ACUTE HEART FAILURE Yu Jin Kim Department of
![(2017) [R-type] ① apical 4 chamber view ② apical 2 chamber view ③ apical (2017) [R-type] ① apical 4 chamber view ② apical 2 chamber view ③ apical](https://slidetodoc.com/presentation_image/3ac2305f5a8a4d91b82204fe2196360e/image-2.jpg)


- Slides: 65
ACUTE HEART FAILURE Yu Jin Kim Department of Emergency Medicine, Seoul National University Bundang Hospital
![2017 Rtype ① apical 4 chamber view ② apical 2 chamber view ③ apical (2017) [R-type] ① apical 4 chamber view ② apical 2 chamber view ③ apical](https://slidetodoc.com/presentation_image/3ac2305f5a8a4d91b82204fe2196360e/image-2.jpg)
(2017) [R-type] ① apical 4 chamber view ② apical 2 chamber view ③ apical 5 chamber view ④ apical 3 chamber view ⑤ parasternal long view ⑥ parasternal short view ⑦ subcostal view ⑧ suprasternal view 문제 1. 심초음파에서 IVC phlethora를 확인할 수 있는 view는? (한가지) 답 : 7 문제 2. 심초음파에서 M-mode로 EF를 측정할 수 있는 view는? (두가지) 답 : 5, 6
• (2013) 60세 남자 BP 180/100, HR 100회, Sa. O 2 90% 촉진상 심장박동이 가장 잘 느껴지는 부위가 왼쪽으로 전위, 청진 상 양측폐야의 쌕쌕거림, EKG상 LVH, X-ray상 양측폐 간질 음영이 보인다. 치료제는? ① Dobu+Furosemide ② NTG+Furosemide ③ NTG+Digoxin ④ Salbutamol+Dobutamine ⑤ Salbutamol+Methylprednisolone
INTRODUCTION
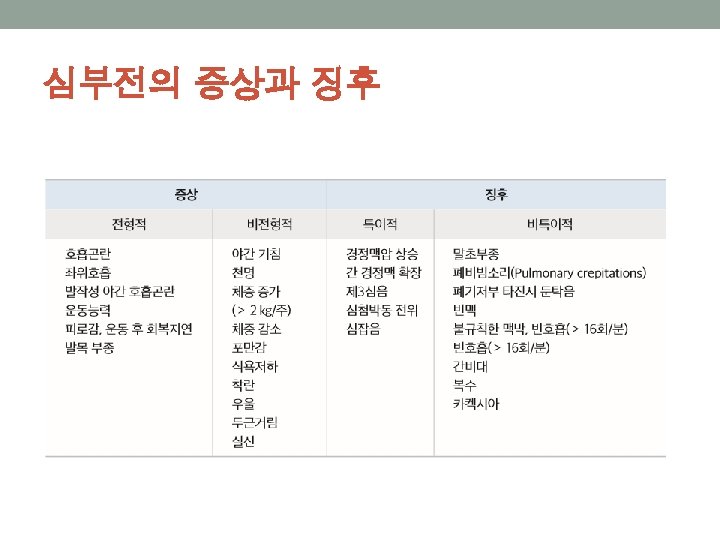
Introduction • Cardinal symptoms of HF • Leg swelling, • Shortness of breath, • Fatigue, General weakness • Acute therapies include nitrates, diuretics, and positive pressure ventilation, the same as in 1974. • Mortality • 50% within 5 years • Hospitalization – poor prognosis
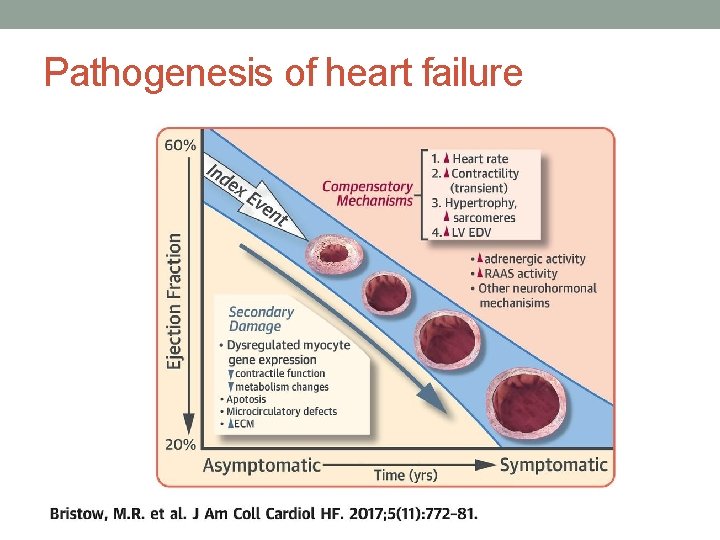
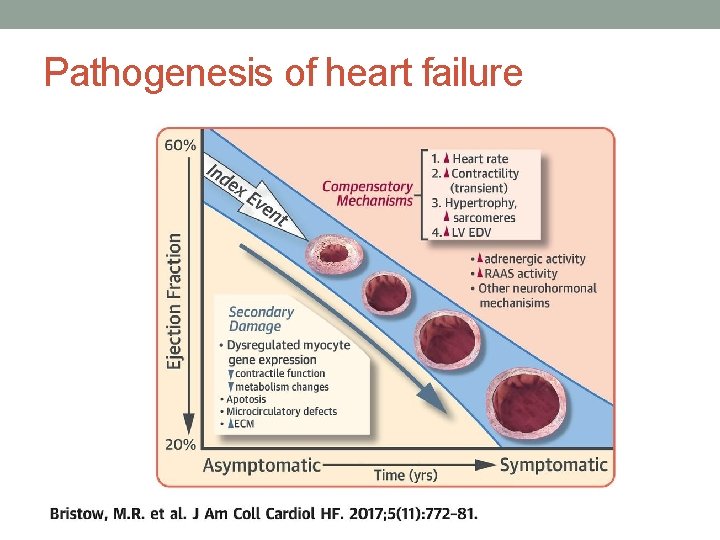
Pathogenesis of heart failure
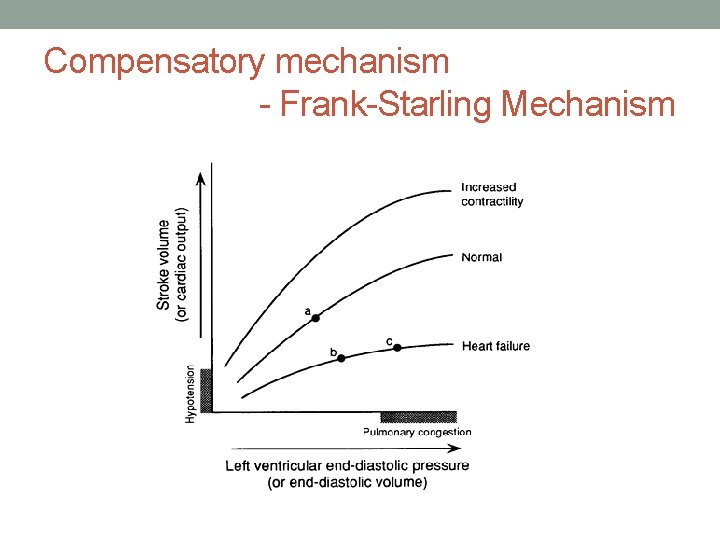
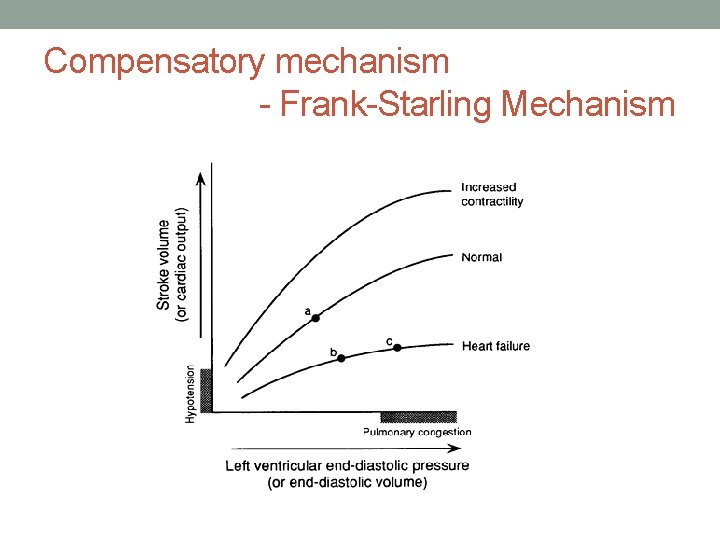
Compensatory mechanism - Frank-Starling Mechanism
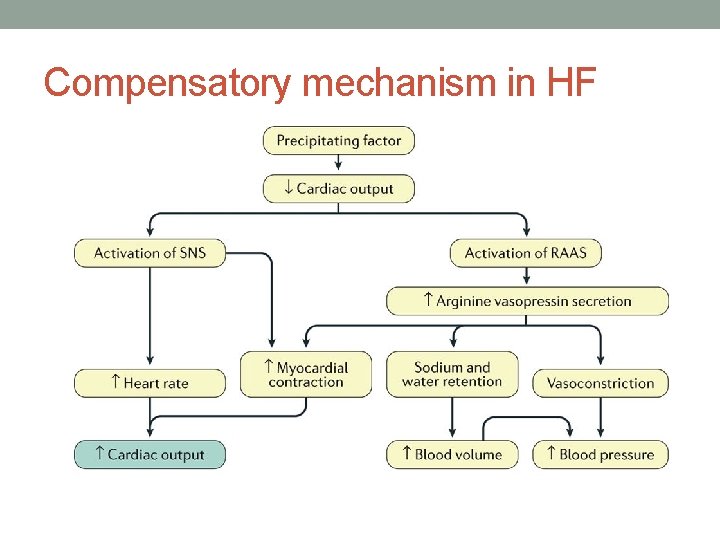
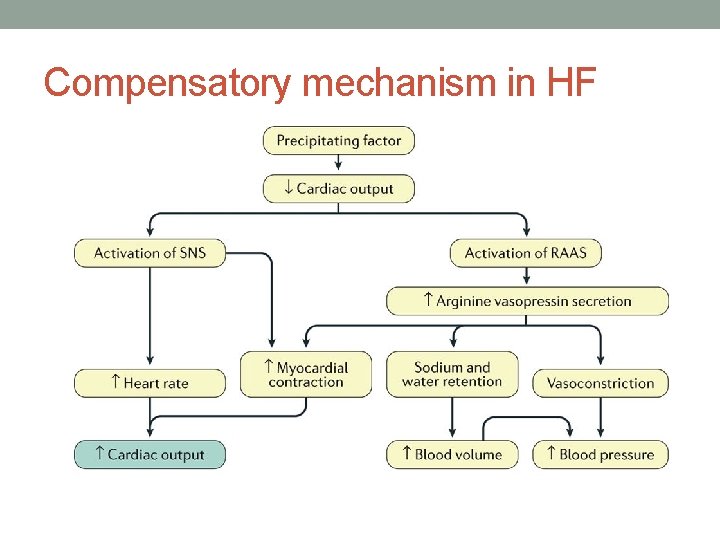
Compensatory mechanism in HF
