Acute gastroenteritis Acute gastroenteritis Diarrhea Increase in stool
- Slides: 35
Acute gastroenteritis
Acute gastroenteritis Diarrhea Increase in stool frequency, fluidity (water content), or volume, in comparison with the previously established “normal” pattern • Acute diarrhea Less than 2 weeks • With or without vomiting, fever or abdominal pain
Epidemiology • Second most common cause of death in pediatric • 2 -4 million deaths annually • 2. 5 billion case annually in <5 years • 3. 6 episode/child – year • 10% of admissions • Rota virus is the most common cause worldwide
Risk factors • • • AGE is associated with poverty and poor hygiene Contamination of water and food supply (cholera) Young age Malnutrtion: Zinc and Vitamin A deficiency Immunodeficiency Transmission: fecal-oral or direct contact
Mechanisms of Diarrhea Ø Osmotic Ø Secretory Ø Exudative Ø Motility disorders
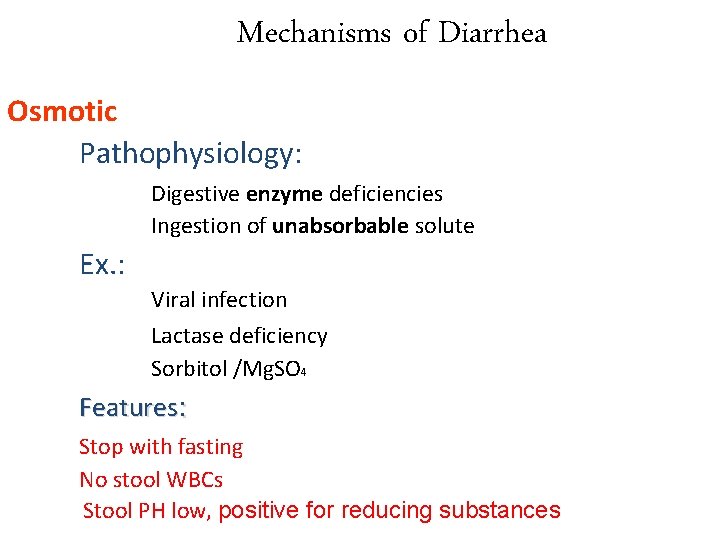
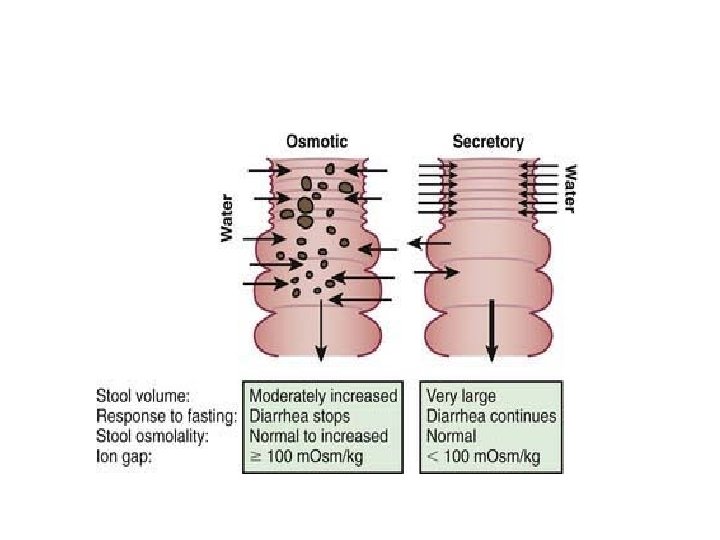
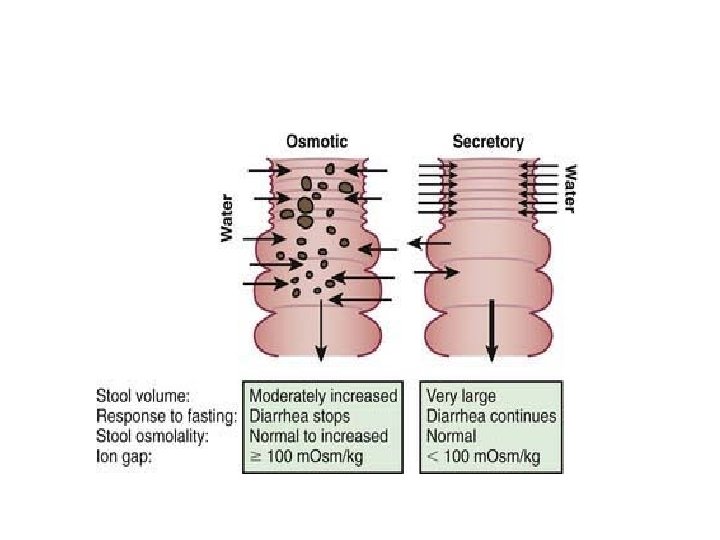
