Acute Liver Failure Dr Eduardo Martinez Foie Gras














- Slides: 57
Acute Liver Failure Dr. Eduardo Martinez

Foie Gras � Foie gras (pronounced /fwɑːˈɡrɑː/ in English; French for "fat liver") is a food product made of the liver of a duck or goose that has been specially fattened.
Functions of the Liver � Metabolic ◦ ◦ Carb metabolism Protein and lipoprotein metabolism Fatty acid metabolism Biotransformation of drugs � Storage ◦ Glycogen ◦ Vitamins A, D, E, and K ◦ Iron and copper
Functions of the Liver � Immunological ◦ ◦ function s Synthesis of immunoglobulins Phagocytosis by Kupffer cells Filtration of bacteria Degradation of endotoxins � Excretion of bilirubin and urea formation � Haematological functions ◦ Blood reservoir ◦ Haematopoiesis in the foetus
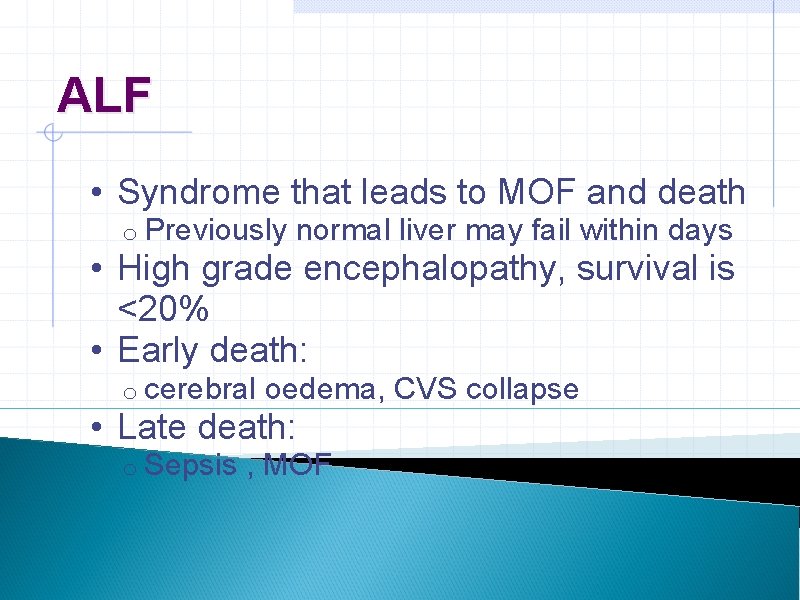
ALF • Syndrome that leads to MOF and death o Previously normal liver may fail within days • High grade encephalopathy, survival is <20% • Early death: o cerebral oedema, CVS collapse • Late death: o Sepsis , MOF
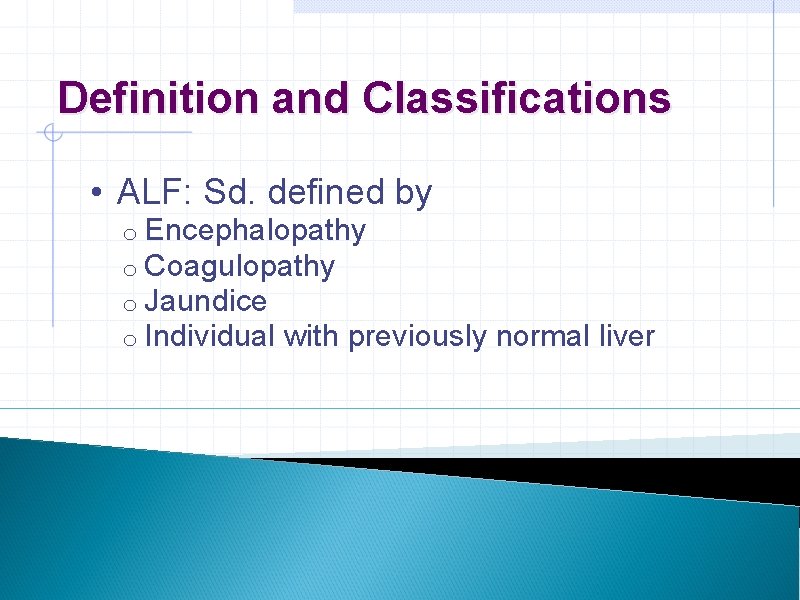
Definition and Classifications • ALF: Sd. defined by o Encephalopathy o Coagulopathy o Jaundice o Individual with previously normal liver

