Acute Limb Ischemia Definition Etiology Patophysiology Clinical Evaluation
Acute Limb Ischemia Definition, Etiology & Patophysiology Clinical Evaluation & Classes Ali SABBOUR Prof. of Vascular Surgery, Ain Shams University Management

Definition of Acute Limb Ischemia Sudden decrease of arterial limb perfusion causing threat to limb viability

Etiology of acute limb ischemia Acute arterial embolism: Acute arterial thrombosis: Acute traumatic ischemia: Of a relatively health arterial tree Of a previously diseased arterial tree
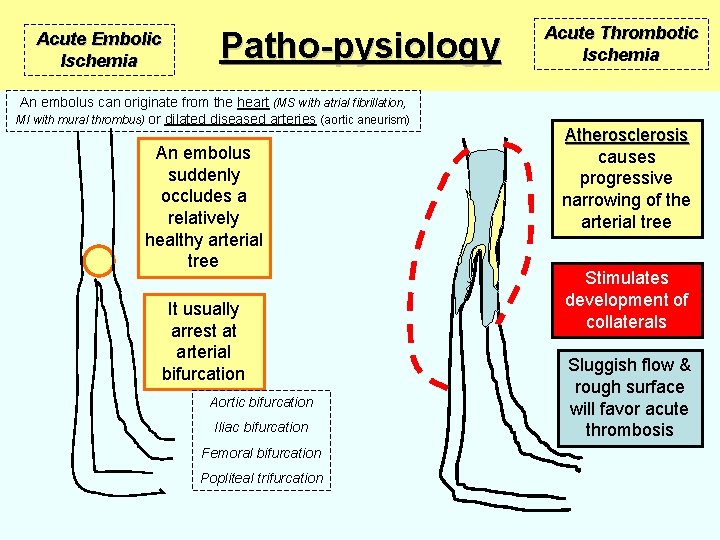
Acute Embolic Ischemia Patho-pysiology An embolus can originate from the heart (MS with atrial fibrillation, MI with mural thrombus) or dilated diseased arteries (aortic aneurism) An embolus suddenly occludes a relatively healthy arterial tree It usually arrest at arterial bifurcation Aortic bifurcation Iliac bifurcation Femoral bifurcation Popliteal trifurcation Acute Thrombotic Ischemia Atherosclerosis causes progressive narrowing of the arterial tree Stimulates development of collaterals Sluggish flow & rough surface will favor acute thrombosis
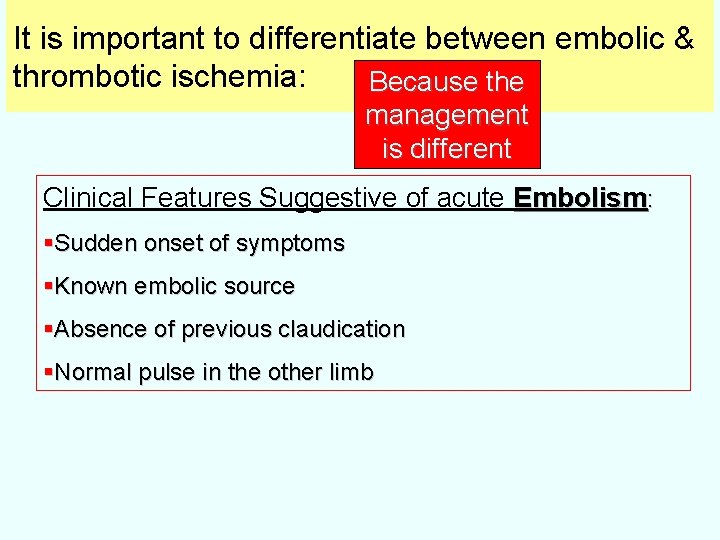
It is important to differentiate between embolic & thrombotic ischemia: Because the management is different Clinical Features Suggestive of acute Embolism: §Sudden onset of symptoms §Known embolic source §Absence of previous claudication §Normal pulse in the other limb
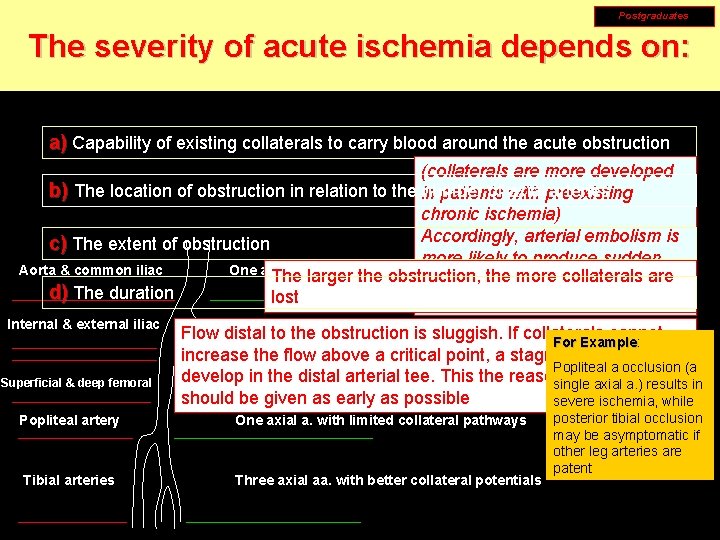
