Actionable Insights to Operational Excellence Clinical Variation Reduction
Actionable Insights to Operational Excellence Clinical Variation Reduction 6 th Biennial HIMSS Northwest Fall Conference October 15, 2018
“We are challenged by change, but excited to attack the future with great purpose” Pete Carroll Head Coach, Seattle Seahawks 2
Agenda Setting the Stage Case Studies Questions / Discussion 3
Healthcare – Past The first hospital in the United States was the brain child of Benjamin Franklin and Dr. Thomas Bond. Together they “conceived the idea of establishing a hospital in Philadelphia for the reception and cure of poor sick persons. " History of Pennsylvania Hospital, Penn Medicine 4
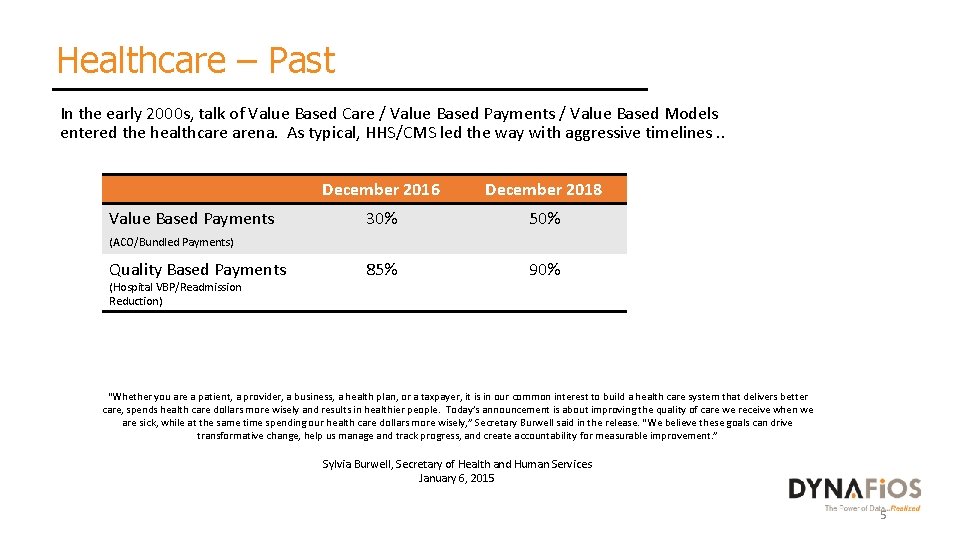
Healthcare – Past In the early 2000 s, talk of Value Based Care / Value Based Payments / Value Based Models entered the healthcare arena. As typical, HHS/CMS led the way with aggressive timelines. . December 2016 December 2018 Value Based Payments (ACO/Bundled Payments) 30% 50% Quality Based Payments 85% 90% (Hospital VBP/Readmission Reduction) “Whether you are a patient, a provider, a business, a health plan, or a taxpayer, it is in our common interest to build a health care system that delivers better care, spends health care dollars more wisely and results in healthier people. Today’s announcement is about improving the quality of care we receive when we are sick, while at the same time spending our health care dollars more wisely, ” Secretary Burwell said in the release. “We believe these goals can drive transformative change, help us manage and track progress, and create accountability for measurable improvement. ” Sylvia Burwell, Secretary of Health and Human Services January 6, 2015 5
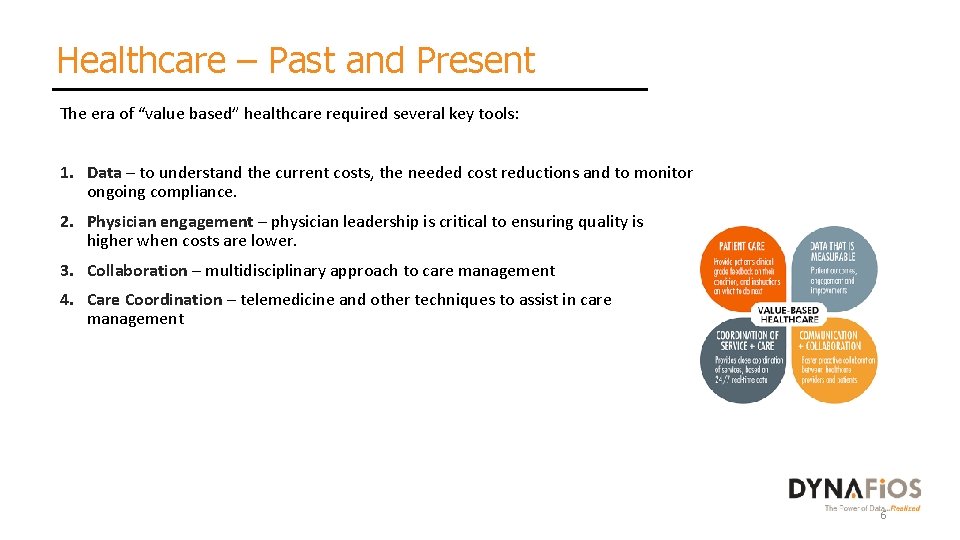
Healthcare – Past and Present The era of “value based” healthcare required several key tools: 1. Data – to understand the current costs, the needed cost reductions and to monitor ongoing compliance. 2. Physician engagement – physician leadership is critical to ensuring quality is higher when costs are lower. 3. Collaboration – multidisciplinary approach to care management 4. Care Coordination – telemedicine and other techniques to assist in care management 6