Definition and Classifications • Fulminant Hepatic Failure o Potentially reversible condition o Consequence of severe liver injury o Encephalopathy appears within 8 wks. of initial Sx. o Absence of pre-existing liver ds.
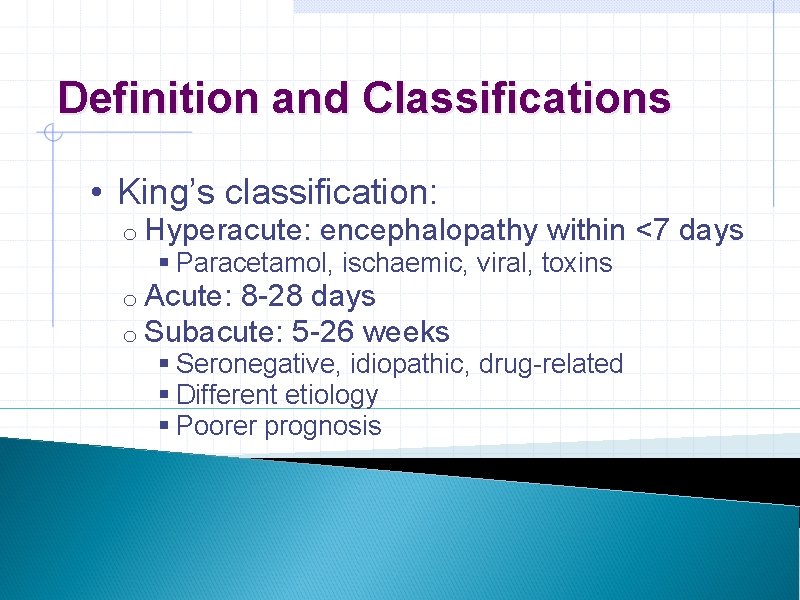
Definition and Classifications • King’s classification: o Hyperacute: encephalopathy within <7 days § Paracetamol, ischaemic, viral, toxins o Acute: 8 -28 days o Subacute: 5 -26 weeks § Seronegative, idiopathic, drug-related § Different etiology § Poorer prognosis
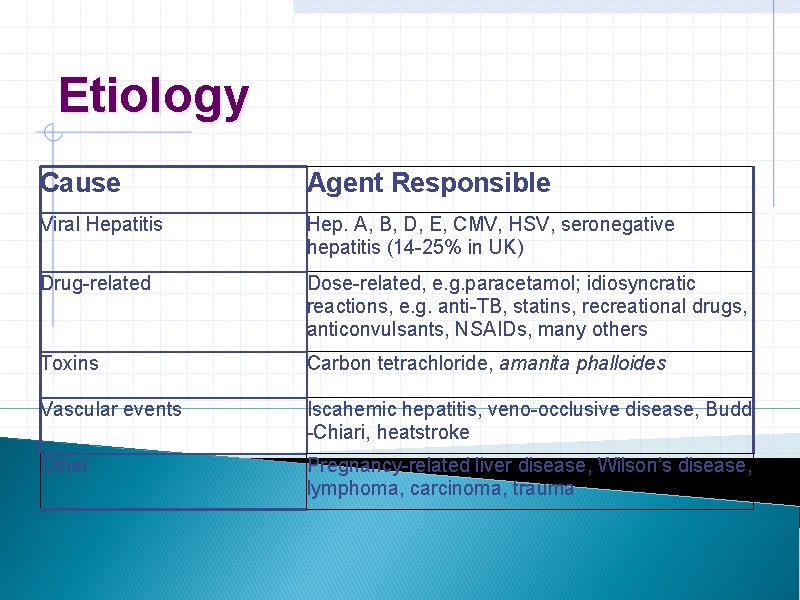
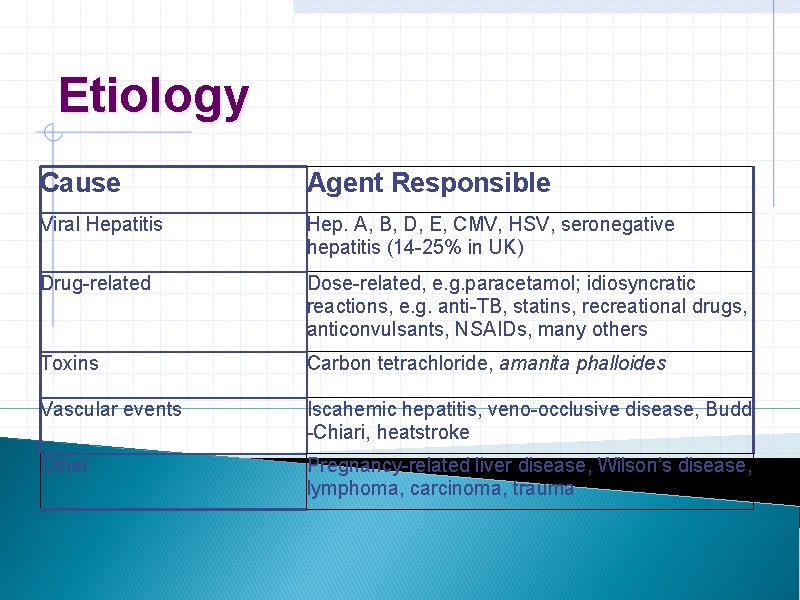
Etiology Cause Agent Responsible Viral Hepatitis Hep. A, B, D, E, CMV, HSV, seronegative hepatitis (14 -25% in UK) Drug-related Dose-related, e. g. paracetamol; idiosyncratic reactions, e. g. anti-TB, statins, recreational drugs, anticonvulsants, NSAIDs, many others Toxins Carbon tetrachloride, amanita phalloides Vascular events Iscahemic hepatitis, veno-occlusive disease, Budd -Chiari, heatstroke Other Pregnancy-related liver disease, Wilson’s disease, lymphoma, carcinoma, trauma

