ACTion An Interdisciplinary Approach to OutpatientBased Transitions of
ACTion: An Interdisciplinary Approach to Outpatient-Based Transitions of Care Mark Gwynne, DO; Sam Weir, MD STFM April 2012
Goals of this session: • Identify the key components of coordinated care transitions • Evaluate the evolution of the CRC (Complex Return Continuity) hospital follow-up visit and PDSA process • Identify evolving roles for outpatient physician-led teams in transitional care • Identify possible applications of the CRC visit or variations in your residency program 2
Transitions of Care: Costs • $17. 4 Billion to Medicare • Medicare Readmission rate = 18% • Patterns of re-hospitalization » 19. 6% within 30 days » 34% within 90 days » 67% within 1 year • Risk of readmission without Primary Care » 50% of readmissions at 30 days had no PCP visit » Timeliness of PCP visit • Timely visit readmit rate = 3% • Not timely re-admit rate = 21% 3
Transitions of Care: Barriers • Coordination/communication with primary care • Availability of discharge summary » 12 -34% at first post-hospital visit » 57 -77% at 4 week visit » Often lack vital information • Often no knowledge of ancillary services • Direct communication occurred 3 -20% of time • Patient self-management skills • Medication errors/Medication reconciliation • Health literacy and impaired cognition • Patients are confused about who to contact with postdischarge questions • 4