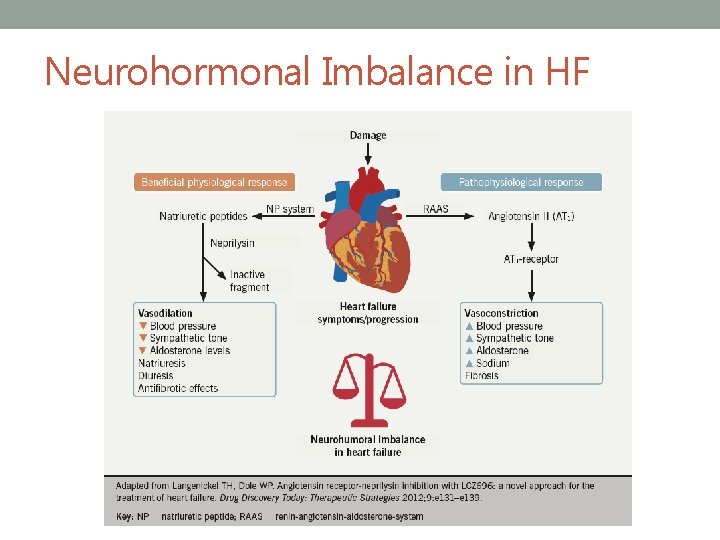
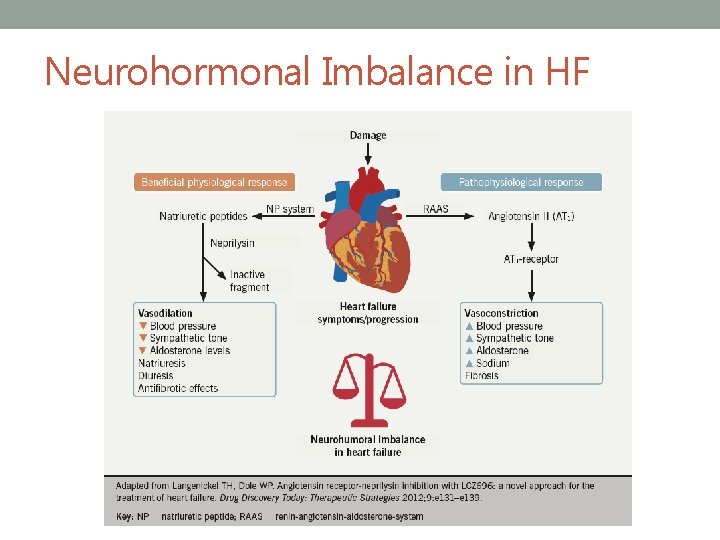
Neurohormonal Imbalance in HF
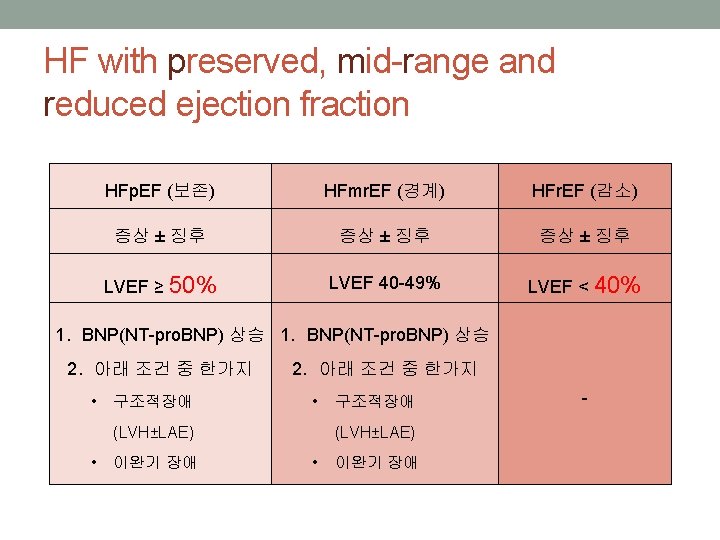
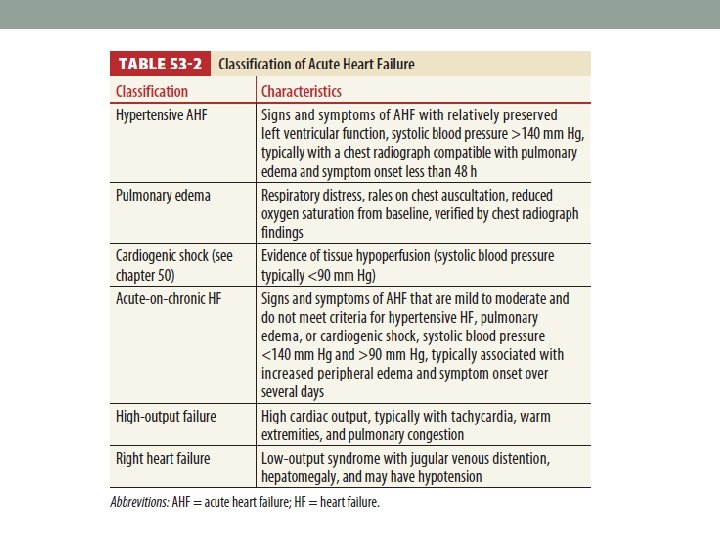
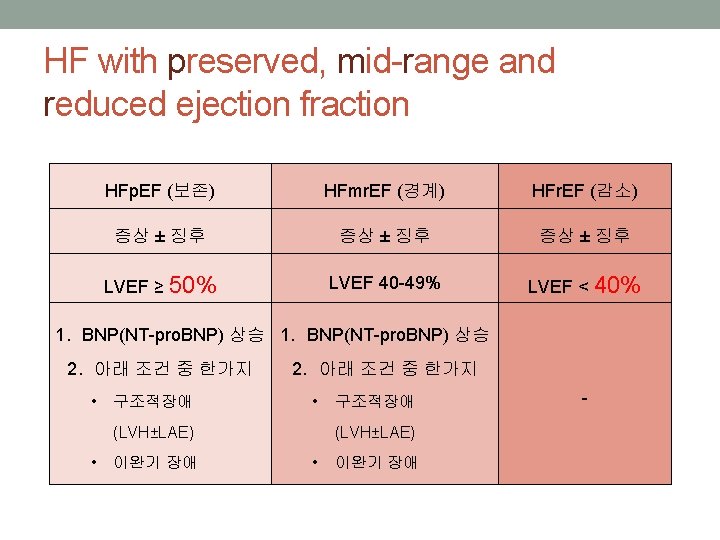
Classification of Heart Failure • Acute vs Chronic • Rt sided vs Lt sided • High output vs Low output • Systolic vs Diastolic • -> Useful in Early stage • -> These distinctions blur in Late stage • Classification by EF preservation
SYSTOLIC AND DIASTOLIC HEART FAILURE
Common Causes in ED • Acute coronary syndrome* • Hypertensive emergency • Arrhythmia (esp. Af with RVR)* • Cardiomyopathy (esp. dilated) • Valvular dysfunction (Myocardial infarction 관련 *) • Myocarditis* • Pericarditis • Anemia* • (*) 기저병력없이 새로 진단되는 급성 심부전증 • 응급실에 오는 급성 심부전증 환자의 80%는 만성 심질환의 급성 대상부전(acute decompensation)에 의해서 발생한다.
Trigerring factor • Excess salt or Excess fluid intake* • Medication nonadherence* • Renal failure (especially missed dialysis)* • Poorly controlled hypertension • Iatrogenic (medication change) • (* common in ED)
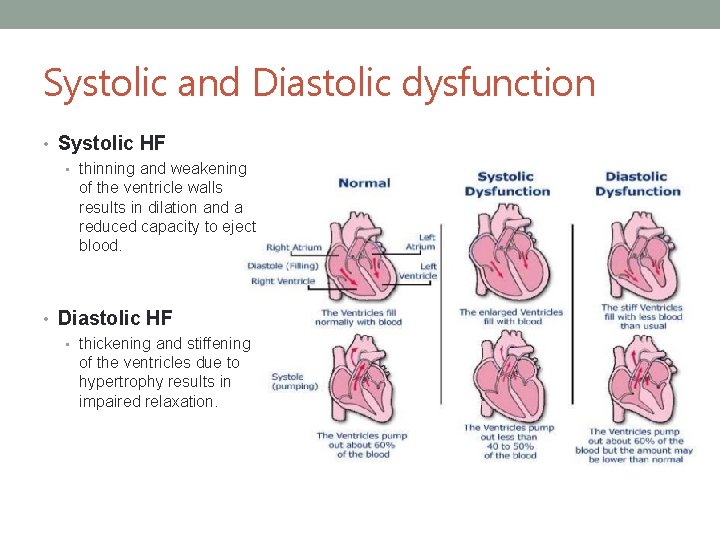
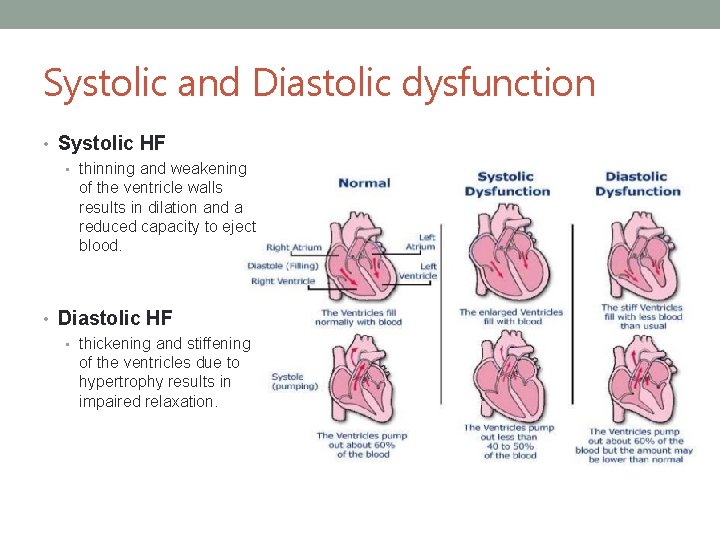
Systolic and Diastolic dysfunction • Systolic HF • thinning and weakening of the ventricle walls results in dilation and a reduced capacity to eject blood. • Diastolic HF • thickening and stiffening of the ventricles due to hypertrophy results in impaired relaxation.
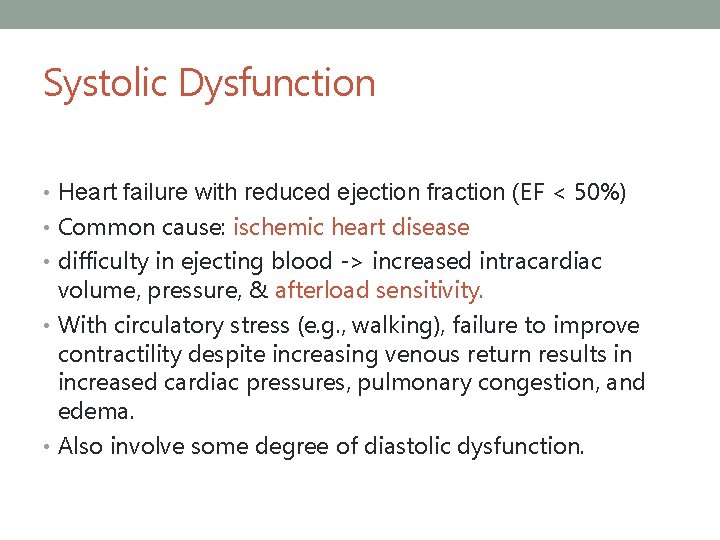
Systolic Dysfunction • Heart failure with reduced ejection fraction (EF < 50%) • Common cause: ischemic heart disease • difficulty in ejecting blood -> increased intracardiac volume, pressure, & afterload sensitivity. • With circulatory stress (e. g. , walking), failure to improve contractility despite increasing venous return results in increased cardiac pressures, pulmonary congestion, and edema. • Also involve some degree of diastolic dysfunction.
