Acute Necrotizing Encephalopathy Neuroimaging Diagnosis and Differentials Kevin


- Slides: 46
Acute Necrotizing Encephalopathy: Neuroimaging Diagnosis and Differentials Kevin Y Wang, Doris DM Lin MD Ph. D Division of Neuroradiology Department of Radiology and Radiological Science Johns Hopkins School of Medicine, Baltimore, Maryland Presentation # e. Ed. E-163 Presented by: Kevin Y Wang ASNR, Chicago, April 25 -30, 2015
Disclosures • We have no financial disclosures or conflicts of interest to declare.
Purpose 1. To review neuroimaging features of acute necrotizing encephalopathy (ANE) 2. To evaluate the current diagnostic criteria of ANE 3. To provide a radiologic differential diagnosis of ANE
Methods • Reviewed English literature for reported cases of ANE – Retrieved 11 publications with both neuroimaging and histopathology findings of ANE – Retrieved 53 publications with general neuroimaging findings of ANE • Reviewed imaging features and clinical diagnosis of pediatric cases with bilateral thalamic lesions at home institution
Outline 1 Clinical, Imaging, and Pathology Features 2 Literature Review 3 Radiologic Differential Diagnosis 4 Appendix Click here to return to title slide Click on any link above to jump directly to a particular section return to this slide at anytime

Acute Necrotizing Encephalopathy CLINICAL, IMAGING, & PATHOLOGY FEATURES
Epidemiology and Clinical Features • Acute encephalopathy with distinct imaging features • First described in 1995 by Mizuguchi et al • Higher incidence in children and in Far East • Rapid deterioration of consciousness until comatose, usually within 24 hours • Antecedent acute febrile illness • Associated with wide range of viral agents (Influenza A most common)
Neuroimaging Features • Symmetric, bilateral, multifocal lesions – Thalami always involved – Variable additional involvement: • • Lentiform nuclei Brainstem tegmentum Cerebral white matter Cerebellum • Variable enhancement, hemorrhage • Imaging findings evident after coma ensues
Illustrative Case 9 -month old previously healthy female presenting with 4 days of upper respiratory symptoms and 1 day of suspected seizures
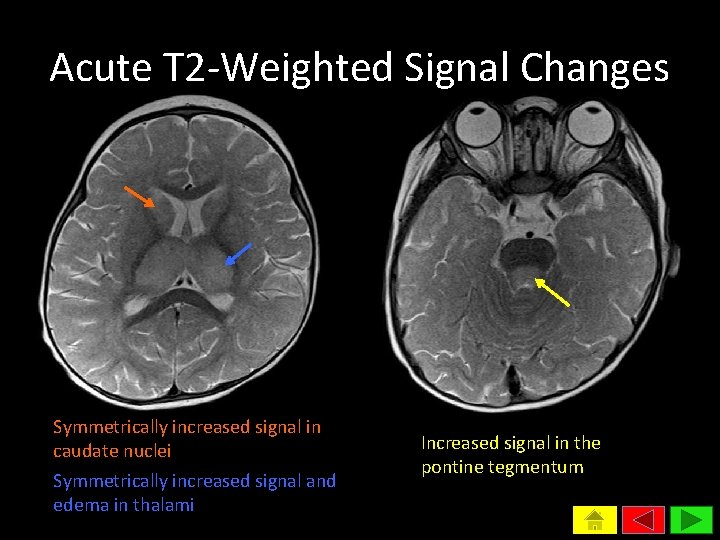
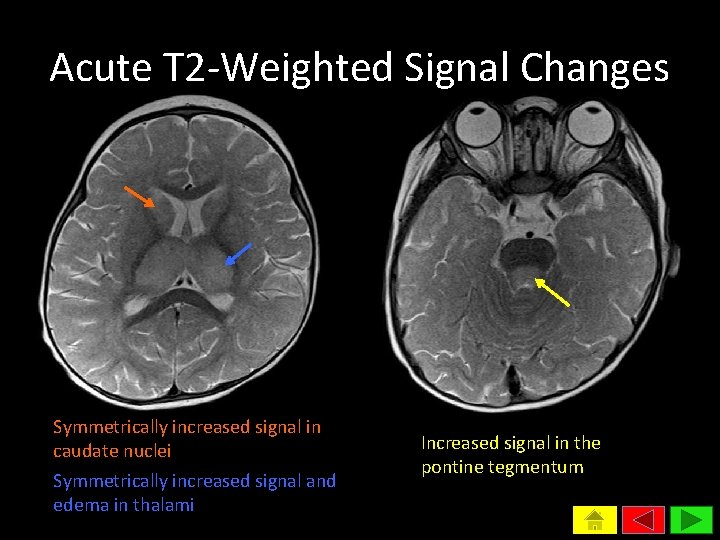
Acute T 2 -Weighted Signal Changes Symmetrically increased signal in caudate nuclei Symmetrically increased signal and edema in thalami Increased signal in the pontine tegmentum
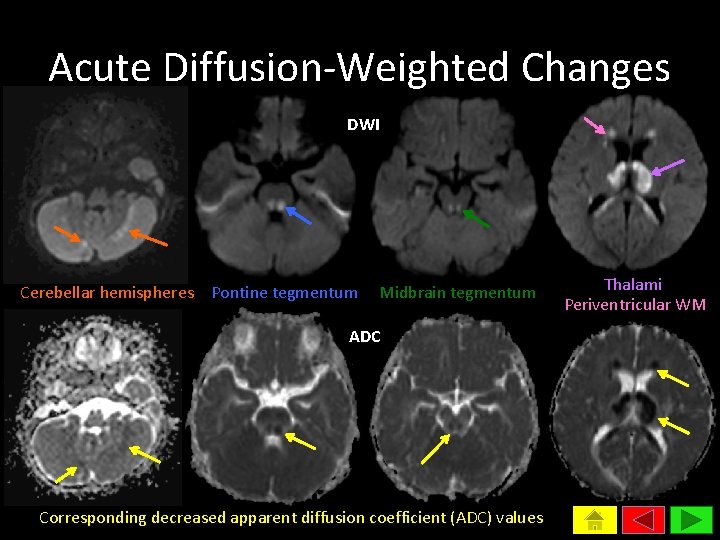
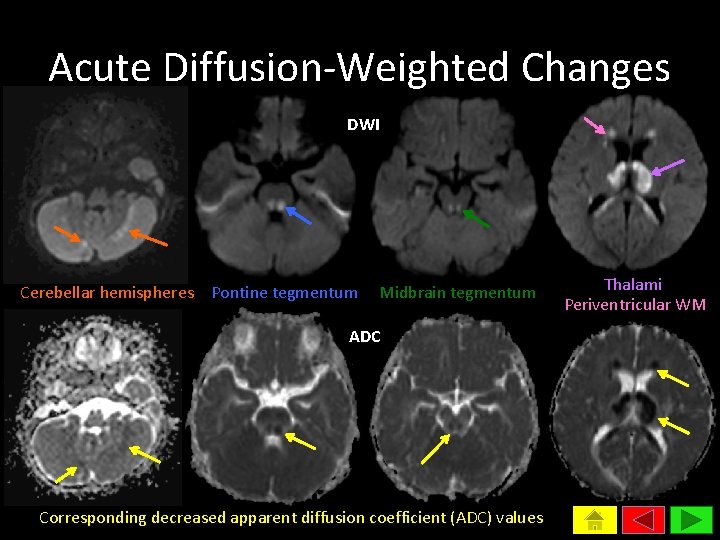