Mechanisms of Diarrhea Osmotic Pathophysiology: Digestive enzyme deficiencies Ingestion of unabsorbable solute Ex. : Viral infection Lactase deficiency Sorbitol /Mg. SO 4 Features: Stop with fasting No stool WBCs Stool PH low, positive for reducing substances
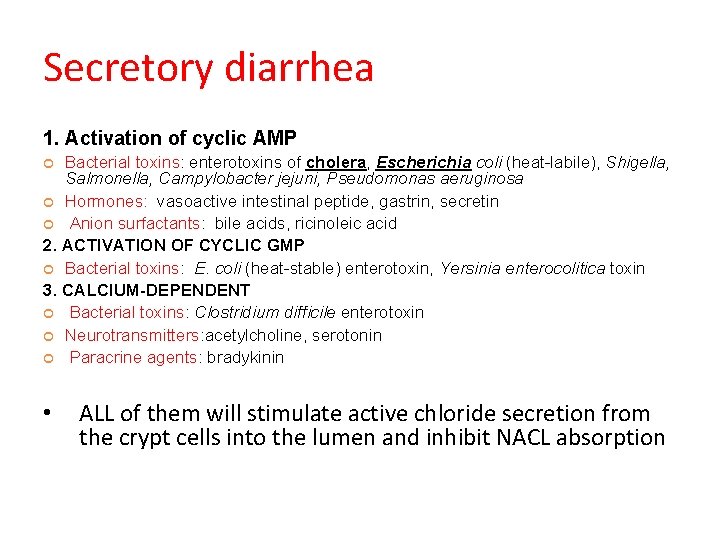
Secretory diarrhea 1. Activation of cyclic AMP Bacterial toxins: enterotoxins of cholera, Escherichia coli (heat-labile), Shigella, Salmonella, Campylobacter jejuni, Pseudomonas aeruginosa Hormones: vasoactive intestinal peptide, gastrin, secretin Anion surfactants: bile acids, ricinoleic acid 2. ACTIVATION OF CYCLIC GMP Bacterial toxins: E. coli (heat-stable) enterotoxin, Yersinia enterocolitica toxin 3. CALCIUM-DEPENDENT Bacterial toxins: Clostridium difficile enterotoxin Neurotransmitters: acetylcholine, serotonin Paracrine agents: bradykinin • ALL of them will stimulate active chloride secretion from the crypt cells into the lumen and inhibit NACL absorption
