ACUTE GASTRO INTESTINAL BLEEDING Dr Pratyusha Alamuri FELLOW

ACUTE GASTRO INTESTINAL BLEEDING Dr. Pratyusha Alamuri FELLOW IN CRITICAL CARE AWARE GLOBAL HOSPITAL
Introduction • Acute GI bleeding is a common admission to the ICU • Also a major cause of morbidity & mortality
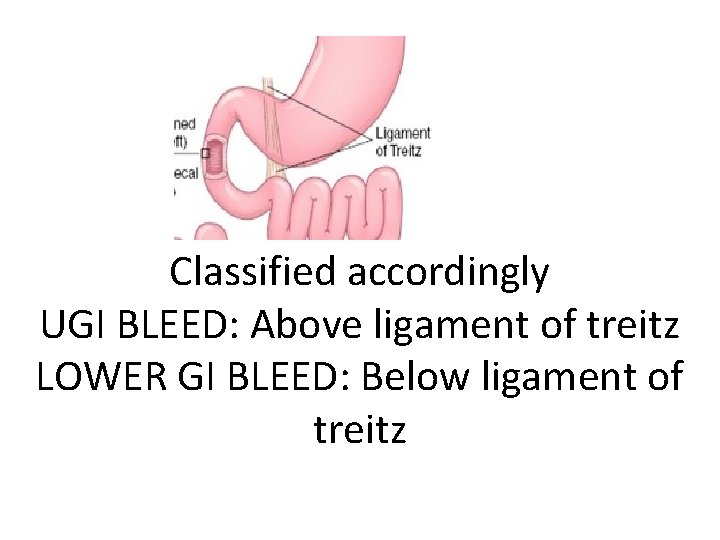
Classified accordingly UGI BLEED: Above ligament of treitz LOWER GI BLEED: Below ligament of treitz

Causes of UGI bleed • • 1. Peptic ulcers(DU: GU 3: 1) 2. Varices(EV: GV 9: 1) 3. Portal hypertensive gastropathy 4. Mallory weiss tears 5. Gastritis, duodenitis & esophagitis 6. Hemobilia: Bleed from biliary tree 7. Hemosuccus pancreaticus: Bleed from PD Dieulafoy lesion

• PUD-accounts for 75% of UGI bleeding • Bleeding from varices, esophagitis, duodenitis, mallory weiss tear-Each account for between 5% & 15%
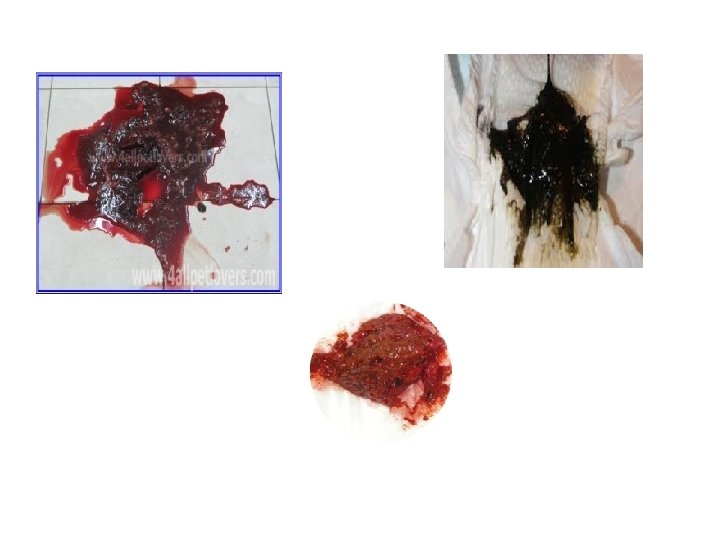
CLINICAL PRESENTATION Hematemesis & melena are the most common presentations of acute UGI bleed Hematochezia: Passage of bright red to maroon blood from the rectum-usually represents a lower GI bleed. Also can be feature of massive upper GI bleed Vomiting & retching preceding hematemesis suggests mallory weiss tears
Other symptoms include: 1. Pain epigastrium or diffuse abdominal pain 2. Burning type of epigastric pain 3. Heart burn, retching 4. Giddiness
Signs include: • Pallor • Icterus-in case of CLD Signs of hypovolemic shock: Hypotension, tachycardia, cold extremities Mental confusion, oliguria
HIGH RISK PATIENT Hematemesis Syncope SBP <100 mm. Hg Postural hypotension Blood transfusion requirement of more than 4 units of blood in 12 hours to maintain blood pressure • Age over 60 years • Multiple comorbidities • • •