Acute Diffusion-Weighted Changes DWI Cerebellar hemispheres Pontine tegmentum Midbrain tegmentum ADC Corresponding decreased apparent diffusion coefficient (ADC) values Thalami Periventricular WM
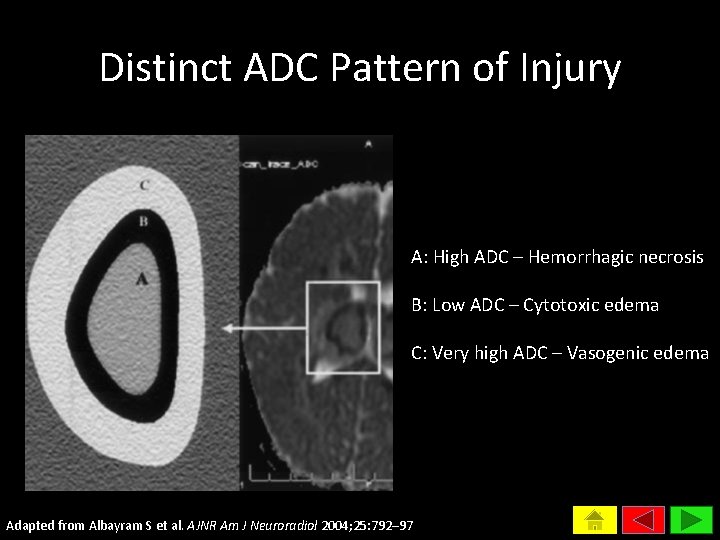
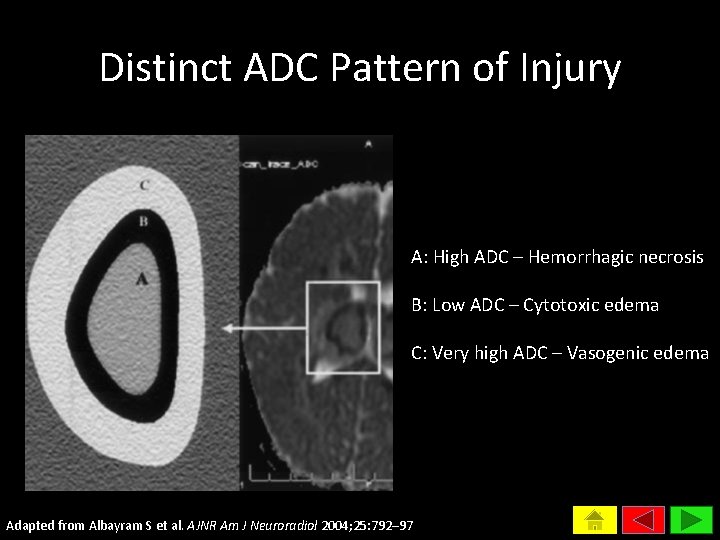
Distinct ADC Pattern of Injury A: High ADC – Hemorrhagic necrosis B: Low ADC – Cytotoxic edema C: Very high ADC – Vasogenic edema Adapted from Albayram S et al. AJNR Am J Neuroradiol 2004; 25: 792– 97
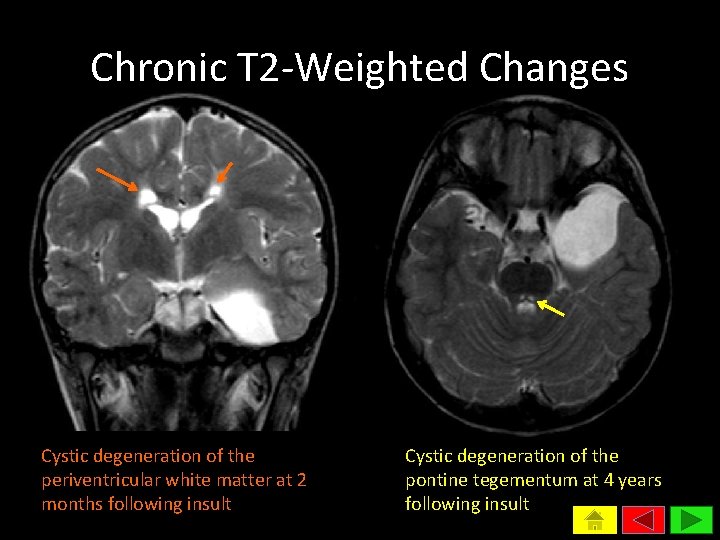
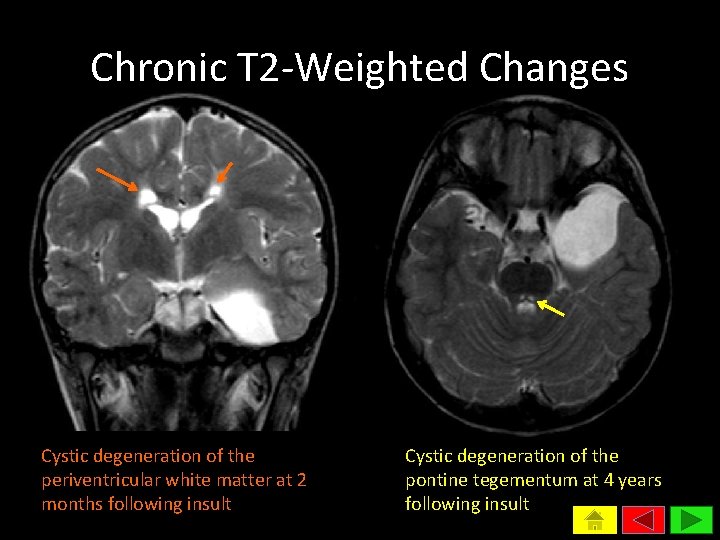
Chronic T 2 -Weighted Changes Cystic degeneration of the periventricular white matter at 2 months following insult Cystic degeneration of the pontine tegementum at 4 years following insult
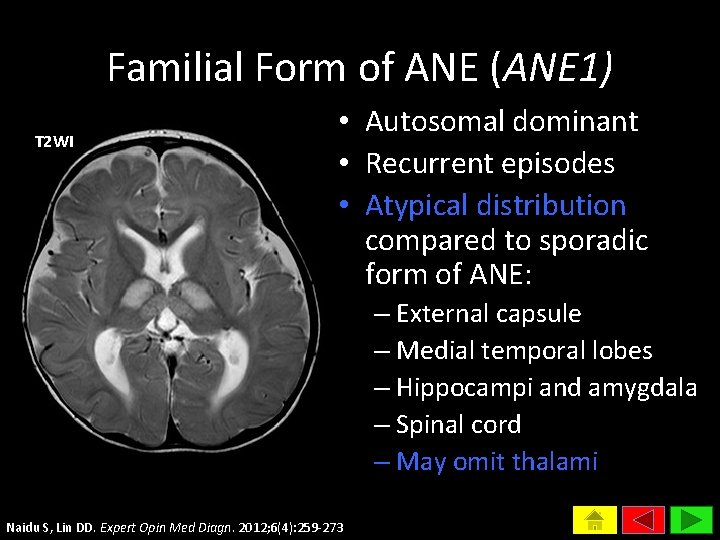
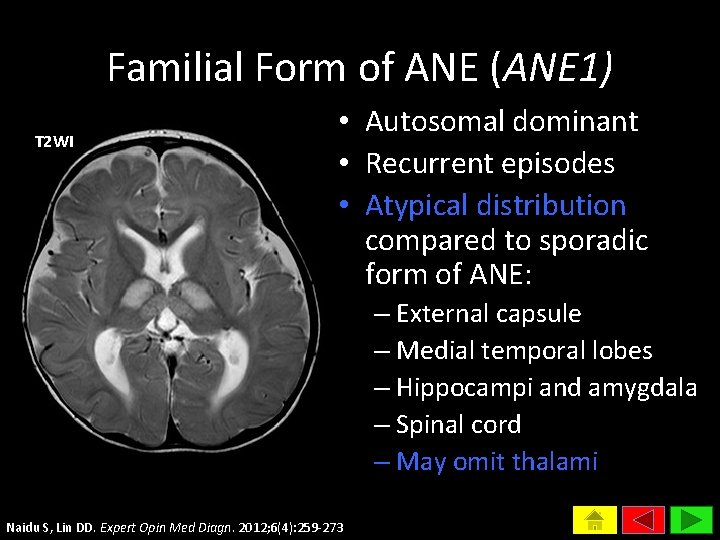
Familial Form of ANE (ANE 1) T 2 WI • Autosomal dominant • Recurrent episodes • Atypical distribution compared to sporadic form of ANE: – External capsule – Medial temporal lobes – Hippocampi and amygdala – Spinal cord – May omit thalami Naidu S, Lin DD. Expert Opin Med Diagn. 2012; 6(4): 259 -273
Pathology Features • Grey matter – Necrosis – Petechial hemorrhage • White matter – Plasma-like substance extravasation – Myelin pallor • Lack of inflammation, apoptosis, and viral pathogen
Proposed Diagnostic Criteria for ANE 1. Acute encephalopathy following febrile illness 2. No CSF pleocytosis 1 3. No elevated serum ammonia 2 4. CT or MRI evidence of symmetric thalamic lesions 5. Exclusion of resembling diseases Modified from Mizuguchi et al, 1997 1 Primarily intended to exclude viral encephalitis and acute disseminated encephalomyelitis 2 Primarily intended to exclude Reye’s syndrome, given frequent elevation of transaminase levels in ANE
Acute Necrotizing Encephalopathy LITERATURE REVIEW
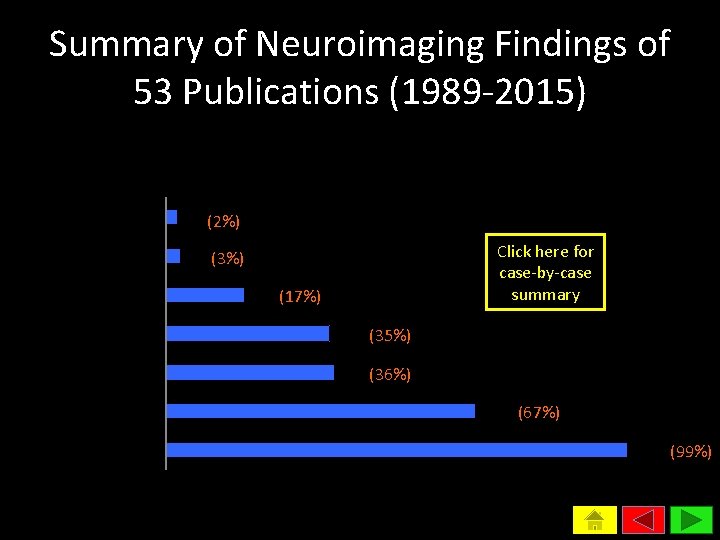
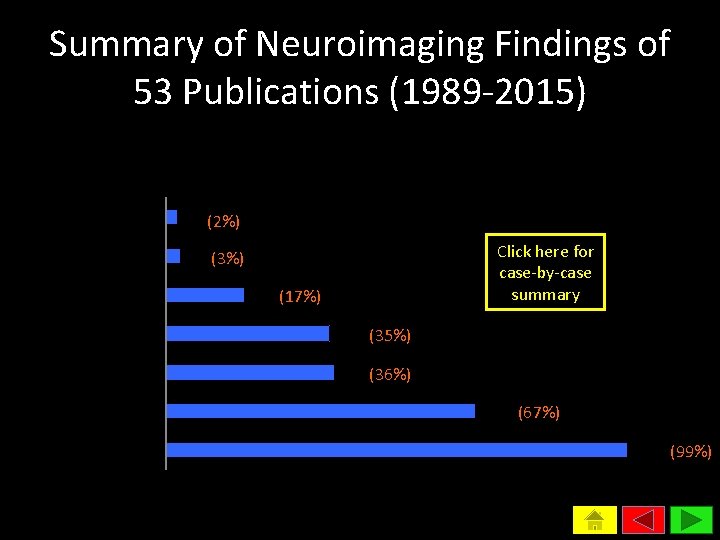
Summary of Neuroimaging Findings of 53 Publications (1989 -2015) Frequency of Involvement in CNS Structures (Percentage reported in 165 cases) Caudate nuclei Globus pallidi Putamen White matter Cerebellum Brainstem Thalami 4 (2%) 5 Click here for case-by-case summary (3%) 28 (17%) 58 (35%) 60 (36%) 110 (67%) 164 (99%)
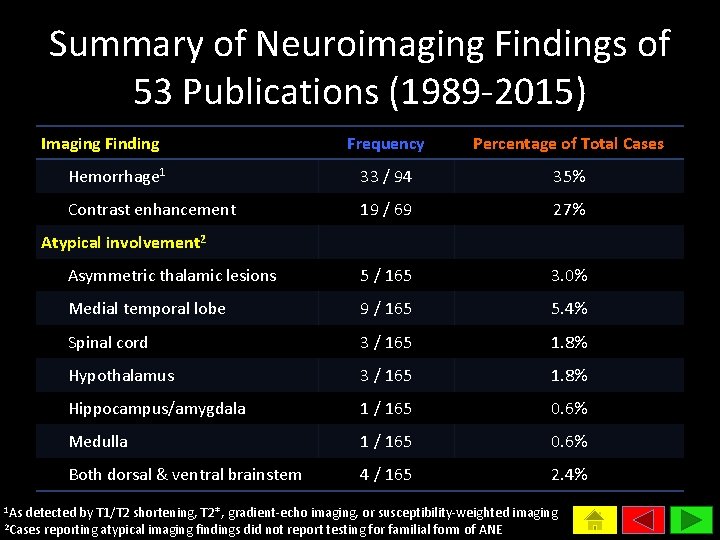
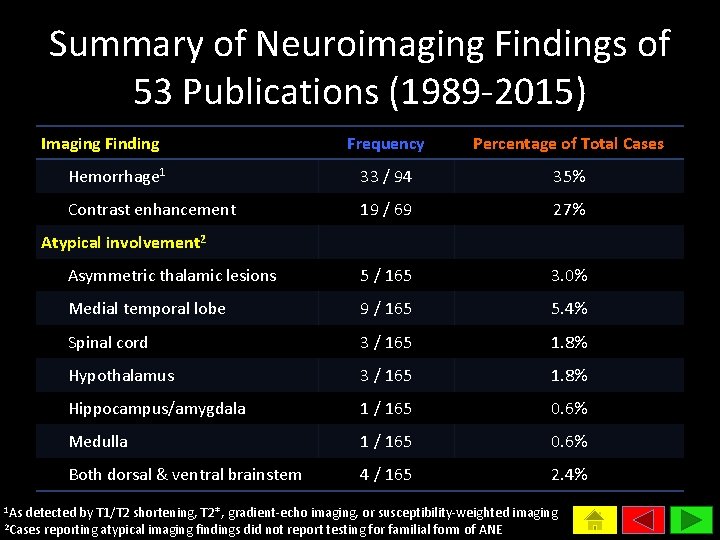