Postgraduates The severity of acute ischemia depends on: a) Capability of existing collaterals to carry blood around the acute obstruction (collaterals are more developed b) The location of obstruction in relation to the in number of with axialpreexisting arteries patients chronic ischemia) Accordingly, arterial embolism is c) The extent of obstruction more likely to produce sudden One axial a. with limited collateral pathways Aorta & common iliac The larger the obstruction, the&more collaterals symptoms severe ischemiaare d) The duration lost then arterial thrombosis Internal & external iliac Superficial & deep femoral Popliteal artery Tibial arteries Two axial aa. With better collateral potentials Flow distal to the obstruction is sluggish. If collaterals cannot For Example: Example increase the flow above a critical point, a stagnation clot will Popliteal a occlusion (a develop in axial the distal arterial tee. Thispotentials the reason whyaxial heparin Two aa. With better collateral single a. ) results in should be given as early as possible severe ischemia, while One axial a. with limited collateral pathways Three axial aa. with better collateral potentials posterior tibial occlusion may be asymptomatic if other leg arteries are patent
Definition: Sudden decrease of arterial limb perfusion causing threat to limb viability Etiology: 1 -Embolic (Rh. heart w mitral stenosis & AF or Ischemic heart w acute myocardial infarction & mural thrombus or extra-cardiac embolism from aneurismal arteries) 2 -Thrombotic acute ischemia on top of atherosclerotic arterial stenosis Pathology: onset of symptoms is more acute in embolic ischemia (absent collaterals) Other factors determine the severity of acute ischemia Clinical Picture Management