Etiology • Most common causes: o Worldwide: § Hepatotrophic viruses A-E o UK § Paracetamol overdose § Seronegative or non-A-E hepatitis § Idiosynchratic drug rxs. or Wilson’s ds.
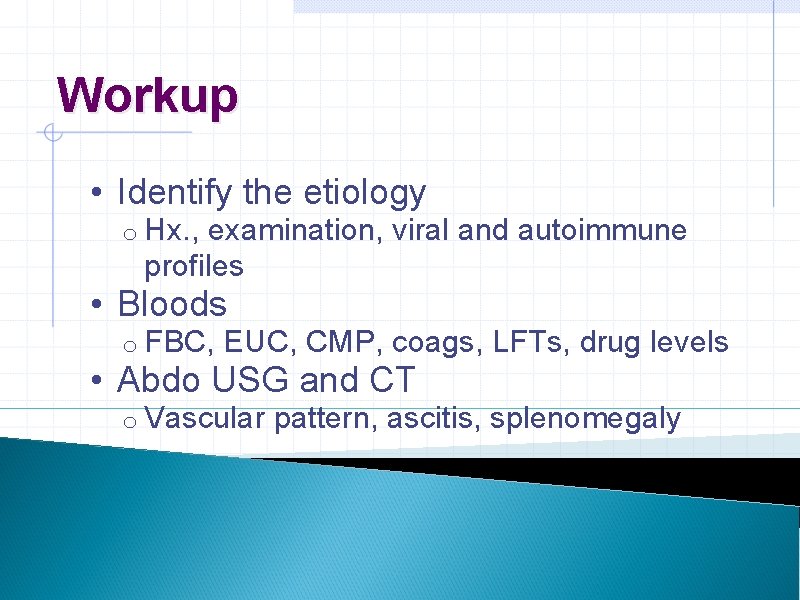
Workup • Identify the etiology o Hx. , examination, viral and autoimmune profiles • Bloods o FBC, EUC, CMP, coags, LFTs, drug levels • Abdo USG and CT o Vascular pattern, ascitis, splenomegaly
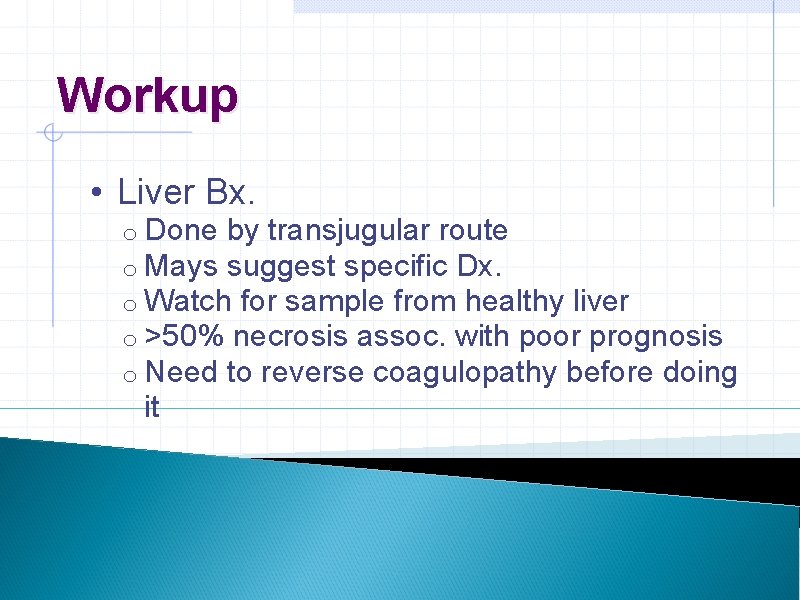
Workup • Liver Bx. o Done by transjugular route o Mays suggest specific Dx. o Watch for sample from healthy liver o >50% necrosis assoc. with poor prognosis o Need to reverse coagulopathy before doing it
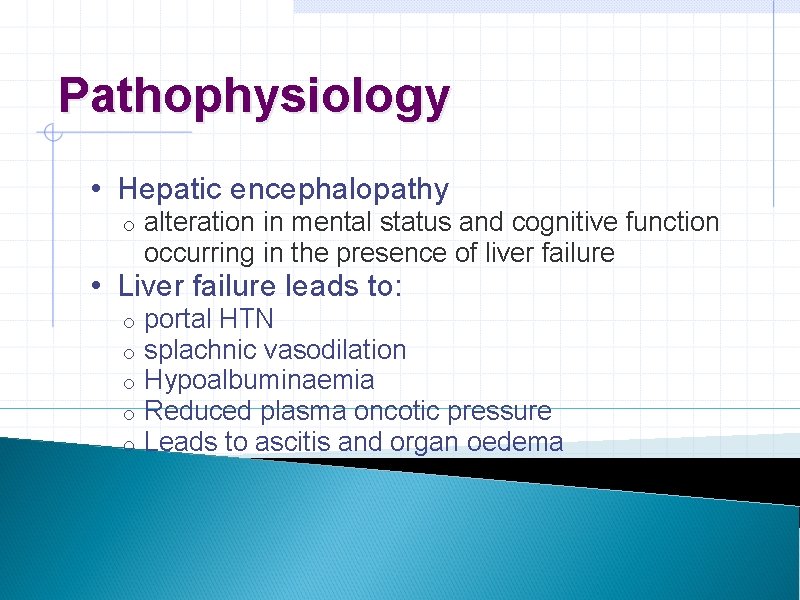
Pathophysiology • Hepatic encephalopathy o alteration in mental status and cognitive function occurring in the presence of liver failure • Liver failure leads to: o o o portal HTN splachnic vasodilation Hypoalbuminaemia Reduced plasma oncotic pressure Leads to ascitis and organ oedema
Pathophysiology • Decreased intravascular volume o Kidneys try to “compensate” and retain Na+ and water making oedema worse • Also, • Gut-derived toxins reach the liver o Ammonia levels are often high o Correlation between ammonia and symptoms is poor