Healthcare - Future Population Health experts agree … data is critical to the success of your model: "The first component is understanding what you are trying to do with your population health framework, from the standpoint of the health system, and using data to identify and understand the opportunities to be gained, the resources already in place, and your overall strategy of healthcare delivery” Health IT News, August 24, 2016 7
Healthcare - Future According to the Health Research Institute report this month, mega-health systems will continue to be formed and ultimately must place themselves in one of four different models: • Product Leader – Delivering the most advanced care and best outcomes • Experience Leader – Achieving the greatest customer satisfaction • Integrator – Integrator Emphasizing value by having the greatest scope and scale • Health Manager – Improving the health of entire populations over time While care delivery represents two-thirds of the $3 trillion healthcare market annually, growth is expected to shift away from care delivery toward wellness, information technology and support services, according to an analysis by Pw. C’s Health Research Institute (HRI). Provider systems of the future: What happens when the hospital is no longer the center of the health universe? Pw. C Health Research Institute, October 2018 8
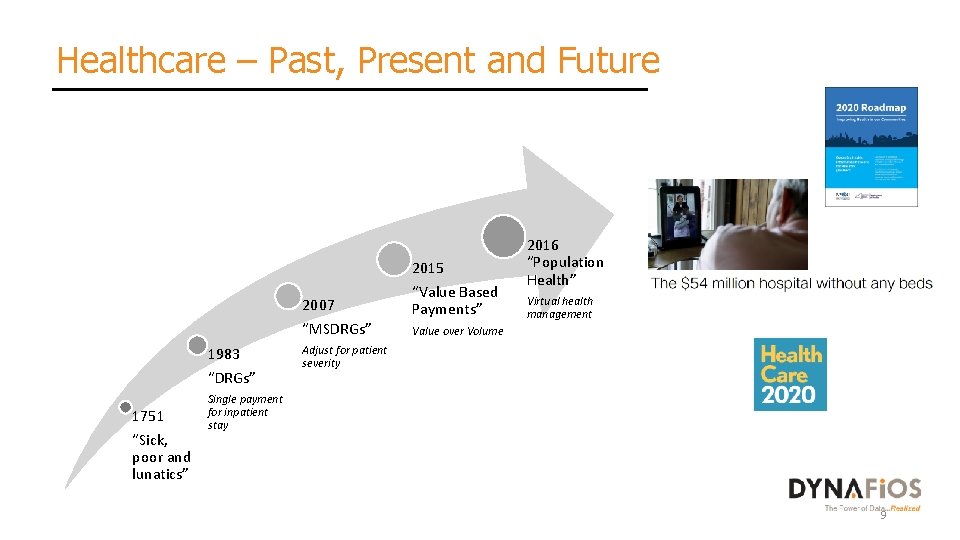
Healthcare – Past, Present and Future 2007 “MSDRGs” 1983 “DRGs” 1751 “Sick, poor and lunatics” 2015 “Value Based Payments” 2016 “Population Health” Virtual health management Value over Volume Adjust for patient severity Single payment for inpatient stay 9
Healthcare – Present and Future 10
Actionable Insights According to the most recent Advisory Board survey, 62% of CEOs are concerned about sustainable cost savings through the reduction of clinical variation. 11
Actionable Insights “Great insights are achieved when you combine different data sources. ” Mark van Rijmenam, International Speaker and Expert in Disruptive Innovation 12
Actionable Insights “Real time data (Analytics) isn’t just a good idea, it is a necessity. ” Gil Allouche, CEO Metadata. io 13
Actionable Insights 14
Actionable Insights Successful clinical reduction initiatives require: ØDisparate data in a single analytics platform ØReal time monitoring and access to the analyzed data ØPhysician leadership and involvement (not just engagement) Now let’s talk about real situations…… 15
