ACUTE COLITIS PATTERN Acute colitis An injury pattern








- Slides: 47

ACUTE COLITIS PATTERN
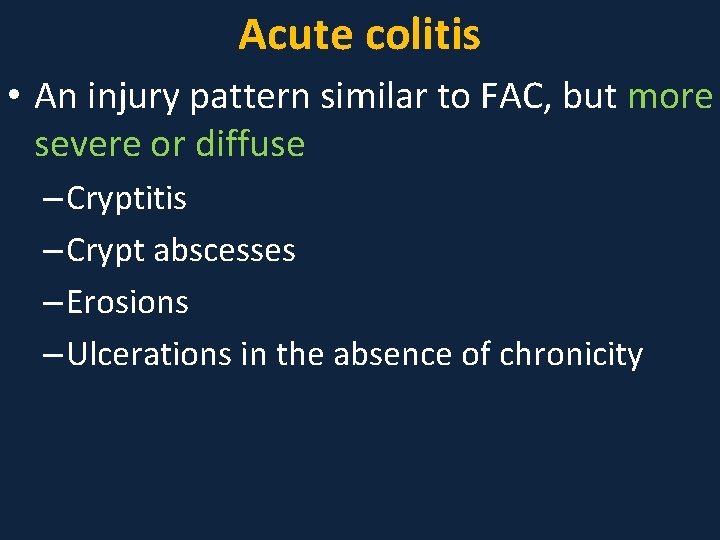
Acute colitis • An injury pattern similar to FAC, but more severe or diffuse – Cryptitis – Crypt abscesses – Erosions – Ulcerations in the absence of chronicity
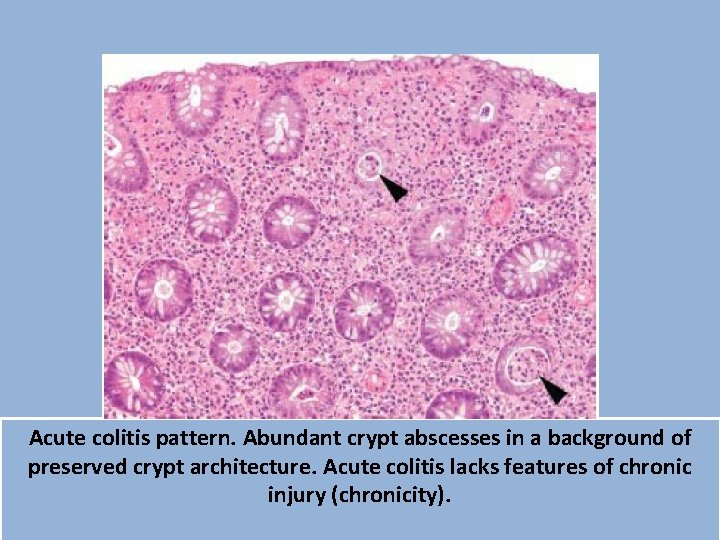
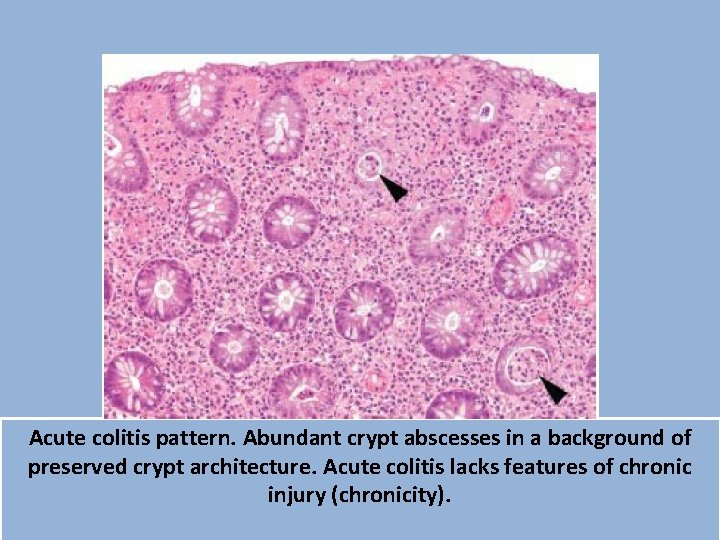
Acute colitis pattern. Abundant crypt abscesses in a background of preserved crypt architecture. Acute colitis lacks features of chronic injury (chronicity).
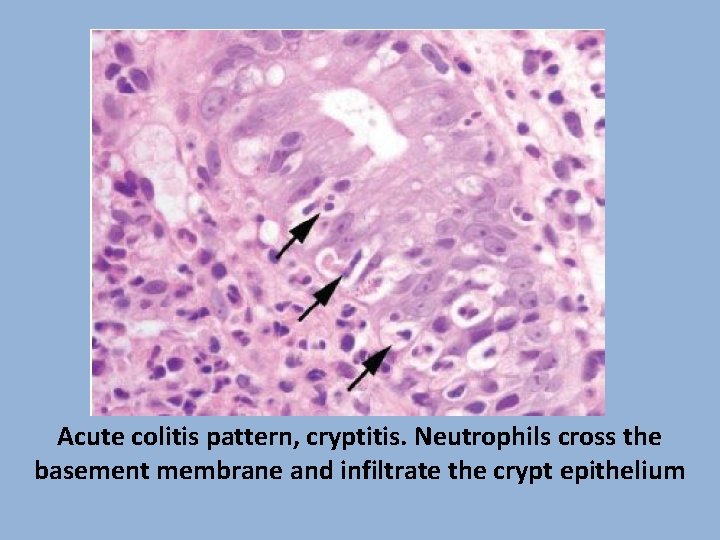
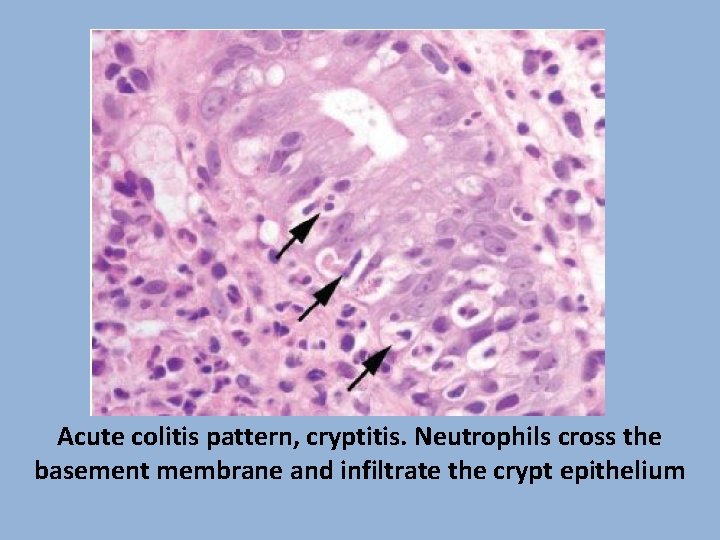
Acute colitis pattern, cryptitis. Neutrophils cross the basement membrane and infiltrate the crypt epithelium
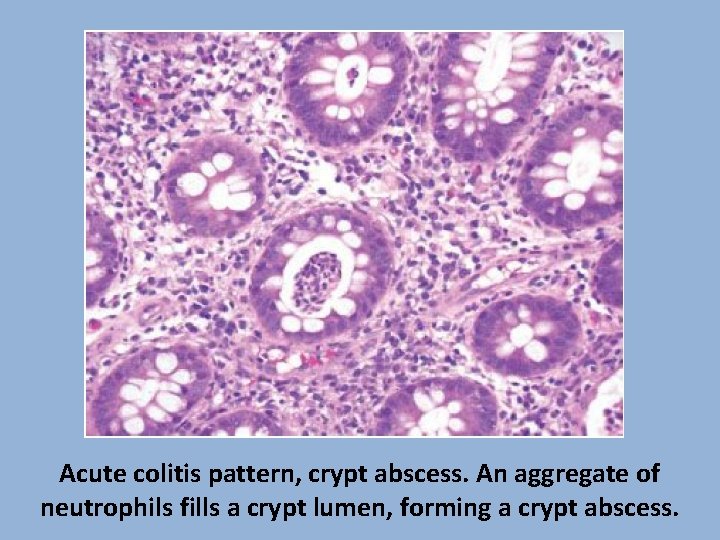
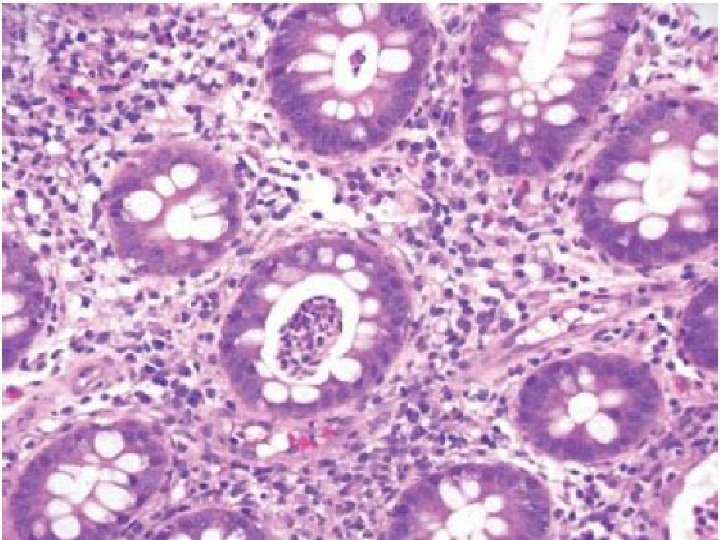
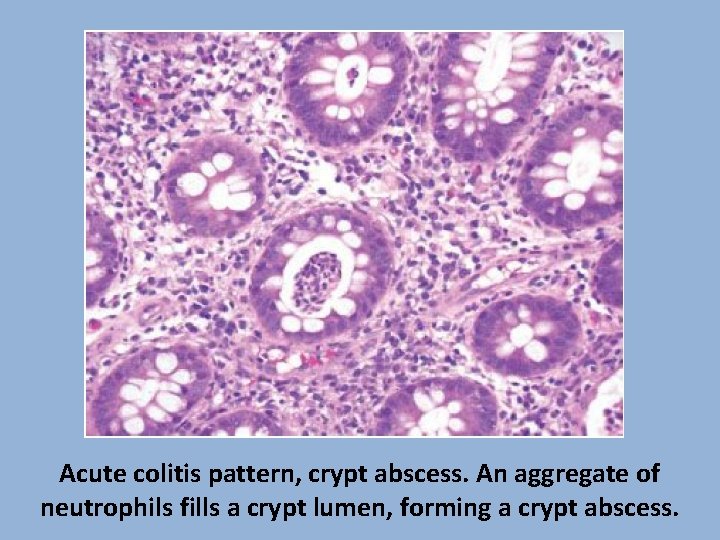
Acute colitis pattern, crypt abscess. An aggregate of neutrophils fills a crypt lumen, forming a crypt abscess.