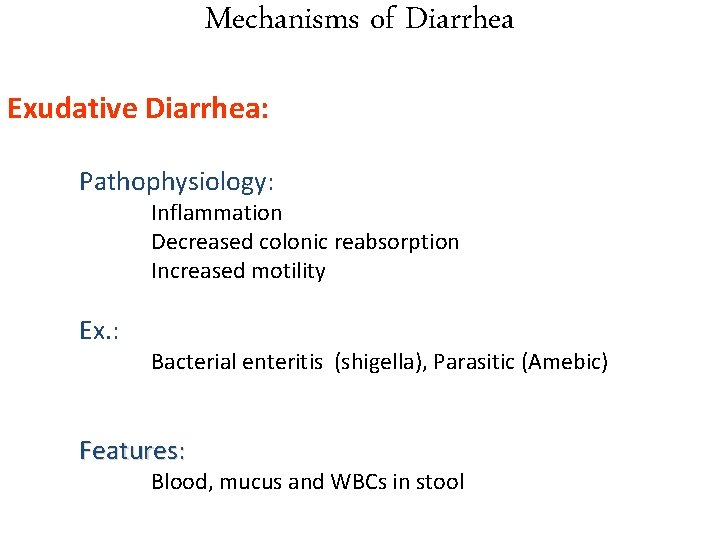
Mechanisms of Diarrhea Exudative Diarrhea: Pathophysiology: Inflammation Decreased colonic reabsorption Increased motility Ex. : Bacterial enteritis (shigella), Parasitic (Amebic) Features: Blood, mucus and WBCs in stool
Mechanisms of Diarrhea Reduction in anatomic surface area of absorption Short bowel syndrome celiac disease partial villous atrophy secondary to postgastroenteritis malabsorption syndrome, tropical sprue, microvillous inclusion disease
Causes • Viral • Bacterial • Parasitic
Viral • Rota • Norovirus • Other viral agents (astroviruses, adenoviruses, parvoviruses)
Rota • • Most common 4 serotypes (G 1, G 2, G 3, G 4) IP: 1 -3 d, duration: 4 -8 days Watery diarrhea, vomitting, fever Dx: Stool immunoassay Tx: supportive Prevention: Rota vaccine
Calicivirus • including norovirses and sapoviruses • Vomitting is more prominent in children, diarrhea in adult • Routine RT-PCR and EM on fresh unpreserved stool samples • Dx: Routine RT-PCR and EM on fresh unpreserved stool samples • Tx: supportive
