ACNE VULGARIS ROSACEA AND PERIORAL DERMATITIS Dr M


- Slides: 21
ACNE VULGARIS, ROSACEA AND PERIORAL DERMATITIS Dr M. W. Mokgatle F. C. Derm (S. A. ) Consultant 1 Military Hospital 2012 1
Acne Vulgaris • • Disease of the pilosebaceous unit. Affects both sexes. Onset common around puberty (hormonal growth spurt). Duration and intensity of the disease vary. 2

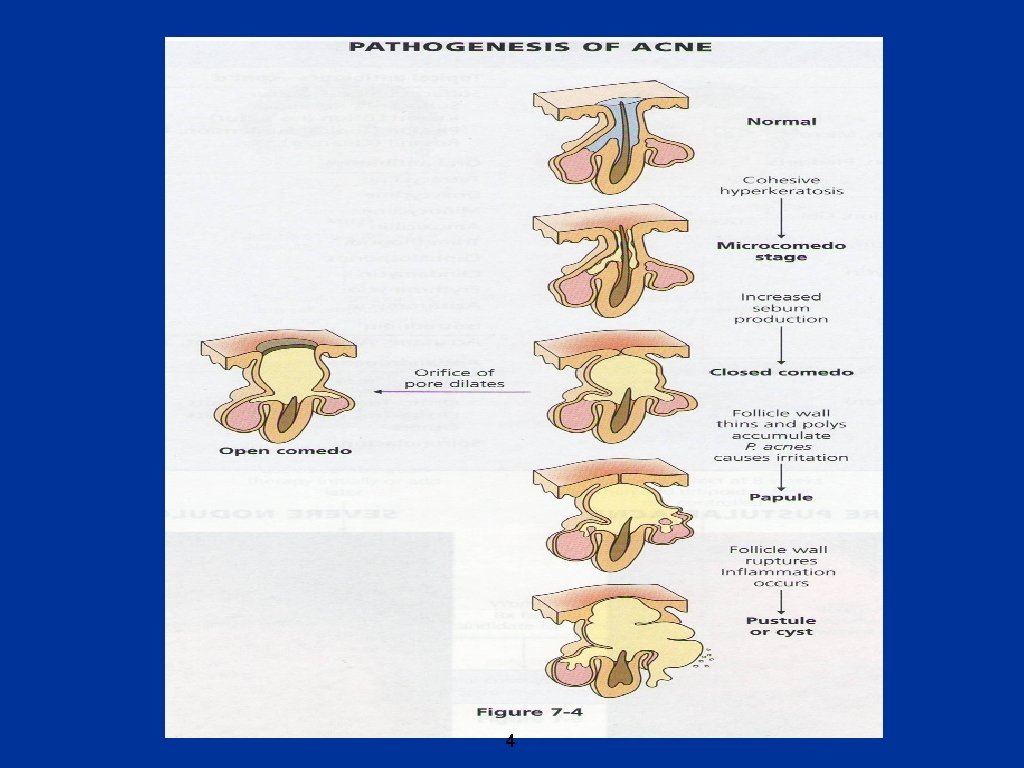
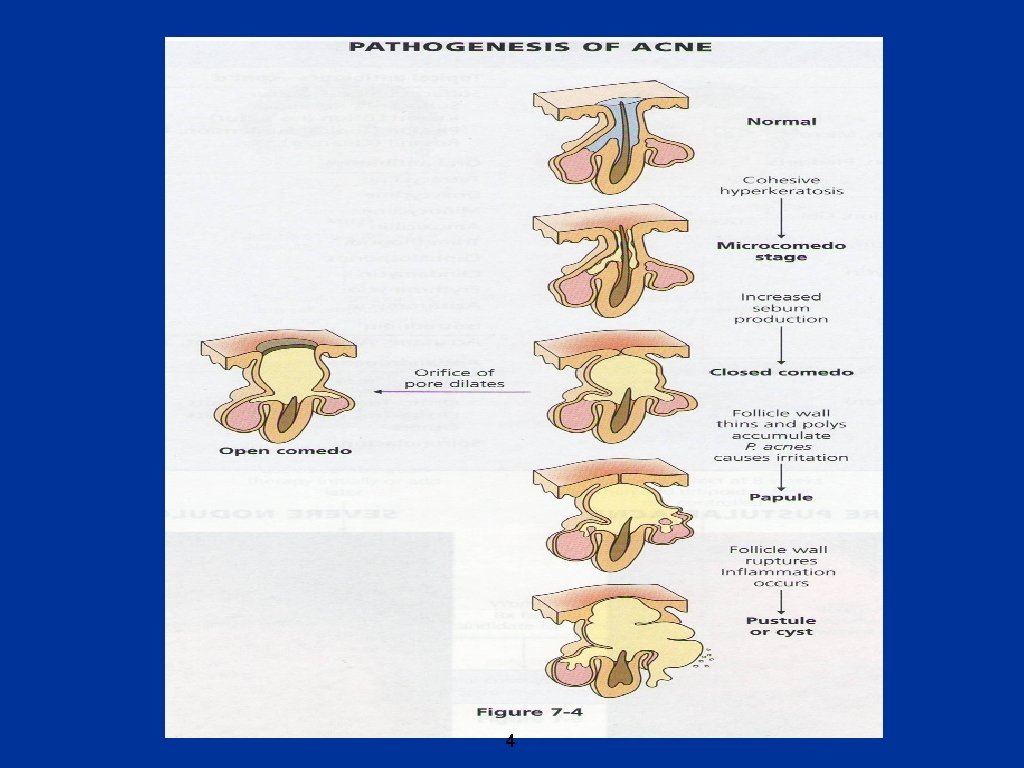
Aetiopathogenesis • • • 4 main causes. Follicular/ductal hyperkeratosis – plug – microcomedones. Increased sebum production (androgenic stimulation) - comedones. Propionebacterium acnes (P. acnes) proliferation – papules/pustules (increased sebum). Inflammation – nodules/cysts - P. acnes metabolises sebum, producing free fatty acids – inflammation. 3
4
Clinical presentation • • Affects face, upper chest, back and upper outer arms (areas with large and numerous sebaceous glands). Non inflammatory lesions – closed (white) and open (black) comedones. Inflammatory lesions – papules, pustules, nodules and cysts. Severity grading based on lesion count/type – mild, moderate and severe. 5
