Acute Heart Failure Presented by Dr T Naveen
Acute Heart Failure Presented by Dr. T. Naveen Kumar
HEART FAILURE 1. Its is a pathophysiological state in which heart is unable to maintain enough cardiac output as per requirement of body metabolic demand. 2. New York Heart Association (NYHA): Classification Class I – Patients have no limitation of physical activity. Class II – Patients have slight limitation of physical activity. Class III – Patients have marked limitation of physical activity. Class IV – Patients have symptoms even at rest and are unable to carry on any physical activity without discomfort.

3. Stages of Heart Failure : • Stage A – Asymptomatic with no heart damage but have risk factors for heart failure. • Stage B – Asymptomatic but have signs of structural heart damage • Stage C – Have symptoms and heart damage • Stage D – Refractory heart failure requiring specialized intraventions

Types of Heart Failure : Classification EF (%) Description I. Heart failure with reduced ejection fraction (HFr. EF) ≤ 40 Also referred to as systolic HF. II. Heart failure with preserved ejection fraction (HFp. EF) ≥ 50 Also referred to as diastolic HF. a. HFp. EF, borderline 41 to 49 These patients fall into a borderline or intermediate group. Their characteristics, treatment patterns, and outcomes appear similar to those of patients with HFp. EF. b. HFp. EF, improved >40 It has been recognized that a subset of patients with HFp. EF previously had HFr. EF. These patients with improvement or recovery in EF may be clinically distinct from those with persistently preserved or reduced EF.
Other types of Heart Failure: • - Based on cardiac output A. High output failure – Anaemia Pregnancy Beri beri Paget’s disease Hyperthyroidism AV malformations

B. Low output failure – 1. Impaired contractions – Ischemia / infractions - Acute mitral / Aortic regurgitation - Myocarditis - Cardiomyopathy - Sepsis - Drugs like calcium channel blockers 2. Impaired filling – Hypertension - Mitral / Tricuspid stenosis - Restrictive cardiomyopathy - Constrictive pericarditis
• 3. Excessive after load – Aortic / pulmonary stenosis - Hypertension - Pulmonary embolism 4. Dysarrythmia
- It may be Left side / Right side heart failure - It may be Forward / Backward heart failure - It may be Acute / Chronic / Acute on chronic heart failure
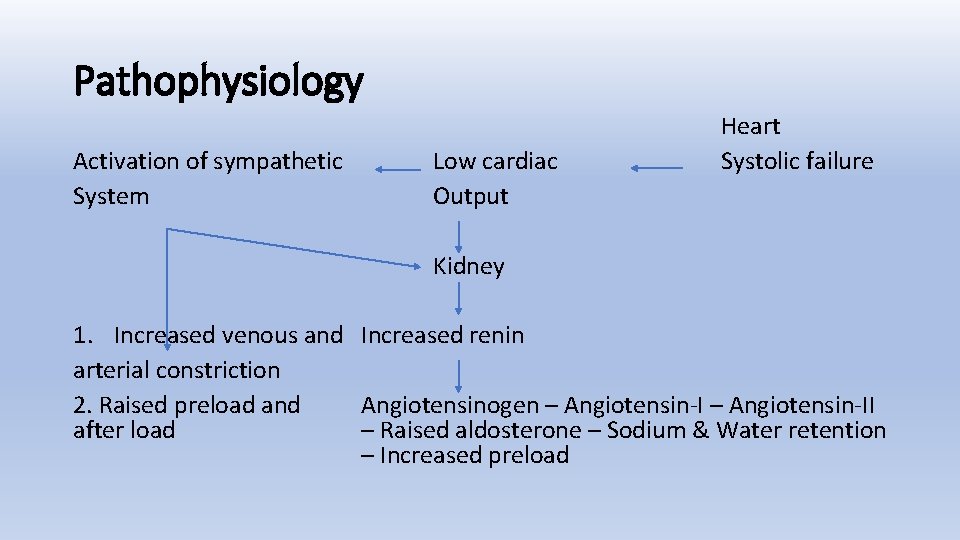
Pathophysiology Activation of sympathetic System Low cardiac Output Heart Systolic failure Kidney 1. Increased venous and Increased renin arterial constriction 2. Raised preload and Angiotensinogen – Angiotensin-II after load – Raised aldosterone – Sodium & Water retention – Increased preload
Management of Acute Heart Failure • Step I - Initial Resuscitation – Administer oxygen in high concentration to maximize tissue oxygenation as hypoxia can depress myocardial function - Assess the response clinically, by SPO 2 and ABG assessment - If not responding to oxygen alone CPAP / NIV indicated - If not responding intubation and mechanical ventilation
- Asscess the circulatory status by pulse, BP and status of major organ perfusion - Initiate inotropes or vasopressors or advanced cardiac support based on haemodynamic compromise - Therapy should be directed to treat the cause of heart failure to improve circulation and optimise BP and Cardiac output
• Prevent and treat pain – 1. 5 -3. 0 mg morphine 50 -100 mcg fentanyl • Relieve anxiety – provide reassurance and anxiolytics
