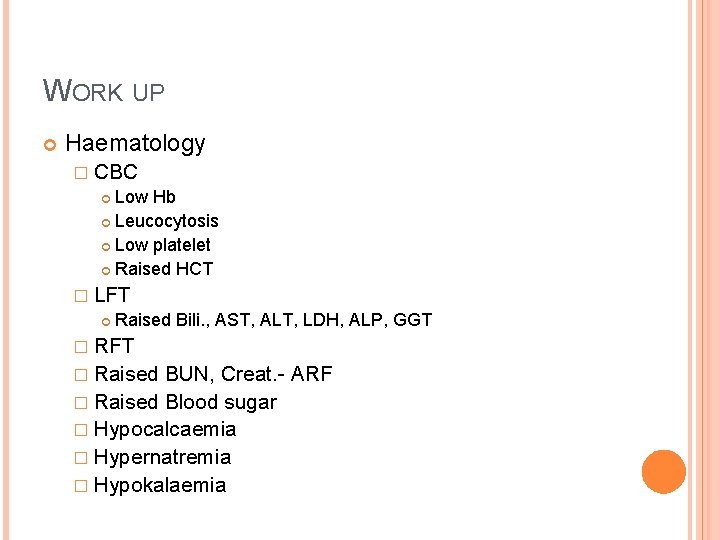
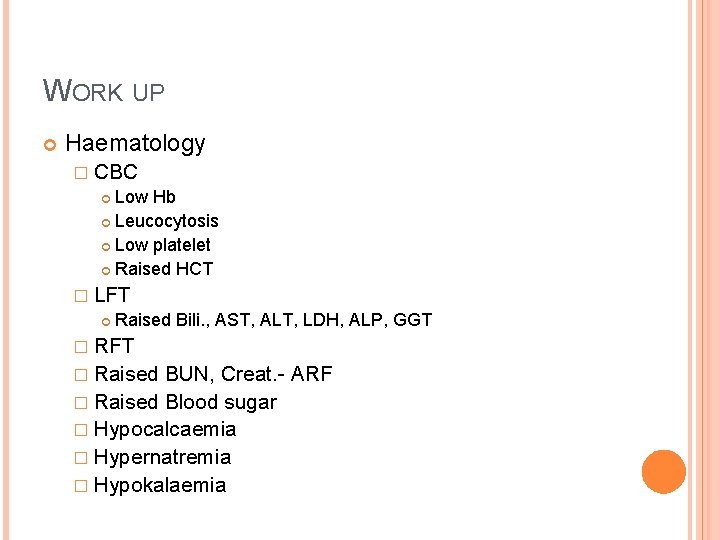
WORK UP Haematology � CBC Low Hb Leucocytosis Low platelet Raised HCT � LFT Raised Bili. , AST, ALT, LDH, ALP, GGT � RFT � Raised BUN, Creat. - ARF � Raised Blood sugar � Hypocalcaemia � Hypernatremia � Hypokalaemia
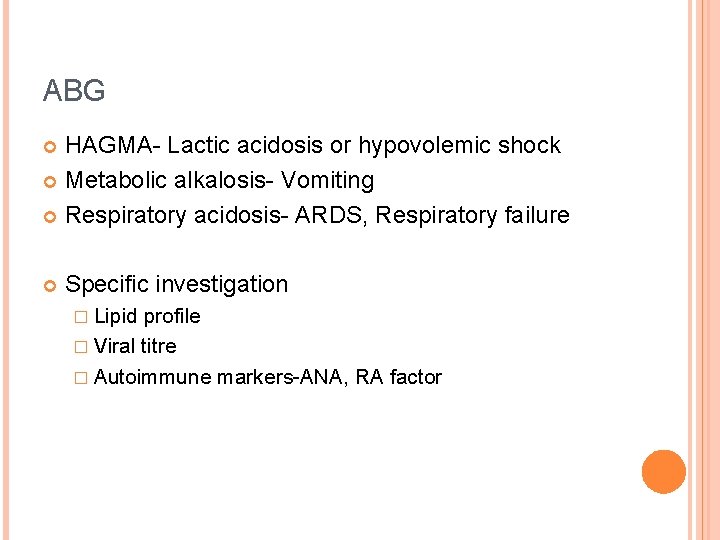
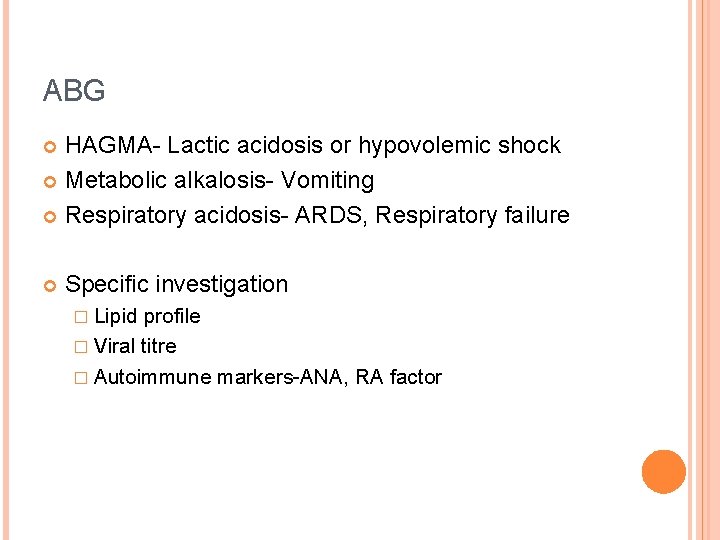
ABG HAGMA- Lactic acidosis or hypovolemic shock Metabolic alkalosis- Vomiting Respiratory acidosis- ARDS, Respiratory failure Specific investigation � Lipid profile � Viral titre � Autoimmune markers-ANA, RA factor
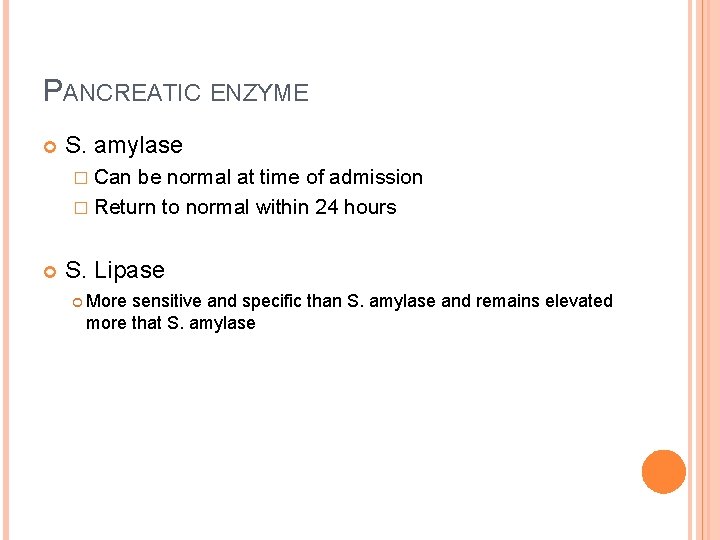
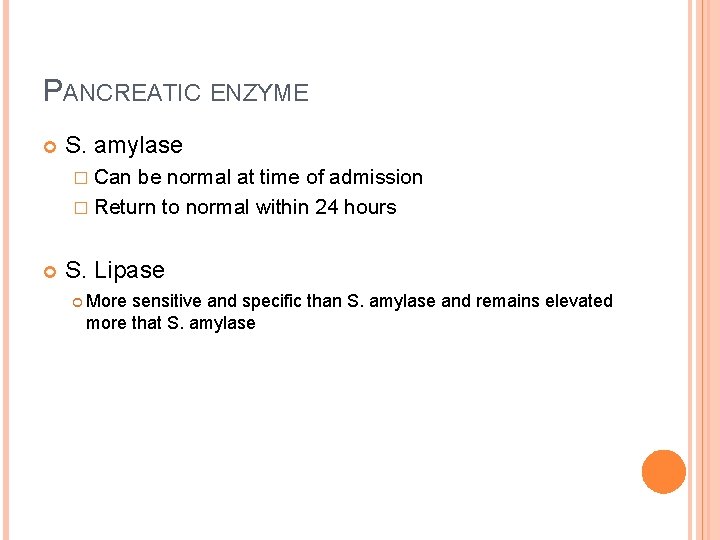
PANCREATIC ENZYME S. amylase � Can be normal at time of admission � Return to normal within 24 hours S. Lipase More sensitive and specific than S. amylase and remains elevated more that S. amylase
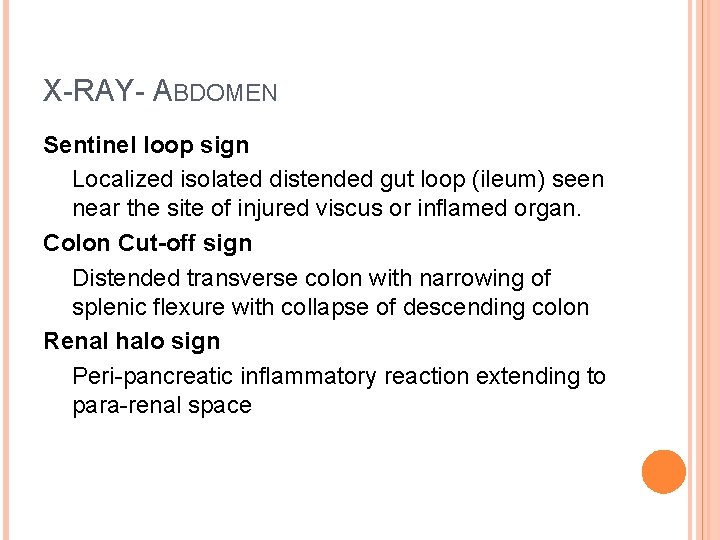
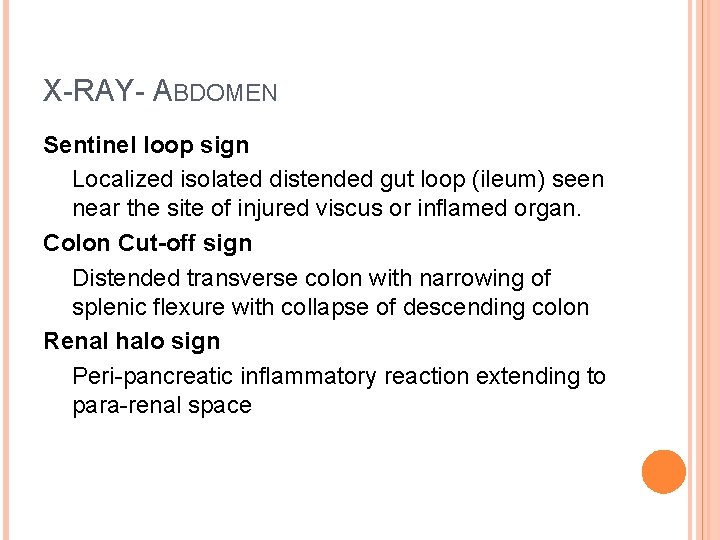