Successful transition programs • • Project RED (Boston) Transitional Care Model (Upenn) Care Transitions Program (Coleman, Colorado) Evercare (dually eligible) Kaiser Permanente Chronic Disease Coordination Heart Failure Resource Center (Atlanta) CCNC – Community Care of NC (Medicaid) Cambridge Health Alliance 5
Features of Successful Transition Programs • Pre-discharge: » Medication reconciliation » Structured discharge communication » Patient education • Post-discharge: Less Clear » » Multidisciplinary team approach Patient-centered discharge plans Medication reconciliation Coordination of services (Care Managers) – facilitated communication (PCP) » Education and support – facilitate patient self care methods » Emerging: patient risk stratification 6
CRC (Complex Return Continuity) Visit • Hospital follow-up appointment linked through GE scheduling system » Includes visit with Clinical Pharmacist followed by » Primary Care Provider visit and, if needed, » Care Manager • Goals of implementation » Address common principles of care transitions • Multidisciplinary team, coordination of care, medication reconciliation » Model and teach physician-led team based care » Improve patient centered outcomes, utilization and clinical outcomes 7
UNC Family Medicine Center • • 16, 500 patients 64 PCP’s 50, 000 visits 2010 -2011 PCMH level 3 (2011 standards) • 2100 Inpatient admissions/year
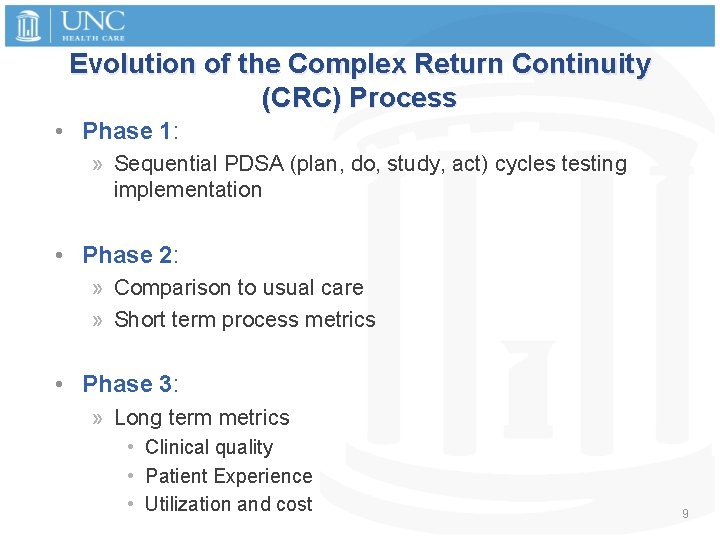
Evolution of the Complex Return Continuity (CRC) Process • Phase 1: » Sequential PDSA (plan, do, study, act) cycles testing implementation • Phase 2: » Comparison to usual care » Short term process metrics • Phase 3: » Long term metrics • Clinical quality • Patient Experience • Utilization and cost 9