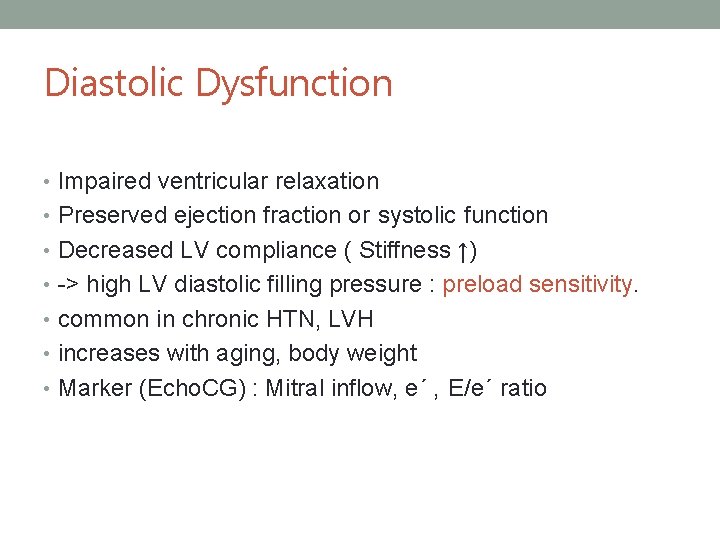
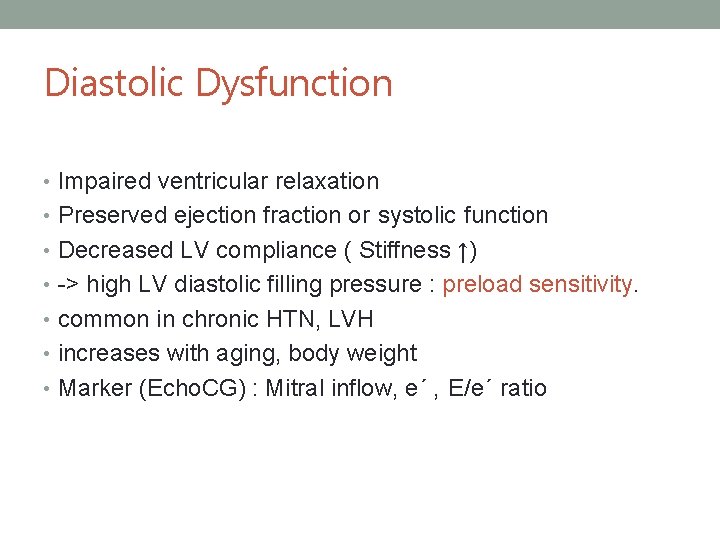
Diastolic Dysfunction • Impaired ventricular relaxation • Preserved ejection fraction or systolic function • Decreased LV compliance ( Stiffness ↑) • -> high LV diastolic filling pressure : preload sensitivity. • common in chronic HTN, LVH • increases with aging, body weight • Marker (Echo. CG) : Mitral inflow, e´ , E/e´ ratio
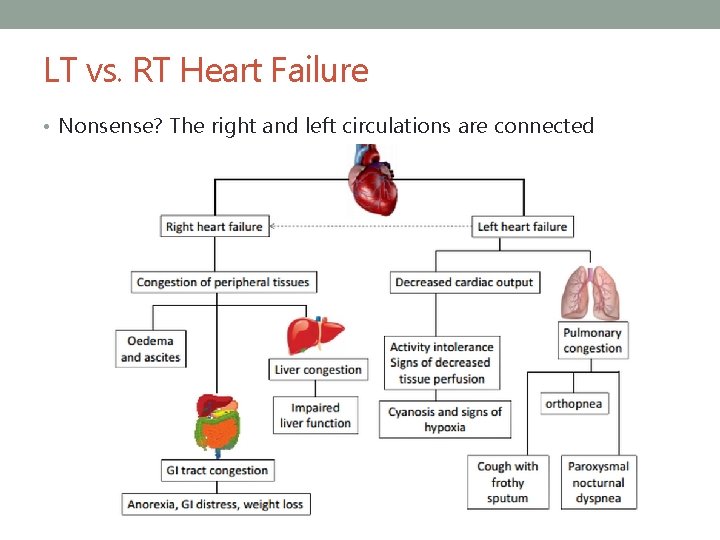
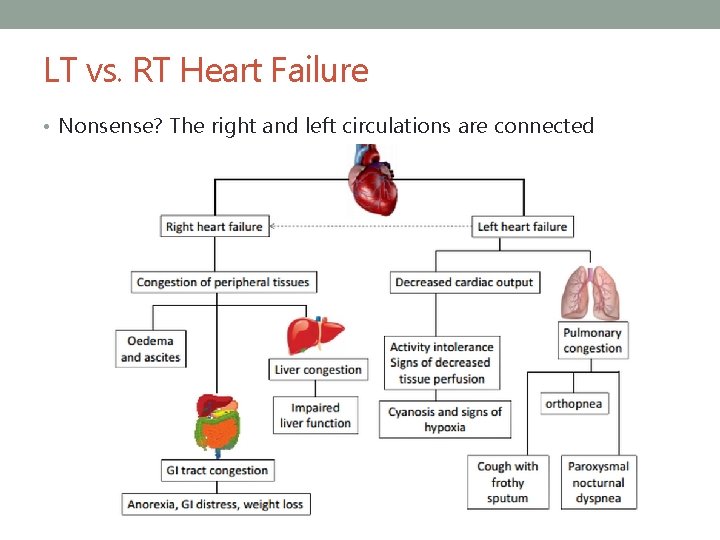
LT vs. RT Heart Failure • Nonsense? The right and left circulations are connected

CLINICAL FEATURES
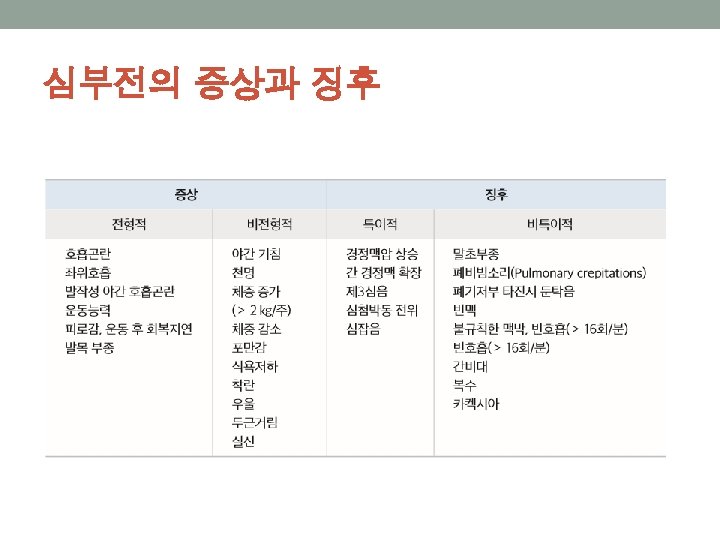
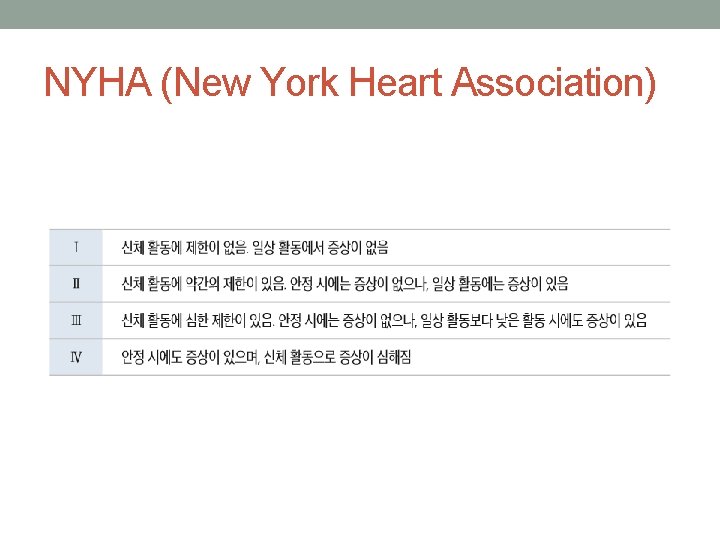
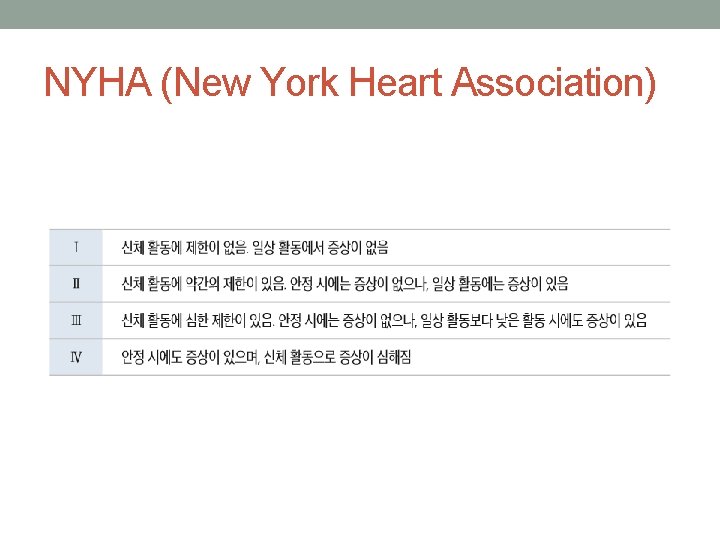
NYHA (New York Heart Association)
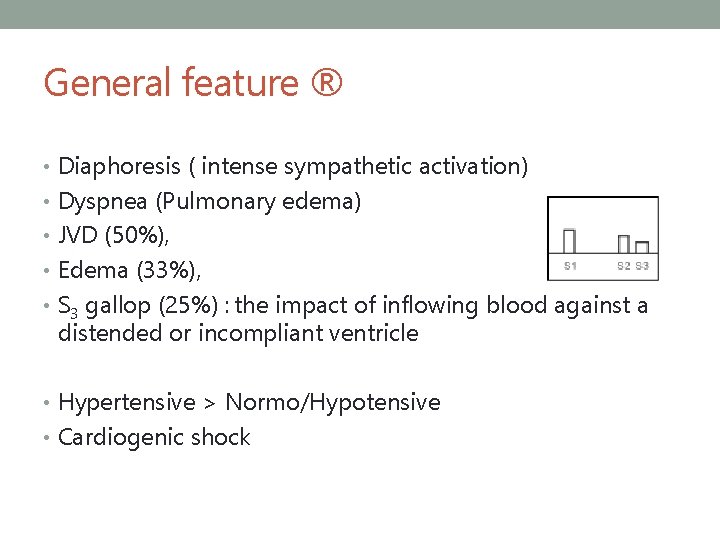
General feature ® • Diaphoresis ( intense sympathetic activation) • Dyspnea (Pulmonary edema) • JVD (50%), • Edema (33%), • S 3 gallop (25%) : the impact of inflowing blood against a distended or incompliant ventricle • Hypertensive > Normo/Hypotensive • Cardiogenic shock
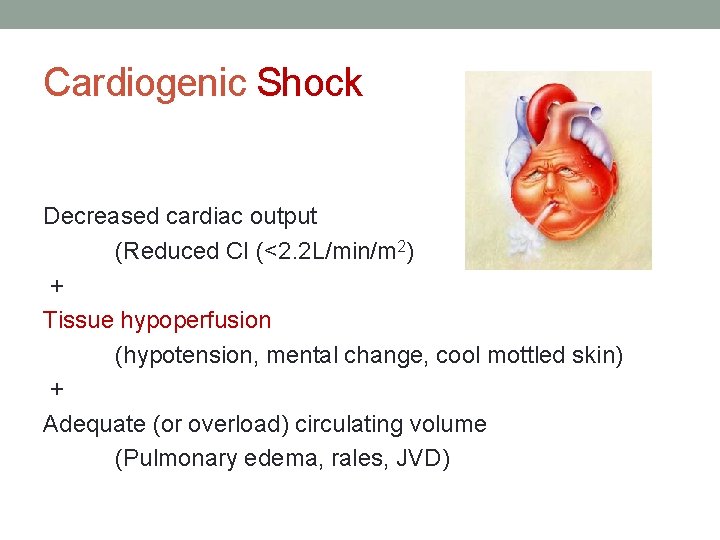
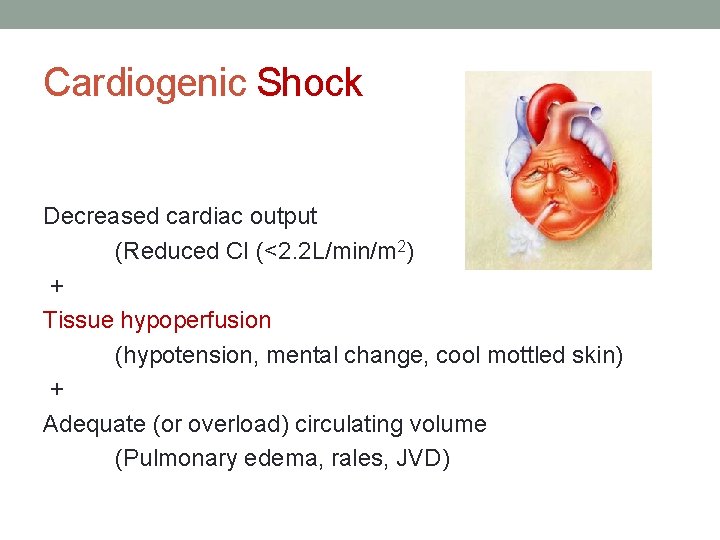
Cardiogenic Shock Decreased cardiac output (Reduced CI (<2. 2 L/min/m 2) + Tissue hypoperfusion (hypotension, mental change, cool mottled skin) + Adequate (or overload) circulating volume (Pulmonary edema, rales, JVD)
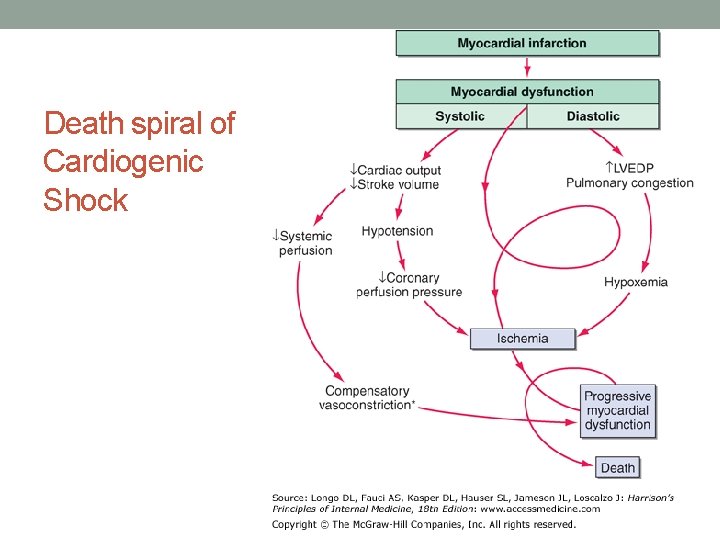
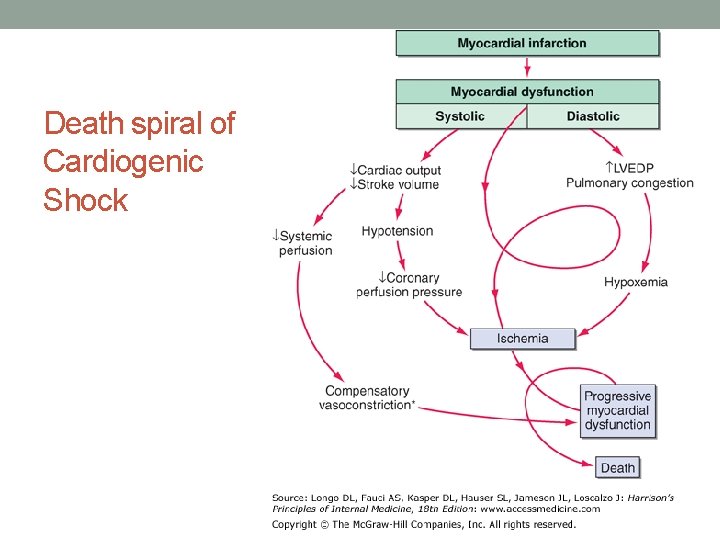
Death spiral of Cardiogenic Shock
DIAGNOSIS There is no single diagnostic test for heart failure
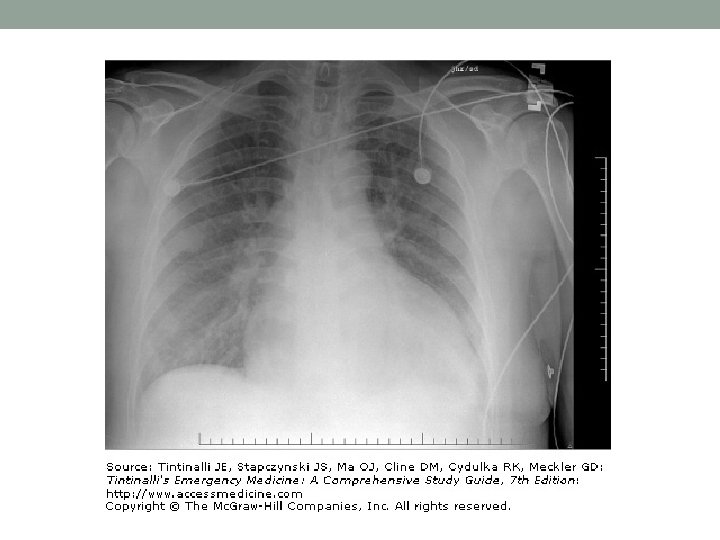