X-RAY- ABDOMEN Sentinel loop sign Localized isolated distended gut loop (ileum) seen near the site of injured viscus or inflamed organ. Colon Cut-off sign Distended transverse colon with narrowing of splenic flexure with collapse of descending colon Renal halo sign Peri-pancreatic inflammatory reaction extending to para-renal space
USG ABDOMEN Performed within 24 hours in all Pts to Detect gall stone R/O acute cholesystitis Dilated CBD DEMERIT- Overlying gas shadows 2 nd to bowel dystension Therapeutic � USG guided aspiration for C/S and pig tail cath. insertion
IV CONTRAST ENHANCED CT SCAN 90% Sensitivity and Specificity Indicated in � Diagnostic uncertainty � Severe Acute Pancreatitis � Systemic complications � Localized complications � Not improving Pt. condition after 72 hr. with initial treatment � Assessed prognosis � CT guided aspiration
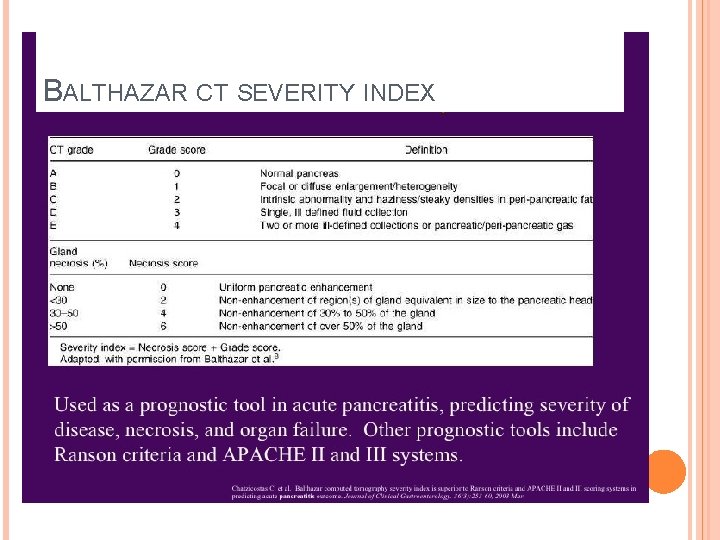
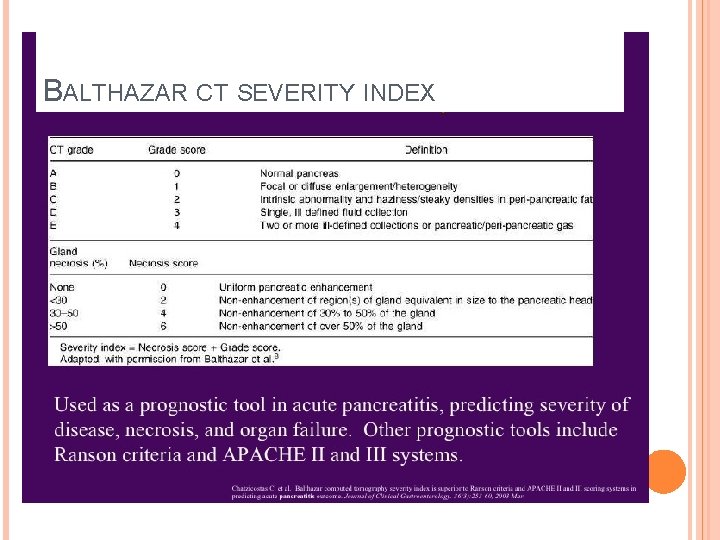