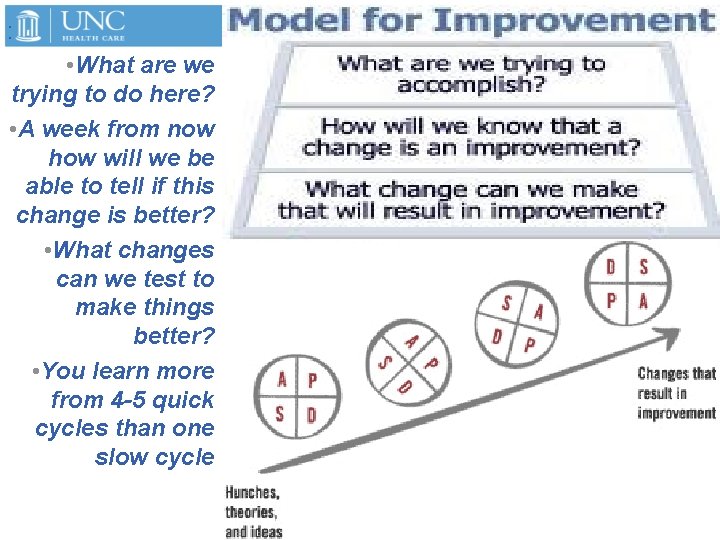
: • What are we trying to do here? • A week from now how will we be able to tell if this change is better? • What changes can we test to make things better? • You learn more from 4 -5 quick cycles than one slow cycle Trick to obscu re Trick to obscu 10
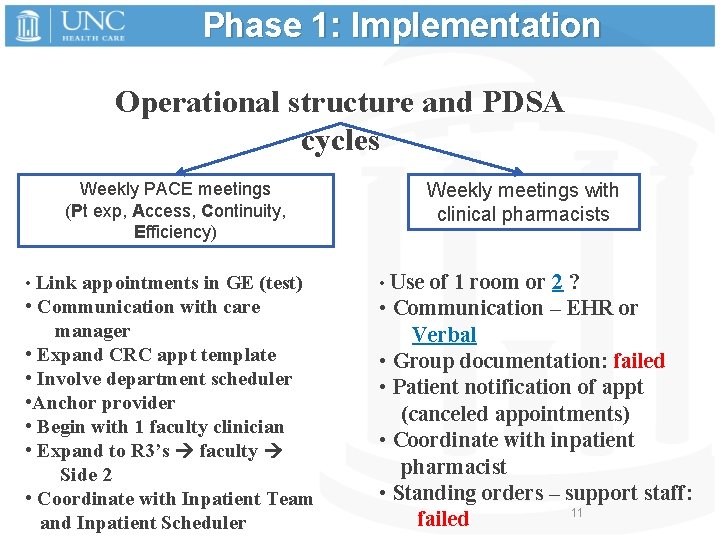
Phase 1: Implementation Operational structure and PDSA cycles Weekly PACE meetings (Pt exp, Access, Continuity, Efficiency) Weekly meetings with clinical pharmacists • Link appointments in GE (test) • Use of 1 room or 2 ? • Communication with care manager • Expand CRC appt template • Involve department scheduler • Anchor provider • Begin with 1 faculty clinician • Expand to R 3’s faculty Side 2 • Coordinate with Inpatient Team and Inpatient Scheduler • Communication – EHR or Verbal • Group documentation: failed • Patient notification of appt (canceled appointments) • Coordinate with inpatient pharmacist • Standing orders – support staff: 11 failed
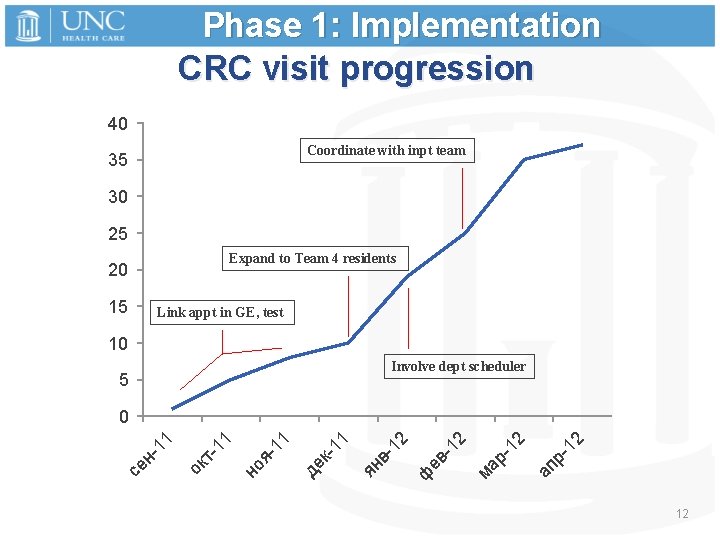
Phase 1: Implementation CRC visit progression 40 Coordinate with inpt team 35 30 25 Expand to Team 4 residents 20 15 Link appt in GE, test 10 Involve dept scheduler 5 -1 2 ап р 12 ма р- ф ев - 12 12 вян 11 де к- 11 яно 11 ток се н- 11 0 12
Q+A: Discussion of PDSA Process? 13
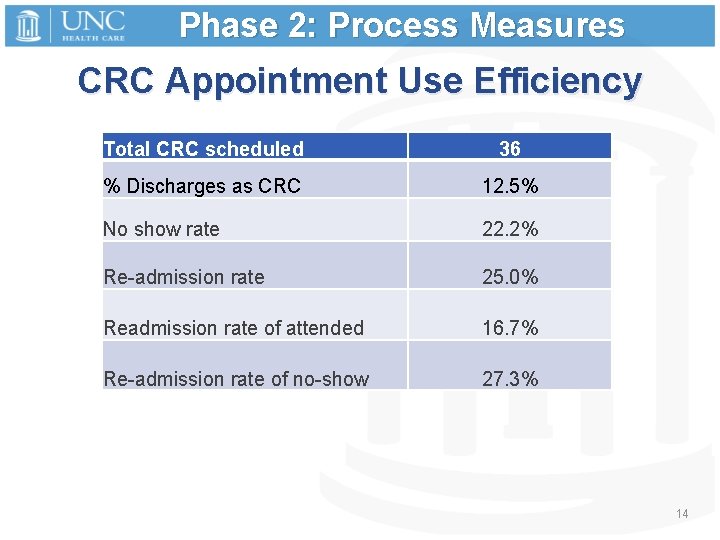
Phase 2: Process Measures CRC Appointment Use Efficiency Total CRC scheduled 36 % Discharges as CRC 12. 5% No show rate 22. 2% Re-admission rate 25. 0% Readmission rate of attended 16. 7% Re-admission rate of no-show 27. 3% 14
