Acute kidney Injury AKILecture8 Hazem AlKhafaji Consultant physician
- Slides: 25
Acute kidney Injury (AKI)-Lecture-8 - Hazem Al-Khafaji Consultant physician Department of medicine Al-Qadissia University
Overview o o o o Introduction Epidemiology Definitions & staging Classification and causes Presentation Approach to diagnosis. Treatment
Introduction Acute renal failure (ARF) is a complex disorder that occurs in a variety of settings with clinical manifestations ranging from minimal elevation in serum creatinine(subclinical) to anuric renal failure. The first description of ARF , then termed ischuria renalis, was by William Heberdenin 1802. A recent survey revealed the use of at least 35 definitions for ARF in the literatures, this state of confusion has given rise to wide variation in reported incidence and clinical significance of ARF. Acute kidney injury (AKI) has now replaced the term acute renal failure and an universal definition and staging system has been proposed to allow earlier detection and management of AKI and the term ARF preferably should be restricted to patients who have AKI and need renal replacement therapy (RRT).
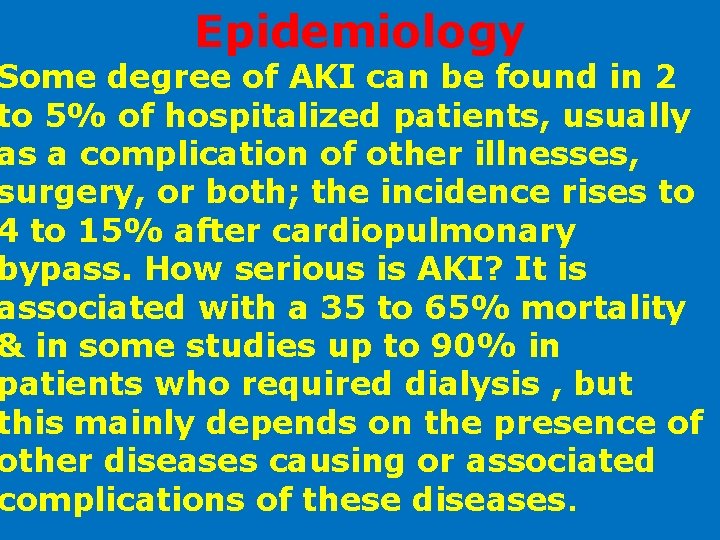
Epidemiology Some degree of AKI can be found in 2 to 5% of hospitalized patients, usually as a complication of other illnesses, surgery, or both; the incidence rises to 4 to 15% after cardiopulmonary bypass. How serious is AKI? It is associated with a 35 to 65% mortality & in some studies up to 90% in patients who required dialysis , but this mainly depends on the presence of other diseases causing or associated complications of these diseases.