Step II – Take clinical history: - Clinical history should be obtained to find the cause of AHF - Look for precipitating factors like Anaemia, Hypertension, Arrythmia, Thyroid disorders, Sepsis, Dietary and medical non compliance - Make an attempt to detect whether AHF is due to ACS, which requires urgent revascularisation
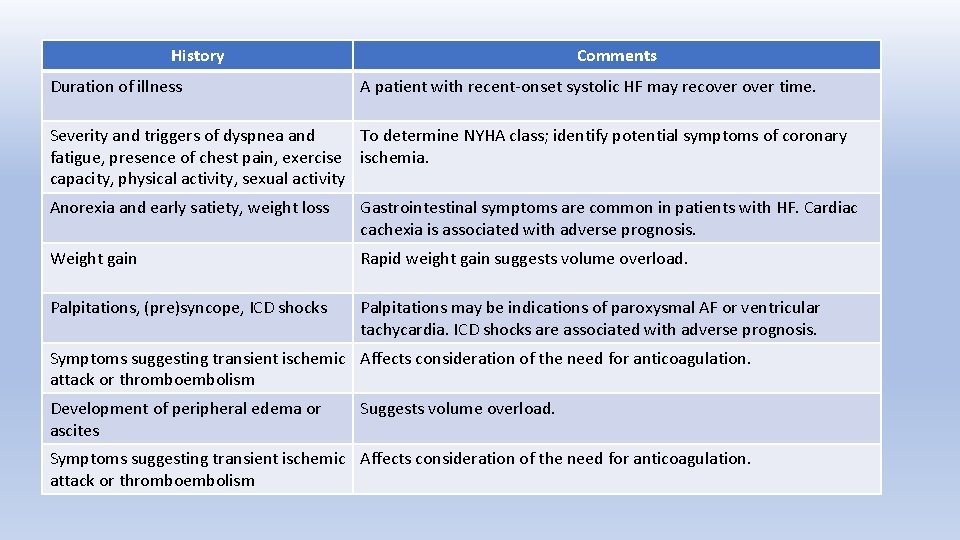
History Duration of illness Comments A patient with recent-onset systolic HF may recover time. Severity and triggers of dyspnea and To determine NYHA class; identify potential symptoms of coronary fatigue, presence of chest pain, exercise ischemia. capacity, physical activity, sexual activity Anorexia and early satiety, weight loss Gastrointestinal symptoms are common in patients with HF. Cardiac cachexia is associated with adverse prognosis. Weight gain Rapid weight gain suggests volume overload. Palpitations, (pre)syncope, ICD shocks Palpitations may be indications of paroxysmal AF or ventricular tachycardia. ICD shocks are associated with adverse prognosis. Symptoms suggesting transient ischemic Affects consideration of the need for anticoagulation. attack or thromboembolism Development of peripheral edema or ascites Suggests volume overload. Symptoms suggesting transient ischemic Affects consideration of the need for anticoagulation. attack or thromboembolism
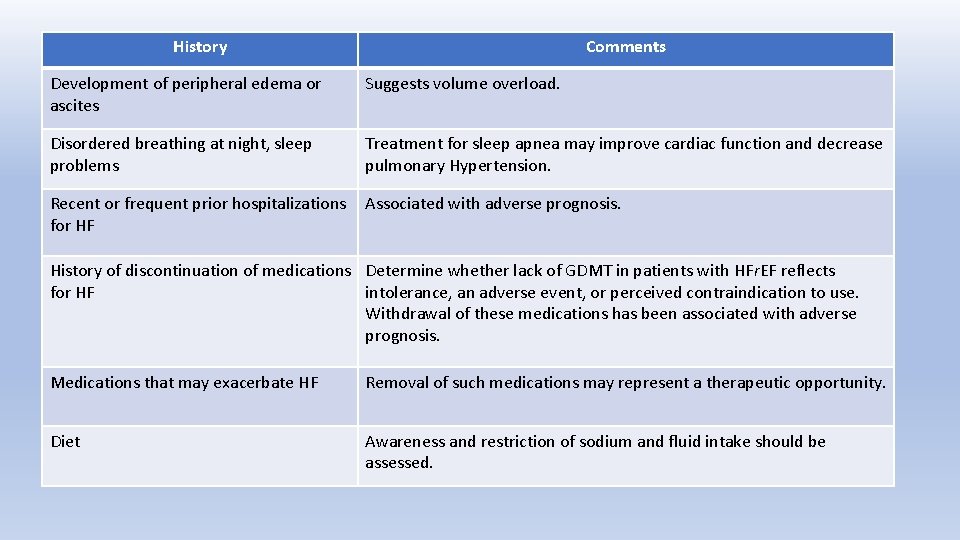
History Comments Development of peripheral edema or ascites Suggests volume overload. Disordered breathing at night, sleep problems Treatment for sleep apnea may improve cardiac function and decrease pulmonary Hypertension. Recent or frequent prior hospitalizations for HF Associated with adverse prognosis. History of discontinuation of medications Determine whether lack of GDMT in patients with HFr. EF reflects for HF intolerance, an adverse event, or perceived contraindication to use. Withdrawal of these medications has been associated with adverse prognosis. Medications that may exacerbate HF Removal of such medications may represent a therapeutic opportunity. Diet Awareness and restriction of sodium and fluid intake should be assessed.
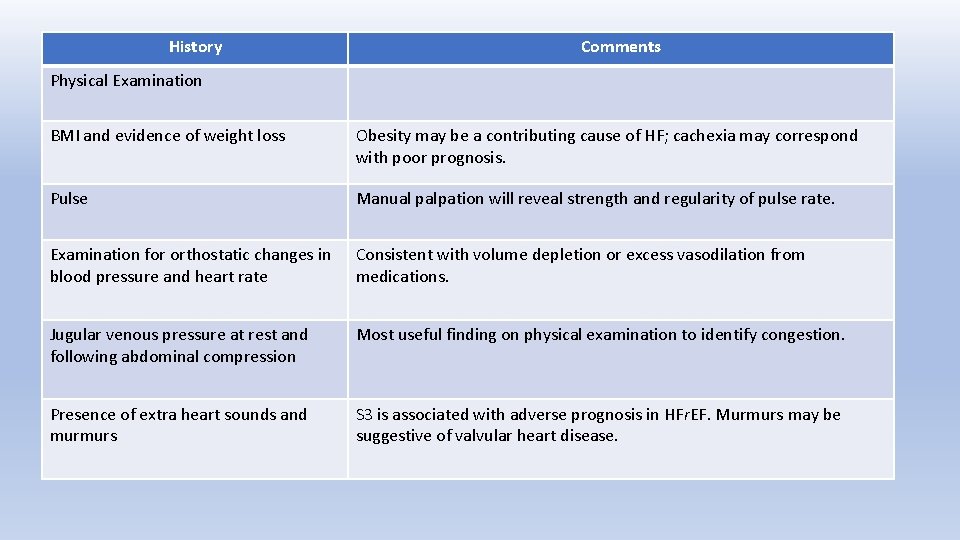
History Comments Physical Examination BMI and evidence of weight loss Obesity may be a contributing cause of HF; cachexia may correspond with poor prognosis. Pulse Manual palpation will reveal strength and regularity of pulse rate. Examination for orthostatic changes in blood pressure and heart rate Consistent with volume depletion or excess vasodilation from medications. Jugular venous pressure at rest and following abdominal compression Most useful finding on physical examination to identify congestion. Presence of extra heart sounds and murmurs S 3 is associated with adverse prognosis in HFr. EF. Murmurs may be suggestive of valvular heart disease.
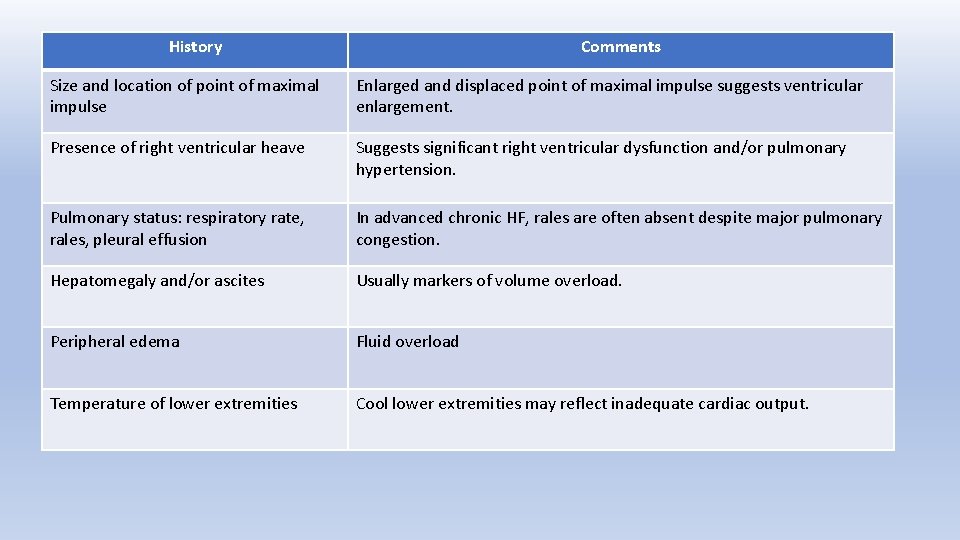
History Comments Size and location of point of maximal impulse Enlarged and displaced point of maximal impulse suggests ventricular enlargement. Presence of right ventricular heave Suggests significant right ventricular dysfunction and/or pulmonary hypertension. Pulmonary status: respiratory rate, rales, pleural effusion In advanced chronic HF, rales are often absent despite major pulmonary congestion. Hepatomegaly and/or ascites Usually markers of volume overload. Peripheral edema Fluid overload Temperature of lower extremities Cool lower extremities may reflect inadequate cardiac output.