Diagnosis • ‘Clinical gestalt’ • Chest radiography • Lab including natriuretic peptide concentration, and cardiac markers • ECG, Bedside Echocardiography
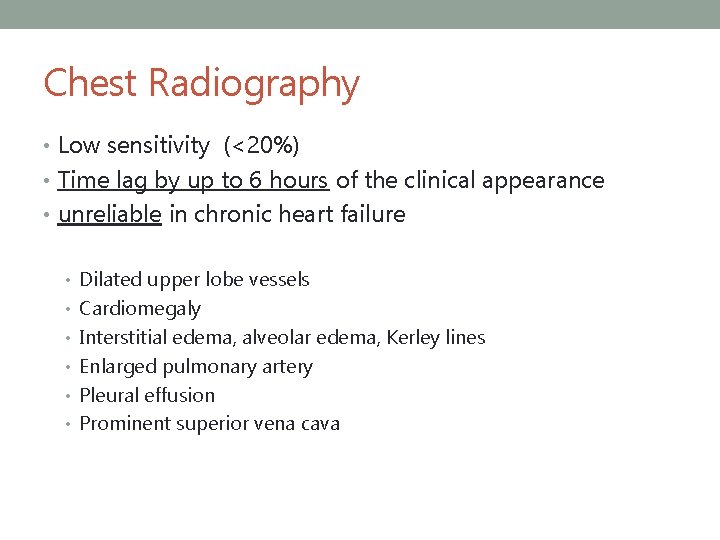
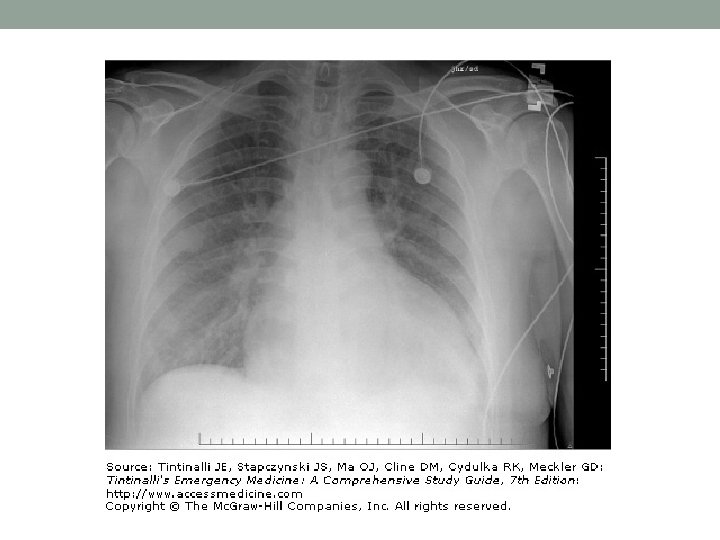
Chest Radiography • Low sensitivity (<20%) • Time lag by up to 6 hours of the clinical appearance • unreliable in chronic heart failure • Dilated upper lobe vessels • Cardiomegaly • Interstitial edema, alveolar edema, Kerley lines • Enlarged pulmonary artery • Pleural effusion • Prominent superior vena cava
ECG • Not useful for diagnosis • reveal an underlying cause or precipitant. • Ischemia • AMI • Dysrhythmias • Af • New T wave change
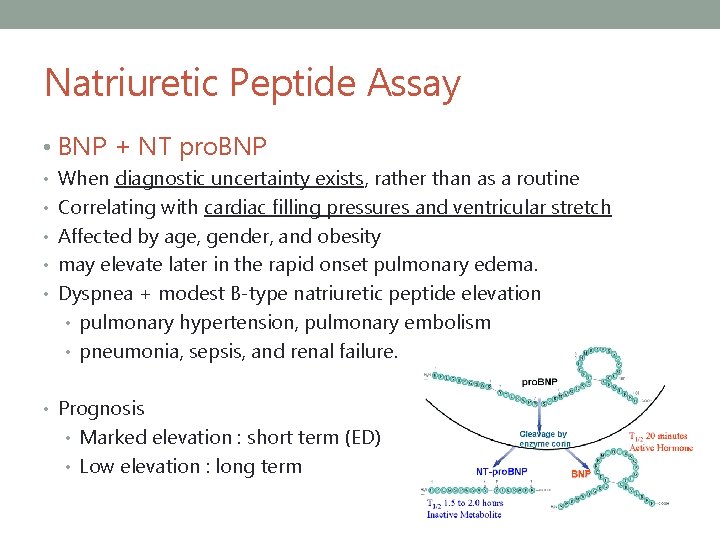
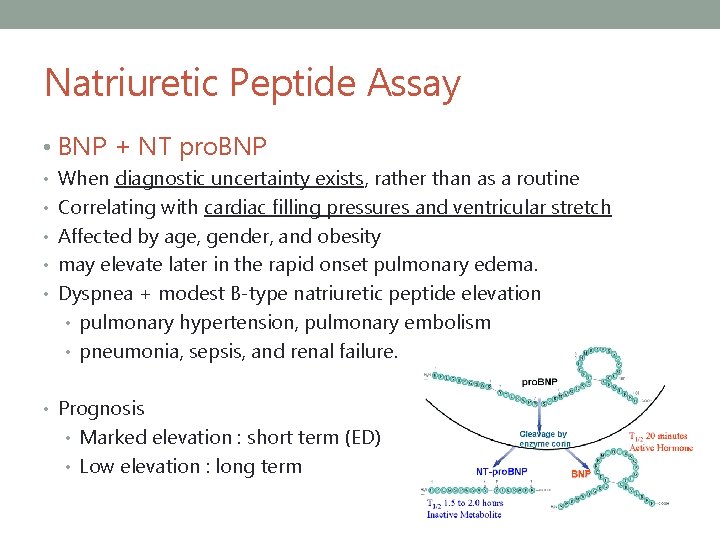
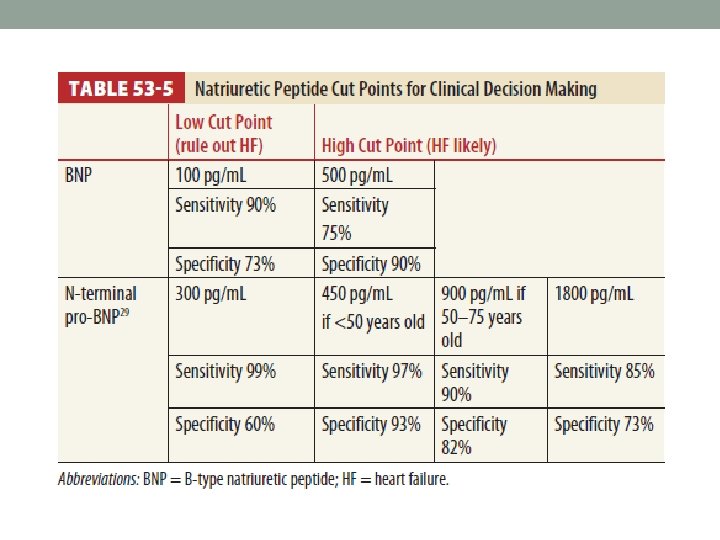
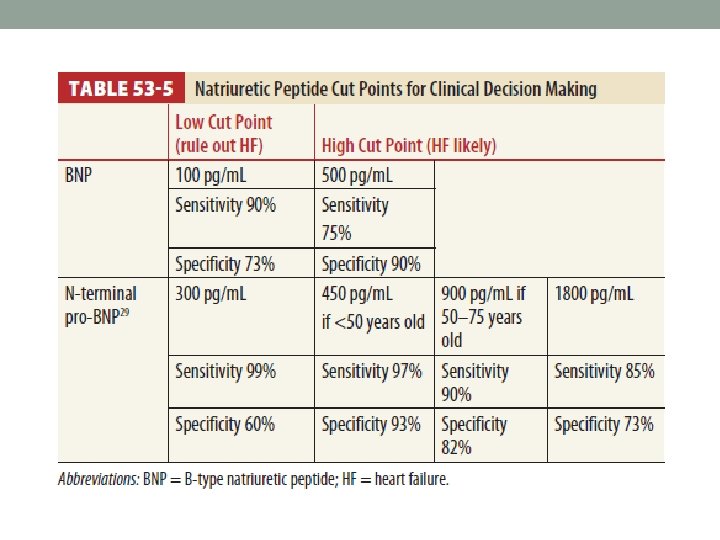
Natriuretic Peptide Assay • BNP + NT pro. BNP • When diagnostic uncertainty exists, rather than as a routine • Correlating with cardiac filling pressures and ventricular stretch • Affected by age, gender, and obesity • may elevate later in the rapid onset pulmonary edema. • Dyspnea + modest B-type natriuretic peptide elevation • pulmonary hypertension, pulmonary embolism • pneumonia, sepsis, and renal failure. • Prognosis • Marked elevation : short term (ED) • Low elevation : long term
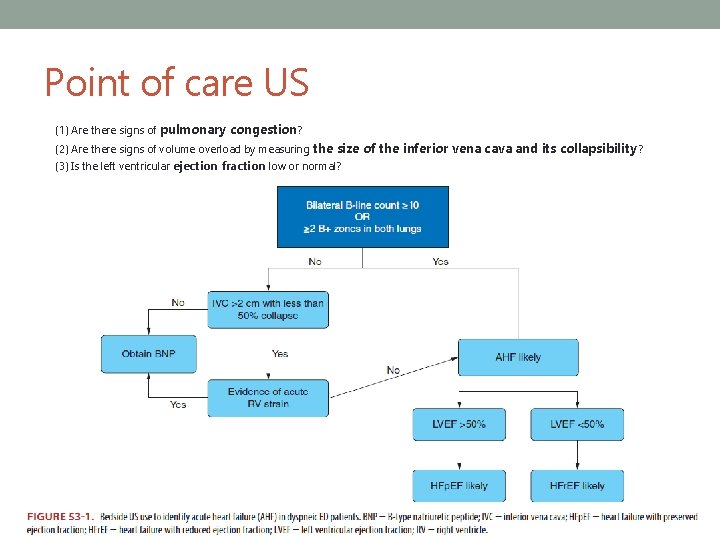
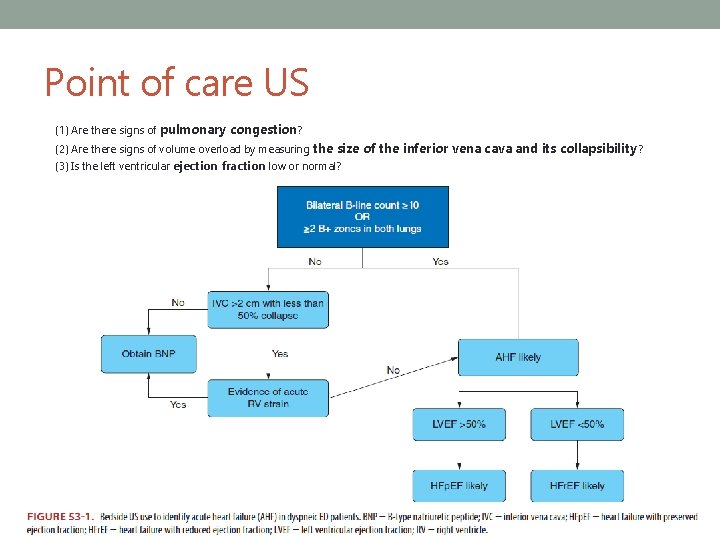
Point of care US (1) Are there signs of pulmonary congestion? (2) Are there signs of volume overload by measuring the size of the inferior vena cava and its collapsibility ? (3) Is the left ventricular ejection fraction low or normal?