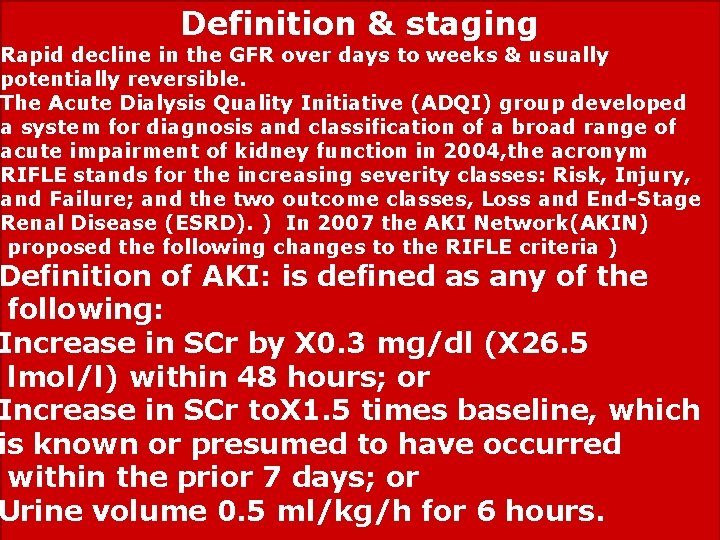
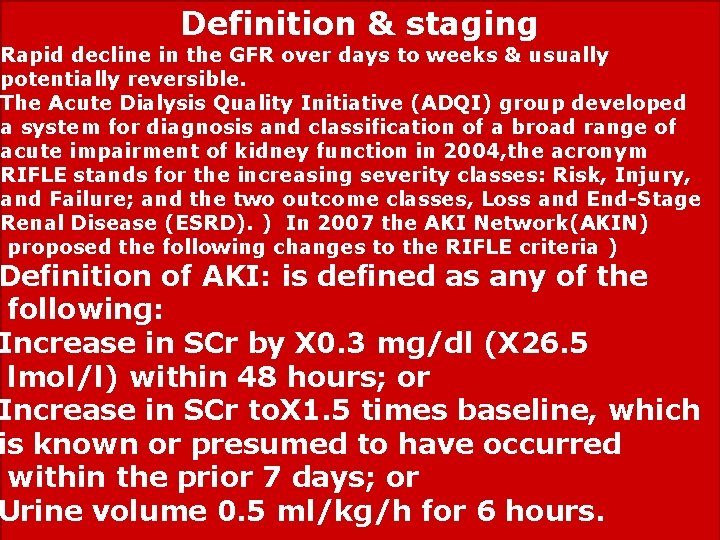
Definition & staging Rapid decline in the GFR over days to weeks & usually potentially reversible. The Acute Dialysis Quality Initiative (ADQI) group developed a system for diagnosis and classification of a broad range of acute impairment of kidney function in 2004, the acronym RIFLE stands for the increasing severity classes: Risk, Injury, and Failure; and the two outcome classes, Loss and End-Stage Renal Disease (ESRD). ) In 2007 the AKI Network(AKIN) proposed the following changes to the RIFLE criteria ) Definition of AKI: is defined as any of the following: Increase in SCr by X 0. 3 mg/dl (X 26. 5 lmol/l) within 48 hours; or Increase in SCr to. X 1. 5 times baseline, which is known or presumed to have occurred within the prior 7 days; or Urine volume 0. 5 ml/kg/h for 6 hours.
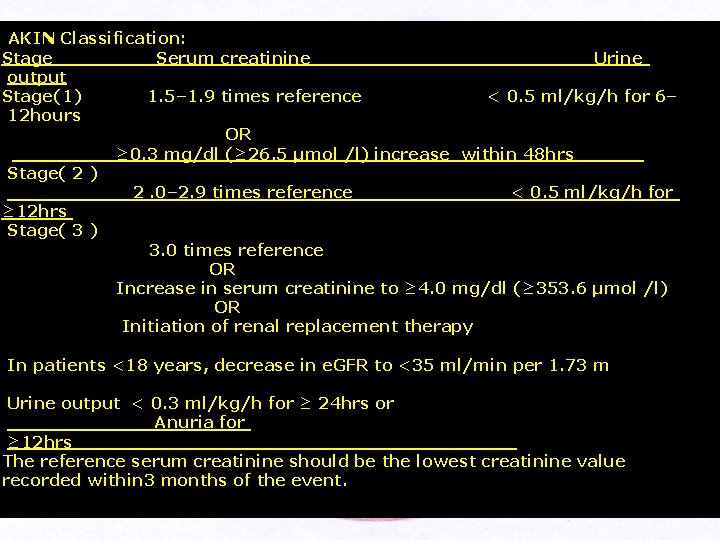
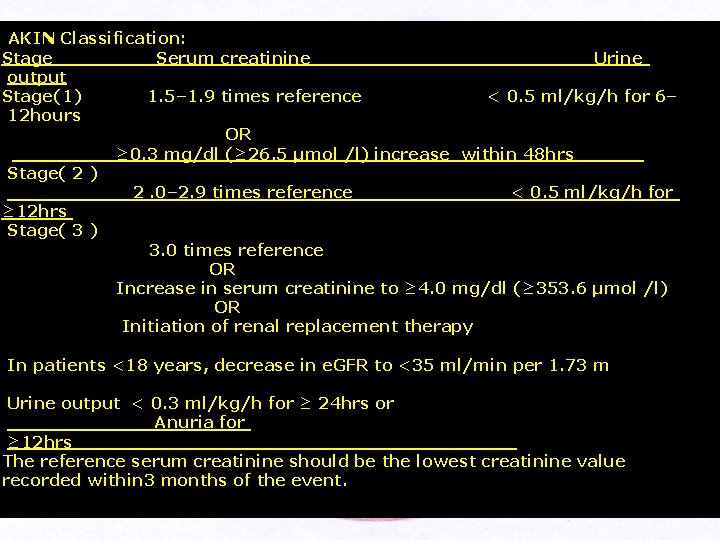
AKIN Classification: Stage Serum creatinine Urine output Stage(1) 1. 5– 1. 9 times reference < 0. 5 ml/kg/h for 6– 12 hours OR ≥ 0. 3 mg/dl (≥ 26. 5 µmol /l) increase within 48 hrs______. Stage( 2 ) 2. 0– 2. 9 times reference < 0. 5 ml/kg/h for ≥ 12 hrs Stage( 3 ) 3. 0 times reference OR Increase in serum creatinine to ≥ 4. 0 mg/dl (≥ 353. 6 µmol /l) OR Initiation of renal replacement therapy In patients <18 years, decrease in e. GFR to <35 ml/min per 1. 73 m Urine output < 0. 3 ml/kg/h for ≥ 24 hrs or Anuria for ≥ 12 hrs____________________ The reference serum creatinine should be the lowest creatinine value recorded within 3 months of the event.