Summary of Neuroimaging Findings of 53 Publications (1989 -2015) Imaging Finding Frequency Percentage of Total Cases Hemorrhage 1 33 / 94 35% Contrast enhancement 19 / 69 27% Asymmetric thalamic lesions 5 / 165 3. 0% Medial temporal lobe 9 / 165 5. 4% Spinal cord 3 / 165 1. 8% Hypothalamus 3 / 165 1. 8% Hippocampus/amygdala 1 / 165 0. 6% Medulla 1 / 165 0. 6% Both dorsal & ventral brainstem 4 / 165 2. 4% Atypical involvement 2 1 As detected by T 1/T 2 shortening, T 2*, gradient-echo imaging, or susceptibility-weighted imaging reporting atypical imaging findings did not report testing for familial form of ANE 2 Cases
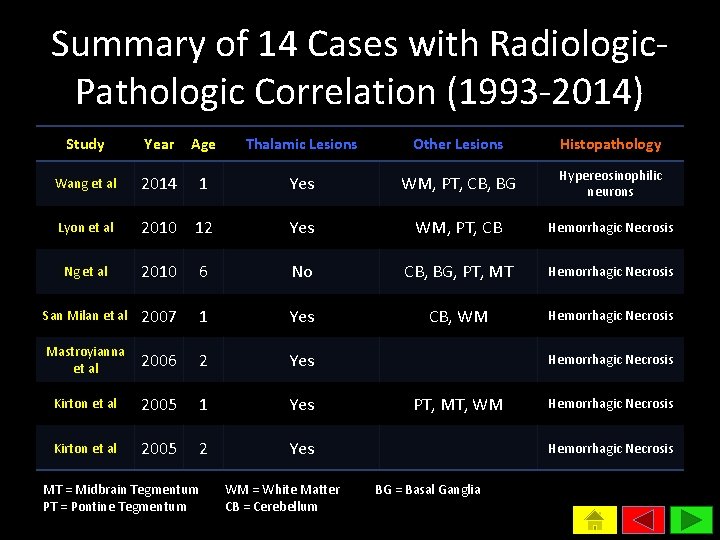
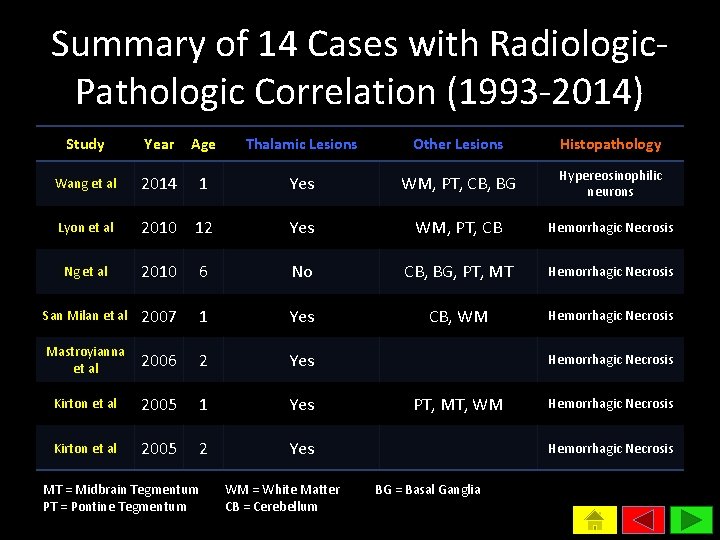
Summary of 14 Cases with Radiologic. Pathologic Correlation (1993 -2014) Study Year Age Thalamic Lesions Other Lesions Histopathology Wang et al 2014 1 Yes WM, PT, CB, BG Hypereosinophilic neurons Lyon et al 2010 12 Yes WM, PT, CB Hemorrhagic Necrosis Ng et al 2010 6 No CB, BG, PT, MT Hemorrhagic Necrosis San Milan et al 2007 1 Yes CB, WM Hemorrhagic Necrosis Mastroyianna et al 2006 2 Yes Kirton et al 2005 1 Yes Kirton et al 2005 2 Yes MT = Midbrain Tegmentum PT = Pontine Tegmentum WM = White Matter CB = Cerebellum Hemorrhagic Necrosis PT, MT, WM Hemorrhagic Necrosis BG = Basal Ganglia
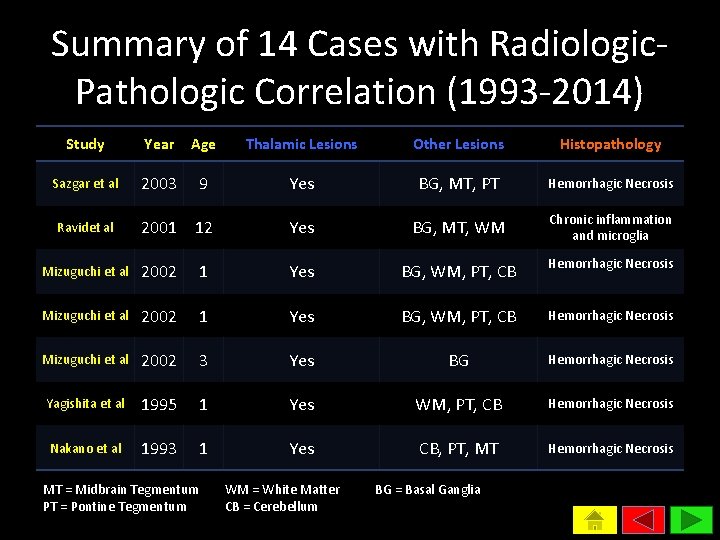
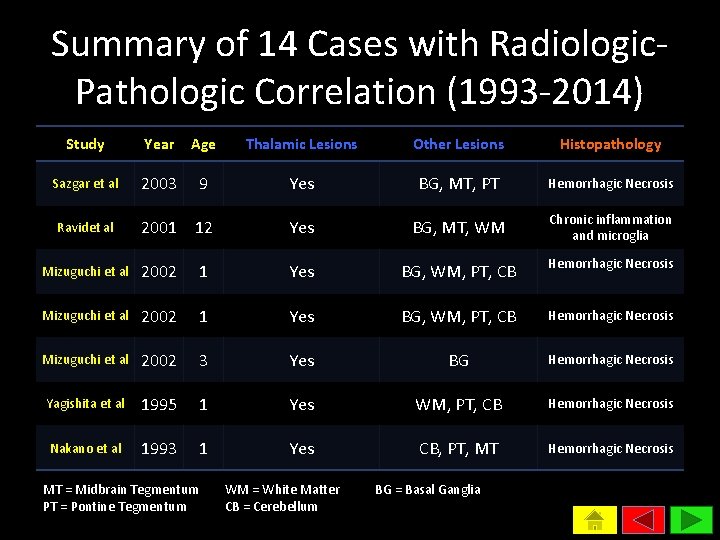
Summary of 14 Cases with Radiologic. Pathologic Correlation (1993 -2014) Study Year Age Thalamic Lesions Other Lesions Histopathology Sazgar et al 2003 9 Yes BG, MT, PT Hemorrhagic Necrosis 2001 12 Yes BG, MT, WM Chronic inflammation and microglia Mizuguchi et al 2002 1 Yes BG, WM, PT, CB Hemorrhagic Necrosis Mizuguchi et al 2002 3 Yes BG Hemorrhagic Necrosis Yagishita et al 1995 1 Yes WM, PT, CB Hemorrhagic Necrosis Nakano et al 1993 1 Yes CB, PT, MT Hemorrhagic Necrosis Ravidet al MT = Midbrain Tegmentum PT = Pontine Tegmentum WM = White Matter CB = Cerebellum BG = Basal Ganglia
Summary • Sporadic ANE may rarely demonstrate atypical neuroimaging findings not encompassed in current, proposed diagnostic criteria • Rarely, imaging features may also be consistent with ANE but not confirmed on neuropathology • Accuracy of neuroimaging to positively and negatively predict ANE is high but not perfect
Implication • A combination of clinical and radiological features may at most be suggestive of ANE • Neuropathology may ultimately be necessary for definitive diagnosis • However, biopsy may be of little clinical and practical utility, and unlikely to change management • Post-test probability from imaging is likely sufficiently high to treat presumptively for ANE in most cases