MANAGEMENT OF NON VARICEAL BLEEDING 1. Initial resuscitation is important Blood & plasma expanders should be given through large bore IV cannulae Vital signs should be closely monitored Observe central venous pressure & hourly urine out put in case of hypovolemic shock Consider endoscopy after resuscitation
UGI ENDOSCOPY • Allows identification of the site, nature of bleeding & appropriate treatment • Source of bleeding like ulcers, varices, mallory weiss tears & other lesions with bleeding are identified • Peptic ulcers that are actively bleeding or have bleed recently may show stigmata of hemorrhage on endoscopy

Stigmata of hemorrhage HIGH RISK ULCERS 1. Spurter or oozer: % recurrent bleeding 85 -90% 2. Protuberant vessel % recurrent bleeding 35 -55% 3. Adherent clot % recurrent bleeding 30 -40% 4. Flat spot % recurrent bleeding 5 -10% 5. None % recurrent bleeding 5%
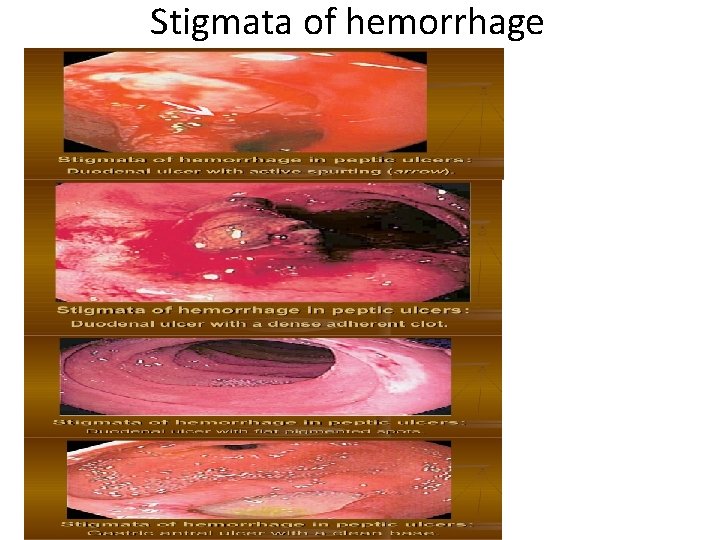
Stigmata of hemorrhage
HIGH RISK ULCERS • Proximal postero-inferior wall of duodenal bulb-(Gastro duodenal artery) • High lesser curvature of the stomach-(Left gastric artery) These are the sites for severe recurrent bleeding
TREATMENT • Patients at high risk of recurrent bleeding pharmacological control without endoscopic haemostasis is inadequate thus combination offers best therapy for ulcer bleeding • Pharmacological+Endoscopic therapy is best