Clinical Evaluation of Acute Ischemia (Clinical Picture) Symptoms of acute ischemia: Pain Diffuse foot & leg severe aching pain of acute onset (more acute in embolic ischemia) Pain may diminish in intensity by time if collaterals open improving circulation, or if ischemia progresses causing ischemic sensory loss Coldness is an early symptom Numbness followed by sensory loss (late) Muscle weakness (heavy limb) followed by paralysis (late)
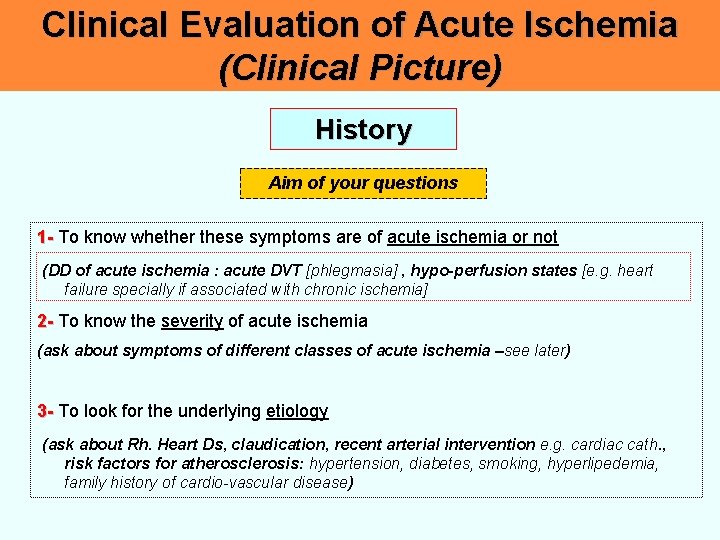
Clinical Evaluation of Acute Ischemia (Clinical Picture) History Aim of your questions 1 - To know whether these symptoms are of acute ischemia or not (DD of acute ischemia : acute DVT [phlegmasia] , hypo-perfusion states [e. g. heart failure specially if associated with chronic ischemia] 2 - To know the severity of acute ischemia (ask about symptoms of different classes of acute ischemia –see later) 3 - To look for the underlying etiology (ask about Rh. Heart Ds, claudication, recent arterial intervention e. g. cardiac cath. , risk factors for atherosclerosis: hypertension, diabetes, smoking, hyperlipedemia, family history of cardio-vascular disease)
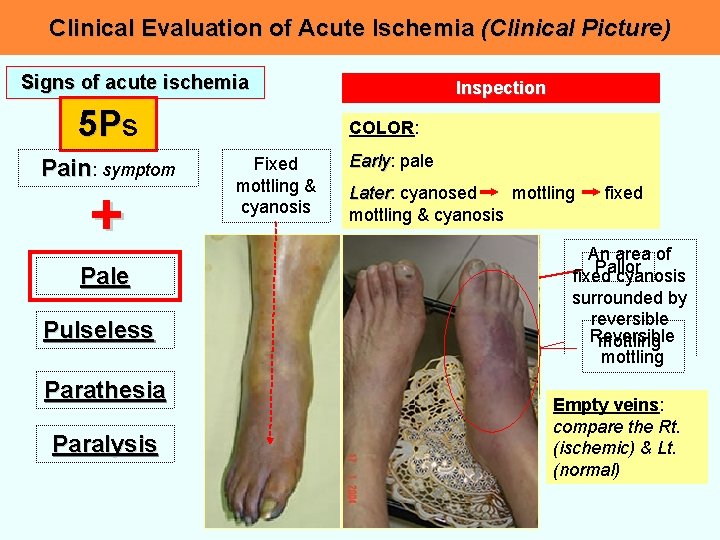
Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia 5 Ps Pain: symptom + Pale Pulseless Parathesia Paralysis Inspection COLOR: Fixed mottling & cyanosis Early: Early pale Later: mottling Later cyanosed mottling & cyanosis fixed An area of Pallor fixed cyanosis surrounded by reversible Reversible mottling Empty veins: compare the Rt. (ischemic) & Lt. (normal)

Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia Palpation 5 Ps Pain: symptom + Femoral Popliteal Posterior tibial Dorsalis pedis Pale Pulseless Parathesia Palpate peripheral pulses, compare with the other side & write it down on a sketch Paralysis Temperature: Temperature the limb is cold with a level of temperature change (compare the two limbs) Slow capillary refilling of the skin after finger pressure