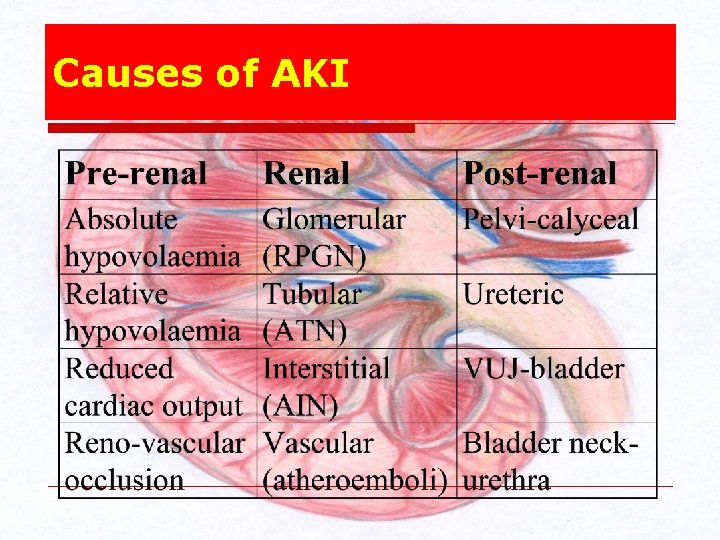
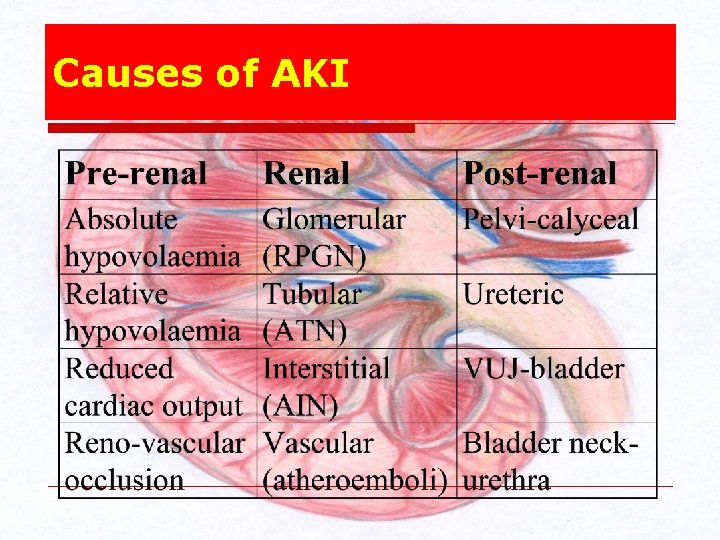
Causes of AKI
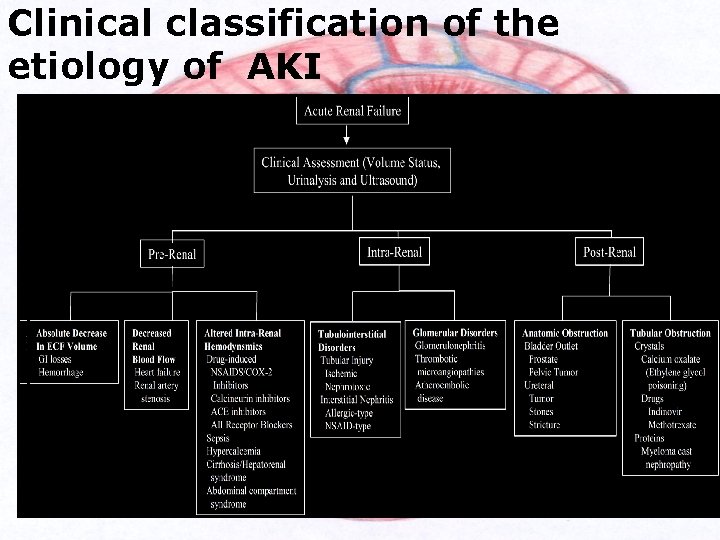
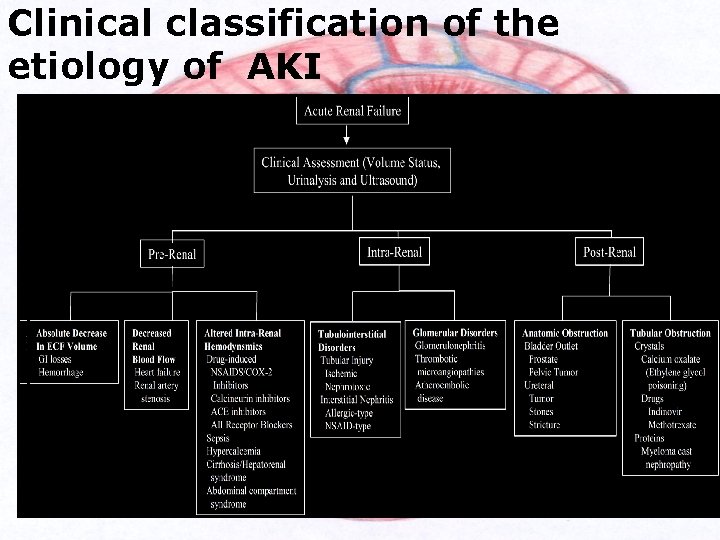
Clinical classification of the etiology of AKI
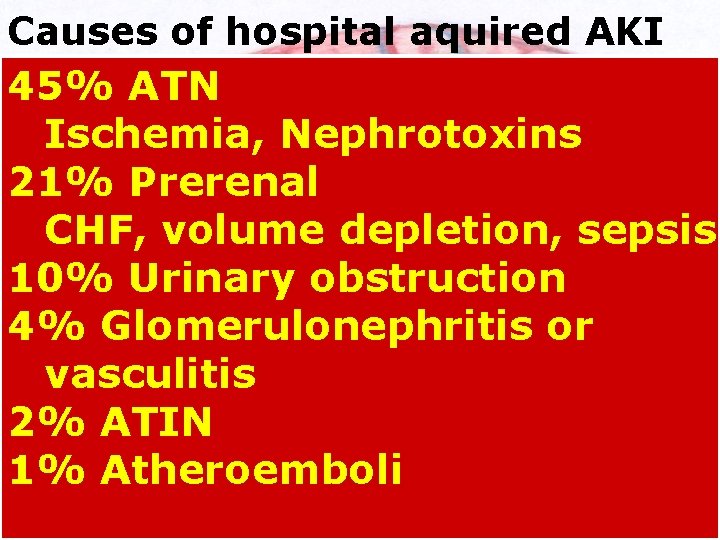
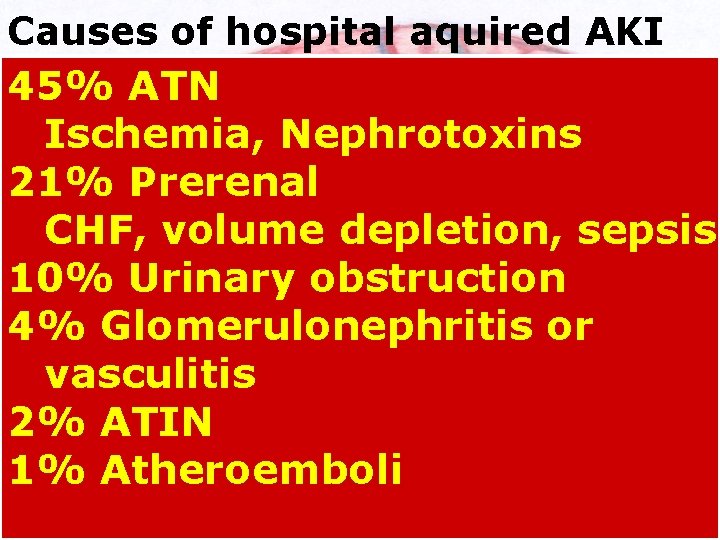
Causes of hospital aquired AKI 45% ATN o. Ischemia, Nephrotoxins 21% Prerenal o. CHF, volume depletion, sepsis 10% Urinary obstruction 4% Glomerulonephritis or vasculitis 2% ATIN 1% Atheroemboli
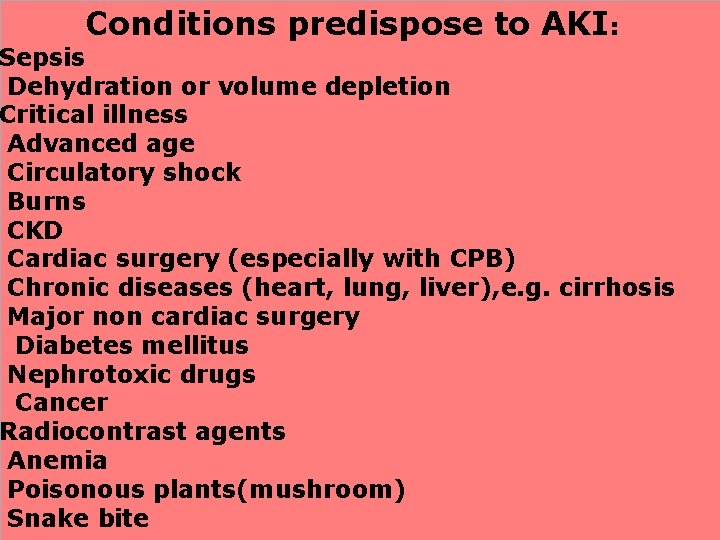
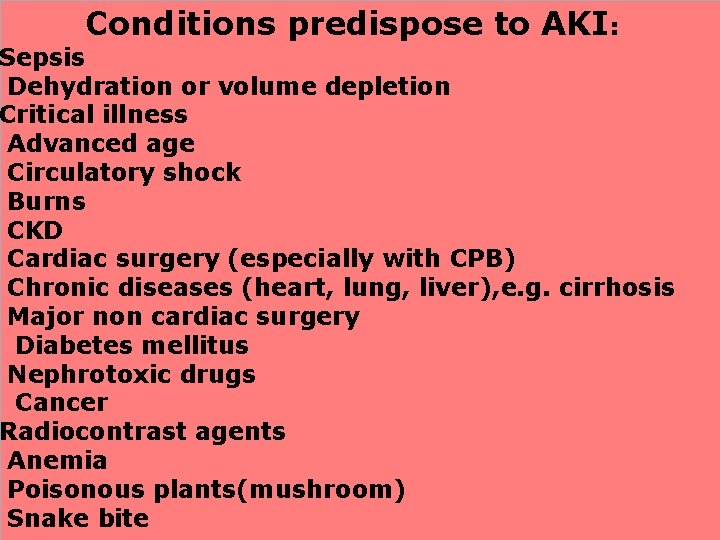
