ACUTE CHRONIC AORTIC DISSECTION Constandinos A Pamboucas MD
ACUTE & CHRONIC AORTIC DISSECTION Constandinos A. Pamboucas MD, Ph. D Department Of Clinical Therapeutics, University Of Athens, Alexandra Hospital
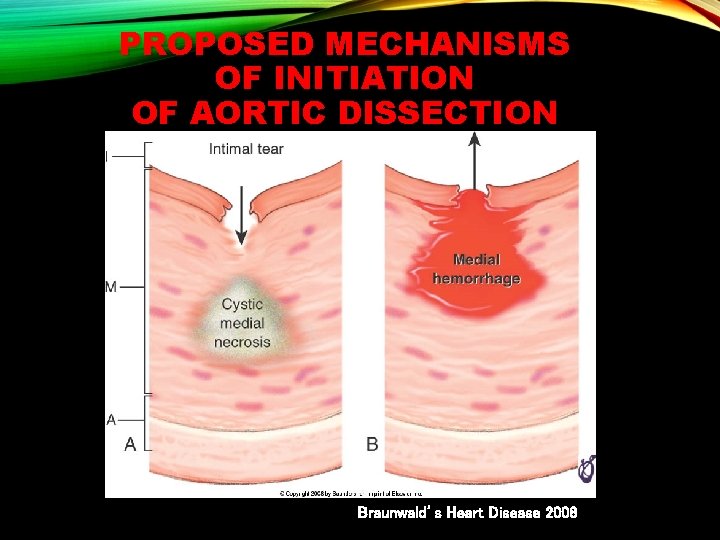
PROPOSED MECHANISMS OF INITIATION OF AORTIC DISSECTION Braunwald’s Heart Disease 2008
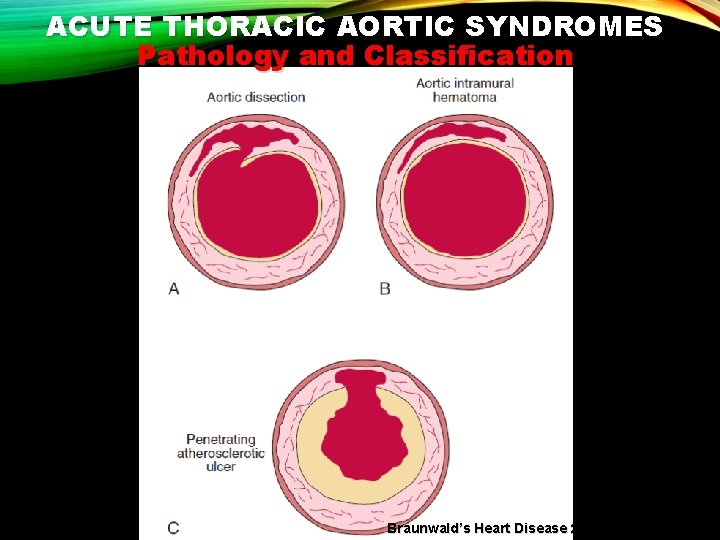
ACUTE THORACIC AORTIC SYNDROMES Pathology and Classification Braunwald’s Heart Disease 2012

ACUTE THORACIC AORTIC SYNDROMES Pathology and Classification Class 1: Classic AD with true and FL with or without communication between the two lumina Class 2: Intramural haematoma Class 3: Subtle or discrete AD with bulging of the aortic wall Eur Heart J 2014 Class 4: Ulceration of aortic plaque following plaque rupture
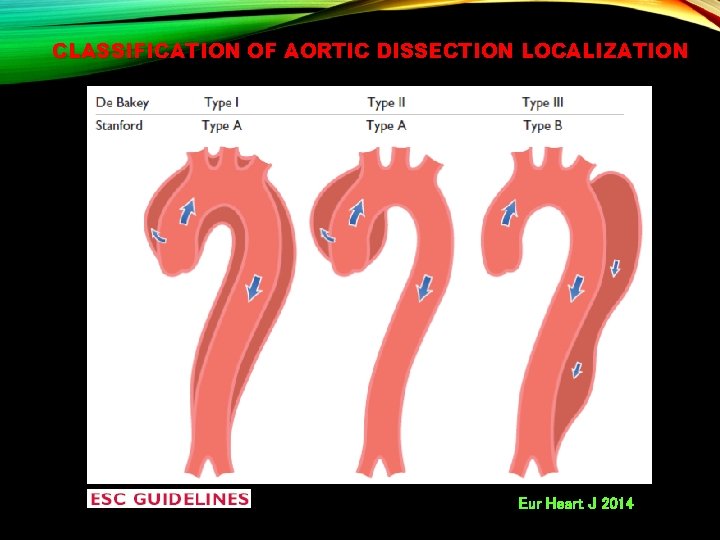
CLASSIFICATION OF AORTIC DISSECTION LOCALIZATION Eur Heart J 2014
AORTIC DISSECTION Classification Acute: <14 days Sub-acute: 15– 90 days Chronic: >90 days Eur Heart J 2014
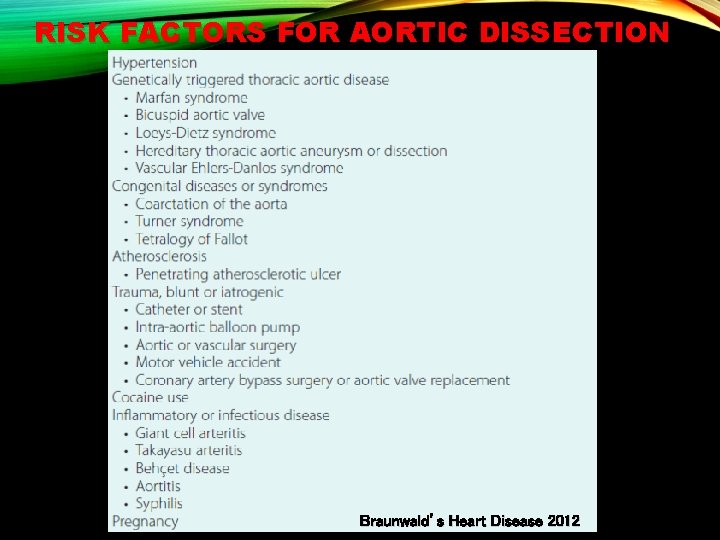
RISK FACTORS FOR AORTIC DISSECTION Braunwald’s Heart Disease 2012