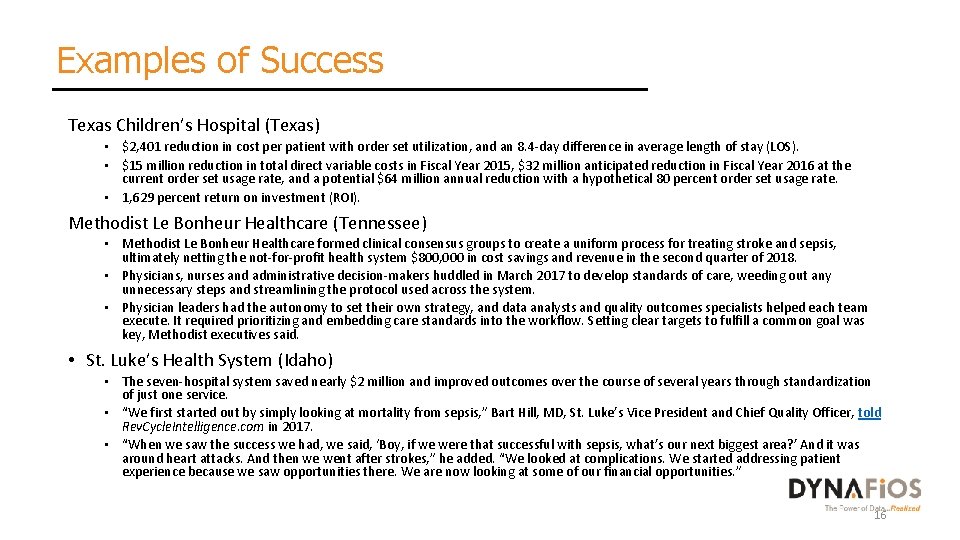
Examples of Success Texas Children’s Hospital (Texas) • $2, 401 reduction in cost per patient with order set utilization, and an 8. 4 -day difference in average length of stay (LOS). • $15 million reduction in total direct variable costs in Fiscal Year 2015, $32 million anticipated reduction in Fiscal Year 2016 at the current order set usage rate, and a potential $64 million annual reduction with a hypothetical 80 percent order set usage rate. • 1, 629 percent return on investment (ROI). Methodist Le Bonheur Healthcare (Tennessee) • Methodist Le Bonheur Healthcare formed clinical consensus groups to create a uniform process for treating stroke and sepsis, ultimately netting the not-for-profit health system $800, 000 in cost savings and revenue in the second quarter of 2018. • Physicians, nurses and administrative decision-makers huddled in March 2017 to develop standards of care, weeding out any unnecessary steps and streamlining the protocol used across the system. • Physician leaders had the autonomy to set their own strategy, and data analysts and quality outcomes specialists helped each team execute. It required prioritizing and embedding care standards into the workflow. Setting clear targets to fulfill a common goal was key, Methodist executives said. • St. Luke’s Health System (Idaho) • The seven-hospital system saved nearly $2 million and improved outcomes over the course of several years through standardization of just one service. • “We first started out by simply looking at mortality from sepsis, ” Bart Hill, MD, St. Luke’s Vice President and Chief Quality Officer, told Rev. Cycle. Intelligence. com in 2017. • “When we saw the success we had, we said, ‘Boy, if we were that successful with sepsis, what’s our next biggest area? ’ And it was around heart attacks. And then we went after strokes, ” he added. “We looked at complications. We started addressing patient experience because we saw opportunities there. We are now looking at some of our financial opportunities. ” 16