Conditions predispose to AKI: Sepsis Dehydration or volume depletion Critical illness Advanced age Circulatory shock Burns CKD Cardiac surgery (especially with CPB) Chronic diseases (heart, lung, liver), e. g. cirrhosis Major non cardiac surgery Diabetes mellitus Nephrotoxic drugs Cancer Radiocontrast agents Anemia Poisonous plants(mushroom) Snake bite
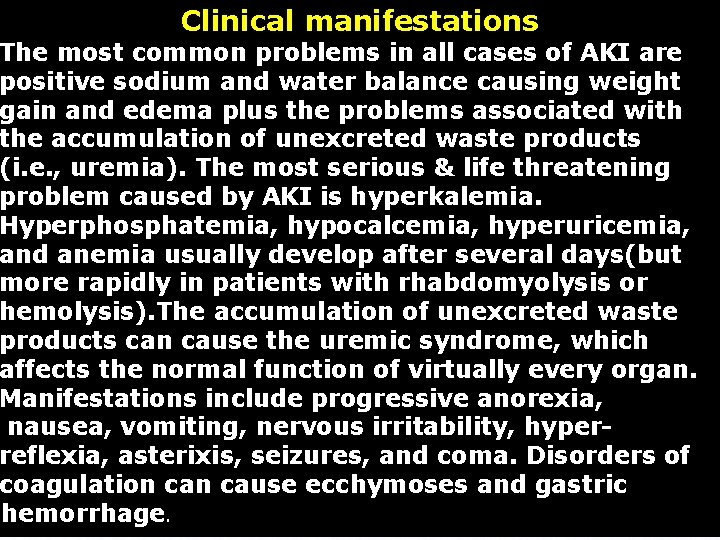
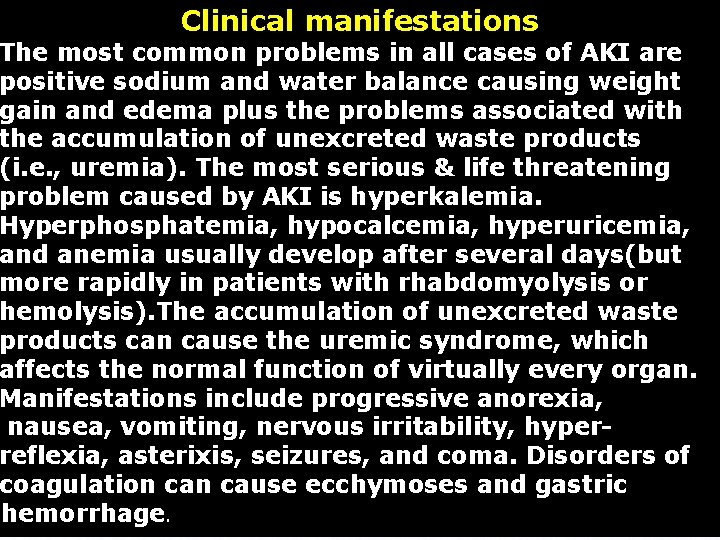
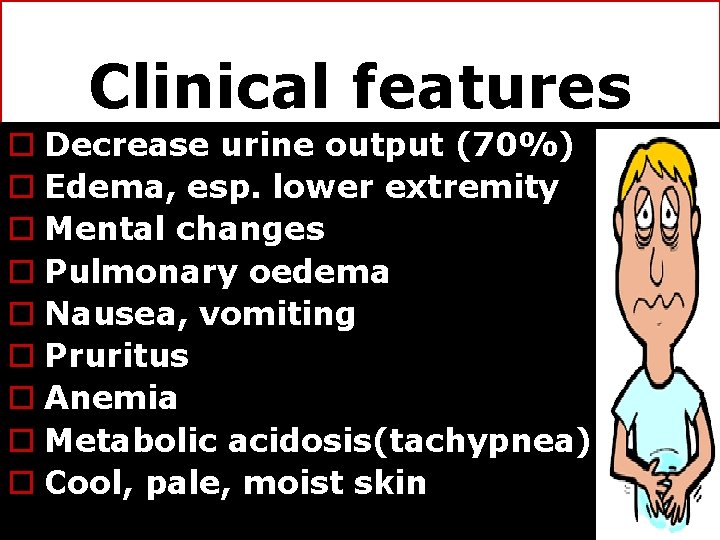
Clinical manifestations The most common problems in all cases of AKI are positive sodium and water balance causing weight gain and edema plus the problems associated with the accumulation of unexcreted waste products (i. e. , uremia). The most serious & life threatening problem caused by AKI