Acne and Diet • • • Diet - controversial, but some authors now believe it to play a role in acne. High glycaemic index foods e. g. breads, doughnuts, cakes, chips, french fries, candy and chocolate. Increased blood glucose – increased insulin production – increased hormone production including androgen – increased sebum – acne. Others – dairy products. 6
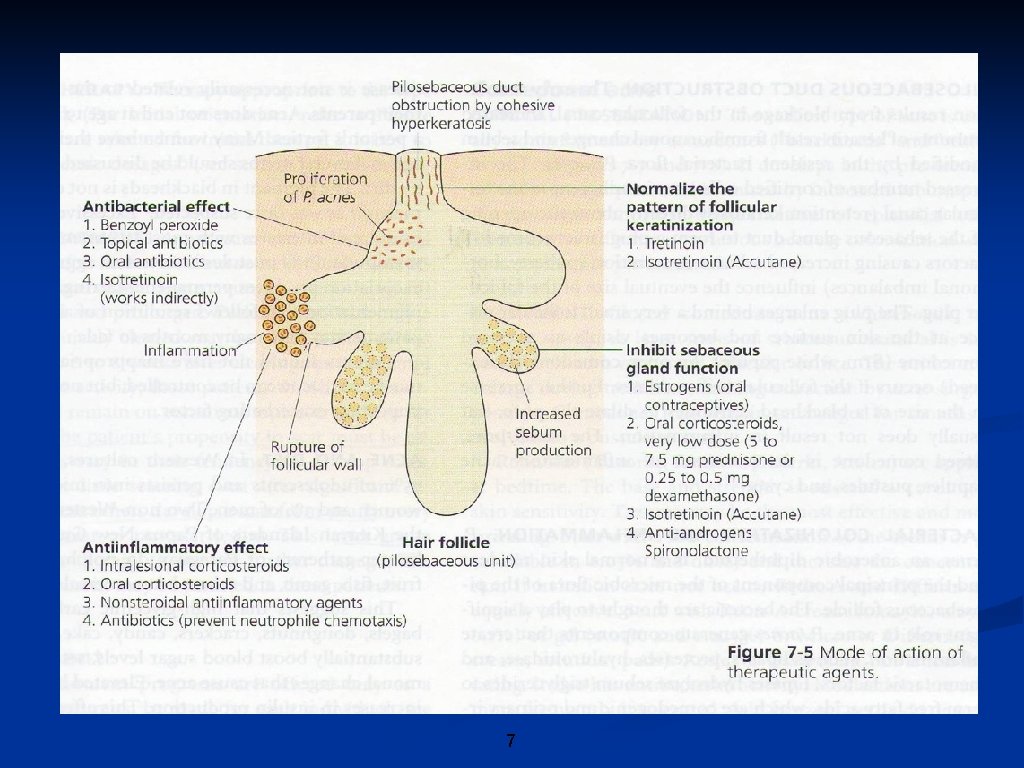
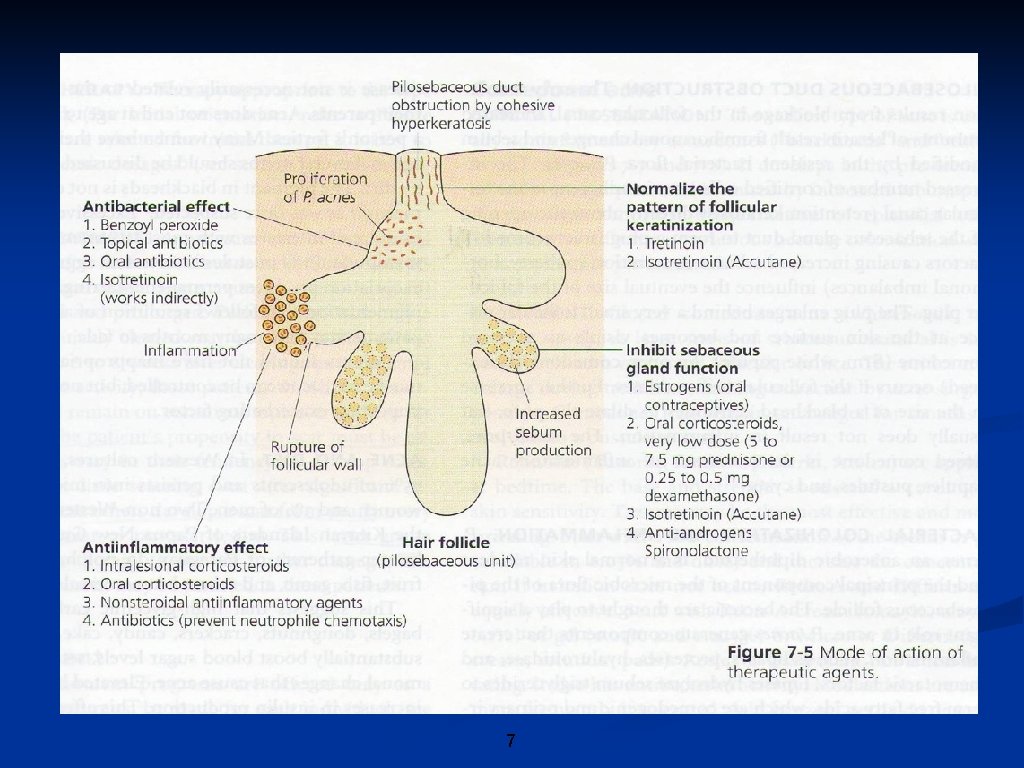
7
Treatment • • • Mild – topical medications. Topical retinoids – retin-A, isotrex, iliotycin. A cream, differin. Benzoyl peroxide – benzac, brevoxyl, panoxyl. Topical antibiotics – erythromycin, clindamycin. Topical resorcinol, sulfar, and salicylic acid 8
Treatment • • Moderate acne – combination of topical and oral medication. 2 topical agents + oral antibiotics or oral contraceptives. Oral antibiotics – (doxycycline, minocycline, tetracycline, limecycline), erythromycin, bactrim, dapsone. Oral contraceptives – use in females ONLY. Diane, yasmin, yaz (contain anti-androgens cyproterone acetate/drosperinone + ethinyl oestradiol). 9
Treatment • • Severe nodulocystic acne. Oral isotretinoin. Cumulative dose 120 mg/kg divided to 0, 5 -1 mg/kg/month. Teratogenic. Various side effects - commonly mucocutaneous. 10
Mode of Action of Therapeutic Agents • • 1. Normalization of follicular hyperkeratosis: Retinoids 2. Inhibition of sebaceous hypersecretion: Oestrogen/Anti-androgens, Retinoids 3. Antibacterial effect: Benzoyl peroxide, Antibiotics, Retinoids 4. Anti-inflammatory effects: Benzoyl peroxide, Antibiotics, Retinoids 11