Bacterial • • • Salmonella Shigella E. coli Campylobacter jejuni Others: Bacillus cerus, staph aureus, clostridium perferngis, Listeria, cholera, yersenia
Campylobacter jejuni • Most common bacterial • IP 2 -6 days • From mild watery diarrhea to bloody diarrhea, abdominal cramps, fever, • May mimic appenicitis • Duration: 2 -10 days • Dx: routine stool culture • Tx: supportive, in severe cases erythromycin • Complications: GBS
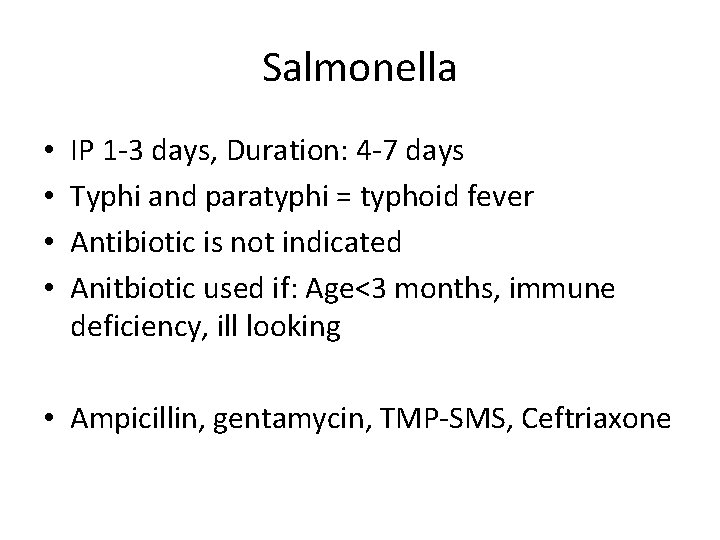
Salmonella • • IP 1 -3 days, Duration: 4 -7 days Typhi and paratyphi = typhoid fever Antibiotic is not indicated Anitbiotic used if: Age<3 months, immune deficiency, ill looking • Ampicillin, gentamycin, TMP-SMS, Ceftriaxone
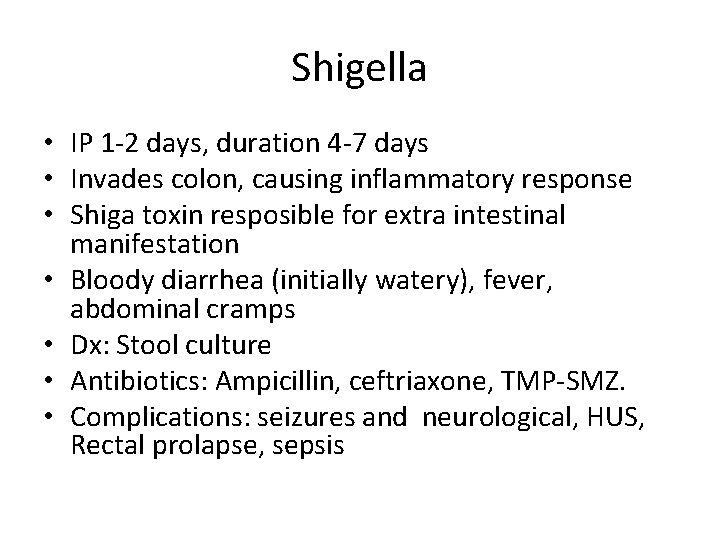
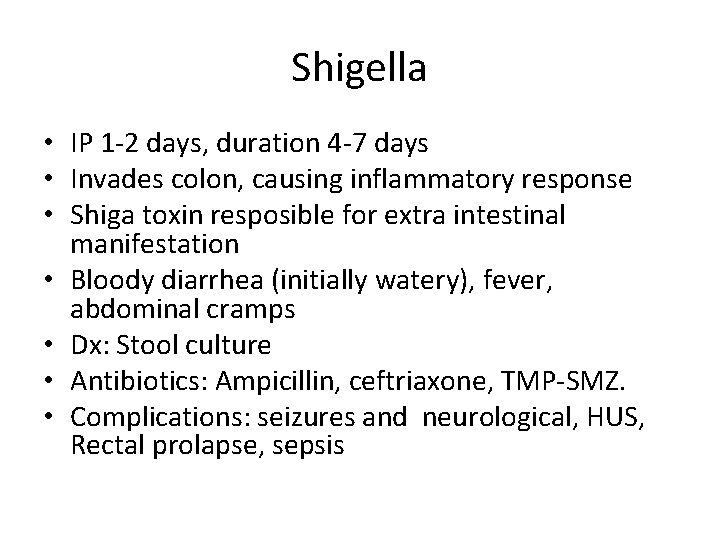
Shigella • IP 1 -2 days, duration 4 -7 days • Invades colon, causing inflammatory response • Shiga toxin resposible for extra intestinal manifestation • Bloody diarrhea (initially watery), fever, abdominal cramps • Dx: Stool culture • Antibiotics: Ampicillin, ceftriaxone, TMP-SMZ. • Complications: seizures and neurological, HUS, Rectal prolapse, sepsis
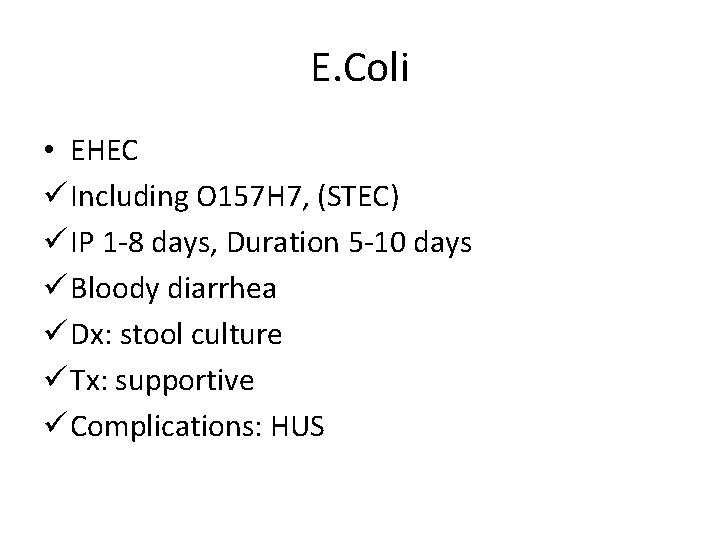
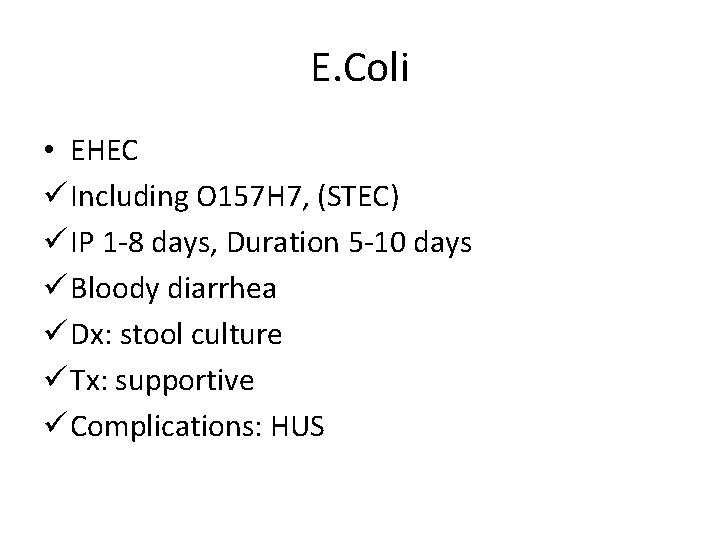
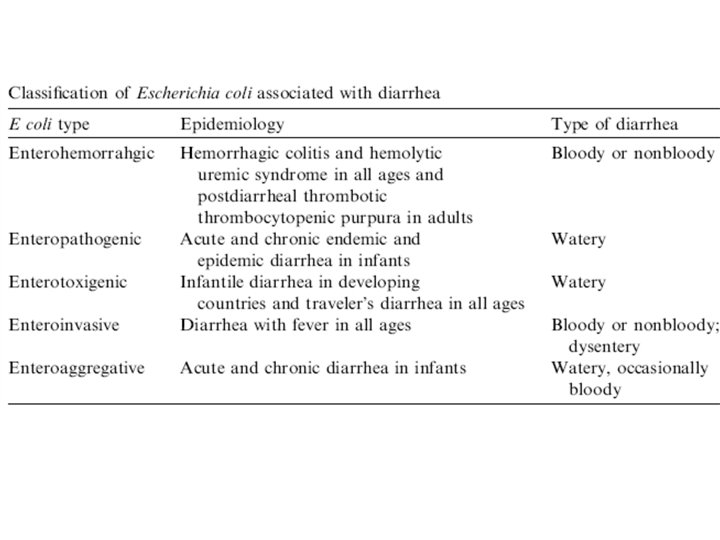
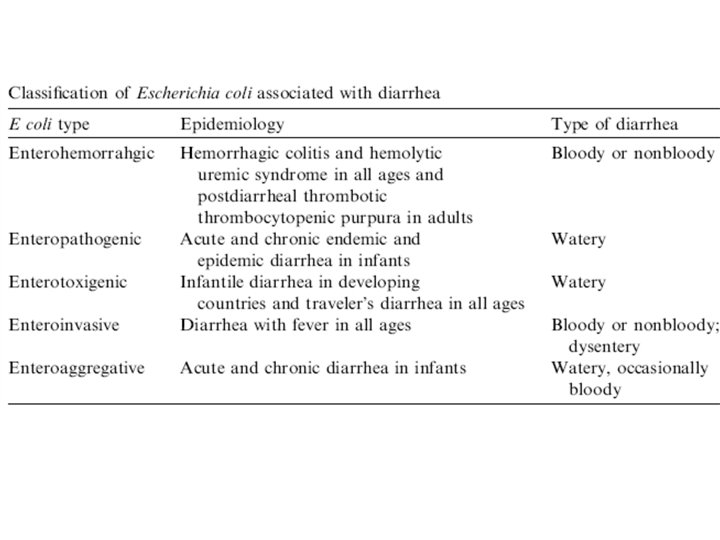
E. Coli • EHEC ü Including O 157 H 7, (STEC) ü IP 1 -8 days, Duration 5 -10 days ü Bloody diarrhea ü Dx: stool culture ü Tx: supportive ü Complications: HUS
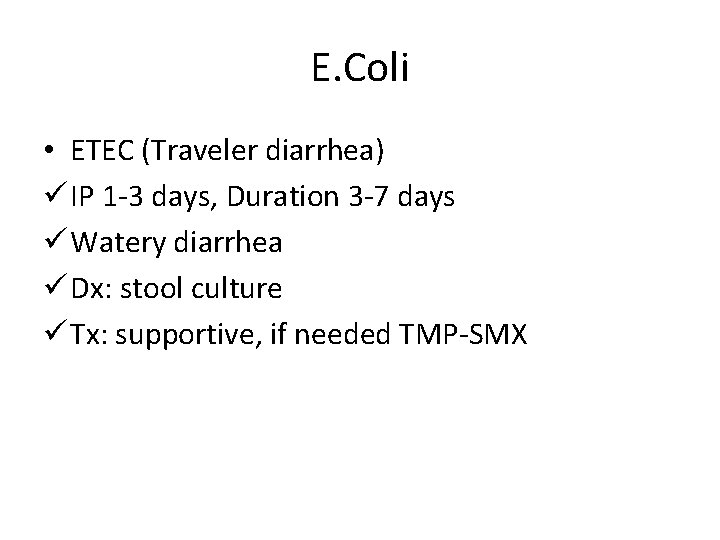
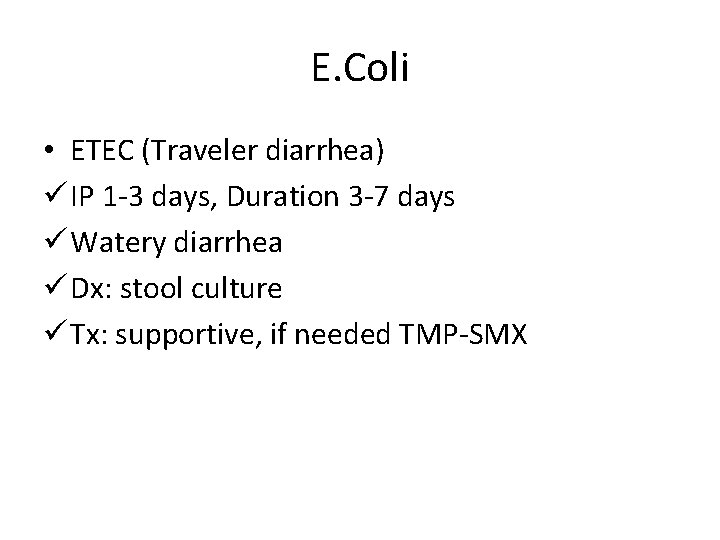
E. Coli • ETEC (Traveler diarrhea) ü IP 1 -3 days, Duration 3 -7 days ü Watery diarrhea ü Dx: stool culture ü Tx: supportive, if needed TMP-SMX
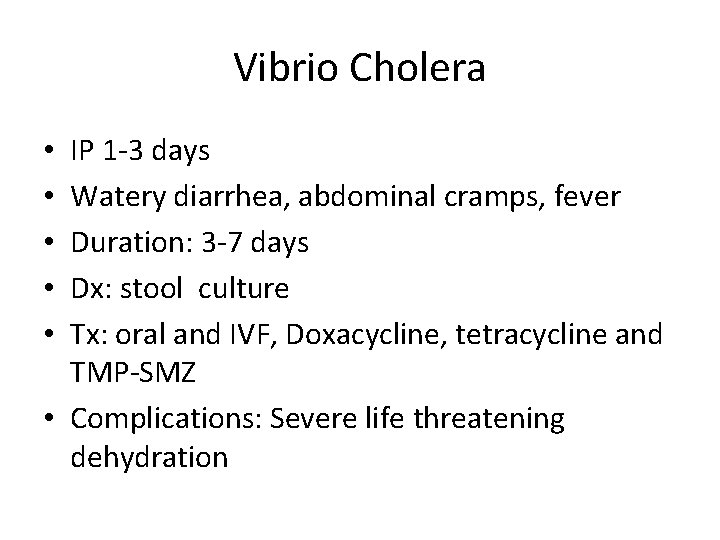
Vibrio Cholera IP 1 -3 days Watery diarrhea, abdominal cramps, fever Duration: 3 -7 days Dx: stool culture Tx: oral and IVF, Doxacycline, tetracycline and TMP-SMZ • Complications: Severe life threatening dehydration • • •