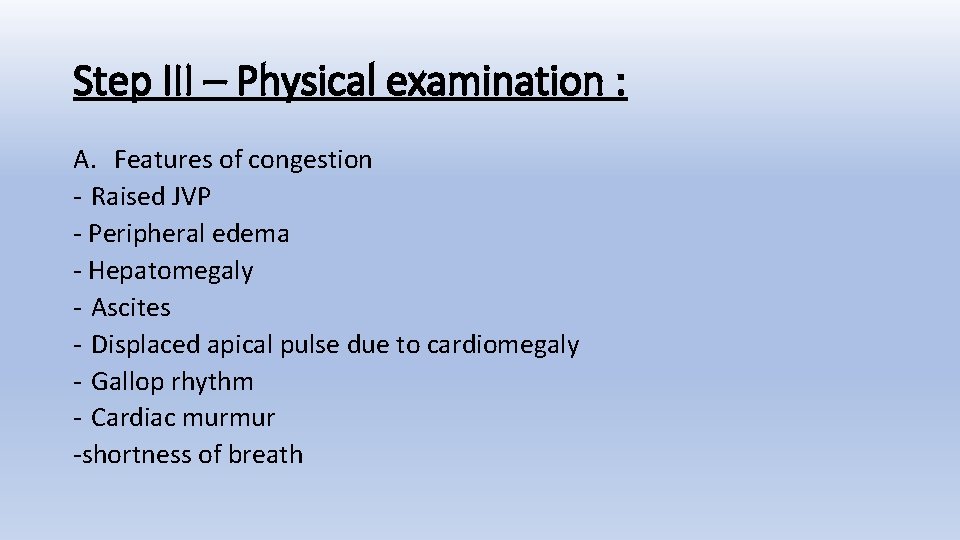
Step III – Physical examination : A. Features of congestion - Raised JVP - Peripheral edema - Hepatomegaly - Ascites - Displaced apical pulse due to cardiomegaly - Gallop rhythm - Cardiac murmur -shortness of breath
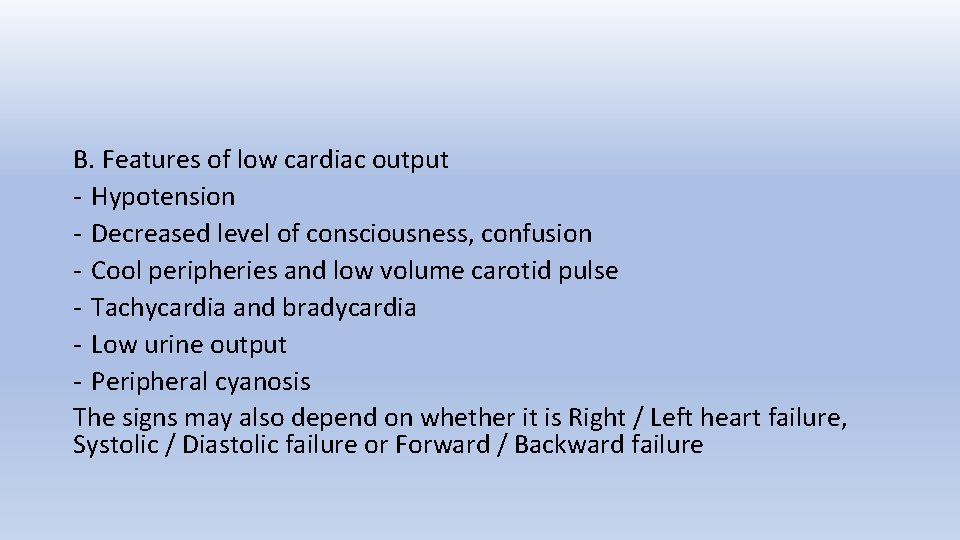
B. Features of low cardiac output - Hypotension - Decreased level of consciousness, confusion - Cool peripheries and low volume carotid pulse - Tachycardia and bradycardia - Low urine output - Peripheral cyanosis The signs may also depend on whether it is Right / Left heart failure, Systolic / Diastolic failure or Forward / Backward failure
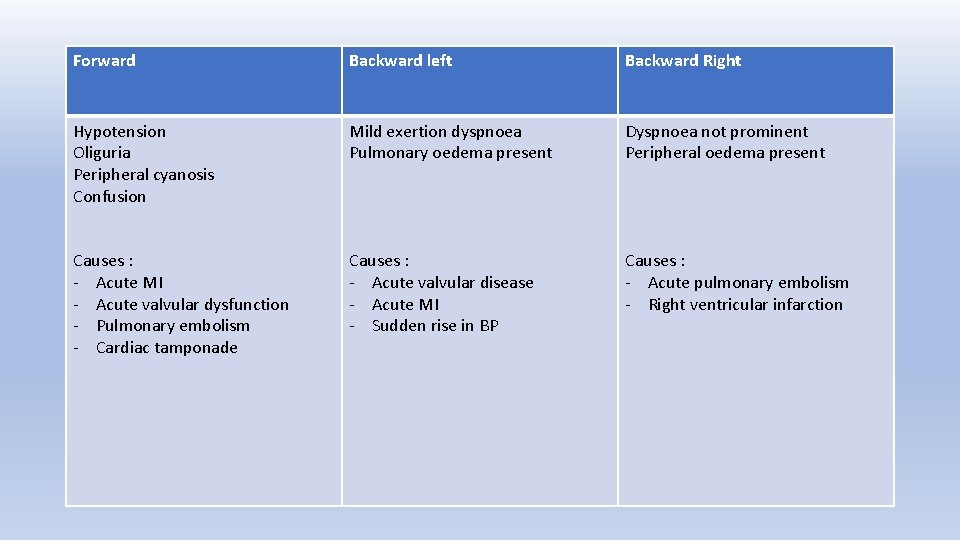
Forward Backward left Backward Right Hypotension Oliguria Peripheral cyanosis Confusion Mild exertion dyspnoea Pulmonary oedema present Dyspnoea not prominent Peripheral oedema present Causes : - Acute MI - Acute valvular dysfunction - Pulmonary embolism - Cardiac tamponade Causes : - Acute valvular disease - Acute MI - Sudden rise in BP Causes : - Acute pulmonary embolism - Right ventricular infarction
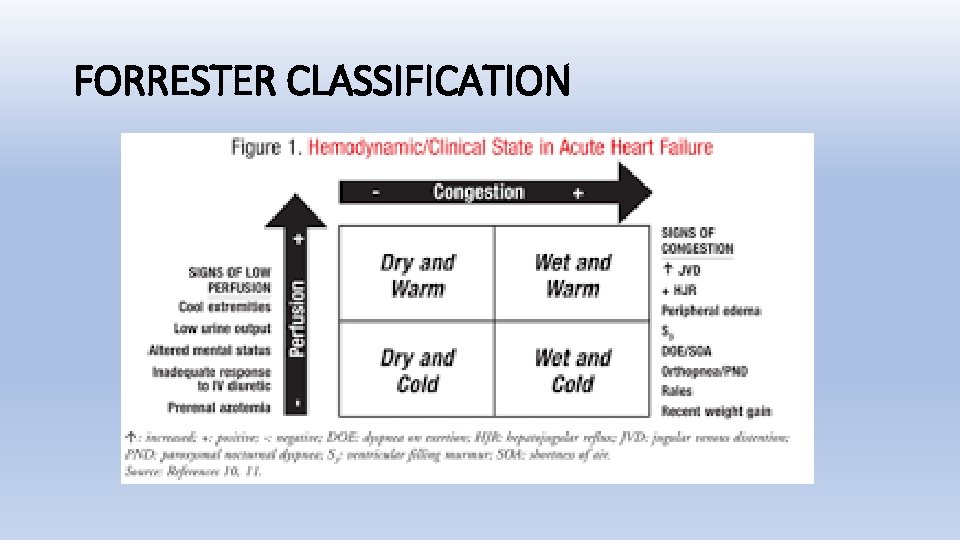
FORRESTER CLASSIFICATION
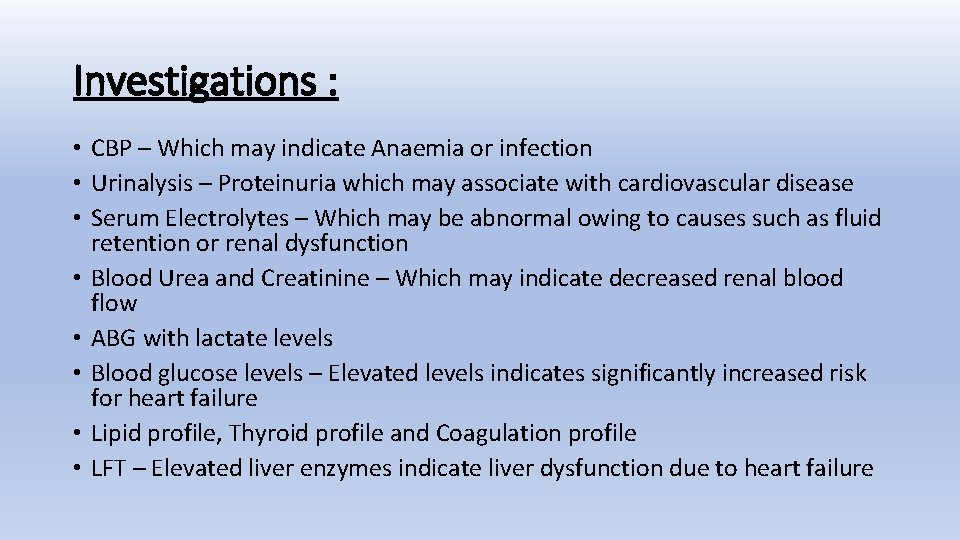
Investigations : • CBP – Which may indicate Anaemia or infection • Urinalysis – Proteinuria which may associate with cardiovascular disease • Serum Electrolytes – Which may be abnormal owing to causes such as fluid retention or renal dysfunction • Blood Urea and Creatinine – Which may indicate decreased renal blood flow • ABG with lactate levels • Blood glucose levels – Elevated levels indicates significantly increased risk for heart failure • Lipid profile, Thyroid profile and Coagulation profile • LFT – Elevated liver enzymes indicate liver dysfunction due to heart failure
• ECG – Arrythemias - Ischemia / Infarction - Acute MI - Pulmonary embolism
• Cardiac markers – CPK, Troponin-T (>0. 01 mcg/L- HF) Troponin-I (>0. 12 mcg/L- HF) CPK-MB (>3. 0 mcg/L- HF)
• Chest radiograph – Cardiac size and shape - Pulmonary congestion – Alveolar and Intestitial edema - Rule out Pneumothorax and Pneumonitis Usual findings- cardiomegaly -upper zone vessel enlargement-sign of pulmonary venous hypertension -septal (kerley B)lines- sign of interstitial edema -air space shadowing-due to alveolar edema –acutely in peri hilar (bats wing) distribution -blunt costophrenic angles-pleural effusions
