Acute Myocardial Infarction and Cardiac Arrest Due to
- Slides: 14
Acute Myocardial Infarction and Cardiac Arrest Due to Coronary Artery Perforation After Mitral Valve Surgery : Successful Treatment with a Covered Stent Harshal P. Sheth MD Rajiv S. Swamy MD Atman P. Shah MD FACC FSCAI University of Chicago Medical Center
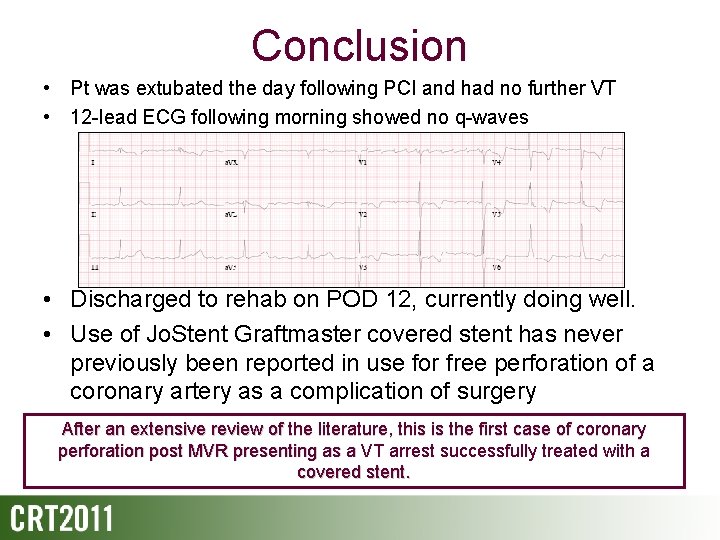
History of Present Illness • 82 yo male with a bioprosthetic MVR (27 mm Carpentier. Edwards Pericardial Valve) placed in 2002 secondary to infective endocarditis, presents with increasing dyspnea on exertion • TTE: severe MS w/ a 26 mm. Hg gradient and severe MR elects for redo MVR • Pre-op EKG NSR and coronary angiography revealed a 50% mid-RCA (co-dominant) stenosis
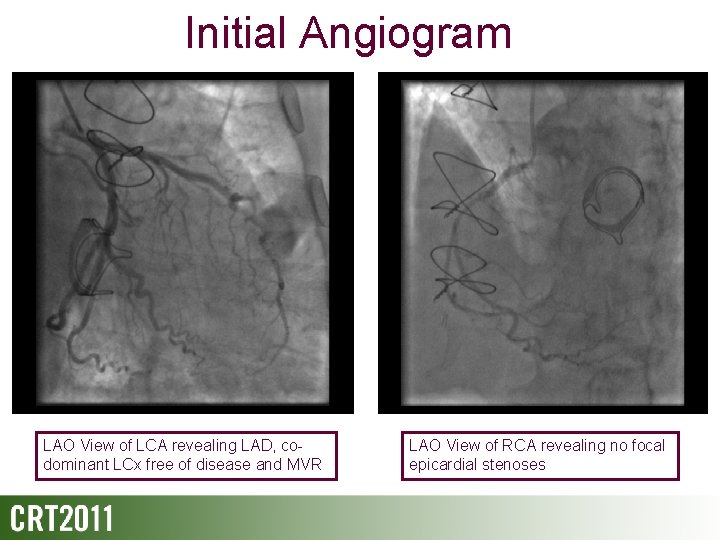
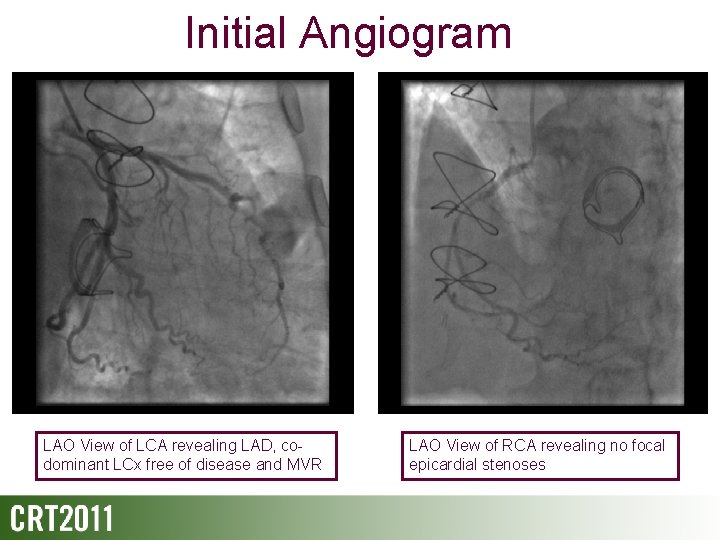
Initial Angiogram LAO View of LCA revealing LAD, codominant LCx free of disease and MVR LAO View of RCA revealing no focal epicardial stenoses
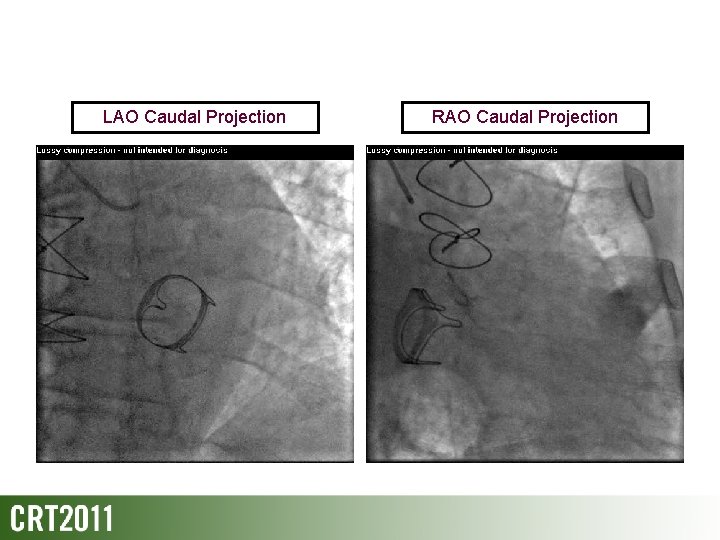
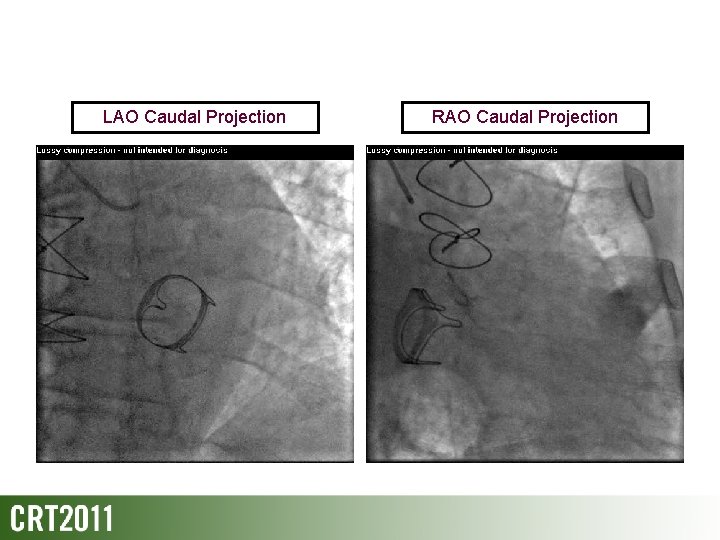
LAO Caudal Projection RAO Caudal Projection
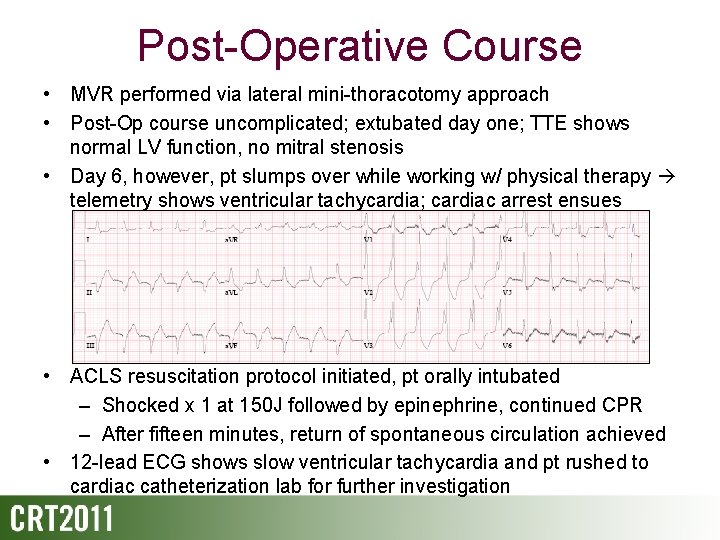
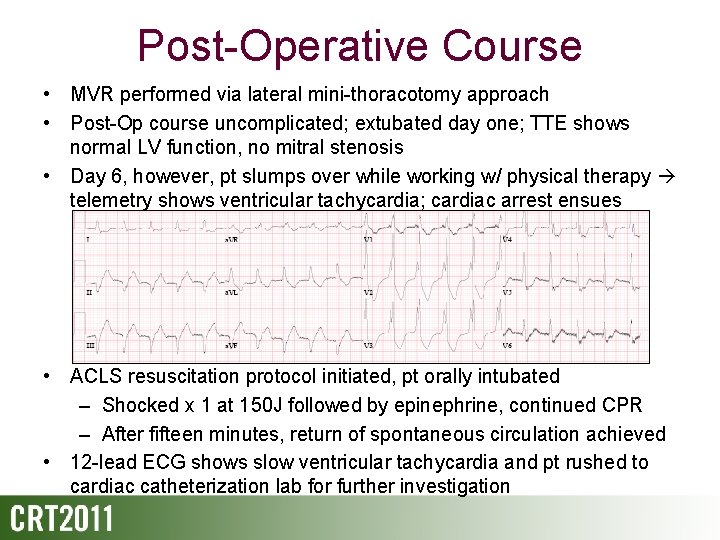