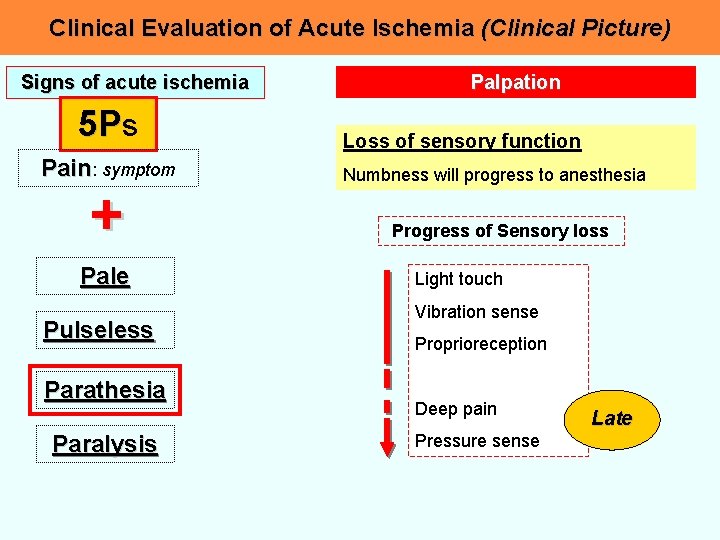
Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia 5 Ps Pain: symptom + Pale Pulseless Parathesia Paralysis Palpation Loss of sensory function Numbness will progress to anesthesia Progress of Sensory loss Light touch Vibration sense Proprioreception Deep pain Pressure sense Late
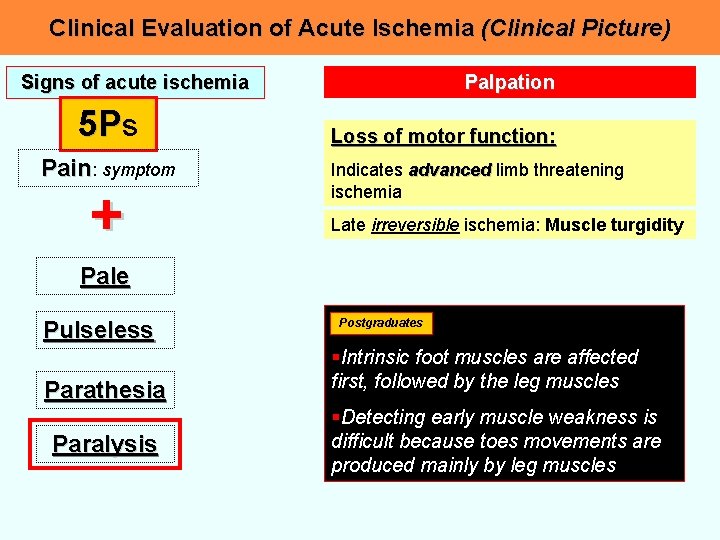
Clinical Evaluation of Acute Ischemia (Clinical Picture) Signs of acute ischemia 5 Ps Pain: symptom + Palpation Loss of motor function: Indicates advanced limb threatening ischemia Late irreversible ischemia: Muscle turgidity Pale Pulseless Parathesia Paralysis Postgraduates §Intrinsic foot muscles are affected first, followed by the leg muscles §Detecting early muscle weakness is difficult because toes movements are produced mainly by leg muscles
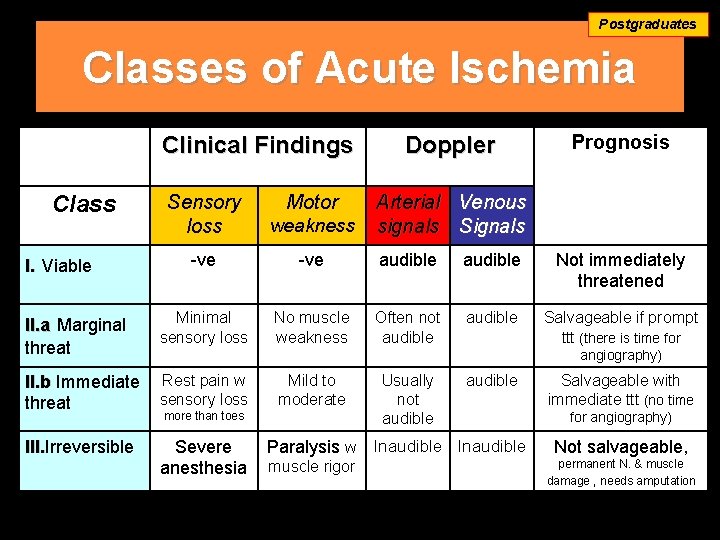
Postgraduates Classes of Acute Ischemia Clinical Findings Prognosis Sensory loss weakness -ve audible Not immediately threatened II. a Marginal threat Minimal sensory loss No muscle weakness Often not audible Salvageable if prompt ttt (there is time for II. b Immediate threat Rest pain w sensory loss III. Irreversible III. Severe anesthesia Class I. Viable Motor Doppler Arterial Venous signals Signals angiography) Mild to moderate more than toes Usually not audible Paralysis w Inaudible muscle rigor Salvageable with immediate ttt (no time for angiography) Not salvageable, permanent N. & muscle damage , needs amputation