• Serum BNP - <100 pg/ml rules out heart failure >500 pg/ml confirms heart failure Pro BNP >100 S/o Heart failure NT Pro BNP age <50, >450 Heart failure age 50 -75, >900 Heart failure age 75, >1800 Heart failure
• Serum BNP levels also high in - Advancing age Anaemia - Renal failure - Pulmonary Obstructive Sleep Apnoea, Severe Pneumonia, Pulmonary Hypotension - Critical illness - Bacterial sepsis, Severe burns - Chemotherapy
• Echocardiogram – Global and regional LV function, valvular abnormalities, diastolic function, diagnostic of cardiac tamponade, RV dysfunction due to pulmonary embolism • Holter monitoring – Which may reveal arrhythmias or abnormal electrical activity • Cardiac catherization and Coronary angiogram
Other Investigations: • Serum and Urine Electrophoresis for light chain disease • Testing for rheumatologic diseases, amyloidosis which can cause cardiomyopathy • Screening for sleep disturbed breathing which can effect neuro hormonal activation • Genetic testing for at risk patients with a first degree relative who has been diagnosed with a cardiomyopathy leading to heart failure • Screening for haemochromatosis in which iron over load effects cardiac function • Screening for HIV, which may result in heart failure
Right Heart Catheterization : • Right Heart Catheterization to estimate the cardiac output cardiac index • Indications: • Patients with significant hypotension (SBP <90 mm. Hg) • Worsening renal function during initial therapy • Patients being considered for cardiac transplantation or placement of MCS device
Left Heart Catheterization / CAG : • It is indicated for patients with HF and angina and may be useful for those persons without angina but with LV dysfunction • In patients with known CAD and angina or with significant ischemia diagnosed by ECG or non invasive testing and impaired ventricular function CAG is indicated