ENDOSCOPIC THERAPY • Endoscopic haemostasis should be used in patients with a high risk of persistent or recurrent bleeding 1. Epinephrine(adrenaline)injection-1: 10, 000 dilution 2. Coaptive coagulation: Uses direct pressure & heat energy(heater probe)—limits view of lesser curve & posterior wall of duodenal bulb 3. Hemoclips: Clipping of bleeding vessel Lesser curve, gastric fundus & posterior wall of duodenum technically difficult
PHARMACOLOGICAL CONTROL • High dose, constant infusion of IV PPI will sustain intragastric p. H >6 & enhance clot stability(80 mg IV bolus & 8 mg/hour infusion) Example: IV Pantoprazole as mentioned To prevent acidic environment Given after endoscopic therapy
SURGERY • Indications: 1. Arterial bleeding that cant be controlled by endoscopic haemostasis 2. Massive transfusion(ie total of 6 -8 units of blood required to maintain BP 3. Recurrent clinical bleeding after initial success in endoscopic haemostasis 4. Evidence suggestive of GI perforation *Surgical procedures include various types of gastrectomy How ever morbidity is significantly high in surgical patients
Variceal Bleeding • Serious complication of portal HTN with a high mortality • Child pugh’s classification is most important prognostic factor for early rebleeding & survival
Treatment-Variceal bleeding • Initial resuscitation is again important Fresh frozen plasma & platelet transfusion may be indicated Lactulose via ryles tube(15 -30 ml every 4 -6 hours should be given)to prevent or correct hepatic encephalopathy Prevent overt transfusions-may increase portal pressure rebleed Close hemodynamic monitoring is required
PHARMACOLOGICAL CONTROL OF VARICEAL BLEEDING • Infusion of octreotide(somatostatin analogue) reduces portal blood pressure— 50 mcg bolus followed by 50 mcg/hour for 2 -5 days safe & effective vasoactive agents used in acute varcieal bleeding Effective when used in combination with endoscopic therapy Terlipressin(vasopressin analouge) also used in variceal bleed. Given at a dose of 2 mg IV every four hours during the first 48 hours reducing to 1 mg every 4 hours for another 3 days. Also improves renal perfusion in HRS. But limited in ischemic heart disease.
ENDOSCOPIC VARICEAL THERAPY 1. Endoscopic sclerotherapy: sclerosants used(ethanolamine oleate, sodium tetradecyl sulphate 1 -3%, polidocanol Mainstay of treatment-controls 80 -90% of acute variceal bleeding Complications: ulcer formation, fever, chest pain, mediastinitis 2. Endoscopic variceal ligation: Mechanical methodstrangulate varices Less complications-coz no chemical irritation More preferred in many centers
BALLOON TAMPONADE-VARICEAL BLEEDING • Balloon tamponade: Exert pressure directly on the bleeding point • Sengstaken blackmore tube has been replaced by the four lumen minnesota tube which allows aspiration of gastric & esophageal contents • Limited to 24 hours to avoid tissue pressure necrosis • Used in exceptional cases when therapies fail to control bleeding
TIPS-In variceal bleed • Transjugular Intrahepatic Portosystemic Shunt In good hands success can be achieved in over 90% of cases Strongly considered in child’s pugh class C with 10 -13 score with in 1 -2 days of hospitalization Complications: Intra-abdominal hemorrahage & stent occlusion
SURGERY-In variceal bleed • Include direct devascularization of the lower esophagus plus the proximal stomach & a variety of surgical shunts • But role of surgery has diminished since the advent of endoscopic therapy & TIPS • Is now 2 nd line treatment when bleeding continues or recurs after two sessions of sclerotherapy or EVL

EV & EVL
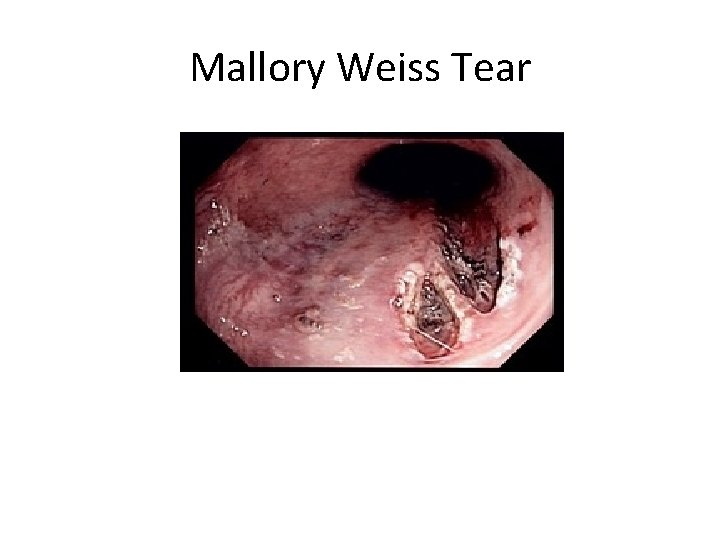
Mallory Weiss Tear
Mallory weiss tear VS Boerhaaves Mallory weiss tear: Linear mucosal tears at gastroesophageal junction Boerhaaves syndrome: Complete transmural(full thickness) laceration or perforation of esophagus at GE junction
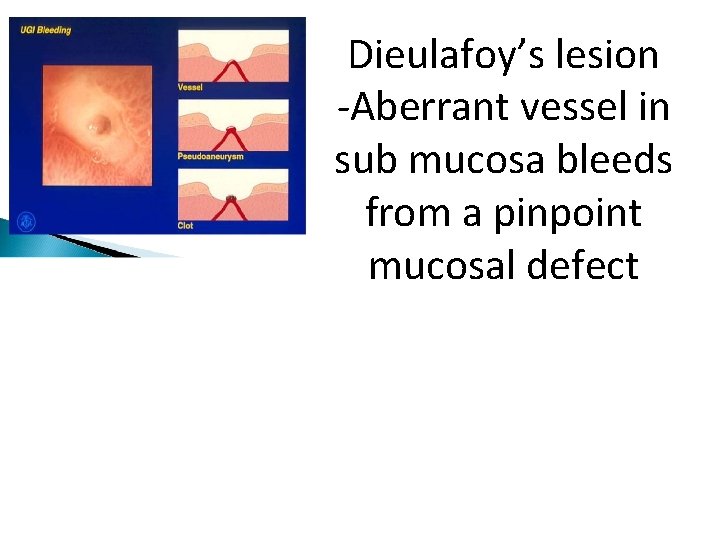
Dieulafoy’s lesion -Aberrant vessel in sub mucosa bleeds from a pinpoint mucosal defect