Parasitic • Entamoeba histolytica • Cryptosporidium • Giardia lamblia
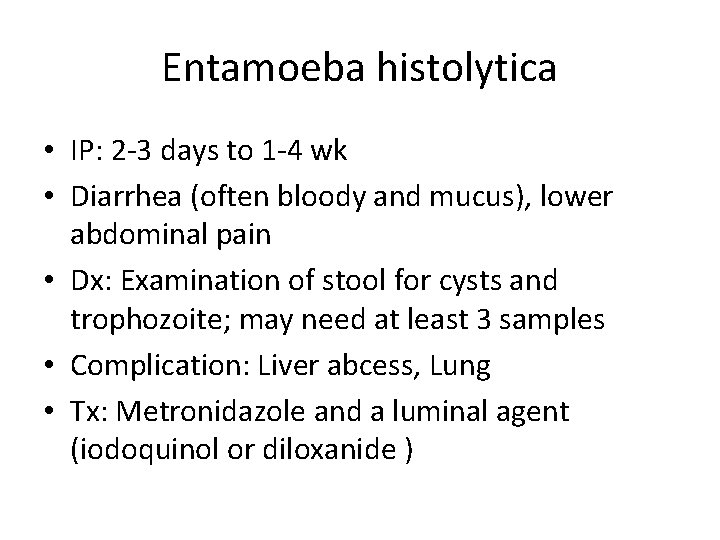
Entamoeba histolytica • IP: 2 -3 days to 1 -4 wk • Diarrhea (often bloody and mucus), lower abdominal pain • Dx: Examination of stool for cysts and trophozoite; may need at least 3 samples • Complication: Liver abcess, Lung • Tx: Metronidazole and a luminal agent (iodoquinol or diloxanide )
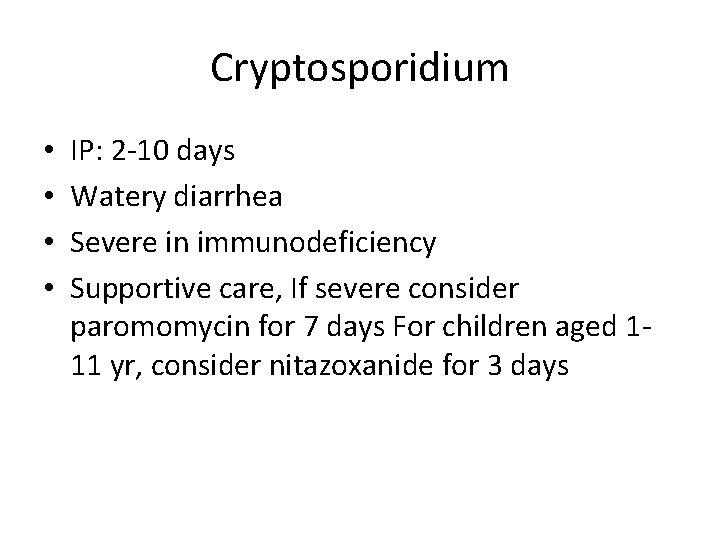
Cryptosporidium • • IP: 2 -10 days Watery diarrhea Severe in immunodeficiency Supportive care, If severe consider paromomycin for 7 days For children aged 111 yr, consider nitazoxanide for 3 days
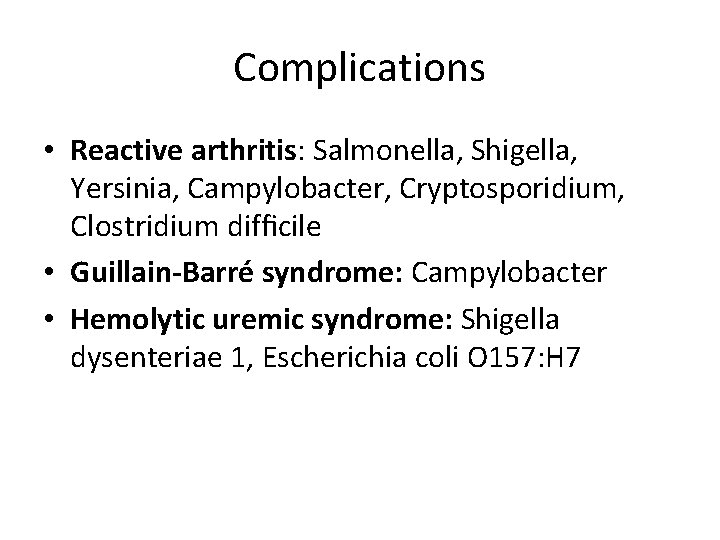
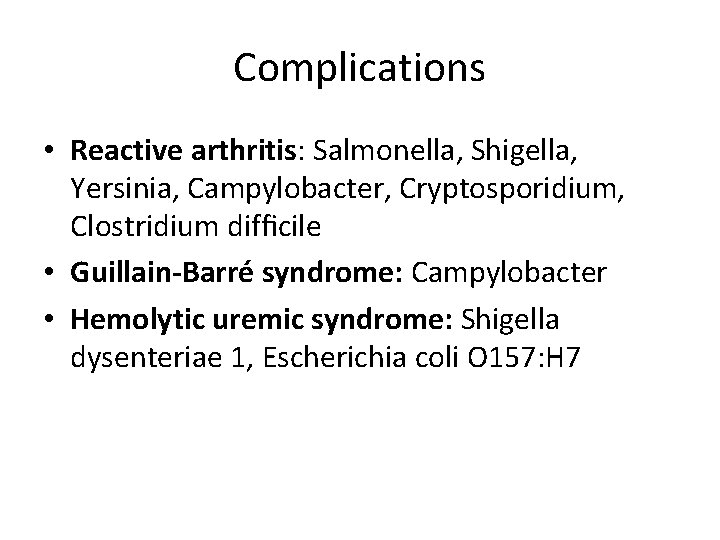
Complications • Reactive arthritis: Salmonella, Shigella, Yersinia, Campylobacter, Cryptosporidium, Clostridium difficile • Guillain-Barré syndrome: Campylobacter • Hemolytic uremic syndrome: Shigella dysenteriae 1, Escherichia coli O 157: H 7