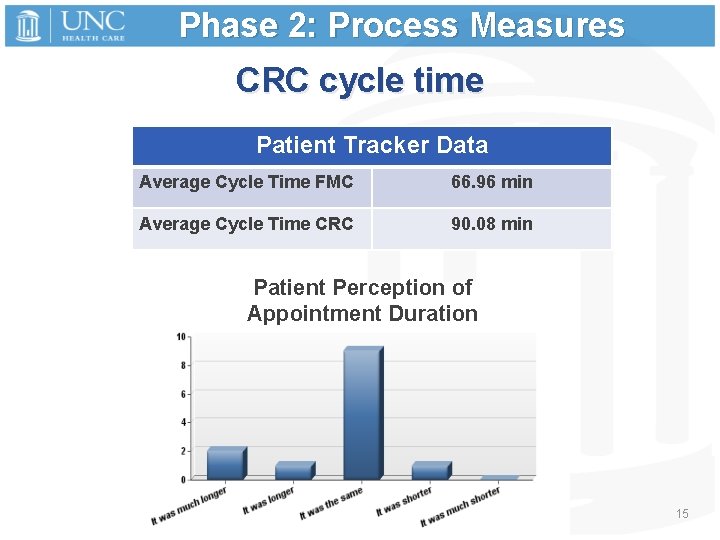
Phase 2: Process Measures CRC cycle time Patient Tracker Data Average Cycle Time FMC 66. 96 min Average Cycle Time CRC 90. 08 min Patient Perception of Appointment Duration 15
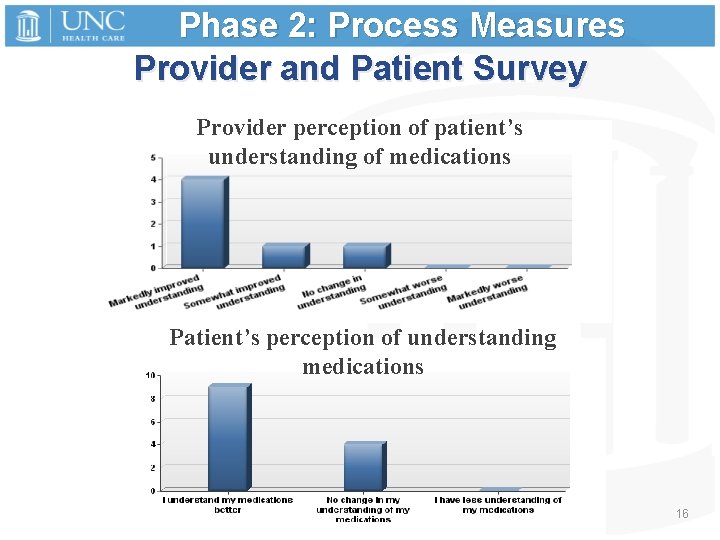
Phase 2: Process Measures Provider and Patient Survey Provider perception of patient’s understanding of medications Patient’s perception of understanding medications 16
![Phase 2: Process Measures Provider Satisfaction: Comments • …[patient] was very happy with her Phase 2: Process Measures Provider Satisfaction: Comments • …[patient] was very happy with her](http://slidetodoc.com/presentation_image_h2/bf306b6cc0fdd3b6679ff54c0dfe79ea/image-17.jpg)
Phase 2: Process Measures Provider Satisfaction: Comments • …[patient] was very happy with her visit with Gretchen (pharmacist). She found the medicine chart Gretchen made for her very helpful. • Sometimes in a busy clinic it can be challenging for Zack (pharmacist) and/or Amy (care manager) to find me or vice versa to pass along pertinent info point-ofcare. However, it is a huge improvement. 17
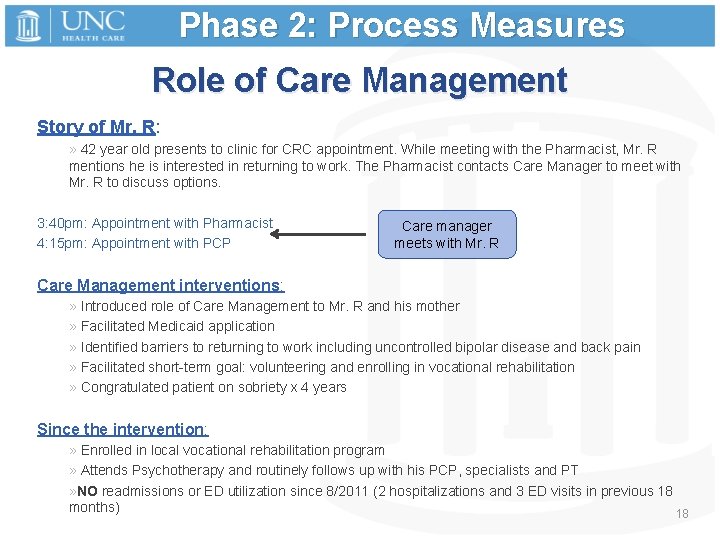
Phase 2: Process Measures Role of Care Management Story of Mr. R: » 42 year old presents to clinic for CRC appointment. While meeting with the Pharmacist, Mr. R mentions he is interested in returning to work. The Pharmacist contacts Care Manager to meet with Mr. R to discuss options. 