Clinical Features • Depend on the severity, which depends on: o Etiology o Speed of onset of symptoms • Non-specific o N&V, abdo pain • Neurological o Confusion, agitation, coma

Scale Of Hepatic Encephalopathy Grade Level of Consciousness Personality and Intellect Neurologic Signs Electroencephalogram (EEG) Abnormalities 0 Normal None Subclini cal Normal Abnormalities only on psychometric testing None 1 Day/night sleep reversal, restlessness Forgetfulness, mild confusion, agitation, irritability Tremor, apraxia, incoordination, impaired handwriting Triphasic waves (5 Hz) 2 Lethargy, slowed responses Disorientation to time, loss of inhibition, inappropriate behavior Asterixis, dysarthria, ataxia, hypoactive reflexes Triphasic waves (5 Hz) 3 Somnolence, confusion Disorientation to place, aggressive behavior Asterixis, muscular rigidity, Babinski signs, hyperactive reflexes Triphasic waves (5 Hz) 4 Coma None Decerebration Delta/slow wave activity

Clinical Features • Mortality is higher for Grade III/IV o Mostly due to cerebral oedema o Occurs in 80% of pts. w/ALF § Due to lack of equilibration of osmotic gradient § 30% of those have cerebellar tonsil and/or temporal lobe herniation causing death o We’re now better at treating cerebral oedema
Clinical Features • Elevated ICP o HTN, bradycardia, blown pupils: occur late o CTB won’t tell you o ICP monitor is best way of knowing • CVS changes o Similar to sepsis o Might be due to infection
Clinical Features • Renal failure o Oliguric o Poor prognosis § Except with paracetamol overdose where it has a good prognosis • Impaired immunity o Decreased complement synthesis, Kupffer cell dysfunction, poor neutrophil adhesion and superoxide production

Clinical Features • Increased susceptibility to infection o 80% of pts. have bacteriologically proven infections o Major sepsis is contributor to death in 20% of cases § Staph. aureus 70% of gram (+) § E. Coli most common gram (-) § C. albicans in 30% of pts.
Monitoring • Pts. need HDU/ICU • Need CVC and continuous IBP monitoring and IDC • Baseline ABG and lactate o Lactate >3 mmo/L after adequate resus has same sensi. and speci. for death as The King’s College Hospital criteria
Prognosis • Early indicators of prognosis in fulminant hepatic failure. § O'Grady JG, Alexander GJ, Hayllar KM, Williams R. § Gastroenterology. 1989 Aug; 97(2): 439 -45. • King’s Collage Hospital Criteria Originally devised as prognostic criteria to predict patient survival without liver transplant o Now used as selection criteria for potential liver transplant recipients o