IATROGENIC AORTIC DISSECTION Catheter-based coronary procedures Cardiac surgery Endovascular treatment of aortic coarctation Aortic endografting Peripheral interventions Intra-aortic balloon counterpulsation Transcatheter aortic valve implantation Eur Heart J 2014
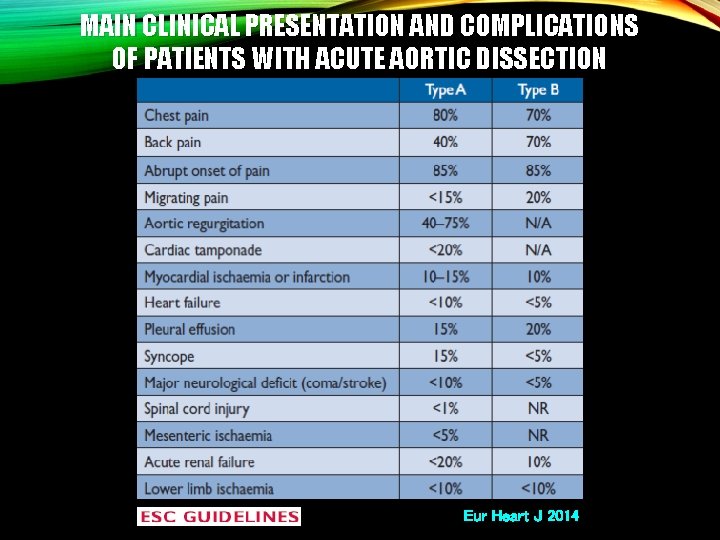
MAIN CLINICAL PRESENTATION AND COMPLICATIONS OF PATIENTS WITH ACUTE AORTIC DISSECTION Eur Heart J 2014
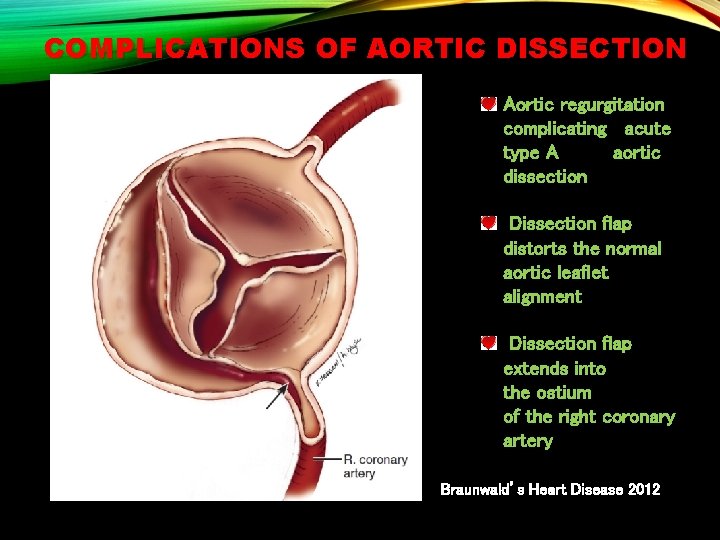
COMPLICATIONS OF AORTIC DISSECTION Aortic regurgitation complicating acute type A aortic dissection Dissection flap distorts the normal aortic leaflet alignment Dissection flap extends into the ostium of the right coronary artery Braunwald’s Heart Disease 2012
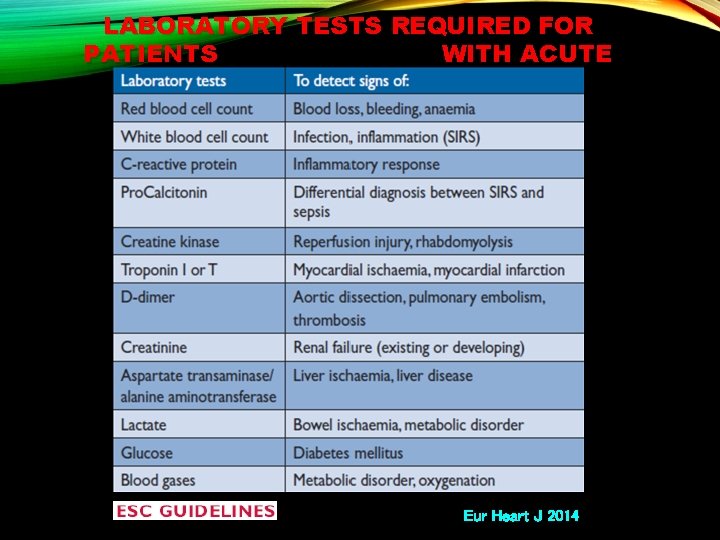
LABORATORY TESTS REQUIRED FOR PATIENTS WITH ACUTE AORTIC DISSECTION Eur Heart J 2014
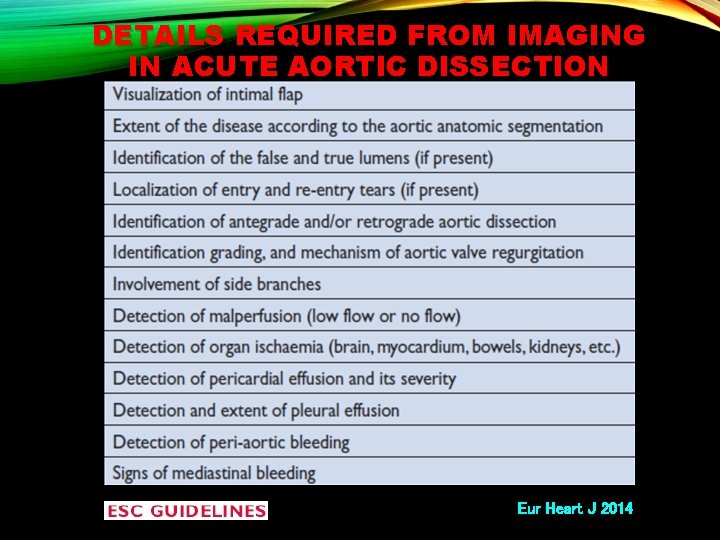
DETAILS REQUIRED FROM IMAGING IN ACUTE AORTIC DISSECTION Eur Heart J 2014
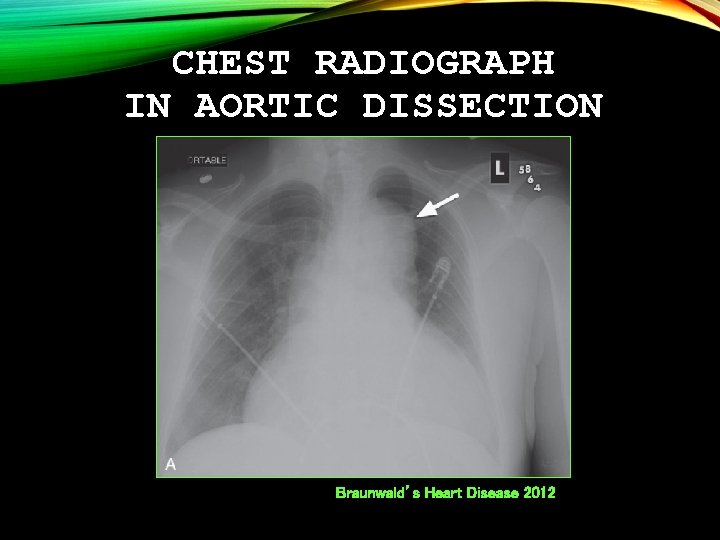
CHEST RADIOGRAPH IN AORTIC DISSECTION Braunwald’s Heart Disease 2012
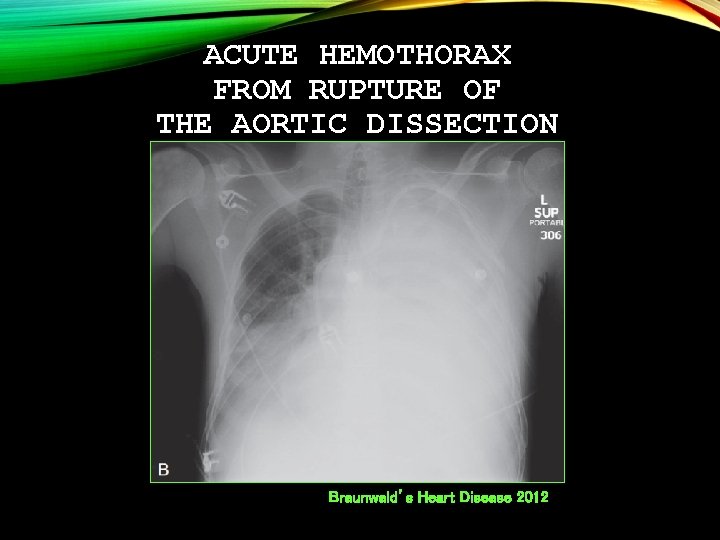
ACUTE HEMOTHORAX FROM RUPTURE OF THE AORTIC DISSECTION Braunwald’s Heart Disease 2012
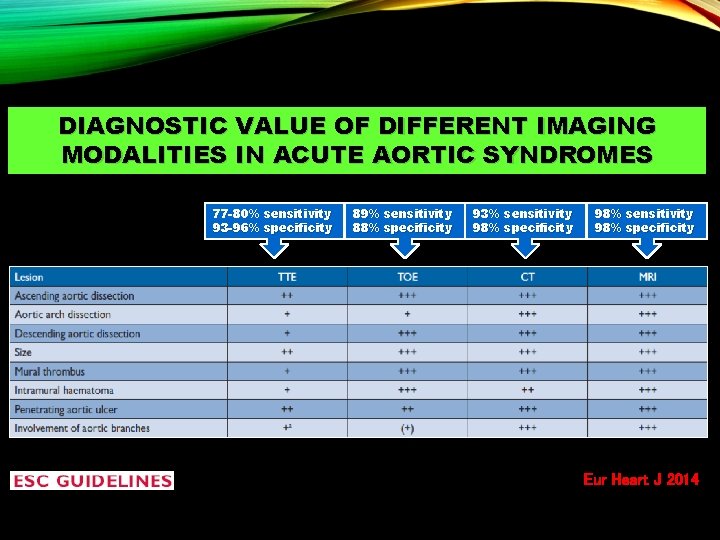