Endomyocardial biopsy : • It is indicated in patients with rapid progressive HF despite of appropriate medical therapy • Acute cardiac rejection status after cardiac transplantation • Rapidly progressive and unexplained cardiomyopathy
Framingham criteria • Diagnosis of CHF requires the simultaneous presence of at least 2 major criteria or 1 major and 2 minor criteria Major criteria -paroxysmal nocturnal dyspnoea -neck vein distention -radiographic cardiomegaly - Acute pulmonary edema - -s 3 gallop - Hepato jugular reflex - Weight loss more than 4. 5 kg in 5 days in response to treatment
• Minor criteria -bilateral ankle edema -nocturnal cough -dyspnoea on ordinary exertion -hepatomegaly -pleural effusion -tachycardia more than 120/min
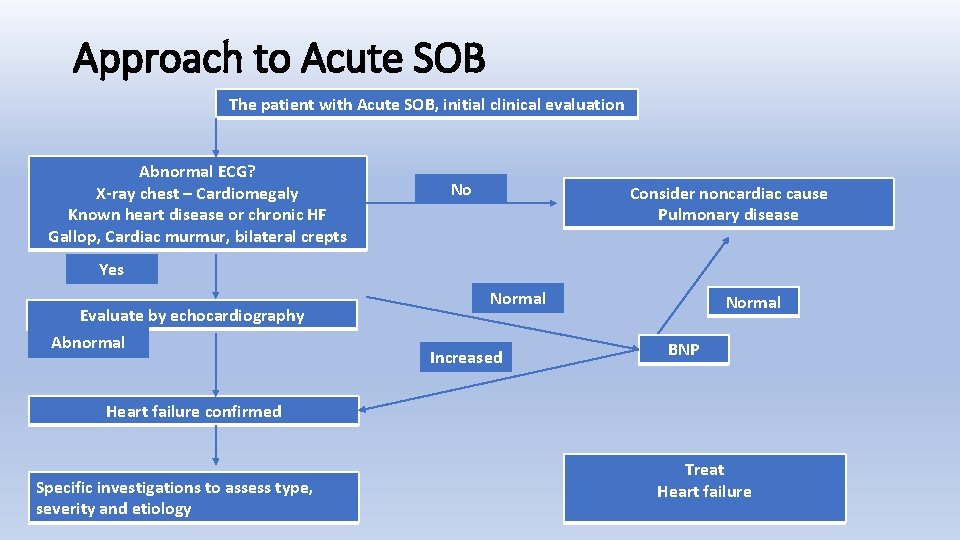
Approach to Acute SOB The patient with Acute SOB, initial clinical evaluation Abnormal ECG? X-ray chest – Cardiomegaly Known heart disease or chronic HF Gallop, Cardiac murmur, bilateral crepts No Consider noncardiac cause Pulmonary disease Yes Evaluate by echocardiography Abnormal Normal Increased Normal BNP Heart failure confirmed Specific investigations to assess type, severity and etiology Treat Heart failure
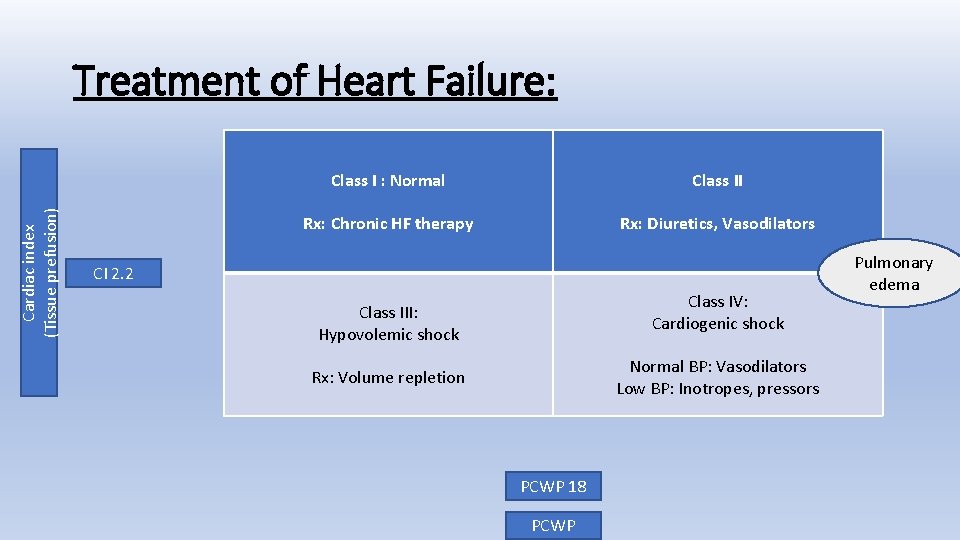
Cardiac index (Tissue prefusion) Treatment of Heart Failure: Class I : Normal Class II Rx: Chronic HF therapy Rx: Diuretics, Vasodilators CI 2. 2 Class IV: Cardiogenic shock Class III: Hypovolemic shock Normal BP: Vasodilators Low BP: Inotropes, pressors Rx: Volume repletion PCWP 18 PCWP Pulmonary edema
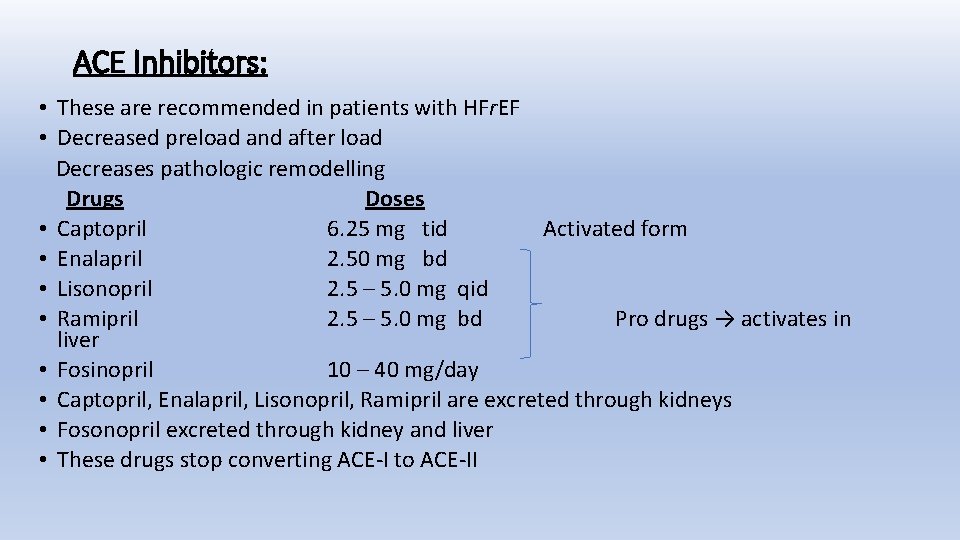
ACE Inhibitors: • These are recommended in patients with HFr. EF • Decreased preload and after load Decreases pathologic remodelling Drugs Doses • Captopril 6. 25 mg tid Activated form • Enalapril 2. 50 mg bd • Lisonopril 2. 5 – 5. 0 mg qid • Ramipril 2. 5 – 5. 0 mg bd Pro drugs → activates in liver • Fosinopril 10 – 40 mg/day • Captopril, Enalapril, Lisonopril, Ramipril are excreted through kidneys • Fosonopril excreted through kidney and liver • These drugs stop converting ACE-I to ACE-II
Side effects: • Cough • Angioedema • Proteinuria • Hypotension • Rashes • Increased renin • Low aldosterone • Hyponatremia with hyperkalemia
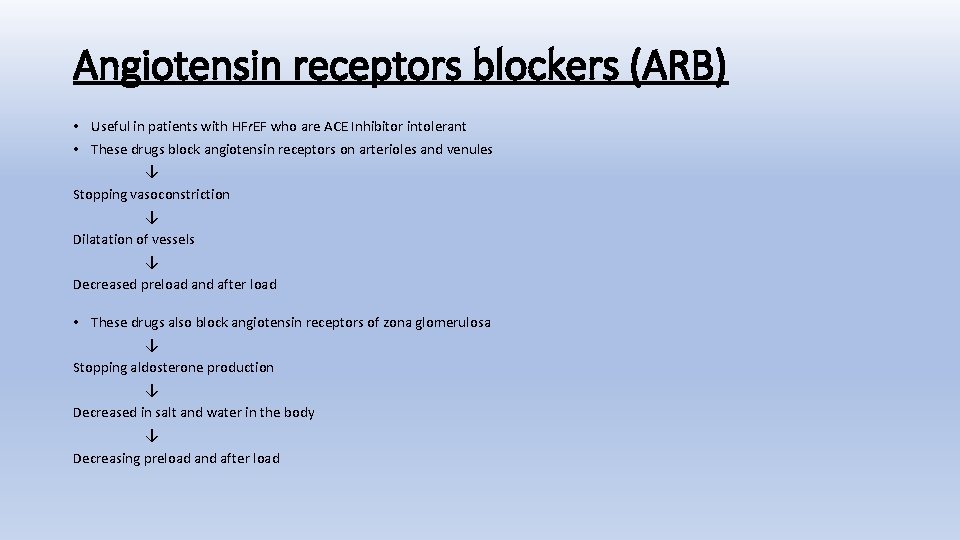