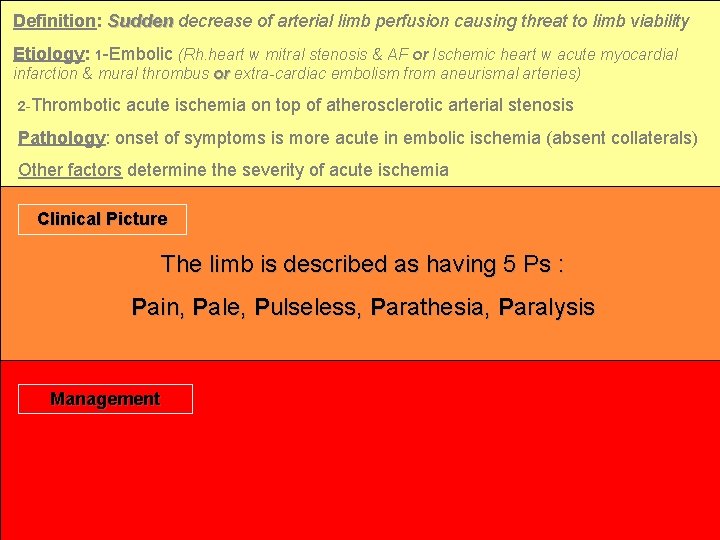
Definition: Sudden decrease of arterial limb perfusion causing threat to limb viability Etiology: 1 -Embolic (Rh. heart w mitral stenosis & AF or Ischemic heart w acute myocardial infarction & mural thrombus or extra-cardiac embolism from aneurismal arteries) 2 -Thrombotic acute ischemia on top of atherosclerotic arterial stenosis Pathology: onset of symptoms is more acute in embolic ischemia (absent collaterals) Other factors determine the severity of acute ischemia Clinical Picture The limb is described as having 5 Ps : Pain, Pale, Pulseless, Parathesia, Paralysis Management
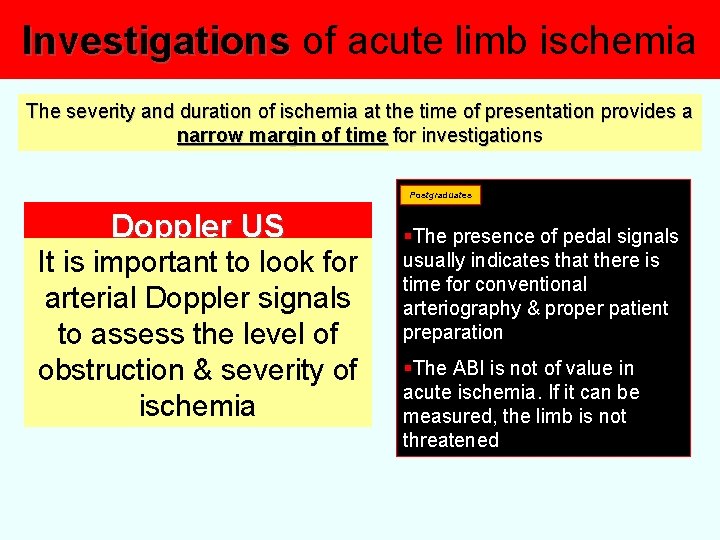
Investigations of acute limb ischemia The severity and duration of ischemia at the time of presentation provides a narrow margin of time for investigations Postgraduates Doppler US It is important to look for arterial Doppler signals to assess the level of obstruction & severity of ischemia §The presence of pedal signals usually indicates that there is time for conventional arteriography & proper patient preparation §The ABI is not of value in acute ischemia. If it can be measured, the limb is not threatened
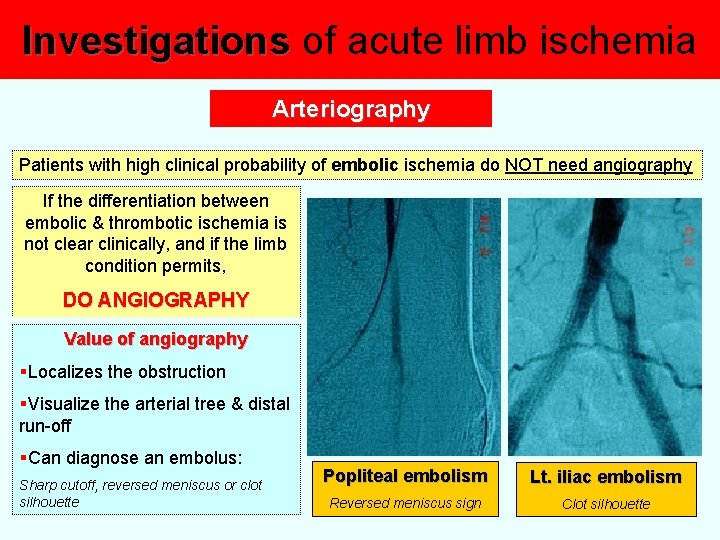
Investigations of acute limb ischemia Arteriography Patients with high clinical probability of embolic ischemia do NOT need angiography If the differentiation between embolic & thrombotic ischemia is not clear clinically, and if the limb condition permits, DO ANGIOGRAPHY Value of angiography §Localizes the obstruction §Visualize the arterial tree & distal run-off §Can diagnose an embolus: Sharp cutoff, reversed meniscus or clot silhouette Popliteal embolism Lt. iliac embolism Reversed meniscus sign Clot silhouette