DIAGNOSTIC VALUE OF DIFFERENT IMAGING MODALITIES IN ACUTE AORTIC SYNDROMES 77 -80% sensitivity 93 -96% specificity 89% sensitivity 88% specificity 93% sensitivity 98% specificity 98% sensitivity 98% specificity Eur Heart J 2014
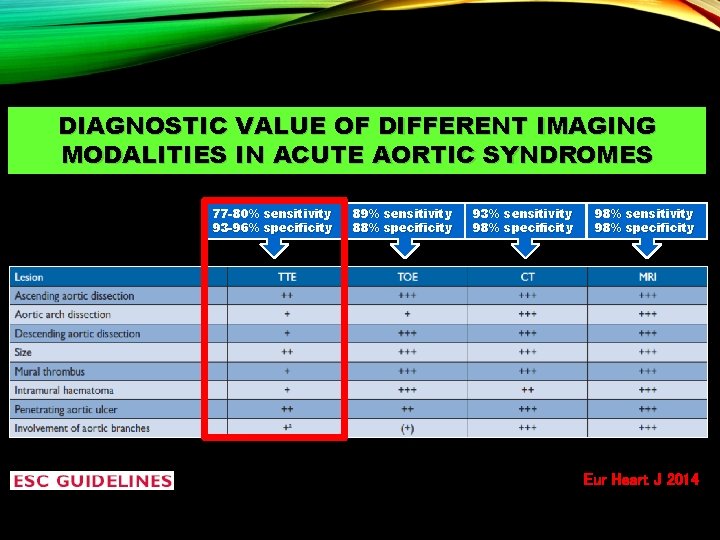
DIAGNOSTIC VALUE OF DIFFERENT IMAGING MODALITIES IN ACUTE AORTIC SYNDROMES 77 -80% sensitivity 93 -96% specificity 89% sensitivity 88% specificity 93% sensitivity 98% specificity 98% sensitivity 98% specificity Eur Heart J 2014
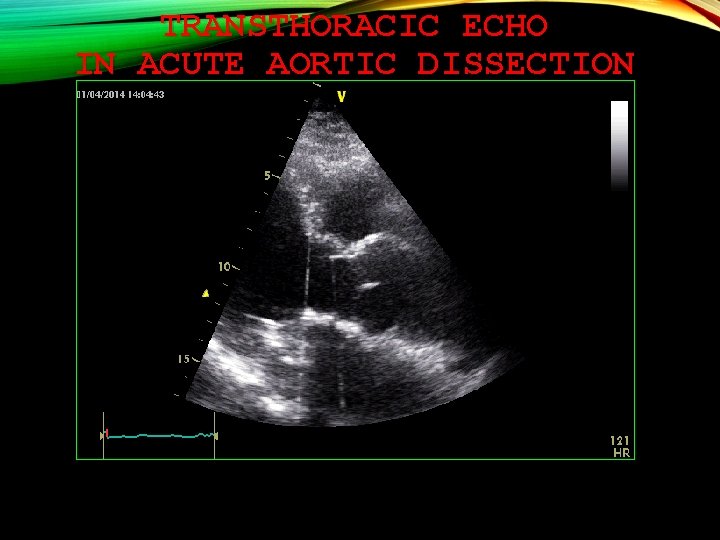
TRANSTHORACIC ECHO IN ACUTE AORTIC DISSECTION
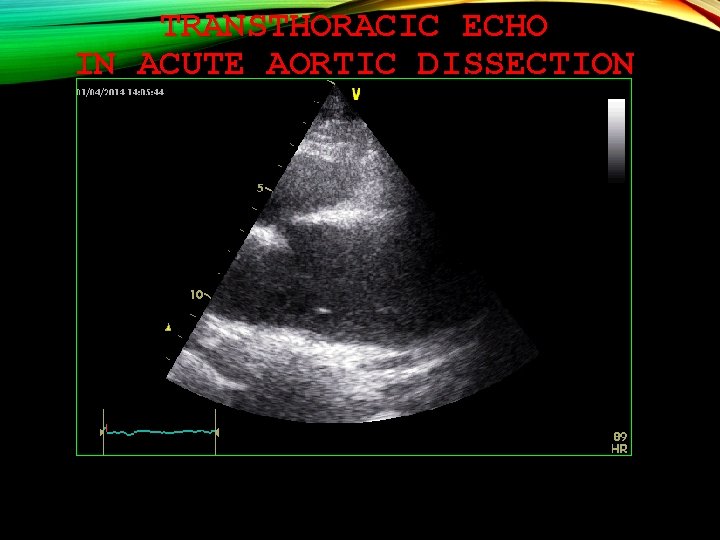
TRANSTHORACIC ECHO IN ACUTE AORTIC DISSECTION
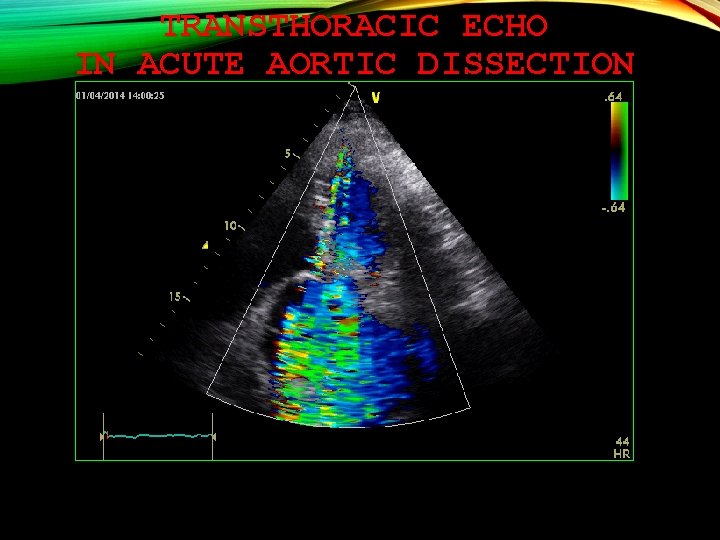
TRANSTHORACIC ECHO IN ACUTE AORTIC DISSECTION
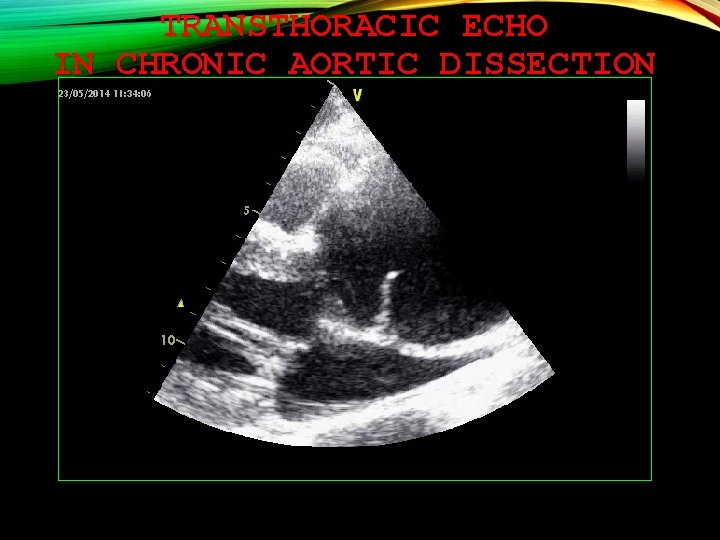
TRANSTHORACIC ECHO IN CHRONIC AORTIC DISSECTION
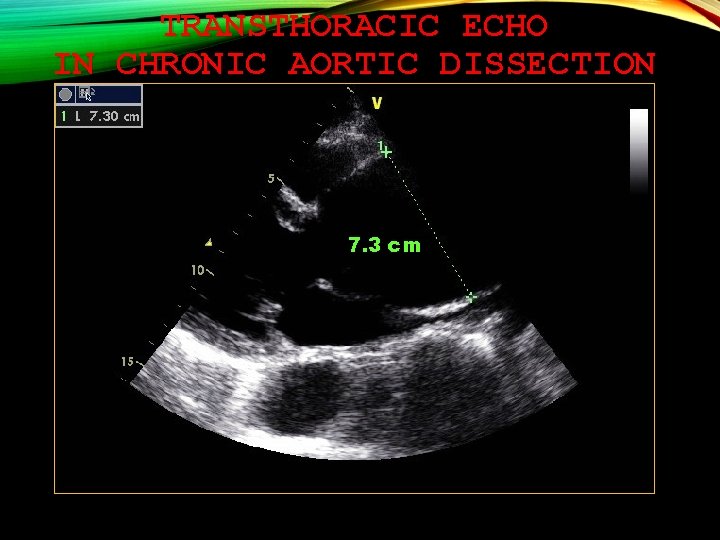
TRANSTHORACIC ECHO IN CHRONIC AORTIC DISSECTION 7. 3 cm
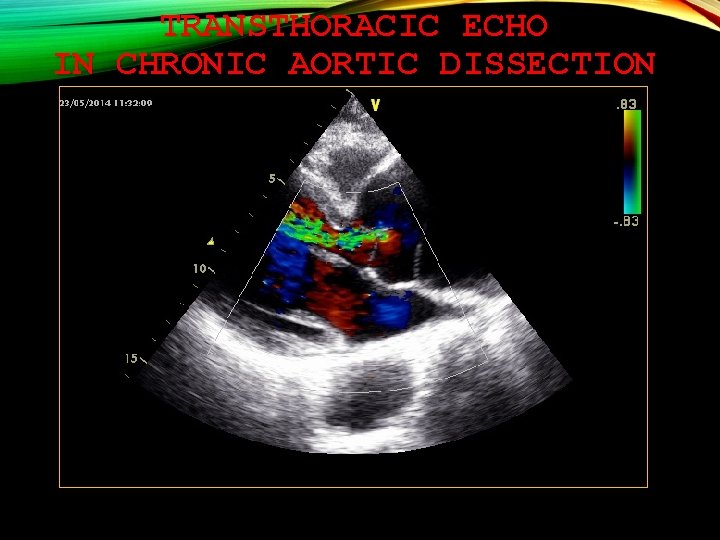
TRANSTHORACIC ECHO IN CHRONIC AORTIC DISSECTION
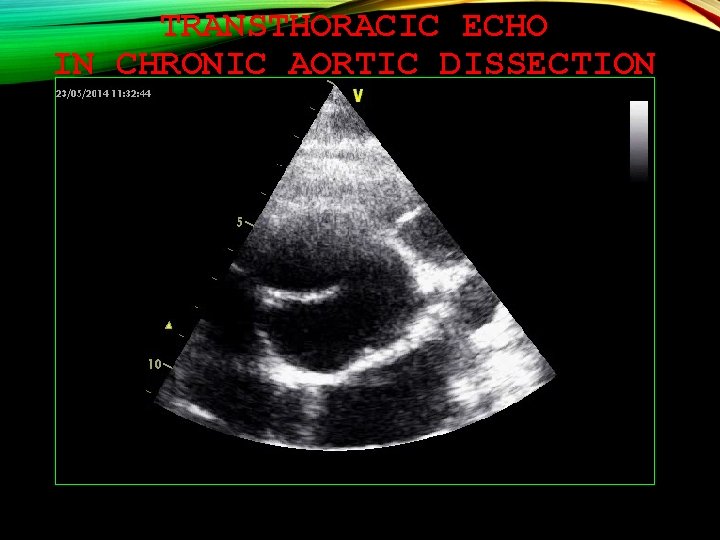
TRANSTHORACIC ECHO IN CHRONIC AORTIC DISSECTION
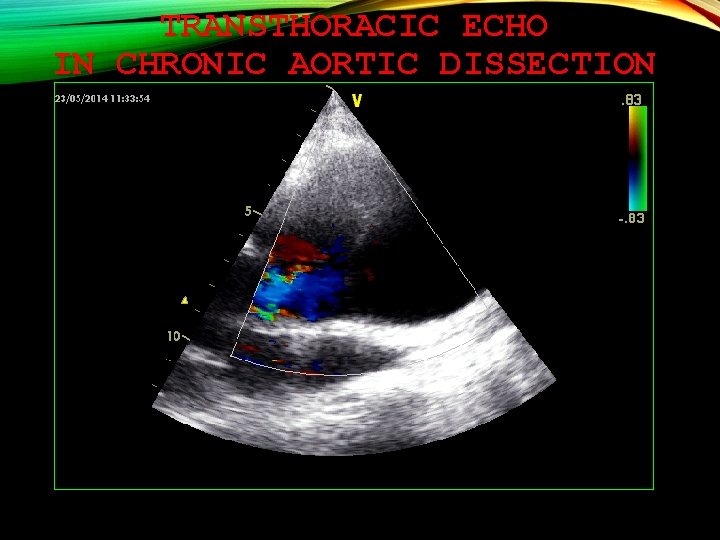
TRANSTHORACIC ECHO IN CHRONIC AORTIC DISSECTION
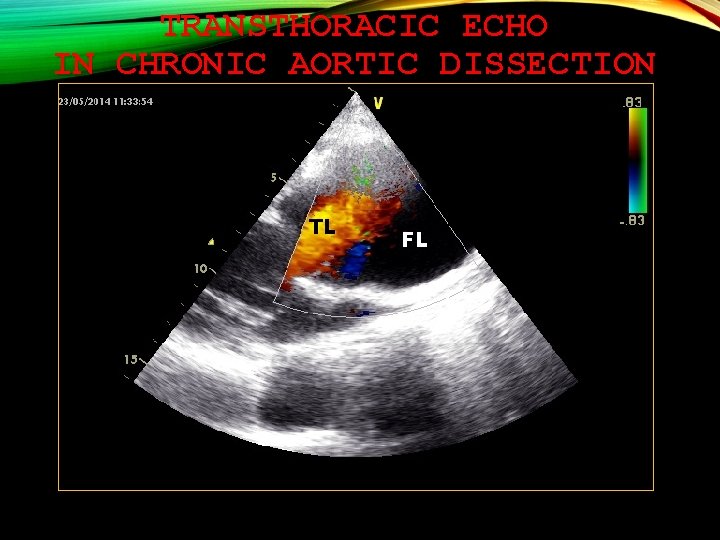
TRANSTHORACIC ECHO IN CHRONIC AORTIC DISSECTION TL FL
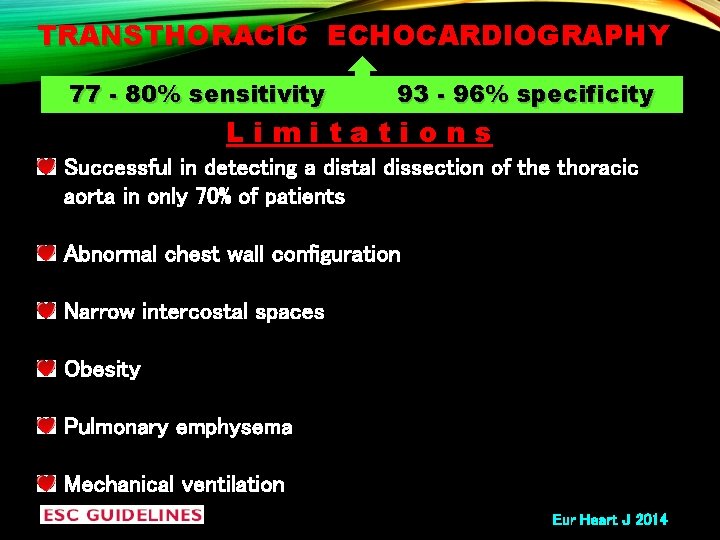