Acute Necrotizing Encephalopathy RADIOLOGIC DIFFERENTIAL DIAGNOSIS
Radiologic Differential Diagnosis 1 2 3 4 5 Severe Hypoxic-Ischemic Injury Arterial Infarct Venous Infarct Acute Disseminated Encephalomyelitis (ADEM) Hemolytic Uremic Syndrome (HUS) Encephalopathy 6 Viral Encephalitis 7 Bilateral Thalamic Glioma
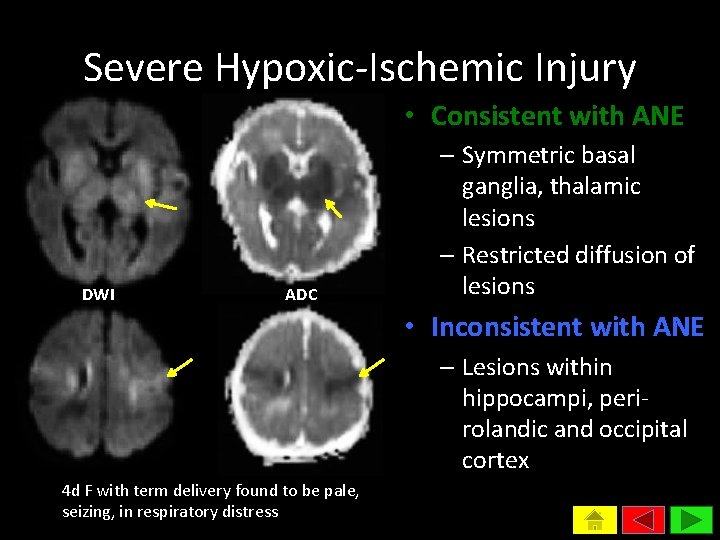
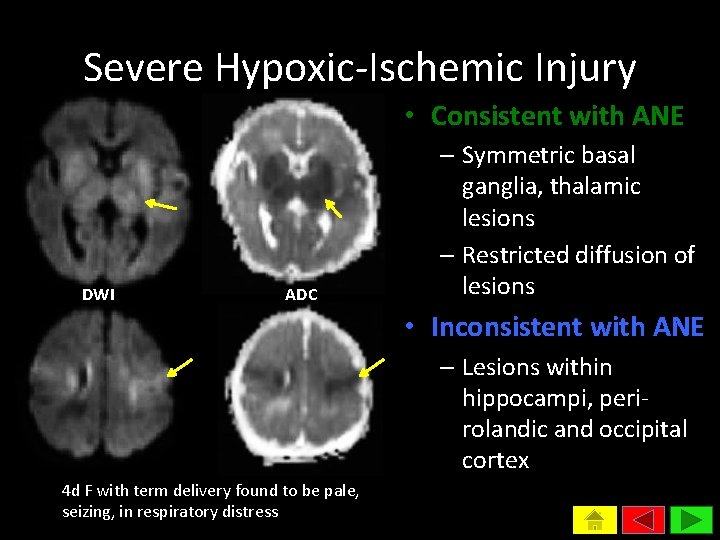
Severe Hypoxic-Ischemic Injury • Consistent with ANE DWI ADC – Symmetric basal ganglia, thalamic lesions – Restricted diffusion of lesions • Inconsistent with ANE – Lesions within hippocampi, perirolandic and occipital cortex 4 d F with term delivery found to be pale, seizing, in respiratory distress
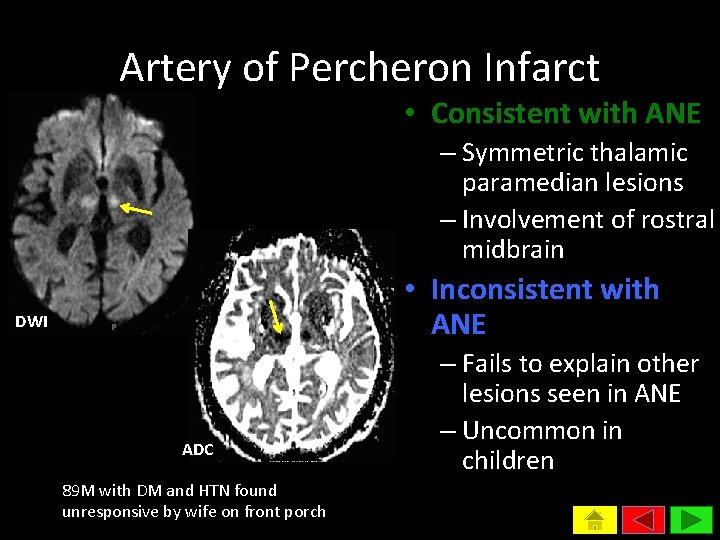
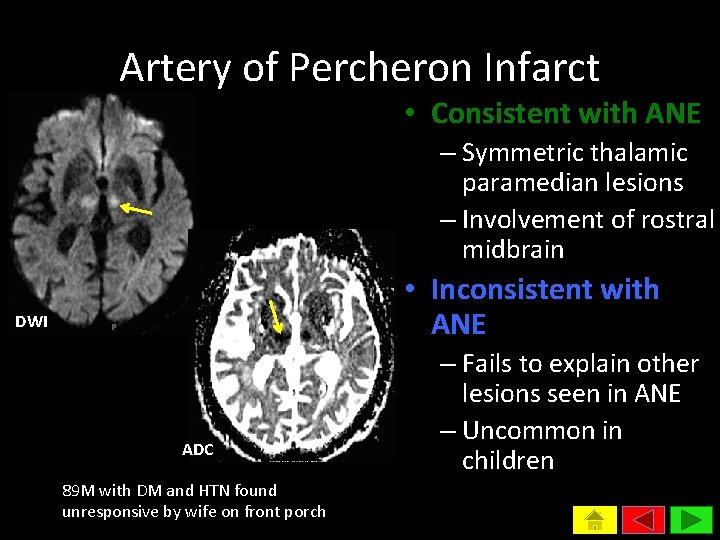
Artery of Percheron Infarct • Consistent with ANE – Symmetric thalamic paramedian lesions – Involvement of rostral midbrain • Inconsistent with ANE DWI ADC 89 M with DM and HTN found unresponsive by wife on front porch – Fails to explain other lesions seen in ANE – Uncommon in children
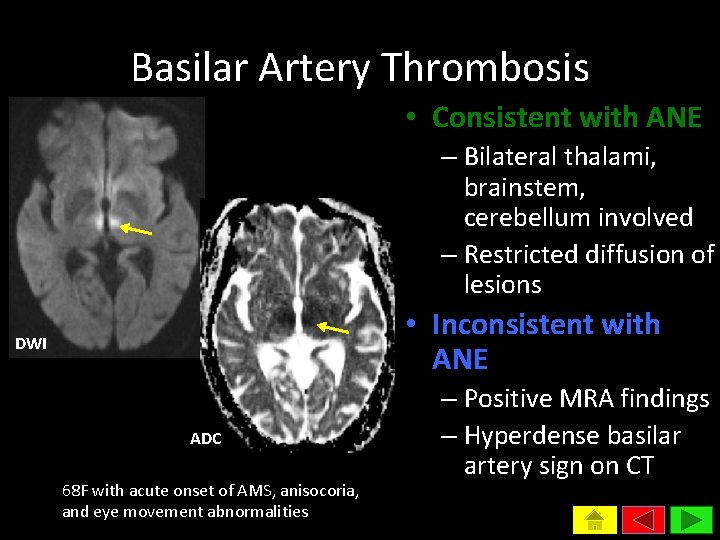
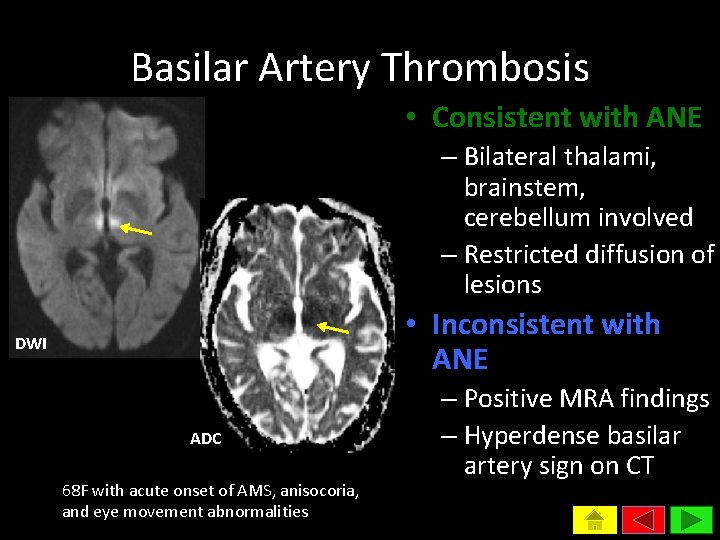
Basilar Artery Thrombosis • Consistent with ANE – Bilateral thalami, brainstem, cerebellum involved – Restricted diffusion of lesions • Inconsistent with ANE DWI ADC 68 F with acute onset of AMS, anisocoria, and eye movement abnormalities – Positive MRA findings – Hyperdense basilar artery sign on CT
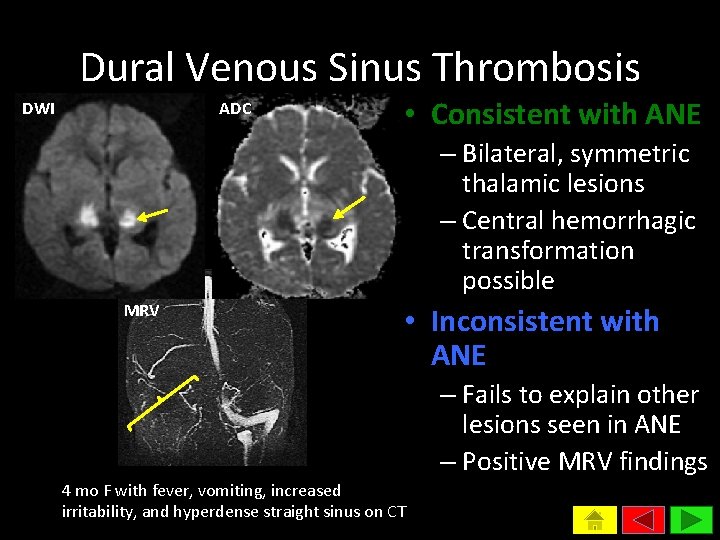
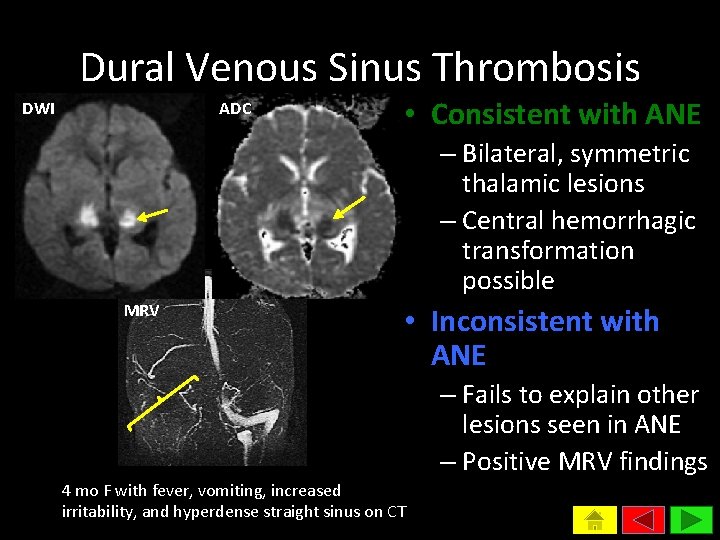
Dural Venous Sinus Thrombosis DWI ADC • Consistent with ANE – Bilateral, symmetric thalamic lesions – Central hemorrhagic transformation possible MRV • Inconsistent with ANE – Fails to explain other lesions seen in ANE – Positive MRV findings 4 mo F with fever, vomiting, increased irritability, and hyperdense straight sinus on CT
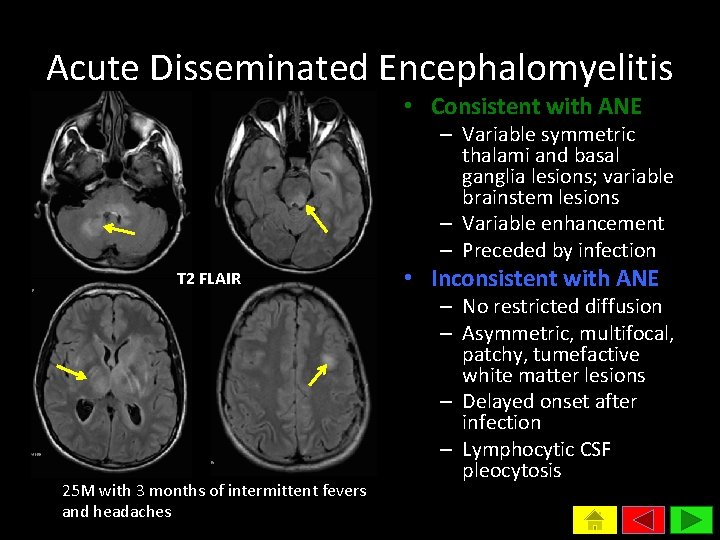
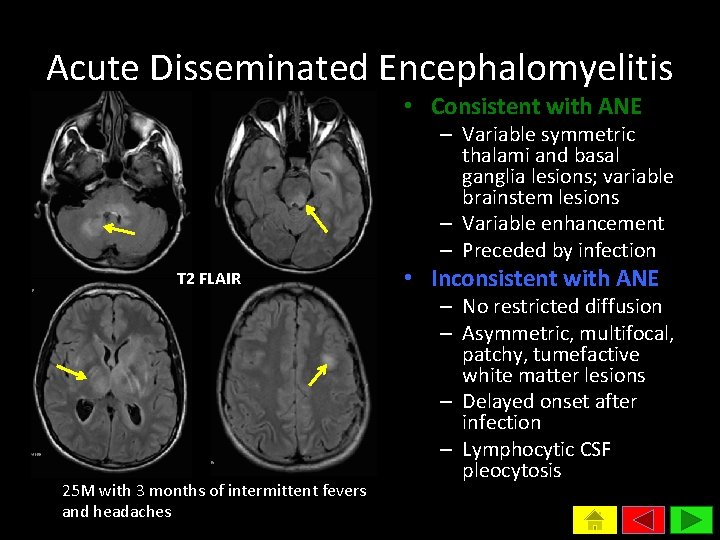
Acute Disseminated Encephalomyelitis • Consistent with ANE – Variable symmetric thalami and basal ganglia lesions; variable brainstem lesions – Variable enhancement – Preceded by infection T 2 FLAIR 25 M with 3 months of intermittent fevers and headaches • Inconsistent with ANE – No restricted diffusion – Asymmetric, multifocal, patchy, tumefactive white matter lesions – Delayed onset after infection – Lymphocytic CSF pleocytosis