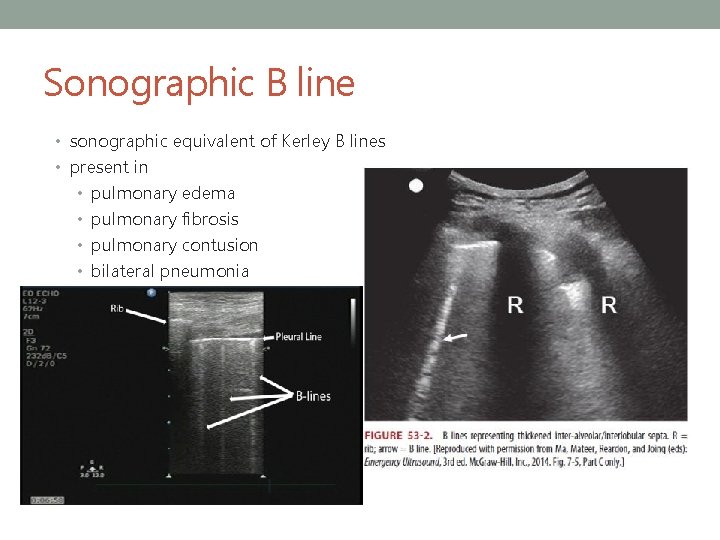
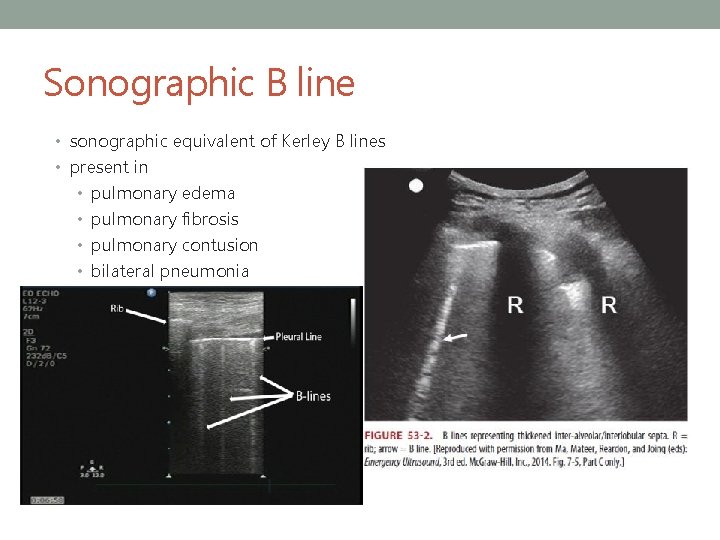
Sonographic B line • sonographic equivalent of Kerley B lines • present in • pulmonary edema • pulmonary fibrosis • pulmonary contusion • bilateral pneumonia
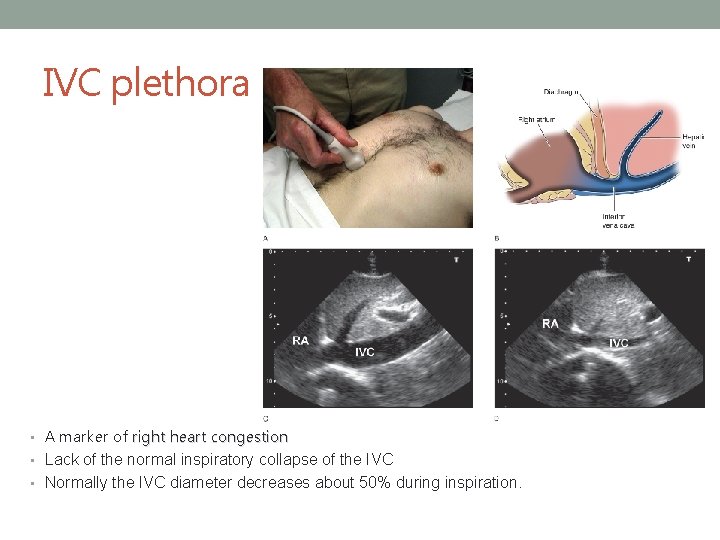
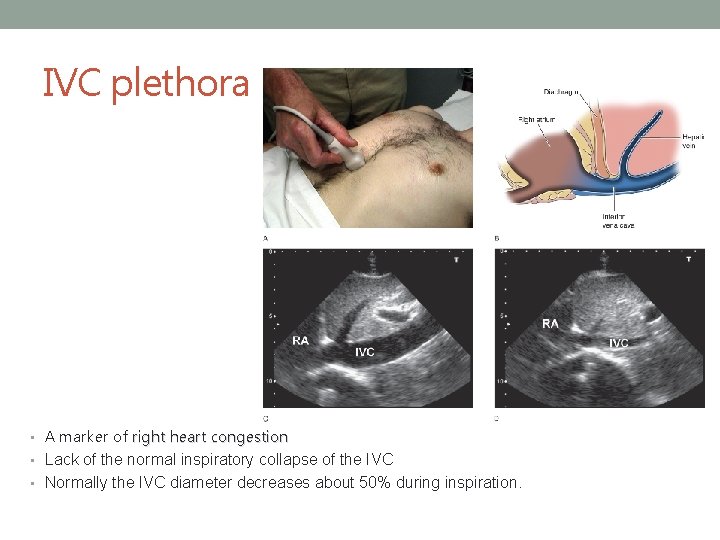
IVC plethora • A marker of right heart congestion • Lack of the normal inspiratory collapse of the IVC • Normally the IVC diameter decreases about 50% during inspiration.
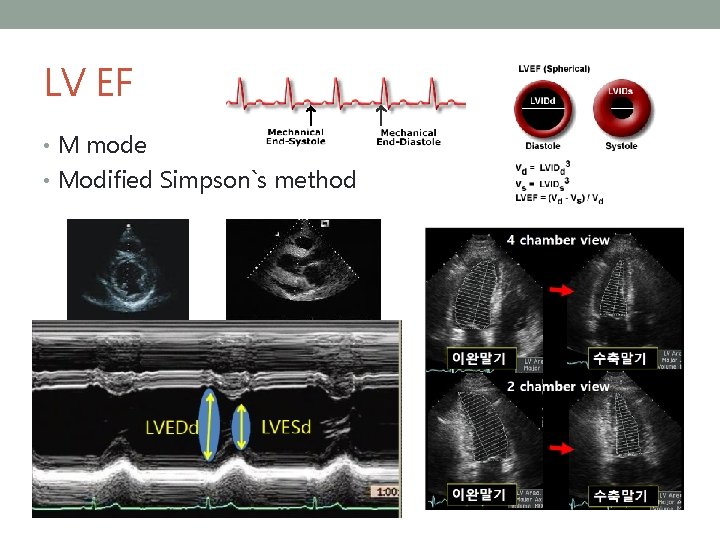
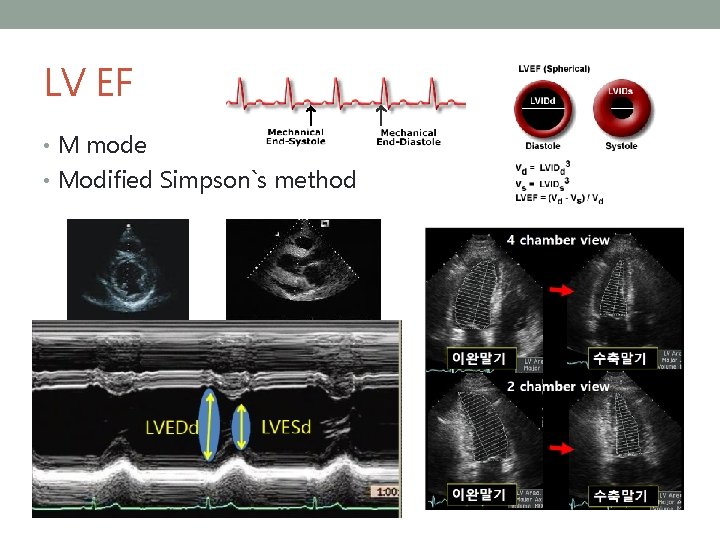
LV EF • M mode • Modified Simpson`s method
TREATMENT Hypertensive AHF Normotensive AHF
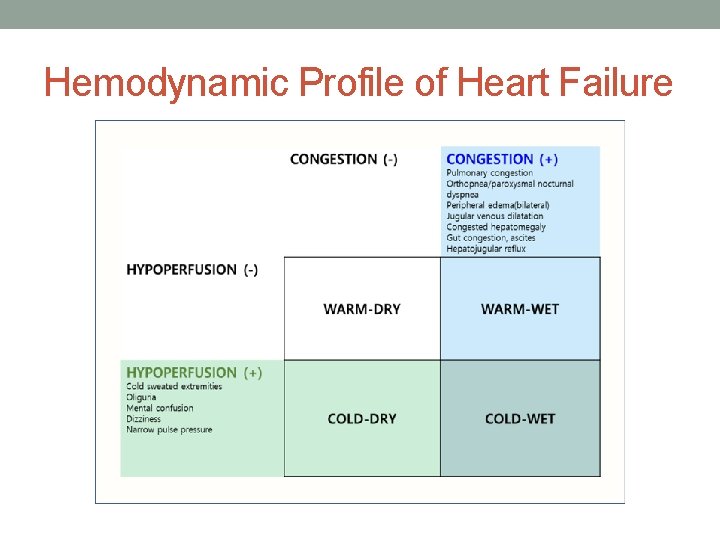
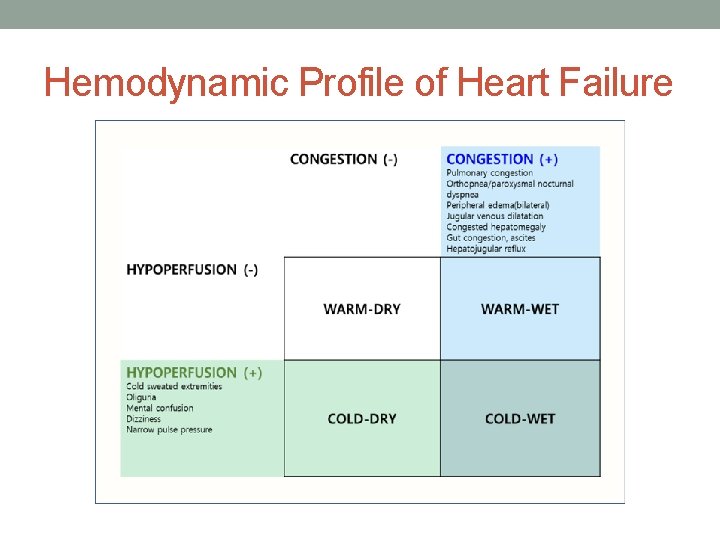
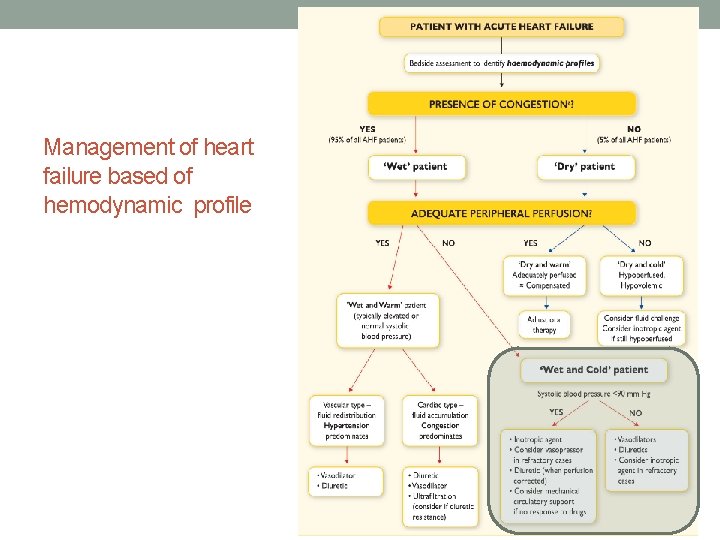
Hemodynamic Profile of Heart Failure
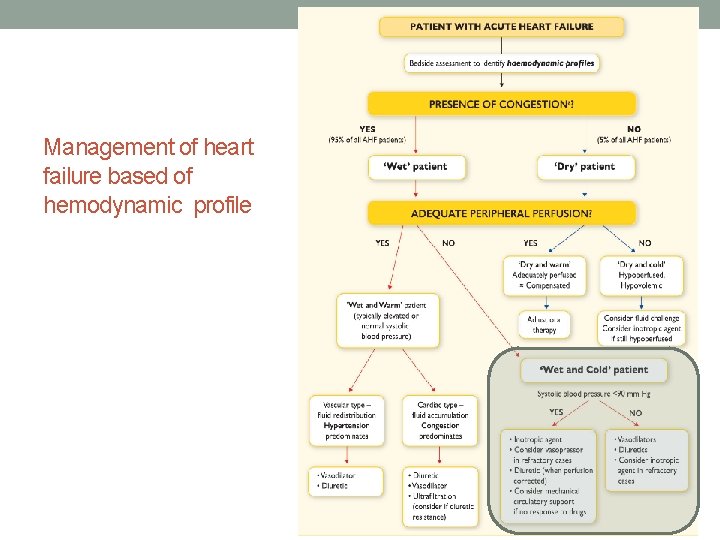
Management of heart failure based of hemodynamic profile
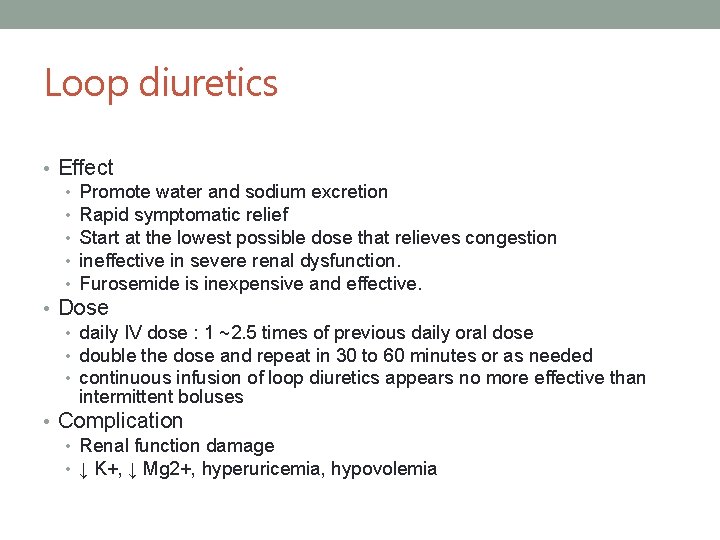
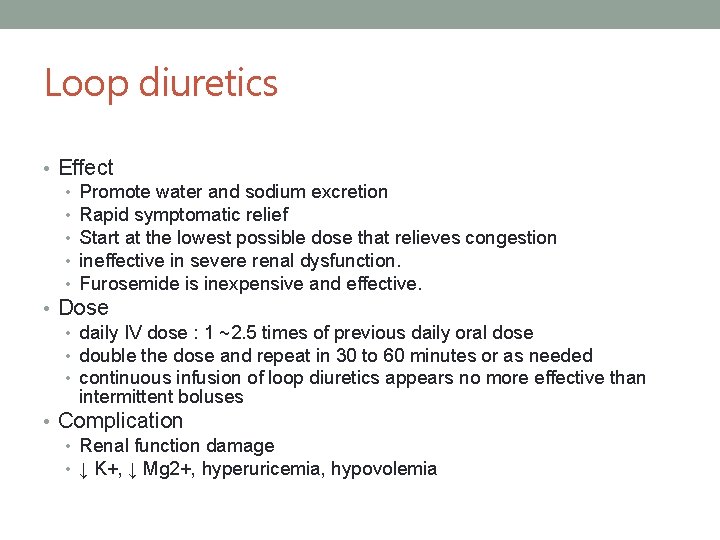
Loop diuretics • Effect • Promote water and sodium excretion • Rapid symptomatic relief • Start at the lowest possible dose that relieves congestion • ineffective in severe renal dysfunction. • Furosemide is inexpensive and effective. • Dose • daily IV dose : 1 ~2. 5 times of previous daily oral dose • double the dose and repeat in 30 to 60 minutes or as needed • continuous infusion of loop diuretics appears no more effective than intermittent boluses • Complication • Renal function damage • ↓ K+, ↓ Mg 2+, hyperuricemia, hypovolemia