Acute colitis • This pattern of injury is entirely nonspecific • Is most commonly caused by – Acute viral and bacterial infections – Medications (NSAIDs, Kayexalate, sevelamer, ipilimumab) – Emerging or partially treated IBD • Although ancillary findings of lamina propria hemorrhage or fibrin deposition may be seen in acute colitis pattern, the distinctive findings of microcrypts or pseudomembranes raise a unique set of differential diagnoses
Etiologic Considerations for the Acute Colitis Pattern • Infection – CMV – Salmonella – Shigella – Campylobacter • Medication – NSAIDs – Kayexalate – Sevelamer – Ipilimumab • IBD – Emerging – Partially treated
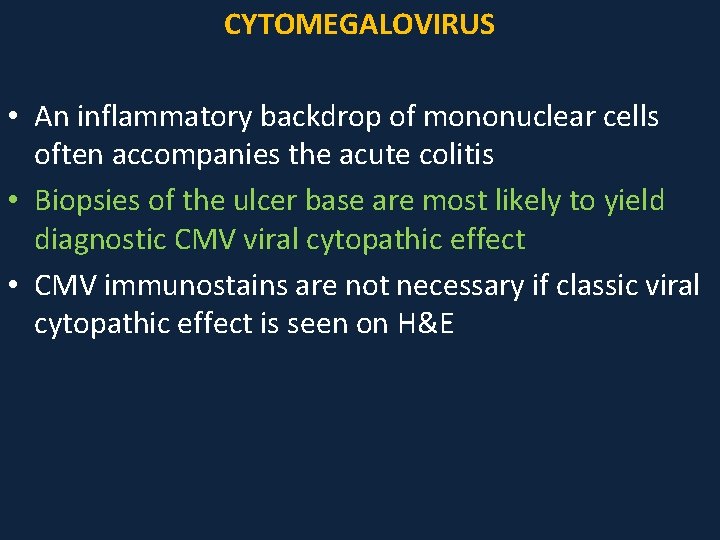
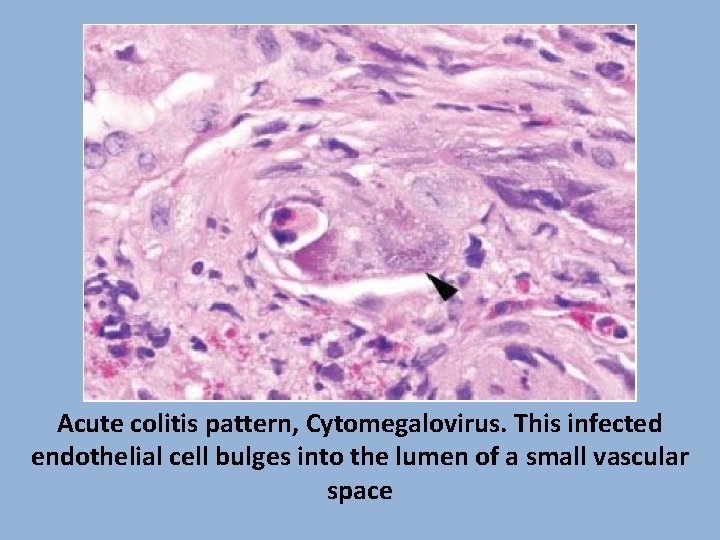
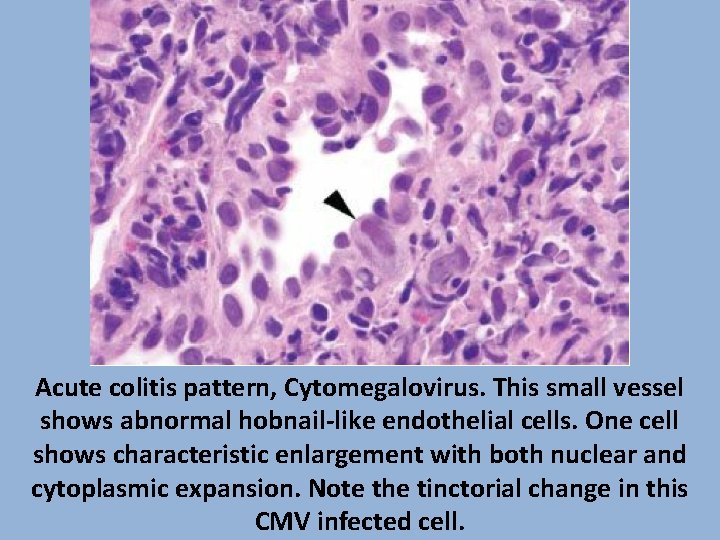
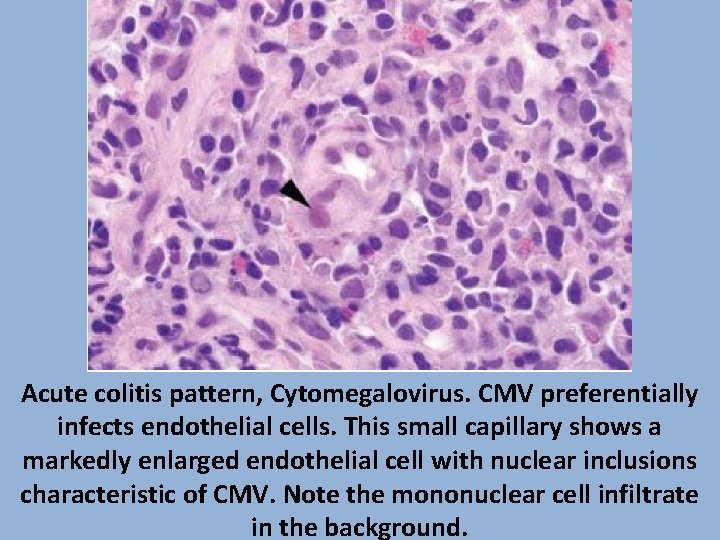
CYTOMEGALOVIRUS • >immunocompromised patients, transplant patients, elderly • Endothelial cells, macrophages, and stromal cells are preferentially affected by CMV, although epithelial involvement is common • Viral cytopathic effect – Cytomegaly (cell enlargement) – Nuclear (“owl’s eye”) and cytoplasmic inclusion bodies that have a distinctive magenta tinctorial quality
CYTOMEGALOVIRUS • An inflammatory backdrop of mononuclear cells often accompanies the acute colitis • Biopsies of the ulcer base are most likely to yield diagnostic CMV viral cytopathic effect • CMV immunostains are not necessary if classic viral cytopathic effect is seen on H&E
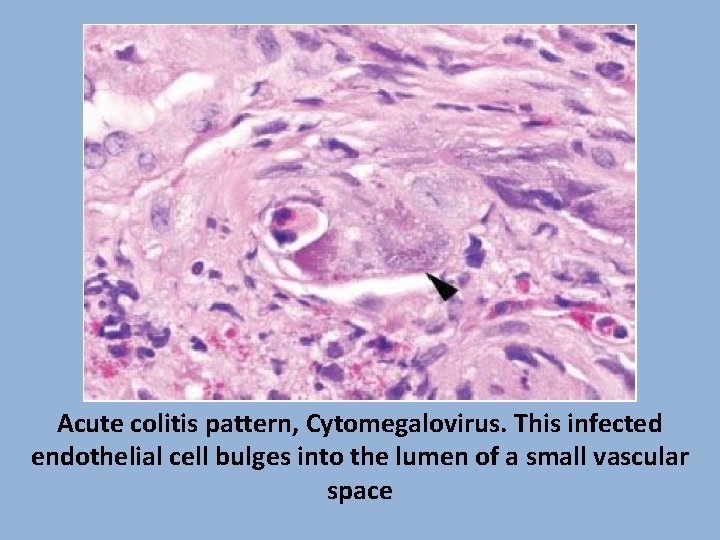
Acute colitis pattern, Cytomegalovirus. This infected endothelial cell bulges into the lumen of a small vascular space
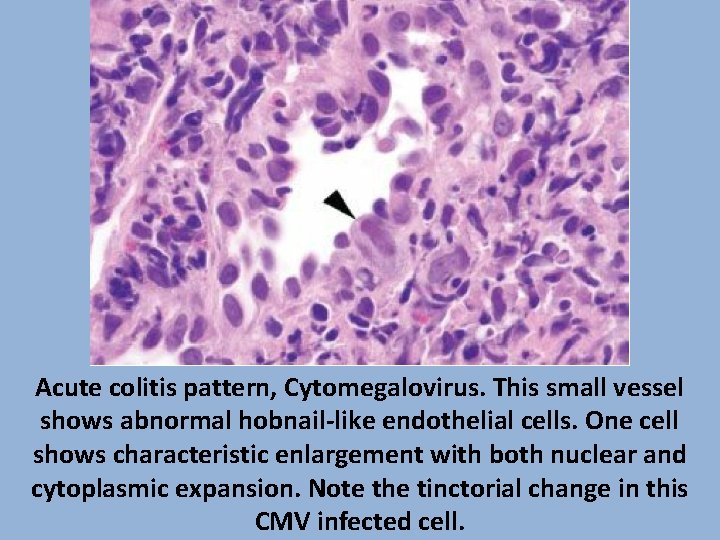
Acute colitis pattern, Cytomegalovirus. This small vessel shows abnormal hobnail-like endothelial cells. One cell shows characteristic enlargement with both nuclear and cytoplasmic expansion. Note the tinctorial change in this CMV infected cell.
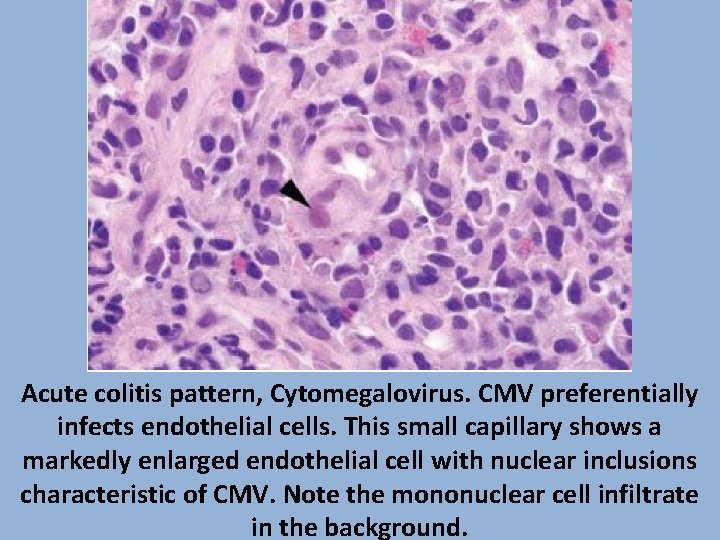
Acute colitis pattern, Cytomegalovirus. CMV preferentially infects endothelial cells. This small capillary shows a markedly enlarged endothelial cell with nuclear inclusions characteristic of CMV. Note the mononuclear cell infiltrate in the background.