Hemolytic Uremic Syndrome Encephalopathy • Consistent with ANE – Bilateral basal ganglia lesions most characteristic – Variable thalami, brainstem, cerebellum involvement – Restricted diffusion of lesions – May be preceded by infection • Inconsistent with ANE – Hippocampi, insula, and cerebral peduncle variably involved – Responsive to plasmapheresis Steinborn M et al. Pediatr Radiol 2004; 34: 805 -10.
Viral Encephalitis • Consistent with ANE – Basal ganglia and thalamic lesions in EBV – Bilateral thalamic, brainstem, cerebellar lesions in Japanese encephalitis virus – Bilateral thalamic, basal ganglia, midbrain lesions in West Nile virus • Inconsistent with ANE – CSF pleocytosis – Positive viral PCR or culture in CSF Smith AB et al. AJR. American journal of roentgenology. Feb 2009; 192(2): W 53 -62.

Bilateral Thalamic Glioma • Consistent with ANE – Bilateral thalamic lesions • Inconsistent with ANE T 2 FLAIR Post-Gad T 1 WI 22 F with progressive left UE weakness and difficulty concentrating – No restricted diffusion – No contrast enhancement – Fails to explain other lesions seen in ANE
Summary • ANE is distinctly characterized by symmetric thalamic lesions • Given clinical and radiologic features may lack specificity, neuropathology may be required for definitive diagnosis of ANE • ANE, as well as a number of other diagnoses, should be considered in a child with an acute presentation of bilateral thalamic lesions
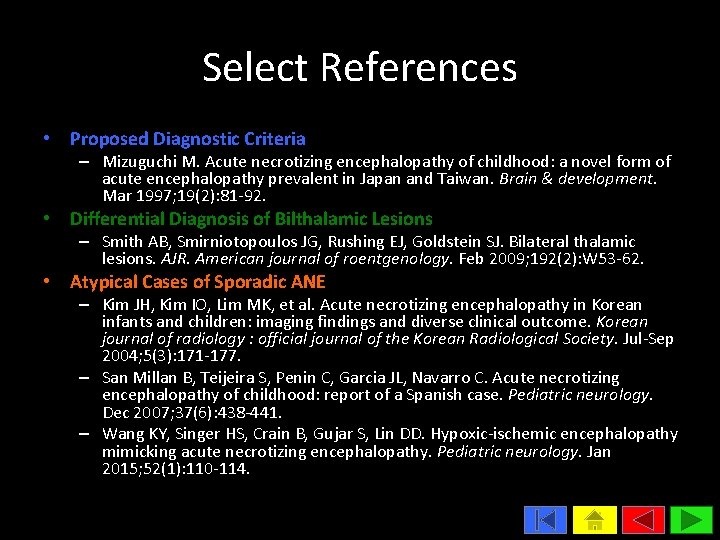
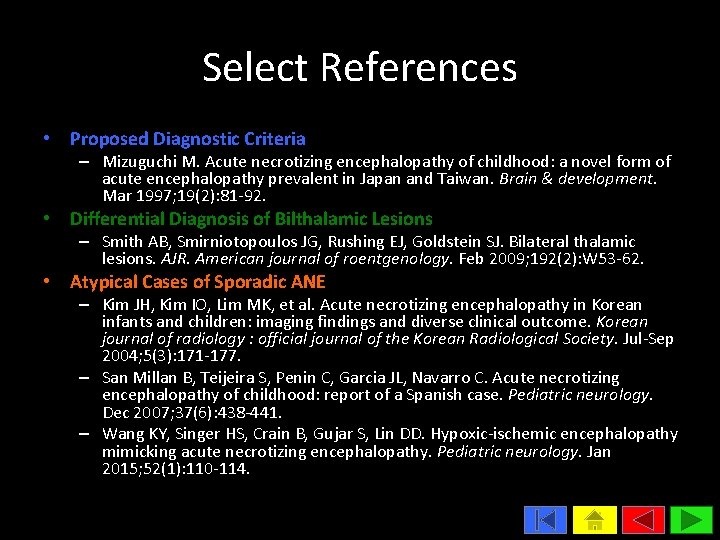
Select References • Proposed Diagnostic Criteria – Mizuguchi M. Acute necrotizing encephalopathy of childhood: a novel form of acute encephalopathy prevalent in Japan and Taiwan. Brain & development. Mar 1997; 19(2): 81 -92. • Differential Diagnosis of Bilthalamic Lesions – Smith AB, Smirniotopoulos JG, Rushing EJ, Goldstein SJ. Bilateral thalamic lesions. AJR. American journal of roentgenology. Feb 2009; 192(2): W 53 -62. • Atypical Cases of Sporadic ANE – Kim JH, Kim IO, Lim MK, et al. Acute necrotizing encephalopathy in Korean infants and children: imaging findings and diverse clinical outcome. Korean journal of radiology : official journal of the Korean Radiological Society. Jul-Sep 2004; 5(3): 171 -177. – San Millan B, Teijeira S, Penin C, Garcia JL, Navarro C. Acute necrotizing encephalopathy of childhood: report of a Spanish case. Pediatric neurology. Dec 2007; 37(6): 438 -441. – Wang KY, Singer HS, Crain B, Gujar S, Lin DD. Hypoxic-ischemic encephalopathy mimicking acute necrotizing encephalopathy. Pediatric neurology. Jan 2015; 52(1): 110 -114.