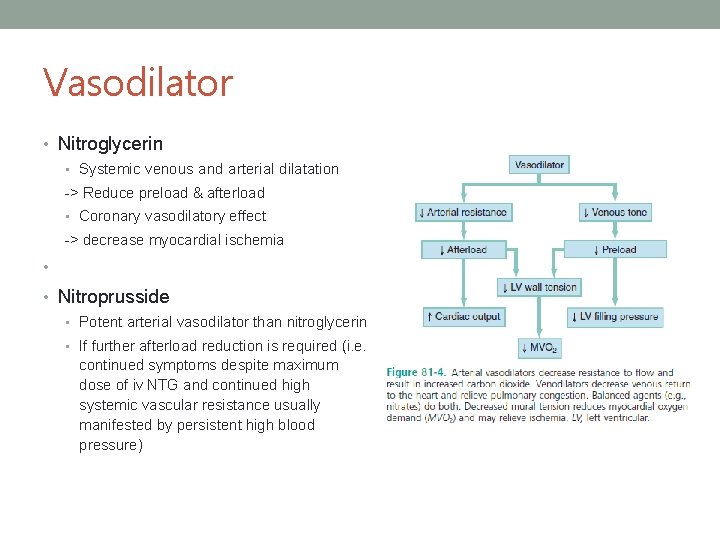
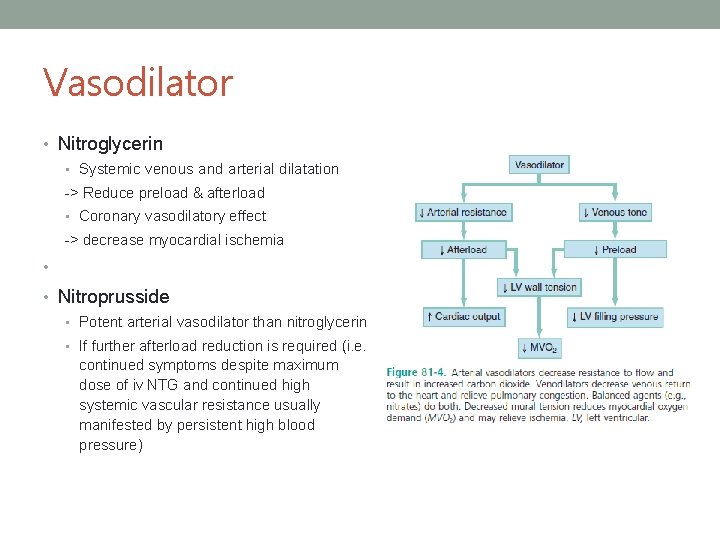
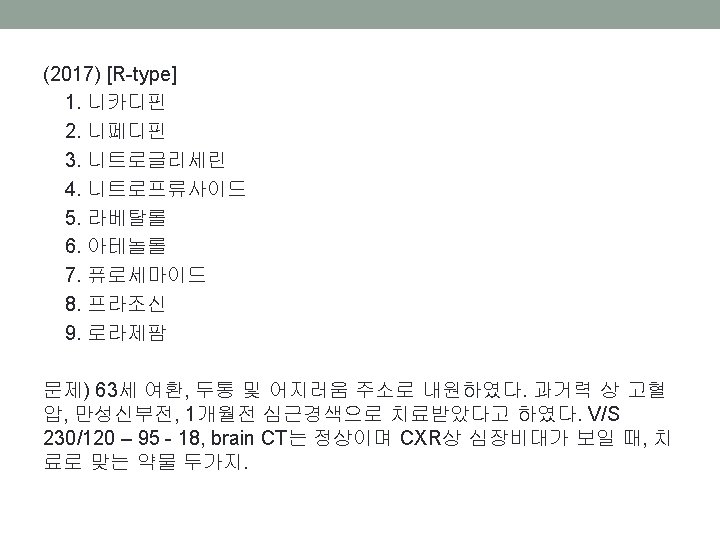
Vasodilator • Nitroglycerin • Systemic venous and arterial dilatation -> Reduce preload & afterload • Coronary vasodilatory effect -> decrease myocardial ischemia • • Nitroprusside • Potent arterial vasodilator than nitroglycerin • If further afterload reduction is required (i. e. continued symptoms despite maximum dose of iv NTG and continued high systemic vascular resistance usually manifested by persistent high blood pressure)
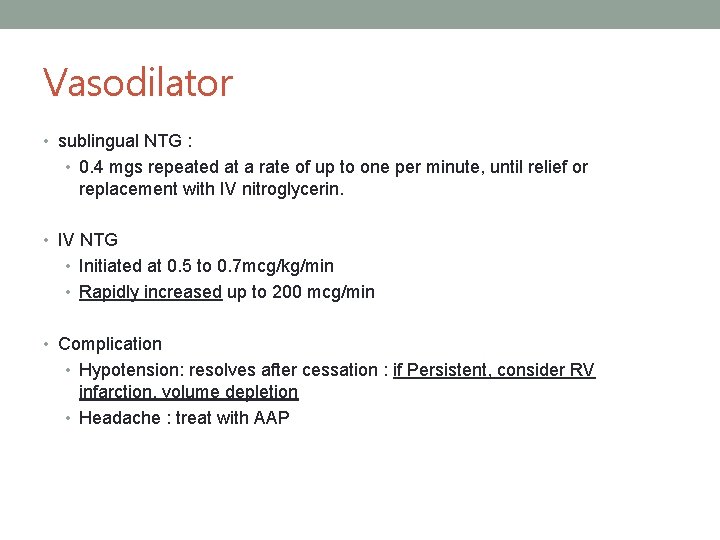
Vasodilator • sublingual NTG : • 0. 4 mgs repeated at a rate of up to one per minute, until relief or replacement with IV nitroglycerin. • IV NTG • Initiated at 0. 5 to 0. 7 mcg/kg/min • Rapidly increased up to 200 mcg/min • Complication • Hypotension: resolves after cessation : if Persistent, consider RV infarction, volume depletion • Headache : treat with AAP
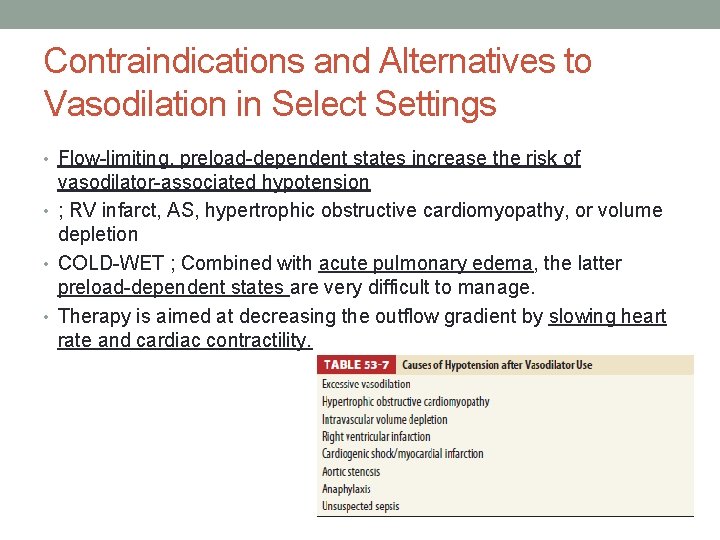
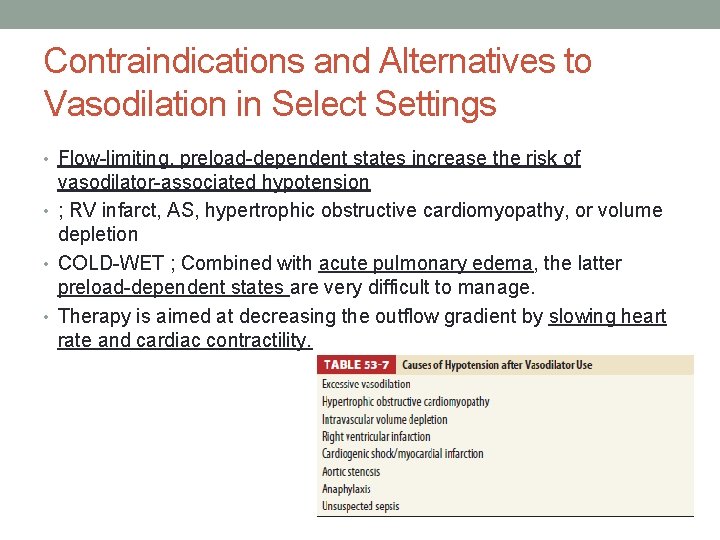
Contraindications and Alternatives to Vasodilation in Select Settings • Flow-limiting, preload-dependent states increase the risk of vasodilator-associated hypotension • ; RV infarct, AS, hypertrophic obstructive cardiomyopathy, or volume depletion • COLD-WET ; Combined with acute pulmonary edema, the latter preload-dependent states are very difficult to manage. • Therapy is aimed at decreasing the outflow gradient by slowing heart rate and cardiac contractility.