Post-Operative Course • MVR performed via lateral mini-thoracotomy approach • Post-Op course uncomplicated; extubated day one; TTE shows normal LV function, no mitral stenosis • Day 6, however, pt slumps over while working w/ physical therapy telemetry shows ventricular tachycardia; cardiac arrest ensues • ACLS resuscitation protocol initiated, pt orally intubated – Shocked x 1 at 150 J followed by epinephrine, continued CPR – After fifteen minutes, return of spontaneous circulation achieved • 12 -lead ECG shows slow ventricular tachycardia and pt rushed to cardiac catheterization lab for further investigation
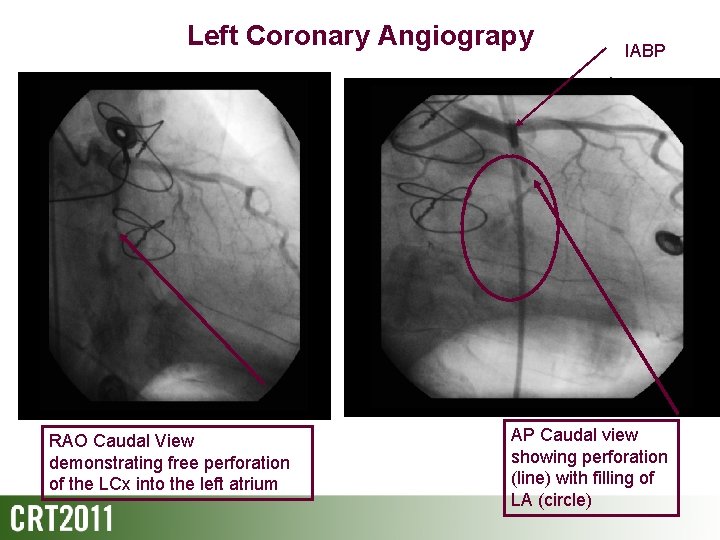
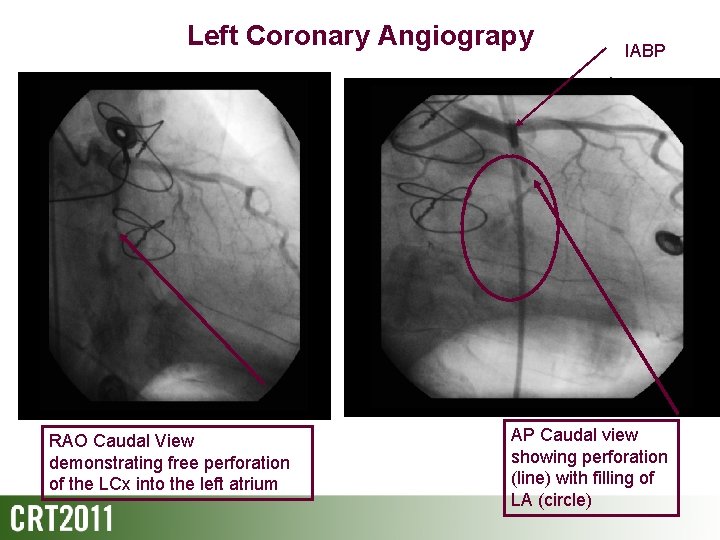
Left Coronary Angiograpy RAO Caudal View demonstrating free perforation of the LCx into the left atrium IABP AP Caudal view showing perforation (line) with filling of LA (circle)
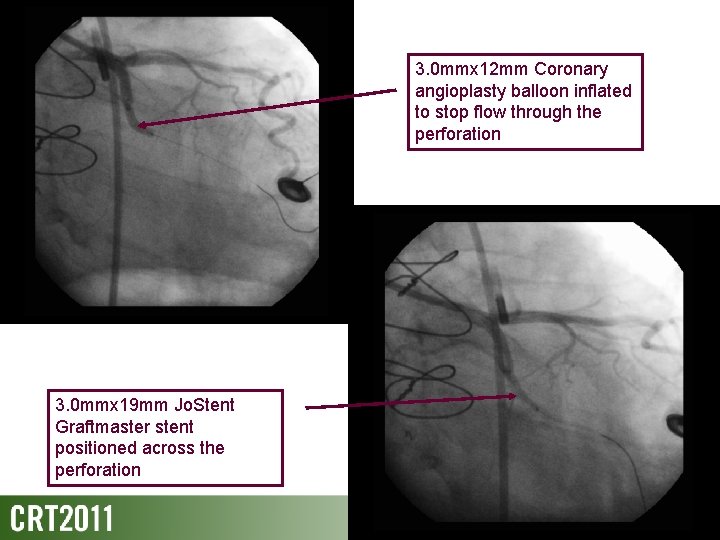
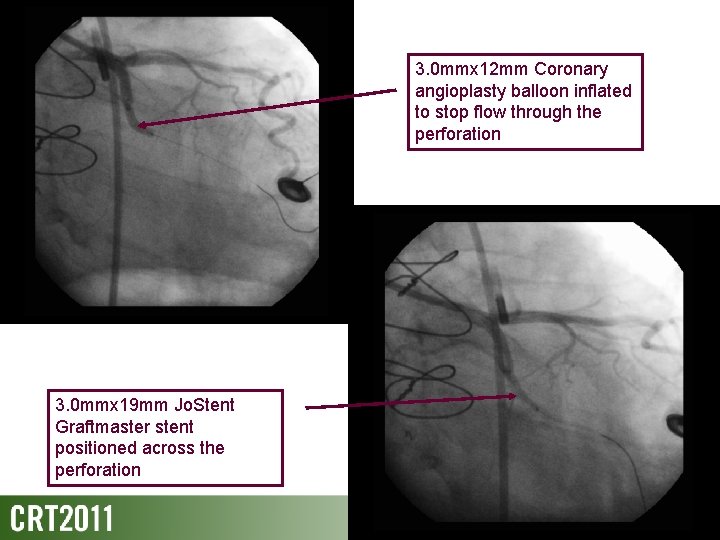
3. 0 mmx 12 mm Coronary angioplasty balloon inflated to stop flow through the perforation 3. 0 mmx 19 mm Jo. Stent Graftmaster stent positioned across the perforation
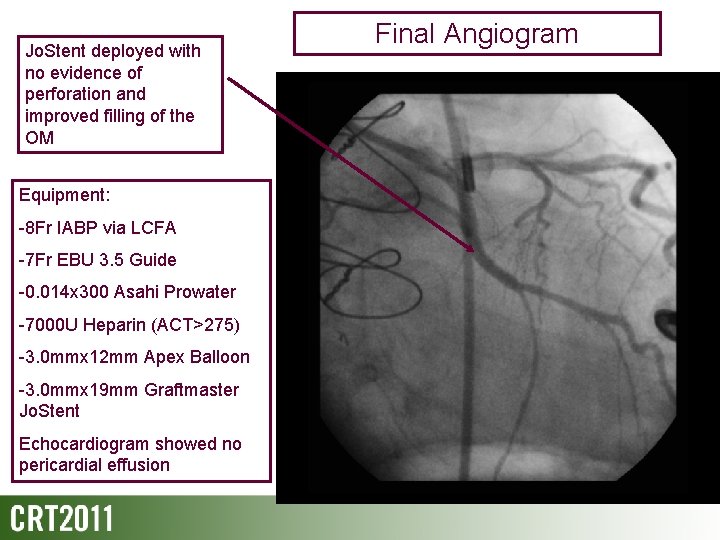
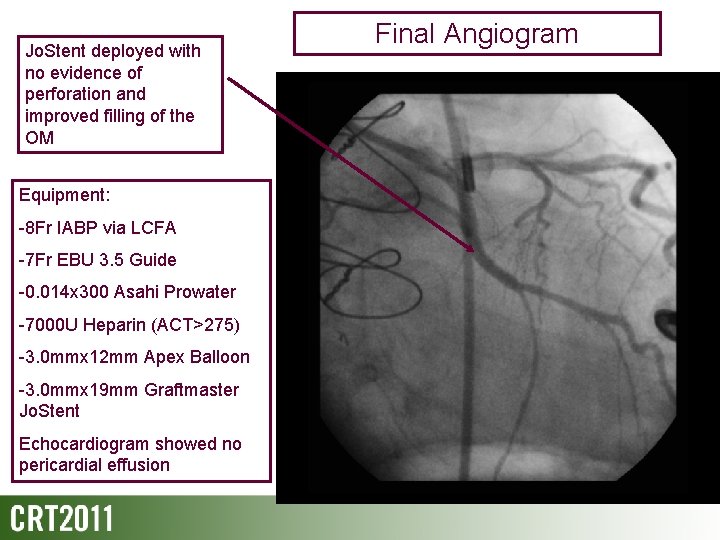