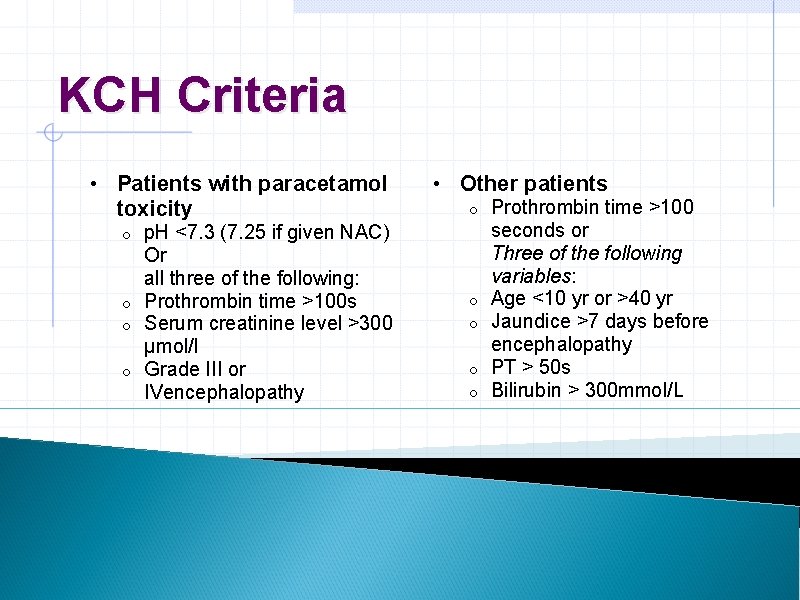
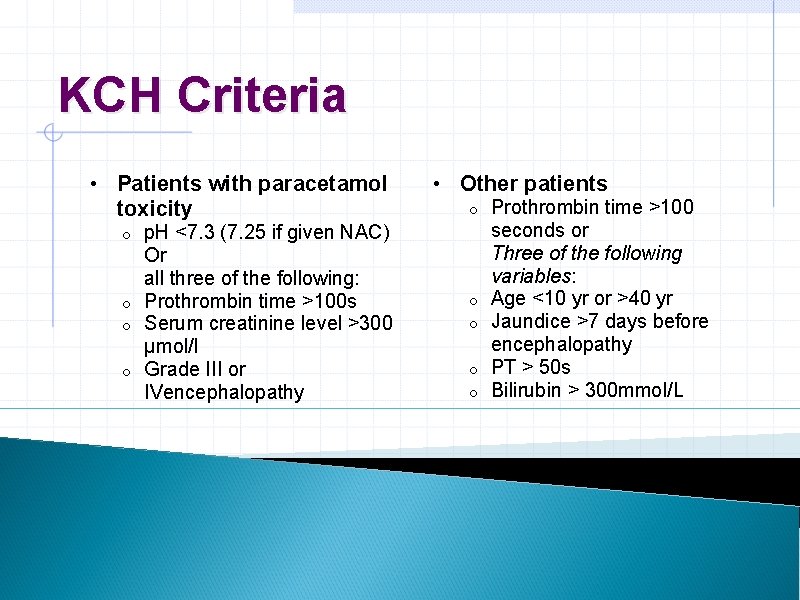
KCH Criteria • Patients with paracetamol toxicity o o o o p. H <7. 3 (7. 25 if given NAC) Or all three of the following: Prothrombin time >100 s Serum creatinine level >300 μmol/l Grade III or IVencephalopathy • Other patients o o o Prothrombin time >100 seconds or Three of the following variables: Age <10 yr or >40 yr Jaundice >7 days before encephalopathy PT > 50 s Bilirubin > 300 mmol/L
KCH Criteria � Positive predictive value for ICU death without transplantation of 0. 98 � Negative predictive value of 0. 82
Treatment • Intensive care of patients with acute liver failure: recommendations of the U. S. Acute Liver Failure Study Group. § Stravitz RT, Kramer AH, Davern T, Shaikh AO, Caldwell SH et al. § Critical Care Medicine 2007; 35: 2498 -508
Treatment • Adult U. S. Acute Liver Failure Study Group o Data from § 23 liver transplant centers § >1, 110 pts. o In 2005 convened to § review literature on management § Care of pts. w/high ICPs § Compare practices of different centers
General Management • Admit to hospital and HDU/ICU o When evidence of ALF § E. g. : INR>1. 5 o D/W: § Physician § Intensivist § Nearest transplant center § Regarding best time to refer
General Management • Etiology-specific treatment o Studies only for paracetamol overdose o NAC regardless of time of overdose § IV if Grade I encephalopathy § Hypotension § Any other reason PO NAC is not tolerated o HELLP or acute fatty liver of pregnancy § Tx. Is immediate delivery
General Management • NAC o 150 mg/kg IV in 200 ml NS over 15 -60 mins o 50 mg/kg IV over 4 hrs o 100 mg/kg IV over 16 hrs § Total dose: 300 mg/kg over 20 hrs o Infusion recommended until there is evidence of improved hepatic function rather than time or paracetamol levels
Management of Complications • Hepatic encephalopathy and hyperammonaemia • Infections • Sedation and analgesia • Bleeding diathesis • Nutrition • Seizures • Circulatory dysfunction
Encephalopathy • Standard treatment: o Lactulose § Watch for: § Abdo distension § Oesophageal varices will need a scope § Avoid intravascular depletion o Non-absorbable ATBs § Neomycin not recommended by ALFSG because of nephrotoxicity
Infection prophylaxis and surveillance • Infection is one of main causes of death in ALF • Most common sites: o o o Lung Urinary tract Blood o o o Gram (+) cocci: Staph aureus Gram (-) rods: E. coli Fungi: candida • Most common M. O.
Infection prophylaxis and surveillance • Empirical ATBs are recommended by ALFSG when: o o Surveillance cultures reveal significant isolates Advanced stage (III/IV) encephalopathy Refractory hypotension SIRS • 3 rd gen. Cephalosporin or Timentin, Vancomycin, Fluconazole