BALTHAZAR CT SEVERITY INDEX
MRI Alternative to CT, in Pts with � Renal insufficiency � Pregnancy � Contrast allergy
MRCP Diagnosis of suspected biliary or pancreatic duct obstruction Repeated attacks of AP Non-invasive, fast, safe and high quality image
ERCP Indicated in severe gall stone AP or acute cholangitis/ biliary obstruction ERCP within 24 -75 hrs of admission Sphincterotomy/ stent placement Not indicated in gall stone pancreatitis who do not have lab. Or clinical evidence of biliary obstruction Associated with Post ERCP pancreatitis
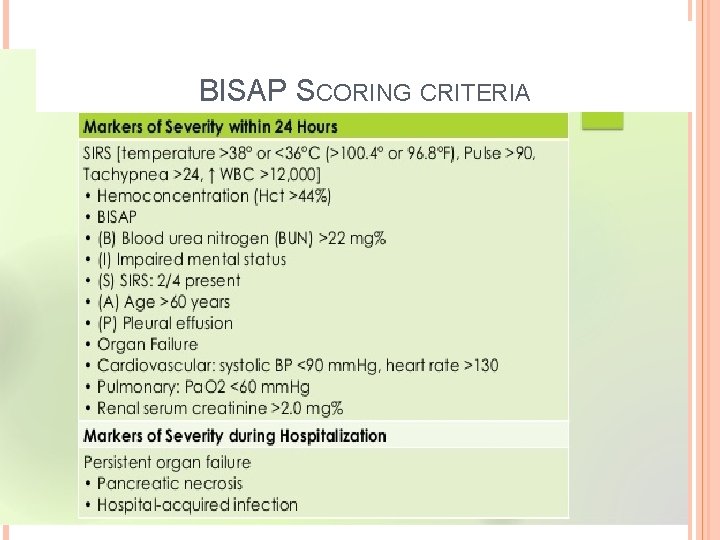
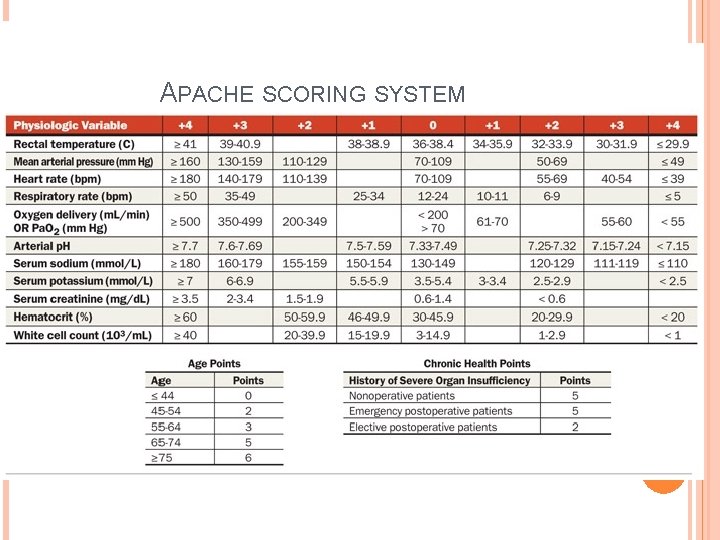
SEVERITY SCORING SYSTEM Ranson score BISAP score Glasgow Imrie score APACHE II Score SOFA Score
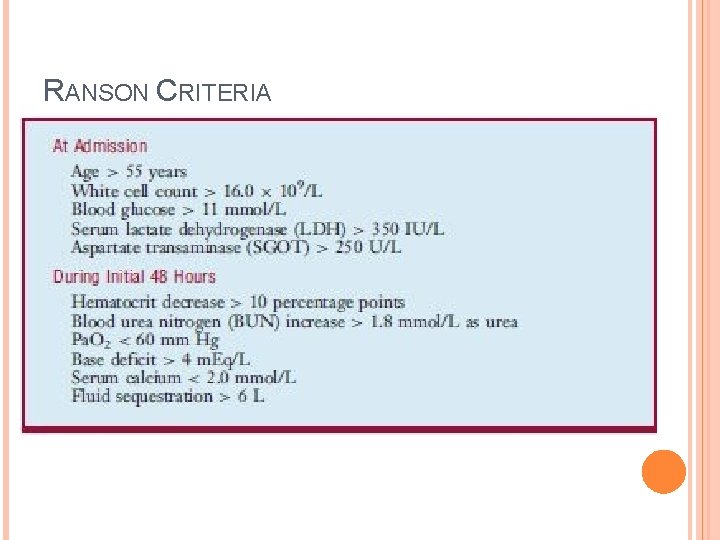
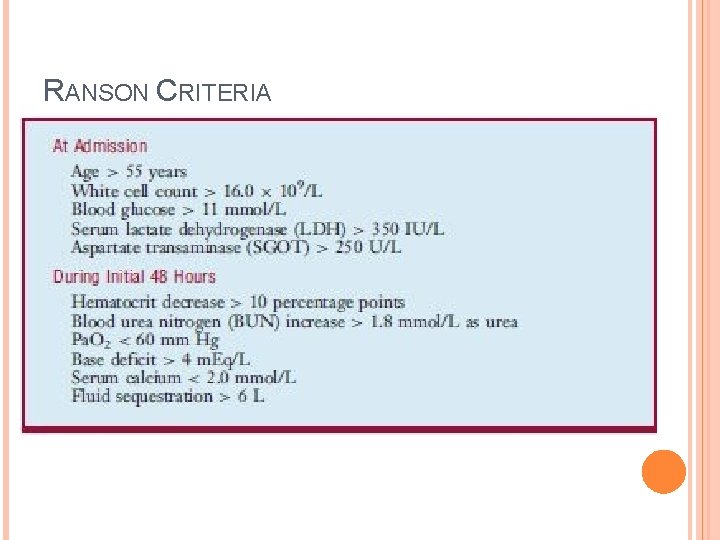
RANSON CRITERIA
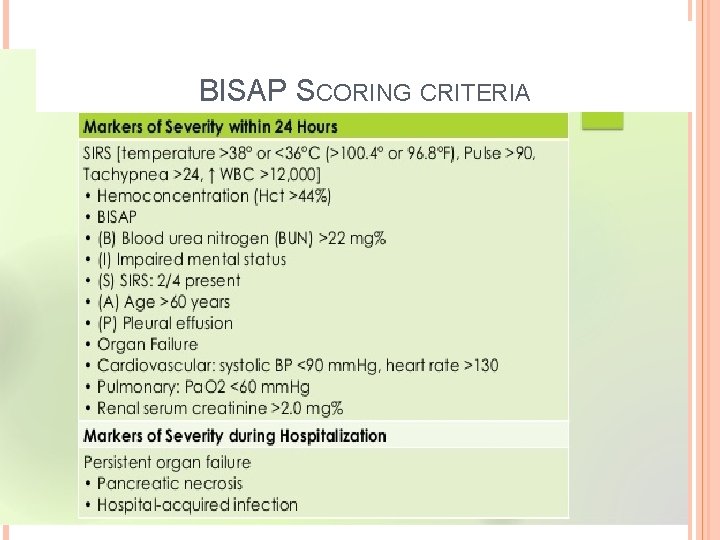
BISAP SCORING CRITERIA
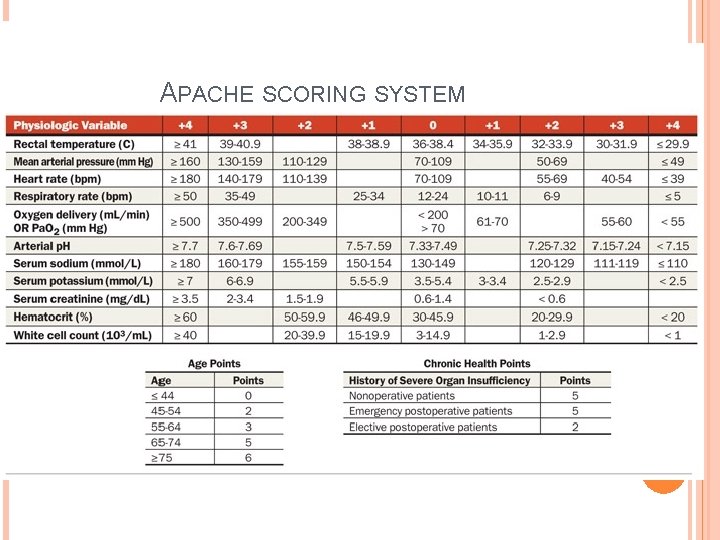
APACHE SCORING SYSTEM