is hyperkalemia. Hyperphosphatemia, hypocalcemia, hyperuricemia, and anemia usually develop after several days(but more rapidly in patients with rhabdomyolysis or hemolysis). The accumulation of unexcreted waste products can cause the uremic syndrome, which affects the normal function of virtually every organ. Manifestations include progressive anorexia, nausea, vomiting, nervous irritability, hyperreflexia, asterixis, seizures, and coma. Disorders of coagulation cause ecchymoses and gastric hemorrhage.
Clinical features o Decrease urine output (70%) o Edema, esp. lower extremity o Mental changes o Pulmonary oedema o Nausea, vomiting o Pruritus o Anemia o Metabolic acidosis(tachypnea). o Cool, pale, moist skin
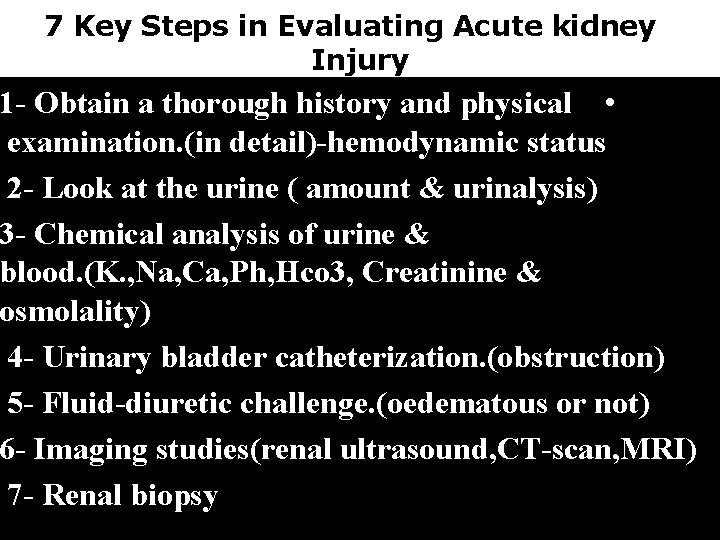
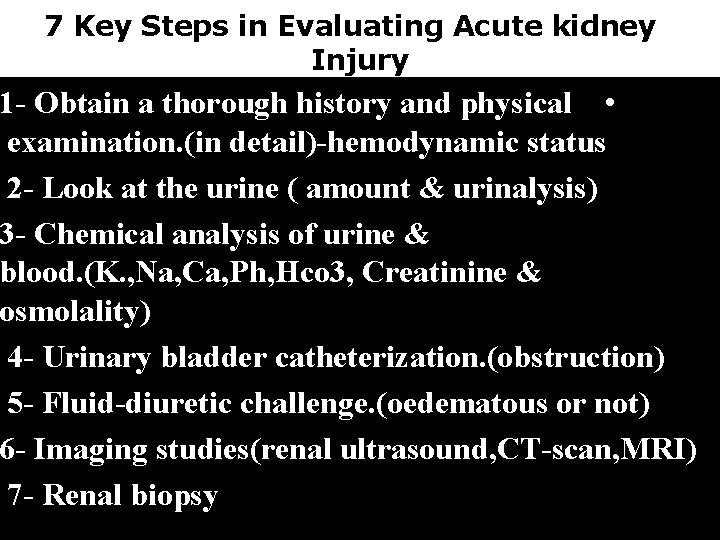
7 Key Steps in Evaluating Acute kidney Injury 1 - Obtain a thorough history and physical • examination. (in detail)-hemodynamic status 2 - Look at the urine ( amount & urinalysis) 3 - Chemical analysis of urine & blood. (K. , Na, Ca, Ph, Hco 3, Creatinine & osmolality) 4 - Urinary bladder catheterization. (obstruction) 5 - Fluid-diuretic challenge. (oedematous or not) 6 - Imaging studies(renal ultrasound, CT-scan, MRI) 7 - Renal biopsy
Management
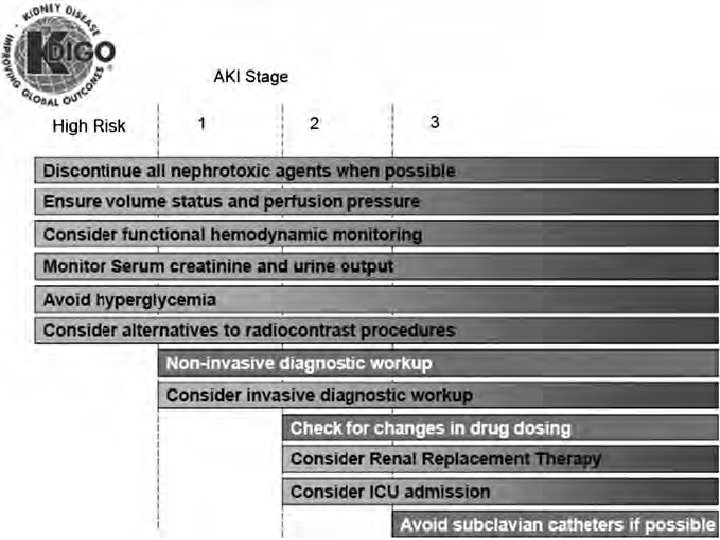
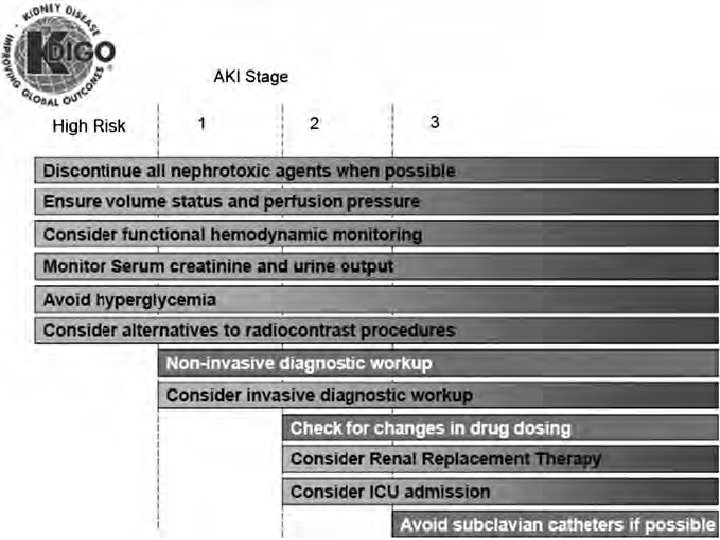
TREATMENT Treatment of AKI includes: 1 -Emergent intervention: treatment of hyperkalaemia. 2 -Correction of reversible causes. 3 -Prevention of additional injury. 4 - Supportive therapy( use of metabolic support during the maintenance and recovery phases of the syndrome) 5 -Attempts to convert oliguric to nonoliguric renal failure. 6 - Dialysis
Hyperkalaemia o The most common biochemical cause of death in patient with acute tubular necrosis. o Clinical features: o Paresthesia, muscular weakness, depressed deep tendon reflexes, flaccid paralysis´ respiratory failure. o The sequential ECG changes: o Peaked T wave. o Prolongation of PR interval. o Widening of QRS complex. o Sine wave pattern.