Sedation and analgesia • Agitation contributes to raised ICP • Propofol vs. Benzos Both increase GABA neurotransmission, therefore may exacerbate encephalopathy o Propofol decreases ICP and wears off quickly o • Opioids o o Shorter acting are preferable When there is concommitant ARF, avoid morphine or pethidine due to metabolite accumulation
Correction of bleeding diathesis • Pts. with ALF are by definition coagulopathic o o Low plts. and fibrinogen, Vit. K deficient Spontaneous bleeding is rare o o INR 1. 5 Plts. 50, 000 • Very difficult to obtain complete correction • ALFSG recommends aiming for:
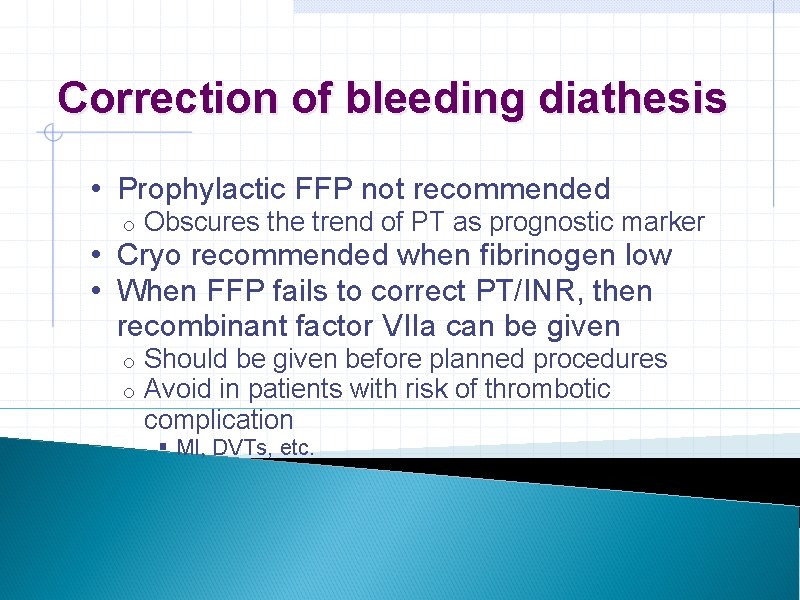
Correction of bleeding diathesis • Prophylactic FFP not recommended o Obscures the trend of PT as prognostic marker o o Should be given before planned procedures Avoid in patients with risk of thrombotic complication • Cryo recommended when fibrinogen low • When FFP fails to correct PT/INR, then recombinant factor VIIa can be given § MI, DVTs, etc.
Correction of bleeding diathesis • UGI bleeding o reduced by H 2 antagonists or PPIs • TEDS and Scuds
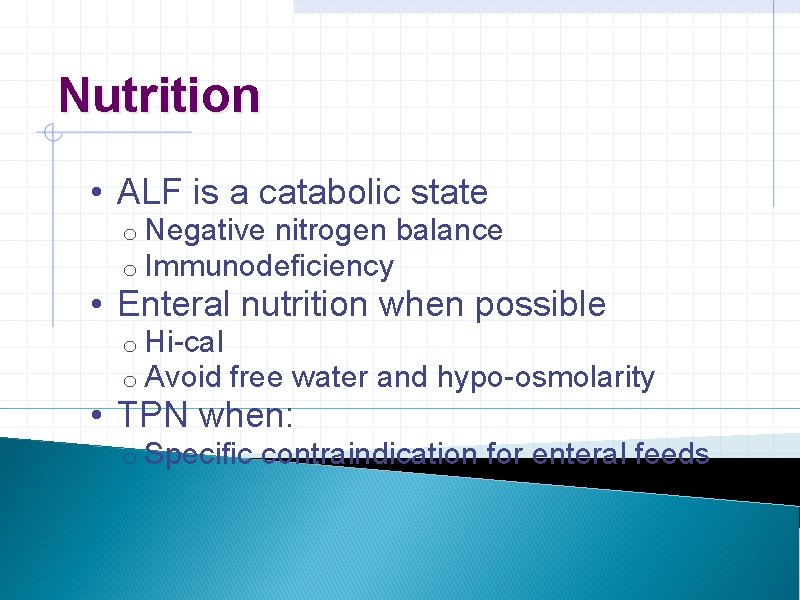
Nutrition • ALF is a catabolic state o Negative nitrogen balance o Immunodeficiency • Enteral nutrition when possible o Hi-cal o Avoid free water and hypo-osmolarity • TPN when: o Specific contraindication for enteral feeds
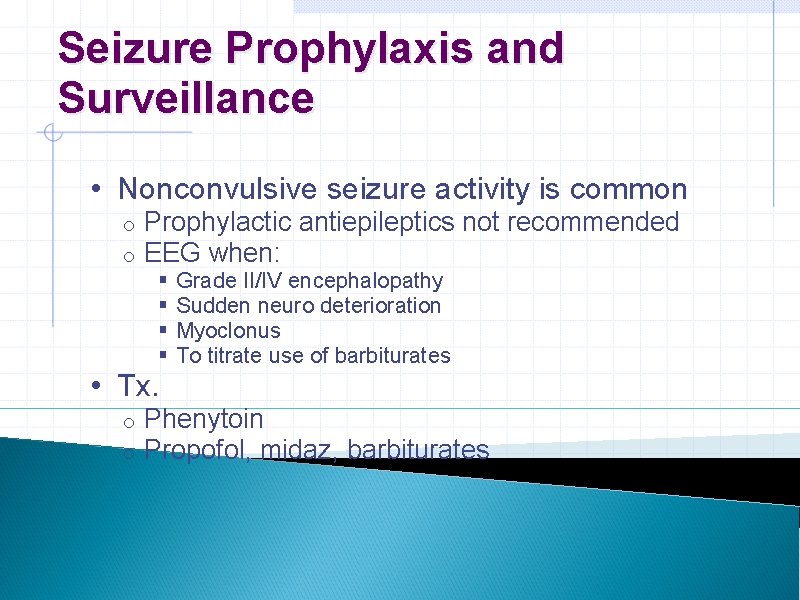
Seizure Prophylaxis and Surveillance • Nonconvulsive seizure activity is common o o Prophylactic antiepileptics not recommended EEG when: § § Grade II/IV encephalopathy Sudden neuro deterioration Myoclonus To titrate use of barbiturates • Tx. o o Phenytoin Propofol, midaz, barbiturates
CVS Dysfunction • Correct hypovolaemia before starting vasopressors • Pressors needed for hypotension and low CPP o o o Norad is first line, can give high dose dopamine Adrenaline may compromise HBF Vasopressin not recommended because directly causes cerebral vasodilation and high ICPs • Medium doses of steroid may improve pressor response