TRANSTHORACIC ECHOCARDIOGRAPHY 77 - 80% sensitivity 93 - 96% specificity Limitations Successful in detecting a distal dissection of the thoracic aorta in only 70% of patients Abnormal chest wall configuration Narrow intercostal spaces Obesity Pulmonary emphysema Mechanical ventilation Eur Heart J 2014
TRANSESOPHAGEAL ECHO
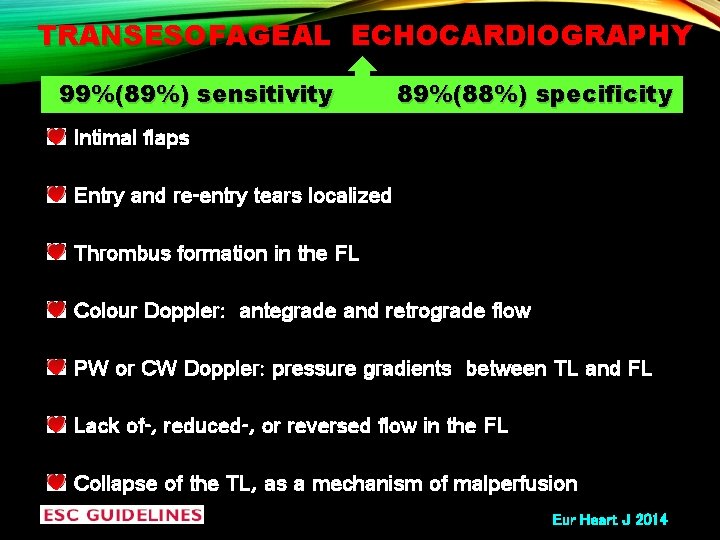
TRANSESOFAGEAL ECHOCARDIOGRAPHY 99%(89%) sensitivity 89%(88%) specificity Intimal flaps Entry and re-entry tears localized Thrombus formation in the FL Colour Doppler: antegrade and retrograde flow PW or CW Doppler: pressure gradients between TL and FL Lack of-, reduced-, or reversed flow in the FL Collapse of the TL, as a mechanism of malperfusion Eur Heart J 2014
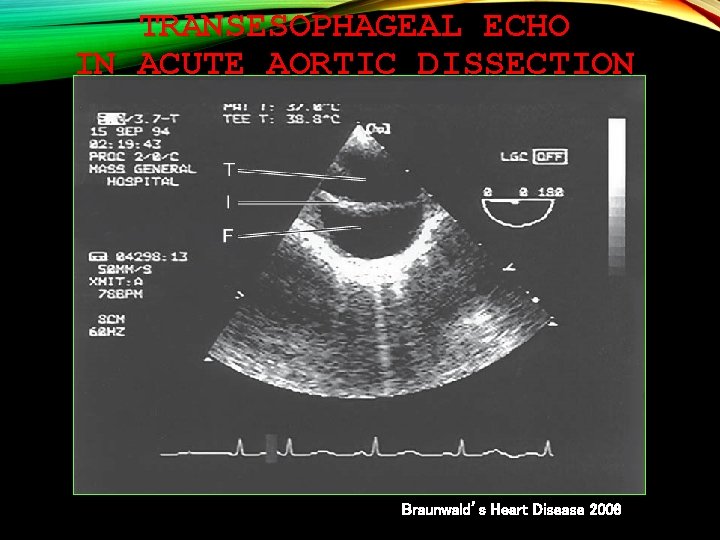
TRANSESOPHAGEAL ECHO IN ACUTE AORTIC DISSECTION Braunwald’s Heart Disease 2008
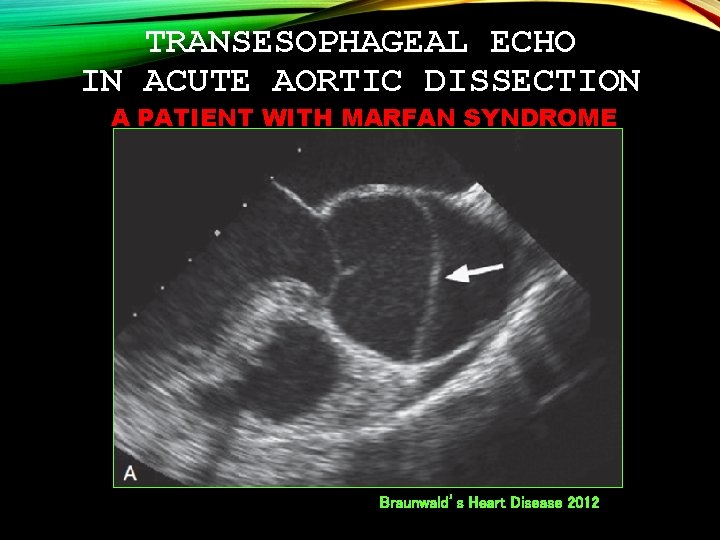
TRANSESOPHAGEAL ECHO IN ACUTE AORTIC DISSECTION A PATIENT WITH MARFAN SYNDROME Braunwald’s Heart Disease 2012
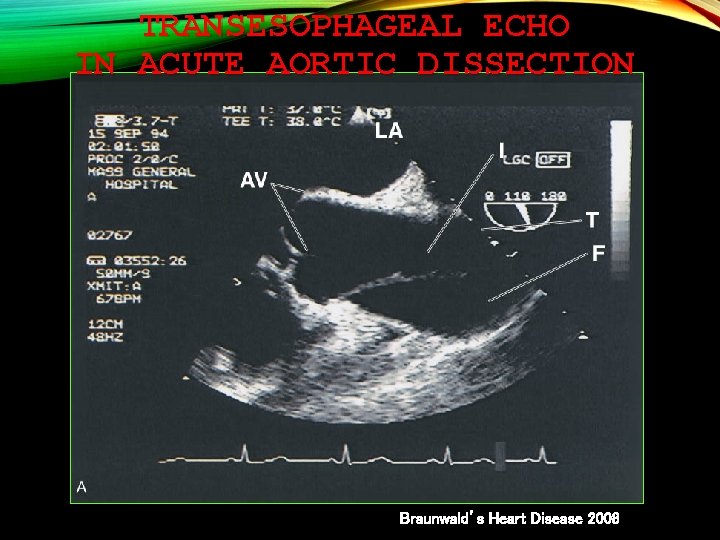
TRANSESOPHAGEAL ECHO IN ACUTE AORTIC DISSECTION Braunwald’s Heart Disease 2008

TRANSESOPHAGEAL ECHO IN ACUTE AORTIC DISSECTION Braunwald’s Heart Disease 2008