Treatment of acute limb ischemia A Once you diagnose §Immediate anticoagulation with heparin to avoid clot propagation §Appropriate analgesia §Simple measures to improve existing perfusion: • Keep the foot dependant • Avoid pressure over the heal • Avoid extremes of temperature (cold induces vasospasm, heal raises the metabolic rate) • Maximum tissue oxygenation (oxygen inhalation) • Correct hypotension §Start treatment of other associated cardiac conditions (CHF, AF)
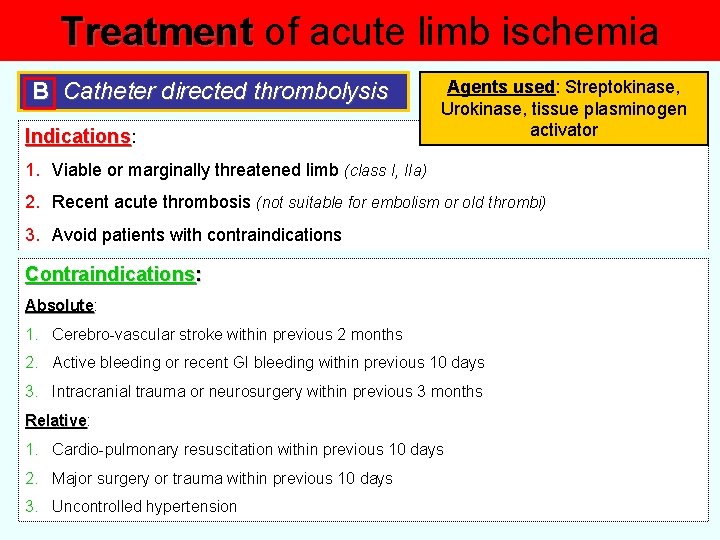
Treatment of acute limb ischemia B Catheter directed thrombolysis Indications: Agents used: Streptokinase, Urokinase, tissue plasminogen activator 1. Viable or marginally threatened limb (class I, IIa) 2. Recent acute thrombosis (not suitable for embolism or old thrombi) 3. Avoid patients with contraindications Contraindications: Absolute 1. Cerebro-vascular stroke within previous 2 months 2. Active bleeding or recent GI bleeding within previous 10 days 3. Intracranial trauma or neurosurgery within previous 3 months Relative: Relative 1. Cardio-pulmonary resuscitation within previous 10 days 2. Major surgery or trauma within previous 10 days 3. Uncontrolled hypertension
Treatment of acute limb ischemia C Surgery 1 - Acute embolism: Catheter embolectomy under local anesthesia 2 - Immediate surgical revascularization is indicated in class IIb, or class I, IIa when thrombolysis is not possible or contraindicated A combination of different procedures can be done: §Arterial exploration at different sites §Arterial thrombectomy §Bypass surgery based on pre-operative angiography if available or intra-operative angiography