Acne and complications • • • Ice-pick and depressed scars. Hyperpigmented marks (type iv-vi skin). Hypertrophic scars and keloidal. Acne may lead to low self-esteem, social withdrawal. Important to treat early to prevent/reduce complications. 12
Other acne types • • • Drug-induced – steroids, anti-convulsants, iodides, bromides, lithium. Neonatal acne – maternal androgens. Cosmetic acne. Pomade acne – greasy hair products. Occupational acne – industrial solvents, oils, chlorinated hydrocarbons. Mechanical acne – occlusive bands, straps, helmets. 13
Rosacea • • Chronic inflammatory acne-like eruption – mid face (cheeks, nose, forehead, chin). Mainly Caucasian women aged 30 - 40 yrs. Rare and usually severe in men (rhinophyma). Usually affects cheeks, chin 14
Aetiopathogenesis • • • Abnormal vasomotor response to heat and other stimuli – flushing. Hot beverages and sunlight exposure Alcohol – induces flushing. Prolonged use of topical corticosteroids. ? Demodex folliculorum (mites). Chronic vasodilatation and oedema telangiectasia, and fibrosis. 15
Clinical features • • • 4 main stages: Erythema. Telangiectasia. Erythematous papules and/or pustules. Hypertrophy (rhinophyma). May get eye involvement (stinging, burning, gritty). 16