Acute Necrotizing Encephalopathy APPENDIX
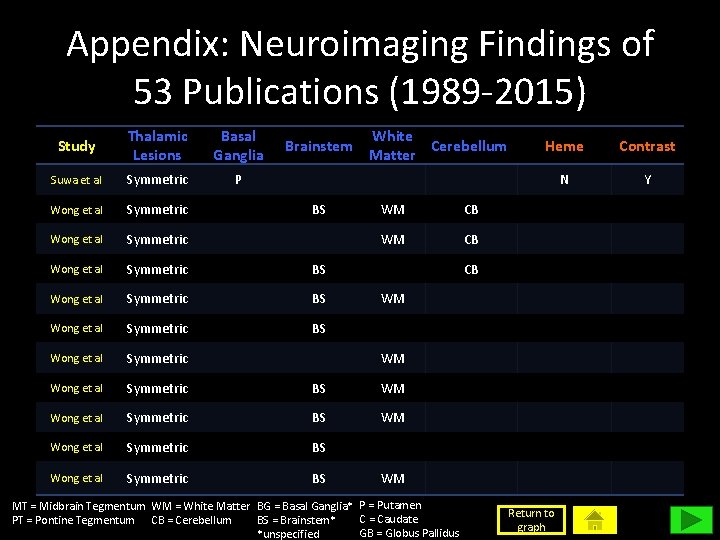
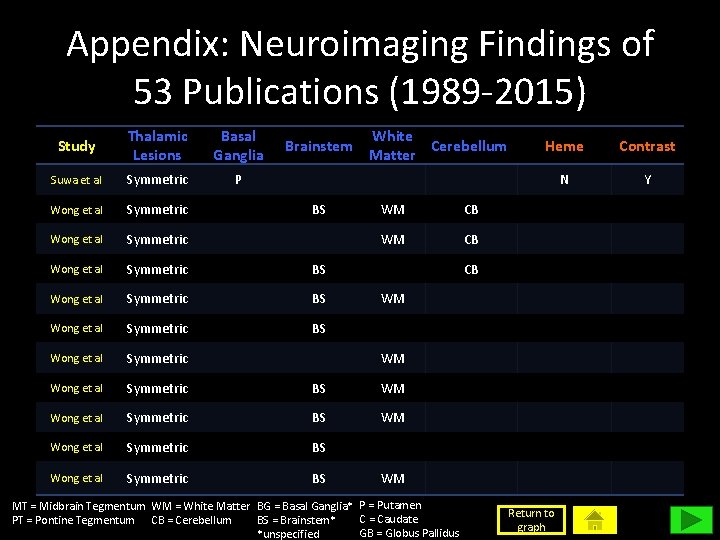
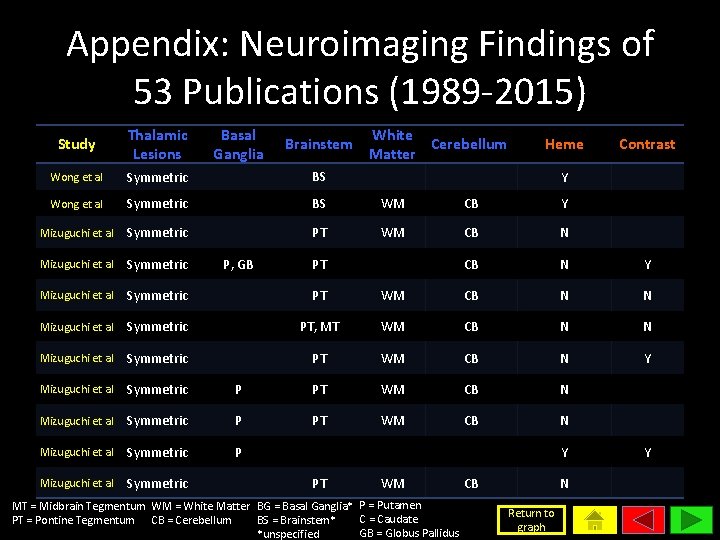
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Suwa et al Symmetric P Wong et al Symmetric BS Wong et al Symmetric BS WM Wong et al Symmetric BS Brainstem BS White Cerebellum Matter WM CB Heme Contrast N Y CB WM WM WM MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified Return to graph
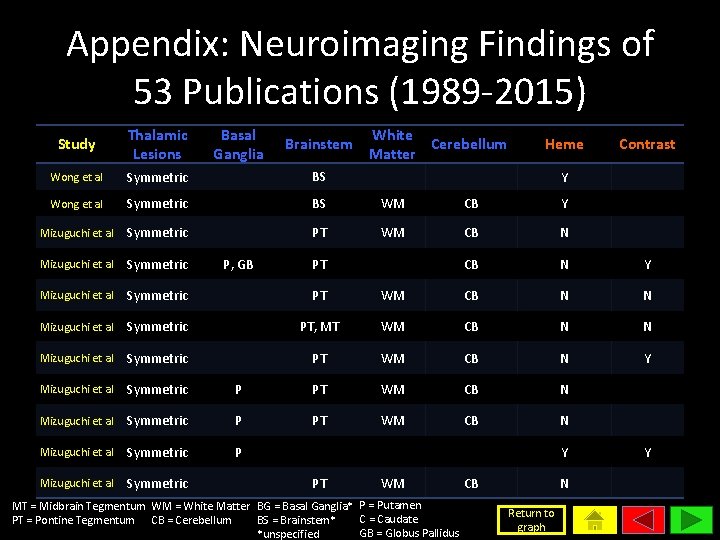
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Wong et al Symmetric BS WM CB Y Mizuguchi et al Symmetric PT WM CB N Mizuguchi et al Symmetric CB N Y Mizuguchi et al Symmetric PT WM CB N N Mizuguchi et al Symmetric PT, MT WM CB N N Mizuguchi et al Symmetric PT WM CB N Y Mizuguchi et al Symmetric P PT WM CB N Mizuguchi et al Symmetric P, GB Brainstem White Cerebellum Matter Heme Y PT Contrast WM MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified CB N Return to graph Y
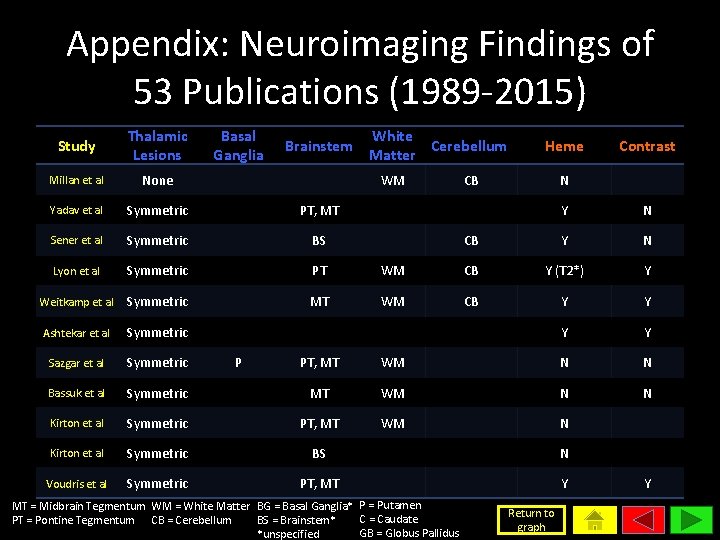
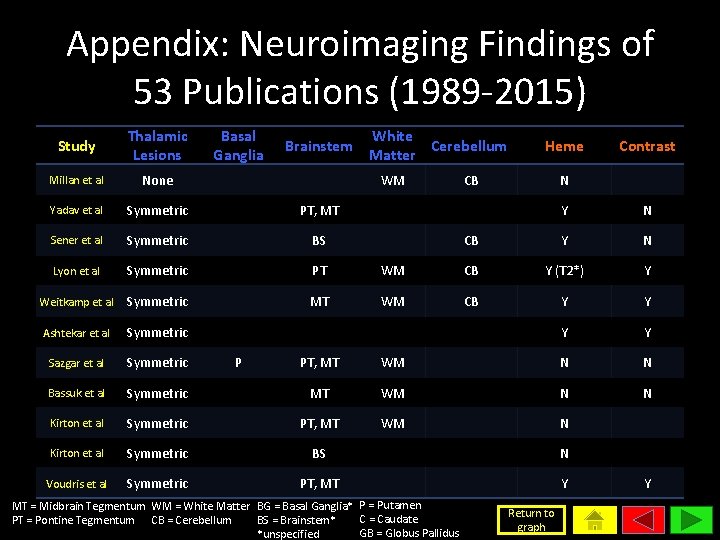
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Millan et al None Yadav et al Symmetric PT, MT Sener et al Symmetric BS Lyon et al Symmetric PT Weitkamp et al Symmetric MT Ashtekar et al Symmetric Sazgar et al Symmetric Bassuk et al Brainstem White Cerebellum Matter WM P Heme CB Contrast N Y N CB Y N WM CB Y (T 2*) Y WM CB Y Y PT, MT WM N N Symmetric MT WM N N Kirton et al Symmetric PT, MT WM N Kirton et al Symmetric BS N Voudris et al Symmetric PT, MT Y MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified Return to graph Y
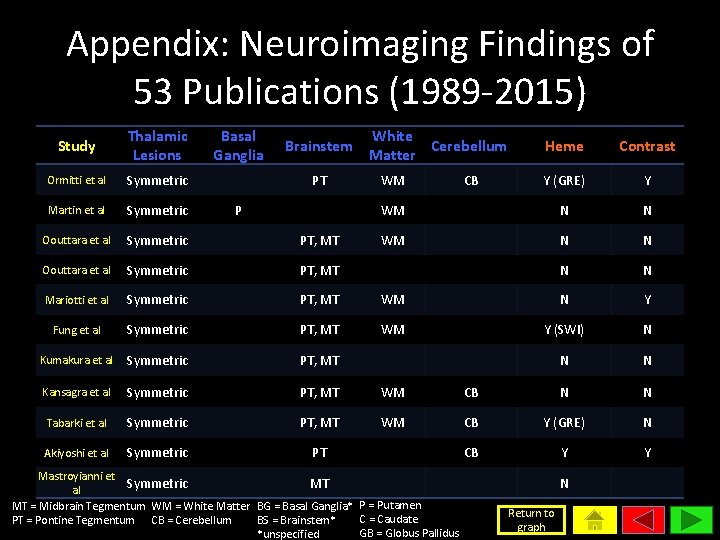
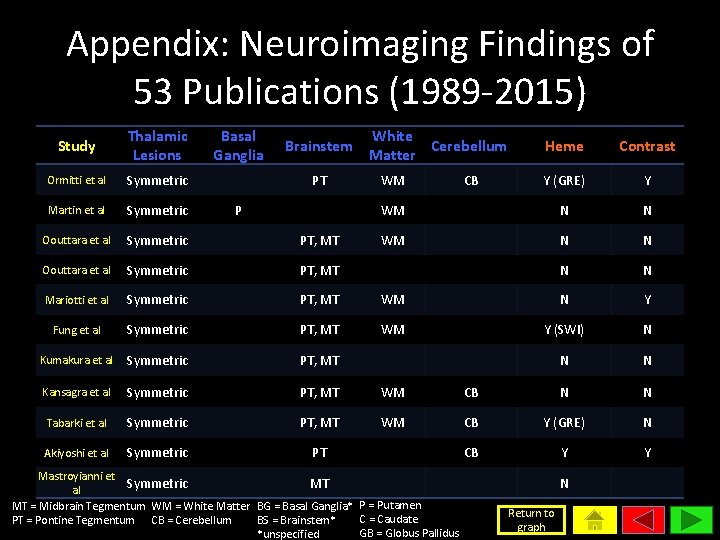
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Ormitti et al Symmetric Martin et al Symmetric Oouttara et al Symmetric PT, MT Mariotti et al Symmetric PT, MT Fung et al Symmetric PT, MT Kumakura et al Symmetric PT, MT Kansagra et al Symmetric PT, MT WM Tabarki et al Symmetric PT, MT WM Akiyoshi et al Symmetric PT Brainstem PT P White Cerebellum Matter Heme Contrast Y (GRE) Y WM N N N N WM N Y WM Y (SWI) N N N CB Y (GRE) N CB Y Y WM Mastroyianni et Symmetric MT al MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified CB N Return to graph
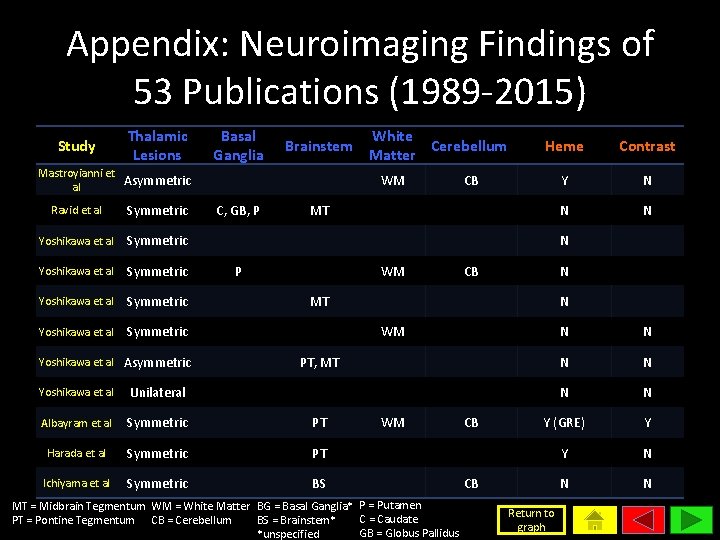
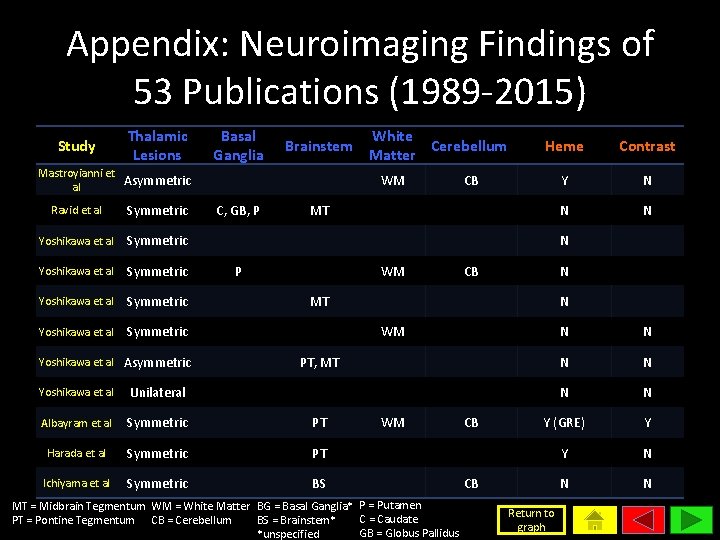
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Brainstem Mastroyianni et Asymmetric al Ravid et al Symmetric Yoshikawa et al Symmetric Yoshikawa et al Asymmetric White Cerebellum Matter WM C, GB, P Heme Contrast Y N N N CB MT N P WM CB N MT N WM N N N Y (GRE) Y Y N N N PT, MT Yoshikawa et al Unilateral Albayram et al Symmetric PT Harada et al Symmetric PT Ichiyama et al Symmetric BS WM MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified CB CB Return to graph