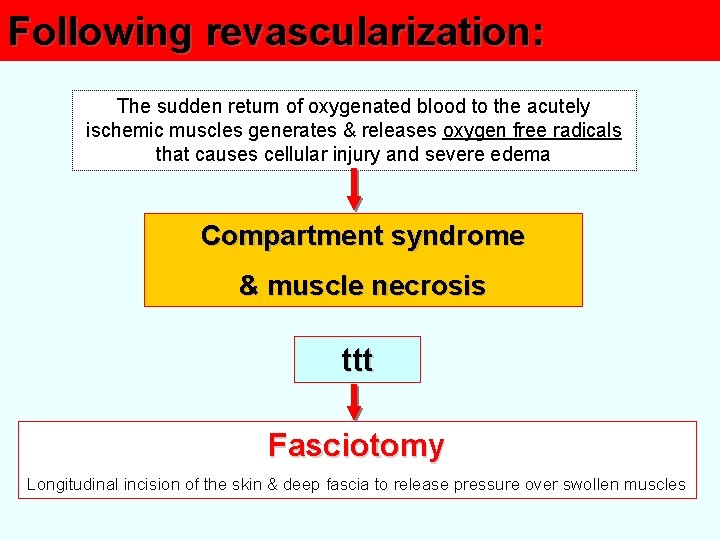
Following revascularization: The sudden return of oxygenated blood to the acutely ischemic muscles generates & releases oxygen free radicals that causes cellular injury and severe edema Compartment syndrome & muscle necrosis ttt Fasciotomy Longitudinal incision of the skin & deep fascia to release pressure over swollen muscles
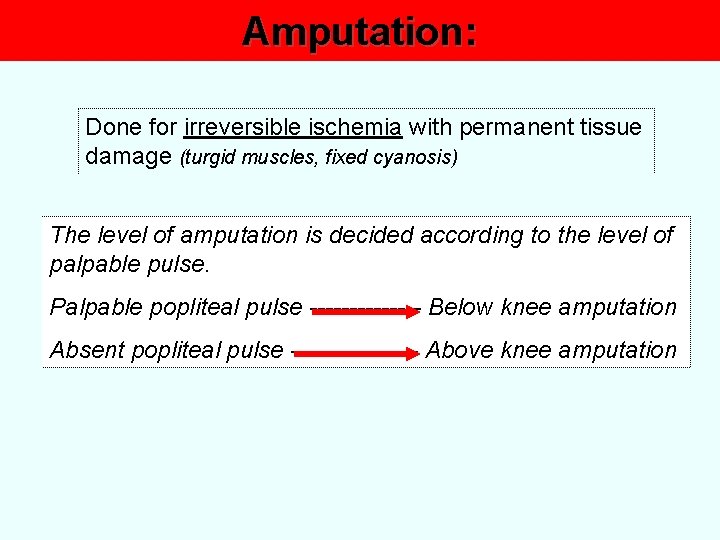
Amputation: Done for irreversible ischemia with permanent tissue damage (turgid muscles, fixed cyanosis) The level of amputation is decided according to the level of palpable pulse. Palpable popliteal pulse ------- Below knee amputation Absent popliteal pulse -------- Above knee amputation
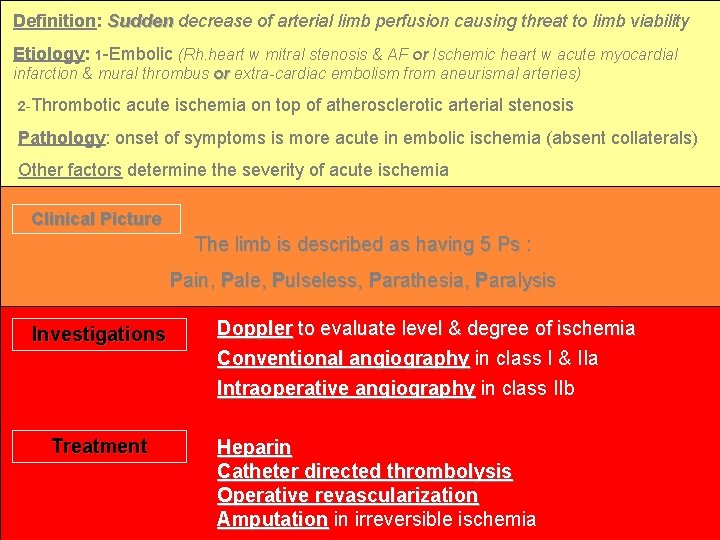
Definition: Sudden decrease of arterial limb perfusion causing threat to limb viability Etiology: 1 -Embolic (Rh. heart w mitral stenosis & AF or Ischemic heart w acute myocardial infarction & mural thrombus or extra-cardiac embolism from aneurismal arteries) 2 -Thrombotic acute ischemia on top of atherosclerotic arterial stenosis Pathology: onset of symptoms is more acute in embolic ischemia (absent collaterals) Other factors determine the severity of acute ischemia Clinical Picture The limb is described as having 5 Ps : Pain, Pale, Pulseless, Parathesia, Paralysis Investigations Treatment Doppler to evaluate level & degree of ischemia Conventional angiography in class I & IIa Intraoperative angiography in class IIb Heparin Catheter directed thrombolysis Operative revascularization Amputation in irreversible ischemia
- Slides: 23