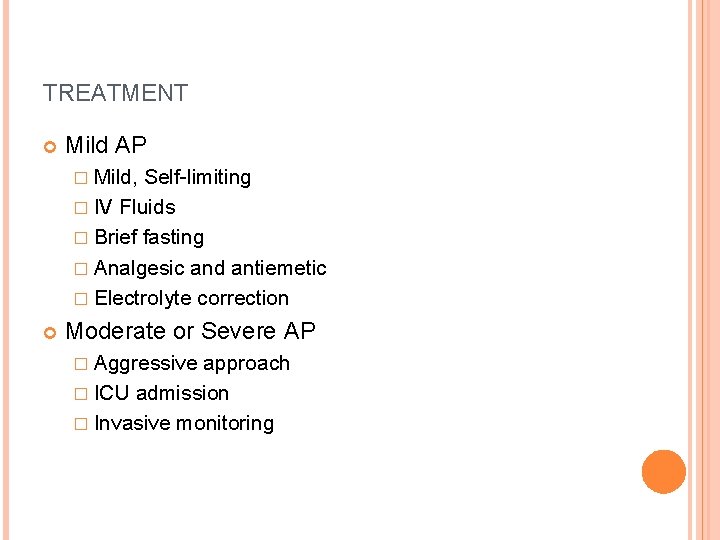
TREATMENT Mild AP � Mild, Self-limiting � IV Fluids � Brief fasting � Analgesic and antiemetic � Electrolyte correction Moderate or Severe AP � Aggressive approach � ICU admission � Invasive monitoring
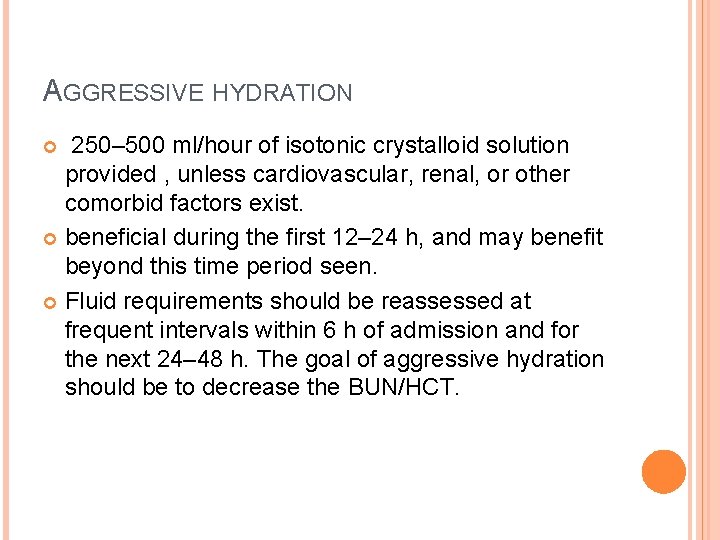
AGGRESSIVE HYDRATION 250– 500 ml/hour of isotonic crystalloid solution provided , unless cardiovascular, renal, or other comorbid factors exist. beneficial during the first 12– 24 h, and may benefit beyond this time period seen. Fluid requirements should be reassessed at frequent intervals within 6 h of admission and for the next 24– 48 h. The goal of aggressive hydration should be to decrease the BUN/HCT.
ERCP IN AP Patients with AP and concurrent acute cholangitis should undergo ERCP within 24 h of admission ERCP is not needed early in most patients with gallstone pancreatitis who lack laboratory or clinical evidence of on-going biliary obstruction In the