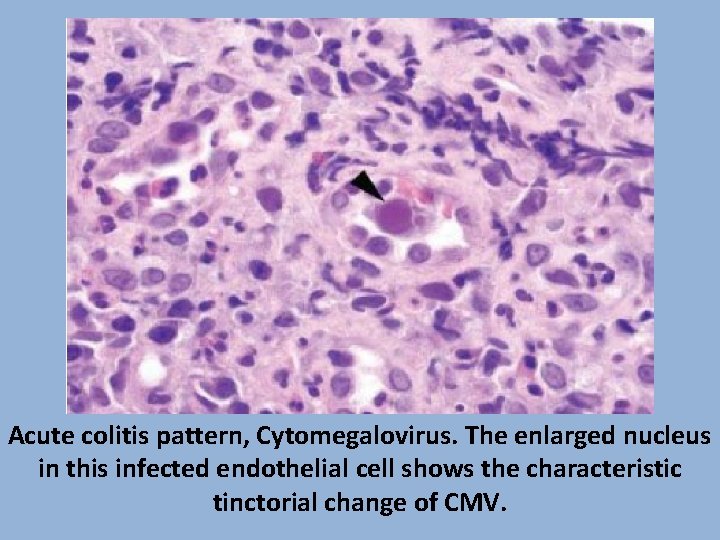
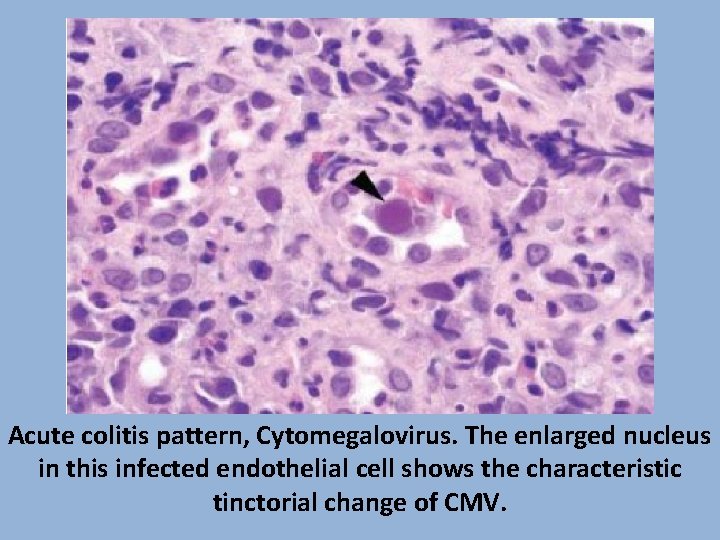
Acute colitis pattern, Cytomegalovirus. The enlarged nucleus in this infected endothelial cell shows the characteristic tinctorial change of CMV.
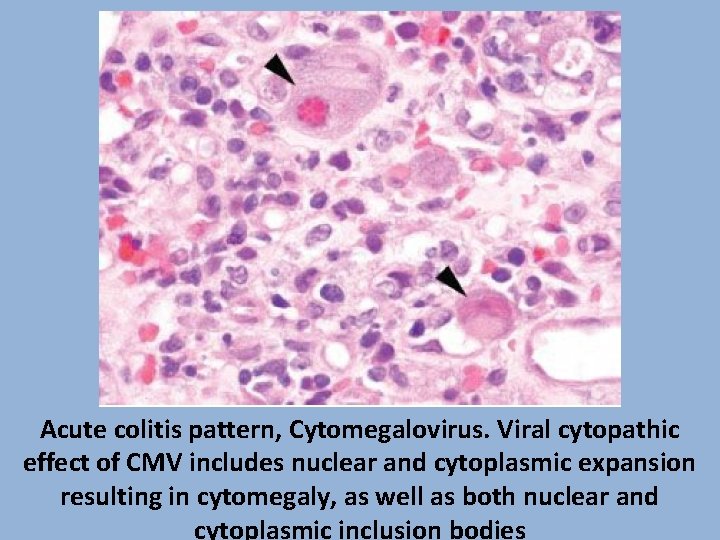
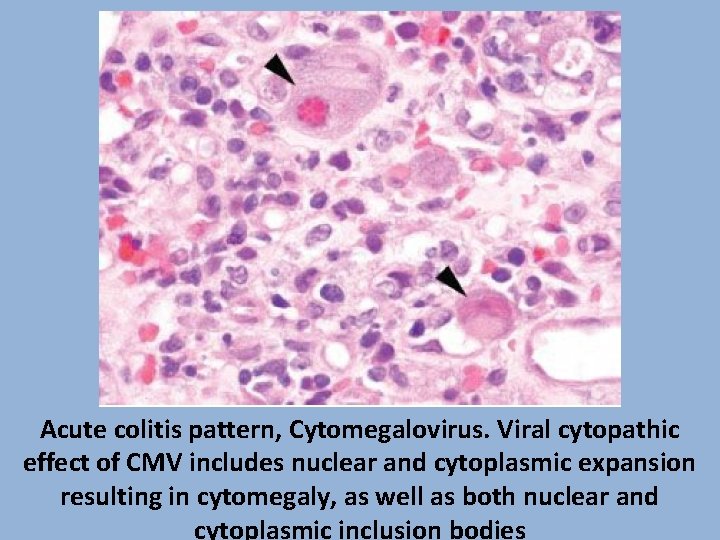
Acute colitis pattern, Cytomegalovirus. Viral cytopathic effect of CMV includes nuclear and cytoplasmic expansion resulting in cytomegaly, as well as both nuclear and cytoplasmic inclusion bodies
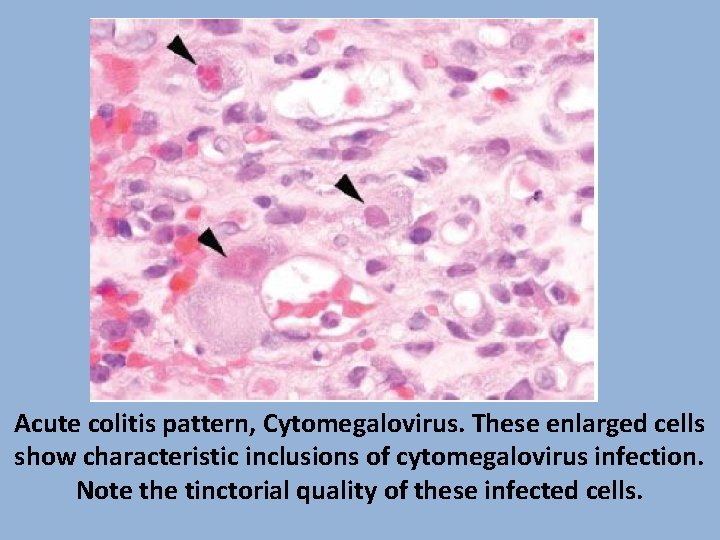
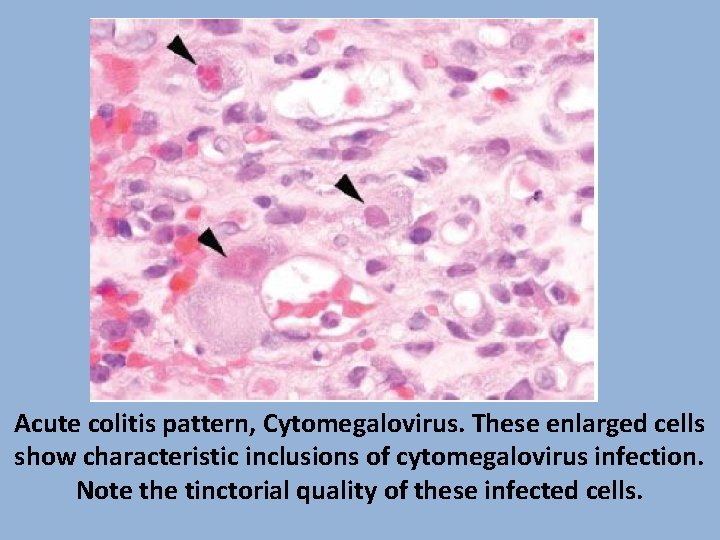
Acute colitis pattern, Cytomegalovirus. These enlarged cells show characteristic inclusions of cytomegalovirus infection. Note the tinctorial quality of these infected cells.
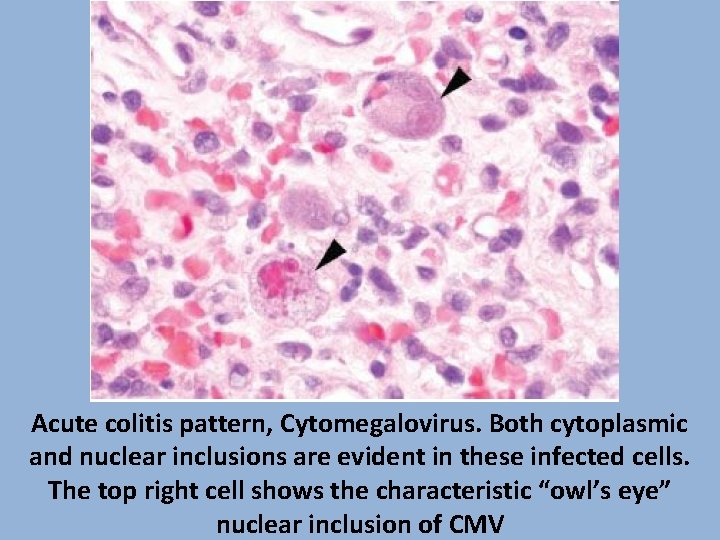
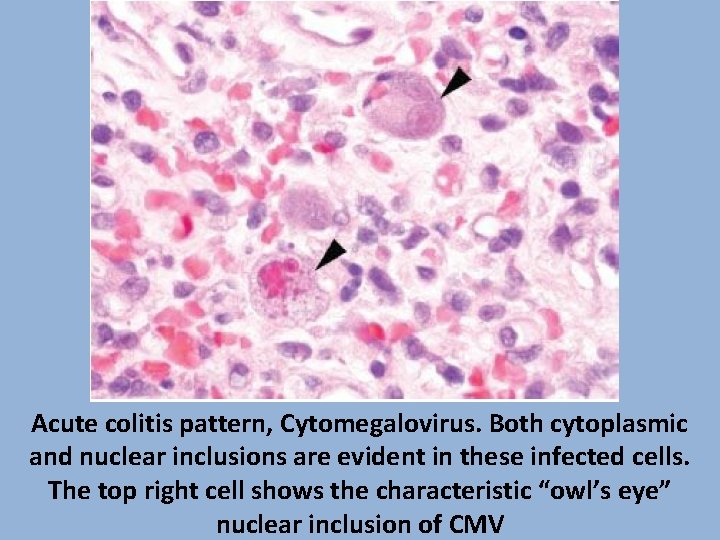
Acute colitis pattern, Cytomegalovirus. Both cytoplasmic and nuclear inclusions are evident in these infected cells. The top right cell shows the characteristic “owl’s eye” nuclear inclusion of CMV
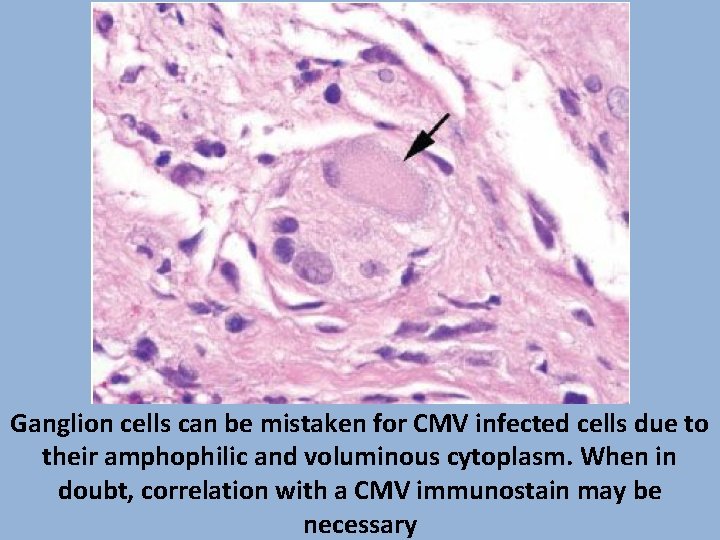
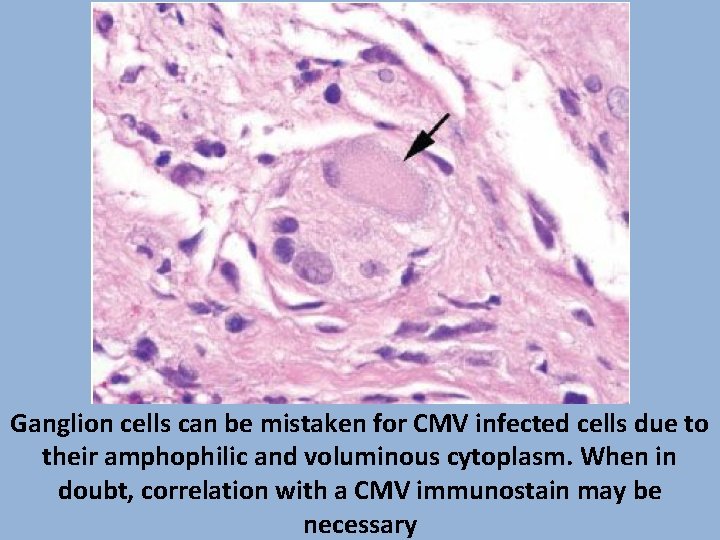
Ganglion cells can be mistaken for CMV infected cells due to their amphophilic and voluminous cytoplasm. When in doubt, correlation with a CMV immunostain may be necessary
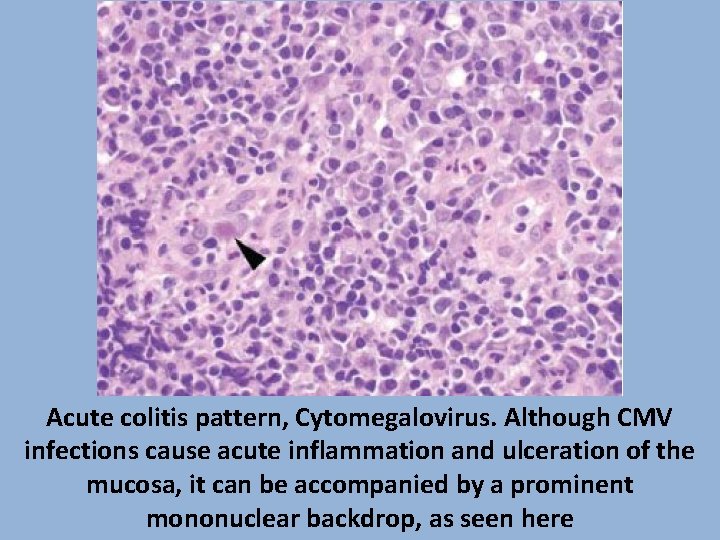