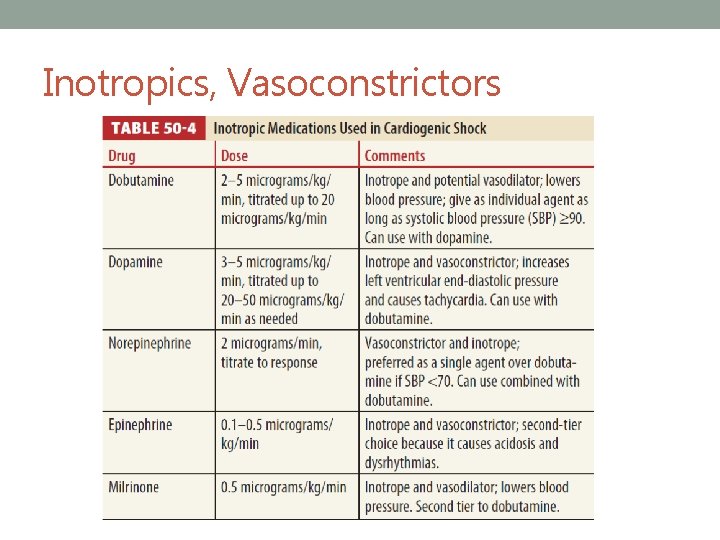
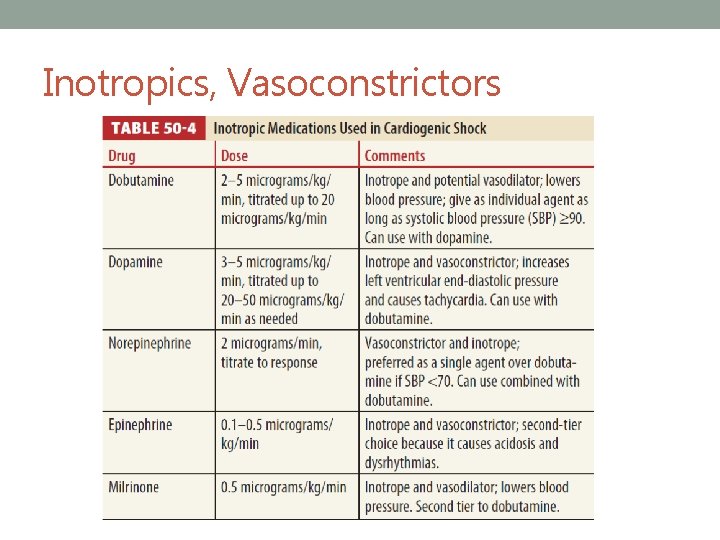
Inotropics, Vasoconstrictors
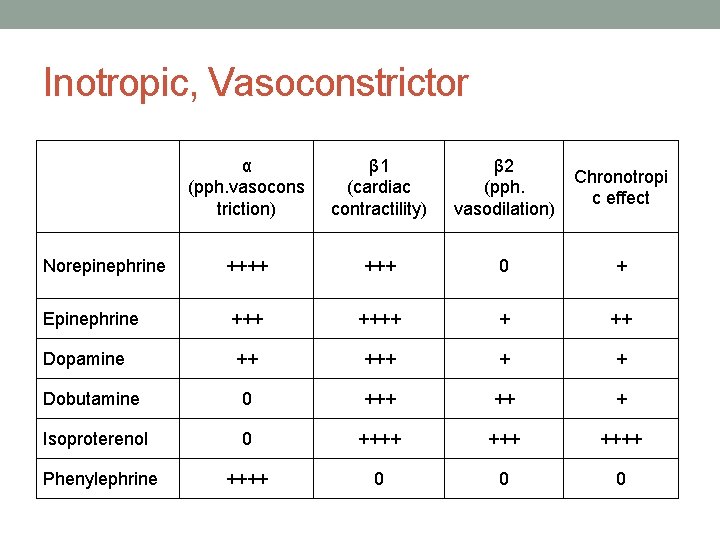
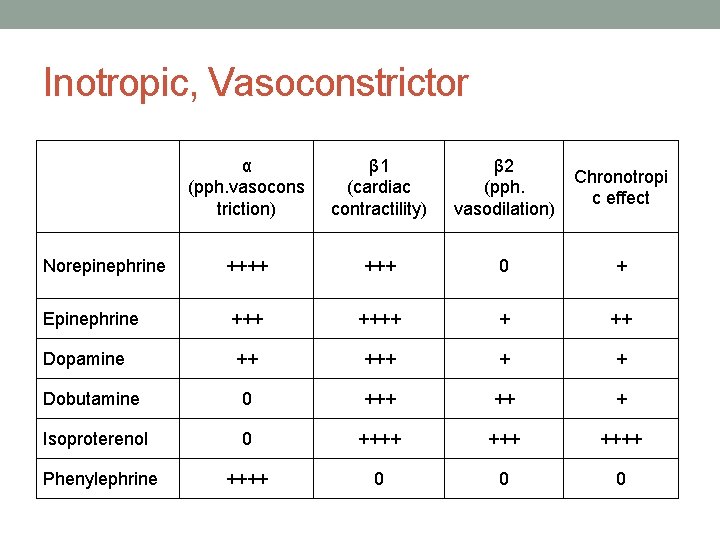
Inotropic, Vasoconstrictor α (pph. vasocons triction) β 1 (cardiac contractility) β 2 (pph. vasodilation) Chronotropi c effect Norepinephrine ++++ 0 + Epinephrine ++++ + ++ Dopamine ++ + + Dobutamine 0 +++ ++ + Isoproterenol 0 ++++ Phenylephrine ++++ 0 0 0
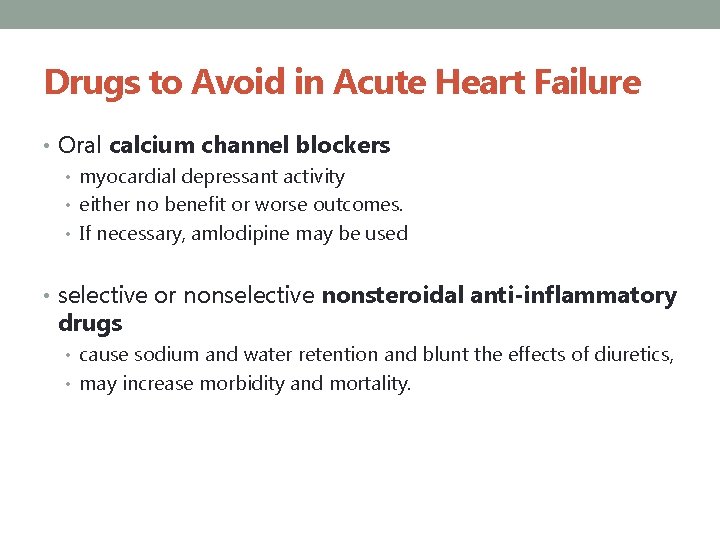
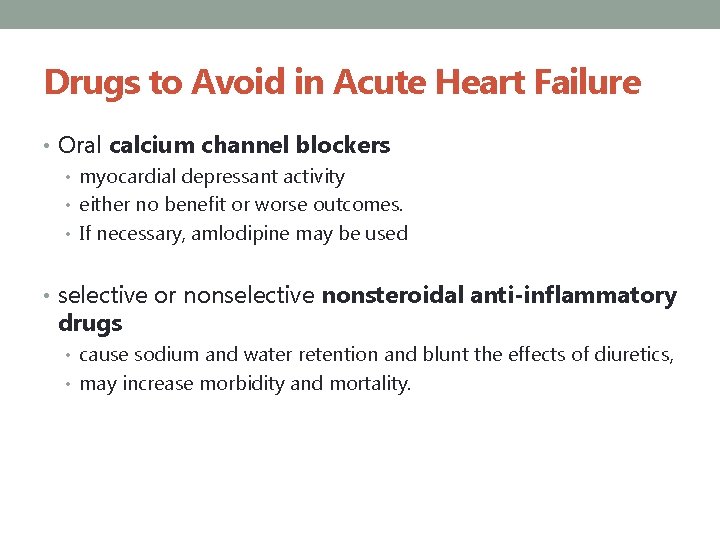
Drugs to Avoid in Acute Heart Failure • Oral calcium channel blockers • myocardial depressant activity • either no benefit or worse outcomes. • If necessary, amlodipine may be used • selective or nonselective nonsteroidal anti-inflammatory drugs • cause sodium and water retention and blunt the effects of diuretics, • may increase morbidity and mortality.