Angiotensin receptors blockers (ARB) • Useful in patients with HFr. EF who are ACE Inhibitor intolerant • These drugs block angiotensin receptors on arterioles and venules ↓ Stopping vasoconstriction ↓ Dilatation of vessels ↓ Decreased preload and after load • These drugs also block angiotensin receptors of zona glomerulosa ↓ Stopping aldosterone production ↓ Decreased in salt and water in the body ↓ Decreasing preload and after load
Drugs: • Losartan 50 mg qid • Valsartan 40 mg bd • Gandesartan 4. 0 – 8. 0 mg bd Advantages : Over ACEI Side effects are similar to ACEI except cough and angio edema • Those patients who develops angioedema and dry cough with ACEI can take ARBS
Beta blockers: • In acute heart failure beta blockers should start with low dose and titrate gradually to achieve the heart rate of <60/min due to its negative inotropic effects DRUG: • Metoprolol 12. 5 – 50 mg – It is a long acting drug • Carvedilol 3. 125 – 25 mg • Blocks α 1 AR → Dilatation of arteriole and venules → Decreased preload and after load • Blocks β 1 AR → Decreased heart rate • Blocks β 2 AR → Decreases renin production
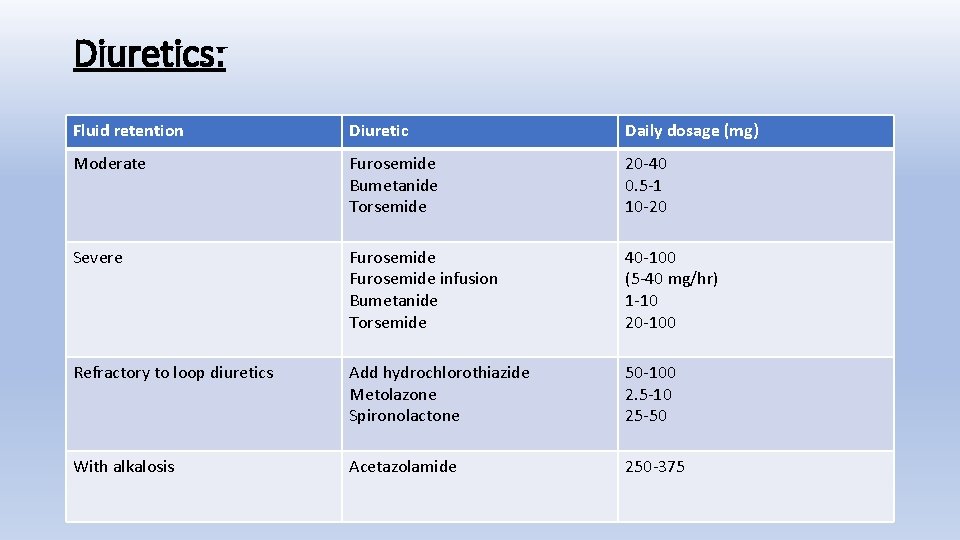
Diuretics: Fluid retention Diuretic Daily dosage (mg) Moderate Furosemide Bumetanide Torsemide 20 -40 0. 5 -1 10 -20 Severe Furosemide infusion Bumetanide Torsemide 40 -100 (5 -40 mg/hr) 1 -10 20 -100 Refractory to loop diuretics Add hydrochlorothiazide Metolazone Spironolactone 50 -100 2. 5 -10 25 -50 With alkalosis Acetazolamide 250 -375
• Loop diuretics are strong diuretics and they work even GFR is low • Thiazide diuretics Have synergetic effect and useful in refractory heart failure Mechanism of action • Loss of salt and water → ↓ blood volume → ↓ decreases preload • Act as vasodilator → decreases preload and after load Side effects: • Electrolyte and fluid imbalance • Hypotension • Azotemia
Aldosterone antagonist: • These drugs binds with aldosterone receptors and decreases aldosterone action → Decreases preload Drug: • Spironolactone – Most common aldosterone antagonist • Eplerenone – Much more selective than spironolactone on target but less effective Adverse effects: - Hyperkalemia - Renal failure
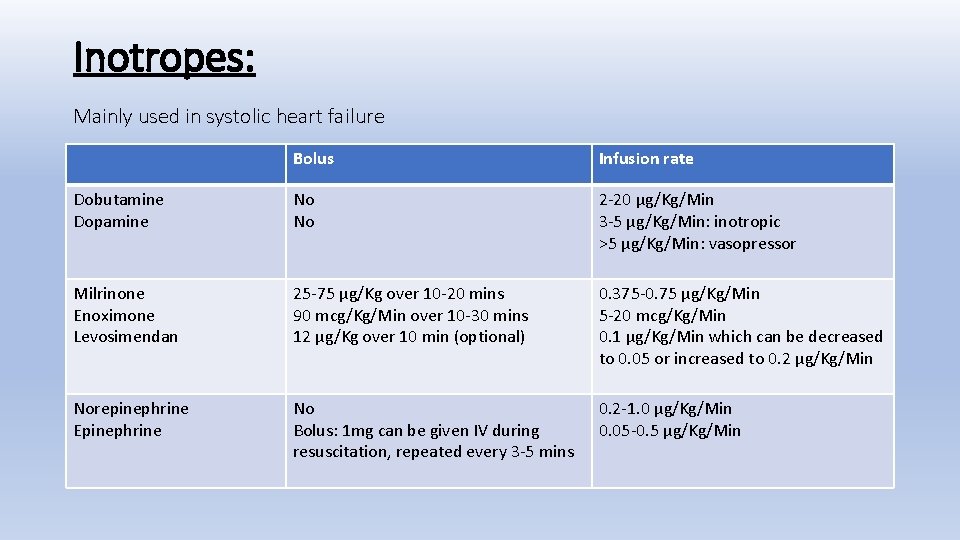