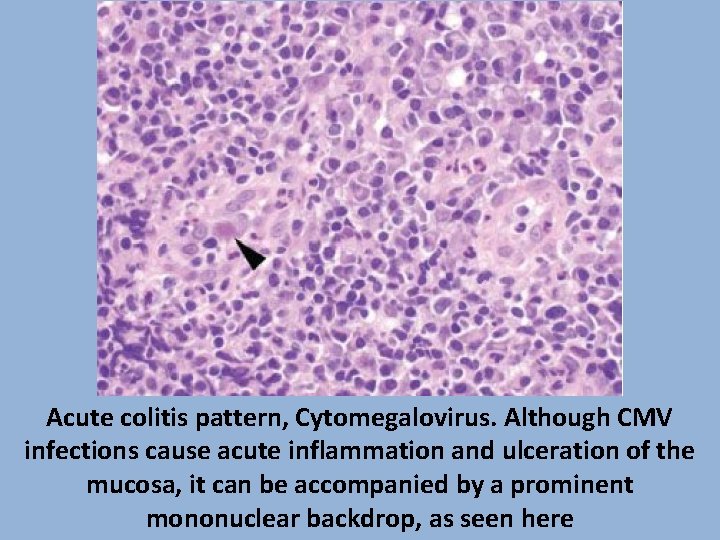
Acute colitis pattern, Cytomegalovirus. Although CMV infections cause acute inflammation and ulceration of the mucosa, it can be accompanied by a prominent mononuclear backdrop, as seen here
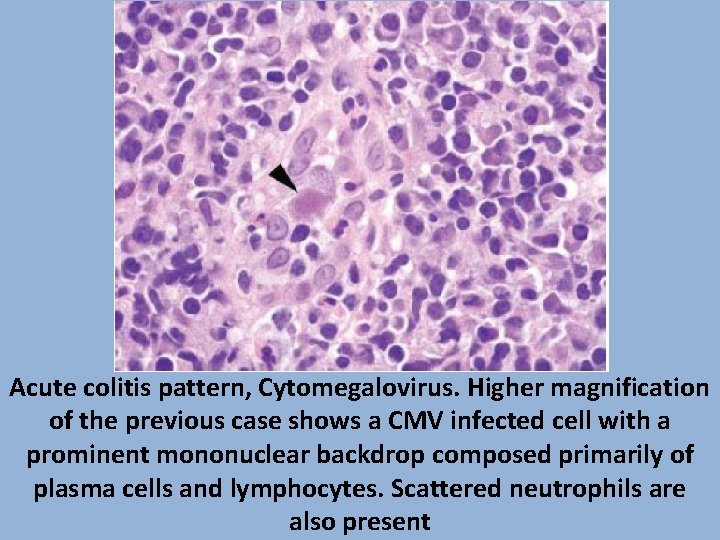
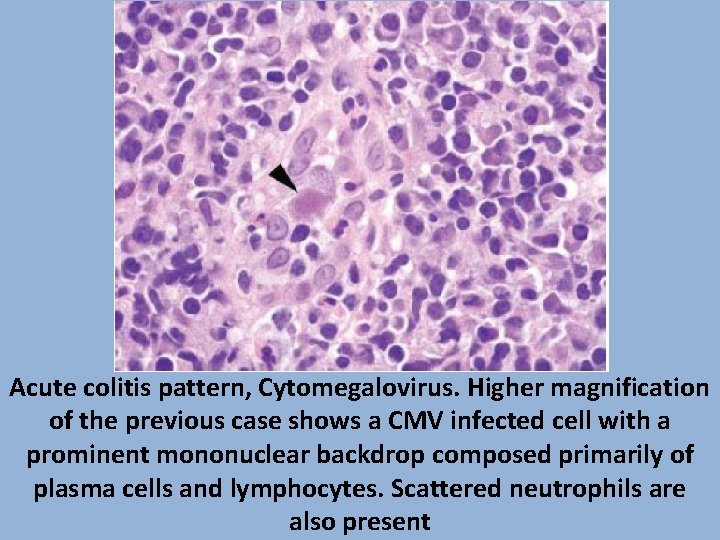
Acute colitis pattern, Cytomegalovirus. Higher magnification of the previous case shows a CMV infected cell with a prominent mononuclear backdrop composed primarily of plasma cells and lymphocytes. Scattered neutrophils are also present
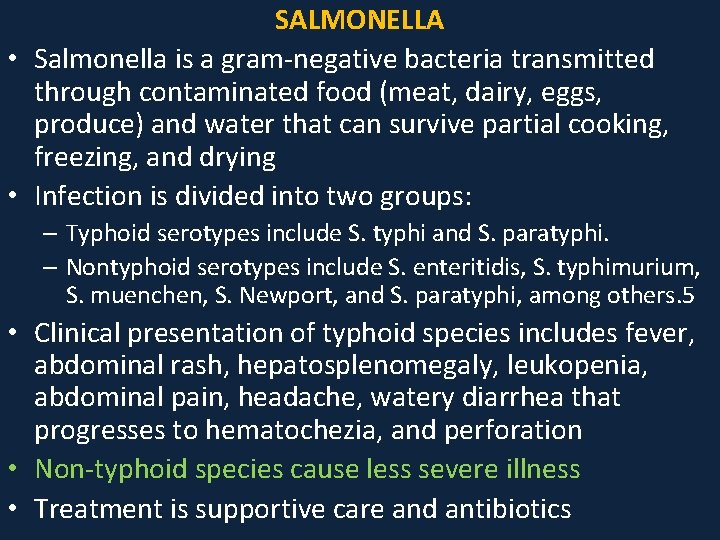
SALMONELLA • Salmonella is a gram-negative bacteria transmitted through contaminated food (meat, dairy, eggs, produce) and water that can survive partial cooking, freezing, and drying • Infection is divided into two groups: – Typhoid serotypes include S. typhi and S. paratyphi. – Nontyphoid serotypes include S. enteritidis, S. typhimurium, S. muenchen, S. Newport, and S. paratyphi, among others. 5 • Clinical presentation of typhoid species includes fever, abdominal rash, hepatosplenomegaly, leukopenia, abdominal pain, headache, watery diarrhea that progresses to hematochezia, and perforation • Non-typhoid species cause less severe illness • Treatment is supportive care and antibiotics
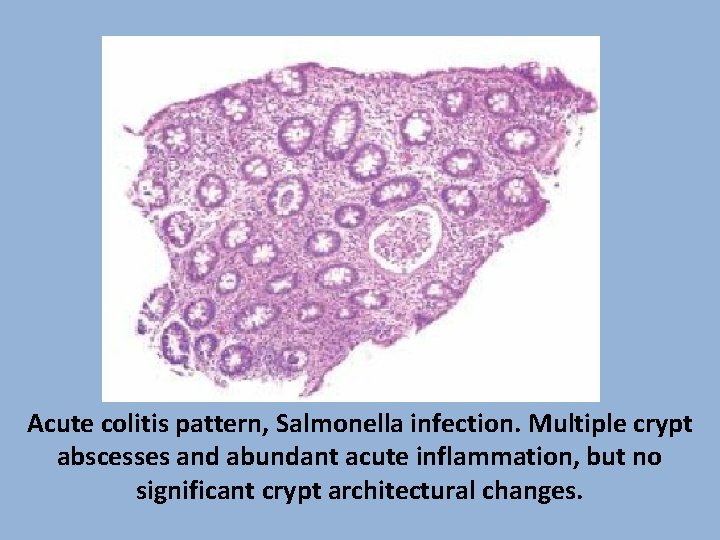