Case Study – Midwestern Hospital Strategic Intent – Identify opportunities for clinical variation reduction throughout the hospital Background • 170 bed hospital in Midwest providing medical, surgical and specialty services. • New hospital leadership wanting to understand opportunities for engaging the physicians and reducing costs. Process 1. Obtain and analyze patient encounter and charge detail data. 2. Benchmark performance internally and to the overall health system. 3. Present opportunities to physician and hospital leadership to determine a course of action. 4. Implement plans to improve performance, measuring performance on a monthly basis. 17
Case Study – Midwestern Hospital Overview of the Major Programs within the hospital Cardiovascular Program PCI program has grown year over year, and contribution margin increased by 232%. . ($2217) to $2921. Medicaid volume is down by 2% and replaced with Medicare and Managed Care payor group which is up 5%. Contribution margin from a $200 K loss to a $400 K positive. Orthopedic Program Total joints has seen market growth from the Dover and Atkins area with loss in Russelville and Clarksville. General Surgery Direct costs are up by 9% with no increased complexity of patients. General Medicine Septicemia is the largest volume within the program and has grown 32 cases. Medicare PPS has decreased and Medicaid has grown. Direct cost per case is up by 6% driven by length of stay and supply management. 18
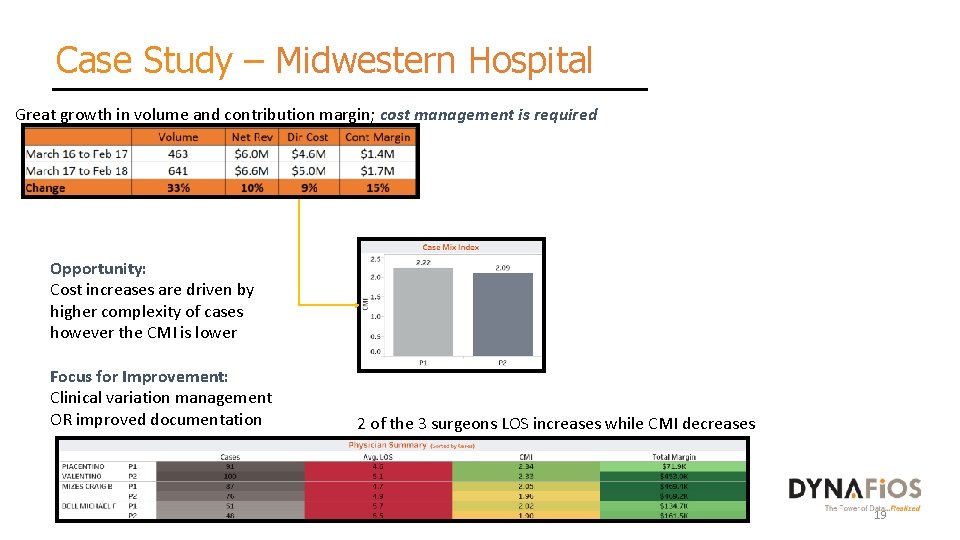
Case Study – Midwestern Hospital Great growth in volume and contribution margin; cost management is required Opportunity: Cost increases are driven by higher complexity of cases however the CMI is lower Focus for Improvement: Clinical variation management OR improved documentation 2 of the 3 surgeons LOS increases while CMI decreases 19
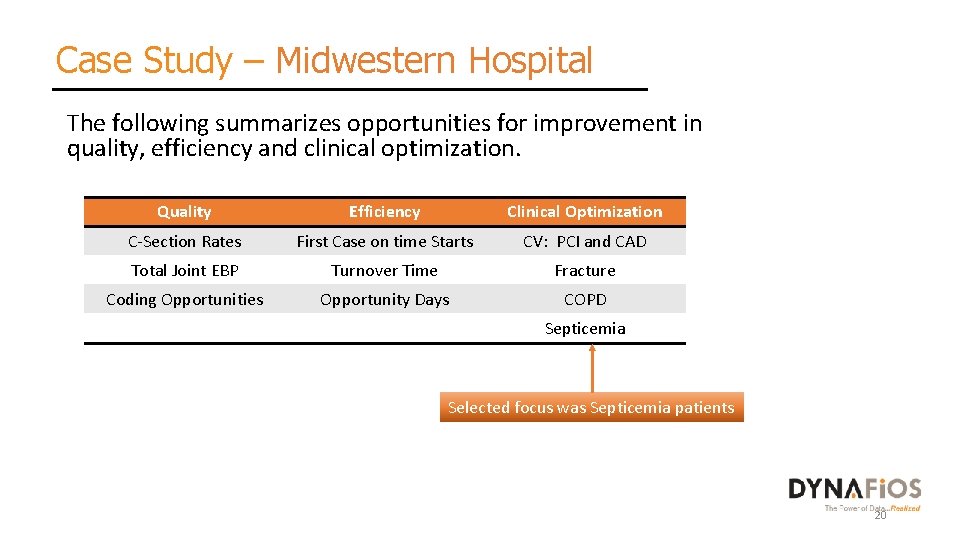
Case Study – Midwestern Hospital The following summarizes opportunities for improvement in quality, efficiency and clinical optimization. Quality Efficiency Clinical Optimization C-Section Rates First Case on time Starts CV: PCI and CAD Total Joint EBP Turnover Time Fracture Coding Opportunities Opportunity Days COPD Septicemia Selected focus was Septicemia patients 20
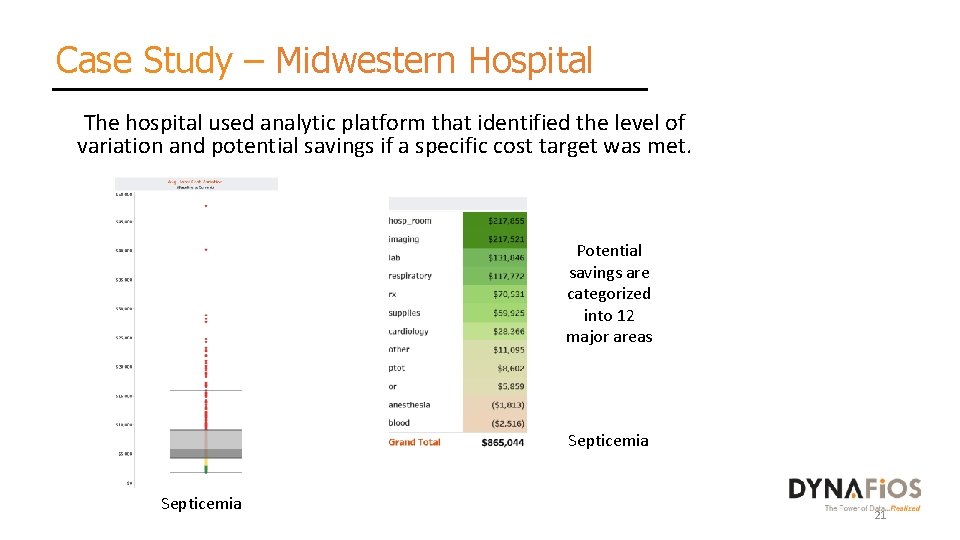
Case Study – Midwestern Hospital The hospital used analytic platform that identified the level of variation and potential savings if a specific cost target was met. Potential savings are categorized into 12 major areas Septicemia 21
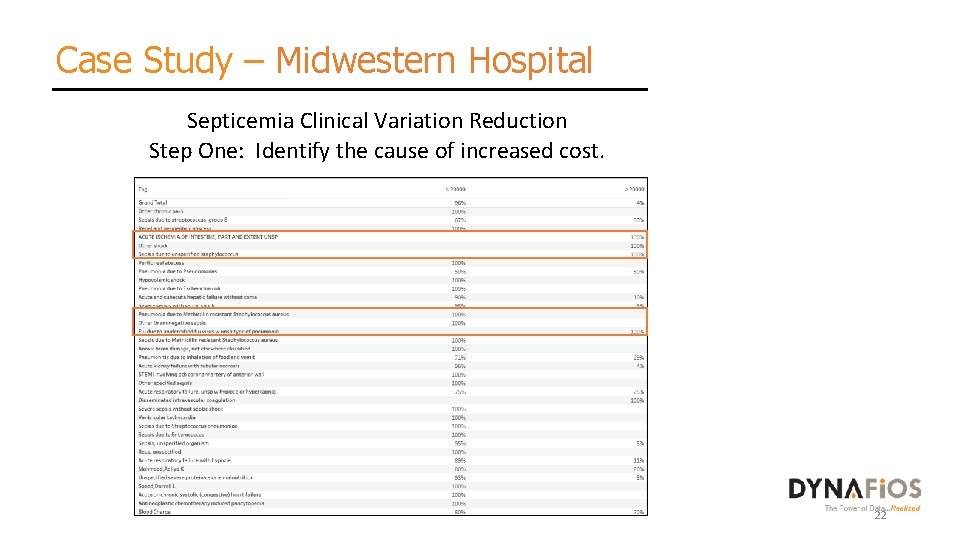