DIAGNOSTIC VALUE OF DIFFERENT IMAGING MODALITIES IN ACUTE AORTIC SYNDROMES 77 -80% sensitivity 93 -96% specificity 89% sensitivity 88% specificity 93% sensitivity 98% specificity 98% sensitivity 98% specificity Eur Heart J 2014
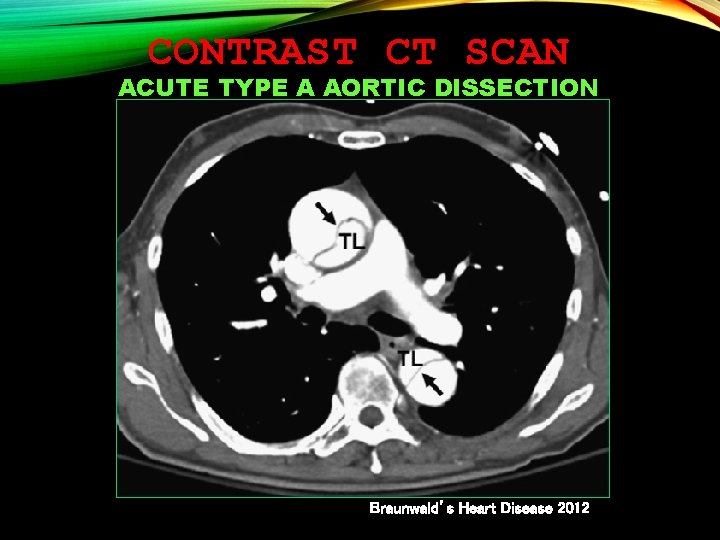
CONTRAST CT SCAN ACUTE TYPE A AORTIC DISSECTION Braunwald’s Heart Disease 2012
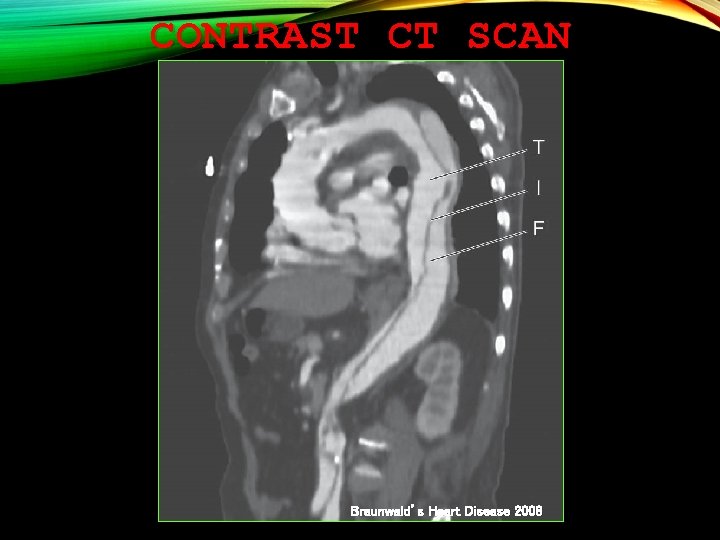
CONTRAST CT SCAN Braunwald’s Heart Disease 2008
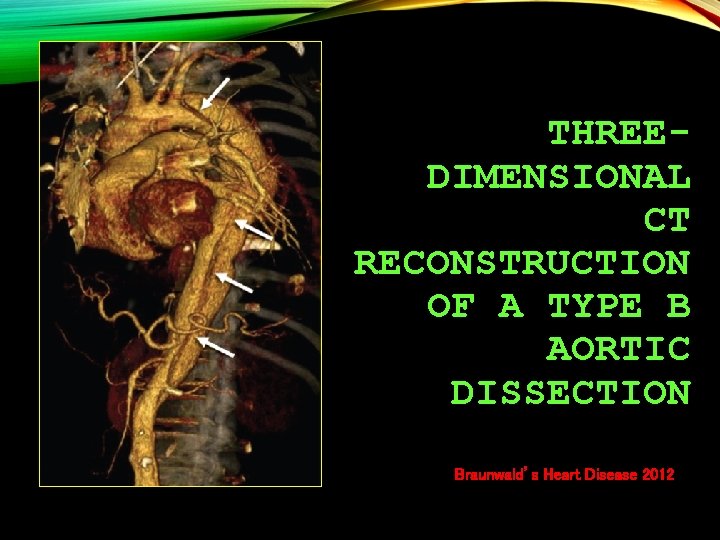
THREEDIMENSIONAL CT RECONSTRUCTION OF A TYPE B AORTIC DISSECTION Braunwald’s Heart Disease 2012
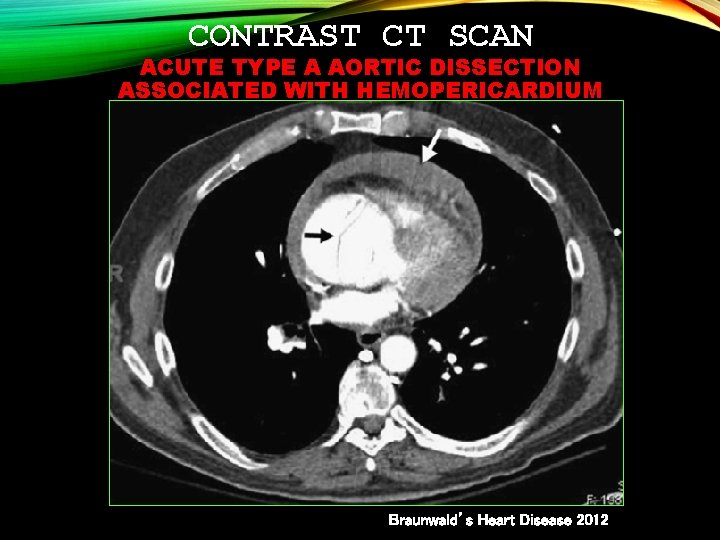
CONTRAST CT SCAN ACUTE TYPE A AORTIC DISSECTION ASSOCIATED WITH HEMOPERICARDIUM Braunwald’s Heart Disease 2012
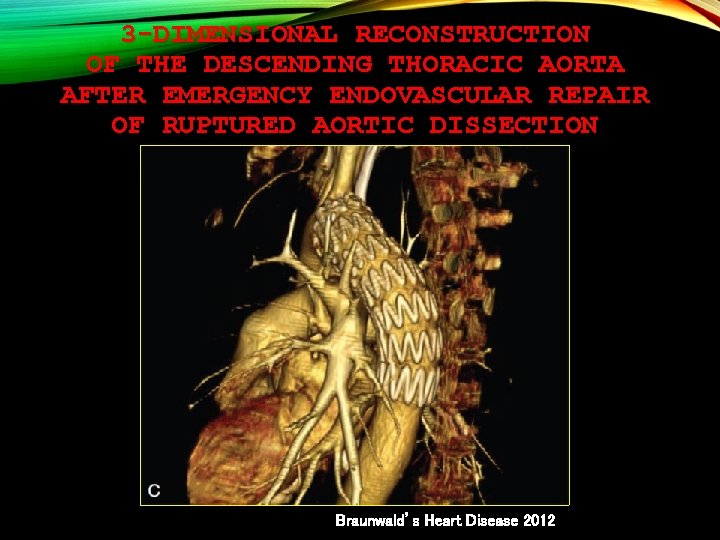
3 -DIMENSIONAL RECONSTRUCTION OF THE DESCENDING THORACIC AORTA AFTER EMERGENCY ENDOVASCULAR REPAIR OF RUPTURED AORTIC DISSECTION Braunwald’s Heart Disease 2012
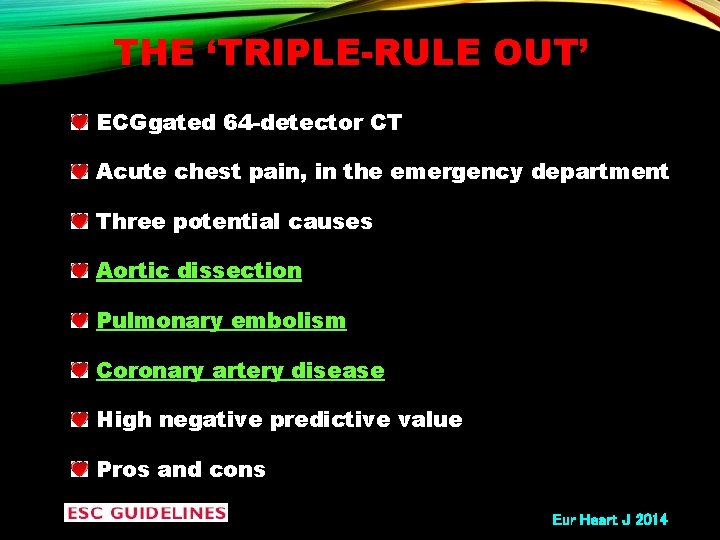
THE ‘TRIPLE-RULE OUT’ ECGgated 64 -detector CT Acute chest pain, in the emergency department Three potential causes Aortic dissection Pulmonary embolism Coronary artery disease High negative predictive value Pros and cons Eur Heart J 2014
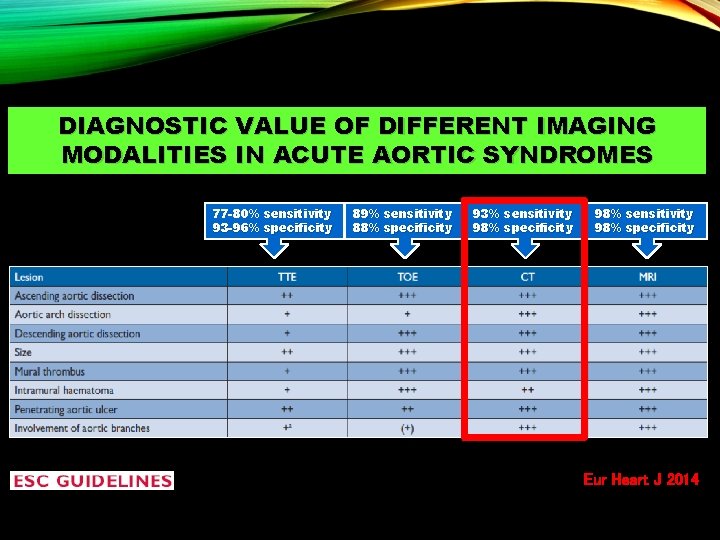