• • • Salmonella Pathology Involvement of the ileum, right colon, and appendix with hyperplastic Peyer patches, deep ulceration, and necrosis Acute inflammation and a mononuclear backdrop are present Architectural distortion of crypts may raise the question of IBD Non-typhoid infection shows an acute colitis, but features can overlap with typhoid fever Culture is required for definitive diagnosis
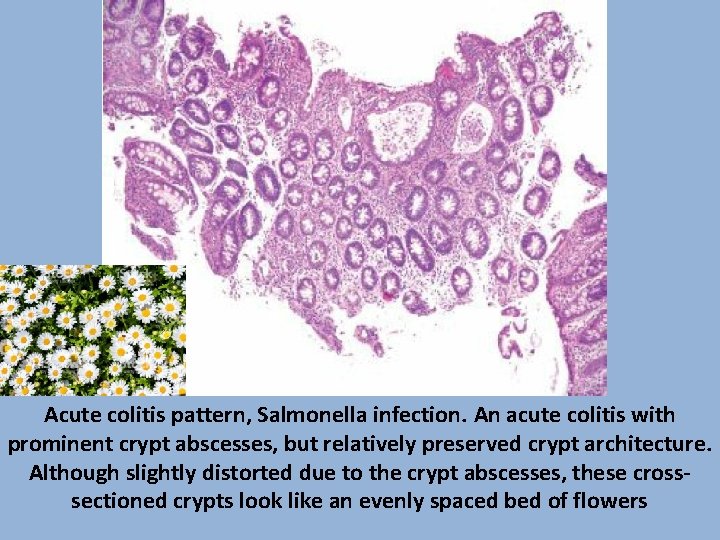
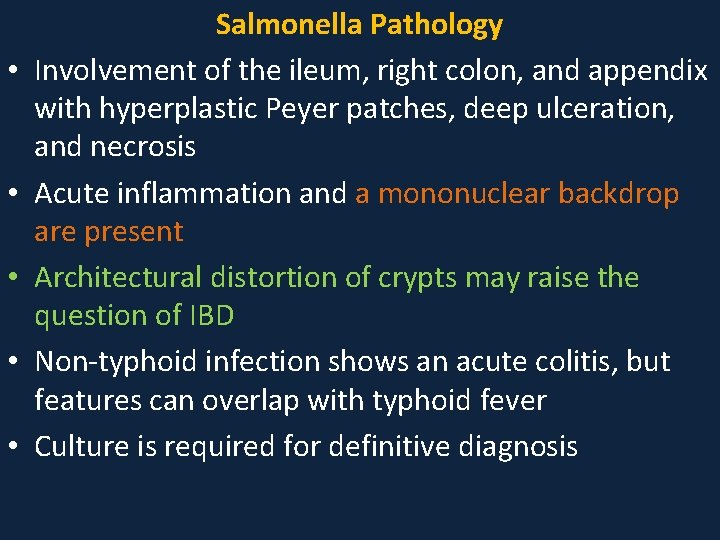
Acute colitis pattern, Salmonella infection. An acute colitis with prominent crypt abscesses, but relatively preserved crypt architecture. Although slightly distorted due to the crypt abscesses, these crosssectioned crypts look like an evenly spaced bed of flowers
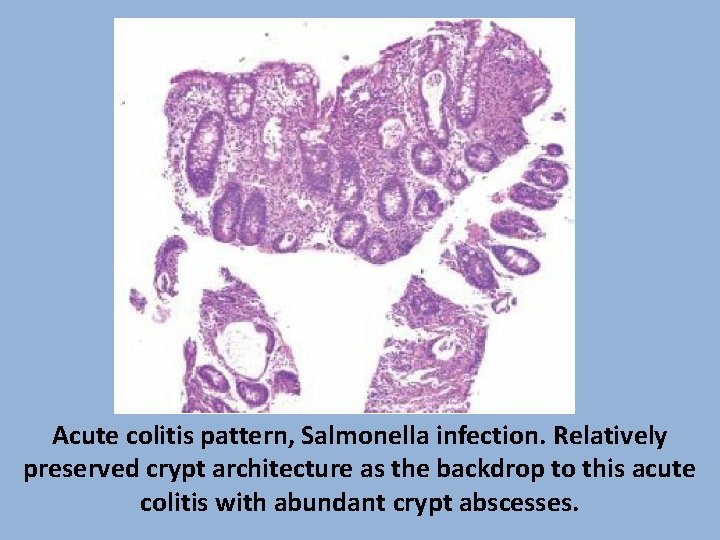
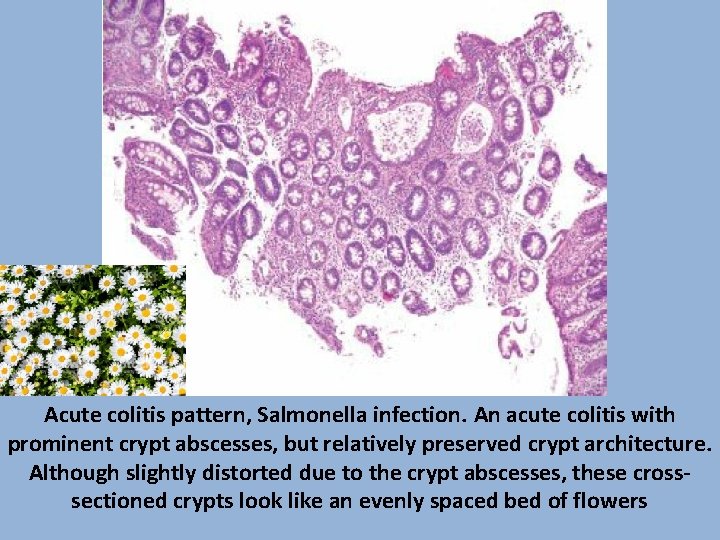
Acute colitis pattern, Salmonella infection. Relatively preserved crypt architecture as the backdrop to this acute colitis with abundant crypt abscesses.
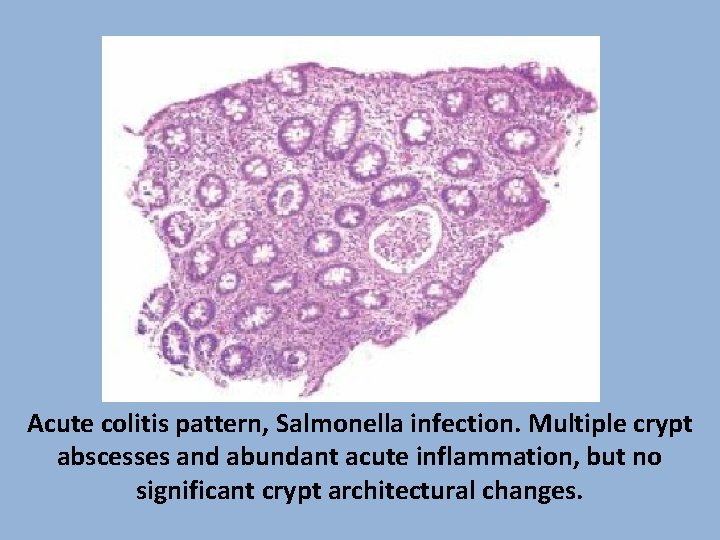
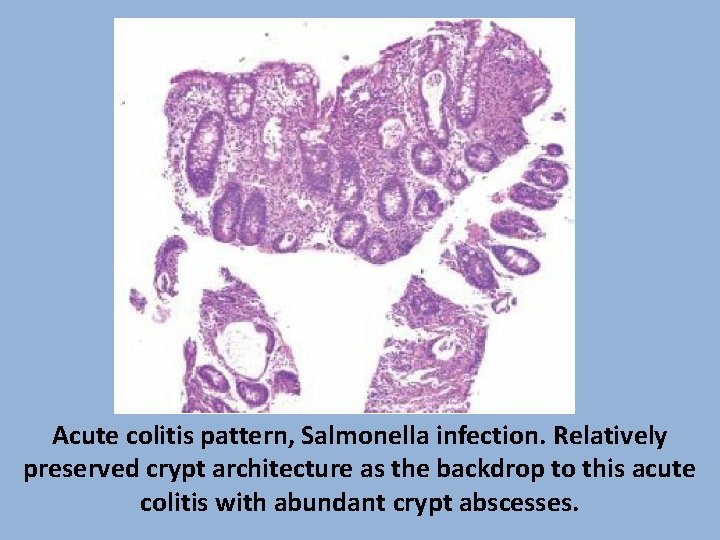
Acute colitis pattern, Salmonella infection. Multiple crypt abscesses and abundant acute inflammation, but no significant crypt architectural changes.
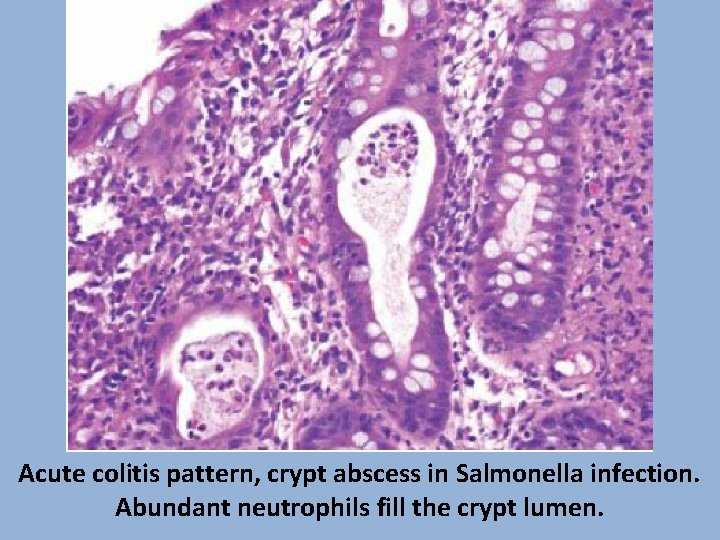
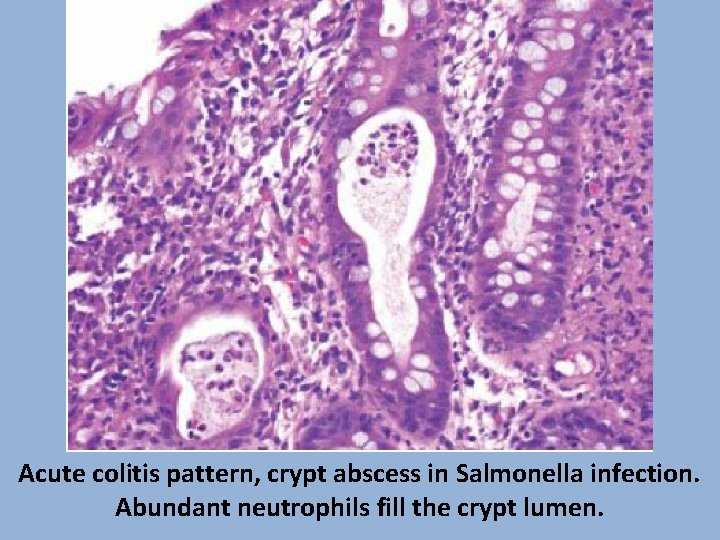
Acute colitis pattern, crypt abscess in Salmonella infection. Abundant neutrophils fill the crypt lumen.