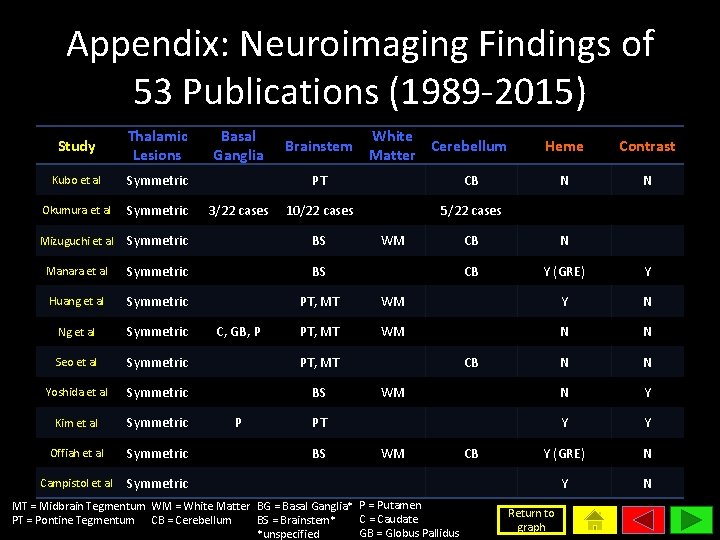
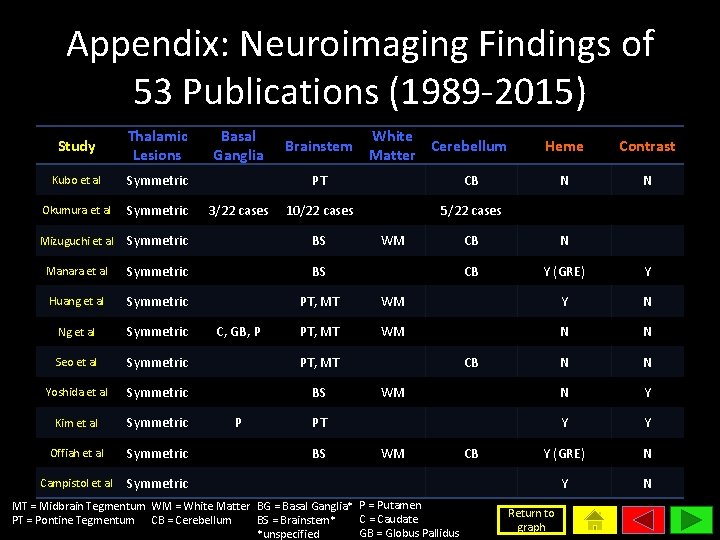
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Kubo et al Symmetric Okumura et al Symmetric Mizuguchi et al Symmetric BS Manara et al Symmetric BS Huang et al Symmetric PT, MT Ng et al Symmetric PT, MT Seo et al Symmetric PT, MT Yoshida et al Symmetric BS Kim et al Symmetric Offiah et al Symmetric Campistol et al Symmetric 3/22 cases C, GB, P P Brainstem White Cerebellum Matter PT CB 10/22 cases 5/22 cases WM Heme Contrast N N CB Y (GRE) Y WM Y N WM N N N Y Y (GRE) N Y N CB WM PT BS WM MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified CB Return to graph
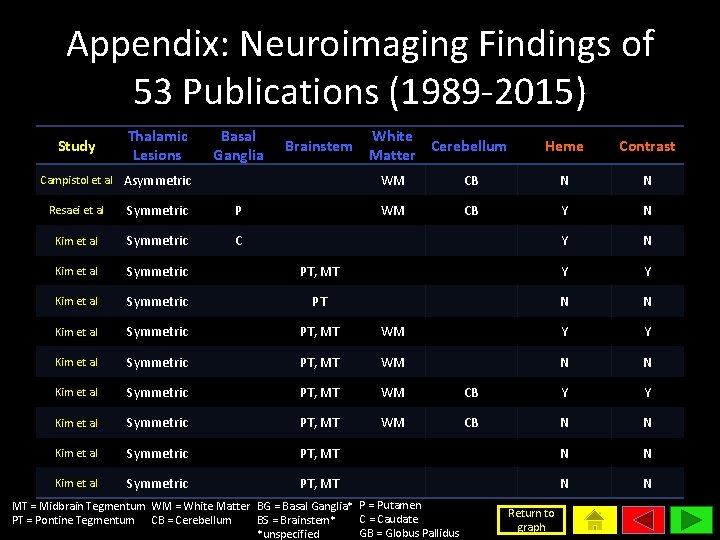
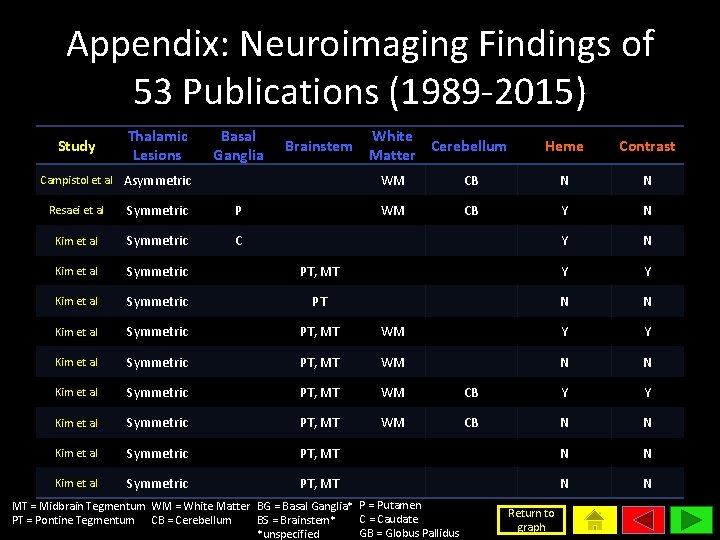
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Brainstem Campistol et al Asymmetric White Cerebellum Matter Heme Contrast WM CB N N WM CB Y N Resaei et al Symmetric P Kim et al Symmetric C Kim et al Symmetric PT, MT Y Y Kim et al Symmetric PT N N Kim et al Symmetric PT, MT WM Y Y Kim et al Symmetric PT, MT WM N N Kim et al Symmetric PT, MT WM CB Y Y Kim et al Symmetric PT, MT WM CB N N Kim et al Symmetric PT, MT N N MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified Return to graph
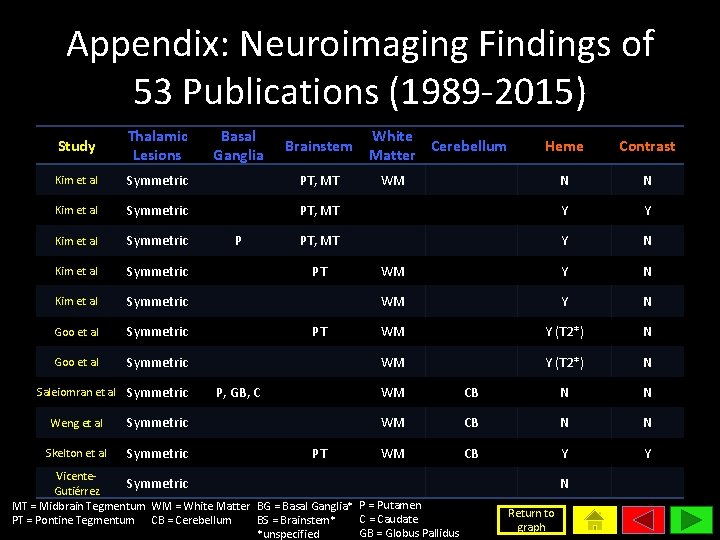
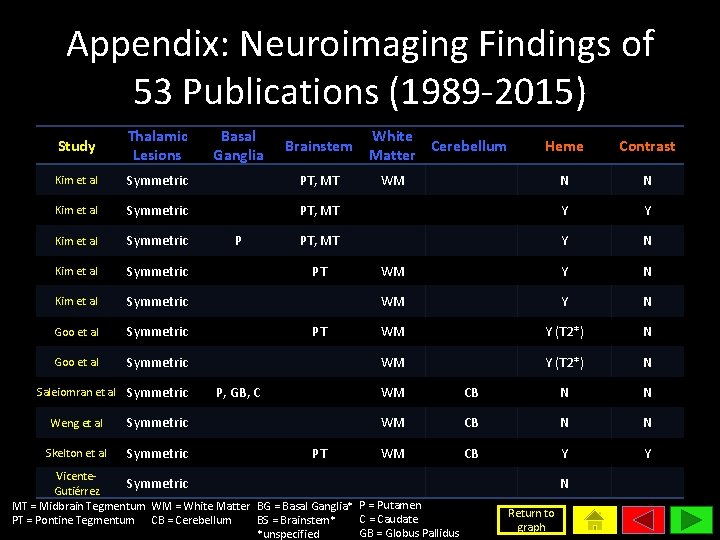
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Kim et al Symmetric PT, MT Kim et al Symmetric Goo et al Symmetric Saleiomran et al Symmetric Weng et al Symmetric Skelton et al Symmetric Basal Ganglia P Brainstem White Cerebellum Matter Heme Contrast N N PT, MT Y Y PT, MT Y N WM Y (T 2*) N PT PT P, GB, C PT WM WM CB N N WM CB Y Y Vicente. Symmetric Gutiérrez MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified N Return to graph
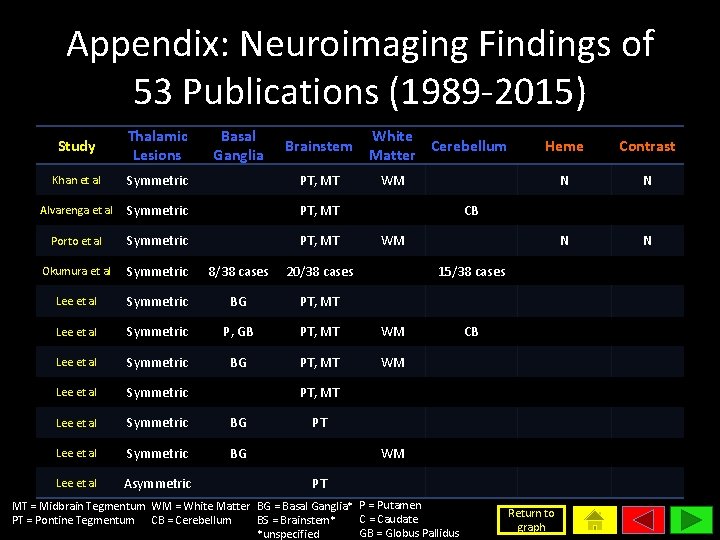
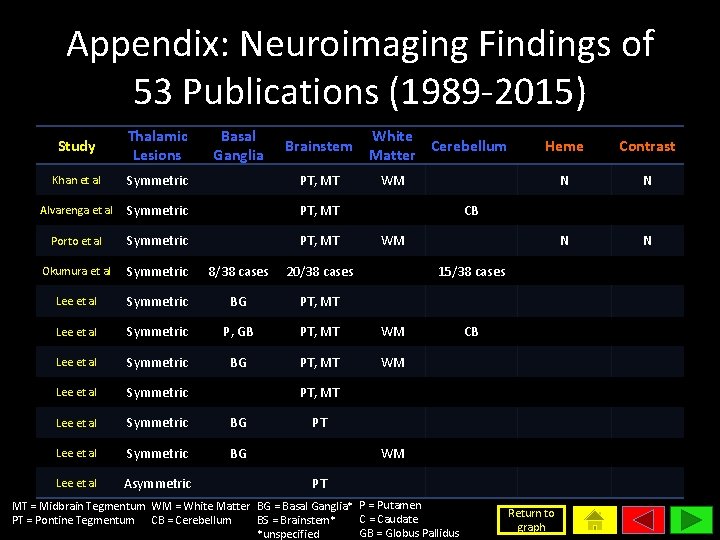
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Khan et al Symmetric PT, MT Alvarenga et al Symmetric PT, MT Porto et al Symmetric PT, MT Okumura et al Symmetric 8/38 cases 20/38 cases Lee et al Symmetric BG PT, MT Lee et al Symmetric P, GB PT, MT WM Lee et al Symmetric BG Lee et al Symmetric BG Lee et al Asymmetric Brainstem White Cerebellum Matter Heme Contrast N N WM CB WM 15/38 cases CB PT, MT PT WM PT MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified Return to graph
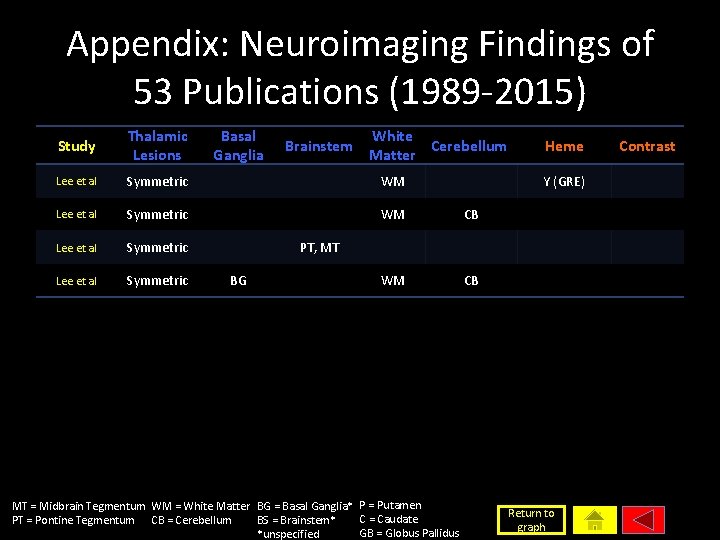
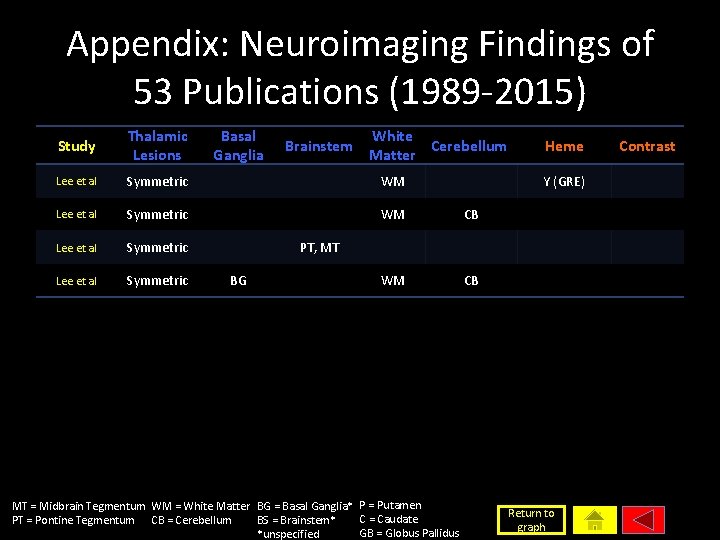
Appendix: Neuroimaging Findings of 53 Publications (1989 -2015) Study Thalamic Lesions Basal Ganglia Lee et al Symmetric WM CB Brainstem White Cerebellum Matter Heme Y (GRE) PT, MT BG MT = Midbrain Tegmentum WM = White Matter BG = Basal Ganglia* P = Putamen C = Caudate PT = Pontine Tegmentum CB = Cerebellum BS = Brainstem* GB = Globus Pallidus *unspecified Return to graph Contrast