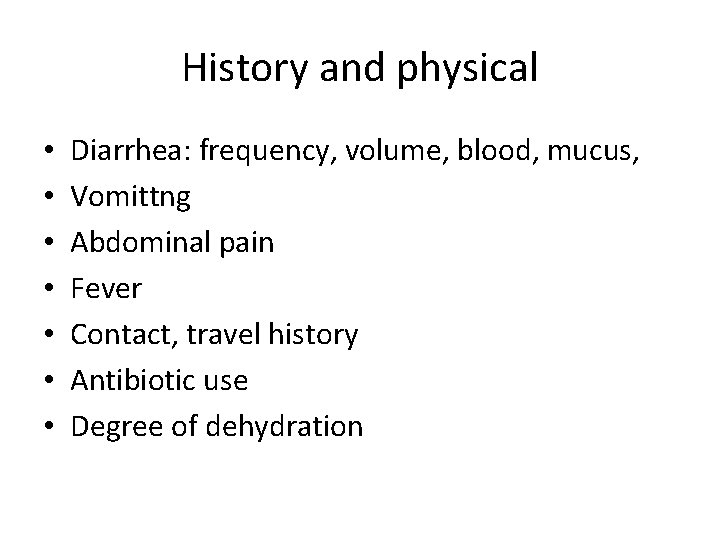
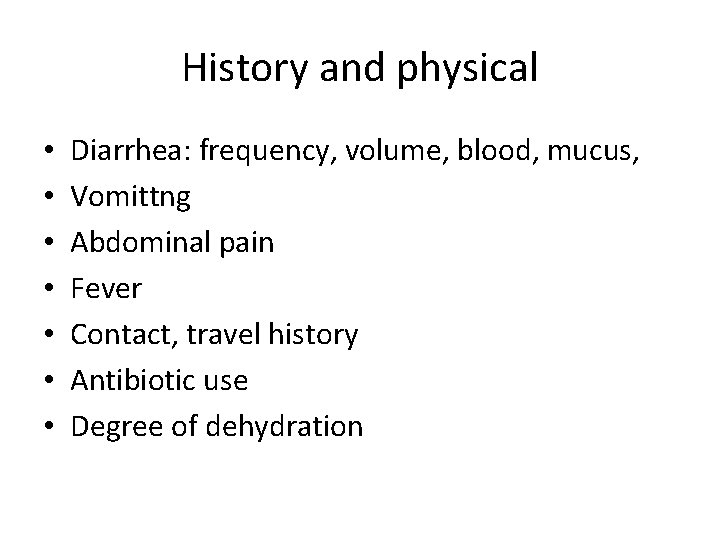
History and physical • • Diarrhea: frequency, volume, blood, mucus, Vomittng Abdominal pain Fever Contact, travel history Antibiotic use Degree of dehydration
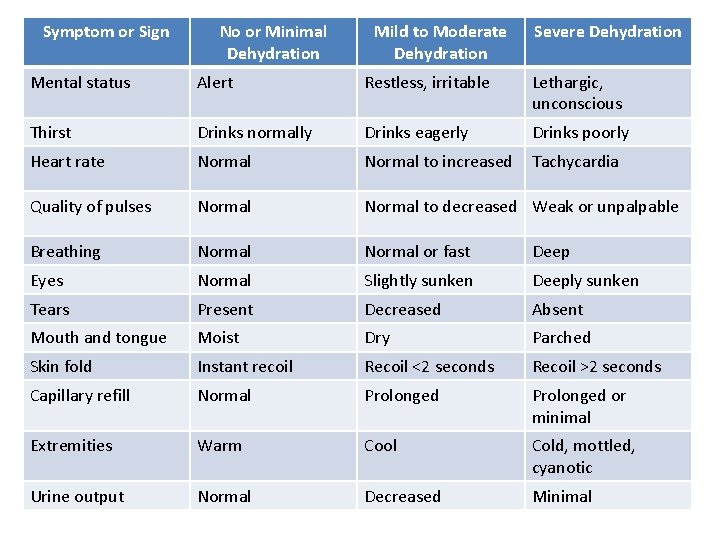
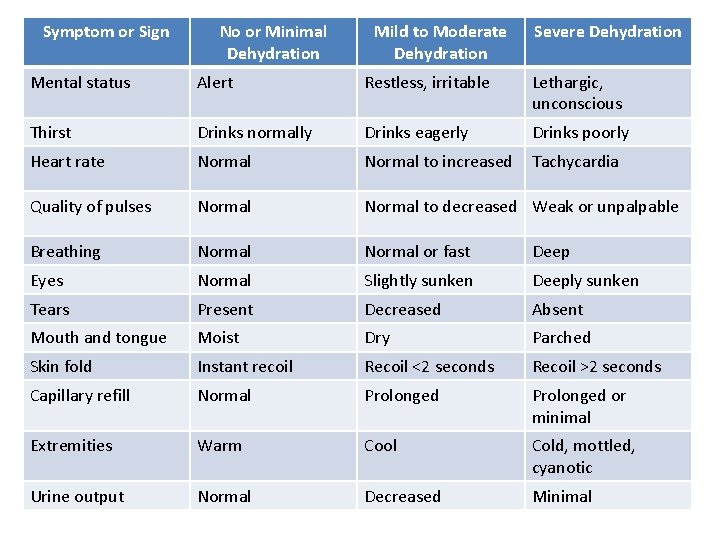
Symptom or Sign No or Minimal Dehydration Mild to Moderate Dehydration Severe Dehydration Mental status Alert Restless, irritable Lethargic, unconscious Thirst Drinks normally Drinks eagerly Drinks poorly Heart rate Normal to increased Tachycardia Quality of pulses Normal to decreased Weak or unpalpable Breathing Normal or fast Deep Eyes Normal Slightly sunken Deeply sunken Tears Present Decreased Absent Mouth and tongue Moist Dry Parched Skin fold Instant recoil Recoil <2 seconds Recoil >2 seconds Capillary refill Normal Prolonged or minimal Extremities Warm Cool Cold, mottled, cyanotic Urine output Normal Decreased Minimal
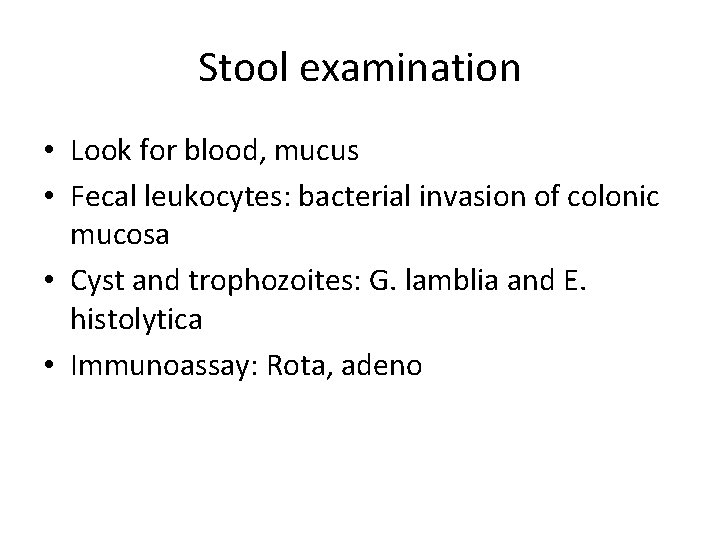