DIAGNOSTIC VALUE OF DIFFERENT IMAGING MODALITIES IN ACUTE AORTIC SYNDROMES 77 -80% sensitivity 93 -96% specificity 89% sensitivity 88% specificity 93% sensitivity 98% specificity 98% sensitivity 98% specificity Eur Heart J 2014
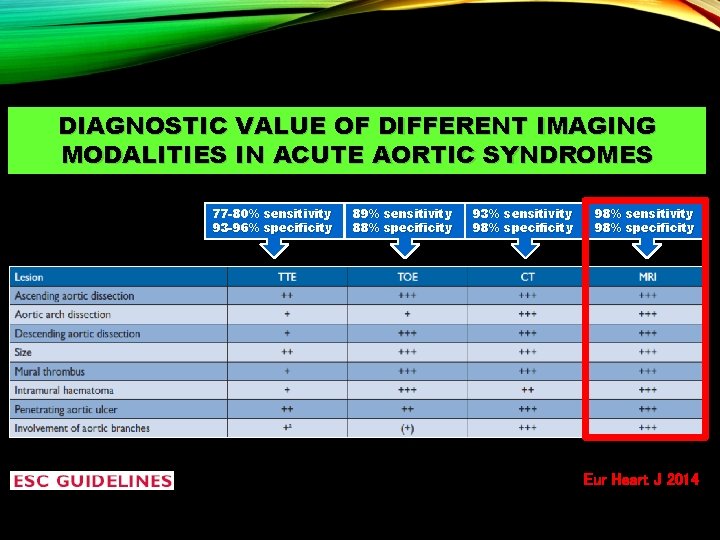
DIAGNOSTIC VALUE OF DIFFERENT IMAGING MODALITIES IN ACUTE AORTIC SYNDROMES 77 -80% sensitivity 93 -96% specificity 89% sensitivity 88% specificity 93% sensitivity 98% specificity 98% sensitivity 98% specificity Eur Heart J 2014
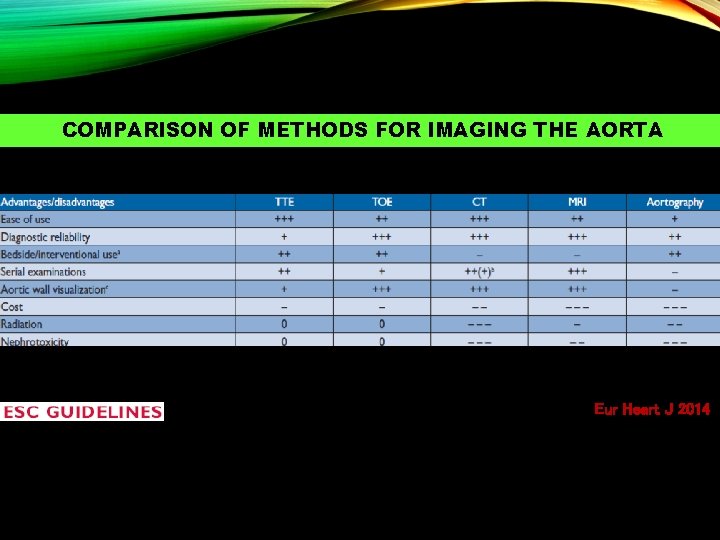
COMPARISON OF METHODS FOR IMAGING THE AORTA Eur Heart J 2014
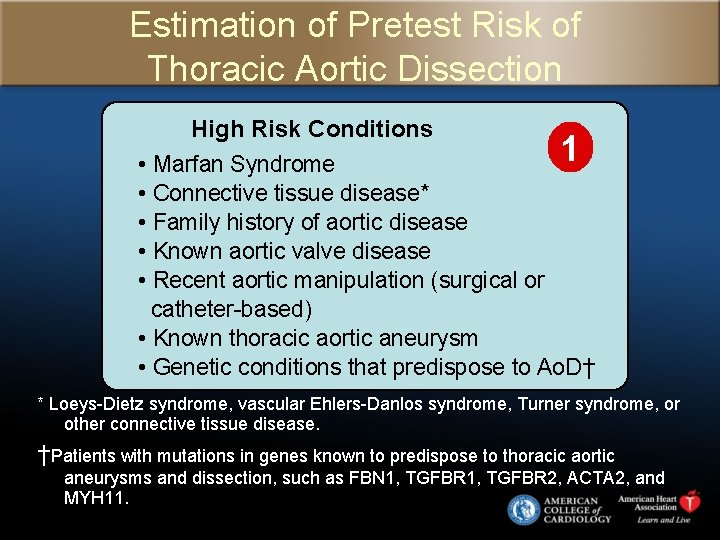
Estimation of Pretest Risk of Thoracic Aortic Dissection High Risk Conditions 1 • Marfan Syndrome • Connective tissue disease* • Family history of aortic disease • Known aortic valve disease • Recent aortic manipulation (surgical or catheter-based) • Known thoracic aortic aneurysm • Genetic conditions that predispose to Ao. D† * Loeys-Dietz syndrome, vascular Ehlers-Danlos syndrome, Turner syndrome, or other connective tissue disease. †Patients with mutations in genes known to predispose to thoracic aortic aneurysms and dissection, such as FBN 1, TGFBR 2, ACTA 2, and MYH 11.