UGI Bleed management algorithm
LOWER GI BLEEDING • About 20% of GI bleeding arises from the lower GI tract • Bleeding source distal to ligament of treitz
Causes of LGI bleed • Diverticular hemorrhage • Angiodysplasia Both occur on right colon • Colonic polyps • Carcinoma • IBD
CLINICAL PRESENTATION • Hematochezia-most common presentation of lower GI bleed • Small intestinal bleed & right colon bleed present as melena • Abdominal pain preceding a massive bleeding episode suggests ischemia or IBD • Diverticulosis, angiodysplasia, mekels diverticulumpresents painless bleeding • PTN hemorrhoids present with massive hematochezia
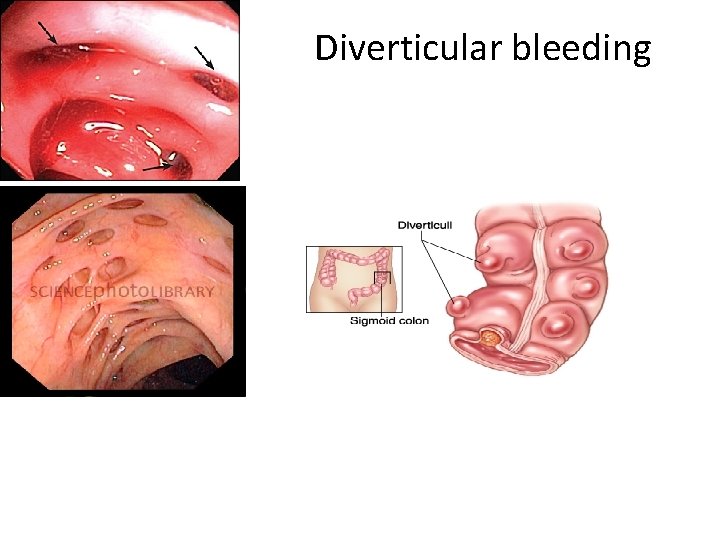
Diverticular bleeding