Inotropes: Mainly used in systolic heart failure Bolus Infusion rate Dobutamine Dopamine No No 2 -20 µg/Kg/Min 3 -5 µg/Kg/Min: inotropic >5 µg/Kg/Min: vasopressor Milrinone Enoximone Levosimendan 25 -75 µg/Kg over 10 -20 mins 90 mcg/Kg/Min over 10 -30 mins 12 µg/Kg over 10 min (optional) 0. 375 -0. 75 µg/Kg/Min 5 -20 mcg/Kg/Min 0. 1 µg/Kg/Min which can be decreased to 0. 05 or increased to 0. 2 µg/Kg/Min Norepinephrine Epinephrine No Bolus: 1 mg can be given IV during resuscitation, repeated every 3 -5 mins 0. 2 -1. 0 µg/Kg/Min 0. 05 -0. 5 µg/Kg/Min
1. Digitalis group : - Digoxin - Digitoxin üDigoxin is short and fast acting and excreted through kidneys üDigoxin is useful in chronic treatment of chronic heart failure Side effects: üCardiac arrythemias üGI symptoms üVisual disturbances and confusion
2. Dopamine and Dobutamine : These drugs binds with β 1 AR and stimulates → increased cyclic AMP levels → increased contractility
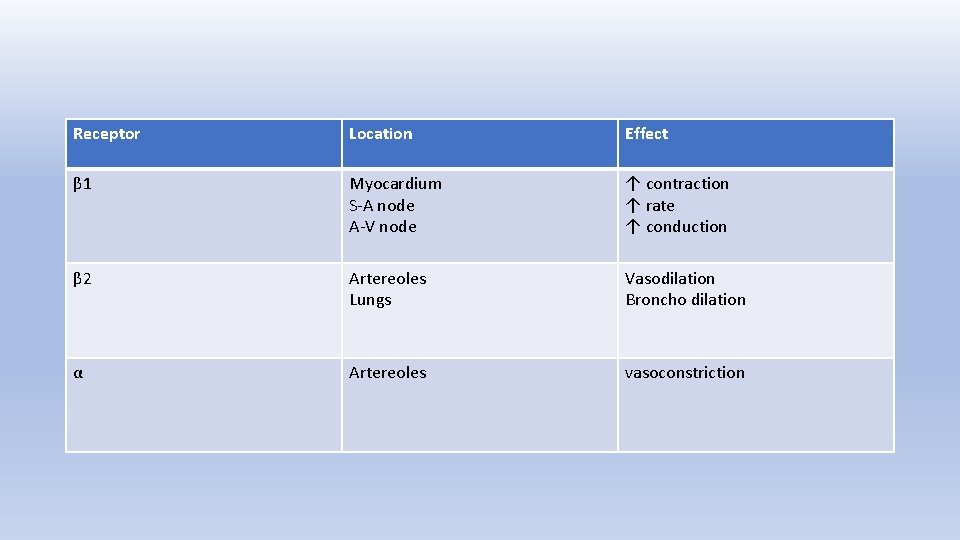
Receptor Location Effect β 1 Myocardium S-A node A-V node ↑ contraction ↑ rate ↑ conduction β 2 Artereoles Lungs Vasodilation Broncho dilation α Artereoles vasoconstriction
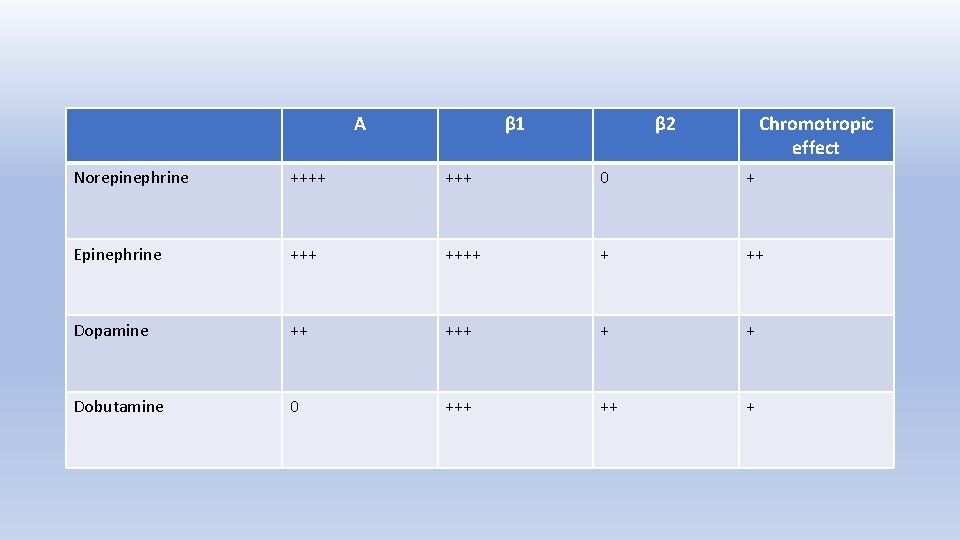
Α β 1 β 2 Chromotropic effect Norepinephrine ++++ 0 + Epinephrine ++++ + ++ Dopamine ++ + + Dobutamine 0 +++ ++ +
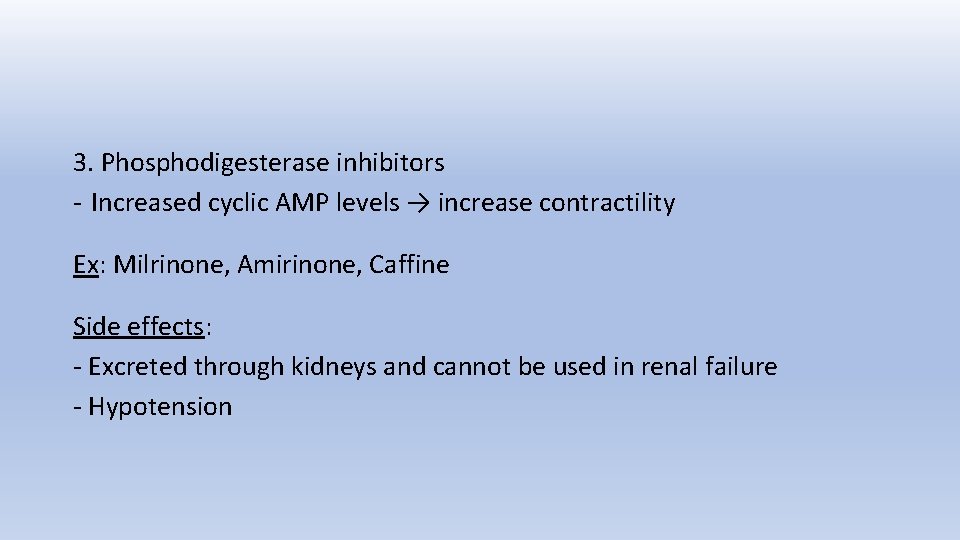
3. Phosphodigesterase inhibitors - Increased cyclic AMP levels → increase contractility Ex: Milrinone, Amirinone, Caffine Side effects: - Excreted through kidneys and cannot be used in renal failure - Hypotension
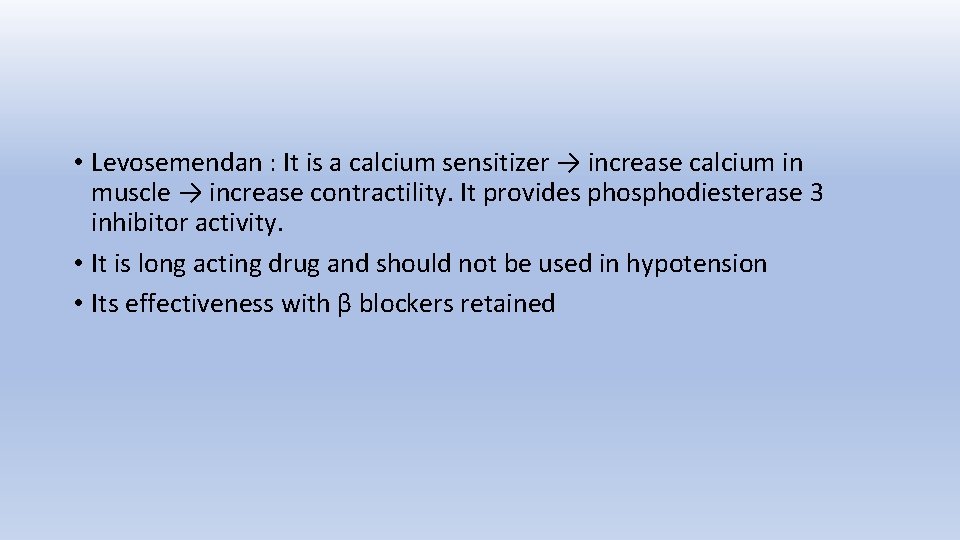
• Levosemendan : It is a calcium sensitizer → increase calcium in muscle → increase contractility. It provides phosphodiesterase 3 inhibitor activity. • It is long acting drug and should not be used in hypotension • Its effectiveness with β blockers retained
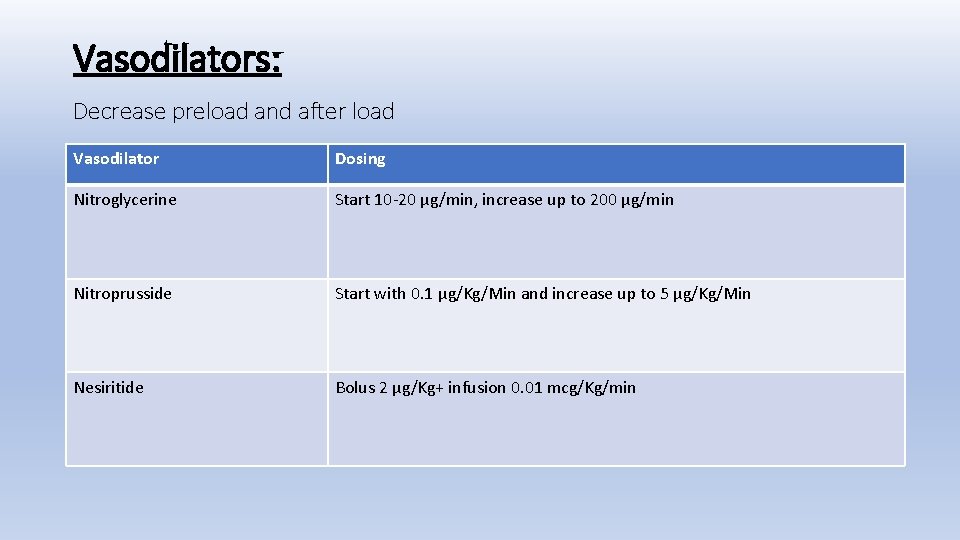
Vasodilators: Decrease preload and after load Vasodilator Dosing Nitroglycerine Start 10 -20 µg/min, increase up to 200 µg/min Nitroprusside Start with 0. 1 µg/Kg/Min and increase up to 5 µg/Kg/Min Nesiritide Bolus 2 µg/Kg+ infusion 0. 01 mcg/Kg/min