Case Study – Midwestern Hospital Septicemia Clinical Variation Reduction Step One: Identify the cause of increased cost. 22
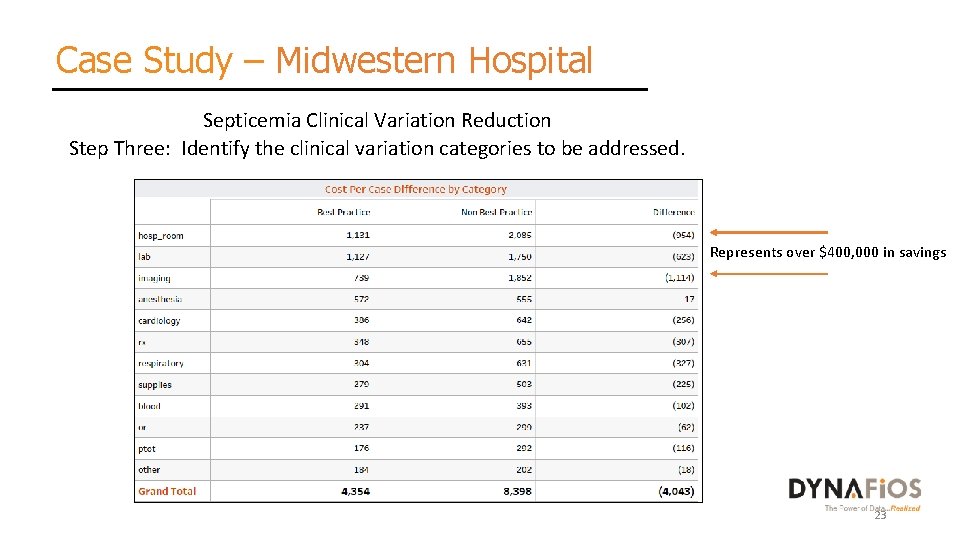
Case Study – Midwestern Hospital Septicemia Clinical Variation Reduction Step Three: Identify the clinical variation categories to be addressed. Represents over $400, 000 in savings 23

Case Study – Midwestern Hospital Septicemia Clinical Variation Reduction Step Four: Identify the cause of increased length of stay. 24
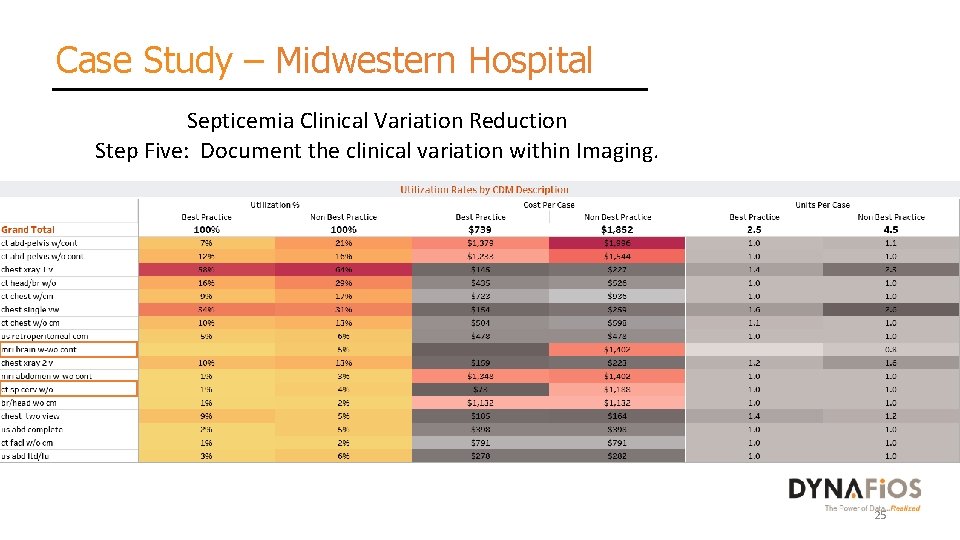
Case Study – Midwestern Hospital Septicemia Clinical Variation Reduction Step Five: Document the clinical variation within Imaging. 25
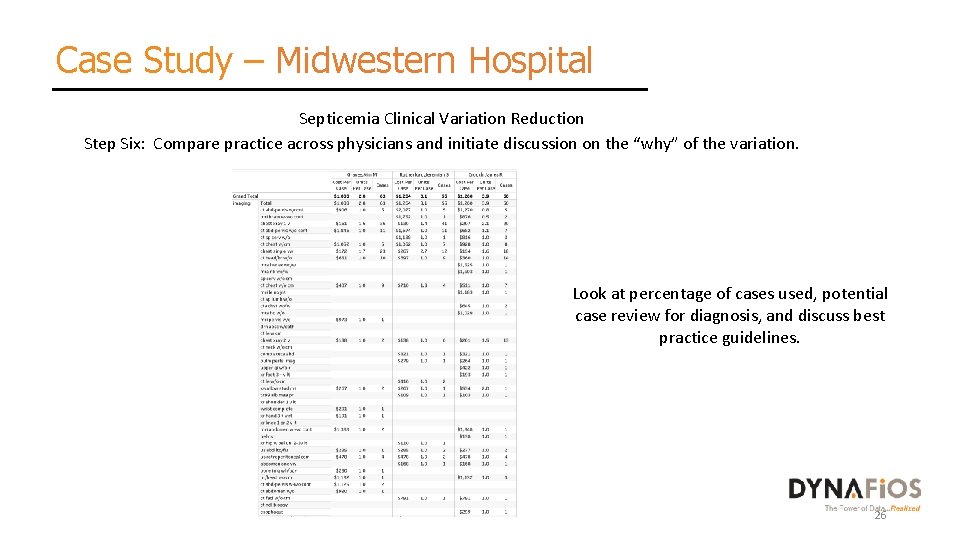
Case Study – Midwestern Hospital Septicemia Clinical Variation Reduction Step Six: Compare practice across physicians and initiate discussion on the “why” of the variation. Look at percentage of cases used, potential case review for diagnosis, and discuss best practice guidelines. 26
Case Study – Midwestern Hospital Results: • Developed best practice pathway identifying the activities by day of stay. • Implemented imaging protocols for MRI and CT • Implemented additional protocols for ER and hospitalists regarding the diagnoses that lead to increased cost and length of stay • Actual savings realized after one year: $800, 000 27
Case Study – Northwest Hospital Strategic Intent – Reduce clinical variation and implement best practices for ortho/spine Background • 107 bed hospital in Northwest providing general medical/surgical and orthopedic/spine surgery. • Hospital and physician practice failed to meet standards for a local payor preferred contract. Process 1. Benchmark program against best practice standards. 2. Identify areas of clinical variation. 3. Implement protocols, order sets, preference cards, etc to drive standardization. 28
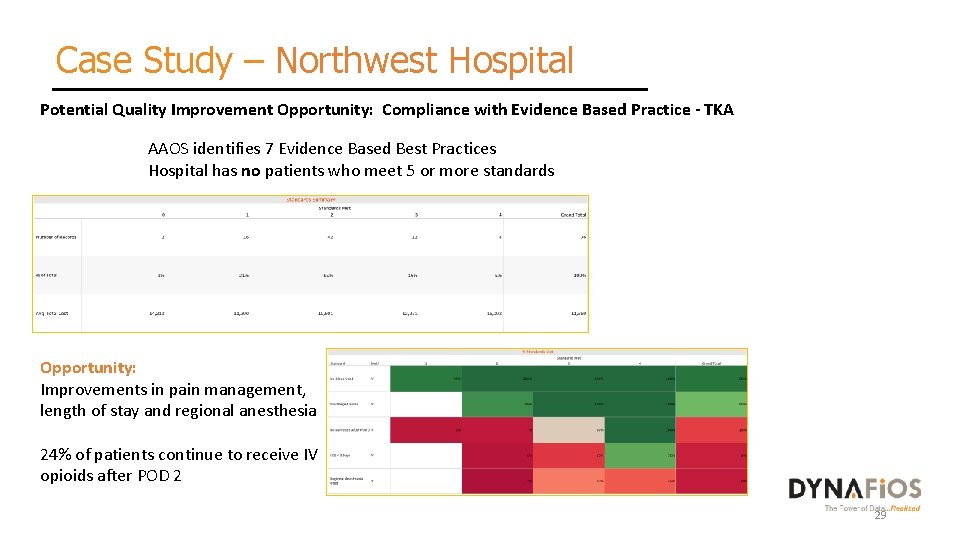
Case Study – Northwest Hospital Potential Quality Improvement Opportunity: Compliance with Evidence Based Practice - TKA AAOS identifies 7 Evidence Based Best Practices Hospital has no patients who meet 5 or more standards Opportunity: Improvements in pain management, length of stay and regional anesthesia 24% of patients continue to receive IV opioids after POD 2 29
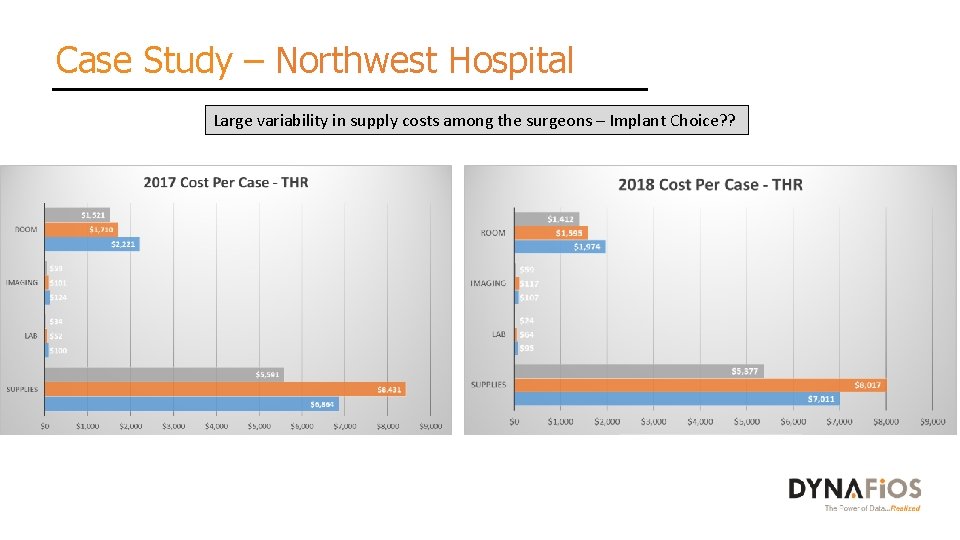
Case Study – Northwest Hospital Large variability in supply costs among the surgeons – Implant Choice? ?