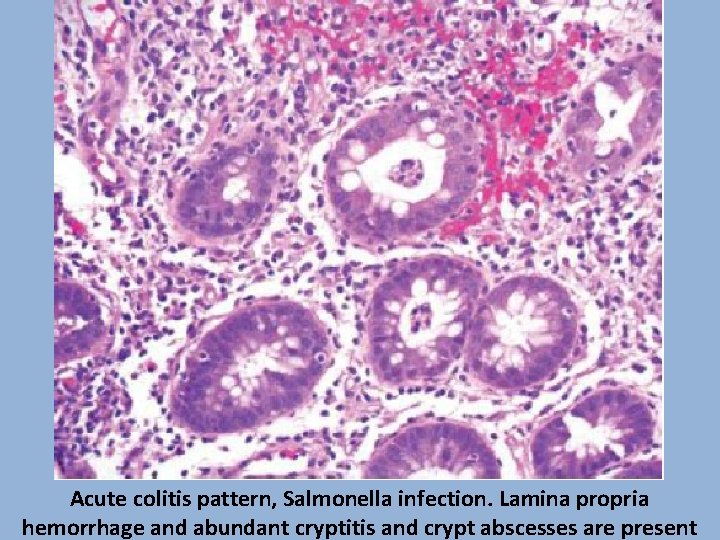
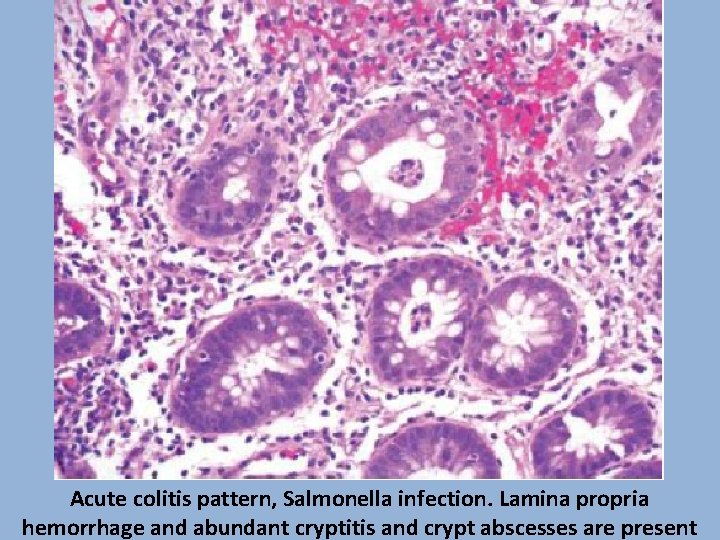
Acute colitis pattern, Salmonella infection. Lamina propria hemorrhage and abundant cryptitis and crypt abscesses are present
• • Shigella An invasive gram-negative bacillus and a major cause of diarrhea across the world S. dysenteriae is the most virulent and most common, but S. sonnei and S. flexneri are increasingly reported in the United States Shigella has the highest infectivity rate among all enteric gram-negative bacteria, with food- and water-borne transmission, as well as the fecal–oral route; rare instances of sexual transmission are also reported Outbreaks are associated with crowded living conditions and poor sanitation, with children less than 6 years most commonly affected
• • • Shigella Patients present with fever, abdominal pain, and watery diarrhea, followed by bloody diarrhea with mucus and pus Onset of symptoms begins within 12 to 50 hours after ingestion of contaminated food or water Medical complications are most commonly seen with S. dysenteriae, and include severe dehydration, sepsis, toxic megacolon and perforation Autoimmune phenomena such as reactive arthritis, reactive arthropathy, and hemolytic–anemic syndrome also occur Treatment is supportive care and antibiotics
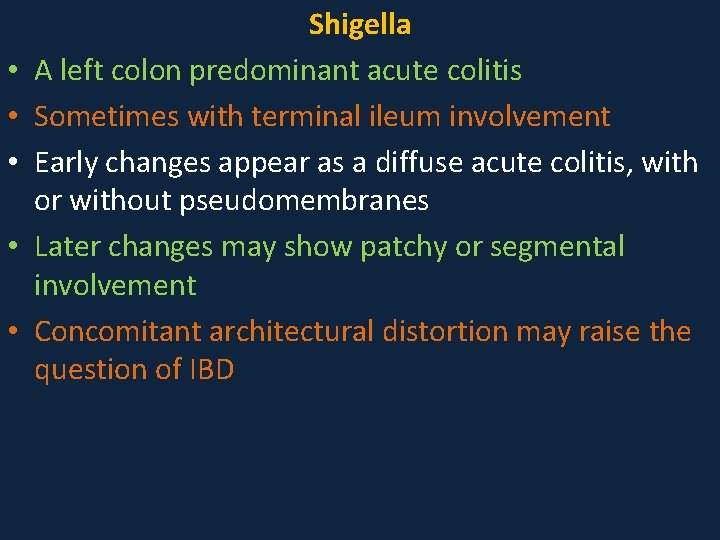
• • • Shigella A left colon predominant acute colitis Sometimes with terminal ileum involvement Early changes appear as a diffuse acute colitis, with or without pseudomembranes Later changes may show patchy or segmental involvement Concomitant architectural distortion may raise the question of IBD
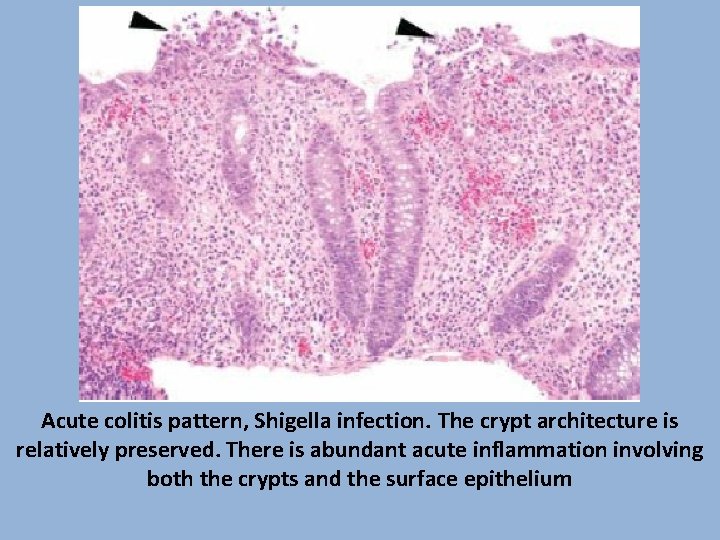
Acute colitis pattern, Shigella infection. The crypt architecture is relatively preserved. There is abundant acute inflammation involving both the crypts and the surface epithelium
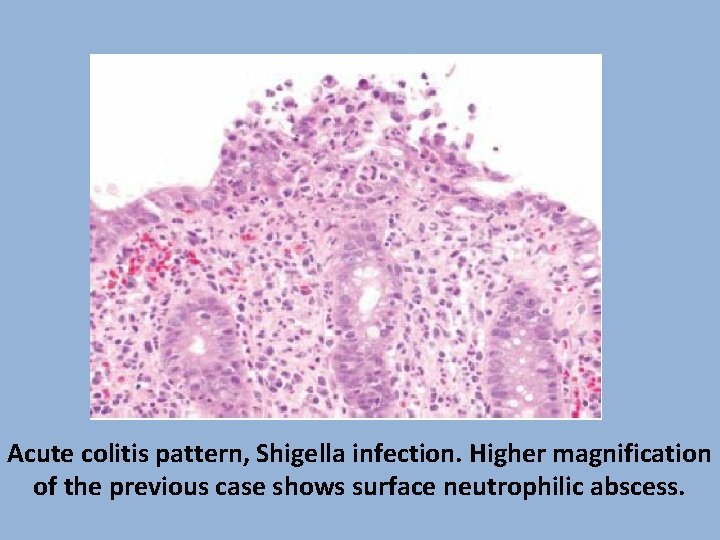
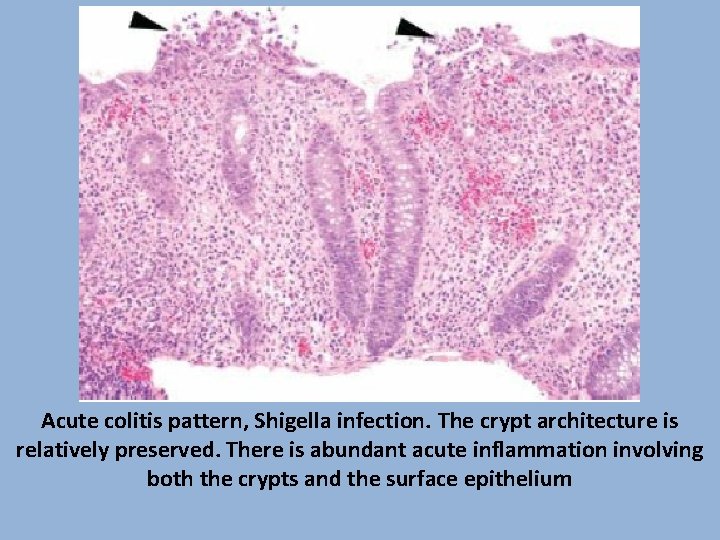
Acute colitis pattern, Shigella infection. Higher magnification of the previous case shows surface neutrophilic abscess.
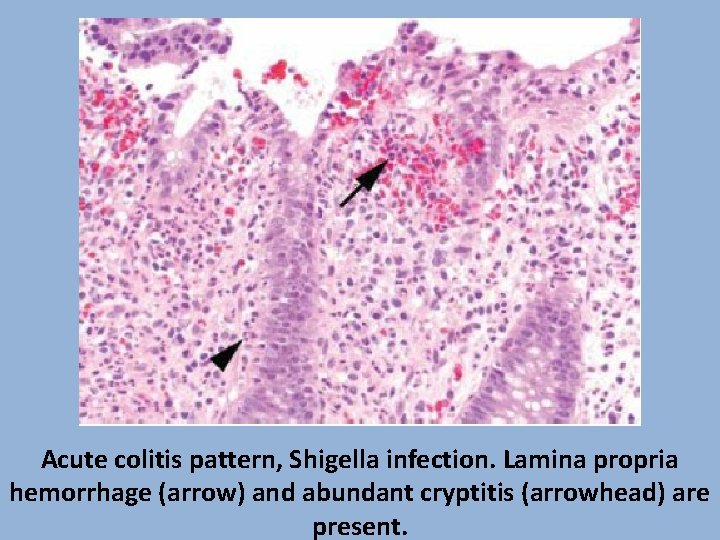
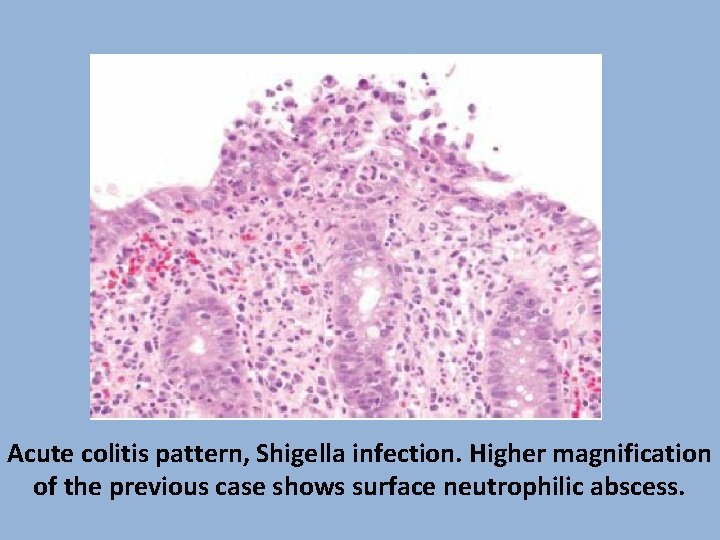
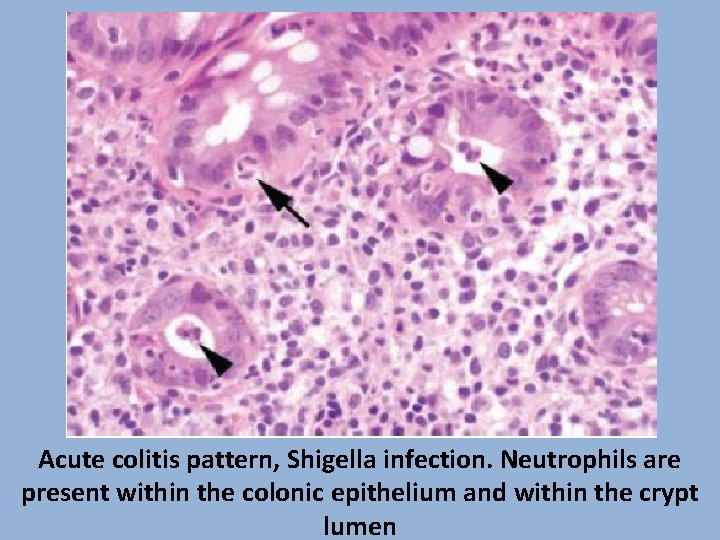
Acute colitis pattern, Shigella infection. Lamina propria hemorrhage (arrow) and abundant cryptitis (arrowhead) are present.