Mx. of Cerebral Oedema and Intracranial Hypertension • Raised ICP due to cerebral oedema is one of major causes of M&M • CTB for Grade III/IV o To rule out anything else, i. e. bleed • ICP monitor o Grade III/IV encephalopathy o To optimize CPP o Not routine
Raised ICP • Aim for o ICP<25 mm. Hg o CPP 50 -80 • General recommendations o Keep it quiet , minimize chest physio and ETT suctioning, head at 30 o o Don’t treat spontaneous hyperventilation, keep Pa. CO 2 35 -40 mm. Hg, treat fever aggressively with physical measures

Raised ICP • Specific management o Manitol: first line therapy o Hypertonic Saline o Induced hypothermia o Barbiturate coma o Indomethacin: 25 mg IV over 1 min.
Mechanical Ventilation • When to intubate: o Respiratory failure o Airway protection in advanced encephalopathy o Agitation o Imminent ICP monitor placement
Mechanical Ventilation • Pts. w/ALF often develop ALI/ARDS o Follow ARDSNet protocol o Avoid high PEEP § Use the minimum needed
CRRT • Indicated for: o Renal failure o Fluid overload o Metabolic derangements o Need to create space for IV colloids, i. e. FFP • CRRT preferred over IRRT o HD instability common
CRRT • Use citrate over heparin o Monitor ionized calcium • Use bicarb buffer over lactate or citrate buffer o Liver won’t be able to convert them to HCO 3 - • Avoid hyponatraemia o May exacerbate cerebral oedema
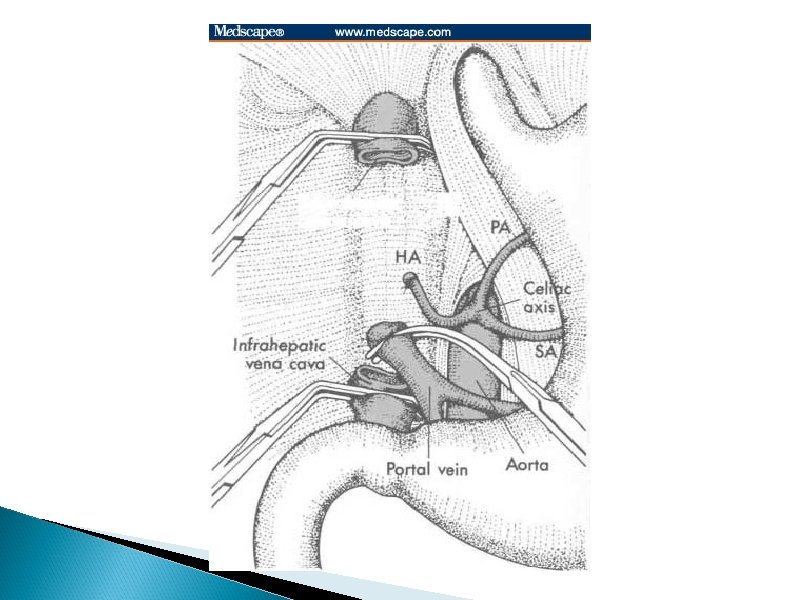
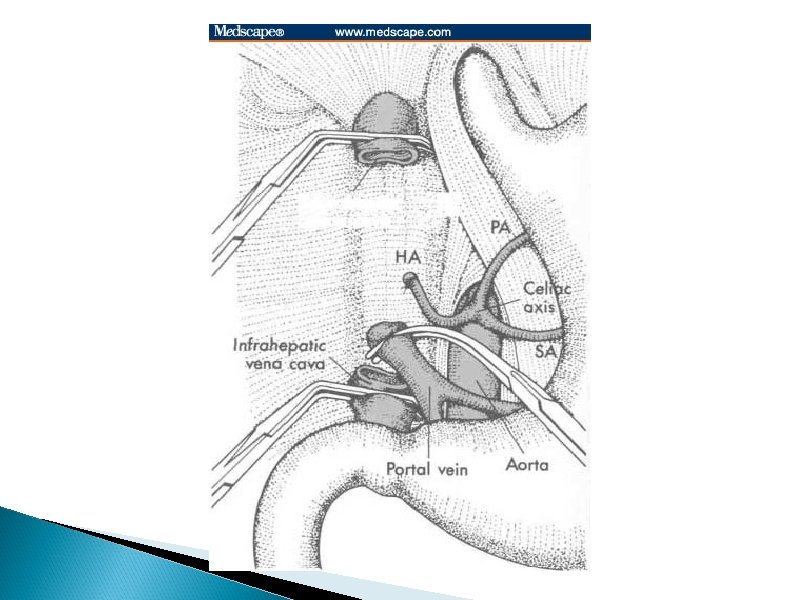
Liver Transplant � Orthotopic liver transplant is the definitive treatment for patients who meet the criteria ◦ or·tho·top·ic (ôrth-tpk)adj. In the normal or usual position � 1 yr. and 5 yr. survival of patients undergoing OLT for ALF is about 20% lower than elective cases for cirrhotic patients � Auxiliary liver transplantation is and alternative
Liver Transplant � Absolute ◦ ◦ contraindications Overwhelming sepsis Refractory hypotension AIDS Uncontrolled raised ICP with likely permanent damange