Treatment of hyperkalaemia 1 -Intravenous calcium gluconate or calcium chloride; this type of therapy is the most rapidly acting method of correcting the cardiac conduction abnormality. 2 -Glucose and insulin (0. 5 U/kg/hour of regular insulin with 3 m. L/kg/hour of 20% glucose) 3 - hypertonic sodium bicarbonate (for acidotic patients) can reduce the serum potassium concentration within 30 to 60 minutes. 4 -Ingesting sodium polystyrene sulfonate exchange resin (20 to 30 g) in a solution containing sorbitol to ensurerequired excretion of potassium polystyrene resin 6 -Dialysis is generally 44 . 5 -ß 2 agonist as inhaled albuterol.
Supportive therapy Indwelling urinary catheters should be avoided in uncomplicated cases; intermittent catheterization using sterile technique usually suffices even in oliguric to reduces the risk of infection. In all patients, maintaining fluid balance is crucial. The simplest and most accurate estimate of fluid balance is by daily measurement of body weight. Fluid intake and output records daily. Initially, the required fluid intake can be approximated by giving the patient fluids (e. g. , water, tea) equal to 500 m. L plus the amount of urine excreted in the preceding 24 hours. The outcome should be no gain of extracellular volume, measured as an increase in weight. In febrile patients this limit can be increased as long as there is no increase in weight. Dietary protein should be limited to 0. 8 -1 g/kg of body weight per day unless the patient is hypercatabolic.
CORRECTION OF REVERSIBLE CAUSES. 1 -In all AKI patients, administration of drugs that interfere with renal perfusion or function or potential nephrotoxins should be stopped. 2 -Radiocontrast agents should be avoided. 3 -For hypovolemic, hypotensive patients in the prerenal classification, blood pressure should be restored by discontinuing the use of antihypertensive drugs and administering blood (if bleeding or anemia is present) or isotonic saline to expand the extracellular volume (unless the patient has edema or ascites). 4 -In oedematous patients, blood
Attempts to convert oliguric to nonoliguric renal failure : Not all patients with intrinsic kidney damage and AKI are oliguric. It may represent a milder form of tubular damage. These patients do not necessarily regain renal function more rapidly, but it is worthwhile to attempt to convert oliguric patients to the nonoliguric state of AKI because fluid balance in nonoliguric patients is more easily managed. In conditions associated with low S. Na and no edema. (dehydrated or blood loss), a challenge with 500 m. L of saline combined with 40 to 80 mg of intravenous furosemide may reverse an oliguric to a nonoliguric state and, in some cases, even prevent progressive tubular damage. Alternatively, a trial of 80 to 100 mg of furosemide can be used in edematous patients to attempt conversion of oliguric to nonoliguric renal failure.
Dialysis Hemodialysis is critical for treating some of the complications of ARF. It should be considered for hyperkalemia that is unresponsive to polystyrene exchange resins or if electrocardiographic abnormalities are present. (Note that hemodialysis invariably requires several hours to reduce serum potassium effectively and should never be considered adequate treatment for acute effects of hyperkalemia. ) Hemodialysis is also required for severe metabolic acidosis that cannot be managed by sodium bicarbonate; it also is used to treat pulmonary edema, progressive azotemia (SUN values >100 mg/d. L), encephalopathy, seizures, bleeding, pericarditis.
Acute kidney injury Prevention, detection and management of acute kidney injury up to the point of renal replacement therapy Issued: August 2013 NICE clinical guideline 169 guidance. nice. org. uk/cg 169 NICE
Thank you o. Next lecture Chronic kidney disease