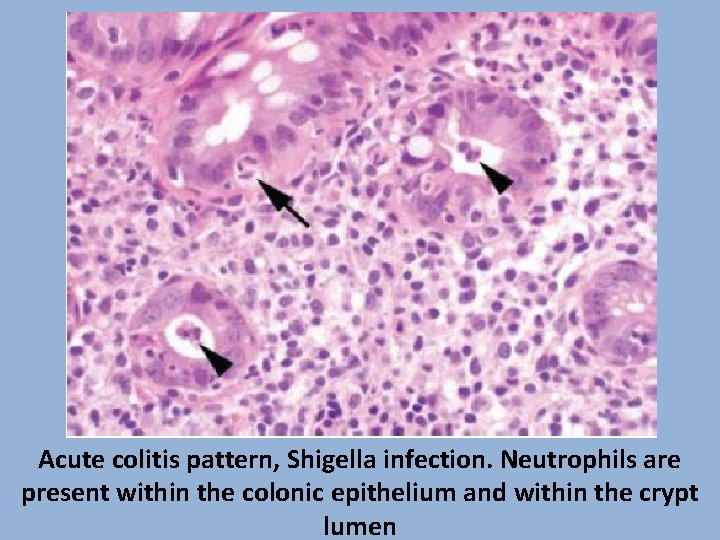
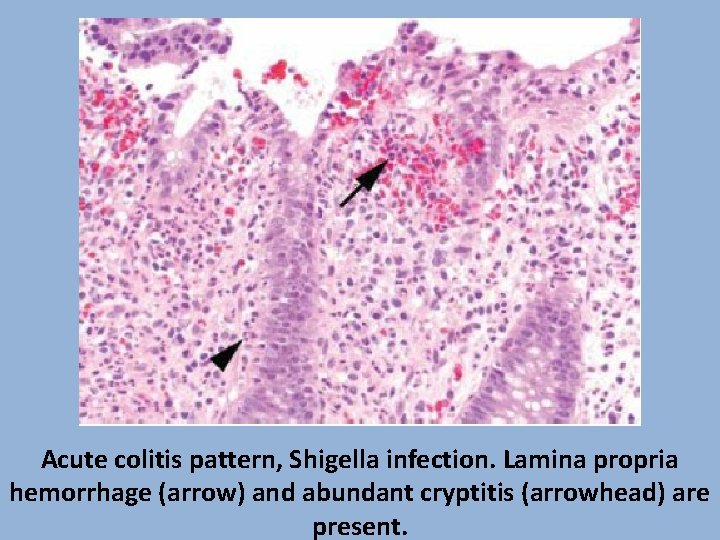
Acute colitis pattern, Shigella infection. Neutrophils are present within the colonic epithelium and within the crypt lumen
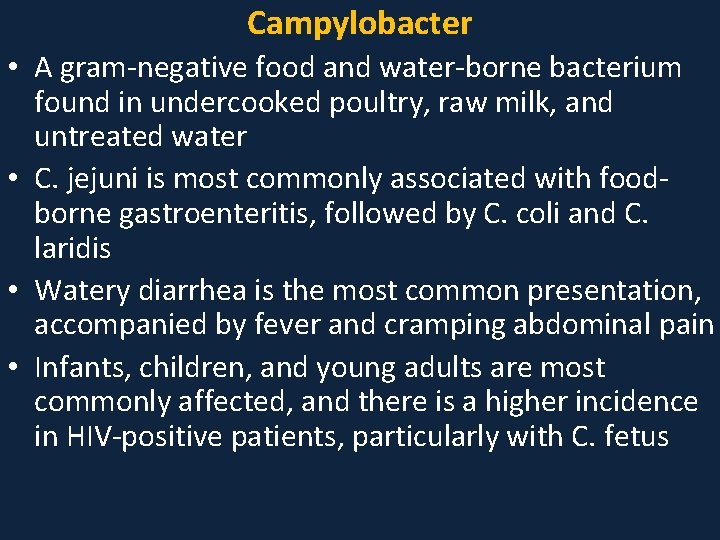
Campylobacter • A gram-negative food and water-borne bacterium found in undercooked poultry, raw milk, and untreated water • C. jejuni is most commonly associated with foodborne gastroenteritis, followed by C. coli and C. laridis • Watery diarrhea is the most common presentation, accompanied by fever and cramping abdominal pain • Infants, children, and young adults are most commonly affected, and there is a higher incidence in HIV-positive patients, particularly with C. fetus
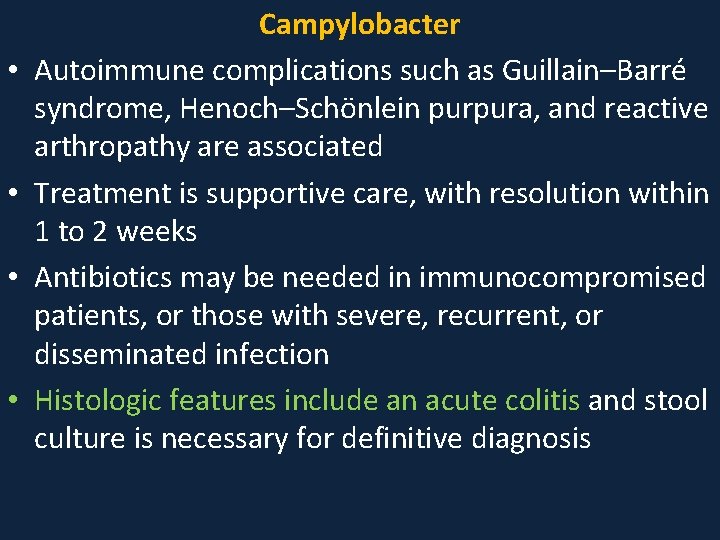
• • Campylobacter Autoimmune complications such as Guillain–Barré syndrome, Henoch–Schönlein purpura, and reactive arthropathy are associated Treatment is supportive care, with resolution within 1 to 2 weeks Antibiotics may be needed in immunocompromised patients, or those with severe, recurrent, or disseminated infection Histologic features include an acute colitis and stool culture is necessary for definitive diagnosis
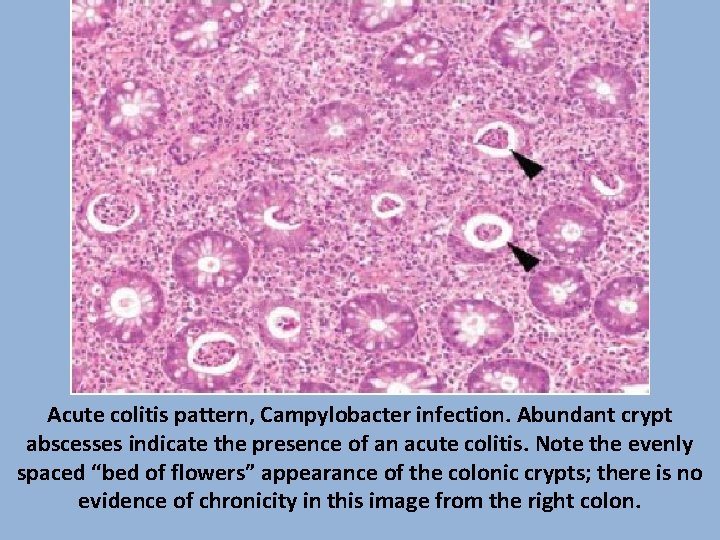
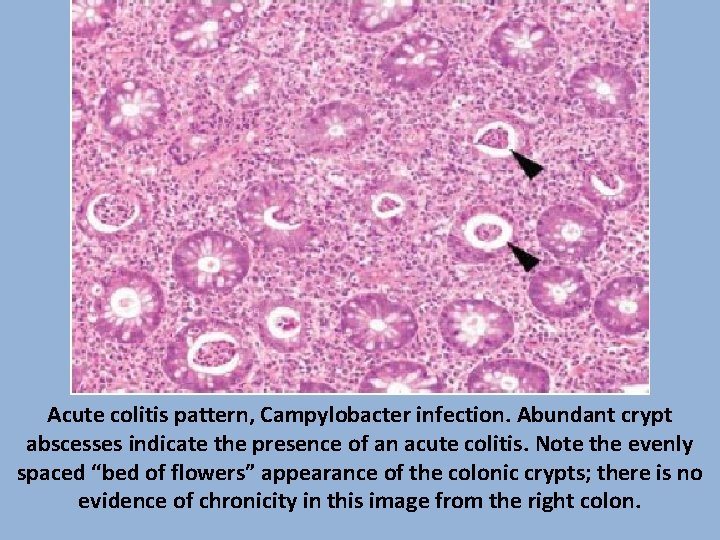
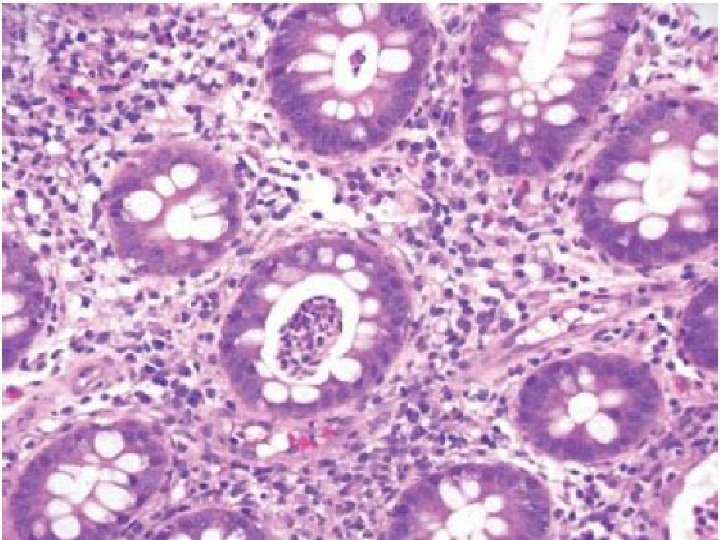
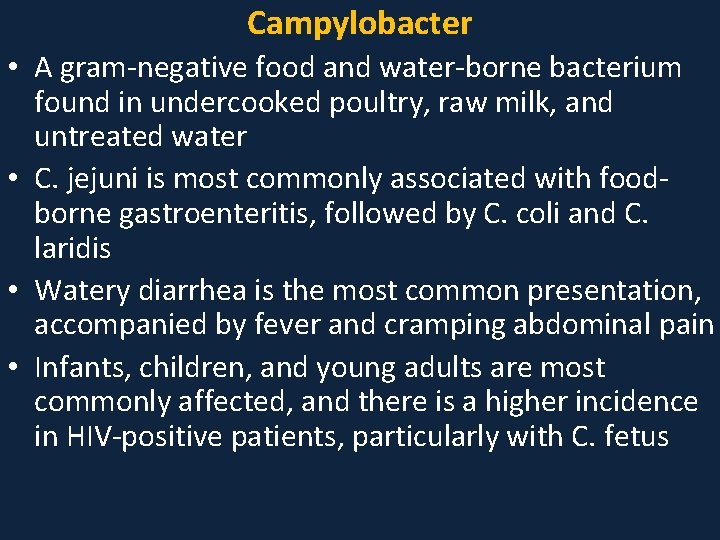
Acute colitis pattern, Campylobacter infection. Abundant crypt abscesses indicate the presence of an acute colitis. Note the evenly spaced “bed of flowers” appearance of the colonic crypts; there is no evidence of chronicity in this image from the right colon.