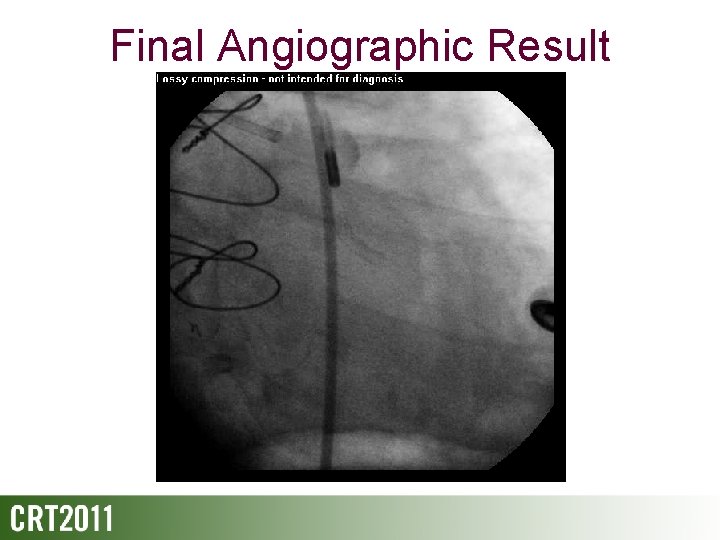
Jo. Stent deployed with no evidence of perforation and improved filling of the OM Equipment: -8 Fr IABP via LCFA -7 Fr EBU 3. 5 Guide -0. 014 x 300 Asahi Prowater -7000 U Heparin (ACT>275) -3. 0 mmx 12 mm Apex Balloon -3. 0 mmx 19 mm Graftmaster Jo. Stent Echocardiogram showed no pericardial effusion Final Angiogram
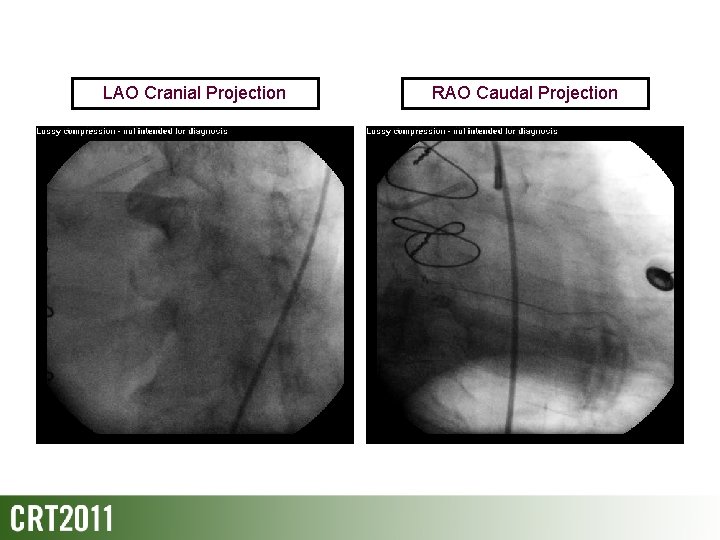
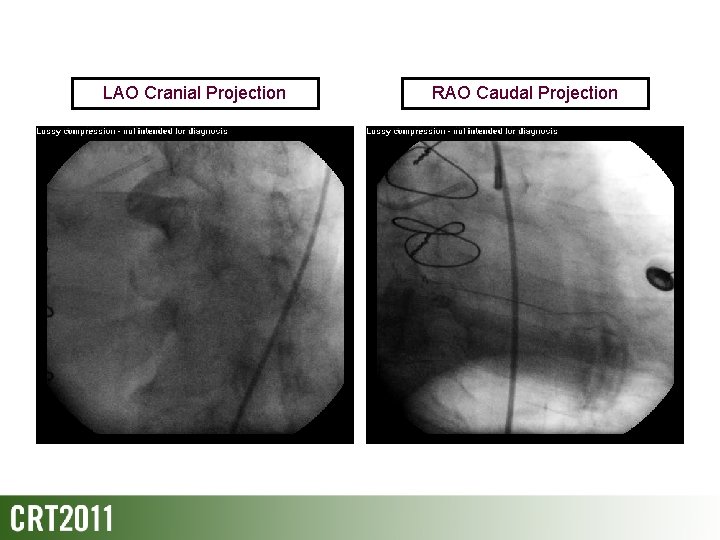
LAO Cranial Projection RAO Caudal Projection
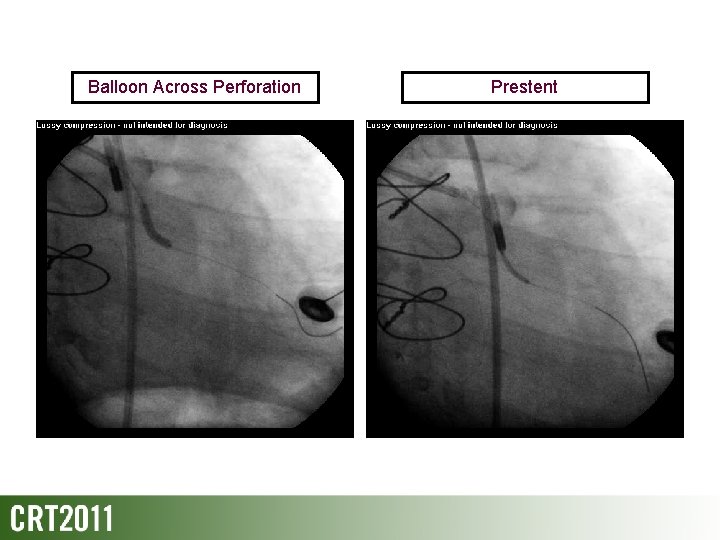
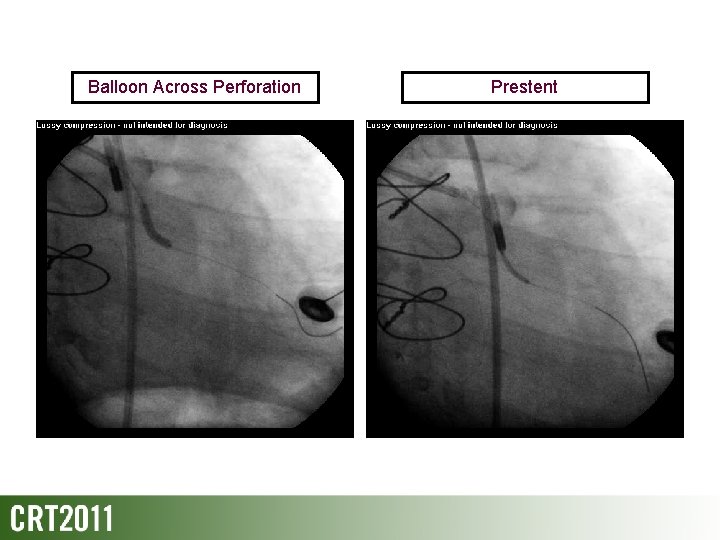