absence of cholangitis and/or jaundice, MRCP or EUS rather than diagnostic ERCP Pancreatic duct stents and/or post procedure rectal nonsteroidal anti-inflammatory drug (NSAID) suppositories should be utilized to lower the risk of severe post-ERCP pancreatitis in high-risk patients
THE ROLE OF ANTIBIOTICS IN AP Antibiotics should be given for an extra pancreatic infection, such as cholangitis, catheter-acquired infections, bacteremia, urinary tract infections, pneumonia Routine use of prophylactic antibiotics in patients with severe AP is not recommended The use of antibiotics in patients with sterile necrosis to prevent the development of infected necrosis is not recommended Infected necrosis should be considered in patients with pancreatic or extra pancreatic necrosis who deteriorate or fail to improve after 7– 10 days of hospitalization. In these patients, either (i) initial CT-guided fine-needle aspiration (FNA) for c/s to guide use of appropriate antibiotics Or empiric use of antibiotics after obtaining necessary cultures for infectious agents, without CT FNA, should be given In patients with infected necrosis, antibiotics known to penetrate pancreatic necrosis, such as carbapenems, quinolones, and metronidazole, may be useful Routine administration of antifungal agents along with prophylactic or therapeutic antibiotics is not recommended.
NUTRITION IN AP In mild AP, oral feedings can be started immediately if there is no nausea and vomiting, and the abdominal pain has resolved In mild AP, initiation of feeding with a low-fat solid diet appears as safe as a clear liquid diet. In severe AP, enteral nutrition is recommended to prevent infectious complications. Parenteral nutrition should be avoided, unless the enteral route is not available, not tolerated, or not meeting caloric requirements. Nasogastric delivery and nasojejunal delivery of enteral feeding appear comparable in efficacy and safety.
THE ROLE OF SURGERY IN AP In patients with mild AP, found to have gallstones in the gallbladder, a cholecystectomy should be performed before discharge to prevent a recurrence of AP In a patient with necrotizing biliary AP, in order to prevent infection, cholecystectomy is to be deferred until active inflammation subsides and fluid collections resolve or stabilize Asymptomatic pseudocysts and pancreatic and/or extra pancreatic necrosis do not warrant intervention regardless of size, location, and/or extension In stable patients with infected necrosis, surgical, radiologic, and/or endoscopic drainage should be delayed preferably for more than 4 weeks to allow liquefication of the contents and the development of a fibrous wall around the necrosis (walledoff necrosis). In symptomatic patients with infected necrosis, minimally invasive methods of necrosectomy are preferred to open necrosectomy

THANK YOU!!!