 Acute toxic encephalopathy icd 10
Acute toxic encephalopathy icd 10 Hepatic coma
Hepatic coma Necrotizing ulcerative gingivitis
Necrotizing ulcerative gingivitis Necrotizing fasciitis hemorrhagic bullae
Necrotizing fasciitis hemorrhagic bullae Nec diagnosis
Nec diagnosis Neuroimaging
Neuroimaging Merle sepp
Merle sepp What is nec in babies
What is nec in babies Linear approximations and differentials
Linear approximations and differentials Differentials of hydrocephalus
Differentials of hydrocephalus Compensating differentials
Compensating differentials Compensating wage differentials definition
Compensating wage differentials definition Compensating wage differentials
Compensating wage differentials Exact
Exact Wage differentials definition
Wage differentials definition Acute productive cough differential diagnosis
Acute productive cough differential diagnosis Diagnosis of post traumatic stress disorder
Diagnosis of post traumatic stress disorder Acute pancreatitis diagnosis criteria
Acute pancreatitis diagnosis criteria Definition of nursing diagnosis
Definition of nursing diagnosis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Second phase of nursing process
Second phase of nursing process Nursing process objectives
Nursing process objectives Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Hypokalemia
Hypokalemia Hepatic precoma definition
Hepatic precoma definition Diet hepatic encephalopathy
Diet hepatic encephalopathy Epiology definition
Epiology definition Diet for hepatitis c
Diet for hepatitis c West haven hepatic encephalopathy
West haven hepatic encephalopathy Hepatic encephalopathy stages
Hepatic encephalopathy stages Paracetamol overdose stages
Paracetamol overdose stages Uremic encephalopathy
Uremic encephalopathy Constructional apraxia hepatic encephalopathy
Constructional apraxia hepatic encephalopathy Uremic encephalopathy
Uremic encephalopathy Hepatic encephalopathy staging
Hepatic encephalopathy staging Encephalopathy stages
Encephalopathy stages Bilirubin encephalopathy
Bilirubin encephalopathy Ctfr
Ctfr Hypertensive encephalopathy
Hypertensive encephalopathy Childs pugh mdcalc
Childs pugh mdcalc Hashimoto encephalopathy diagnostic criteria
Hashimoto encephalopathy diagnostic criteria 5 cardinal signs of inflammation
5 cardinal signs of inflammation Classifying triangles 4-1
Classifying triangles 4-1 Cellular events of acute inflammation
Cellular events of acute inflammation Chapter 18 common chronic and acute conditions
Chapter 18 common chronic and acute conditions Morphology of acute inflammation
Morphology of acute inflammation