Balloon Across Perforation Prestent
Final Angiographic Result
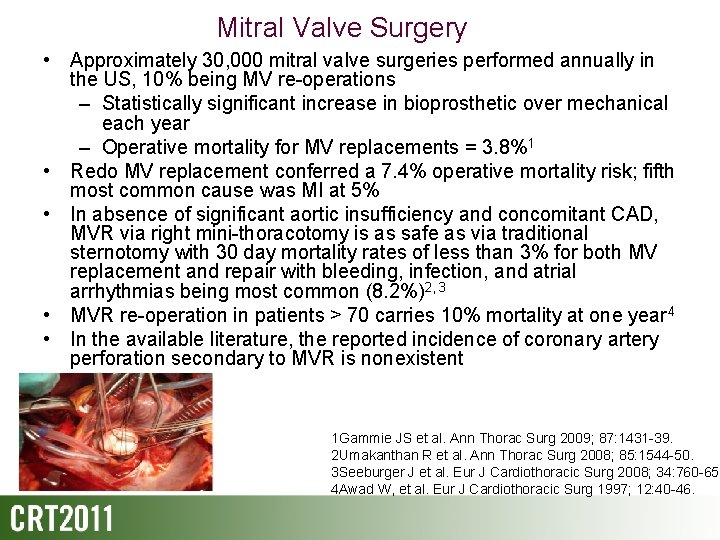
Mitral Valve Surgery • Approximately 30, 000 mitral valve surgeries performed annually in the US, 10% being MV re-operations – Statistically significant increase in bioprosthetic over mechanical each year – Operative mortality for MV replacements = 3. 8%1 • Redo MV replacement conferred a 7. 4% operative mortality risk; fifth most common cause was MI at 5% • In absence of significant aortic insufficiency and concomitant CAD, MVR via right mini-thoracotomy is as safe as via traditional sternotomy with 30 day mortality rates of less than 3% for both MV replacement and repair with bleeding, infection, and atrial arrhythmias being most common (8. 2%)2, 3 • MVR re-operation in patients > 70 carries 10% mortality at one year 4 • In the available literature, the reported incidence of coronary artery perforation secondary to MVR is nonexistent 1 Gammie JS et al. Ann Thorac Surg 2009; 87: 1431 -39. 2 Umakanthan R et al. Ann Thorac Surg 2008; 85: 1544 -50. 3 Seeburger J et al. Eur J Cardiothoracic Surg 2008; 34: 760 -65 4 Awad W, et al. Eur J Cardiothoracic Surg 1997; 12: 40 -46.