3: 40 pm: Appointment with Pharmacist 4: 15 pm: Appointment with PCP Care manager meets with Mr. R Care Management interventions: » Introduced role of Care Management to Mr. R and his mother » Facilitated Medicaid application » Identified barriers to returning to work including uncontrolled bipolar disease and back pain » Facilitated short-term goal: volunteering and enrolling in vocational rehabilitation » Congratulated patient on sobriety x 4 years Since the intervention: » Enrolled in local vocational rehabilitation program » Attends Psychotherapy and routinely follows up with his PCP, specialists and PT » NO readmissions or ED utilization since 8/2011 (2 hospitalizations and 3 ED visits in previous 18 months) 18
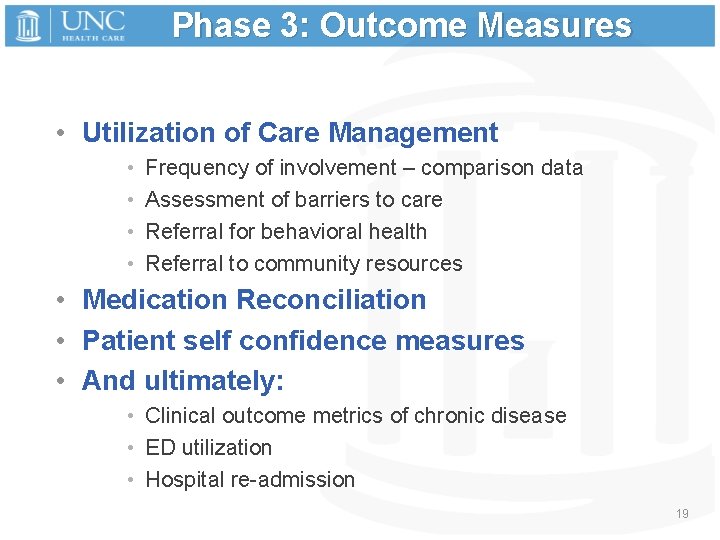
Phase 3: Outcome Measures • Utilization of Care Management • • Frequency of involvement – comparison data Assessment of barriers to care Referral for behavioral health Referral to community resources • Medication Reconciliation • Patient self confidence measures • And ultimately: • Clinical outcome metrics of chronic disease • ED utilization • Hospital re-admission 19
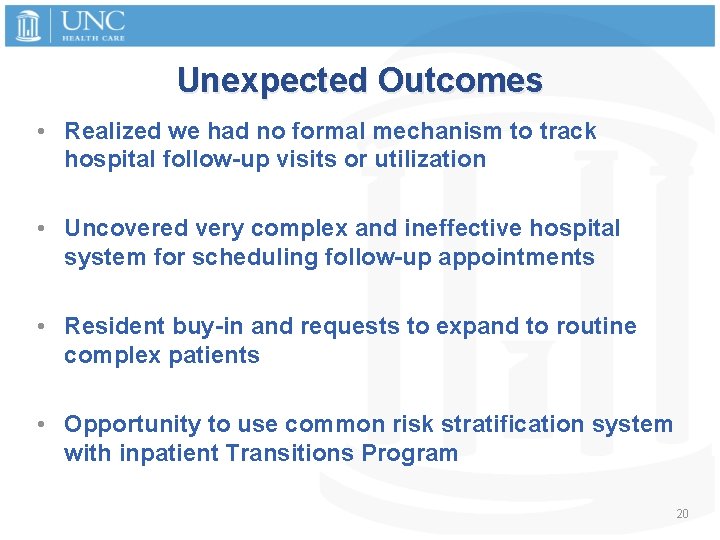
Unexpected Outcomes • Realized we had no formal mechanism to track hospital follow-up visits or utilization • Uncovered very complex and ineffective hospital system for scheduling follow-up appointments • Resident buy-in and requests to expand to routine complex patients • Opportunity to use common risk stratification system with inpatient Transitions Program 20
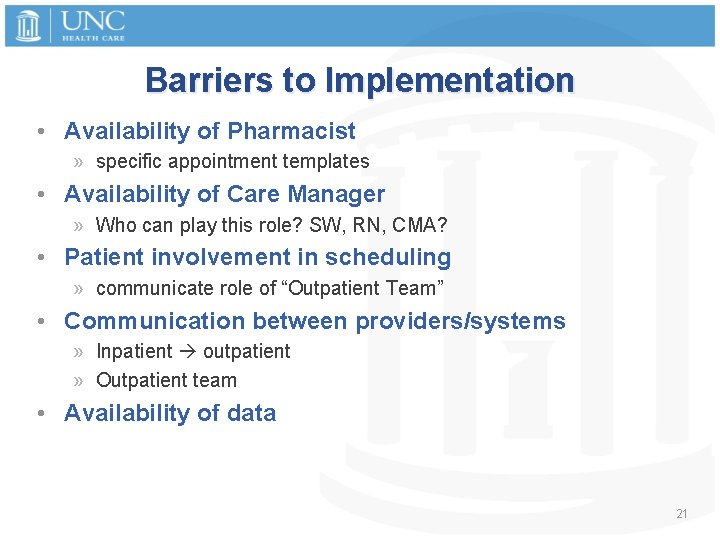