Hepatic assist devices � MARS: molecular absorption and recirculation system ◦ Adaptation of haemodialysis ◦ Blood is dialysed against 20% albumin �Shown to improve encephalopathy, renal function and haemodynamic parameters ◦ The efficacy of this technique has not yet been studied

So, what have we learned?

Thank you!
 West haven criteria hepatic encephalopathy
West haven criteria hepatic encephalopathy Cushings triad
Cushings triad Hepatic encephalopathy stages
Hepatic encephalopathy stages Foie gras egypt
Foie gras egypt Dr eduardo martinez
Dr eduardo martinez Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Neonatal liver failure
Neonatal liver failure Hepatic encephalopathy symptoms
Hepatic encephalopathy symptoms Acute vs chronic heart failure
Acute vs chronic heart failure Acute brain failure
Acute brain failure Urinalysis
Urinalysis Capture beat
Capture beat Ductile fracture mechanism
Ductile fracture mechanism Supparerk vision center
Supparerk vision center Classification aast rate
Classification aast rate Hepar lobatum carcinomatosum
Hepar lobatum carcinomatosum Segmentation hépatique tdm
Segmentation hépatique tdm Foie multinodulaire
Foie multinodulaire Manchon tissulaire
Manchon tissulaire Palpation du foie méthode de gilbert
Palpation du foie méthode de gilbert Ligament rond et falciforme
Ligament rond et falciforme Lobe caudé
Lobe caudé Examen clinique du foie
Examen clinique du foie Pars superior
Pars superior Topographie du foie
Topographie du foie Vsh foie
Vsh foie Gras 40ag
Gras 40ag Who used first the word photography?
Who used first the word photography? Gras mahakosh gov in
Gras mahakosh gov in Gras savoye collectivités locales
Gras savoye collectivités locales Gras mahakosh e challan
Gras mahakosh e challan Fema gras
Fema gras Molire
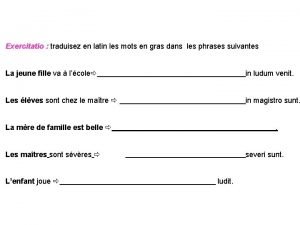
Molire Les mots en gras
Les mots en gras Spring spinnekop
Spring spinnekop Sepa gras savoye
Sepa gras savoye Gras bilong hed
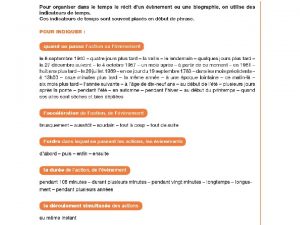
Gras bilong hed Les information suivantes
Les information suivantes Niveles de la escala gras
Niveles de la escala gras The word “photography” literally means
The word “photography” literally means Gras frans
Gras frans Antonio lopo martinez
Antonio lopo martinez Rogelio martinez masegosa
Rogelio martinez masegosa Kristin stephens-martinez
Kristin stephens-martinez Andreu cardo martinez
Andreu cardo martinez Kristian frich martínez de velasco
Kristian frich martínez de velasco Juan antonio martinez segura
Juan antonio martinez segura Eugenia martinez vallejo
Eugenia martinez vallejo Manuel rodriguez martinez
Manuel rodriguez martinez Robert martínez
Robert martínez Vicente balaguer jose rizal
Vicente balaguer jose rizal Mallory martinez
Mallory martinez Yumari martinez
Yumari martinez Sociloga
Sociloga Becca steier
Becca steier Cristo de la clemencia juan martinez montañes
Cristo de la clemencia juan martinez montañes