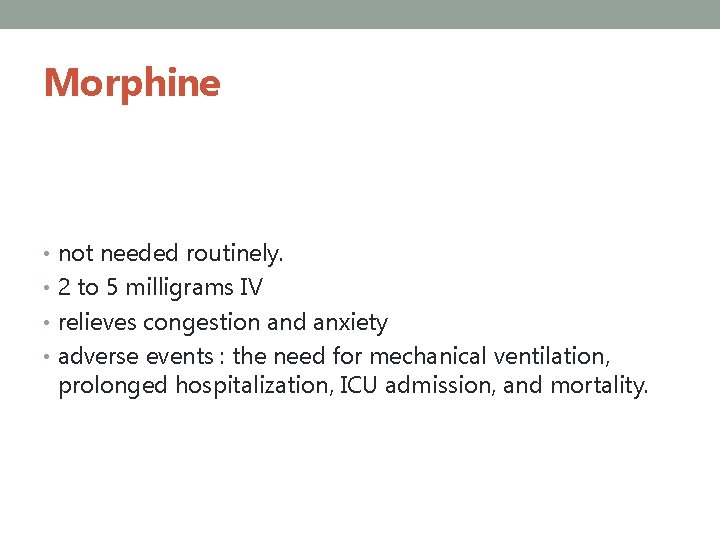
Morphine • not needed routinely. • 2 to 5 milligrams IV • relieves congestion and anxiety • adverse events : the need for mechanical ventilation, prolonged hospitalization, ICU admission, and mortality.
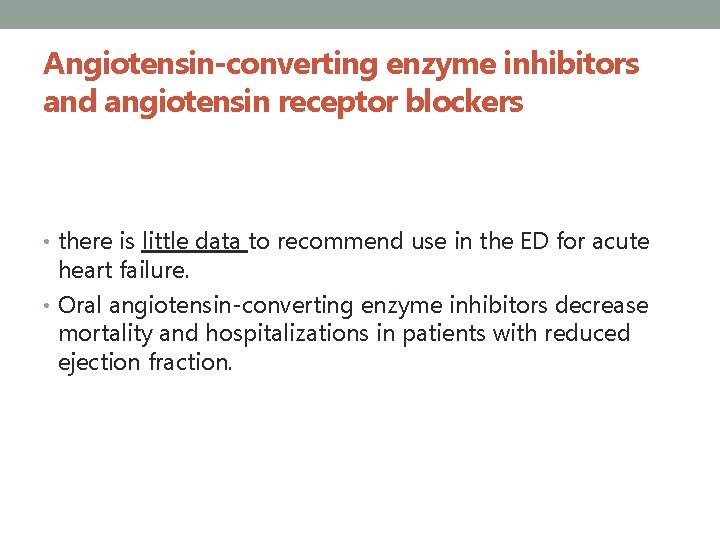
Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers • there is little data to recommend use in the ED for acute heart failure. • Oral angiotensin-converting enzyme inhibitors decrease mortality and hospitalizations in patients with reduced ejection fraction.
β-Blockers • not usually initiated • to control rate-related heart failure. • reduce sympathetic nervous system activity and are used for mortality reduction and symptom relief.
Noninvasive Ventilation • Requirements • Close monitoring • Hemodynamic stability • Facial anatomy that allows an adequate facemask seal • Patient cooperation • CPAP or Bi. PAP : 5 to 10 mm. Hg of CPAP • Reduces hospital mortality and intubation rates • high-flow oxygen recommended in patients with capillary oxygen saturation < 90% or partial pressure of oxygen in arterial blood (Pa. O 2) < 60 mm Hg
Ultrafiltration • Severe or refractory cardiorenal syndorme • Precise regulation of fluid removal • Avoidance of diuretic-associated electrolyte abnormalities • If all diuretic and medical strategies are unsuccessful, consider ultrafiltration for patients with obvious volume overload to alleviate congestive symptoms and excess weight.
Mechanical Circulatory Support • severe or refratory symptom/sign • ECMO or IABP
DISPOSITION AND F/U
• 침습적 모니터링이나 시술이 필요한 고위험군 환자들은 중 환자실로 입원한다. • 표준 치료를 제공한 후 대부분 12~24시간 후에는 증상이 소실되고 안정화된다. • 그러나 다음 조건의 환자들에서는 재검진과 추가 치료를 요한다. • Positive troponin • Blood urea nitrogen >40 milligrams/d. L • Creatinine >3. 0 milligrams/d. L • Sodium <135 m. Eq/L • New ischemic changes on ECG • New onset of acute heart failure • IV vasoactive infusions being actively titrated • Significant comorbidities requiring acute interventions • Respiratory rate ≥ 32 breaths/min and/or requiring noninvasive ventilation at the time of Observation Unit consideration • Signs of poor perfusion at the time of Observation Unit consideration

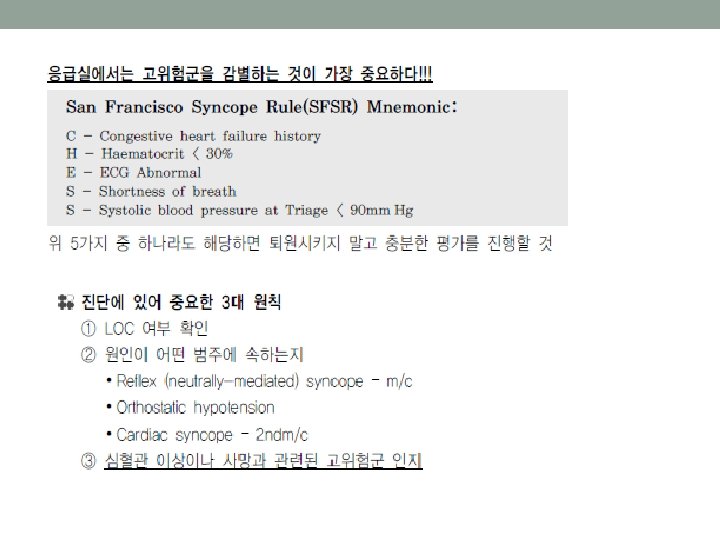
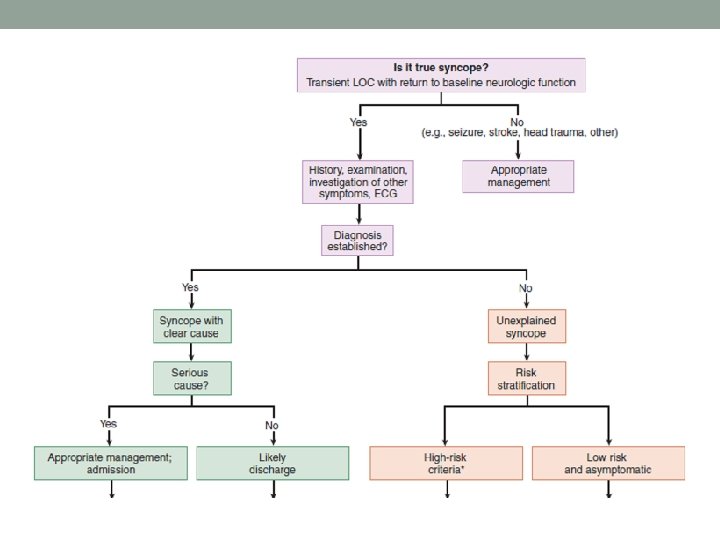
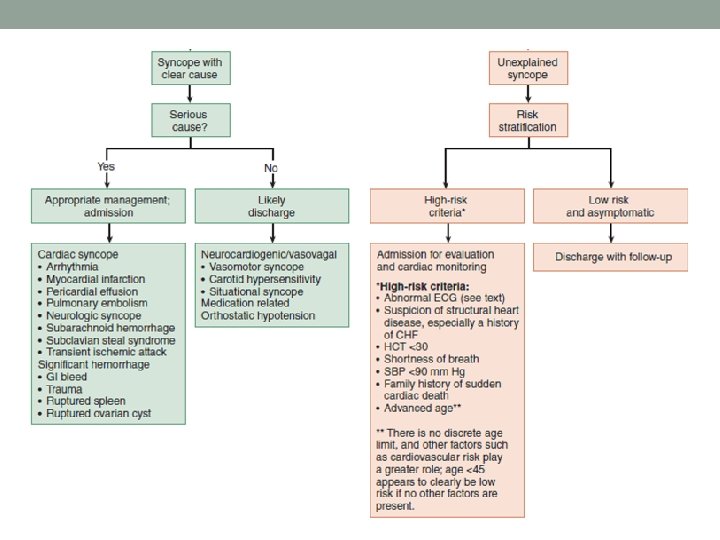
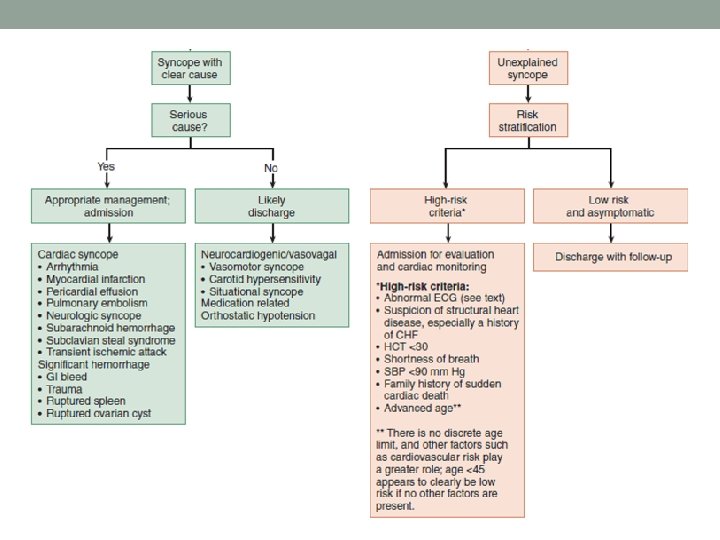
SYNCOPE
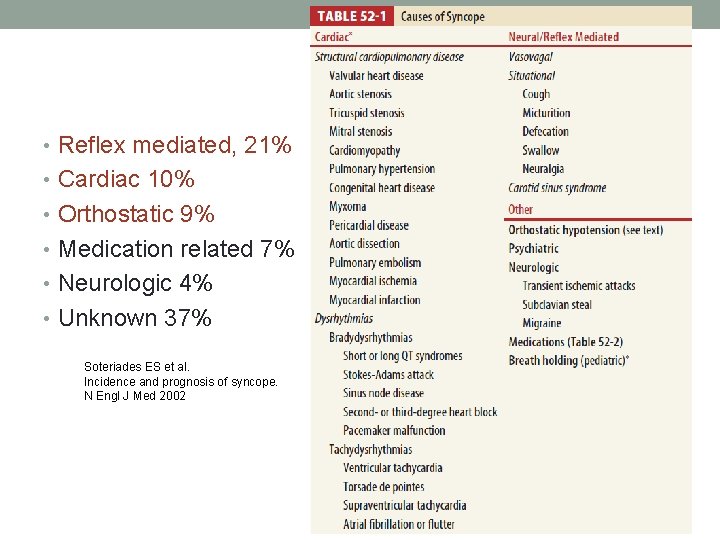
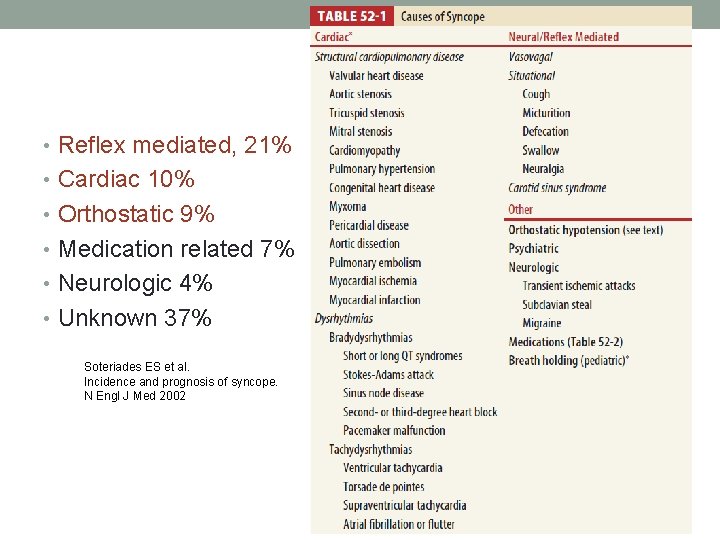
• Reflex mediated, 21% • Cardiac 10% • Orthostatic 9% • Medication related 7% • Neurologic 4% • Unknown 37% Soteriades ES et al. Incidence and prognosis of syncope. N Engl J Med 2002