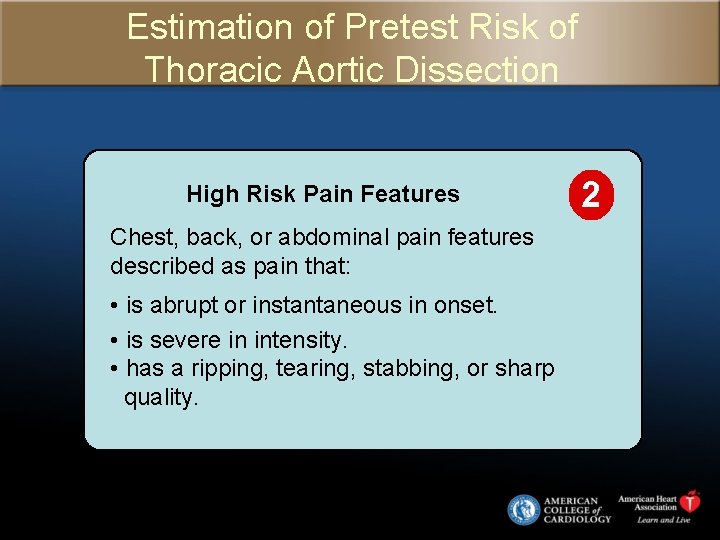
Estimation of Pretest Risk of Thoracic Aortic Dissection High Risk Pain Features Chest, back, or abdominal pain features described as pain that: • is abrupt or instantaneous in onset. • is severe in intensity. • has a ripping, tearing, stabbing, or sharp quality. 2
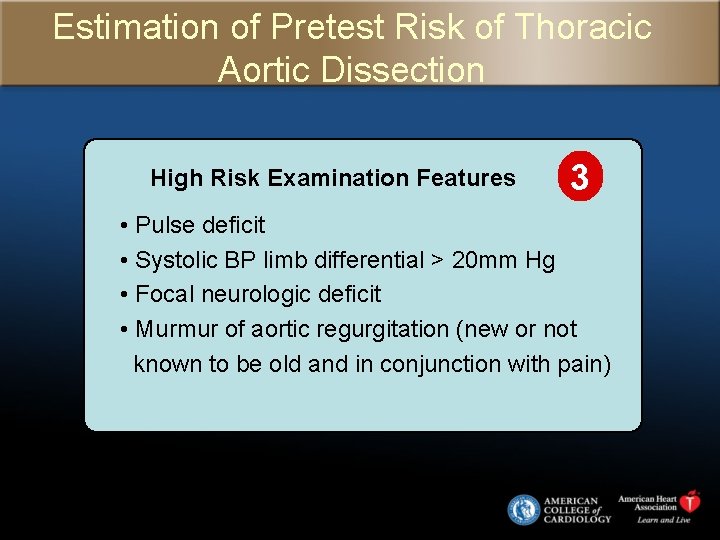
Estimation of Pretest Risk of Thoracic Aortic Dissection High Risk Examination Features 3 • Pulse deficit • Systolic BP limb differential > 20 mm Hg • Focal neurologic deficit • Murmur of aortic regurgitation (new or not known to be old and in conjunction with pain)
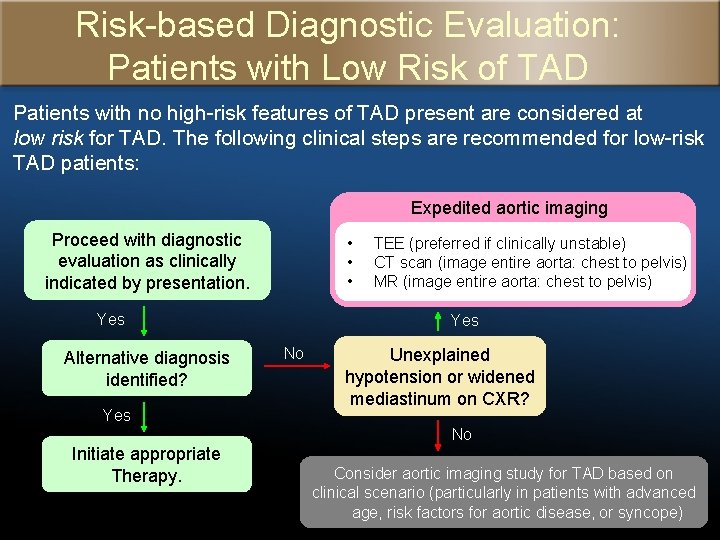
Risk-based Diagnostic Evaluation: Patients with Low Risk of TAD Patients with no high-risk features of TAD present are considered at low risk for TAD. The following clinical steps are recommended for low-risk TAD patients: Expedited aortic imaging Proceed with diagnostic evaluation as clinically indicated by presentation. • • • Yes Alternative diagnosis identified? Yes TEE (preferred if clinically unstable) CT scan (image entire aorta: chest to pelvis) MR (image entire aorta: chest to pelvis) Yes No Unexplained hypotension or widened mediastinum on CXR? No Initiate appropriate Therapy. Consider aortic imaging study for TAD based on clinical scenario (particularly in patients with advanced age, risk factors for aortic disease, or syncope)
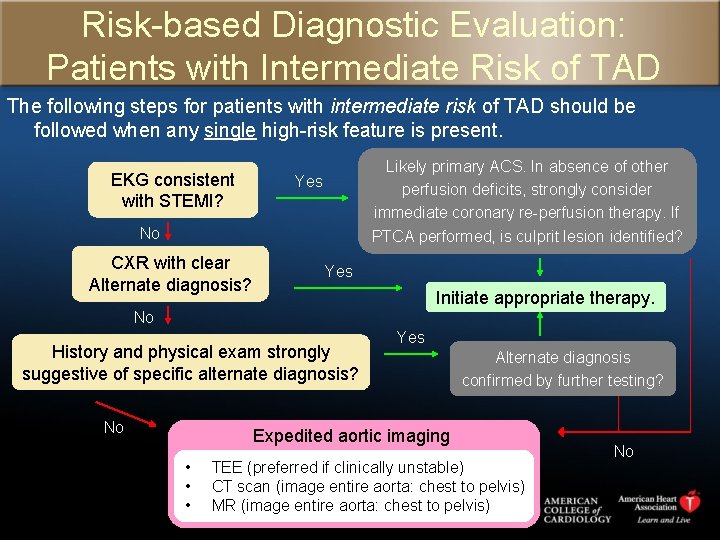
Risk-based Diagnostic Evaluation: Patients with Intermediate Risk of TAD The following steps for patients with intermediate risk of TAD should be followed when any single high-risk feature is present. EKG consistent with STEMI? Likely primary ACS. In absence of other perfusion deficits, strongly consider immediate coronary re-perfusion therapy. If PTCA performed, is culprit lesion identified? Yes No CXR with clear Alternate diagnosis? Yes Initiate appropriate therapy. No History and physical exam strongly suggestive of specific alternate diagnosis? No Yes Alternate diagnosis confirmed by further testing? Expedited aortic imaging • • • TEE (preferred if clinically unstable) CT scan (image entire aorta: chest to pelvis) MR (image entire aorta: chest to pelvis) No

Risk-based Diagnostic Evaluation: Patients with High Risk of TAD Patients at high-risk for TAD are those that present with at least 2 high-risk features (outlined in more detail in the following slides). The recommended course of action for high-risk TAD patients is to seek immediate surgical consultation and arrange for expedited aortic imaging. Expedited aortic imaging • • • TEE (preferred if clinically unstable) CT scan (image entire aorta: chest to pelvis) MR (image entire aorta: chest to pelvis)