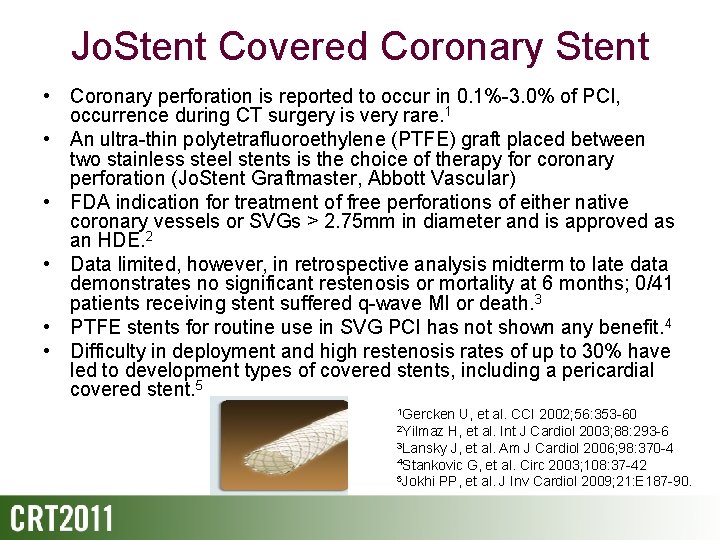
Jo. Stent Covered Coronary Stent • Coronary perforation is reported to occur in 0. 1%-3. 0% of PCI, occurrence during CT surgery is very rare. 1 • An ultra-thin polytetrafluoroethylene (PTFE) graft placed between two stainless steel stents is the choice of therapy for coronary perforation (Jo. Stent Graftmaster, Abbott Vascular) • FDA indication for treatment of free perforations of either native coronary vessels or SVGs > 2. 75 mm in diameter and is approved as an HDE. 2 • Data limited, however, in retrospective analysis midterm to late data demonstrates no significant restenosis or mortality at 6 months; 0/41 patients receiving stent suffered q-wave MI or death. 3 • PTFE stents for routine use in SVG PCI has not shown any benefit. 4 • Difficulty in deployment and high restenosis rates of up to 30% have led to development types of covered stents, including a pericardial covered stent. 5 1 Gercken U, et al. CCI 2002; 56: 353 -60 H, et al. Int J Cardiol 2003; 88: 293 -6 3 Lansky J, et al. Am J Cardiol 2006; 98: 370 -4 4 Stankovic G, et al. Circ 2003; 108: 37 -42 5 Jokhi PP, et al. J Inv Cardiol 2009; 21: E 187 -90. 2 Yilmaz
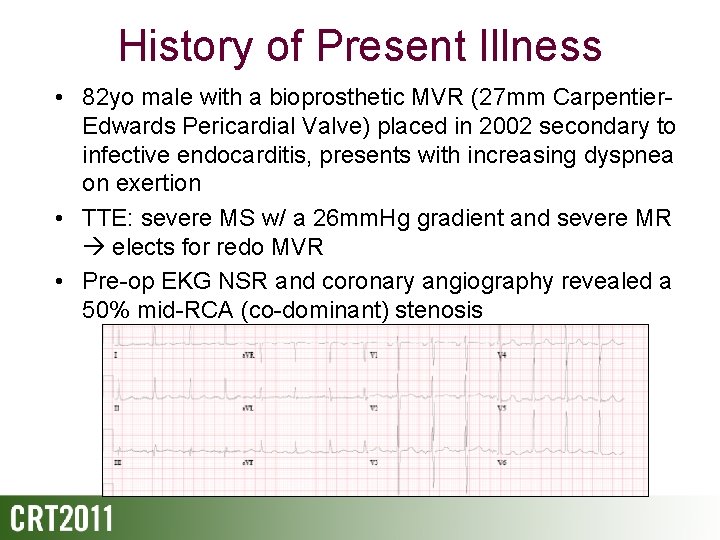
Conclusion • Pt was extubated the day following PCI and had no further VT • 12 -lead ECG following morning showed no q-waves • Discharged to rehab on POD 12, currently doing well. • Use of Jo. Stent Graftmaster covered stent has never previously been reported in use for free perforation of a coronary artery as a complication of surgery After an extensive review of the literature, this is the first case of coronary perforation post MVR presenting as a VT arrest successfully treated with a covered stent.