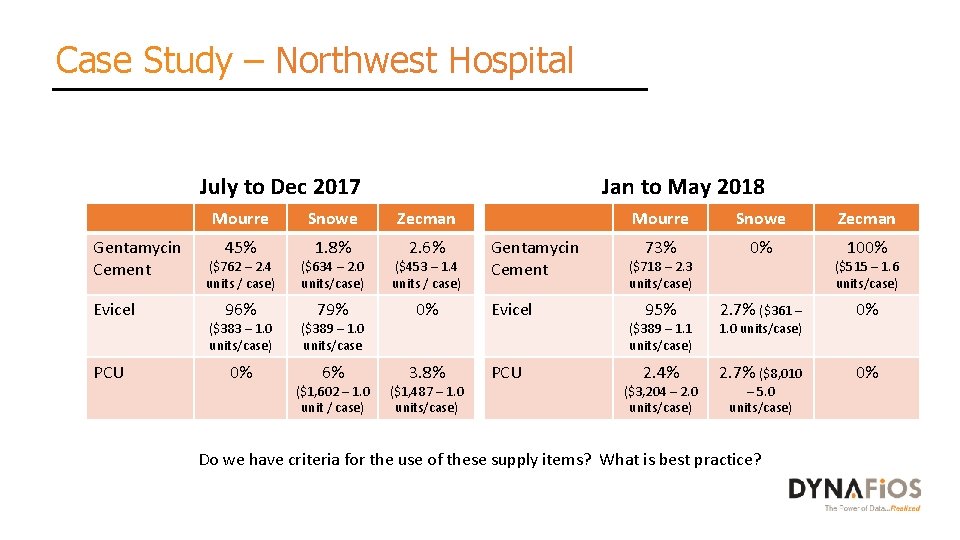
Case Study – Northwest Hospital Jan to May 2018 July to Dec 2017 Mourre Gentamycin Cement Evicel PCU Snowe 45% 1. 8% ($762 – 2. 4 units / case) ($634 – 2. 0 units/case) Mourre Zecman 2. 6% ($453 – 1. 4 units / case) Gentamycin Cement 96% 79% 0% Evicel 0% PCU ($383 – 1. 0 units/case) ($389 – 1. 0 units/case 6% 3. 8% ($1, 602 – 1. 0 unit / case) ($1, 487 – 1. 0 units/case) Snowe 73% ($718 – 2. 3 units/case) 95% 0% Zecman 100% ($515 – 1. 6 units/case) ($389 – 1. 1 units/case) 2. 7% ($361 – 1. 0 units/case) 0% 2. 4% 2. 7% ($8, 010 0% ($3, 204 – 2. 0 units/case) – 5. 0 units/case) Do we have criteria for the use of these supply items? What is best practice?
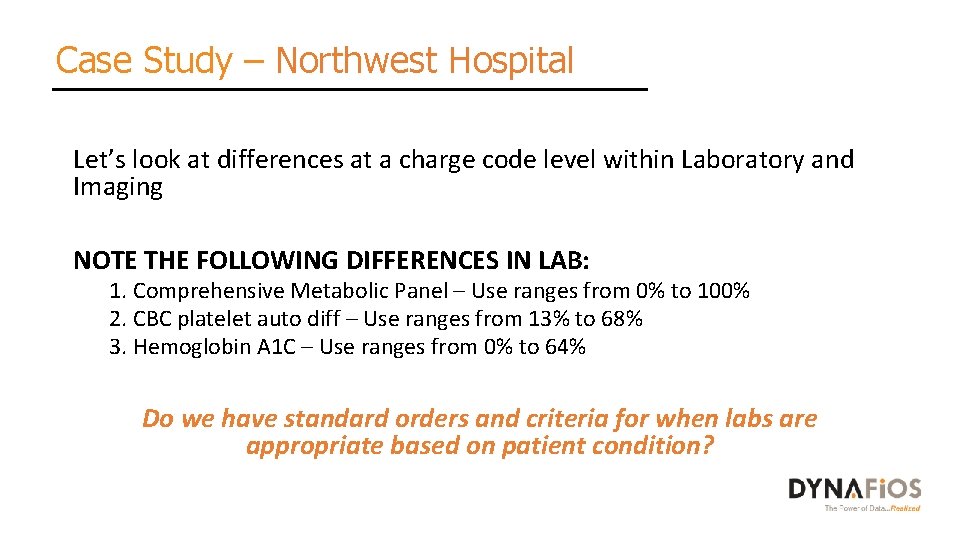
Case Study – Northwest Hospital Let’s look at differences at a charge code level within Laboratory and Imaging NOTE THE FOLLOWING DIFFERENCES IN LAB: 1. Comprehensive Metabolic Panel – Use ranges from 0% to 100% 2. CBC platelet auto diff – Use ranges from 13% to 68% 3. Hemoglobin A 1 C – Use ranges from 0% to 64% Do we have standard orders and criteria for when labs are appropriate based on patient condition?
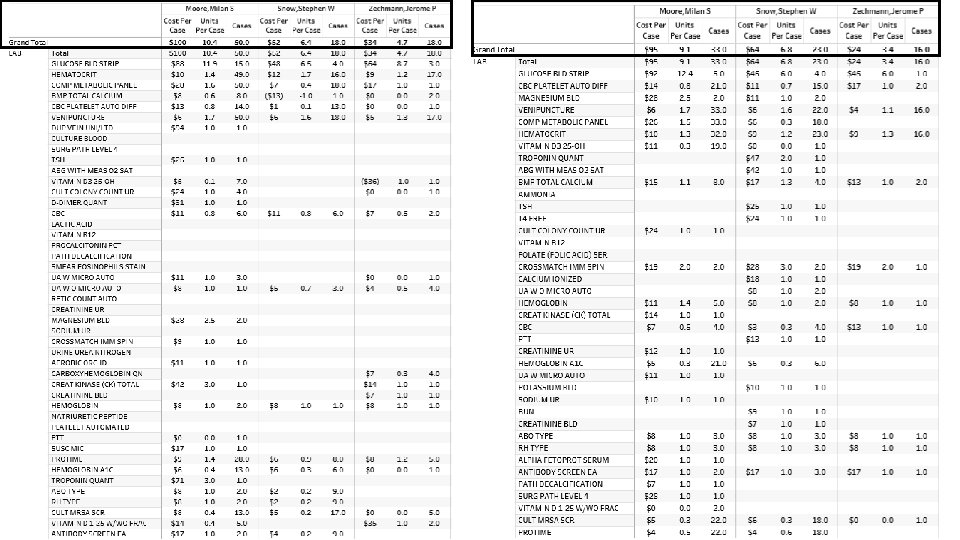
Case Study – Northwest Hospital Let’s look at differences at a charge code level within Laboratory and Imaging NOTE THE FOLLOWING DIFFERENCES IN IMAGING: 1. Frequency of hip x-rays post operatively • Do we have standard orders?