Differential diagnosis • • Malar erythema: SLE –erythematous stage. Acne vulgaris: look for comedones, cysts etc 17
Treatment • • • Avoidance of flushing triggers. Sunscreens daily. Mild cases – topical metronidazole or benzoyl peroxide. Oral tetracyclines the most effective. Resistant cases – isotretinoin. Often recurs on stopping Rx – low dose maintanance suppressive Rx oral tetracyclines. Rhinophyma – surgical (dermabrasion, laser CO 2, electrosurgery). Telangiectasia – pulsed dye laser. Cosmetic camouflage: erythema/telangiectasia 18
Perioral Dermatitis • • • A distinctive eruption – discrete erythematous papules and pustules in the perioral area, sparing the vermilion border of the lips. Resembles acne. Relatively common Affects mostly women aged 23 – 35 yrs. May also involve periocular area. 19
Aetiology • • • Unknown. Strong, fluorinated topical corticosteroids. Fluorinated dentifrices – toothpaste/tooth powder. Demodex folliculorum. Excessive use of moisturizing creams and lipsticks 20
Treatment • • Responds well to tetracyclines (250 mg – 1 g /day) Doxycycline, minocycline, erythromycin. Topical metronidazole/Adapalene/skinoren. Stop use of topical/inhaled corticosteroids 21