Barriers to Implementation • Availability of Pharmacist » specific appointment templates • Availability of Care Manager » Who can play this role? SW, RN, CMA? • Patient involvement in scheduling » communicate role of “Outpatient Team” • Communication between providers/systems » Inpatient outpatient » Outpatient team • Availability of data 21
Discussion • How can our Patient Centered Medical Homes bridge that gap between inpatient Transitions Programs and outpatient practices? • What barriers to quality improvement project implementation exist in your program ? • What barriers exist in your program for developing an interdisciplinary outpatient based transitions program? 22
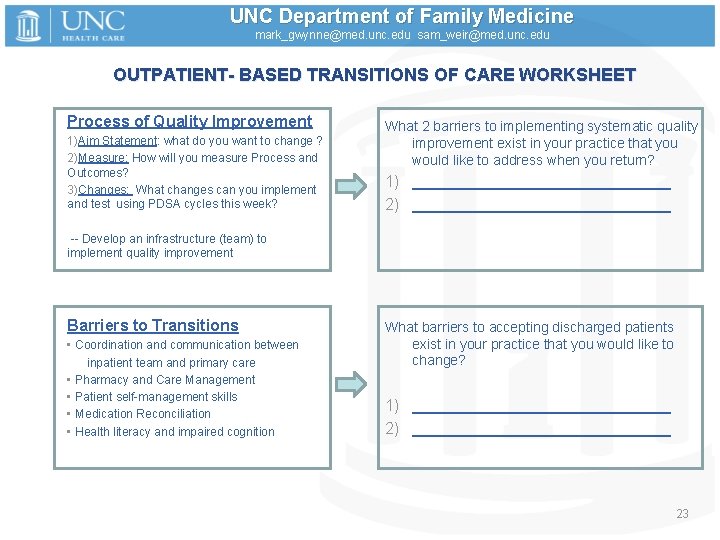
UNC Department of Family Medicine mark_gwynne@med. unc. edu sam_weir@med. unc. edu OUTPATIENT- BASED TRANSITIONS OF CARE WORKSHEET Process of Quality Improvement 1)Aim Statement: what do you want to change ? 2)Measure: How will you measure Process and Outcomes? 3)Changes: What changes can you implement and test using PDSA cycles this week? What 2 barriers to implementing systematic quality improvement exist in your practice that you would like to address when you return? 1) _______________ 2) _______________ -- Develop an infrastructure (team) to implement quality improvement Barriers to Transitions • Coordination and communication between inpatient team and primary care • Pharmacy and Care Management • Patient self-management skills • Medication Reconciliation • Health literacy and impaired cognition What barriers to accepting discharged patients exist in your practice that you would like to change? 1) _____________________________ 23
- Slides: 23