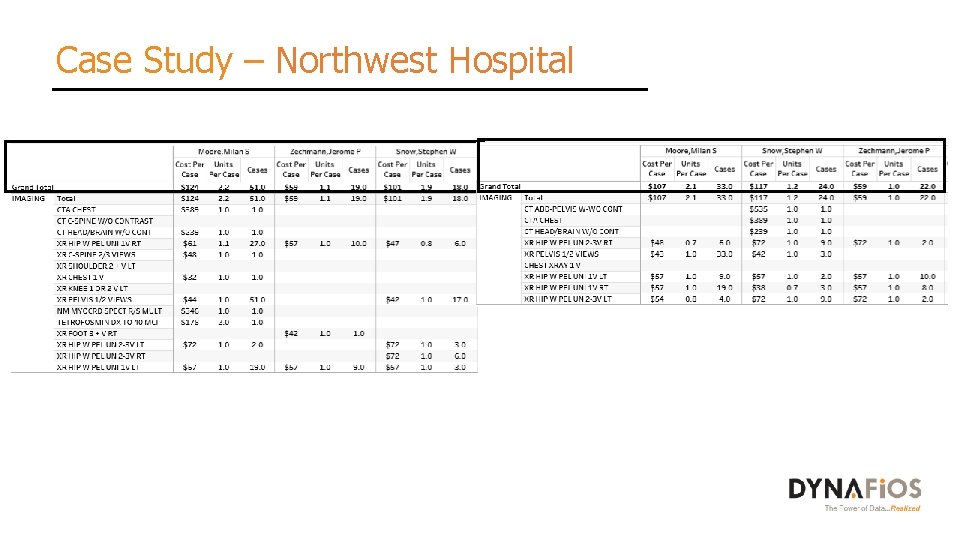
Case Study – Northwest Hospital
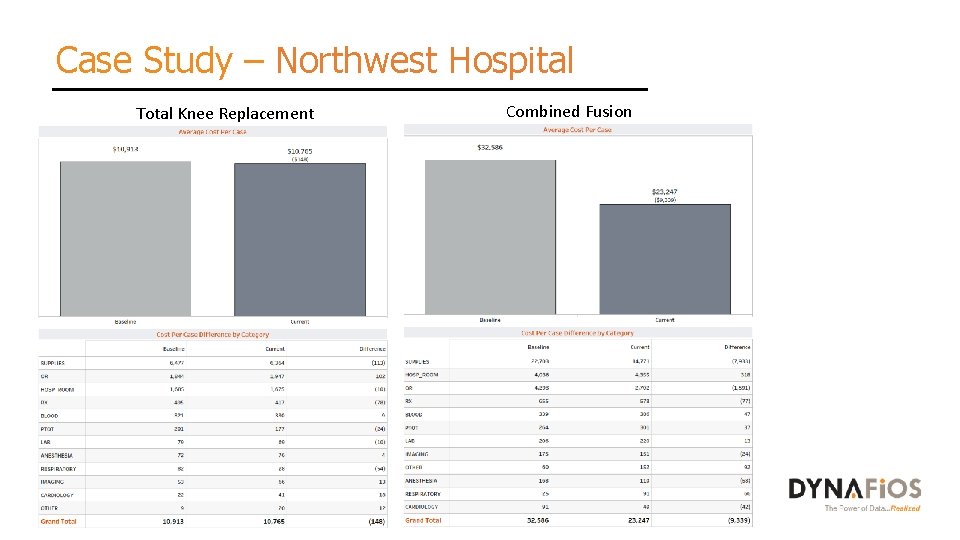
Case Study – Northwest Hospital Total Knee Replacement Combined Fusion
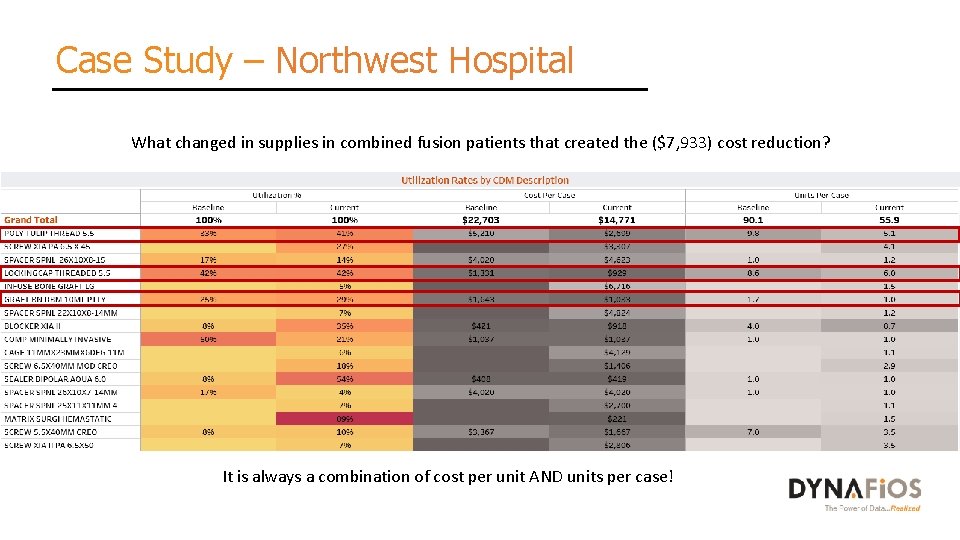
Case Study – Northwest Hospital What changed in supplies in combined fusion patients that created the ($7, 933) cost reduction? It is always a combination of cost per unit AND units per case!