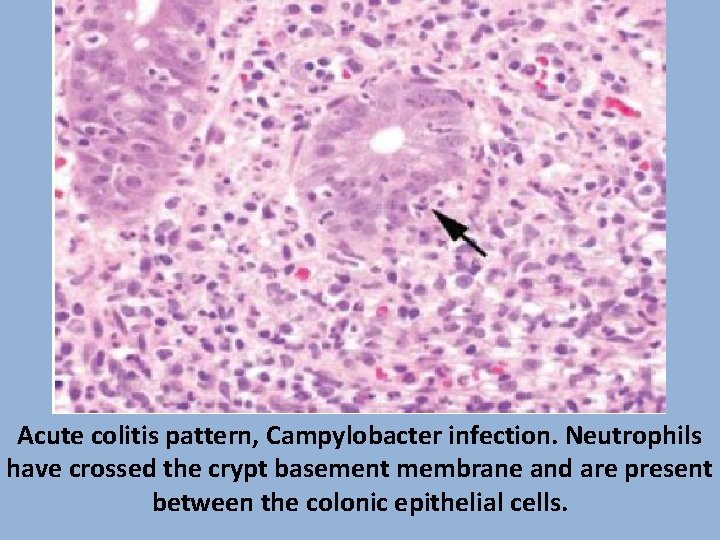
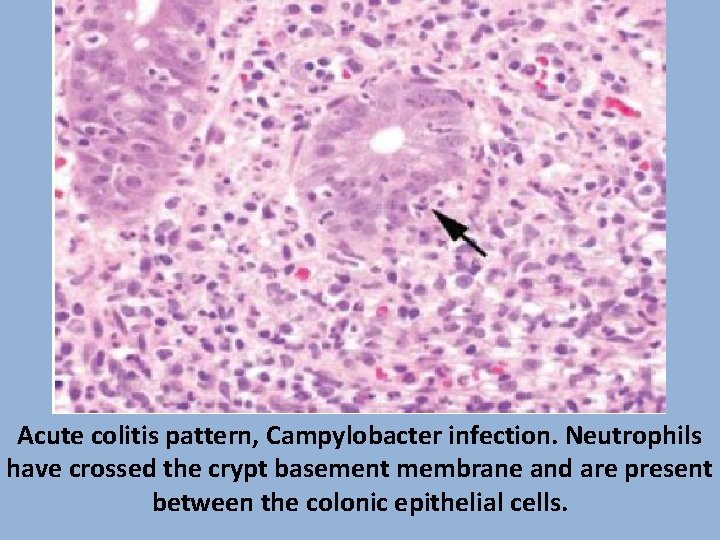
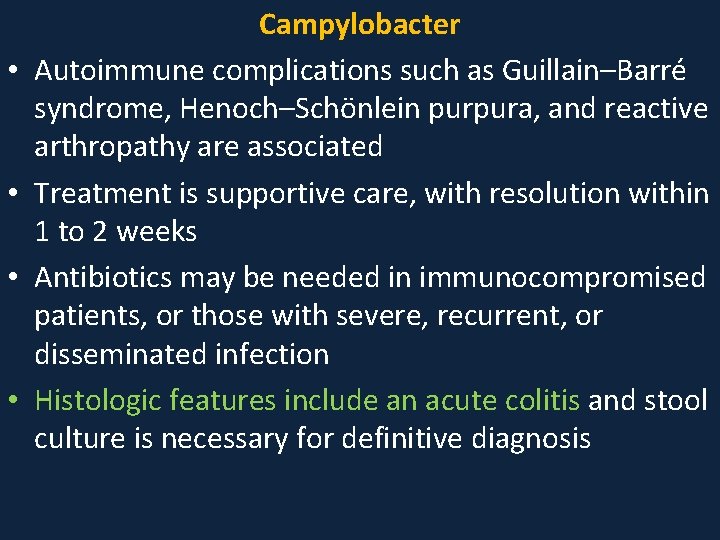
Acute colitis pattern, Campylobacter infection. Neutrophils have crossed the crypt basement membrane and are present between the colonic epithelial cells.
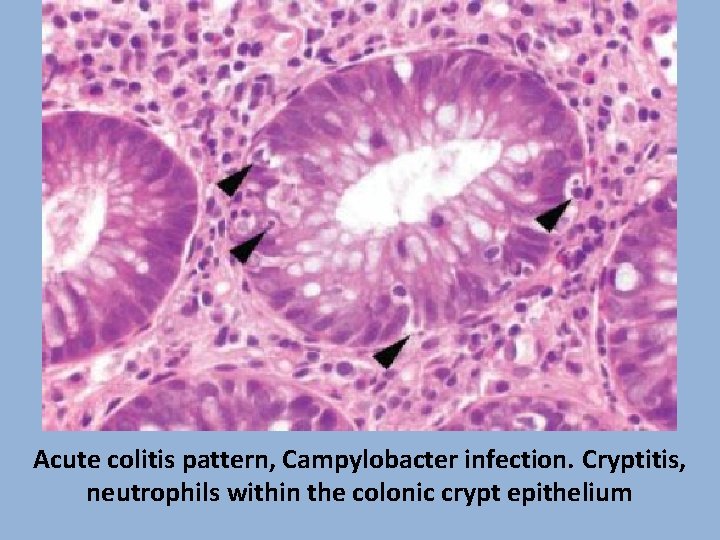
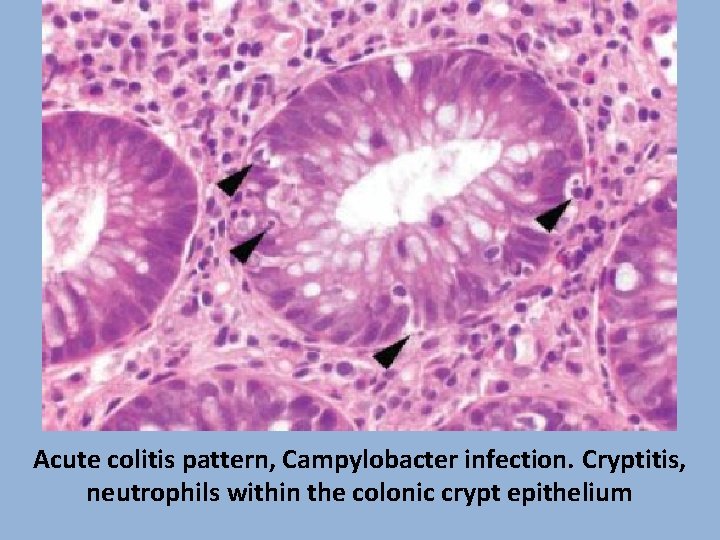
Acute colitis pattern, Campylobacter infection. Cryptitis, neutrophils within the colonic crypt epithelium
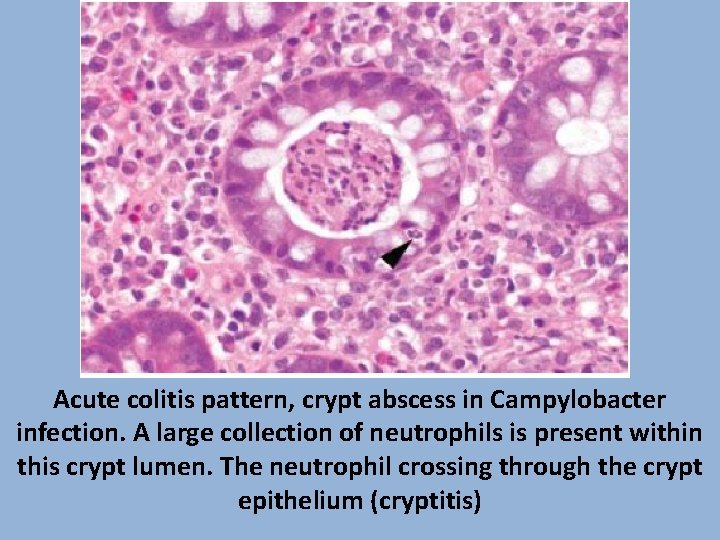
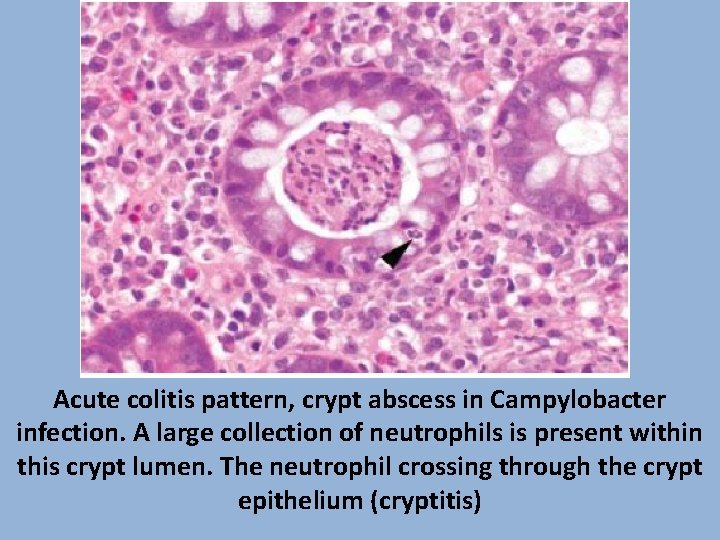
Acute colitis pattern, crypt abscess in Campylobacter infection. A large collection of neutrophils is present within this crypt lumen. The neutrophil crossing through the crypt epithelium (cryptitis)