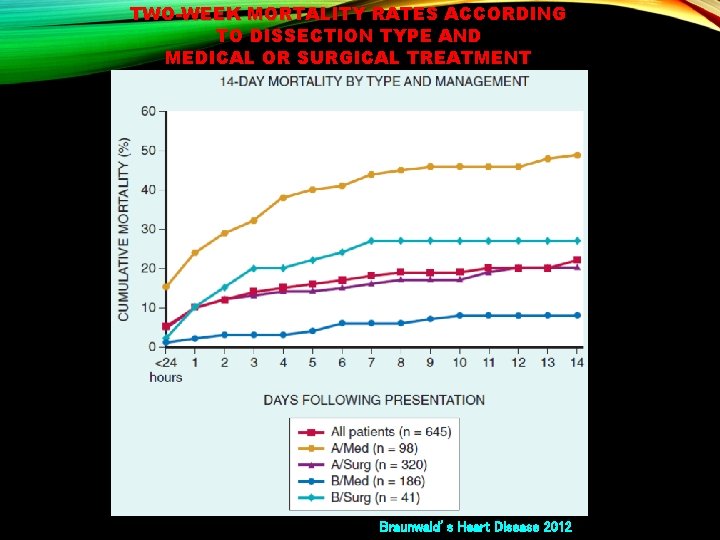
TWO-WEEK MORTALITY RATES ACCORDING TO DISSECTION TYPE AND MEDICAL OR SURGICAL TREATMENT Braunwald’s Heart Disease 2012
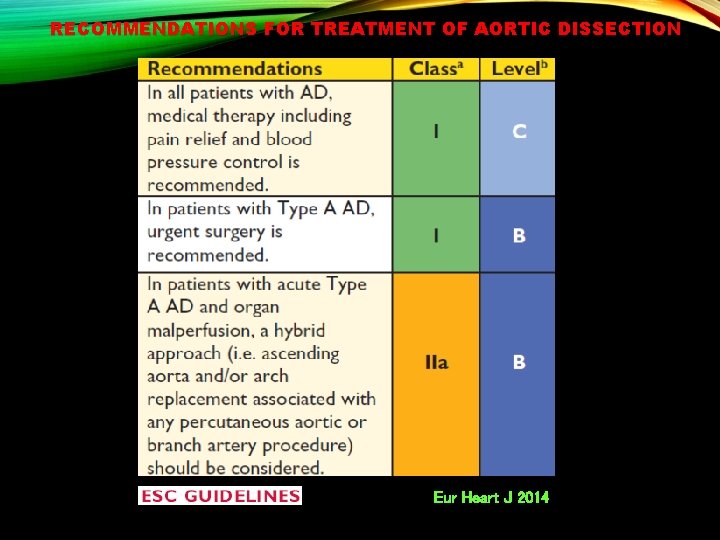
RECOMMENDATIONS FOR TREATMENT OF AORTIC DISSECTION Eur Heart J 2014
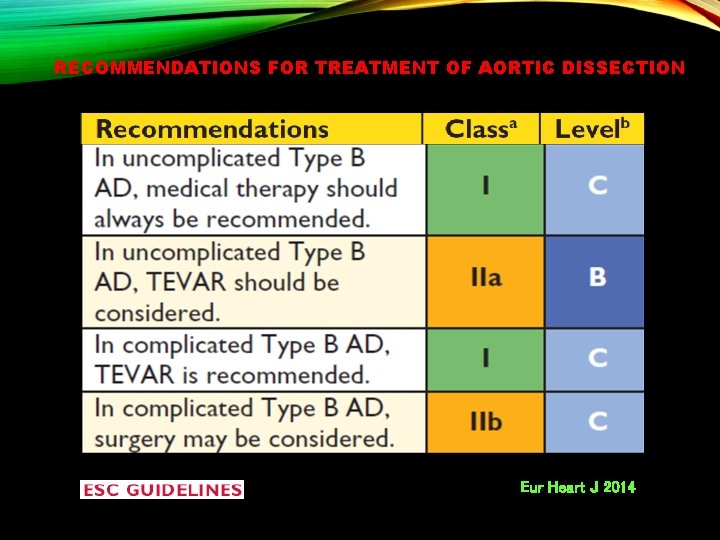
RECOMMENDATIONS FOR TREATMENT OF AORTIC DISSECTION Eur Heart J 2014
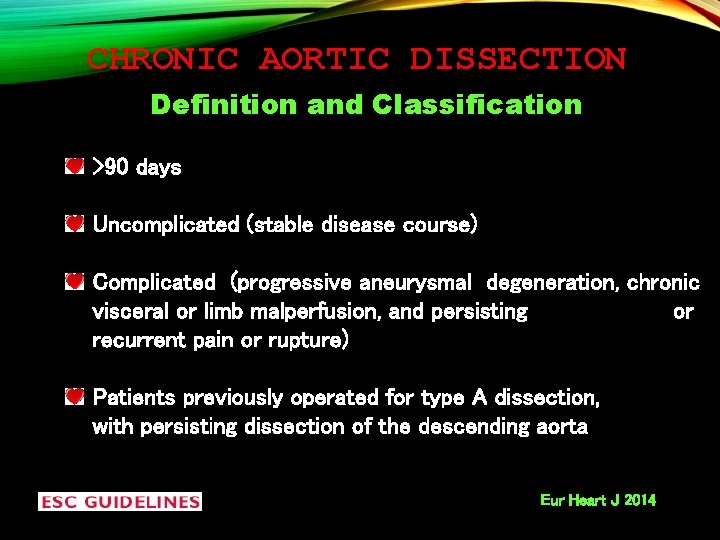
CHRONIC AORTIC DISSECTION Definition and Classification >90 days Uncomplicated (stable disease course) Complicated (progressive aneurysmal degeneration, chronic visceral or limb malperfusion, and persisting or recurrent pain or rupture) Patients previously operated for type A dissection, with persisting dissection of the descending aorta Eur Heart J 2014

CHRONIC AORTIC DISSECTION Presentation Patients with initially acute AD entering the chronic phase of the disease Patients in whom first diagnosis of chronic AD is made Patients with newly diagnosed chronic AD are often asymptomatic Mediastinal widening or prominent aortic knob on chest X-ray Infrequently, symptoms related to the enlarging dissected aorta (hoarseness, new onset chest pain), or chronic malperfusion (abdominal pain, claudication, altered renal function) Eur Heart J 2014
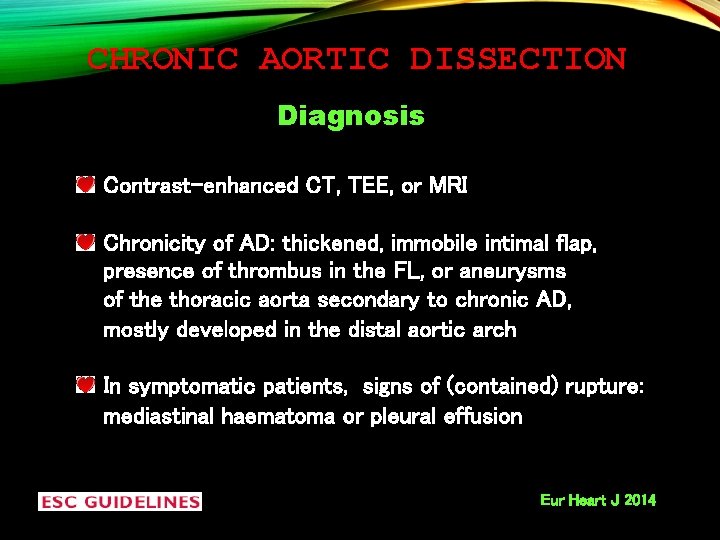
CHRONIC AORTIC DISSECTION Diagnosis Contrast-enhanced CT, TEE, or MRI Chronicity of AD: thickened, immobile intimal flap, presence of thrombus in the FL, or aneurysms of the thoracic aorta secondary to chronic AD, mostly developed in the distal aortic arch In symptomatic patients, signs of (contained) rupture: mediastinal haematoma or pleural effusion Eur Heart J 2014
CHRONIC AORTIC DISSECTION Treatment Chronic, uncomplicated type B AD: medical therapy and repetitive clinical and imaging follow-up Beta-blockers No survival benefit of TEVAR over optimal medical therapy in patients with asymptomatic sub-acute/chronic AD Chronic type B AD complicated by progressive thoracic aortic enlargement (>10 mm/year), FL aneurysms (diameter >60 mm), malperfusion syndrome, or recurrent pain, require TEVAR or surgical treatment Eur Heart J 2014
TAKE HOME MESSAGES High risk features to assess the a priori probability of acute aortic syndrome Expedited aortic imaging CT/MRI (image entire aorta: chest to pelvis) TEE preferred for unstable patients
- Slides: 56