Colonic Angiodysplasia
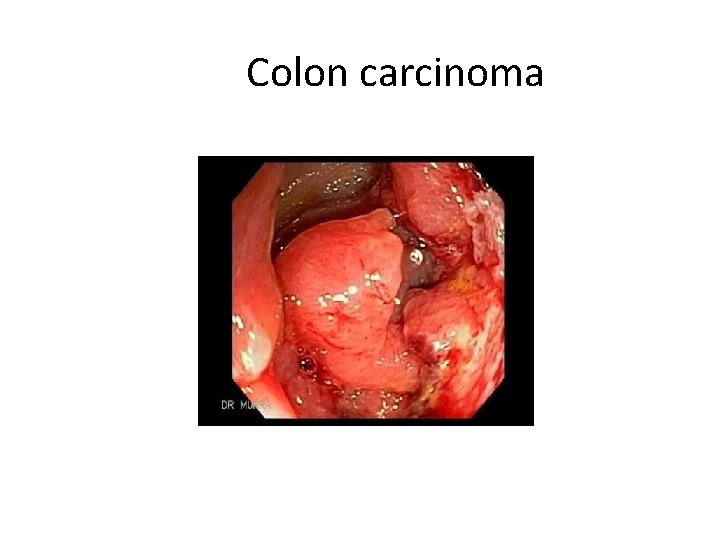
Colon carcinoma
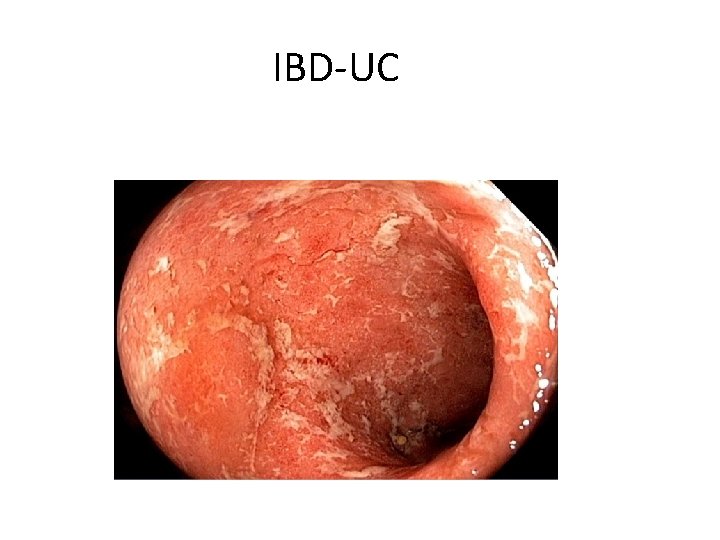
IBD-UC
INVESTIGATIONS • Plan after initial resuscitation/hemodynamic stability • Always exclude UGI bleed before colonoscopy • Proctosigmoidoscopy-helps to identify hemorrhoids & rectal tumors • If proctosigmoidoscopy & gastro-duodenoscopy are negative than lower GI tract should be examined by colonoscopy, angiography or radionucleotide scan
COLONOSCOPY • Difficult in actively bleeding patient • Risk of perforation high • Poor visualization due to blood • Bowel preparation yields better results once bleeding has stopped
Angiography or radionuclide scan • Diagnostic angiography: Helpful when colonoscopic view is completely obscured by active hemorrhage Helpful in defining abnormal vasculature(angiodysplasia, arteriovenous malformations & inherited vascular anomalies like rendu-osler-weber syndrome, pseudoxanthoma elasticum & Ehlers danlos syndrome) Angiography localize the site of bleeding in 80 -85% of patients when bleeding rate is more than 0. 5 ml/min *99 m technetium labelling of RBCs has been reported to detect the source of active bleeding More sensitive than angiography detects bleeding as low as 0. 1 ml/min
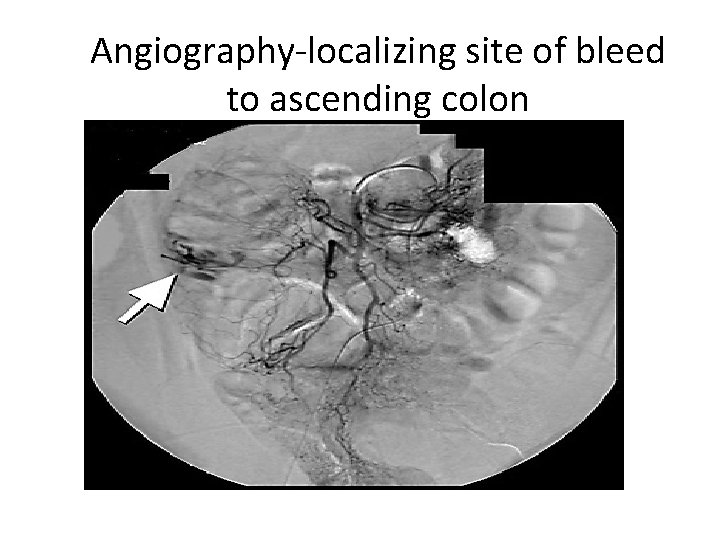
Angiography-localizing site of bleed to ascending colon

99 m technetium labeled red blood cell scan localizing the source of bleed in proximal sigmoid colon
Management/Treatment • Colonoscopic : Bleeding from vascular anamolies can be treated by electrocoagulation, heater probe & laser photocoagulation unless the anamolies are too large or diffuse • Angiographic: Intra-arterial infusion of vasopressin or occlusion of the bleeding artery with embolic agents such as absorbable gelatin sponge used in lower GI bleed • Surgical: Diverticular bleeding usually arises from larger vessel may be difficult to control with colonoscopic or angiographic therapy-require surgery • Surgery also indicated in vascular anamolies when endoscopic treatment fails • Surgeries done are immediate laparotomy to perform colectomy(segmental)

Algorithm for lower GI bleed management

THANK YOU
- Slides: 46