Stool examination • Look for blood, mucus • Fecal leukocytes: bacterial invasion of colonic mucosa • Cyst and trophozoites: G. lamblia and E. histolytica • Immunoassay: Rota, adeno
Stool culture • Bloody diarrhea • Stool microscopy indicates fecal leukocytes • Immunocompromised
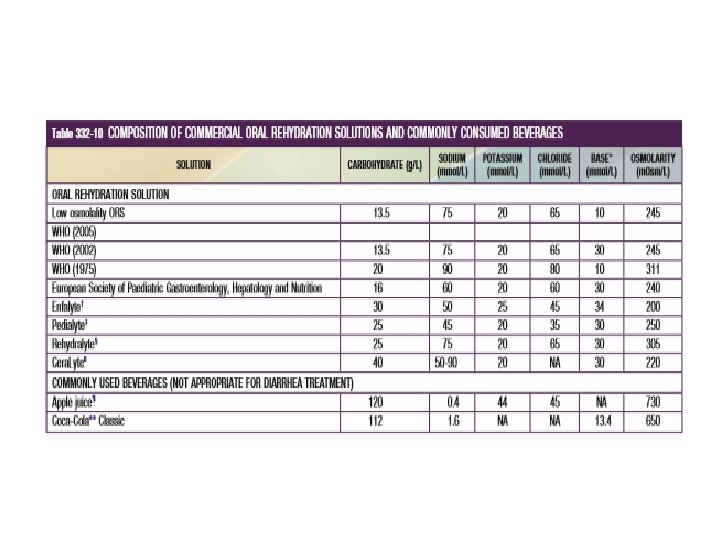
ORS • Concept: Na-glucose cotransporter CI: • Shock • Ileus, intussusception • Carbohydrate intolerance (rare) • Severe emesis • High stool output (>10 m. L/kg/hr)
• Minimal or no dehydration: 5 -10 ml/kg ORS for each diarrhea and vomitting • Mild to moderate: 50 -100 ml/kg over 4 hrs then continue as above • Severe dehydration: IVF
Don’t • Home remedies including soda, fruit juices, and tea are not suitable for rehydration or maintenance therapy because they have inappropriately high osmolalities and low sodium concentrations. • Don’t use antidiarrheal medication
Others • • • Continue feeding: age-appropriate diet Zinc supplements Probiotic Ondansetron Antibiotics