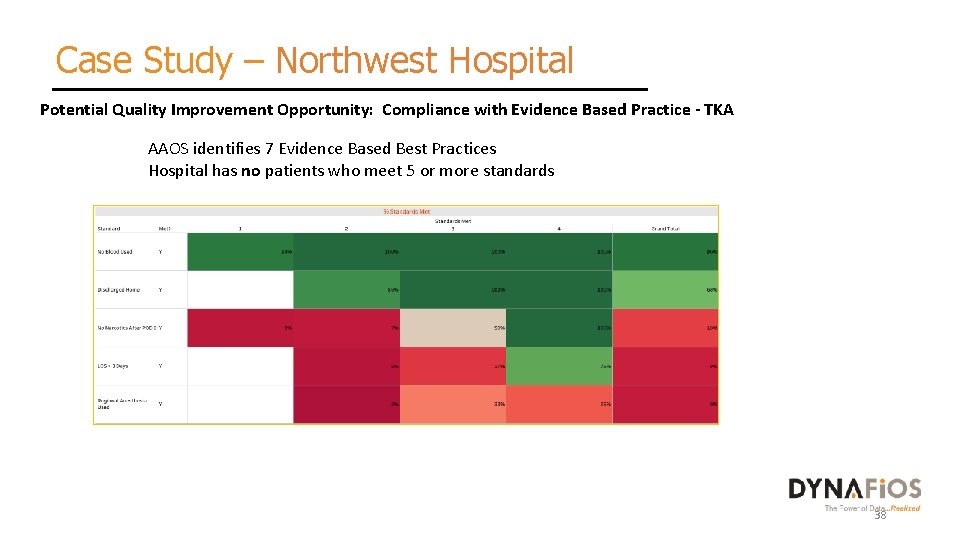
Case Study – Northwest Hospital Potential Quality Improvement Opportunity: Compliance with Evidence Based Practice - TKA AAOS identifies 7 Evidence Based Best Practices Hospital has no patients who meet 5 or more standards 38
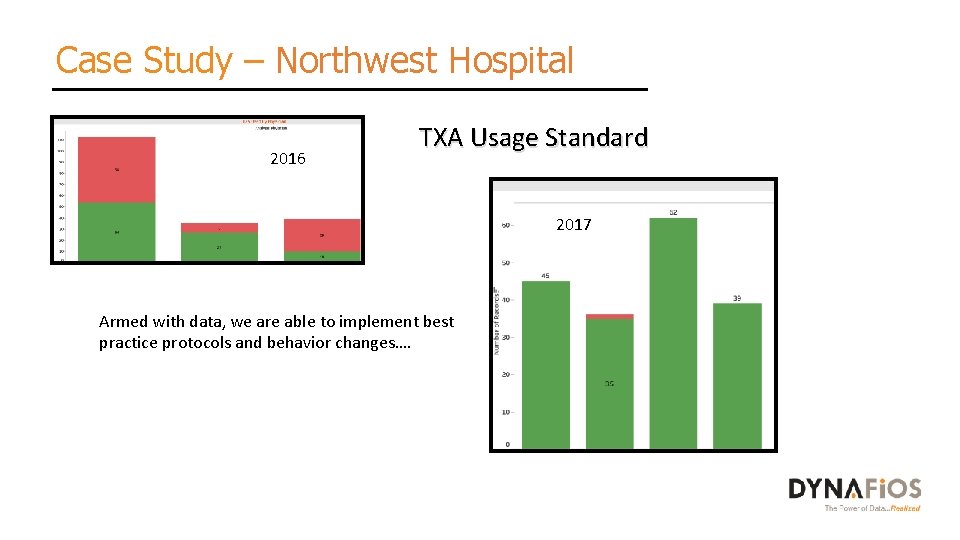
Case Study – Northwest Hospital 2016 TXA Usage Standard 2017 Armed with data, we are able to implement best practice protocols and behavior changes….
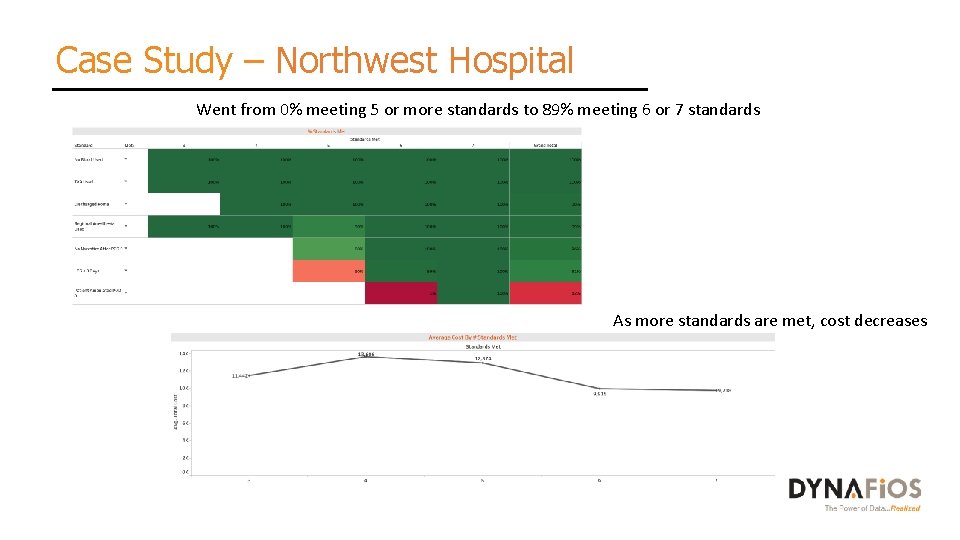
Case Study – Northwest Hospital Went from 0% meeting 5 or more standards to 89% meeting 6 or 7 standards As more standards are met, cost decreases
Case Study – Northwest Hospital Results: • Implemented best practice standards for TJR and saw a corresponding cost reduction. • Standardized supplies for combined fusion resulting in savings. • Implemented best practice standards for the use of antibiotic bone cement and Infuse. • Actual savings realized after one year: $964, 000 41
Actionable Insights 42
Actionable Insights to drive results… 1. Disparate data must be combined to provide care teams with the necessary details to identify, eliminate and monitor improvements. 2. Encounter, charge detail, operational department data (OR, Cath Lab) are critical to the database for improvements. 3. Identify clinical variation to yield both quality and cost improvements through provider engagement. 4. Collaborative structures/teams are critical to provide the venue for data analytics, best practice discussions and monitoring of performance. 5. Individual and collective data analytics should be shared with all the team members…keep visuals simple and actionable! 6. Involvement of physicians and key stakeholders must be real and ongoing. 43
Questions / Discussion Tina R. Brinton, COO Dynafios Email: Tina. Brinton@Dynafios. com Cell phone: 425 -256 -0820 44
- Slides: 44