• AICD implantation indications to prevent sudden cardiac death - All patients with LVEF <30% in Non ischemic cardiomyopathy - LVEF <30% at least after six weeks of MI - Prior to VF/VT • Patient remain symptomatic despite of optimal medical treatment and have LVEF <30% with wide QRS more than 120 ms are candidates for biventricular pacing
Intra aortic ballon pump • Indications -cardiogenic shock -post bypass -post MI -cardiomyopathy -severe IHD awaiting surgery or stenting -prophylactically in high risk patient pre stenting/ cardiac surgery
Ventricular assist device(VAD) • It is a mechanical pump used to provide adequate cardiac output when heart failure is resistant to medical therapy • Indications -severe heart failure and cardiogenic shock ( pt. are usually NYHA class 4 , with EF<25% and vo 2 max <15) Uses -bridge to recovery eg-unable to wean off bypass and transient cardiomyopathy -bridge to herat transplantation -bridge to decision- temporizing measure until a decision can be made on one of the above -destination therapy if not eligible for cardiac transplantation
General Care: • Adequate nutrition • Thromboprophylaxis • Correct electrolyte imbalance • Prevent and treat infections
Treat Specific Cause: • Pulmonary embolism → Thrombolysis / Surgical thromboectomy • Valvular defect → Repair / replace • Coronary artery disease → CABG / PTCA • Cardiac Tamponade → Pericardiocentesis • Arrythemias → Cardioversion, Anti arrythemics
Long term care: - Salt restriction <4 gm/day Statins Fluid restriction 1. 5 -2. 0 Litre/day Regular follow up Anticoagulation therapy Omega 3 fatty acids
Cardio-renal syndrome: • Cardio-renal syndromes are disorders of heart and kidneys where by acute and long term dysfunction in one organ may induce acute or long term dysfunction of other organ Classification: • Type I- ADHF → AKI • Type II- CHF → CKD • Type III- AKI → AHF • Type IV- CKD → CHF • Type V- Co-development of heart failure and CKD
Mechanism: • Low cardiac output leading to kidney failure • In good cardiac output patients → backward pressure → impairment of renal venous return → kidney failure Treatment: • Ultra filtration along with the treatment of heart failure

- Slides: 61